Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Function of neutrophils | Peripheral smear description | Peripheral smear images | Positive markers or stains | Negative markers or stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Wang L, Prakash S. Reactive neutrophilia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/hematologyreactiveneutrophilia.html. Accessed October 2nd, 2025.
Definition / general
- Defined by an absolute neutrophil count (ANC) that exceeds the age related normal range
- Normal reference interval (individually established for each laboratory) is approximately 1.8 - 7.0 x 109/L in adults and 1.0 - 8.5 x 109/L in young children
- Absolute neutrophil count is higher in infants, with newborns having the highest absolute neutrophil count of any age (7.8 - 14.4 x 109/L)
- Neutrophil count also differs by race, with individuals of African descent having lower absolute neutrophil counts
- References: McPherson: Henry's Clinical Diagnosis and Management by Laboratory Methods, 22nd Edition, 2011, Curr Opin Hematol 2014;21:43
Essential features
- Commonly encountered laboratory finding and can be seen in benign and neoplastic disorders
- Clinical findings are extremely helpful in identifying the underlying etiology
- Leukemoid reaction: prominent granulocytosis with a variable degree of left shift
Terminology
- Granulocytosis
ICD coding
Sites
- Blood
Pathophysiology
- Demargination:
- Neutrophils attached to endothelium are released back into circulation
- Seen in stressful conditions that are accompanied by the release of endogenous adrenaline
- Absolute neutrophil counts are doubled within a few minutes but not associated with a left shift
- Decreased transit to solid tissues:
- Neutrophils remain in the blood for about 12 hours, before leaving the circulation and entering solid tissues
- Administration of corticosteroids can delay the transit from blood to solid tissues, resulting in a mild to moderate neutrophilia but not associated with left shift
- Mobilization from the maturation storage pool of the bone marrow:
- A large reserve compartment of neutrophils, bands and metamyelocytes in the bone marrow is released into the circulation, which may cause a mild left shift
- Infections and other inflammatory processes are the most common causes
- Increased production:
- Granulocyte colony stimulating factor (G-CSF) mediated increases of granulopoiesis within the bone marrow
- Seen with administration of G-CSF or in chemokine producing neoplasms
- Reference: Weksler: Wintrobe's Atlas of Clinical Hematology, 2nd Edition, 2017
Etiology
- Infection: bacterial infection is the most common cause; occasional viral infections such as severe acute respiratory distress syndrome (SARS) or Hantavirus pulmonary syndrome (HPS)
- Medication effect: most commonly granulocyte colony stimulating factor (G-CSF) and glucocorticoids
- Others: acute stressful events such as burns or trauma; smoking; paraneoplastic syndrome
- Reference: Kjeldsberg: Practical Diagnosis of Hematologic Disorders, 5th Edition, 2010
Clinical features
- Abnormal CBC with neutrophilia
- Clinical features are variable, based on the etiology of the neutrophilia (e.g., infection, medication use, stressful events)
- Reactive neutrophilia typically does not cause splenomegaly
- Reference: StatPearls: Neutrophilia [Accessed 9 February 2023]
Diagnosis
- Based on automated CBC with differential testing or peripheral blood smear examination
- Normal neutrophil contains 3 to 5 nuclear lobes
Function of neutrophils
- Provide first line of defense against microorganisms
- Mediates acute inflammatory response
- Most abundant leukocyte in the circulation
- Antimicrobial:
- Degranulates and releases myeloperoxidase, an enzyme stored in azurophilic granules of the neutrophils, into the extracellular space
- Phagocytosis of pathogens
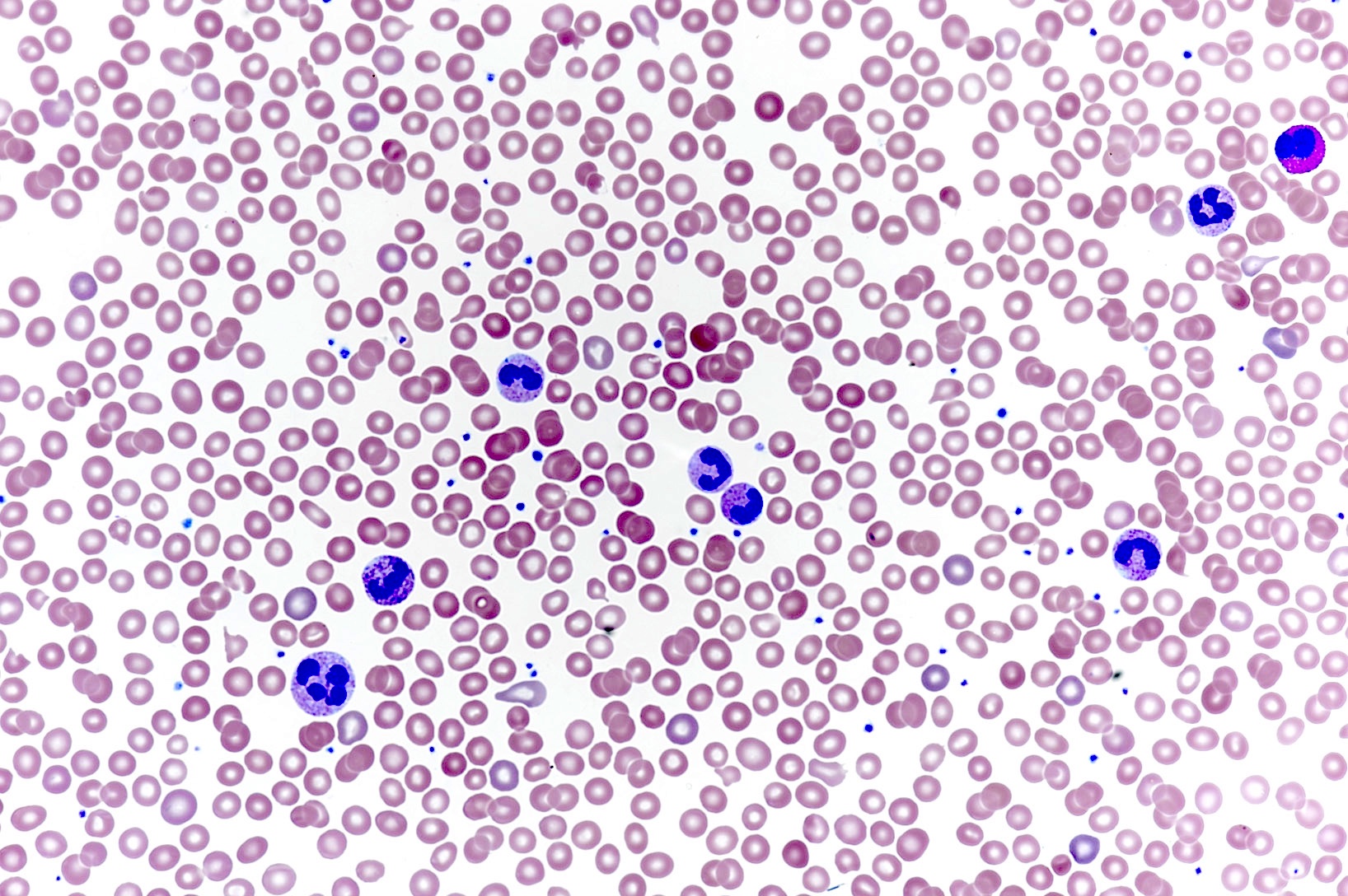
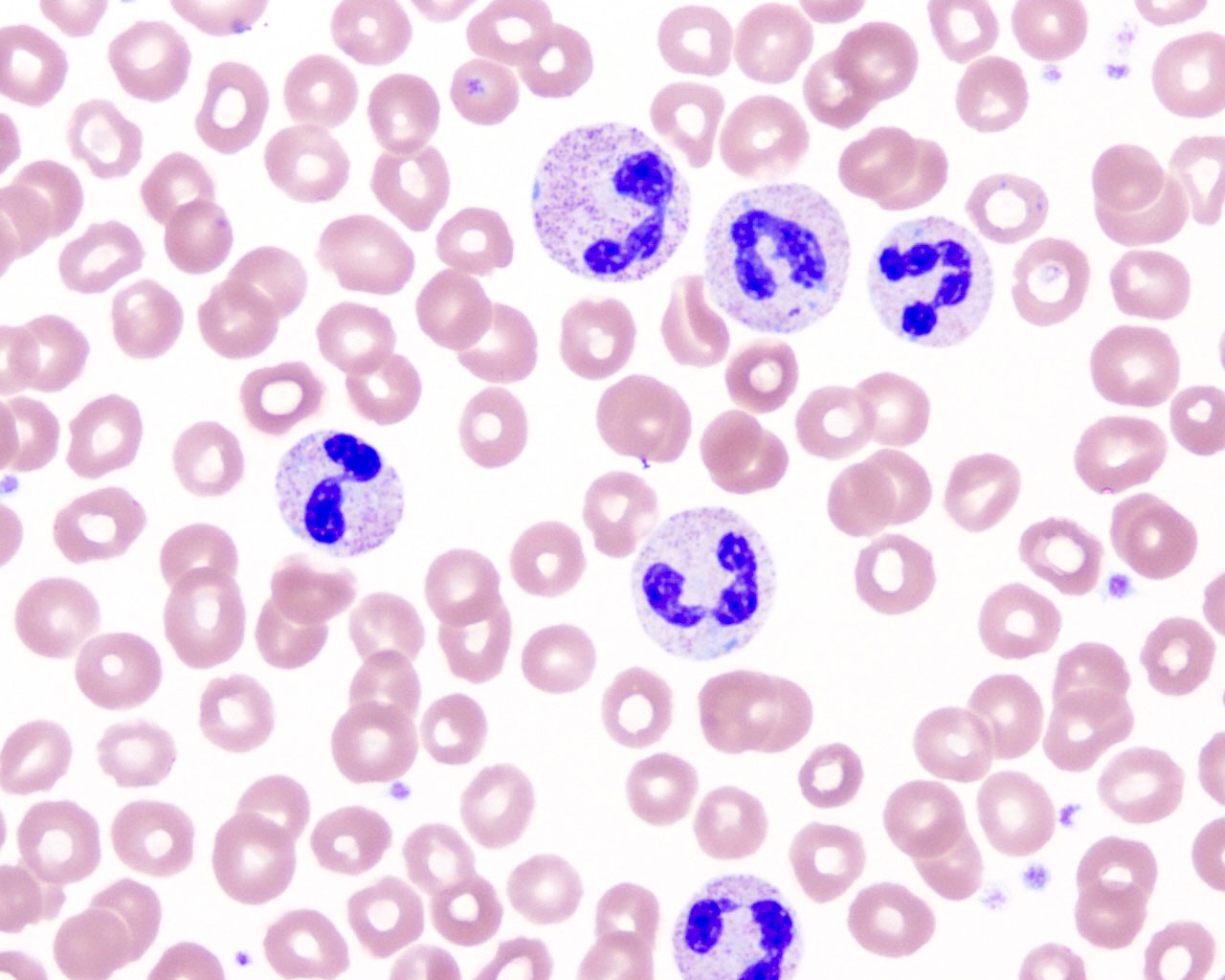
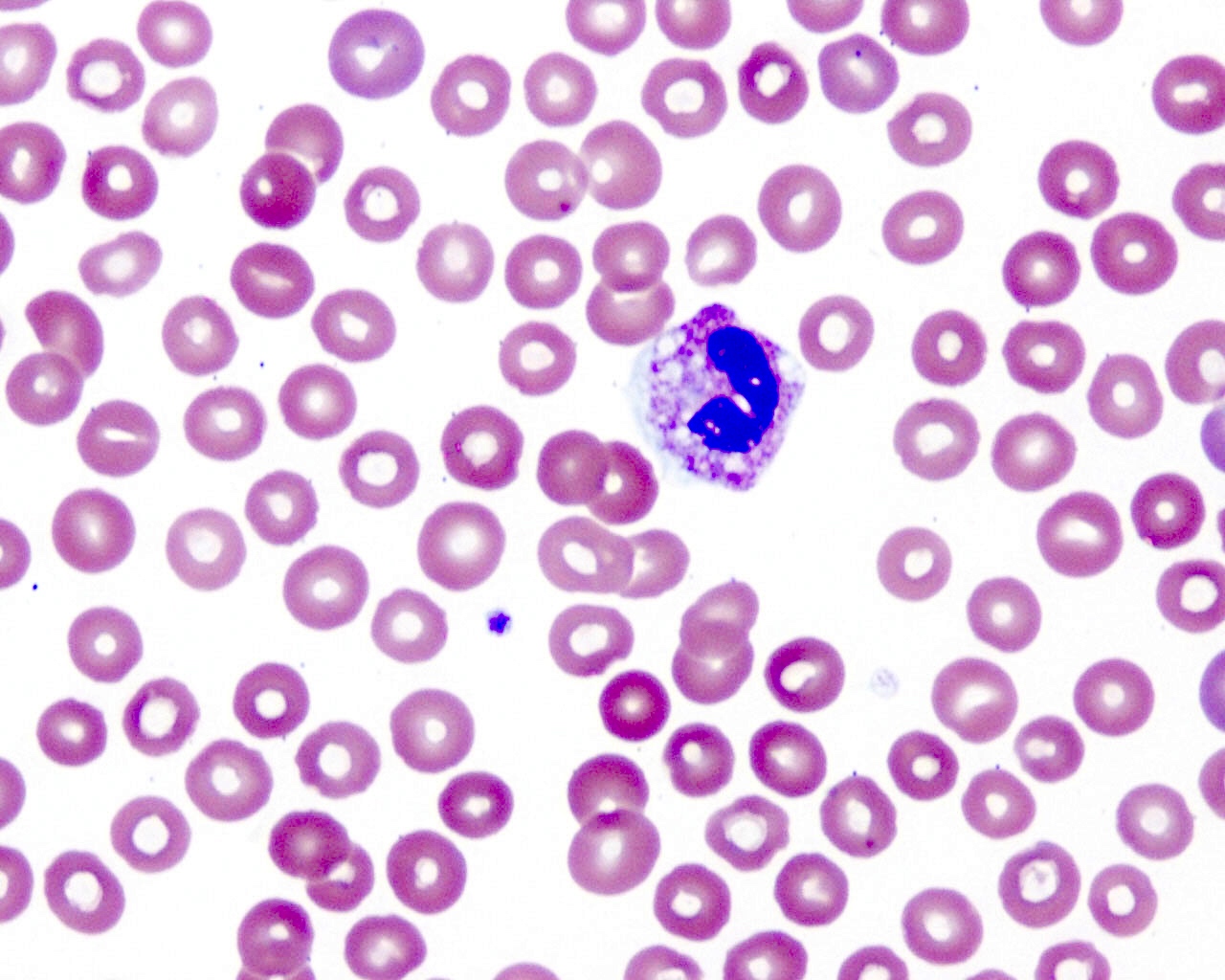
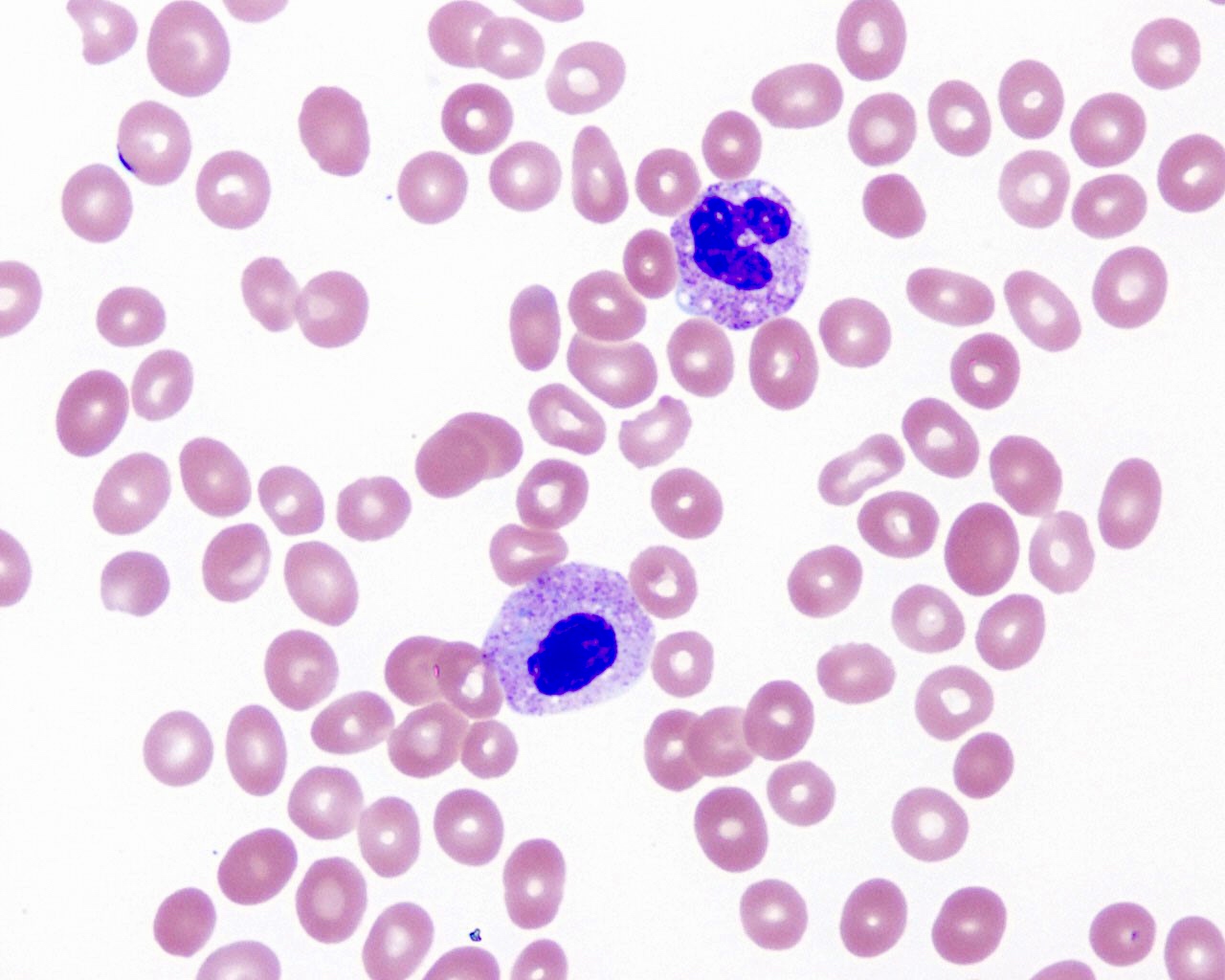
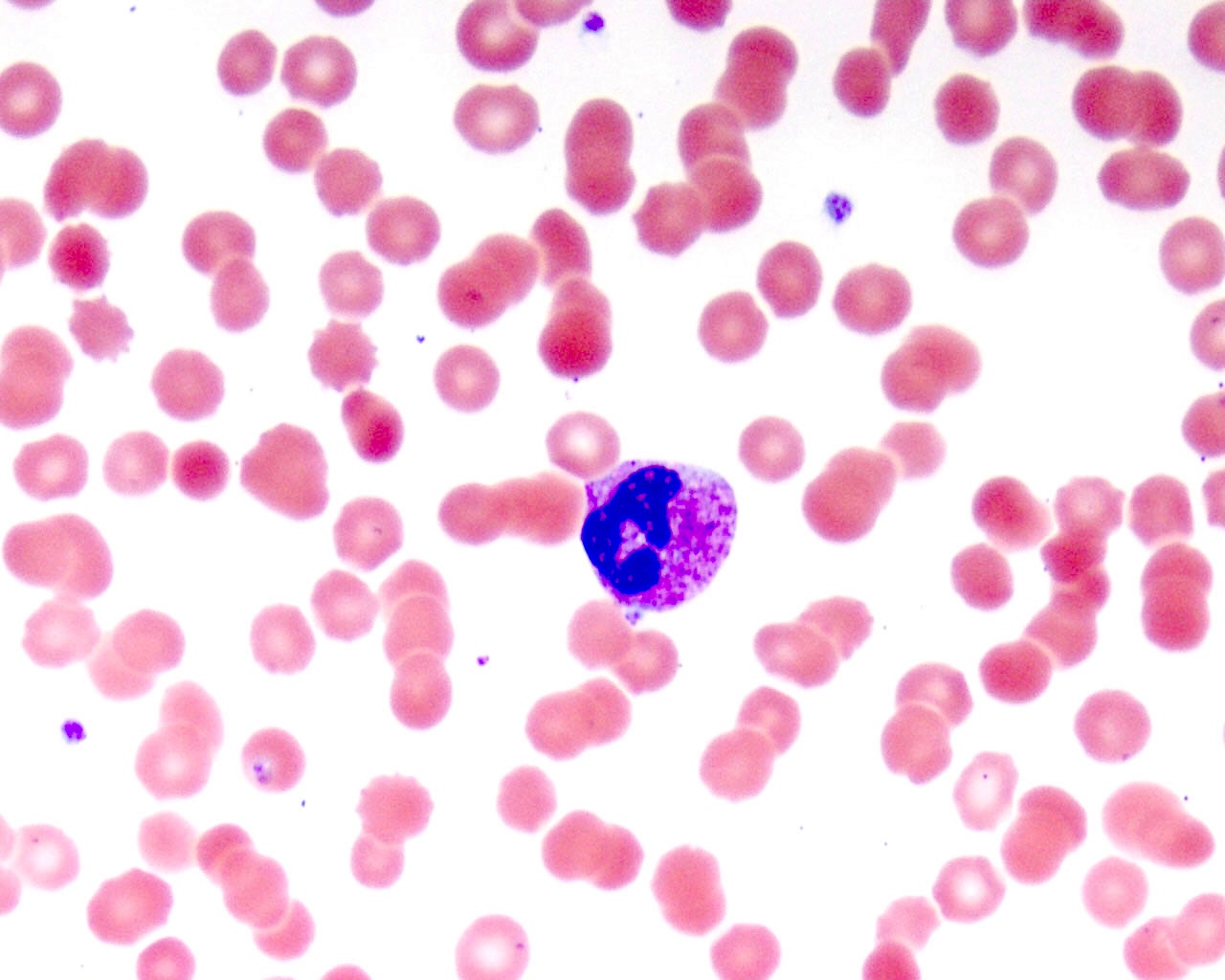
Peripheral smear description
- Absolute neutrophilia
- Reactive neutrophilia, as seen in infections, usually demonstrates toxic granulation, Döhle bodies and cytoplasmic vacuolization
- Döhle bodies are pale cytoplasmic inclusions that are parallel stacks of rough endoplasmic reticulum with bound ribosomes
- Toxic granulation represents either retained primary granules or altered uptake of stain by secondary granules
- Prominent cytoplasmic vacuoles in neutrophils are usually associated with sepsis
- Variable degree of left shift in the granulocytic lineage can be seen
- In adults with infections, the left shift is usually mild (bands and metamyelocytes) with absent or rare blasts
