Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Electron microscopy description | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Bychkov A. Hobnail. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidpapillaryhobnail.html. Accessed May 14th, 2024.
Definition / general
- Aggressive variant of papillary thyroid carcinoma (PTC) characterized by predominance of cells with a hobnail appearance often arranged in micropapillary pattern (Am J Surg Pathol 2017;41:854)
- Hobnail cell appearance designates a peculiar loss of polarity with apically placed bulging nuclei
- Micropapillary pattern is characterized by cancer cells loosely arranged in small clusters lacking fibrovascular cores, lined by hobnail, cuboidal or flat epithelium often with loss of polarity and cohesiveness
- Micropapillary pattern of tumor is recognized in several organs (bladder, breast, colon, gallbladder, kidney, lung, ovary, pancreas and parotid gland), being associated with poor clinical outcome (Rev Endocr Metab Disord 2016;17:521)
- Originally established as distinct PTC variant by Asioli et al. in 2010 (Am J Surg Pathol 2010;34:44)
- Hobnail pattern with micropapillary structures was described by Kakudo group as loss of cellular polarity / cohesiveness in early 2000s (Pathol Int 2003;53:204, J Clin Pathol 2004;57:1041, Cancer Sci 2008;99:1908)
- 70+ cases described (Rev Endocr Metab Disord 2016;17:521)
Essential features
- Recently described rare variant of PTC with aggressive behavior (extrathyroidal extension, nodal and distant metastasis) and relatively poor prognosis (lower long term survival)
- Microscopically characterized by micropapillary growth pattern and hobnail appearance of cells due to apically placed bulging nuclei
- Diagnosis of PTC hobnail variant requires at least 30% of hobnail-micropapillary pattern in the tumor, although minor hobnail-micropapillary features (5 - 30%) are of significance and should be noted in pathology report
Terminology
- Hobnail variant of PTC = Hobnail PTC = PTC with prominent hobnail features
- Previously described as PTC with micropapillary features, micropapillary carcinoma, micropapillary-hobnail variant and loss of cellular polarity / cohesiveness variant
- Term "micropapillary carcinoma" is often confused with papillary microcarcinoma, an indolent thyroid tumor, hence "hobnail" designator is preferred (Am J Surg Pathol 2013;37:1215)
- Hobnail histology is also more consistently observed than the micropapillary pattern, discounting the value of the latter title (Am J Surg Pathol 2017;41:854)
Epidemiology
- Rare tumor, < 1% of all PTC
