Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Nguyen NNJ, Downes MR. Paraganglioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderparaganglioma.html. Accessed July 27th, 2025.
Definition / general
- Nonepithelial neuroendocrine neoplasm producing catecholamine excess and derived from neural progenitors (Endocr Pathol 2022;33:90)
Essential features
- In patients presenting with catecholamine related symptoms, initial workup should include measurement of plasma or urine metanephrine and normetanephrine levels; patients with nonfunctional paraganglioma of the urinary bladder can be asymptomatic or present only with hematuria or irritative symptoms
- Classic histologic morphology: monomorphic cells with abundant eosinophilic / amphophilic cytoplasm arranged in a nested / zellballen pattern and separated by fibrovascular septa with sustentacular cells
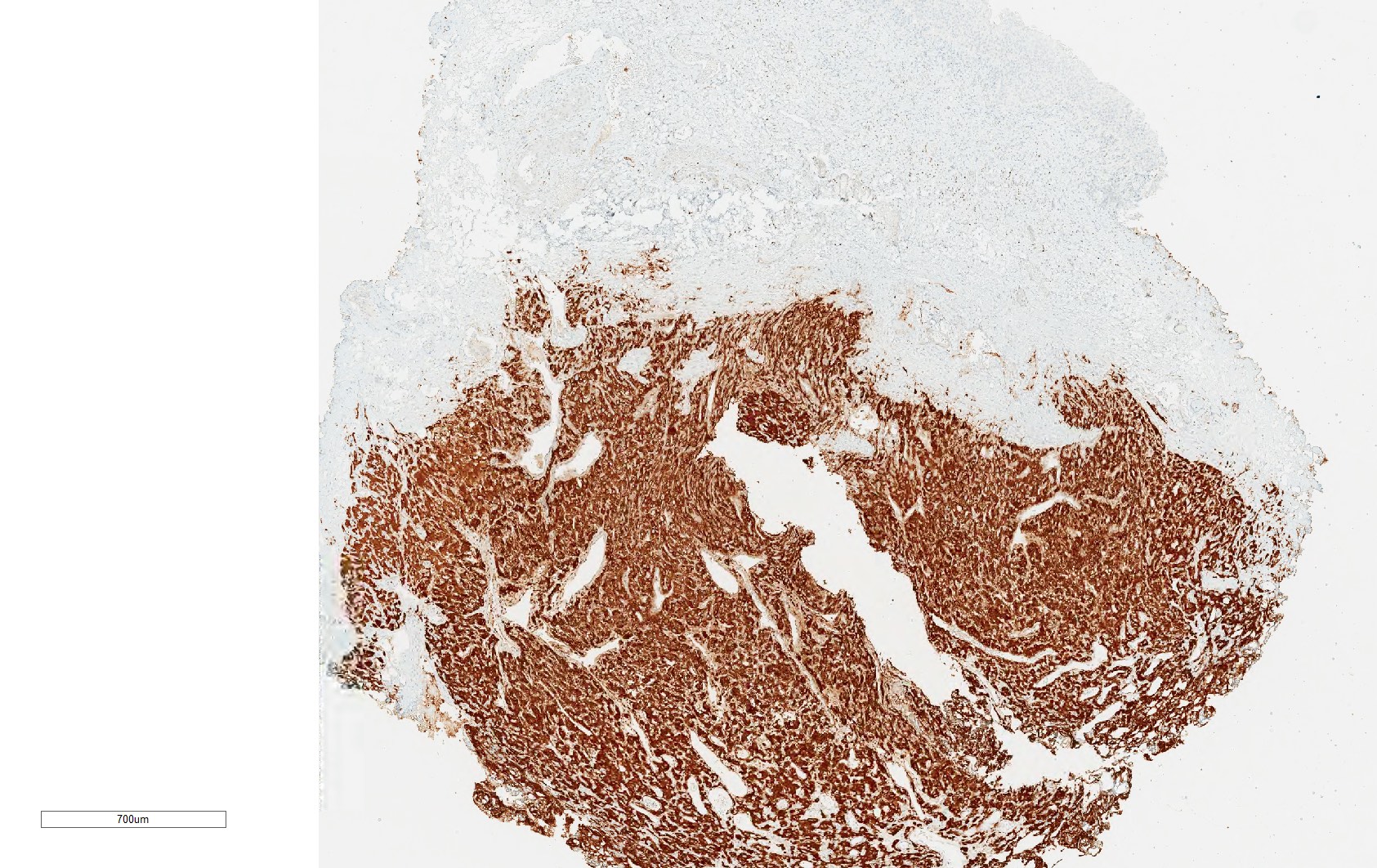
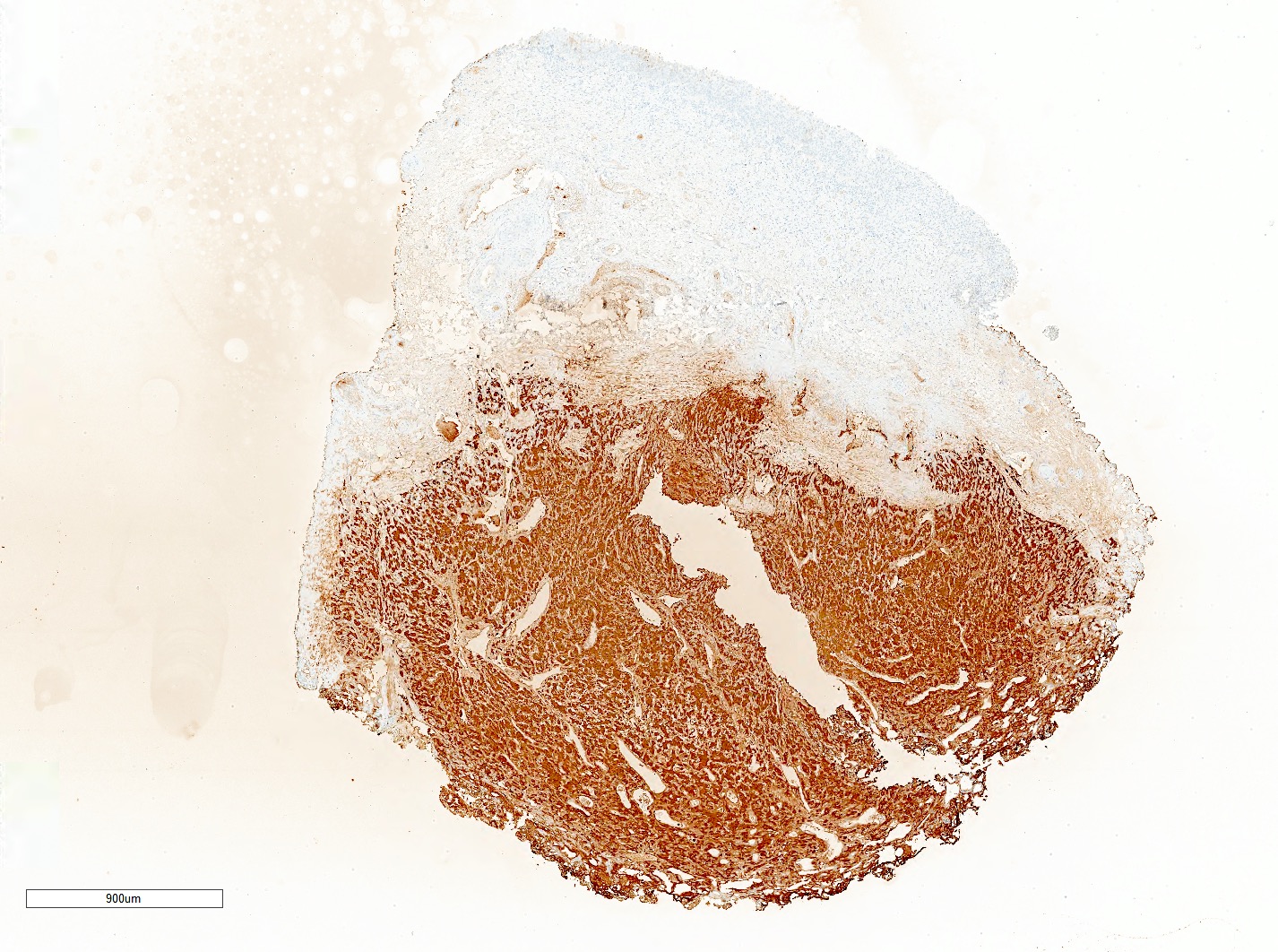
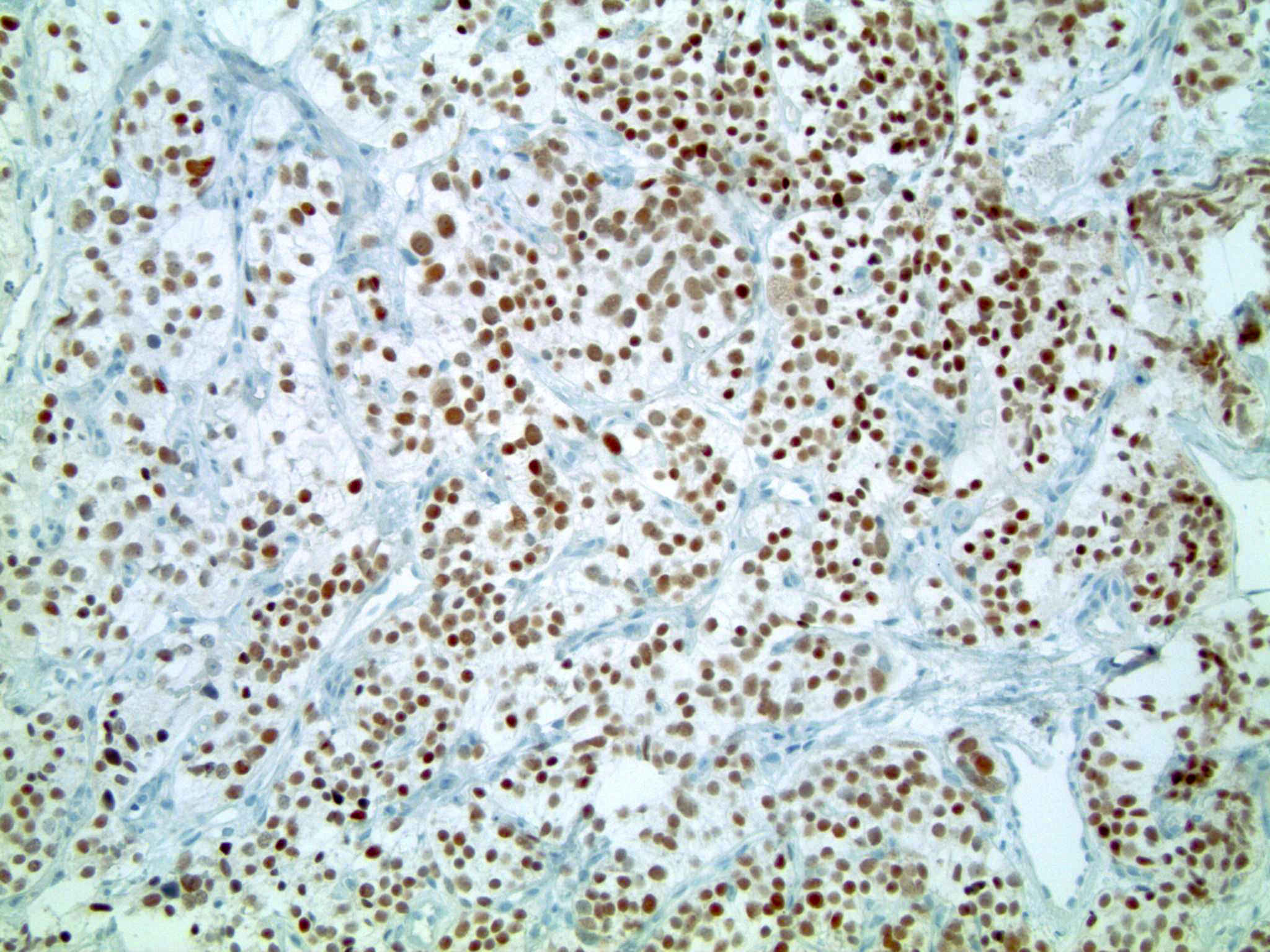
- Tumor cells are positive for GATA3 and neuroendocrine markers while negative for keratins; sustentacular cells are positive for S100 and SOX10
- All paragangliomas have a metastatic potential; many grading systems have been proposed
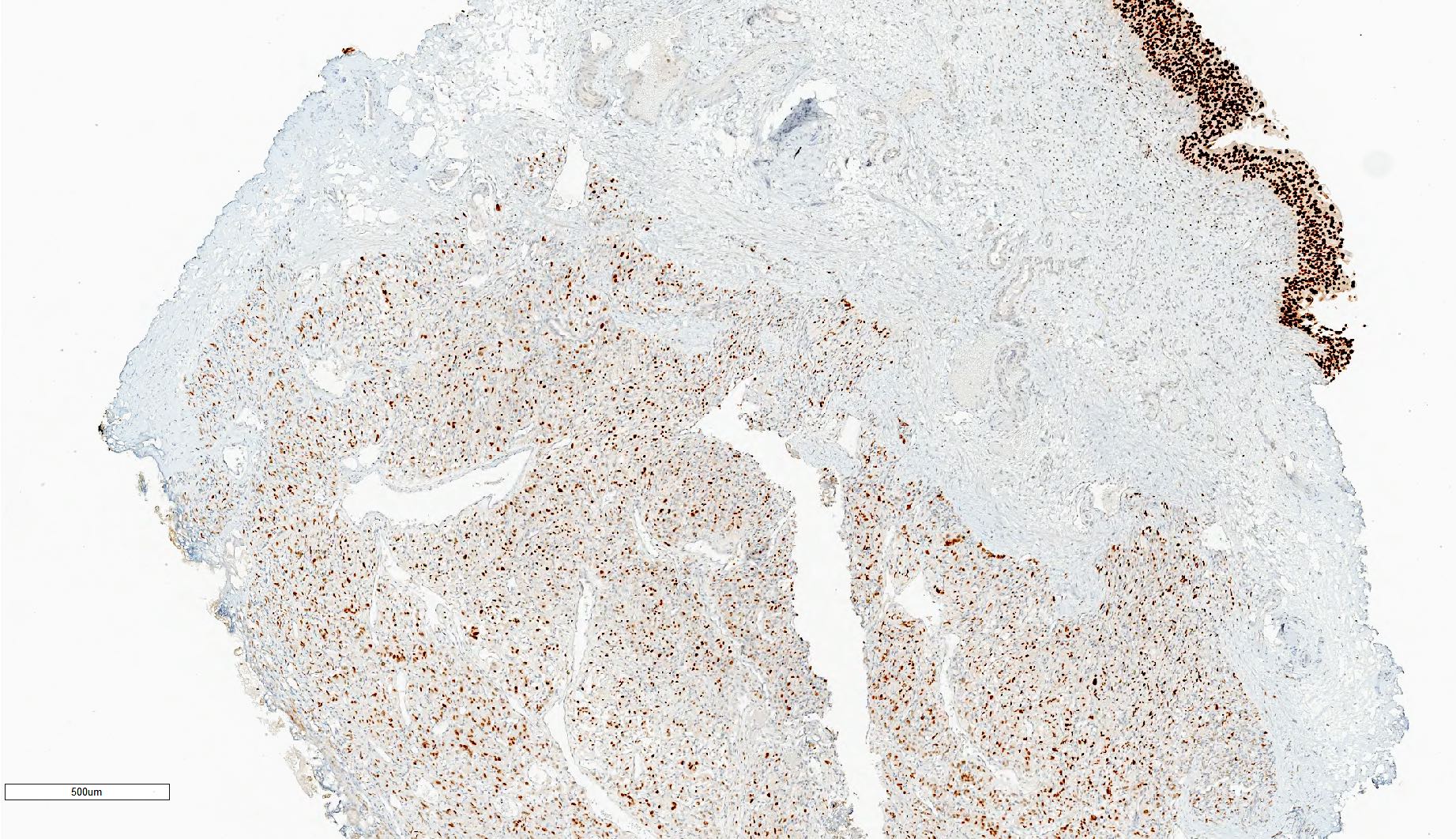
- SDHB germline mutation is the strongest genetic prognosticator of poor outcomes; SDHB immunohistochemistry is routinely used for its identification
Terminology
- Also called extra-adrenal paraganglioma and sympathetic paraganglioma (Endocr Pathol 2022;33:90)
- Discontinuation of the term extra-adrenal pheochromocytoma in the 2022 WHO classification
