Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Karamchandani D. Barrett esophagus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophagusBarrettsgeneral.html. Accessed August 1st, 2025.
Definition / general
- American College of Gastroenterology (ACG) 2016 BE definition: extension of salmon colored mucosa into the tubular esophagus extending ≥ 1 cm proximal to the gastroesophageal (GE) junction with biopsy confirmation of intestinal metaplasia (goblet cells) (Am J Gastroenterol 2016;111:30)
- British Society of Gastroenterology 2014 BE definition: columnar epithelium with or without goblet cells extending ≥ 1 cm proximal to the GE junction (Gut 2014;63:7)
Essential features
- Secondary to longstanding gastroesophageal reflux disease (GERD)
- BE requires both endoscopic (abnormal mucosa ≥ 1 cm proximal to the GE junction) and histologic (metaplastic epithelium) correlation for diagnosis (Am J Gastroenterol 2016;111:30, Am J Surg Pathol 2017;41:e8)
- Necessity of intestinal metaplasia (IM) for diagnosis of BE varies; IM required in United States and part of Europe, IM not necessary in UK and Japan (Am J Gastroenterol 2016;111:30, Gut 2014;63:7)
- BE predisposes patient to dysplasia and adenocarcinoma (Am J Surg Pathol 2017;41:e8, Am J Surg Pathol 2016;40:e45)
- Histologic assessment on H&E slide remains gold standard marker for diagnosing dysplasia and cancer prevention in BE (Am J Surg Pathol 2016;40:e83)