- In pediatric patients and in patients receiving G-CSF, the left shift can be prominent
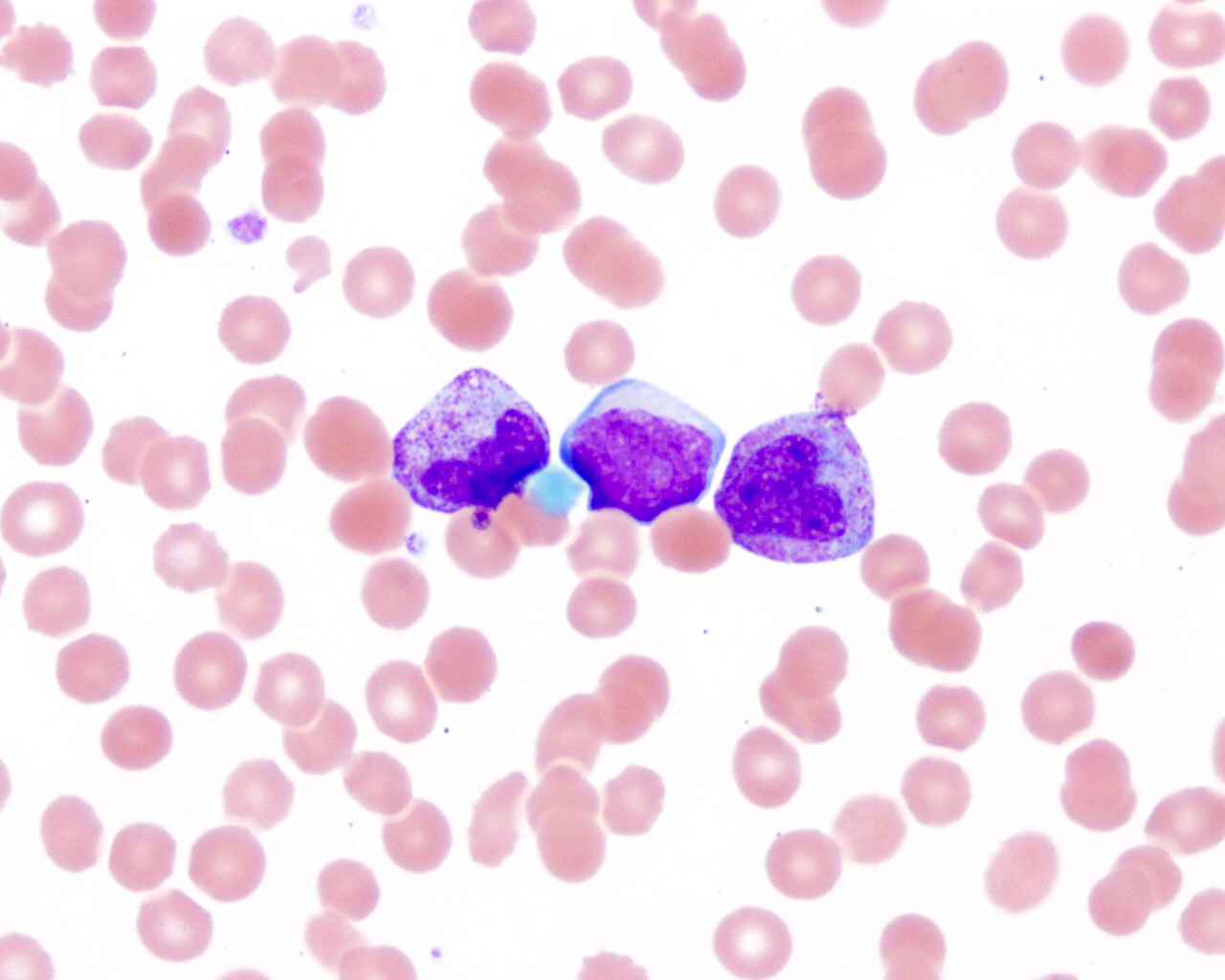
- In these adult and pediatric patients, binucleated neutrophils or very large neutrophils can sometimes be present and should not be interpreted as dysplasia
- Hypergranulation induced by G-CSF therapy shows a high density of granules, which stain redder than toxic granulation and often obscure the nucleus; left shifted granulocytic maturation can be seen in the marrow with G-CSF administration
- In reactive neutrophilia, white blood cell (WBC) count is usually < 30 x 109/L, except in pediatric patients with infection or patients receiving G-CSF; basophils are usually not increased
- Blasts are very rare and are usually seen only in patients receiving G-CSF or in pediatric patients
- With peripheral reactive neutrophilia, the bone marrow demonstrates granulocytic hyperplasia with a full spectrum of maturation
- References: Weksler: Wintrobe's Atlas of Clinical Hematology, 2nd Edition, 2017, Int J Lab Hematol 2014;36:279, Hematol Pathol 1994;8:55
Peripheral smear images
Positive markers or stains