- Range in PTC series from 0.3% (South Korea) to 2.7% (Southern Italy) (Int J Clin Exp Pathol 2015;8:7988, Rev Endocr Metab Disord 2016;17:521)
- Older patients: mean age 57 years, range 17 - 87 (Rev Endocr Metab Disord 2016;17:521)
- F:M about 3:1, similar to all PTC
Pathophysiology
- Hobnail PTC is considered a moderately differentiated thyroid carcinoma placed between well differentiated classic PTC and poorly differentiated thyroid cancer (Am J Surg Pathol 2015;39:260, Am J Surg Pathol 2017;41:854)
- BRAF mutation is a likely driver, followed by second hits in TP53, TERT promoter, PIK3CA or CTNNB1 (Endocr Relat Cancer 2017;24:107)
- Associated events are epithelial-mesenchymal transition (Cancer Lett 2009;281:188) and activation of mTOR pathway (J Clin Exp Pathol 2013;4:152), both characteristic for aggressive thyroid cancer
Clinical features
- Neck mass, sometimes with compressive symptoms (dyspnea, dysphagia, hoarseness) (Am J Surg Pathol 2010;34:44)
- Almost half are incidental findings (Int J Clin Exp Pathol 2015;8:7988)
- Aggressive tumor with relatively poor prognosis (Thyroid 2014;24:958):
- Extrathyroidal extension
- Lymph node metastasis in up to 75%
- Distant metastases in up to 40% (lung, brain, bones)
- Local recurrence
- Progression to poorly differentiated thyroid cancer
- Advanced clinical stage (AJCC Stage III or IV) at presentation
- Increased mortality rates compared to classic PTC in most but not all cases
Diagnosis
- Diagnostic workup is similar to any thyroid mass / nodule:
- Ultrasound with FNA
- CT scan may be useful in locally advanced disease to evaluate extrathyroidal extension and lymph node metastases
- Hobnail PTC is a pathological diagnosis rendered on surgical specimens
- FNAC can suspect hobnail variant and influence surgical tactics
- PTC hobnail variant requires at least 30% of tumor having hobnail-micropapillary pattern
- Minor hobnail micropapillary features (5 - 30%) should also be correctly identified and stated in pathology report due to potential aggressive behavior (Hum Pathol 2012;43:1596)
Radiology description
- Sonography: oval, solid or heterogeneous, coarsened hypoechoic and vascular mass with irregular margins, often accompanied by ipsilateral cervical lymphadenopathy (J Clin Exp Pathol 2013;4:152, Diagn Cytopathol 2013;41:757)
Prognostic factors
- Hobnail PTC itself indicates propensity for higher grade transformation (Am J Surg Pathol 2015;39:260)
- Local recurrence rate is 23%, lymph node metastasis 60 - 75%, distant metastasis 25 - 40%
- Disease specific survival rates are 83%, 71% and 54% at 5, 10 and 20 years after surgery, respectively (Int J Clin Exp Pathol 2015;8:7988)