Terminology
- Long segment: any segment of BE measuring > 3 cm
- Short segment: any segment of BE measuring < 3 cm
- Z line: squamocolumnar junction
ICD coding
Epidemiology
- BE detected in about 10 - 15% of patients with GERD (Am J Gastroenterol 2016;111:30, Gastroenterol Hepatol (N Y) 2016;12:449)
- Symptom duration of GERD is a risk factor for BE
- Screening performed in men with chronic GERD symptoms with at least two additional risk factors (age > 50 years, white race, central obesity, smoking history or a confirmed family history of BE) (Am J Gastroenterol 2016;111:30, Gastroenterol Hepatol (N Y) 2016;12:449)
- Screening no longer indicated in women with chronic symptoms of GERD
- Screening not recommended for general population (patients without reflux symptoms)
Sites
- Distal esophagus, gastroesophageal junction
Pathophysiology
- Metaplasia in BE presumably results from cellular reprogramming
- GERD induced tissue damage reprograms immature progenitor cells to express columnar development transcription factors
- Tissue injury activates signaling pathways such as Hedgehog, BMP4 and NF-KB, and downregulates Notch signaling
- Signals lead to increased expression of SOX9 (induces columnar differentiation), FOXA2, CDX1 and CDX2 (induces intestinal differentiation) (J Clin Invest 2014;124:3767)
- Transdifferentiation (distinctive type of multilayered epithelium at the squamocolumnar junction with features of both squamous and columnar epithelium) may occur in BE (Am J Gastroenterol 2016;111:30)
