Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Du W, Liao X. Apocrine carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anusapocrinecarcinoma.html. Accessed September 4th, 2025.
Definition / general
- Apocrine carcinoma of the anus is a rare, cutaneous, adnexal neoplasm with apocrine differentiation
- It originates from anogenital mammary-like glands, which are analogous to apocrine glands found in other areas of the skin
Essential features
- Apocrine carcinoma is a rare, cutaneous, adnexal neoplasm with apocrine differentiation occurring in the anogenital area
- It may arise de novo or develop from a pre-existing apocrine adenoma
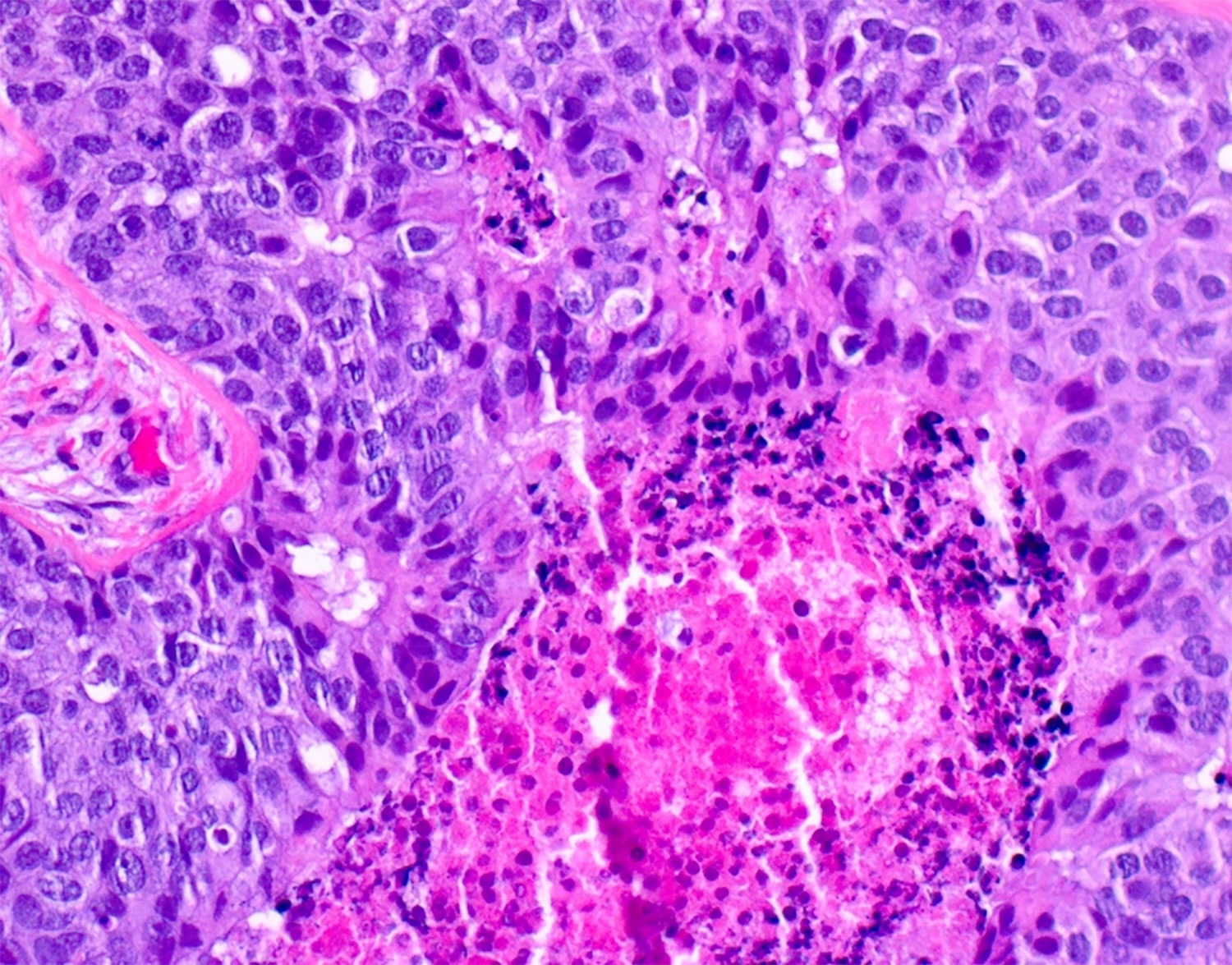
- Histologically, it manifests with unequivocal signs of apocrine secretion, zonal necrosis, cells with pleomorphism and hyperchromatism and increased mitotic activity, including atypical ones
Terminology
