Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Frozen section description | Intraoperative frozen / smear cytology images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Ahrendsen JT. Glioma overview. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnstumorgliomageneral.html. Accessed September 16th, 2025.
Definition / general
- Most common form of intra-axial primary tumors of the central nervous system (CNS)
- Includes adult and pediatric type diffuse gliomas, circumscribed gliomas and ependymal tumors
- Note: pediatric type gliomas occur more frequently in children and adolescents; however, they can also occur in young adults (and vice versa)
- Glioneuronal and neuronal tumors will not be discussed here
- Increasing importance of molecular diagnostics for glioma classification (IDH1 / IDH2, histone H3, etc.)
Essential features
- Group of primary CNS neoplasms with glial differentiation
- Range in biologic aggressiveness from WHO grade 1 (benign) to WHO grade 4 (malignant)
- Changes with the 2021 CNS WHO (5th edition) (Neuro Oncol 2021;23:1231)
- Arabic numbers are now used instead of Roman numerals for grading (i.e., WHO grade 1, 2, 3, 4 instead of WHO grade I, II, III, IV)
- Simplified classification of adult type diffuse gliomas into 3 groups
- Glioblastoma, IDH wildtype, WHO grade 4
- Astrocytoma, IDH mutant, WHO grade 2 - 4
- Oligodendroglioma, IDH mutant and 1p / 19q codeleted, WHO grade 2 - 3
- Additional molecular surrogates for WHO grade 4 designation (i.e., grade 4 designation should be applied even without the presence of grade 4 histology) (Neuro Oncol 2021;23:1231)
- Glioblastoma, IDH wildtype
- Polysomy 7 and monosomy 10 (+7 / -10)
- EGFR amplification
- TERT promoter mutation
- Astrocytoma, IDH mutant
- CDKN2A / CDKN2B homozygous deletion
- Glioblastoma, IDH wildtype
Terminology
- Intra-axial: within the brain or spinal cord parenchyma
- Extra-axial: not within the brain or spinal cord parenchyma (e.g., meningioma)