Etiology
- Known risk factors (Am J Gastroenterol 2016;111:30):
- Chronic (> 5 years) GERD symptoms
- Advancing age (> 50 years)
- Male gender
- Tobacco usage
- Central obesity
- Caucasian race
- More common in first degree relatives of subjects with known BE
Diagrams / tables
Clinical features
- GERD symptoms
Diagnosis
- Characteristic endoscopic appearance (at least 1 cm segment of abnormal mucosa proximal to GE junction) plus characteristic histologic findings (metaplastic epithelium with intestinal metaplasia in USA)
- At least eight random biopsies recommended
- When eight biopsies not obtainable (as in short segment BE), at least four biopsies / cm of circumferential BE and one biopsy / cm in tongues of BE recommended
- Normal Z lines and Z lines with less than 1 cm of variability should not be biopsied (Am J Gastroenterol 2016;111:30, Gastroenterol Hepatol (N Y) 2016;12:449)
Laboratory
- Evaluate H&E step sections from biopsies to document goblet cell metaplasia
Radiology description
- Advanced imaging technologies continue to be an area of research interest
- Routine use of high definition white light endoscopy now recommended as a part of surveillance (Am J Gastroenterol 2016;111:30)
- Other advanced imaging techniques (beyond electronic chromoendoscopy) not recommended at this time
Prognostic factors