- Adnexal carcinoma of skin, apocrine carcinoma, apocrine adenocarcinoma, apocrine gland carcinoma, mammary type tubulocarcinoma of the anogenital area
ICD coding
- ICD-O: 8401/3 - apocrine carcinoma
- ICD-11: 2C33 & XH9L77 - adnexal carcinoma of skin & apocrine adenocarcinoma
Epidemiology
- Extremely rare, with an incidence estimated to be < 0.00001 patients per year (Eur J Cancer Prev 2024;33:77)
- Predominantly affects adults, with slight female predominance
- Often diagnosed in the fifth to seventh decades of life, with a median age of 67 years
Sites
- Axilla and anogenital region are the most common sites
Pathophysiology
- Originates from anogenital apocrine sweat glands or glands with apocrine differentiation
- Associated with genetic alterations, although molecular mechanisms are still being studied
Etiology
- Exact cause of apocrine carcinoma of the skin is unknown
- In the breast, some theories suggest that it may arise from apocrine metaplastic cells, which are often found in breast fibrocystic changes
Clinical features
- Tumor may present as a solitary nodule or multinodular mass (J Surg Case Rep 2020;2020:rjaa463)
- Ulceration and hemorrhage can happen
- Tumor may also present as a perianal mass for several years
Diagnosis
- Diagnosis is based on location and histopathologic findings
Prognostic factors
- Tumor size, depth of invasion and lymph node involvement are key prognostic indicators
- Higher stage at diagnosis is associated with poorer prognosis
- Metastasis can occur in regional lymph nodes in ~40% of cases; less commonly to visceral organs
- In one study including apocrine carcinomas from all sites, 24% of the patients died of metastatic tumor (Am J Surg Pathol 2008;32:682)
- Small, well circumscribed tumors that are easily excised have a good prognosis (Int J Colorectal Dis 2008;23:121, Am J Surg Pathol 2006;30:1193)
- Analogous tumors in the vulva have been reported to respond to tamoxifen therapy (Future Oncol 2012;8:1199)