- Intramedullary: within the spinal cord parenchyma
- Extramedullary: not within the spinal cord parenchyma (e.g., schwannoma)
- Supratentorial: above tentorial membrane - cerebrum
- Infratentorial: below tentorial dura - brainstem, cerebellum, spinal cord
ICD coding
- ICD-O
- 9400/3 - astrocytoma, IDH mutant, grade 2
- 9401/3 - astrocytoma, IDH mutant, grade 3
- 9445/3 - astrocytoma, IDH mutant, grade 4
- 9450/3 - oligodendroglioma, IDH mutant and 1p / 19q codeleted, grade 2
- 9451/3 - oligodendroglioma, IDH mutant and 1p / 19q codeleted, grade 3
- 9440/3 - glioblastoma, IDH wildtype
- 9421/1 - diffuse astrocytoma, MYB or MYBL1 altered
- 9431/1 - angiocentric glioma
- 9413/0 - polymorphous low grade neuroepithelial tumor of the young
- 9421/1 - diffuse low grade glioma, MAPK pathway altered
- 9385/3 - diffuse midline glioma, H3 K27 altered
- 9385/3 - diffuse hemispheric glioma, H3 G34 mutant
- 9385/3 - diffuse pediatric type high grade glioma, H3 wildtype and IDH wildtype
- 9385/3 - infant type hemispheric glioma
- 9421/1 - pilocytic astrocytoma
- 9421/3 - high grade astrocytoma with piloid features
- 9424/3 - pleomorphic xanthoastrocytoma
- 9384/1 - subependymal giant cell astrocytoma
- 9444/1 - chordoid glioma
- 9430/3 - astroblastoma, MN1 altered
- 9391/3 - supratentorial ependymoma, NOS
- 9396/3 - supratentorial ependymoma, ZFTA fusion positive
- 9396/3 - supratentorial ependymoma, YAP1 fusion positive
- 9391/3 - infratentorial ependymoma, NOS
- 9396/3 - posterior fossa group A (PFA) ependymoma
- 9396/3 - posterior fossa group B (PFB) ependymoma
- 9391/3 - spinal ependymoma, NOS
- 9396/3 - spinal ependymoma, MYCN amplified
- 9394/1 - myxopapillary ependymoma
- 9383/1 - subependymoma
- ICD-11
- 2A00.0Y& XH6PH6 - other specified gliomas of brain & astrocytoma, NOS
- 2A00.0Y& XH2HK4 - other specified gliomas of brain & diffuse astrocytoma, IDH mutant