- Risk of cancer progression for nondysplastic BE is 0.2 - 0.5% per year (Am J Gastroenterol 2016;111:30)
- Annual risk of progression with low grade dysplasia (0.7% per year) and high grade dysplasia (7% per year)
Treatment
- BE patients should receive once daily proton pump inhibitor therapy
- Aspirin, other NSAIDs or antireflux surgery not routinely prescribed or performed
- Surveillance should be performed with high definition / high resolution white light endoscopy
- For BE without dysplasia, endoscopic surveillance at intervals of three to five years
- Endoscopic surveillance should employ four quadrant biopsies at 2 cm intervals in patients without dysplasia and 1 cm intervals in patients with prior dysplasia
- For BE dysplasia, refer to BE dysplasia section for surveillance guidelines
- Endoscopic mucosal resection or endoscopic ablation therapy: preferred treatment options for patients with dysplasia (refer to BE dysplasia section) (Am J Gastroenterol 2016;111:30)
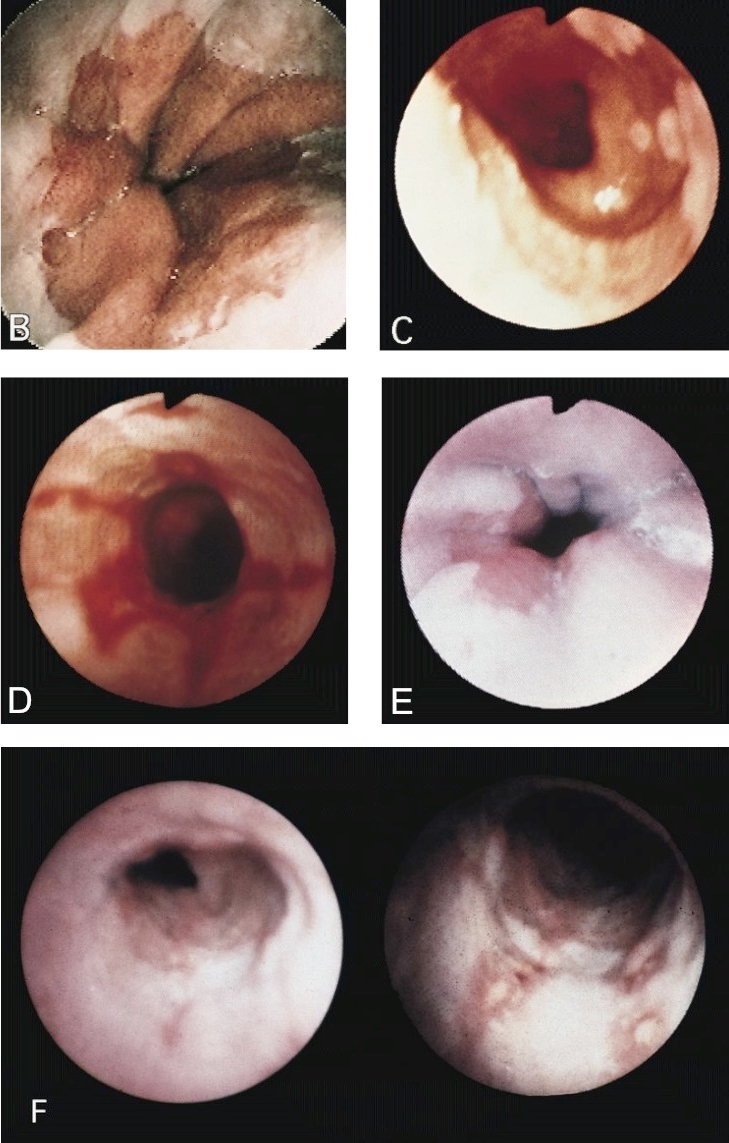
Clinical images
Gross description
- Red / salmon colored mucosa between pale squamous mucosa of lower esophagus and lush pink gastric mucosa; may have tongues extending up from GE junction
- Endoscopists utilize the Prague classification to describe disease extent (include circumferential and maximal segment length) in Barrett mucosa (Am J Gastroenterol 2016;111:30)
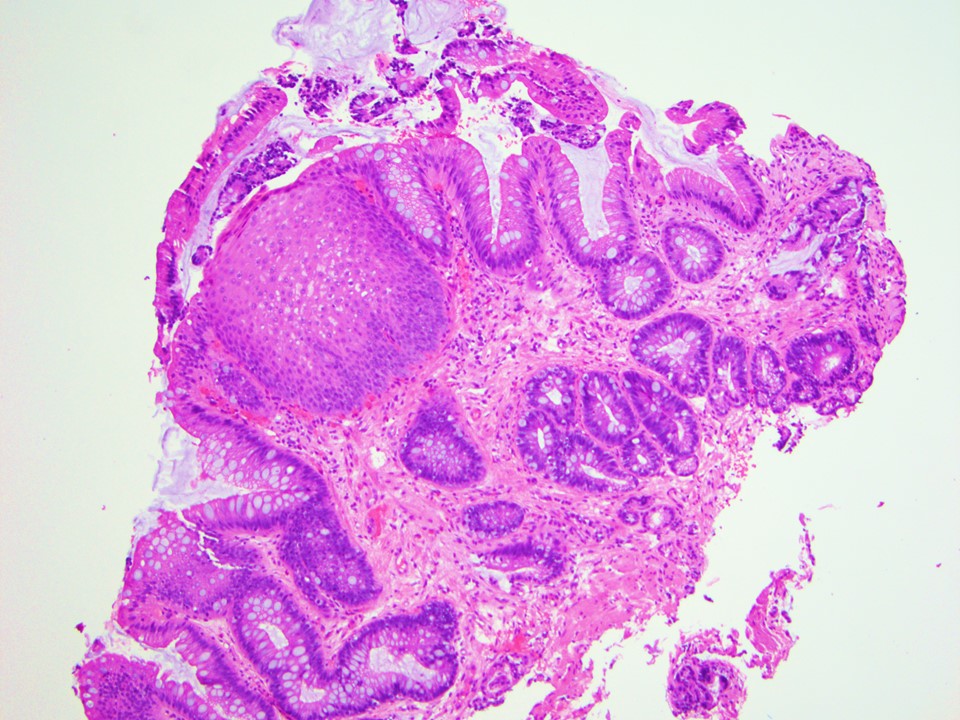