- Invasive apocrine carcinomas may be classified according to the modified Bloom-Richardson grading system for breast carcinomas (also called the Nottingham system) (Am J Surg Pathol 2008;32:682)
- This grades tumors based on 3 criteria
- Mitotic count (number of mitoses/mm2)
- Degree of pleomorphism (mild, moderate or severe)
- Tubule formation
- A score of 1, 2 or 3 is assigned for each criterion and the 3 scores are combined to give an overall tumor grade of 1, 2 or 3
- Statistically significant differences in survival have been found with grade 3 versus grade 1 - 2 tumors
- This grades tumors based on 3 criteria
Case reports
- 45 year old woman presented with an invasive apocrine carcinoma arising in a benign adenoma in the perianal region (J Clin Pathol 2005;58:217)
- 71 year old man presented with soreness in the anal region for 6 weeks (Am J Dermatopathol 2012;34:438)
- 72 year old woman presented for evaluation of a perianal lesion with persistent drainage that she had noticed for over a year (J Surg Case Rep 2020;2020:rjaa463)
Treatment
- Wide local excision
- Chemotherapy or radiotherapy may or may not be needed
Microscopic (histologic) description
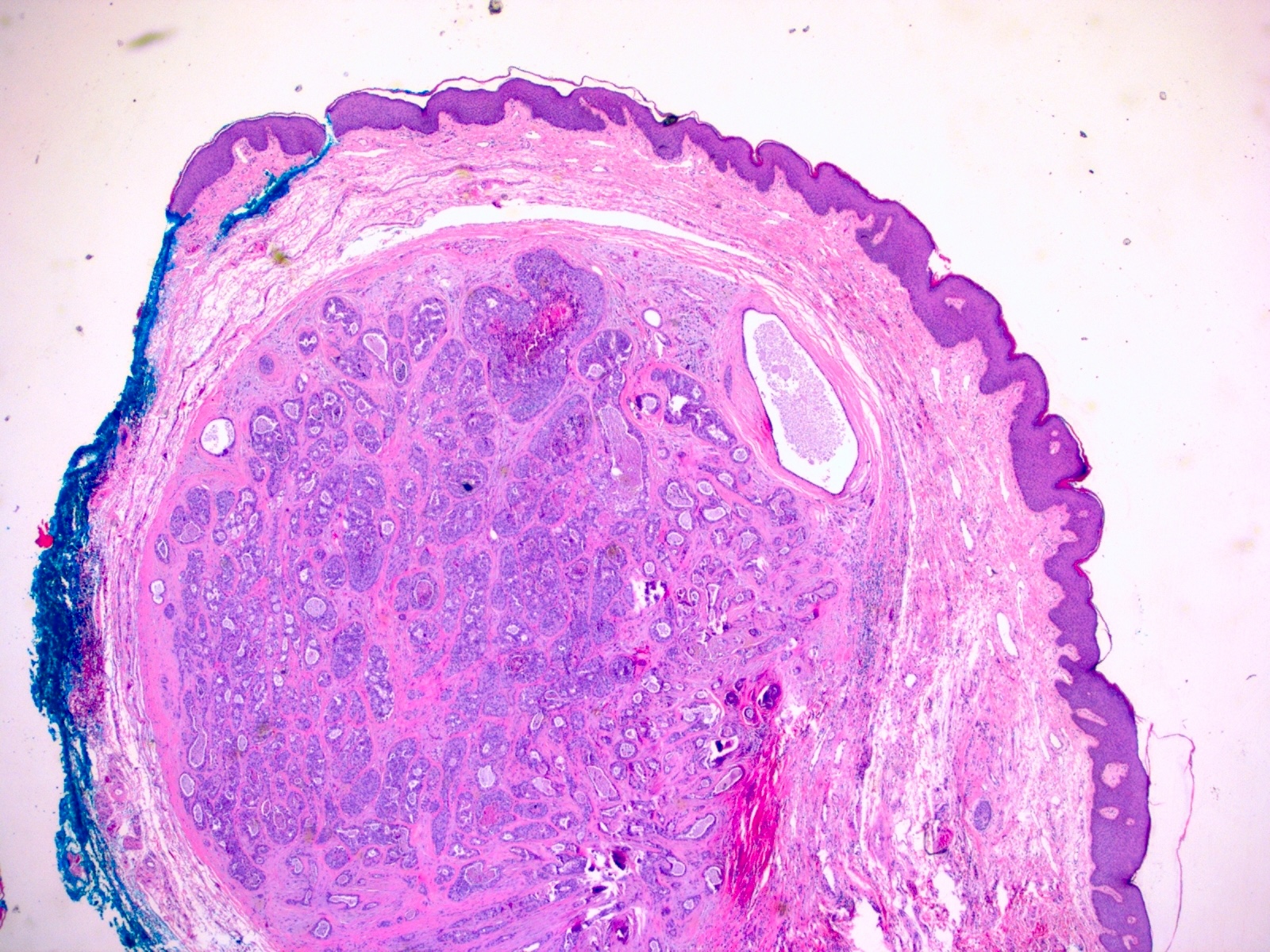
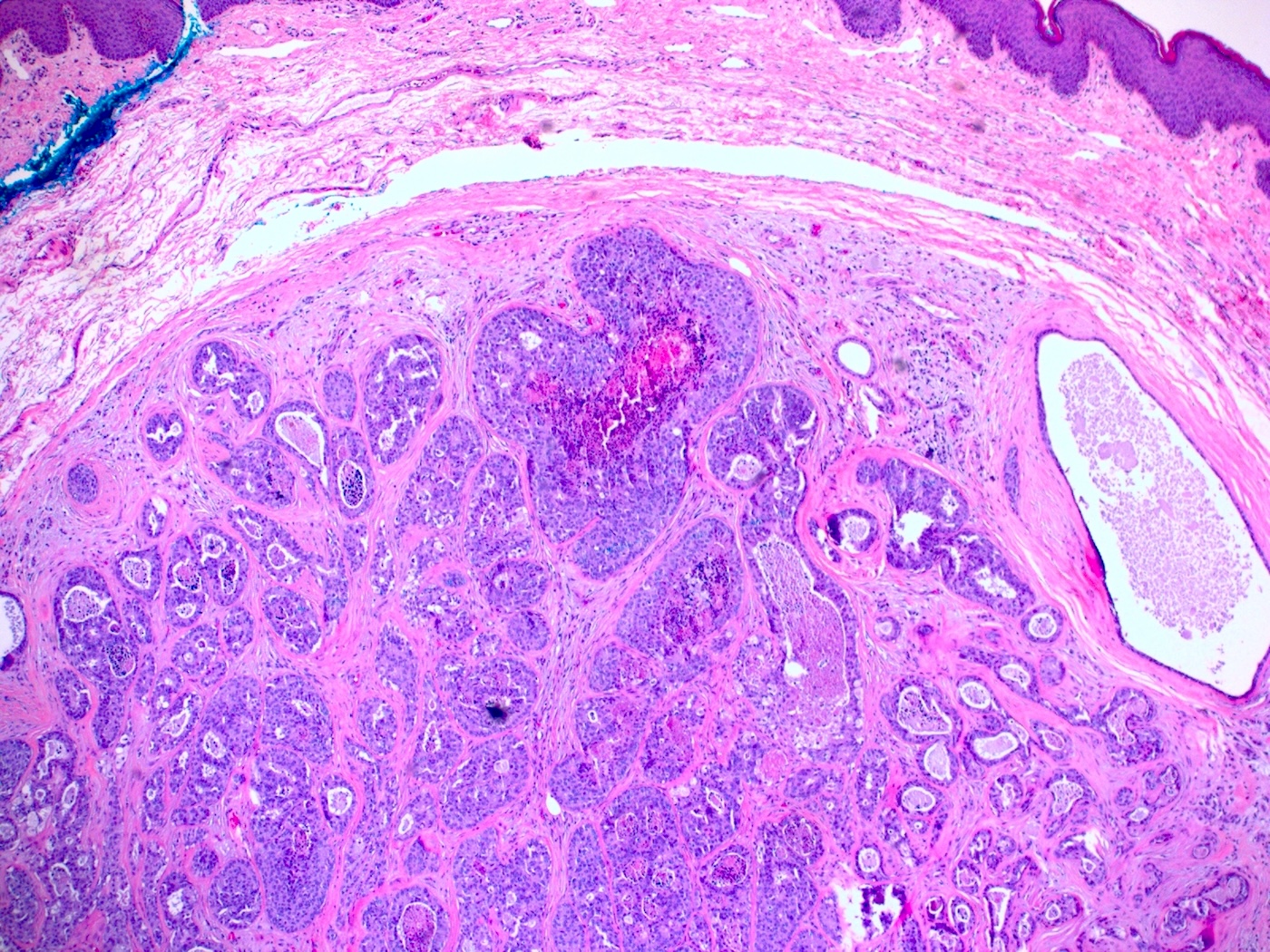
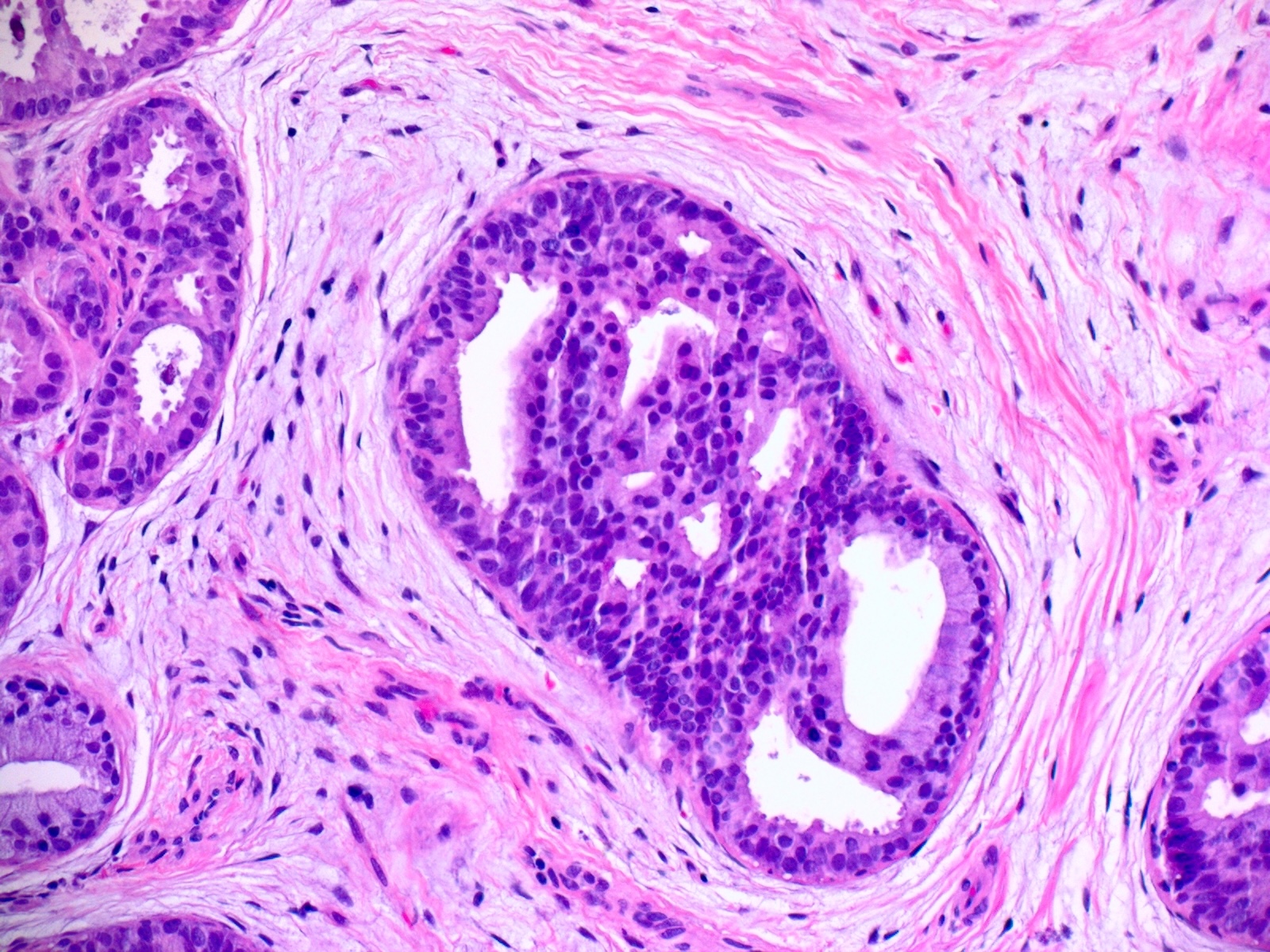
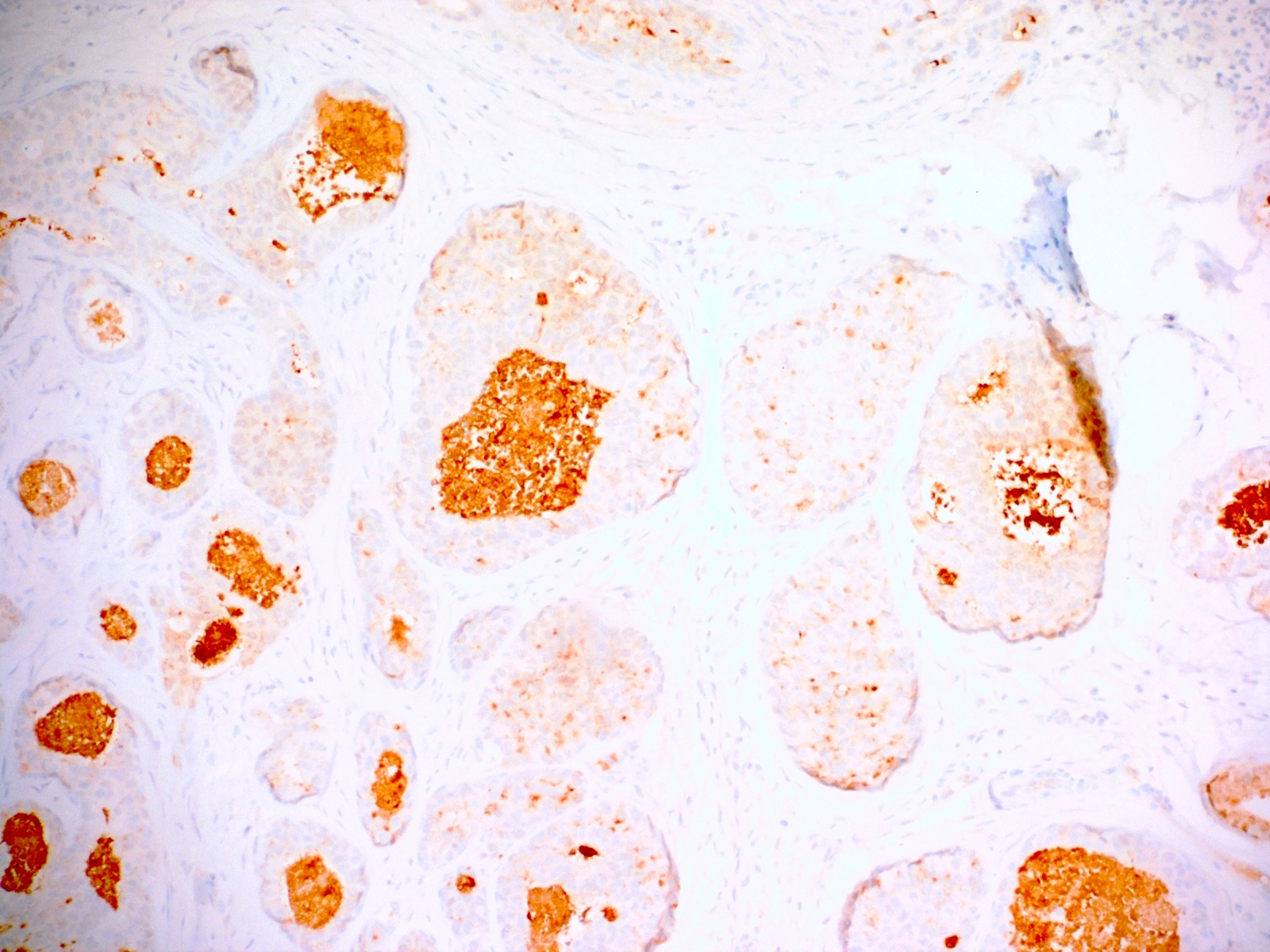
- Tumor is characterized by tubular, ductular and papillary growth patterns, with more solid areas demonstrating significant atypia
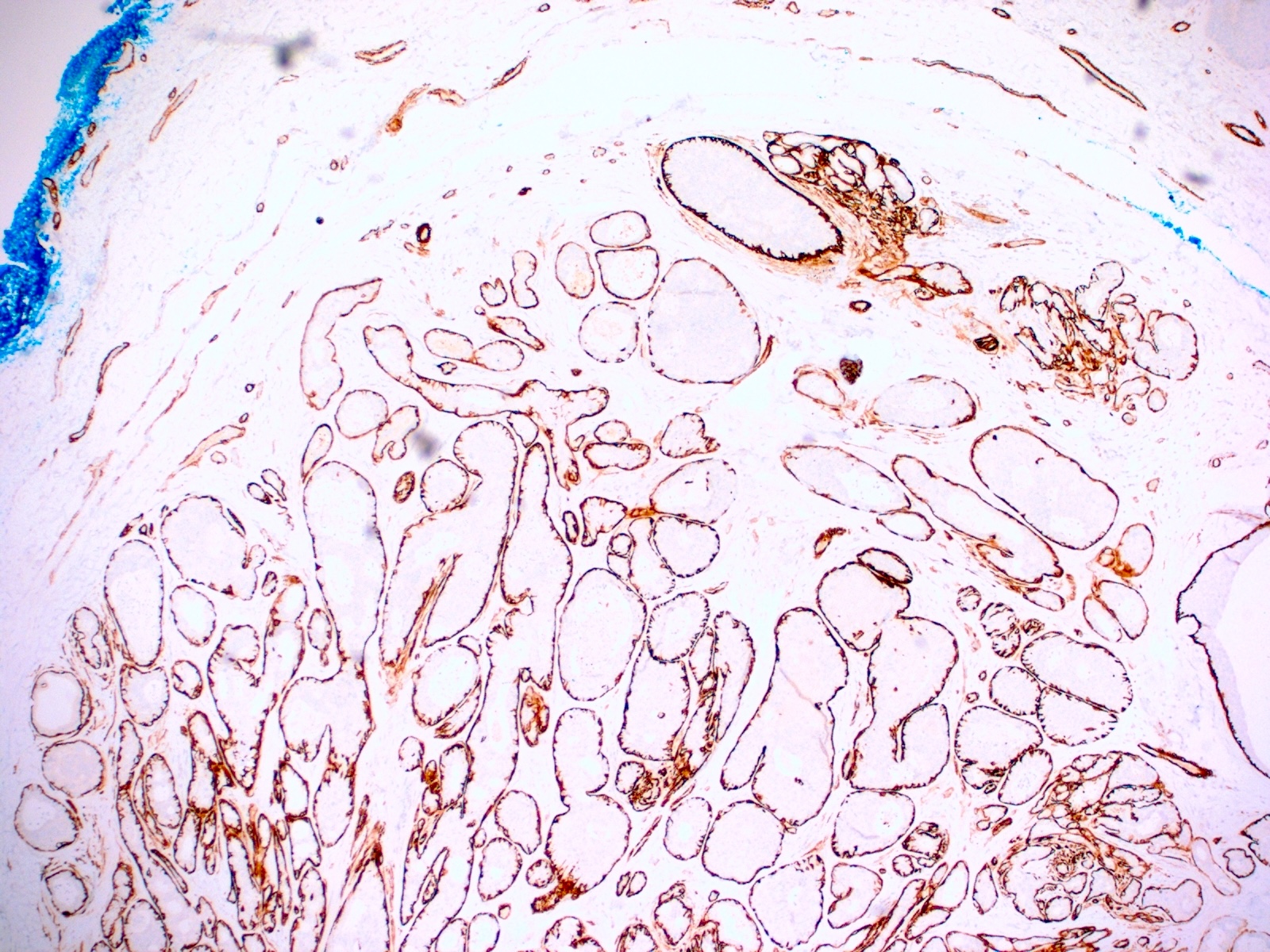
- Peripheral myoepithelial cell layer may or may not be present
- Tumor cells demonstrate features of apocrine differentiation with abundant eosinophilic cytoplasm which may appear either granular or have some vacuolization
- Lumina may be present
- Decapitation secretion is variably present; it is less likely to be seen in poorly differentiated areas of the tumor
- Cytology features variable nuclear pleomorphism and mitotic activity; perineural invasion and intravascular involvement can be seen