Sample pathology report
- Blood smear:
- Reactive neutrophilia (see comment)
- Comment: Neutrophilia with toxic changes, left shift and rare blasts, consistent with cytokine effect or inflammatory changes. Clinical correlation is recommended.
Differential diagnosis
- Chronic myeloid leukemia (CML):
- Usually has very high WBC (> 50 x 109/L) with prominent left shift with a myelocyte bulge and associated basophilia
- Toxic granulation is usually absent
- Blasts can be increased
- Splenomegaly is common
- Positive for BCR::ABL1 gene rearrangement or t(9;22)(q34;q11)
- Chronic neutrophilic leukemia (CNL):
- Marked leukocytosis (> 30 x 109/L) with absolute neutrophilia
- No significant left shift in peripheral blood (immature granulocytes are < 10% of WBC)
- Splenomegaly
- Mutational analysis is positive for CSF3R mutations in > 80% of cases
- In a patient with absolute neutrophilia, the distinction between reactive and neoplastic etiology (especially CML) requires integration of clinical, hematologic, morphologic and other laboratory parameters; it is extremely important to carefully review the clinical history for possible reactive etiologies of neutrophilia
Additional references
Practice question #1
A 45 year old man presented with leukocytosis of 28 x 109/L with prominent left shifted granulocytes, rare blasts and no basophilia in the peripheral smear review. What is the next step?
- Check clinical history and physical examination record
- Order BCR::ABL PCR
- Send peripheral blood for flow cytometry
- Suggest a marrow biopsy
Practice answer #1
A. Check clinical history and physical examination record to assess the possibility of a leukemoid reaction before proceeding to ancillary testing or an invasive procedure.
Comment here
Reference: Reactive neutrophilia
Comment here
Reference: Reactive neutrophilia
Practice question #2
A 2 day old baby girl presented with leukocytosis of 50 x 109/L. The peripheral blood smear review shows marked neutrophilia with prominent left shifted granulocytes and rare blasts. The baby's mother had chorioamnionitis. The baby has no splenomegaly on physical examination. What is the most likely diagnosis or information needed for diagnosis?
- Need flow cytometry study for diagnosis
- Need marrow biopsy for diagnosis
- Neoplasm, since the white cell count is too high
- Reactive neutrophilia
Practice answer #2