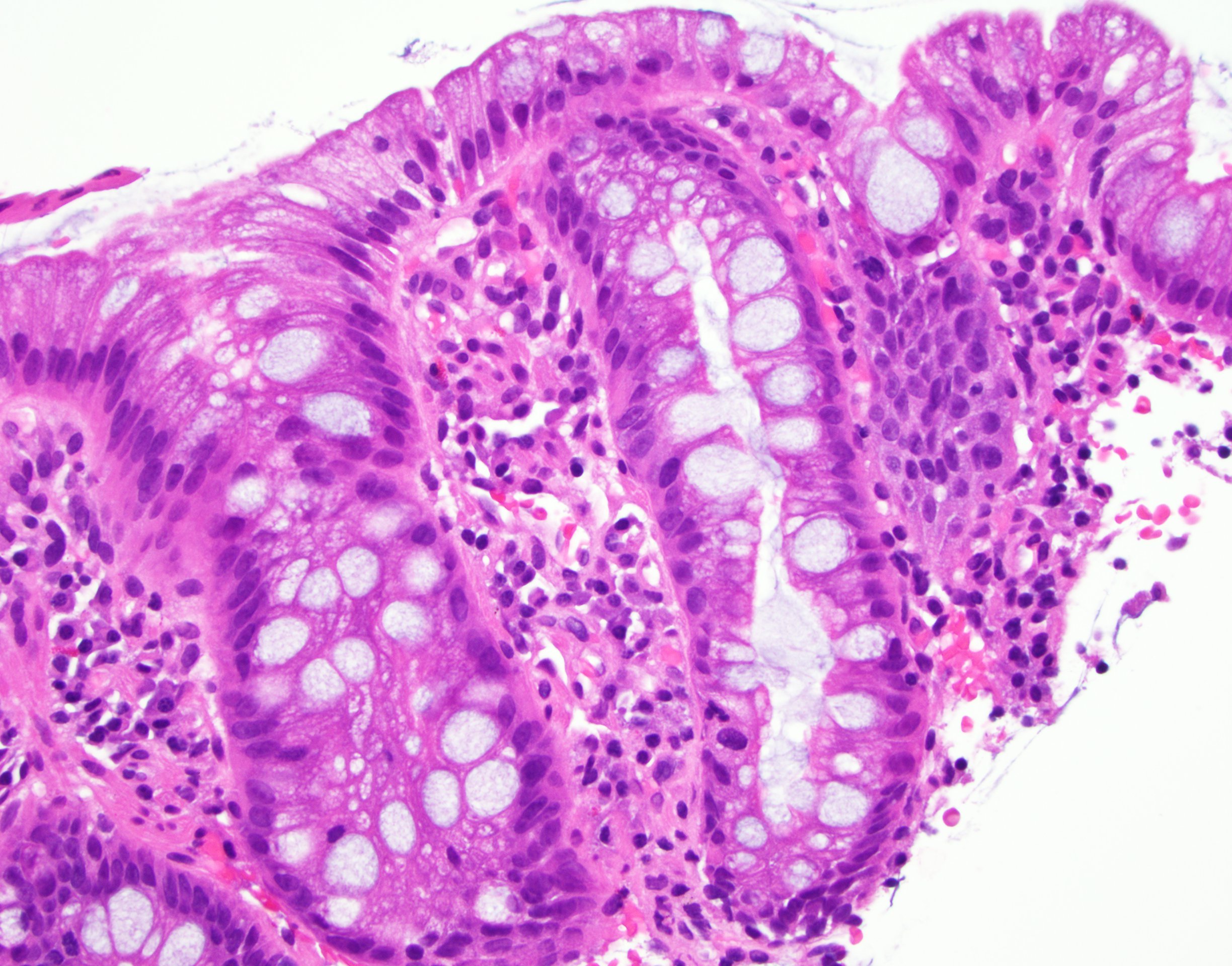
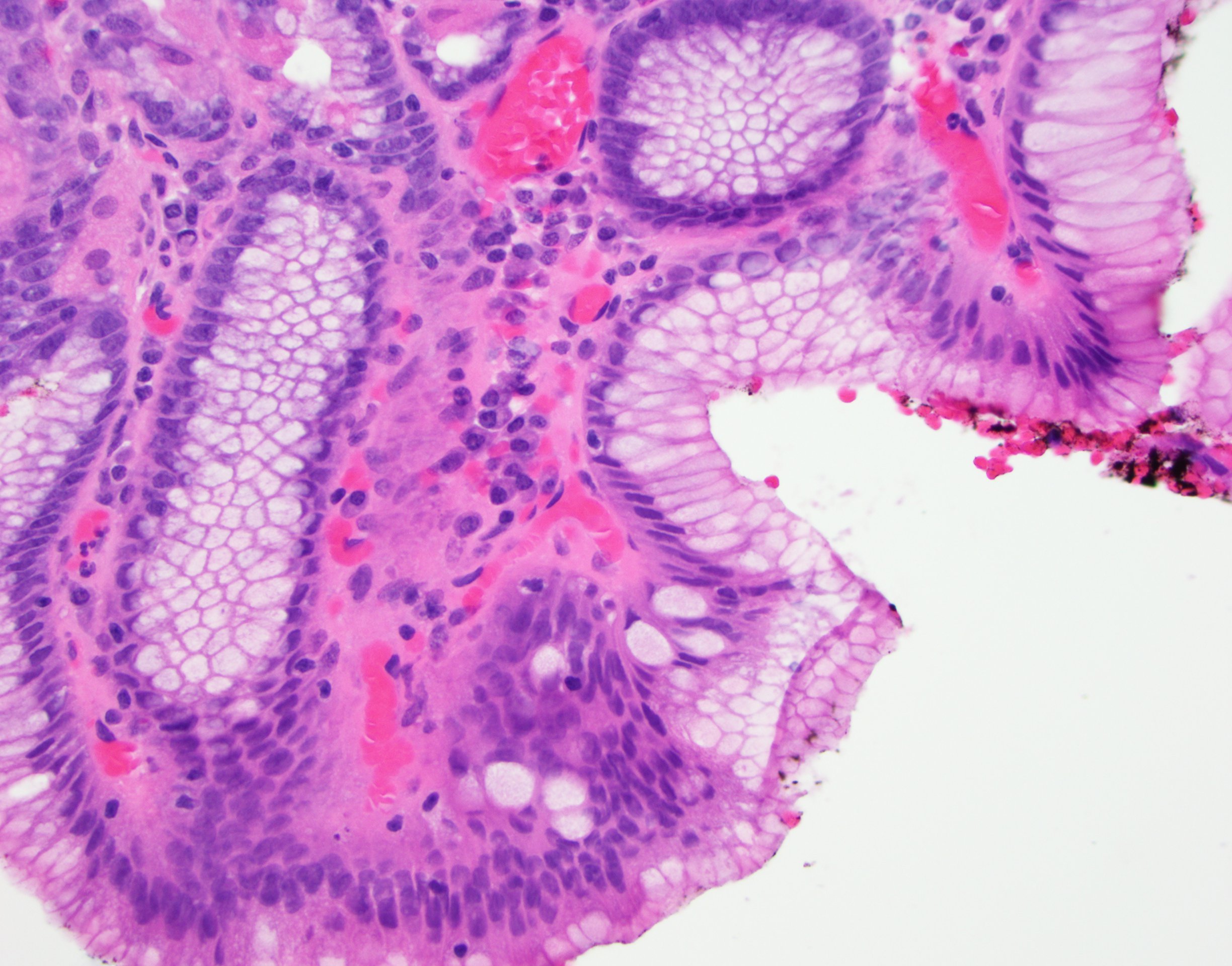
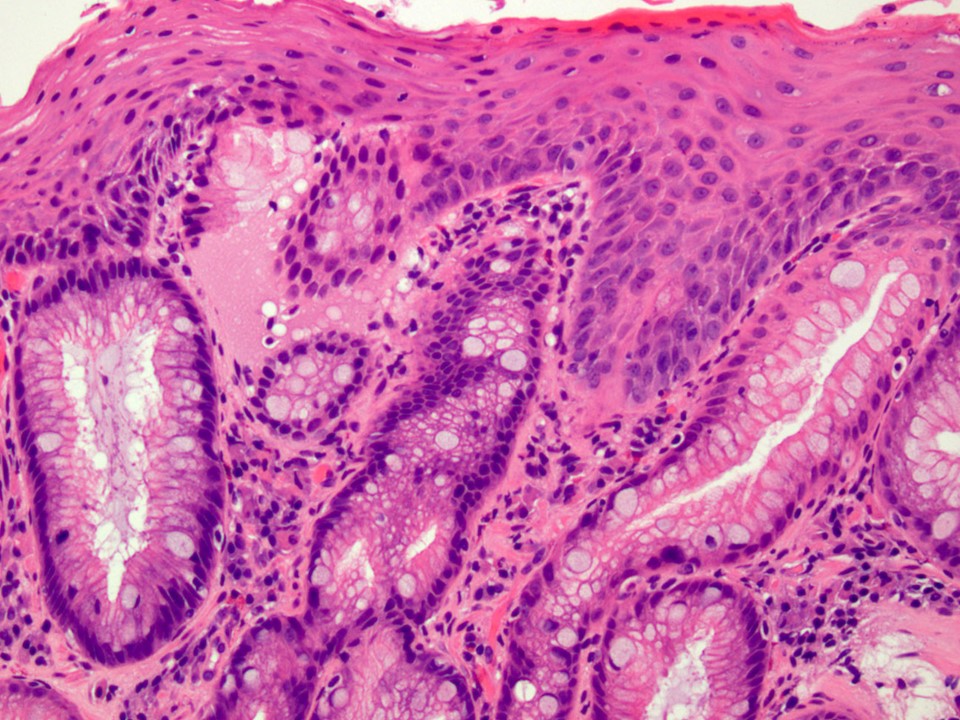
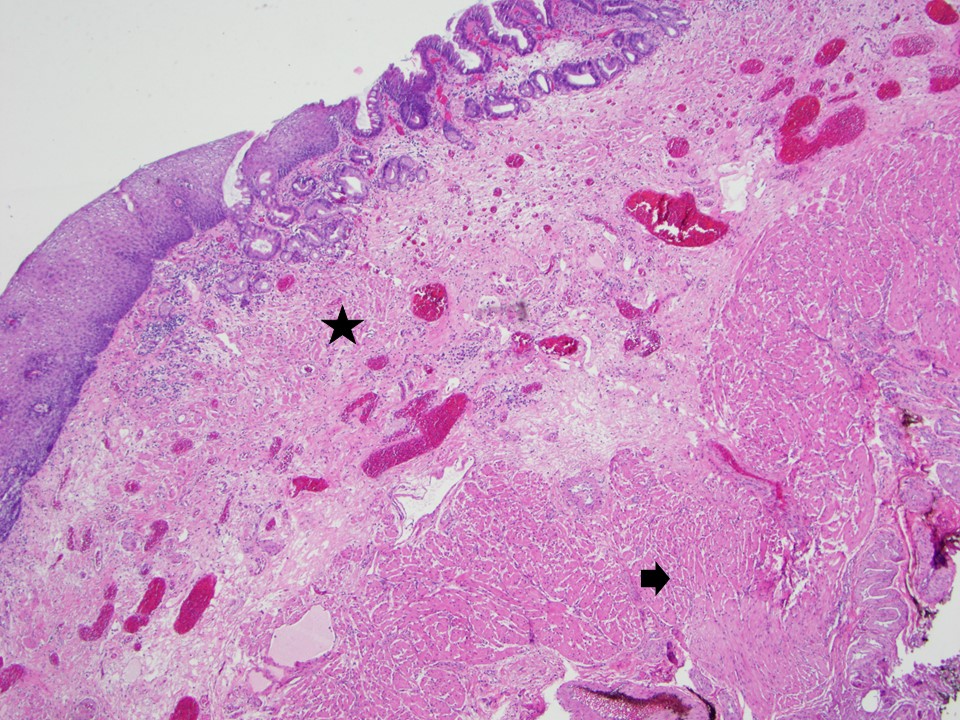
Microscopic (histologic) description
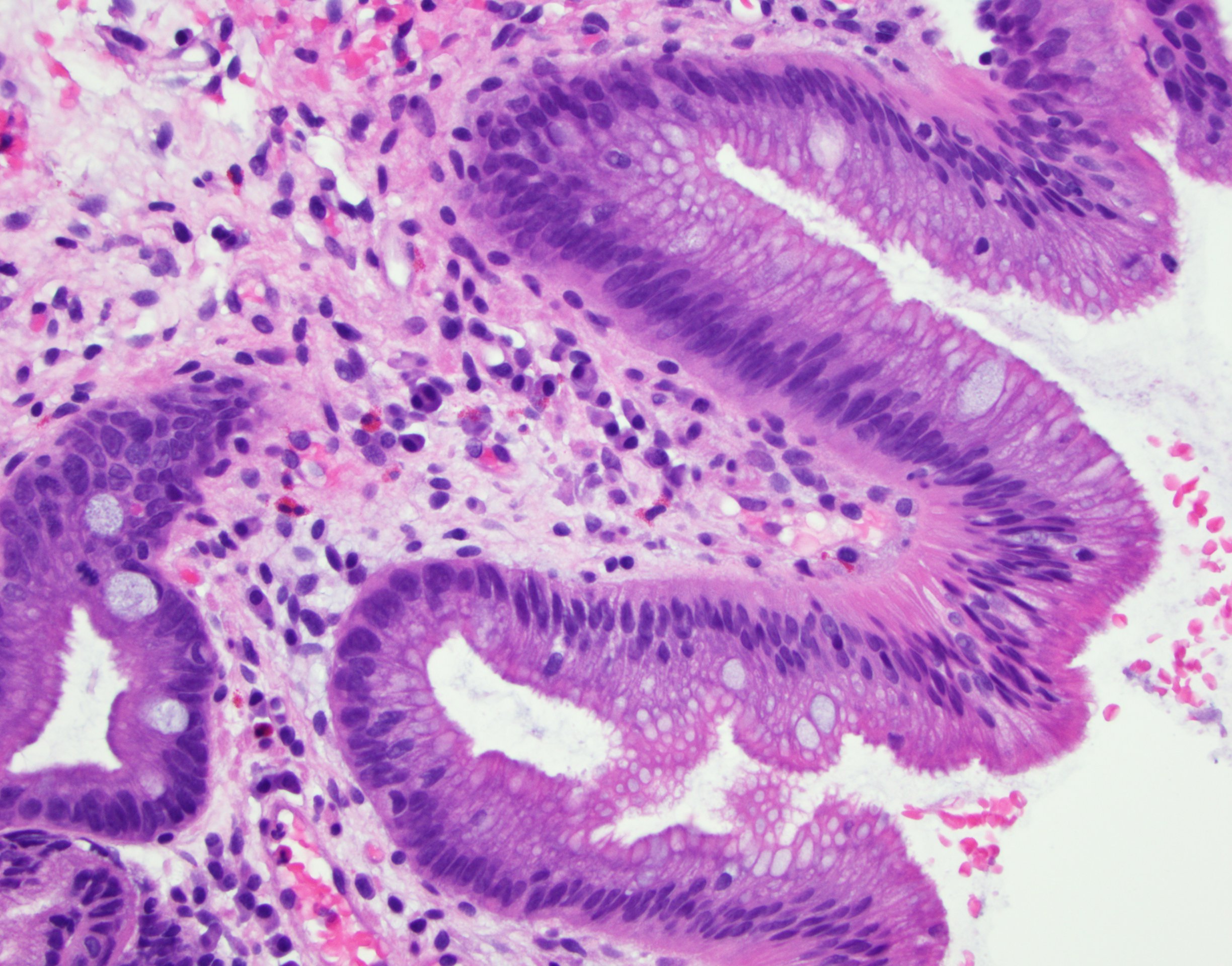
- Esophageal squamous epithelium replaced by columnar epithelium of intestinal type with goblet cells
- True goblet cells: rounded shape, clear to bluish cytoplasmic mucin, randomly scattered, mucin usually indents nucleus
- Nondysplastic reactive BE shows the presence of four lines (Surg Pathol Clin 2017;10:781)
- First line: gastric foveolar type mucin droplet
- Second line: base of the foveolar mucin vacuole
- Third line: cytoplasm below the mucin vacuole
- Fourth line: row of nuclei
- Baseline atypia of Barrett mucosa - some basal glands may show nuclear enlargement and stratification but there is complete surface maturation; this is considered negative for dysplasia
- Duplication of muscularis mucosae characteristic finding in BE; observed in 92% of BE resections, involving 5% of the Barrett segment (Am J Surg Pathol 2007;31:1719)
- Squamous overgrowth over metaplastic epithelium, hybrid glands, presence of esophageal ducts have high specificity for BE (Am J Surg Pathol 2007;31:1733)
- Postablation histology: replacement of columnar mucosa to squamous (neosquamous) mucosa; residual metaplastic epithelium may persist beneath the squamous epithelium (known as buried Barrett’s) and progress to dysplasia or carcinoma