- 2A00.0Y& XH7K31 - other specified gliomas of brain & oligodendroglioma, IDH mutant and 1p / 19q codeleted
- 2A00.0Y& XH5571 - glioblastoma of brain & glioblastoma, IDH wildtype
- 2A00.0Y& XH41C5 - other specified gliomas of brain & angiocentric glioma
- 2A00.2Y - other specified tumors of neuroepithelial tissue of brain
- 2A00.0Y - other specified gliomas of brain
- 2A00.0Y& XH7692 - other specified gliomas of brain & diffuse midline glioma, H3 K27M mutant
- 2A00.0Y& XH29Q5 - other specified gliomas of brain & pilomyxoid astrocytoma
- 2A00.0Y& XH99U2 - other specified gliomas of brain & pleomorphic xanthoastrocytoma
- 2A00.0Y& XH1L48 - other specified gliomas of brain & subependymal giant cell astrocytoma
- 2A00.0Y& XH9HV1 - other specified gliomas of brain & chordoid glioma
- 2A00.0Y& XH1DC5 - other specified gliomas of brain & astroblastoma
- 2A00.0Y & XH1511 - other specified gliomas of brain & ependymoma, NOS
- 2A00.0Z & XH1511 - other and unspecified neoplasms of brain or central nervous system & ependymoma, NOS
- 2A00.0Y& XH15U1 - other specified gliomas of brain & myxopapillary ependymoma
- 2A00.0Y& XH8FZ9 - other specified gliomas of brain & subependymoma
Epidemiology
- CNS tumors account for only 2% of all malignant neoplasms (Neuro Oncol 2021;23:iii1)
- 40% with neuroepithelial origin
- In children, CNS tumors are the leading cause of cancer related death (NCHS Data Brief 2016;257:1, Neuro Oncol 2018;20:iv1)
- Children and adolescents are more likely to acquire pediatric type diffuse gliomas and certain circumscribed gliomas, whereas adults are more likely to acquire adult type diffuse gliomas, though there is considerable overlap (Neuro Oncol 2021;23:iii1)
Sites
- Brain
- Spinal cord
Pathophysiology
- Generally, not well understood
- Most glial tumors are likely derived from populations of CNS progenitor cells, including neural progenitor cells, glial progenitor cells, oligodendrocyte precursor cells, etc. (Cells 2021;10:621)
Etiology