- Categorization into benign and malignant is discouraged since all paragangliomas hold a metastatic potential (Endocr Pract 2022;28:1253)
ICD coding
- ICD-O: 8693/3 - extra-adrenal paraganglioma, malignant
- ICD-11
- 2C9Y & XH1UN6 - other specified malignant neoplasms of urinary tract & extra-adrenal paraganglioma
- 2C9Y & XH0EW6 - other specified malignant neoplasms of urinary tract & paraganglioma, NOS
- 2C9Y & XH4G21 - other specified malignant neoplasms of urinary tract & sympathetic paraganglioma
Epidemiology
- Wide age range with a peak incidence between the third and sixth decades (mean: ~45 years) (Cancer 2000;88:844, BMC Urol 2013:13:22, Cancer Cell 2017;31:181, Urol Oncol 2017;35:457.e9)
- Younger age at diagnosis for patients with known disease causing germline mutations (Urol Oncol 2015;33:167.e13)
- Variation in sex distribution between studies
- Most commonly occurs in White patients, followed by Black patients and then patients of other races
Sites
- Genitourinary paragangliomas are rare among all paragangliomas and genitourinary malignancies (BMC Urol 2013:13:22, Urol Oncol 2017;35:457.e9)
- In the urinary tract, paraganglioma involves most commonly the bladder and rarely the urethra, renal pelvis and ureter
- Bladder paraganglioma can occur anywhere throughout the bladder
Pathophysiology
- Various pathogenetic classification groups
- Pseudohypoxia group (Cancer Cell 2017;31:181, F1000Res 2018:7:1500, Best Pract Res Clin Endocrinol Metab 2020;34:101416, Cancers (Basel) 2021;13:2389)
- VHL / EGLN1 / EPAS1 related (15 - 20% of paragangliomas)
- Tricarboxylic acid cycle (Krebs cycle) related (10 - 15% of paragangliomas; germline mutations in SDH subunits A - D, SDHAF2 assembly factor for SDH and FH gene)