- Overall survival rates are 69% and 64% at 5 and 10 years, respectively (Endocr Relat Cancer 2017;24:107)
- Increased mortality risk in patients harboring multiple mutations, usually BRAF with TP53 or PIK3CA (Thyroid 2014;24:958)
Case reports
- 17 year old girl with PTC hobnail variant diagnosed by FNA (J Clin Exp Pathol 2013;4:152)
- 26 year old woman with hobnail PTC suspected on FNA (Diagn Cytopathol 2015;43:990)
- 31 year old woman with PTC hobnail variant (Diagn Cytopathol 2013;41:757)
- 53 year old woman and 62 year old man with hobnail PTC which progressed to anaplastic carcinoma (Am J Surg Pathol 2017;41:854)
- 54 year old woman with preoperative FNA (Am J Clin Pathol 2015;142:A276)
- 57 year old man with PTC hobnail variant studied by FNA (Acta Cytol 2012;56:560)
- 57 year old man with recurrent tumor (Thyroid 2009;19:535)
- 84 year old woman with hobnail PTC presenting as superior vena cava syndrome (Thyroid 2016;26:129, Poster 353)
Treatment
- Total thyroidectomy with neck lymph node dissection followed by TSH suppression therapy and radioactive iodine treatment (Thyroid 2018;28:96)
Gross description
- Mean size 3.5 cm (larger than average PTC), range 0.5 - 11.0 cm (Int J Clin Exp Pathol 2015;8:7988)
- Infiltrative appearance
- Multiple nodules in one or both thyroid lobes (Am J Surg Pathol 2010;34:44)
- Rarely a single encapsulated nodule
Microscopic (histologic) description
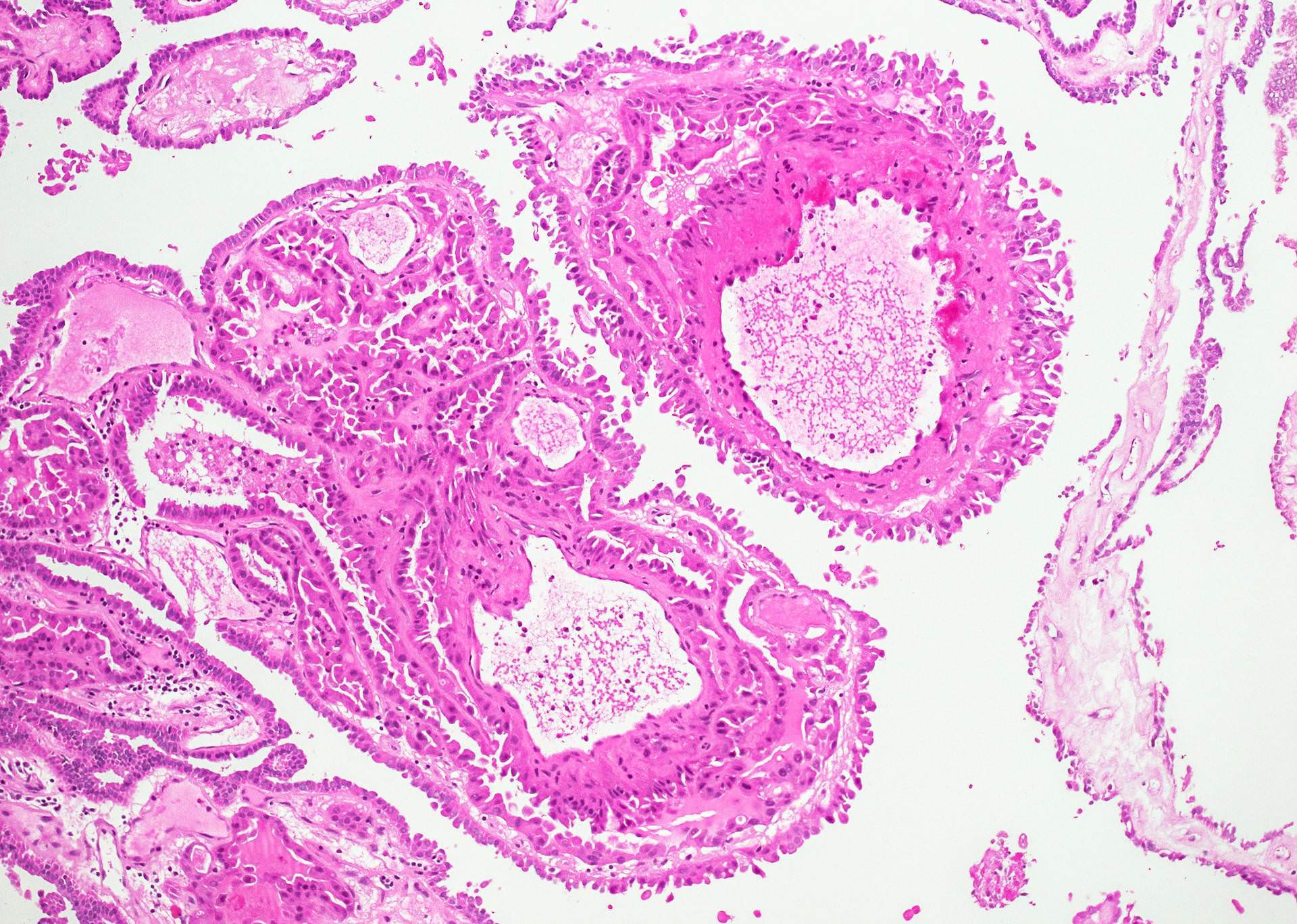
- Histologically, this variant has 3 distinctive features (Am J Surg Pathol 2015;39:260):
- Micropapillae lacking true fibrovascular cores
- Hobnail cells with apically placed protruding nuclei and eosinophilic cytoplasm
- Marked loss of cellular cohesion
- Main architectural patterns (Am J Surg Pathol 2010;34:44):
- Papillary pattern is the most common, with variably sized edematous papillae having vascular cores, rare psammoma bodies and lined by discohesive hobnail epithelium 1 - 4 cells thick
- Clustered pattern represented by micropapillary structures without fibrovascular cores, lined by hobnail cells
- Follicular pattern is rare with variably sized follicles lined by hobnail cells and little to no colloid
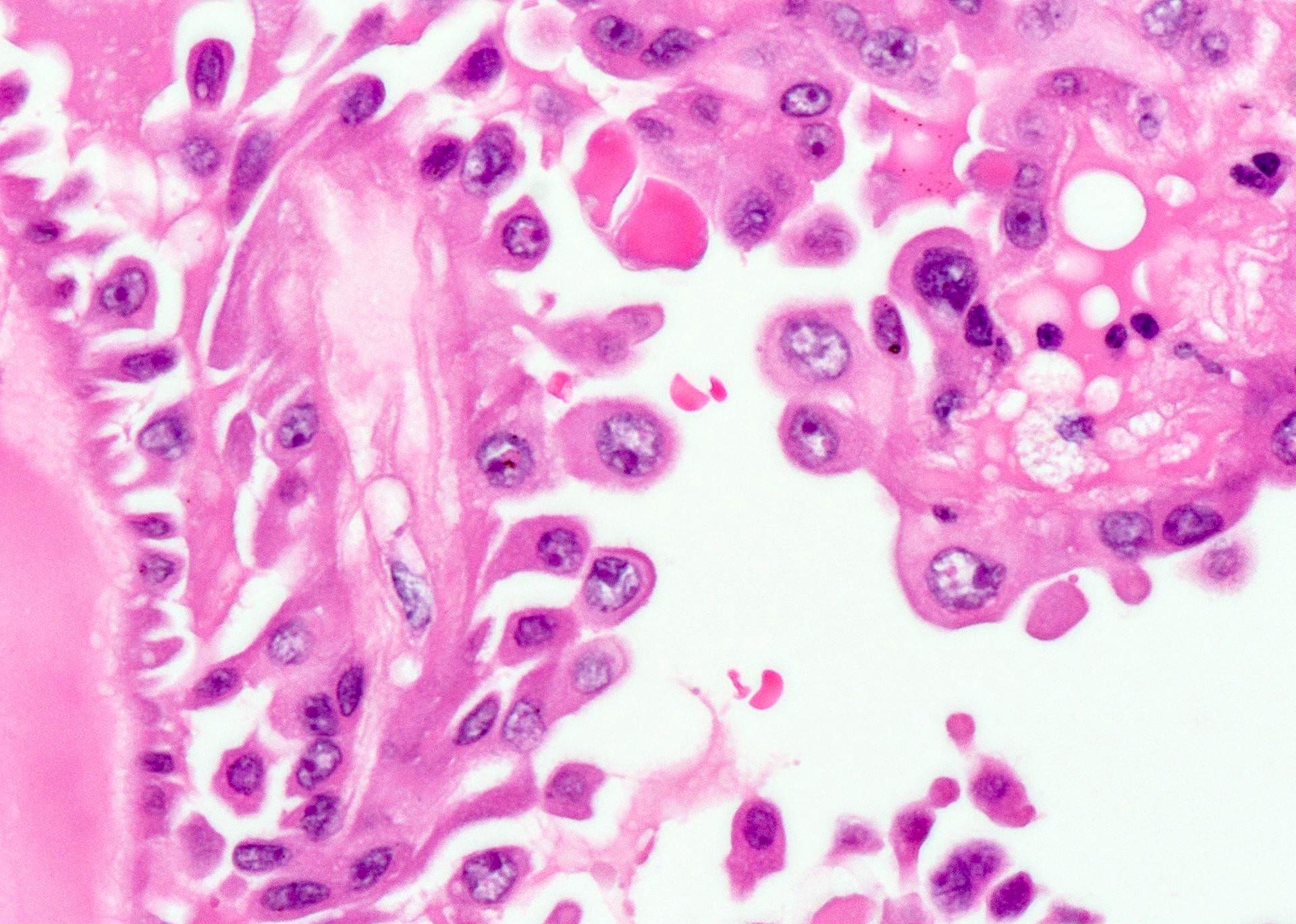
- Hobnail cells:
- Cells with apically placed nuclei and protrusion of the apical surface that gives a hobnail appearance
- Synonyms of hobnailing: tufting, bulging, apocrine snouting; also matchstick, comet tail, teardrop appearance
- Increased N:C ratio
- Characteristic PTC nuclear features are less prominent compared to classic variant