- Carcinoma in situ can arise within an adenoma
- In rare cases of fully invasive carcinoma, the adenomatous component or carcinoma in situ lesion may be overgrown by the invasive tumor mass
- Occasionally, an invasive carcinoma may have developed de novo
- Signet ring and histiocytoid variants have been reported, similar to those reported in periorbital neoplasms
- In situ spread of these tumors into the overlying epithelial structures may lead to extramammary Paget disease in the anogenital region (Am J Surg Pathol 2017;41:1053)
Microscopic (histologic) images
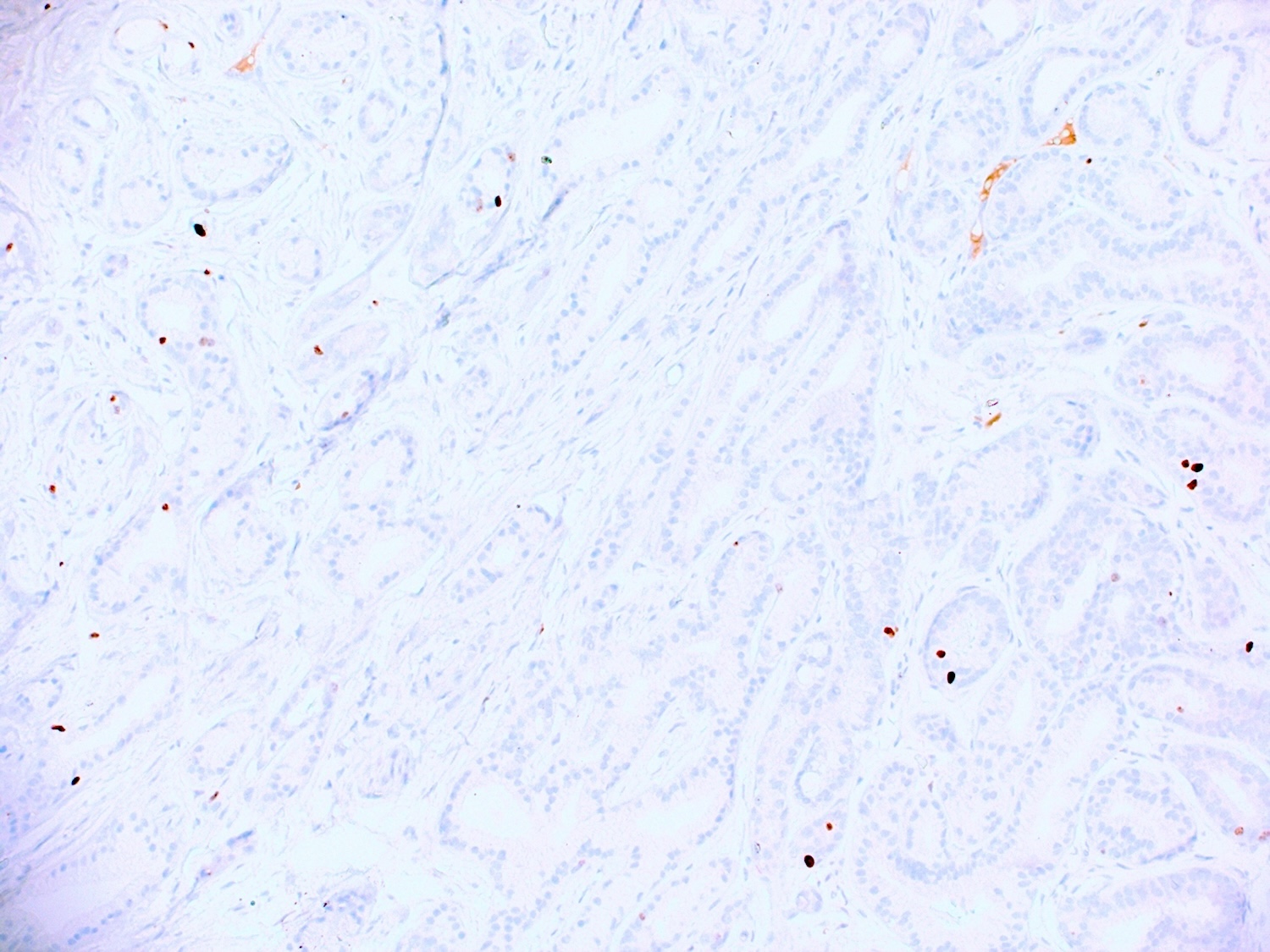
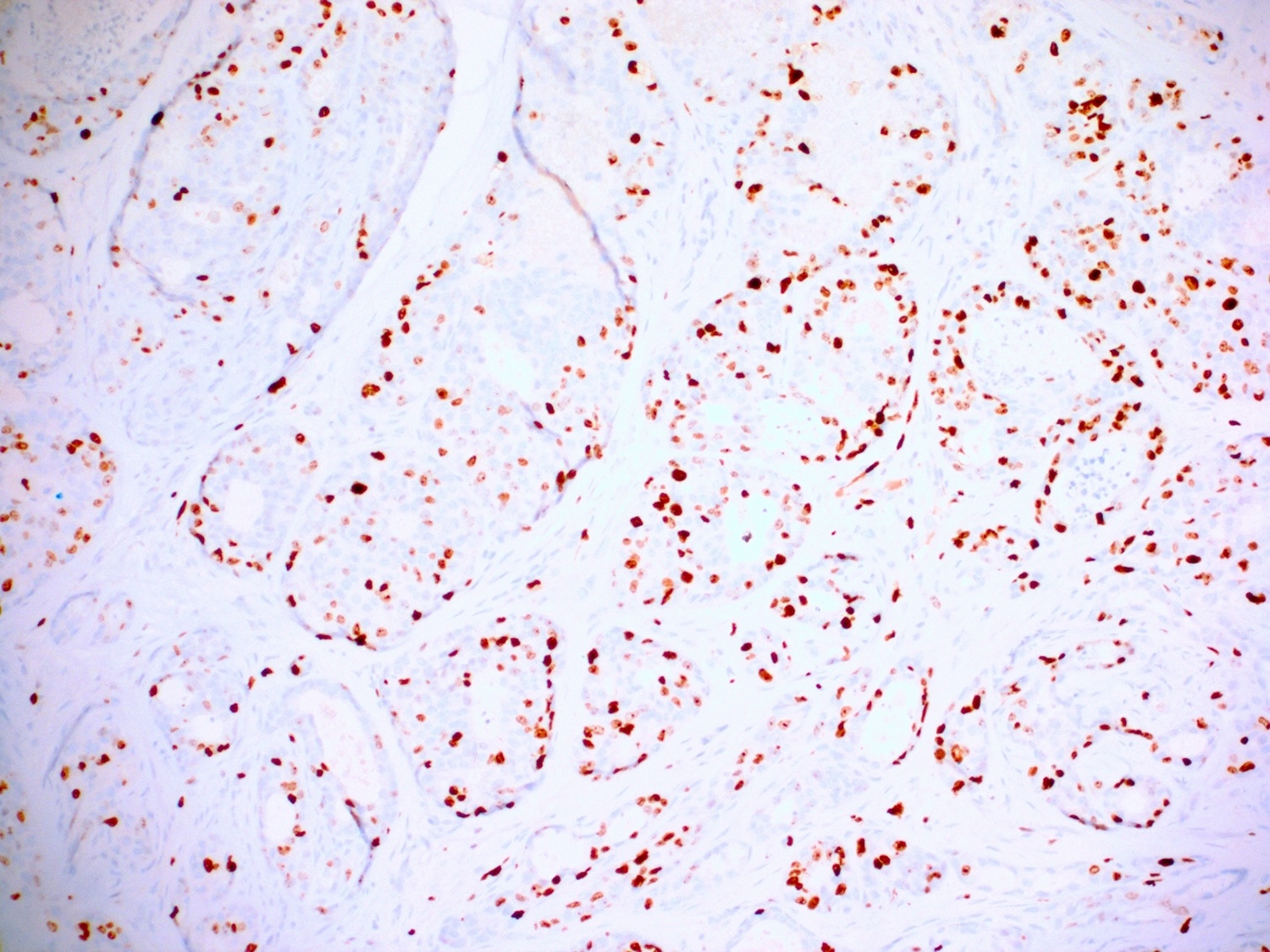
Positive stains
- Gross cystic disease fluid protein-15 (GCDFP-15), GATA3, epithelial membrane antigen (EMA) and CK7 are often positive (J Clin Pathol 2005;58:217, Am J Dermatopathol 2012;34:438)
- Estrogen receptor (ER), progesterone receptor (PR) and androgen receptor (AR) are variably expressed (Clin Case Rep 2020;8:3472)
- Myoepithelial markers, including p63, smooth muscle actin (SMA) and calponin, may also be positive in the myoepithelial cells (Am J Surg Pathol 2017;41:1053)
Molecular / cytogenetics description
- PTEN and PIK3CA mutations have been identified in some cases, although specific alterations are variable (Breast Cancer Res 2010;12:R63)
- Androgen receptor gene amplification may play a role in tumorigenesis, as seen in its breast counterpart (Am J Surg Pathol 2016;40:1109)
Sample pathology report
- Perianal skin, mass, excision:
- Apocrine carcinoma, arising in an apocrine adenoma (see comment)
- Comment: The patient's history of a perianal skin mass, which has been present for many years with a recent increase in size, has been noted. The histology shows the coexistence of both high grade and low grade tumor components, suggesting malignant transformation from a pre-existing adenoma.