- Kinase signaling group (50 - 60% of paragangliomas; germline or somatic mutations in RET, HRAS, NF1, TMEM127 and MAX genes)
- Wnt altered group (5 - 10% of paragangliomas; somatic mutations in CSDE1 and MAML3 genes)
- Disease modifying gene group (somatic mutations in ATRX, KMT2D, SETD2, TERT, TP53, KMT2C and SMARCA4 genes)
- Cortical admixture group (mutations in CYP11B1, CYP21A2 and STAR genes)
- Pseudohypoxia group (Cancer Cell 2017;31:181, F1000Res 2018:7:1500, Best Pract Res Clin Endocrinol Metab 2020;34:101416, Cancers (Basel) 2021;13:2389)
Etiology
- Vast majority of pediatric cases and ~50% of the adult cases have known disease causing germline mutations, most frequently in the SDHB gene (Urol Oncol 2015;33:167.e13, J Clin Endocrinol Metab 2017;102:1122, J Surg Oncol 2018;117:1217, Endocr Pathol 2021;32:134, Endocr Pathol 2022;33:90, Abdom Radiol (NY) 2022;47:1414)
- Genetic syndromes typically associated with paraganglioma include multiple endocrine neoplasia types 2A and 2B, neurofibromatosis type 1, von Hippel-Lindau syndrome, familial paraganglioma syndromes 1 and 4 (PGL1 and PGL4) and the Carney-Stratakis syndrome (J Surg Oncol 2018;117:1217)
Clinical features
- Can be asymptomatic or symptomatic (World J Urol 2022;40:2807)
- Classic presentation consists of catecholamine related symptoms / signs: paroxysmal hypertension, headache, syncope, diaphoresis, palpitations / tachycardia, dizziness (Cancer 2000;88:844, BMC Urol 2013:13:22, Pathol Res Pract 2015;211:183)
- Symptoms can be provoked / aggravated by the manipulation of the mass during cystoscopy or intraoperatively