- Dense eosinophilic cytoplasm with well defined cell borders, similar to oncocytes
- Apical position of nuclei (inversion or loss of polarity) is often accompanied by discohesiveness of the epithelial layer with cell shedding
- Cells with apically placed nuclei and protrusion of the apical surface that gives a hobnail appearance
- Aggressive morphology:
- Extensively invasive cancer with extrathyroidal extension and multiple areas of vascular invasion
- Moderate to marked cellular pleomorphism
- Increased mitotic figures (often ≥ 3 per 10 HPF, reported mean 2.1, range 0 - 9), including atypical mitoses (Int J Clin Exp Pathol 2015;8:7988)
- Necrosis is rare
- Focal transformation into poorly differentiated and even anaplastic thyroid cancer (Am J Surg Pathol 2015;39:260, Am J Surg Pathol 2017;41:854)
- Proportion of hobnail component:
- Presence of at least 30% of cells with hobnail-micropapillary features is required to entitle a tumor as PTC hobnail variant
- In original series, most had 50 - 100% of hobnail component (Am J Surg Pathol 2010;34:44)
- If present, minor hobnail-micropapillary component (5 - 30%) should be correctly identified and stated in the pathology report, because it has adverse prognostic significance (Hum Pathol 2012;43:1596, Hum Pathol 2013;44:320, Endocrine Abstracts 2013;32:P1105, Am J Surg Pathol 2015;39:260, Thyroid 2016;26:129, Poster 198)
- Concomitant patterns are usually represented by classic, tall cell and oncocytic PTC, rarely by PTC follicular and solid variants; all of them can be considered as precursor lesions
- Number of sections studied is critical for evaluation of PTC with hobnail cells, thus increase in the number of sections routinely studied, especially sampling at the tumor infiltrating edge, can likely result in a higher incidence of detection of the hobnail PTC (Hum Pathol 2013;44:320)
- Background: often multinodular goiter or chronic thyroiditis (Rev Endocr Metab Disord 2016;17:521), rarely microcarcinoma (Diagn Cytopathol 2015;43:990)
- Nodal and distant metastases usually preserve hobnail pattern, sometimes may progress toward anaplastic carcinoma (Am J Surg Pathol 2017;41:854)
Microscopic (histologic) images
Contributed by Andrey Bychkov, M.D., Ph.D.
Images hosted on other servers:
Cytology description
- Aspirate is highly cellular with scant colloid and bloody background (Hum Pathol 2013;44:320)
- Patterns:
- Papillary-like clusters with vascular cores, sometimes with central psammoma calcifications (Diagn Cytopathol 2015;43:990)
- Micropapillary groups without fibrovascular cores
- Rarely follicular structures