Microscopic (histologic) images
Cytology description
- Cytology has good sensitivity (82%) and specificity (88%) for identifying intestinal metaplasia with moderate interobserver agreement (J Am Soc Cytopathol 2015;4:113)
- Cytology may be poised to synergize with advances in other techniques for management of patients with Barrett esophagus
- Improvements in brushing devices may help to decrease the nondiagnostic rate (Diagn Cytopathol 2011;39:60)
Positive stains
- H&E remains the gold standard for diagnosis of BE and assessing Barrett dysplasia (Am J Surg Pathol 2016;40:e83)
- Alcian blue (at pH 2.5) stain acidic mucin in true goblet cells as bright purple blue; helpful in distinguishing true goblet cells from pseudogoblet cells in challenging cases, reflexive use on biopsies not justified
Negative stains
- Special stains typically not needed to diagnose BE (Am J Surg Pathol 2016;40:e83)
- Use of mucin glycoproteins (MUC2, MUC5AC) to diagnose BE currently not indicated
- Use of markers of intestinal phenotype (CDX2, Das-1, villin, HepPar1) to diagnose BE currently not indicated
- Use of CK7 and CK20 to distinguish BE from intestinal metaplasia of the gastric cardia not indicated as not adequately specific
Electron microscopy description
- Mucin granules in metaplastic cells
Sample pathology report
- No endoscopy report provided and there is intestinal metaplasia in the biopsy