- In most cases, there is not a strong causal connection
- History of prior craniospinal radiation exposure is a known risk factor for glioma development (J Natl Cancer Inst 2006;98:1528, Neurooncol Adv 2021;3:vdab109)
- Gliomas in hereditary cancer disorders (Neuro Oncol 2010;12:104, Curr Neurol Neurosci Rep 2021;21:64, Neurooncol Pract 2021;8:375)
- Neurofibromatosis type 1: pilocytic astrocytoma (including optic pathway glioma), high and low grade gliomas, which can be difficult to classify
- Neurofibromatosis type 2: ependymomas, most commonly spinal
- Tuberous sclerosis: subependymal giant cell astrocytoma (SEGA)
- Noonan syndrome: pilocytic astrocytoma
- Enchondromatosis (Ollier disease, Maffucci syndrome): diffuse gliomas (IDH mutant)
- Li Fraumeni syndrome: grade 4 gliomas in younger patients, including diffuse pediatric type high grade glioma, H3 wildtype and IDH wildtype; IDH mutant astrocytomas in young adults (Acta Neuropathol Commun 2023;11:3)
- Lynch syndrome (Turcot syndrome): glioblastoma
Clinical features
- Clinical presentation highly variable, depending on patient age, tumor location and tumor type (Acta Neurol Scand 2015;131:88)
- Common presenting symptoms include seizure, cognitive disorder, headache, nausea / vomiting, focal neurologic deficit
Diagnosis
- Combination of clinical findings, imaging (especially magnetic resonance imaging [MRI]) and tissue based biopsy / resection (Lancet Oncol 2017;18:e315)
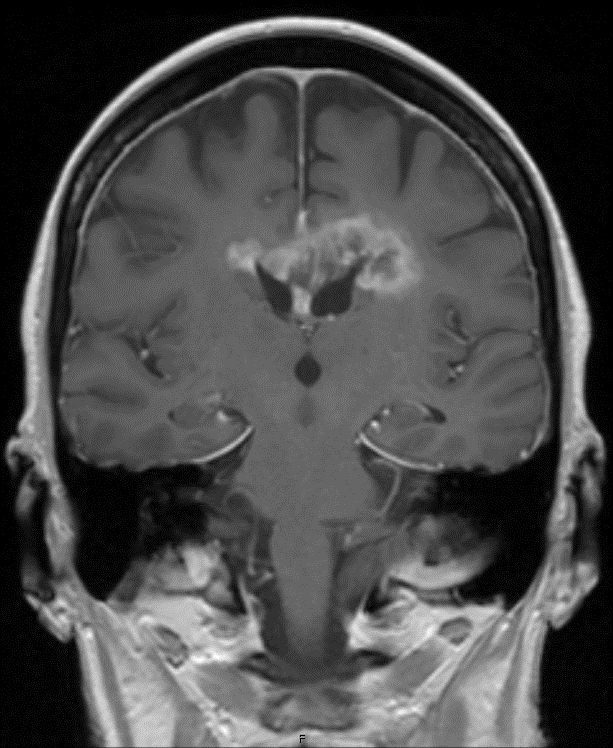
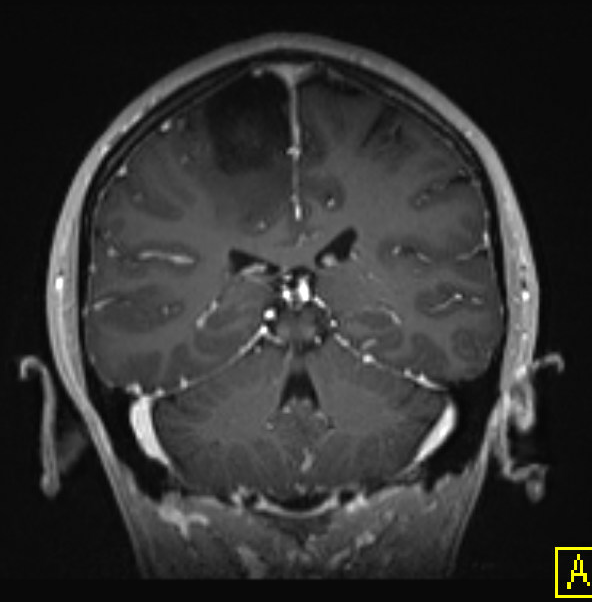
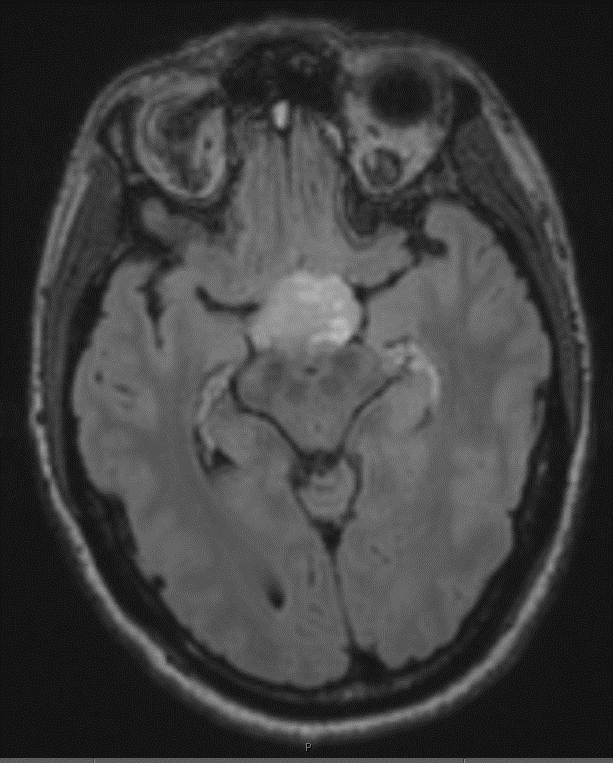
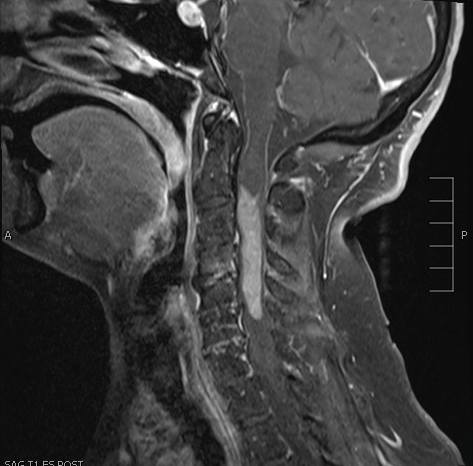
Radiology description
- Highly variable, depending on location and tumor type (Radiology 2022;304:494, Childs Nerv Syst 2009;25:1203)
- Circumscribed gliomas
- Well circumscribed, variably enhancing, occasionally seen as a cystic mass with enhancing mural nodule
- Diffuse low grade gliomas
- Expansile but usually without enhancement