Differential diagnosis
- Tubular apocrine adenoma:
- Benign premalignant lesion arising from apocrine sweat glands (Am J Surg Pathol 2017;41:1053)
- Tubular lining cells exhibit more pronounced decapitation secretion compared to malignant apocrine carcinoma
- Peripheral myoepithelial cell layer is almost always present
- Simple glands and tubules without crowding, minimal cytologic atypia and mitoses
- Anal gland adenocarcinoma:
- Rare malignant tumor originating from the anal glands (Hum Pathol 2012;43:216)
- Typically arises in the perianal or anorectal region, often infiltrating local tissues
- Composed of irregular glandular structures with pleomorphic cells, prominent nucleoli and frequent mitotic figures; can show mucin production
- Commonly presents with anal pain, bleeding or a palpable mass; symptoms may resemble benign conditions, leading to delayed diagnosis
- Tends to be aggressive with potential for local invasion and metastasis, especially to lymph nodes
- No expression of myoepithelial markers
- Metastatic adenocarcinoma:
- Clinical history of malignant neoplasm is important for diagnosis
- Based upon history and cytomorphologic characteristics, site specific lineage markers, such as prostate specific antigen (PSA), GATA3, thyroid transcription factor 1 (TTF1), should be tested to rule out metastasis from other primary sites
- Direct extension or metastatic colorectal adenocarcinoma are usually CK7- and CDX2+
- Metastatic carcinoma of breast can express GCDFP-15 and GATA3 but are usually also positive for ER and PR
Additional references
Practice question #1
Which of the following immunohistochemical markers are commonly positive in apocrine carcinoma?
- CDX2, CK20, EMA
- CK7, CK19, CDX2
- ER, PR, GCDFP-15
- GCDFP-15, androgen receptor, CK7
Practice answer #1
D. GCDFP-15, androgen receptor, CK7. Apocrine carcinoma typically expresses GCDFP-15, AR and CK7. Answer A is incorrect because these markers are associated with gastrointestinal adenocarcinomas, not apocrine carcinomas. CDX2 and CK20 are specific to intestinal differentiation, which is not a feature of apocrine tumors. Answer B is incorrect because while CK7 is positive in apocrine carcinoma, CK19 is not specific to apocrine differentiation and CDX2 indicates intestinal origin. Answer C is incorrect because while GCDFP-15 is typically positive in apocrine carcinoma, ER and PR would likely be negative, differentiating apocrine carcinomas from other hormone sensitive carcinomas, such as breast cancer.
Comment Here
Reference: Apocrine carcinoma
Comment Here
Reference: Apocrine carcinoma
Practice question #2
What is a distinguishing histologic feature of apocrine carcinoma (shown above)?
- Discohesive large cells with prominent nucleoli, brown pigments and necrosis
- Large pleomorphic cells with eosinophilic granular cytoplasm and prominent nucleoli
- Signet ring cells with mucin production
- Small blue cells with hyperchromatic nuclei
Practice answer #2
B. Large pleomorphic cells with eosinophilic granular cytoplasm and prominent nucleoli. Apocrine carcinoma is characterized histologically by large pleomorphic cells with eosinophilic granular cytoplasm and prominent nucleoli, which are hallmark features of apocrine differentiation. Answer A is incorrect because discohesive large cells with prominent nucleoli, brown pigments and necrosis are more suggestive of melanoma rather than apocrine carcinoma. Answer C is incorrect because signet ring cells with mucin production are a defining feature of signet ring cell carcinoma, typically of colorectal or gastric origin, and are not associated with apocrine carcinoma. Answer D is incorrect because small blue cells with hyperchromatic nuclei are characteristic of basal cell carcinoma or small cell neuroendocrine carcinoma. These cells are markedly different in size and morphology from the large pleomorphic apocrine cells seen in apocrine carcinoma.
Comment Here
Reference: Apocrine carcinoma
Comment Here
Reference: Apocrine carcinoma