- Esophagus, distal, biopsy:
- Barrett mucosa, negative for dysplasia (see comment)
- Comment: Per 2016 ACG guidelines, the diagnosis of Barrett esophagus in this case is made owing to the presence of goblet cells, with the assumption that the biopsy is taken from distal esophagus and the mucosal irregularity extends to at least 1 cm above the top of the gastric folds.
- Reference: Am J Gastroenterol 2016;111:30
- Esophagus, distal, biopsy:
- Endoscopy report provided and specifies that mucosal irregularity extends to at least 1 cm proximal to the gastroesophageal junction
- Esophagus, distal, biopsy:
- Barrett mucosa, negative for dysplasia
- Esophagus, distal, biopsy:
- No endoscopy report provided, there is intestinal metaplasia in the biopsy and the biopsy is labeled as gastroesophageal junction
- Gastroesophageal junction, biopsy:
- Gastric cardia type mucosa with intestinal metaplasia, negative for dysplasia (see comment)
- Comment: If the biopsy is taken from tubular esophagus and the mucosal irregularity extends to at least 1 cm above the top of gastric folds, then this represents Barrett esophagus. If the biopsy is taken from gastric cardia, then this represents intestinal metaplasia of the gastric cardia.
- Reference: Am J Gastroenterol 2016;111:30
- Gastroesophageal junction, biopsy:
- References: Ann Diagn Pathol 2019;39:111, Am J Gastroenterol 2016;111:30
Differential diagnosis