- Bladder paragangliomas can be accompanied by hematuria and irritative symptoms including micturition attacks (World J Urol 2022;40:2807)
- Paragangliomas can cause mass effects
Diagnosis
- Recommended initial testing in patients with classic catecholamine related symptoms / signs consists of measuring plasma free or 24 hour urine fractionated metanephrines and normetanephrines (J Clin Endocrinol Metab 2014;99:1915, J Clin Med 2018;7:280)
- Computed tomography (CT) / magnetic resonance imaging (MRI) for the detection of primary / metastatic paraganglioma in the context of positive biochemical testing
- Cystoscopy can be performed in the context of hematuria or imaging detected bladder mass
- Histological diagnosis based on morphology and immunoprofile
- WHO essential criteria: morphology typical of paragangliomas
- WHO desirable criteria
- Identification of specific genetic mutations
- Positivity for synaptophysin and chromogranin A on immunohistochemistry
- Biochemical confirmation of catecholamine excess for functional tumors
- Compatible imaging studies
Laboratory
- Most bladder paragangliomas have elevated plasma and 24 hour urinary fractionated metanephrines and normetanephrines (J Clin Endocrinol Metab 2014;99:1915, J Clin Med 2018;7:280)
- Nonnegligeable number of SDHB mutated abdominal paragangliomas are biochemically silent (J Clin Endocrinol Metab 2008;93:4826)
- Plasma / urine catecholamines (epinephrine, norepinephrine, dopamine) and vanillylmandelic acid (VMA) are less sensitive markers