- T2 FLAIR mismatch sign is a specific (but not sensitive) indicator in adults for astrocytoma, IDH mutant
- Calcifications and cystic components can occasionally be seen in oligodendroglioma, IDH mutant and 1p / 19q codeleted
- Diffuse high grade gliomas
- Expansile and generally with variable enhancement
- Glioblastoma often displays a characteristic ring enhancement with surrounding vasogenic edema and diffusion restriction
- Ependymoma
- Often conspicuous on T2 weighted FLAIR sequences and usually visible on unenhanced T1 weighted images
- Circumscribed gliomas
Radiology images
Prognostic factors
- CNS WHO grade (BMC Cancer 2020;20:35)
- WHO grade 1: generally benign; potentially curable with resection
- WHO grade 2 - 3: intermediate prognosis; survival generally many years with eventual tumor progression
- WHO grade 4: malignant; survival limited to months
- Even low grade tumors can cause significant morbidity and mortality if located in delicate parts of the brain, such as the brainstem
- Other factors that influence prognosis include patient age, comorbid conditions, location of tumor, presence of hydrocephalus, extent of surgical resection, response to adjuvant therapy and molecular features of the tumor (BMC Cancer 2020;20:35, Ann Palliat Med 2021;10:863)
Case reports
- 3 month old girl presents with altered mental status (BMJ Case Rep 2019;12:e228248)
- 39 year old woman with progressive unilateral vision loss (Brain Tumor Pathol 2021;38:59)
- 53 year old woman with unsteady gait (Acta Radiol Open 2020;9:2058460120980143)
- 69 year old woman with radiation induced spinal glioblastoma (BMJ Case Rep 2020;13:e238372)
- 73 year old woman with spinal cord mass (Folia Neuropathol 2020;58:377)
Treatment
- Depends on the location, tumor type and grade (Neurosurg Rev 2017;40:1)