- Proportion of isolated cells versus clusters can vary
- Hobnail cells:
- Medium sized cells with apically placed nuclei, producing surface bulge resulting in hobnail appearance
- Tapered cytoplasm provides "teardrop" or "comet-like" appearance of hobnail cells (Acta Cytol 2012;56:560)
- Severe crowding, high N:C ratio, dense eosinophilic cytoplasm
- Often more than 50% of tumor cells in smear have hobnail morphology
- Additional nuclear features:
- Multiple soap bubble-like intranuclear inclusions
- Occasional grooves and pseudoinclusions (J Clin Exp Pathol 2013;4:152)
- Variable degree of atypia
- Sometimes mitotic figures
- LBP (liquid based preparation) cytology (Int J Clin Exp Pathol 2015;8:7988):
- Frequent syncytial cell clusters with eccentric nuclei
- Papillary and micropapillary structures are rare than in conventional smears
- Comet-like hobnail cells and multiple soap bubble-like intranuclear inclusions
- Typical nuclear features of PTC
- Most of the cases correspond to the Bethesda VI category (Thyroid 2014;24:958)
Positive stains
- Thyroid specific markers: Thyroglobulin, TTF1
- Markers of thyroid neoplasia: CK19, HBME-1
- Markers of tumor aggressiveness (Endocr Relat Cancer 2017;24:107):
- This immunoprofile is shared with other thyroid tumors, especially aggressive PTC variants
- Ancillary markers (rarely used) (Endocr Relat Cancer 2017;24:107):
- E-cadherin and β-catenin with membranous staining
- MUC1 with characteristic "inside out" pattern in micropapillary component
- EMA - membranous or cytoplasmic
- Cyclin D1 (Am J Surg Pathol 2017;41:854)
- Napsin A expression is often found in micropapillary component, can be a pitfall in differentiating from micropapillary lung adenocarcinoma (Am J Surg Pathol 2013;37:1215)
Electron microscopy description
- Cytoplasm of oncocytic cancer cells is packed with mitochondria (Am J Surg Pathol 2010;34:913)
Molecular / cytogenetics description
- Main: BRAF V600E mutation in most cases (50 - 80%)
- Common: TP53 (55%), TERT promoter (45%), PIK3CA (28%)
- Rare: CTNNB1 (17%), EGFR (11%), AKT1 (6%) and NOTCH1 (6%)
- More than 70% of tumors have concurrent mutations (Endocr Relat Cancer 2017;24:107)
- RET / PTC1 is uncommon, up to 20%, based on one study (Thyroid 2014;24:958)
- No RAS family mutations
- Mutation profile in primary tumor and metastasis is usually maintained
Differential diagnosis
- These PTC variants share papillary histoarchitecture with hobnail variant, however they lack hobnailing (apical tufts) feature:
- Cytology (Hum Pathol 2013;44:320)