- Most SHDB mutated paragangliomas hypersecrete norepinephrine or both norepinephrine and dopamine, with a smaller subset hypersecreting only dopamine (Endocr Relat Cancer 2009;16:391)
Radiology description
- Ultrasound and color Doppler
- Heterogeneous echogenicity (hypoechoic > moderately echogenic > hyperechoic) (J Belg Soc Radiol 2020;104:25, Abdom Radiol (NY) 2022;47:1414)
- Bladder paragangliomas show broad based attachment to the bladder wall with peripheral mucosal line (Quant Imaging Med Surg 2023;13:2008)
- Increased color Doppler given high internal vascularity
- CT
- Isodense ovoid mass with feeding vessels in the plain CT (Radiol Oncol 2021;56:46)
- Conspicuous enhancement in the contrast enhanced CT
- MRI
- Superior to ultrasound and CT to determine tumor staging and to distinguish paragangliomas from other masses including leiomyomas, given its improved resolution of soft tissues (Abdom Radiol (NY) 2022;47:4032, Abdom Radiol (NY) 2023;48:1051)
- Typically T1 and T2 hyperintensity with salt and pepper appearance and feeding vessels
- Characteristic restricted diffusion and avid contrast enhancement
- PET
- Pseudohypoxic pathway abnormalities: 68Ga-DOTATATE PET-CT (Endocrinol Metab (Seoul) 2017;32:152)
- Kinase pathway: 18F-DOPA PET-CT (J Clin Endocrinol Metab 2021;106:e1301, J Clin Endocrinol Metab 2013;98:E162)
Radiology images
Prognostic factors
- All paragangliomas carry a metastatic potential (Urol Oncol 2015;33:167.e13)
- Multiple grading systems have been proposed to predict metastasis
- Grading system for adrenal pheochromocytoma and paraganglioma (GAPP), with unfavorable factors being large and irregular cell nest, pseudorosette (even focal), comedo type necrosis, moderate to high cellularity, Ki67 labeling index > 1 - 3%, vascular or capsular invasion and noradrenergic type (Endocr Relat Cancer 2014;21:405)