- Intestinal metaplasia of gastric cardia
- Need endoscopic correlation; lower rate of progression to dysplasia or carcinoma
- Pseudogoblet cells
- Clustered, characteristically arranged in a back to back or linear and continuous array unlike true goblet cells
- PAS / Alcian blue may be helpful, but sometimes pseudogoblet cells show nonspecific weak alcianophilia on PAS / Alcian blue
Additional references
Practice question #1
Below is a picture of endoscopic biopsy from a 60 year old man with a clinical history of reflux symptoms and the biopsy is labeled as gastroesophageal junction. The endoscopy report is not provided. How would you sign out the case?
- Barrett esophagus, negative for dysplasia
- Gastric mucosa with intestinal metaplasia, consistent with Barrett esophagus
- Gastric cardia type mucosa with intestinal metaplasia (see comment)
- Barrett esophagus with low grade dysplasia
Practice answer #1
C. Gastric cardia type mucosa with intestinal metaplasia, with a comment stating that endoscopic evidence of abnormal mucosa for at least 1 cm proximal to the gastroesophageal junction is required for a diagnosis of Barrett esophagus.
Comment Here
Reference: Barrett esophagus
Comment Here
Reference: Barrett esophagus
Practice question #2
What is the best stain to diagnose Barrett esophagus on a biopsy?
- H&E stain
- PAS with Alcian blue special stain
- CDX2 immunostain
- CK7 immunostain
Practice answer #2