- Generally, gross total resection is preferred for most tumors; however, watch and wait approach with close clinical monitoring can be considered for some low grade tumors, especially those in locations unamenable to surgery (World Neurosurg 2013;79:537, World Neurosurg 2014;82:e105)
- Adjuvant radiation or chemotherapy (temozolomide) is often performed for high grade gliomas (N Engl J Med 2005;352:987)
- Targeted therapies available for tumors with certain molecular alterations (Mol Cancer 2022;21:39)
- Several experimental approaches under investigation, including immunotherapeutic approaches (Cancer Lett 2020;476:1, Cell Commun Signal 2023;21:74)
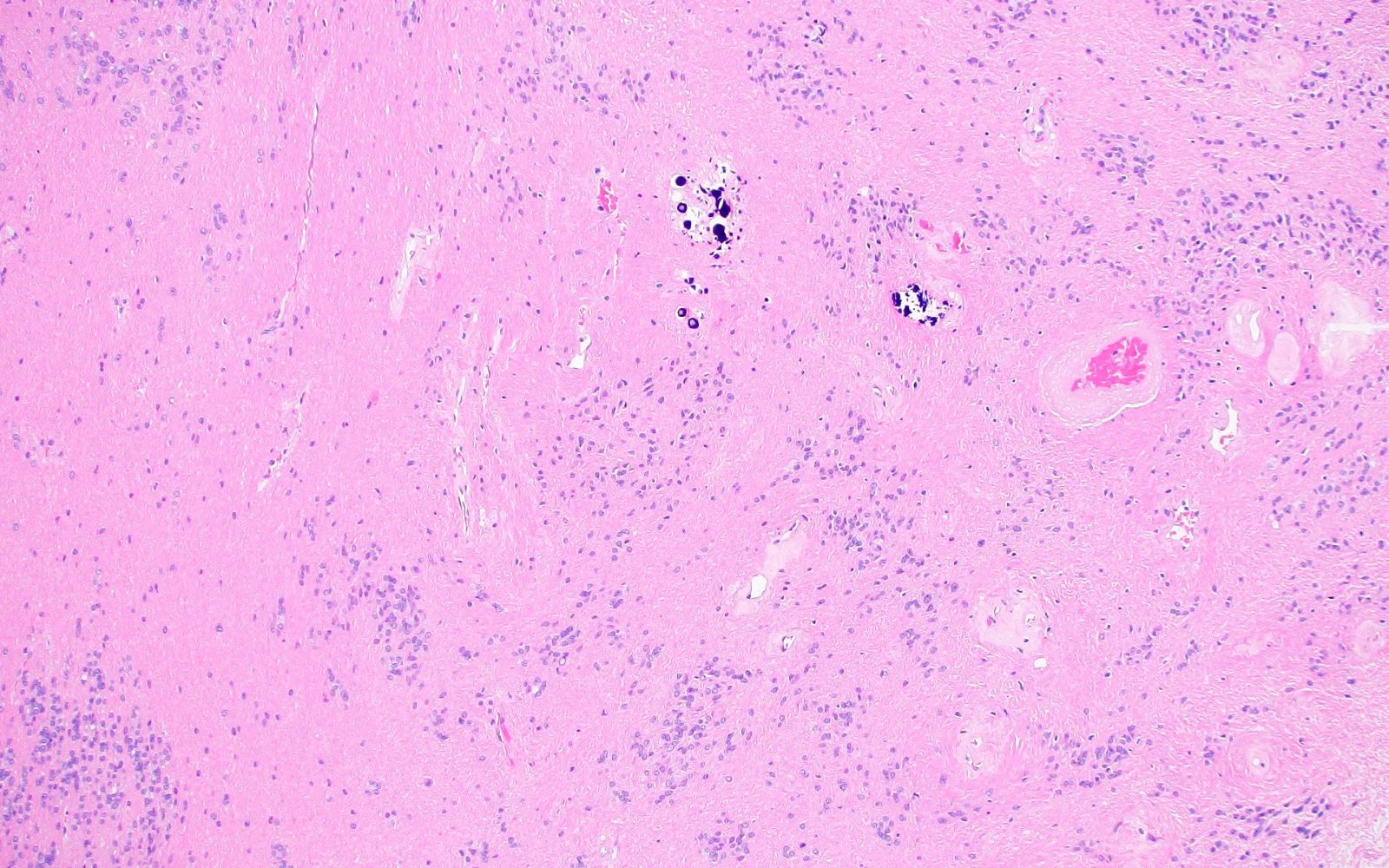
Frozen section description
- Can be useful in some cases to determine circumscribed versus infiltrative growth patterns
- Helpful to identify high grade features, such as mitotic activity, microvascular proliferation and necrosis
- Due to freezing artifact, nuclear atypia is difficult to assess on frozen section (see Cytology description)
- References: Surg Pathol Clin 2015;8:27, Semin Diagn Pathol 2002;19:192
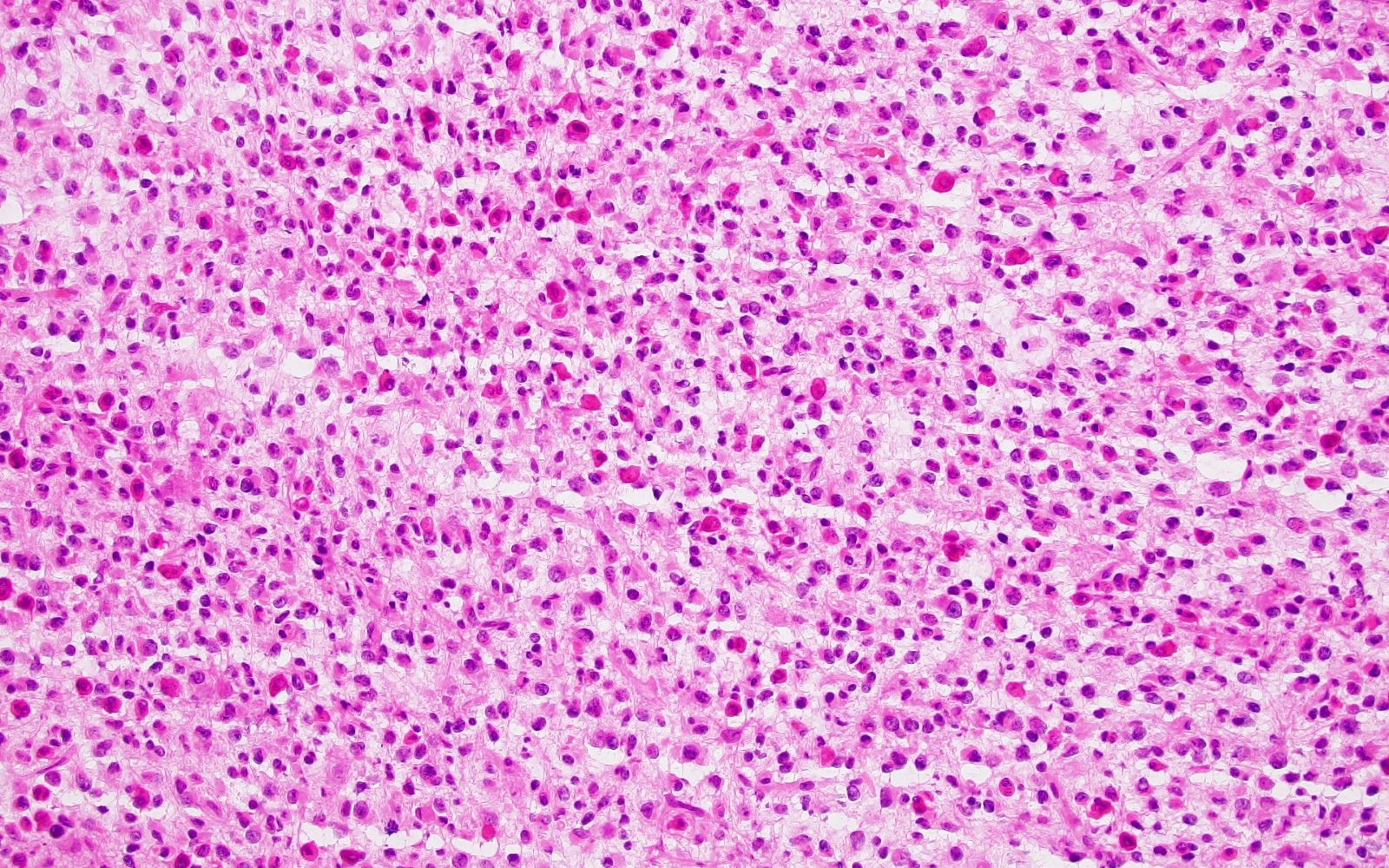
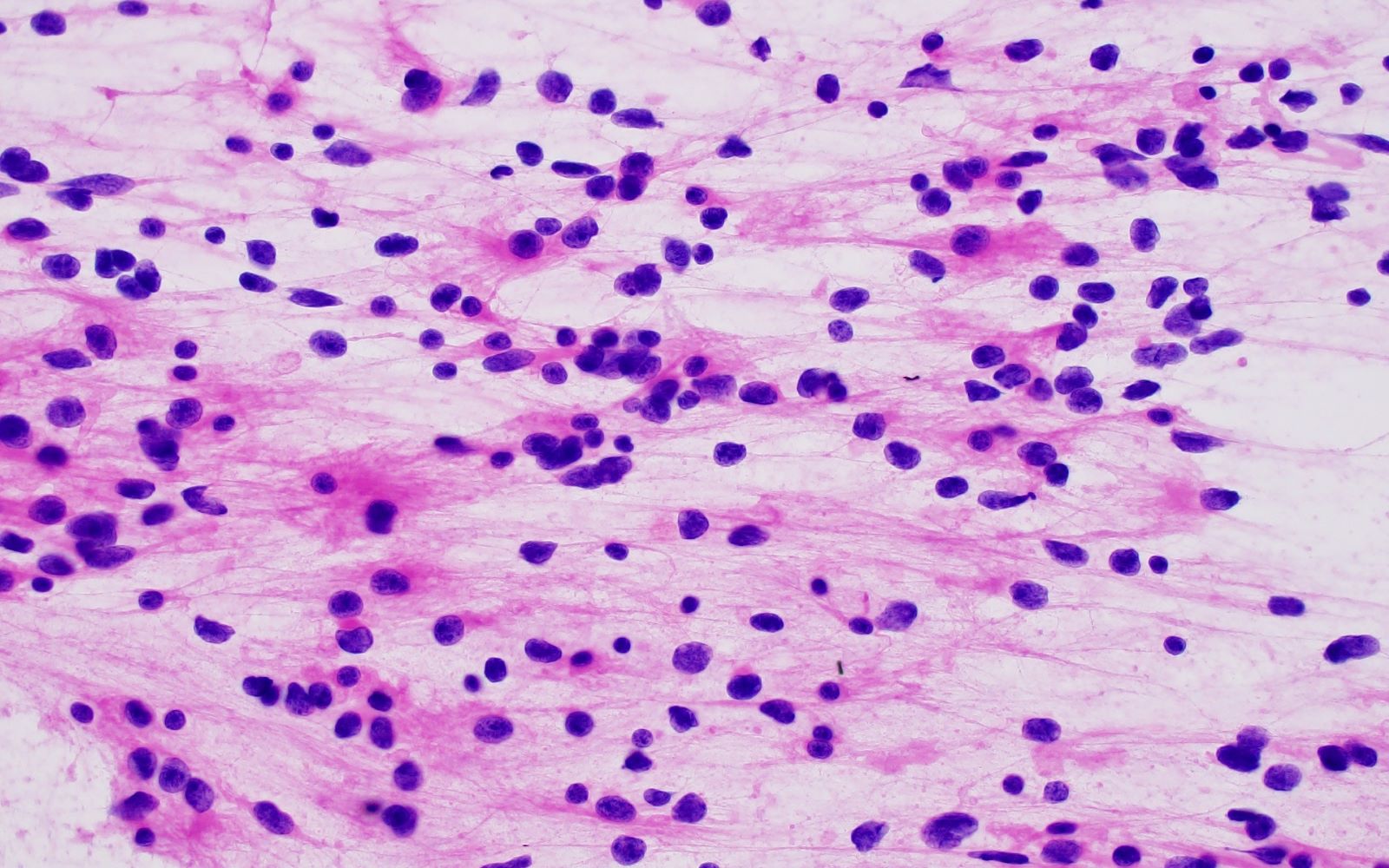
Intraoperative frozen / smear cytology images
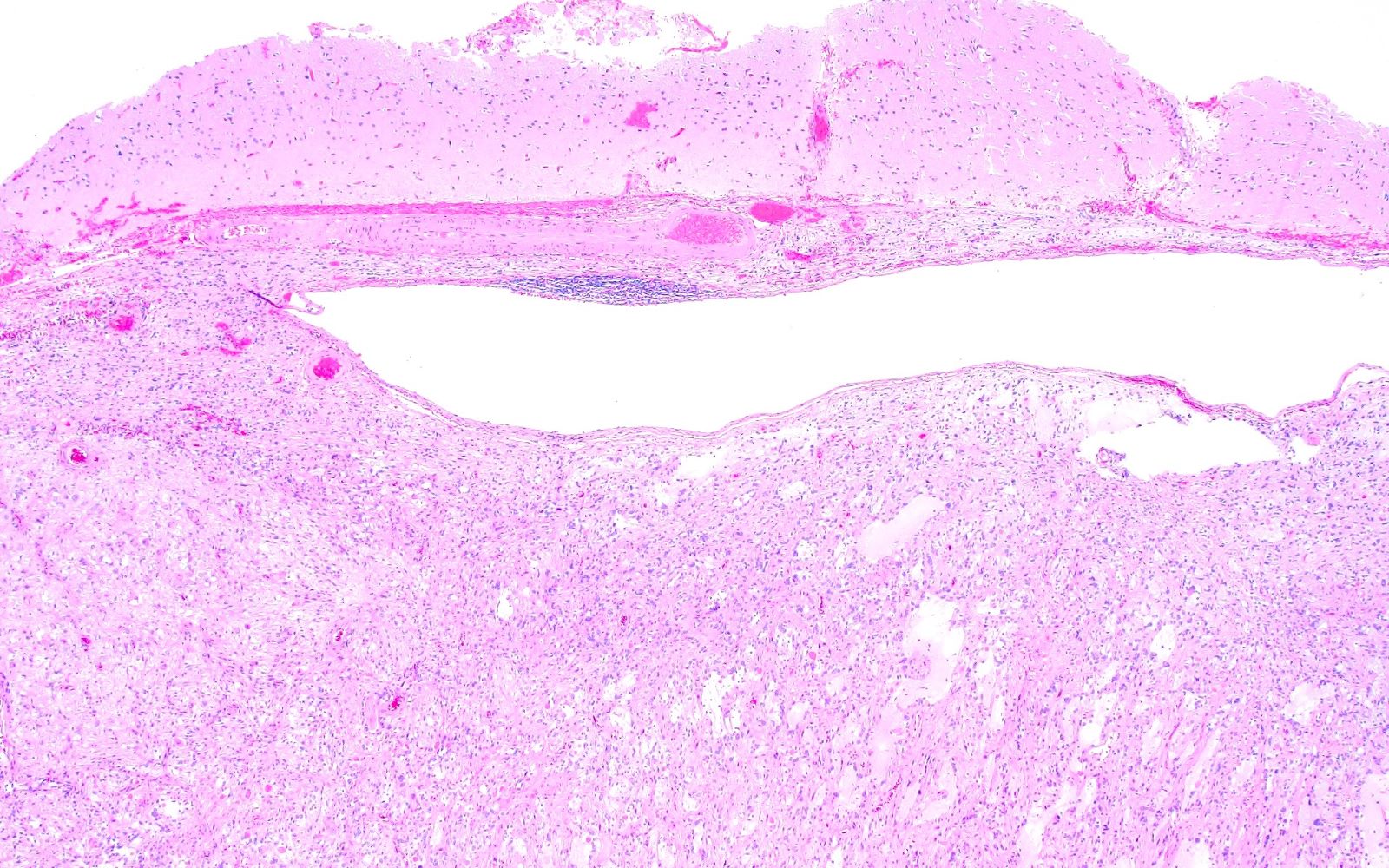
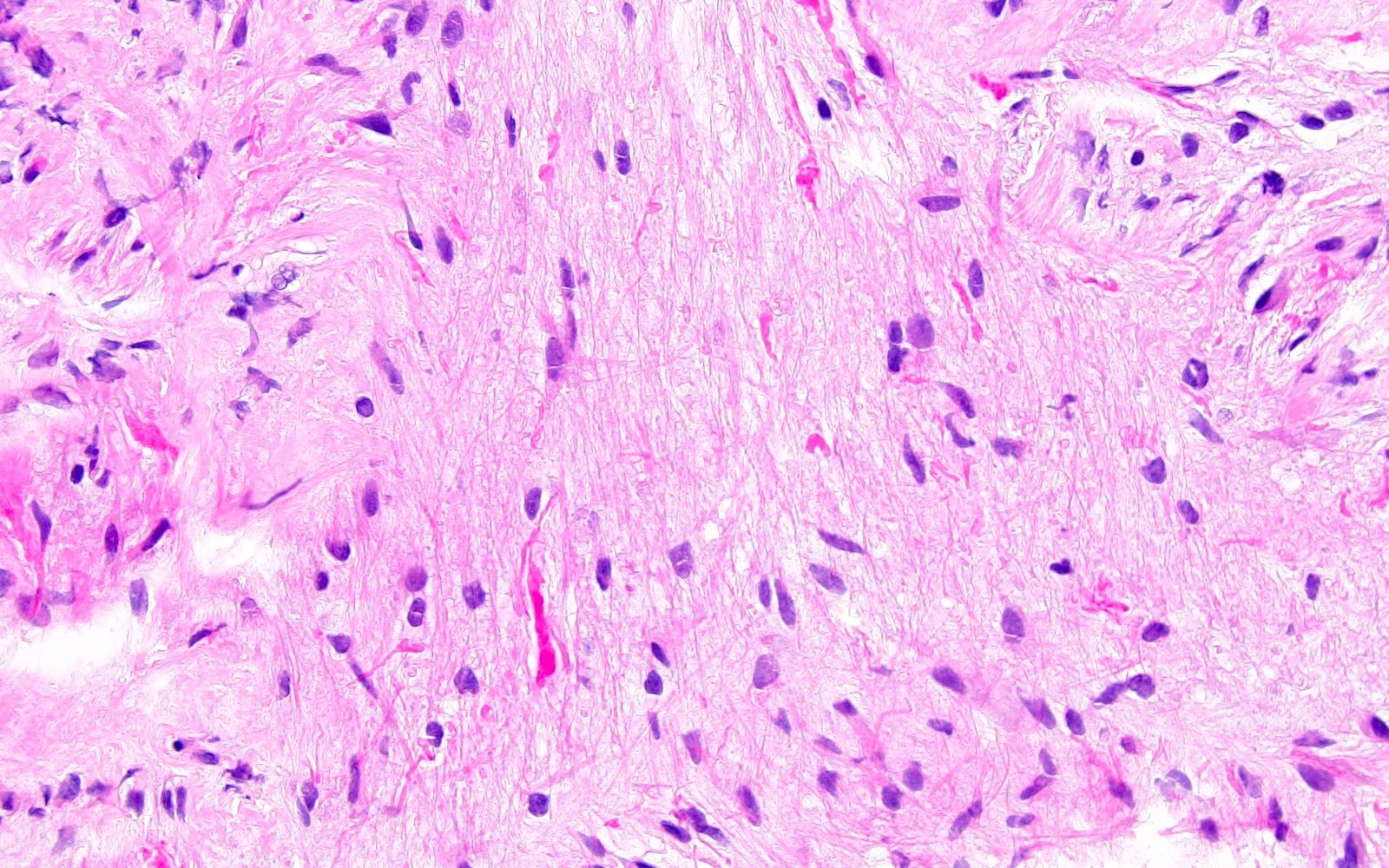
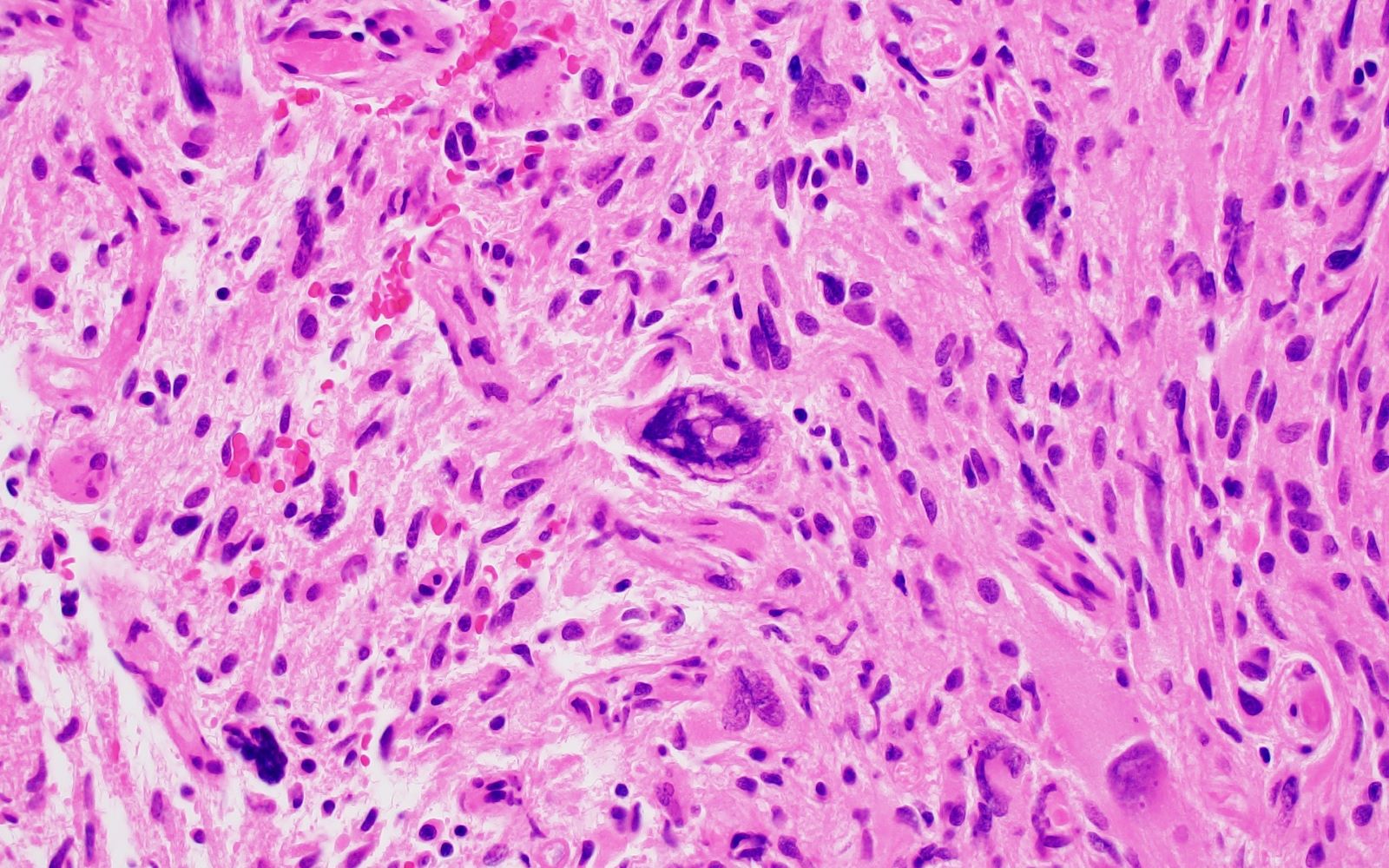
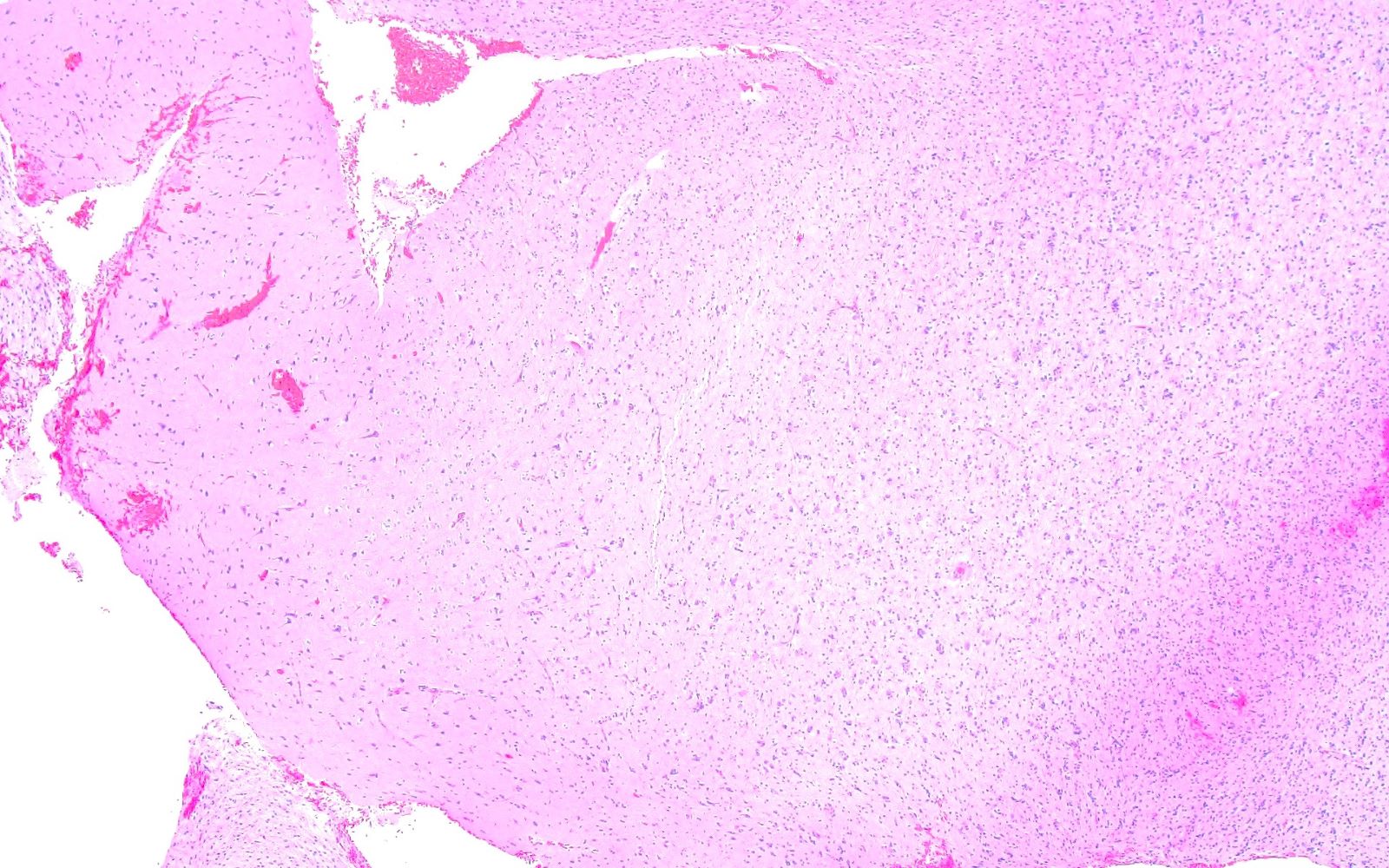
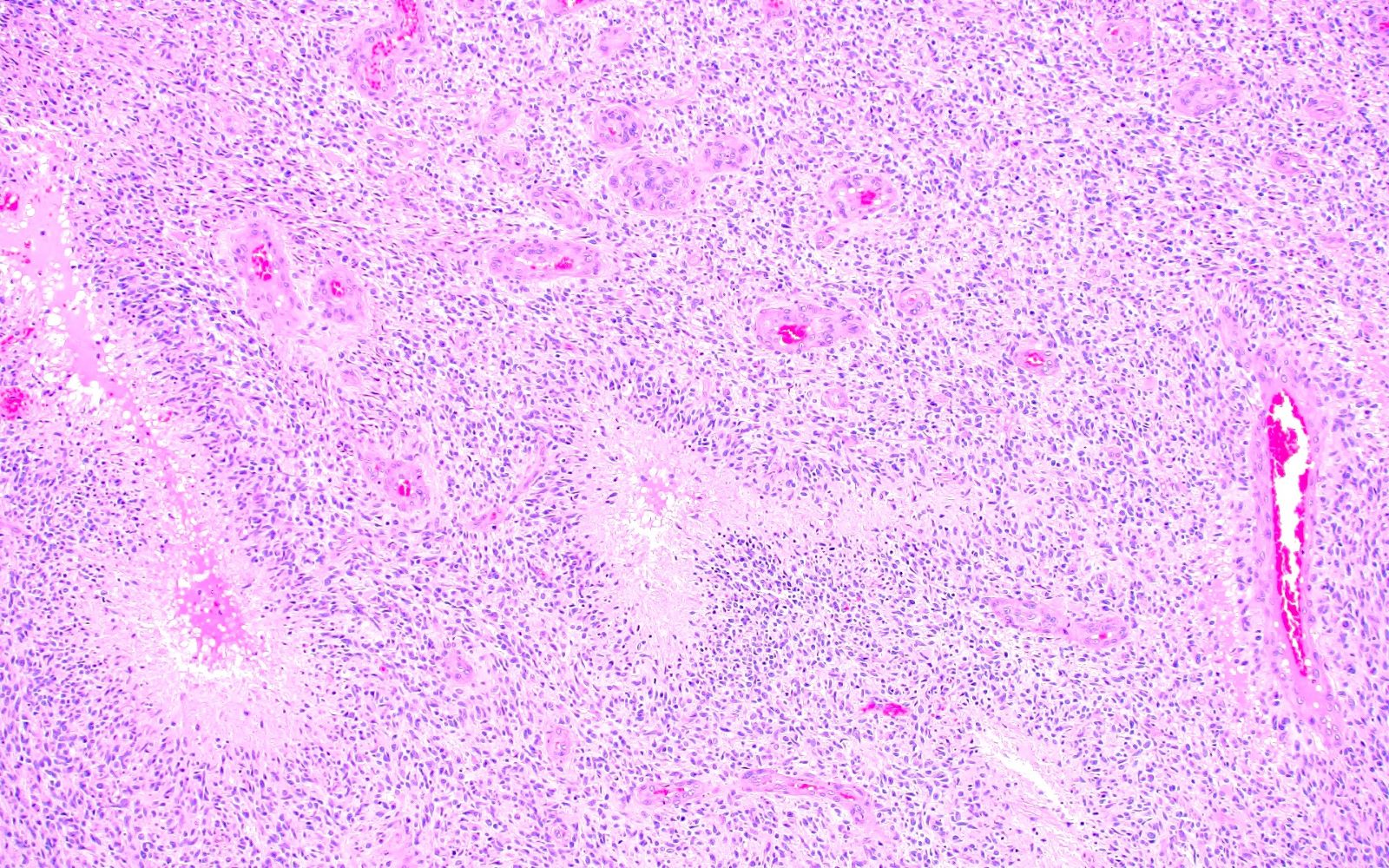
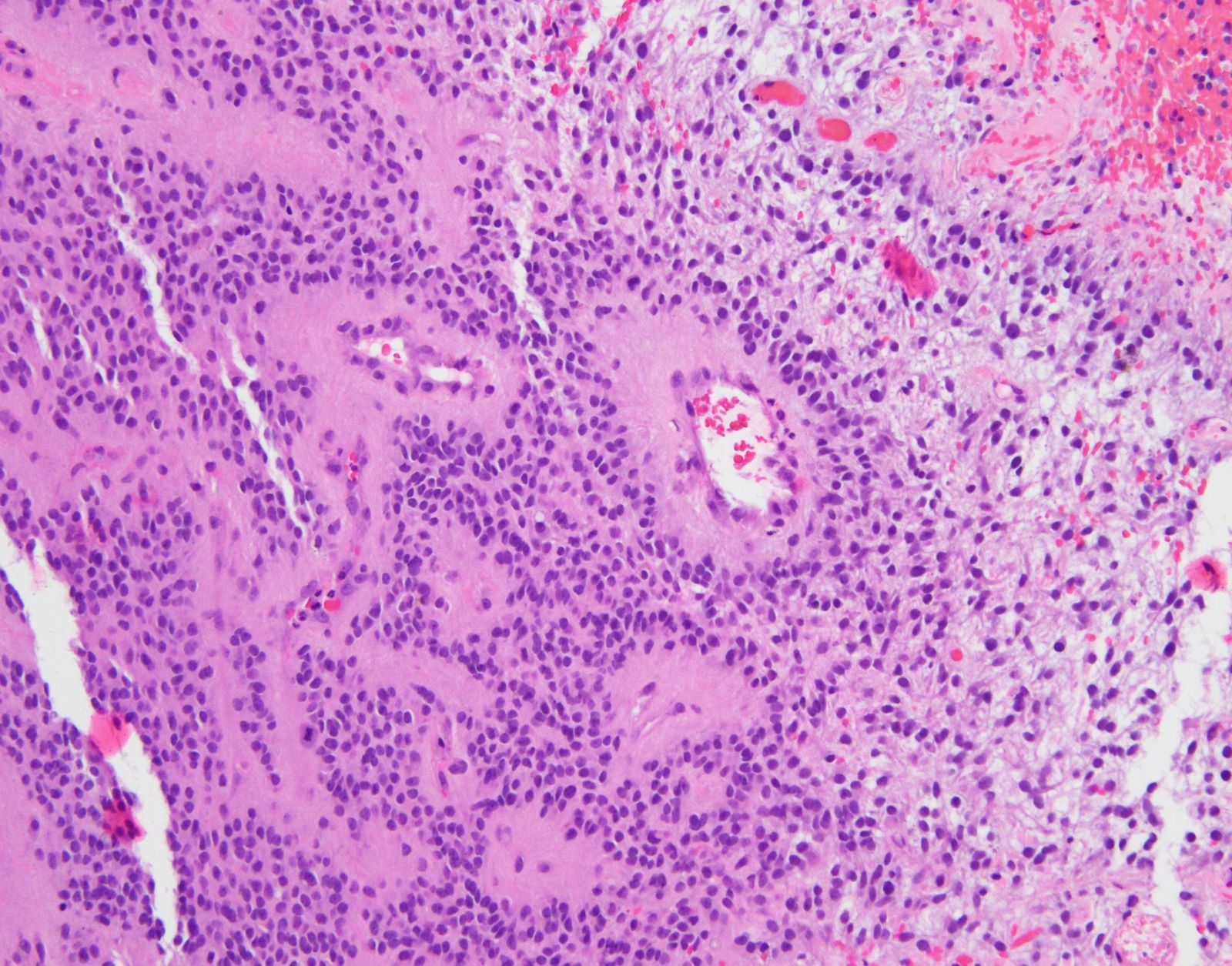
Microscopic (histologic) description
- Diffuse gliomas
- Variably hypercellular with individual tumor cells infiltrating the brain parenchyma
- Diffuse infiltration results in ill defined margin with adjacent brain tissue
- Secondary structures of Scherer, indicative of infiltrative growth
- Perineuronal satellitosis by tumor cells
- Perivascular condensation by tumor cells
- Subpial accumulation of tumor cells
- Spread of tumor cells along white matter tracks
- Variable nuclear atypia, including nuclear enlargement, irregular nuclear contours, hyperchromasia, multinucleation, etc.