- See above PTC variants, all of them lack cytologic features of hobnail appearance and comet-like cells
- Metastases to the thyroid gland with hobnail or micropapillary growth pattern, e.g. serous and clear cell carcinoma of the female genital tract, lung adenocarcinoma with micropapillary and hobnail features, breast micropapillary cancer - these cases can be distinguished by IHC panels (TTF1, thyroglobulin, PAX8, WT1, Napsin A, GATA3, etc.)
- Medullary thyroid carcinoma with discohesive cells: positive for calcitonin
- Florid variant of thyroid papillary hyperplasia: absence of PTC nuclei and hobnailing
- PTC oncocytic variant shares oncocytic (granular eosinophilic cytoplasm) and sometimes micropapillary features with hobnail PTC but it lacks evident hobnailing (> 30%) and loss of cohesiveness
Additional references
Board review style question #1
Which statement is incorrect about hobnail PTC?
- Rare variant of papillary thyroid carcinoma
- Relatively aggressive clinical behavior
- Microscopically characterized by hobnail cells and micropapillary pattern
- Common BRAF V600E, TP53 and TERT promoter mutations
- High mortality
Board review style answer #1
E. High mortality. Hobnail papillary thyroid carcinoma is an unusual and aggressive variant of PTC characterized by predominance of cells with a hobnail appearance often arranged in micropapillary pattern. Despite multiple mutations and frequent nodal (up 75%) and distant (up to 40%) metastases, mortality is relatively low - disease specific survival rates are 80+% and 70+% at 5 and 10 years after surgery.
Comment Here
Reference: Hobnail
Comment Here
Reference: Hobnail
Board review style question #2
What proportion of a hobnail micropapillary pattern in the tumor is required for a diagnosis of PTC hobnail variant?
- 5%
- 10%
- 25%
- 30%
- 50%
Board review style answer #2
D. 30%. The presence of at least 30% of cells with hobnail micropapillary features is mandatory to diagnose a tumor as PTC hobnail variant. Nevertheless, a minor hobnail micropapillary pattern (5 - 30%) has prognostic significance and should be noted in the pathology report.
Comment Here
Reference: Hobnail
Comment Here
Reference: Hobnail
Board review style question #3
What category of the Bethesda System of Reporting Thyroid Cytopathology corresponds best to FNA smears of hobnail PTC with comet-like cells?
- I (non-diagnostic)
- III (AUS/FLUS)
- IV (FN/SFN)
- V (suspicious for malignancy)
- VI (malignant)
Board review style answer #3
E. VI (malignant). Cases with diagnostic hobnail cells are easily placed into the Bethesda VI category.
Comment Here
Reference: Hobnail
Comment Here
Reference: Hobnail