- Some histologic features are suggestive of particular diagnostic entities (see individual chapters for more complete descriptions)
- Astrocytoma, IDH mutant: astrocytic differentiation often in a densely fibrillary background with microcysts
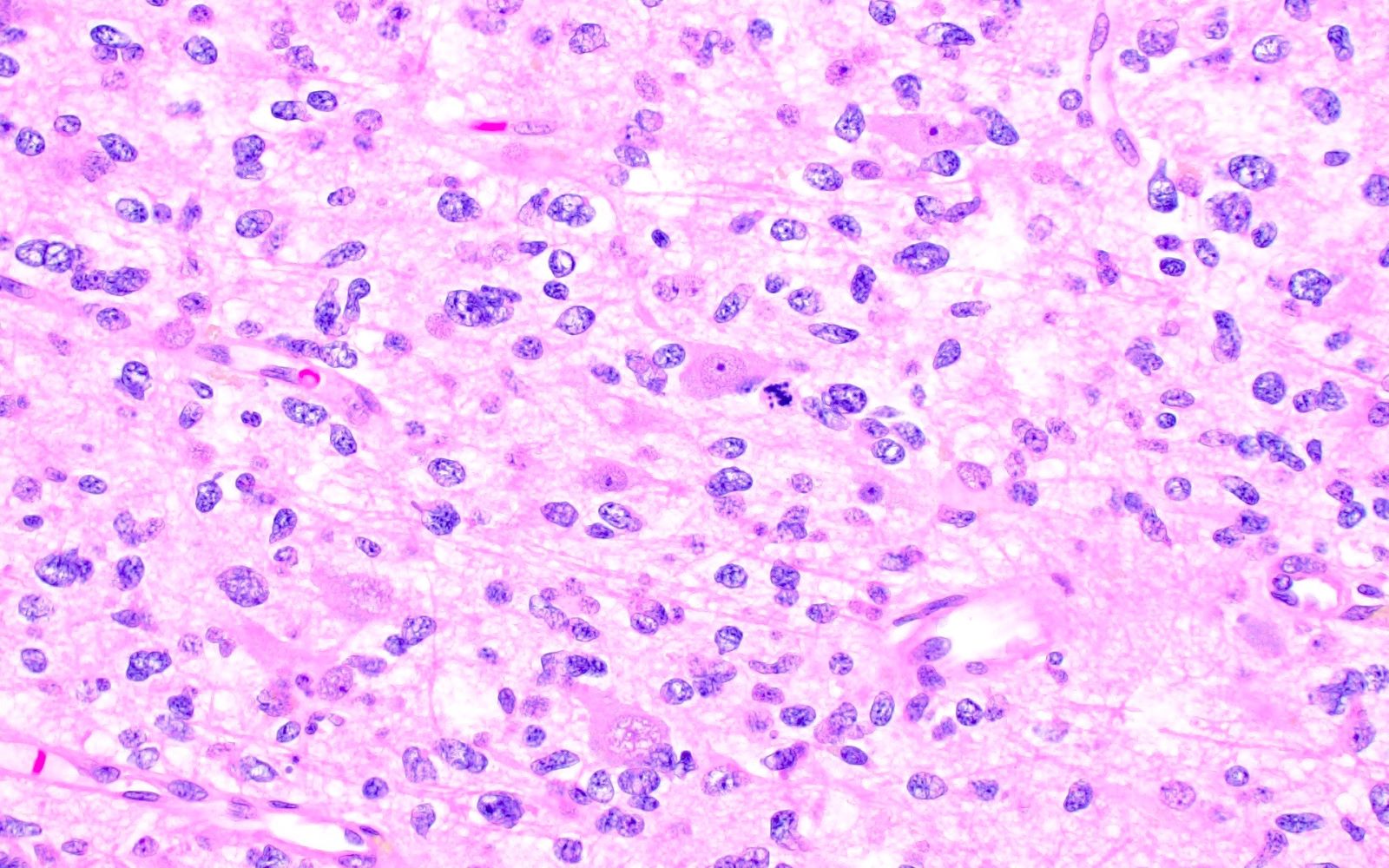
- Oligodendroglioma, IDH mutant and 1p / 19q codeleted: round, monotonous nuclei with characteristic perinuclear halos (fried egg appearance), microcalcifications and chicken wire blood vessels are common
- Glioblastoma, IDH wildtype: densely cellular with brisk mitotic activity and often with microvascular proliferation and pseudopalisading necrosis; tumor microthrombi are characteristic (Acta Neuropathol 2016;132:917)
- Diffuse astrocytoma, MYB or MYBL1 altered & diffuse low grade glioma, MAPK altered: diffuse growth pattern, mild nuclear atypia, minimal to no mitotic activity, absence of anaplastic features (vascular proliferation, necrosis)
- Angiocentric glioma: diffuse glioma with uniform bipolar spindle cells characteristically arranged radially around blood vessels
- Polymorphous low grade neuroepithelial tumor of the young (PLNTY): diffuse growth pattern and tumor cells with oligo-like features (monotonous nuclei, perinuclear halos), minimal mitotic activity, calcifications are common
- Pediatric type diffuse high grade gliomas: distinguishing histologic characteristics are not generally seen; requires immunohistochemistry and molecular testing
- Infant type hemispheric glioma: highly cellular, infiltrative and frequently well demarcated from adjacent brain; often with leptomeningeal involvement
- Circumscribed astrocytic neoplasms
- Pilocytic astrocytoma
- Circumscribed, biphasic (compact and loose) astrocytic neoplasm with piloid cellular processes, bipolar tumor cells, low proliferation and often Rosenthal fibers or eosinophilic granular bodies
- High grade astrocytoma with piloid features
- Histopathologic features vary considerably and molecular testing is generally required for diagnosis
- Pleomorphic xanthoastrocytoma
- Predominantly circumscribed astrocytoma with pleomorphic nuclei, occasional cells with bubbly (xanthomatous) cytoplasm, eosinophilic granular bodies, perivascular lymphocytes and reticulin rich background
- Subependymal giant cell astrocytoma (SEGA)
- Circumscribed, moderately cellular astrocytic neoplasm composed of polygonal cells with abundant eosinophilic cytoplasm and often multinucleated cells
- Chordoid glioma
- Glial neoplasm composed of chords / ribbons of epithelioid cells in a variably myxoid background
- Astroblastoma, MN1 altered
- Glial neoplasm characterized by the presence of astroblastic perivascular pseudorosettes: radially oriented tumor cells with thick cellular processes oriented towards a central blood vessel
- Pilocytic astrocytoma
- Ependymal tumors
- Ependymoma
- Circumscribed neoplasm characterized by monomorphic round tumor cells, often arranged around blood vessels to form perivascular pseudorosettes
- Subependymoma
- Round, uniform tumor cells arranged in clusters / nests within a dense fibrillary background
- Microcystic changes and calcifications are common
- Myxopapillary ependymoma
- Glioma with papillary structures and often prominent myxoid background
- Ependymoma
- Reference: Neuro Oncol 2021;23:1231
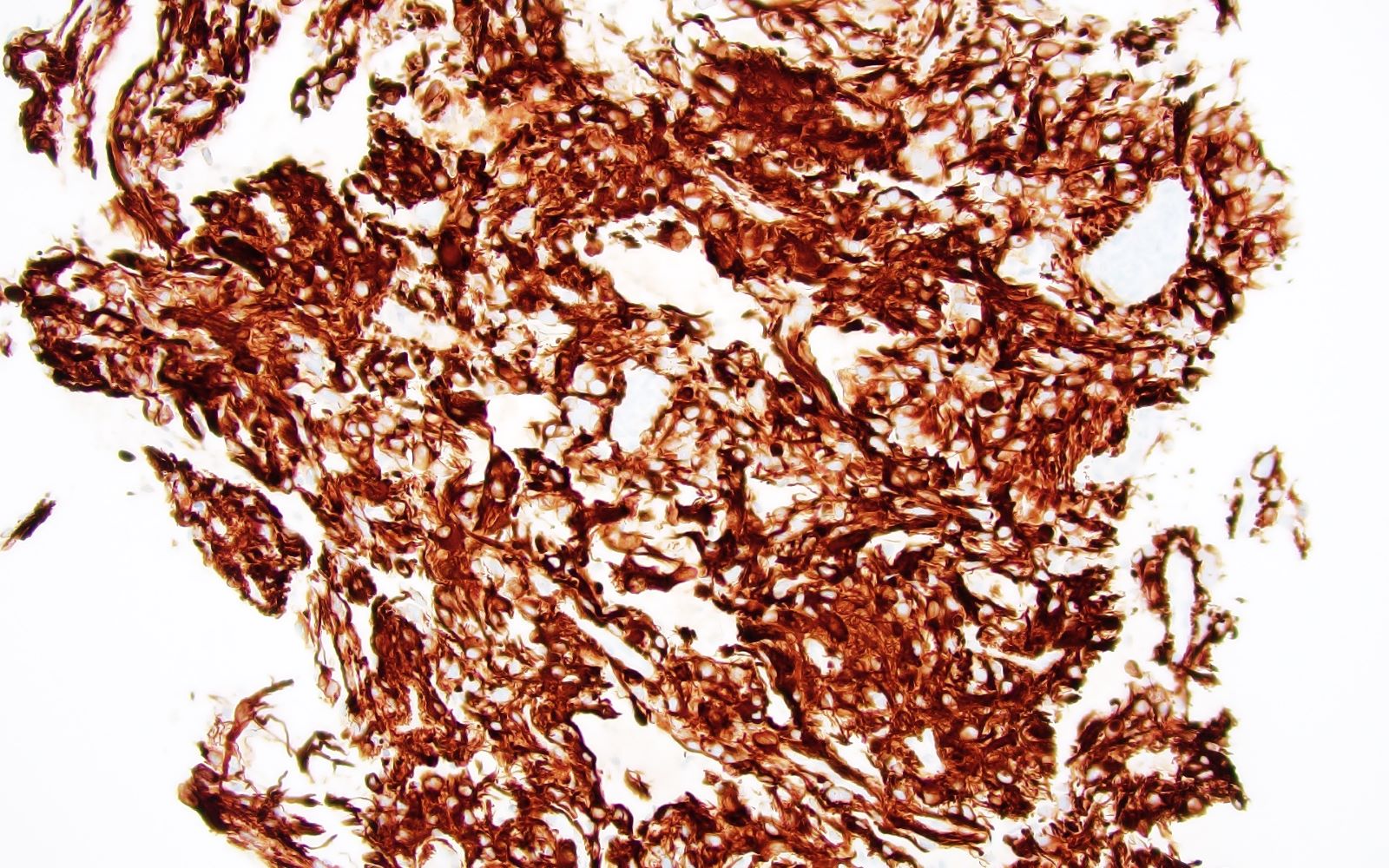
Microscopic (histologic) images
Virtual slides
Cytology description
Negative stains
Molecular / cytogenetics description
- Adult type diffuse gliomas
- Astrocytoma, IDH mutant (J Neuropathol Exp Neurol 2016;75:4, N Engl J Med 2015;372:2481, Acta Neuropathol 2018;136:153)
- By definition, presence of IDH1 / IDH2 mutation and intact chromosomes 1p and 19q
- Co-occurring ATRX and TP53 mutations are common
- Presence of CDKN2A / CDKN2B homozygous deletion associated with poor outcome and sufficient for WHO grade 4 designation, irrespective of histologic grade
- Oligodendroglioma, IDH mutant and 1p / 19q codeleted (N Engl J Med 2015;372:2481, CNS Oncol 2015;4:287)
- By definition, presence of IDH1 / IDH2 mutation and whole arm deletion of chromosomes 1p and 19q
- Co-occurring CIC and TERT promoter mutations are common
- Glioblastoma, IDH wildtype (Acta Neuropathol 2018;136:793, N Engl J Med 2005;352:997)
- By definition, IDH1 / IDH2 wildtype
- Characteristic molecular findings
- TERT promoter mutation
- EGFR amplification
- Polysomy 7 and monosomy 10 (+7 / -10)
- Presence of any of these 3 molecular alterations is sufficient for WHO grade 4 designation in an adult type, IDH wildtype diffuse glioma, irrespective of histologic grade
- MGMT promoter methylation associated with better response to alkylating chemotherapy (temozolomide)
- Many other co-occurring molecular and cytogenetic alterations can be encountered
- Astrocytoma, IDH mutant (J Neuropathol Exp Neurol 2016;75:4, N Engl J Med 2015;372:2481, Acta Neuropathol 2018;136:153)
- Pediatric type diffuse low grade gliomas
- Diffuse astrocytoma, MYB or MYBL1 altered (Acta Neuropathol 2019;137:683)
- Defined by the presence of MYB or MYBL1 fusion, most common fusion partners include PCDHGA1, MMP16 and MAML2
- Typically not MYB::QKI fusion, which characterizes angiocentric glioma (see below)
- Angiocentric glioma (Acta Neuropathol 2019;137:683, Nat Genet 2016;48:273)
- Characterized by alteration of MYB on chromosome 6q, most commonly MYB::QKI fusion
- Polymorphous low grade neuroepithelial tumor of the young (PLNTY) (J Neuropathol Exp Neurol 2021;80:821)
- Characterized by MAPK pathway activating alterations, including BRAF V600E and fusions involving FGFR2 and FGFR3
- Diffuse low grade glioma, MAPK altered (Nat Genet 2013;45:602)
- Defined by the presence of a MAPK pathway activating alteration, in addition to wildtype IDH and H3 as well as absence of CDKN2A / CDKN2B homozygous deletion
- Diffuse astrocytoma, MYB or MYBL1 altered (Acta Neuropathol 2019;137:683)
- Pediatric type diffuse high grade gliomas
- Diffuse midline glioma, H3 K27 altered (Acta Neuropathol 2015;130:815)
- Defined by loss of H3 K27 trimethylation with presence of H3 K27 mutation, EGFR amplification or EZHIP overexpression in a diffusely infiltrating glioma located along the midline
- Can be alternately defined by loss of H3 K27 trimethylation with a methylation profile of diffuse midline glioma in a diffusely infiltrating glioma located along the midline
- Diffuse hemispheric glioma, H3 G34 mutant (Acta Neuropathol 2016;131:137)
- Defined by the presence of H3 G34 mutation in a diffusely infiltrating glioma located in a cerebral hemisphere
- Diffuse pediatric type high grade glioma, H3 wildtype and IDH wildtype (Acta Neuropathol 2017;134:507)
- Diffuse glioma lacking IDH and H3 alterations; often with PDGFRA alteration, EGFR alteration or MYCN amplification
- Infant type hemispheric glioma (Nat Commun 2019;10:4343)
- Characterized by the presence of a receptor tyrosine kinase abnormality, especially fusions involving ROS1, MET1, ALK or NTRK family gene
- Diffuse midline glioma, H3 K27 altered (Acta Neuropathol 2015;130:815)
- Circumscribed astrocytic neoplasms
- Pilocytic astrocytoma (Cancer Res 2008;68:8673, Nat Genet 2013;45:602)
- Cerebellar tumors commonly harbor KIAA1549::BRAF fusion (7q34 duplication); other MAPK pathway alterations can also be encountered
- High grade astrocytoma with piloid features (Acta Neuropathol 2018;136:273)
- Presence of a MAPK pathway alteration along with CDKN2A / CDKN2B homozygous deletion, amplification of CDK4 or ATRX mutation
- DNA methylation profiling is only definitive method for diagnosis
- Pleomorphic xanthoastrocytoma (Hum Pathol 2019;86:38, Brain Pathol 2019;29:85)
- Characterized by the presence of both BRAF V600E and CDKN2A / CDKN2B homozygous deletion
- Subependymal giant cell astrocytoma (SEGA) (Oncotarget 2017;8:95516)
- Seen almost exclusively in patients with tuberous sclerosis (germline mutations in TSC1 or TSC2)
- Chordoid glioma (Nat Commun 2018;9:810)
- Characterized by PRKCA D463 mutation
- Astroblastoma, MN1 altered (Brain Tumor Pathol 2019;36:112)
- Defined by presence of MN1 alteration, most commonly MN1::BEND2 fusion
- Pilocytic astrocytoma (Cancer Res 2008;68:8673, Nat Genet 2013;45:602)
- Ependymal tumors
- Ependymoma (Cancer Cell 2015;27:728, Brain Pathol 2020;30:863)
- Supratentorial ependymoma characterized by ZFTA fusion or YAP1 fusion
- Posterior fossa ependymoma characterized by unique methylation patterns
- Spinal ependymoma characterized by NF2 mutation or MYCN amplification
- Subependymoma (Neuro Oncol 2018;20:1616)
- Recurrent losses of chromosome 19 and partial losses of chromosome 6
- Myxopapillary ependymoma (Neuro Oncol 2018;20:1616)
- Recurrent gains of chromosome 16 and losses of chromosome 10
- Note: ependymomas are defined by both anatomic location as well as molecular features
- Ependymoma (Cancer Cell 2015;27:728, Brain Pathol 2020;30:863)
- Many of these tumors form distinct clusters on DNA methylation profiling (Nature 2018;555:469)
Sample pathology report
- Brain, left frontal lobe mass, resection:
- Integrated diagnosis: glioblastoma, IDH wildtype, WHO grade 4
- Histopathologic classification: glioblastoma
- CNS WHO grade: 4
- Molecular information: TERT promoter mutation, EGFR amplification
- Brain, right parietal mass, resection:
- Integrated diagnosis: supratentorial ependymoma, not otherwise specified (NOS)
- Histopathologic classification: ependymoma
- CNS WHO grade: 3
- Molecular information: genetic material extracted from FFPE tissue was of insufficient quality or quantity for molecular testing
Differential diagnosis
- Reactive gliosis (ischemic, inflammatory, demyelination, infectious, etc.):
- Glioneuronal tumors, especially in the case of a circumscribed astrocytic neoplasm:
- Generally display some degree of neuronal differentiation, including dysmorphic ganglioid cells or expression of neural antigens (such as synaptophysin)
- See individual topics for additional differential considerations for each tumor type
Additional references
Practice question #1
Practice answer #1
D. Subependymoma. The photomicrograph shows round, uniform tumor cells arranged in clusters / nests within a dense fibrillary background. This is highly characteristic histomorphology for subependymoma. Answer C is incorrect because reactive gliosis generally does not form a mass lesion and is characterized by relatively evenly spaced astrocytes with abundant eosinophilic cytoplasm. Answer A is incorrect because astrocytoma, IDH mutant, WHO grade 2 is an infiltrating neoplasm not commonly encountered in the fourth ventricle. Answer B is incorrect because pilocytic astrocytoma is more commonly encountered in the cerebellum or optic pathway and is characterized by bipolar tumor cells, biphasic tumor background (compact areas and cystic areas) and the presence of Rosenthal fibers, eosinophilic granular bodies and degenerative atypia.
Comment Here
Reference: Glioma overview
Comment Here
Reference: Glioma overview
Practice question #2
A 6 year old girl presents with altered mental status. Brain imaging reveals an expansile mass centered in the pons. Biopsy is performed and demonstrates a diffuse glioma with rare mitotic activity. There is no microvascular proliferation or necrosis observed. Immunohistochemistry (IHC) for H3K27me3 shows loss of nuclear expression and H3K27M IHC is positive. By current WHO standards, what is the grade of this tumor?
- 1
- 2
- 3
- 4
Practice answer #2
D. 4. By current WHO classification, a diffuse glioma involving a midline structure that harbors H3K27M alteration is WHO grade 4 and is associated with malignant clinical behavior. Therefore, by definition, Answers A, B and C are incorrect. WHO grade 1 neoplasms (A), including pilocytic astrocytoma, are clinically benign; although these neoplasms can cause significant clinical morbidity if located in neuroanatomically exquisite locations. WHO grade 2 and 3 neoplasms (B and C), such as oligodendroglioma, IDH mutant and 1p / 19q codeleted, represent tumors with intermediate clinical behavior.
Comment Here
Reference: Glioma overview
Comment Here
Reference: Glioma overview