- Modified GAPP: based on the same prognostic factors as GAPP with the addition of SDHB loss on IHC (PLoS One 2017;12:e0187398)
- Age, size, extra-adrenal location, secretory type score (ASES), with unfavorable factors being age ≤ 35 years, tumor size ≥ 6.0 cm and tumor producing only norepinephrine (Surgery 2018;164:511)
- COPPS (composite pheochromocytoma / paraganglioma prognostic score), with unfavorable factors being focal or confluent necrosis, PS100 loss, vascular invasion, SDHB loss, tumor size > 7 cm, capsular invasion, increased mitotic figures and MCM6 (minichromosome maintenance) > 30% (Virchows Arch 2019;474:721)
- Unfavorable factors for disease progression in metastatic bladder paragangliomas: male, advanced age, synchronous metastases, large tumor size, high dopamine level and nonresection of the primary tumor (Urol Oncol 2015;33:167.e13)
- Molecular features associated with poorer outcome: markers associated with poor aggressive disease free survival included MAML3 fusion gene, SDHB germline mutation, somatic mutation in SETD2 or ATRX, high somatic mutation total, Wnt altered and pseudohypoxia expression subtypes and the hypermethylated subtype (Cancer Cell 2017;31:181)
- 40 - 50% risk of developing metastatic disease with SDHB mutations (Endocrinol Metab (Seoul) 2017;32:152)
- Molecular features associated with better outcome: kinase signaling expression subtype and the low methylated subtype
Case reports
- 14 year old girl with minimally invasive robot assisted partial cystectomy with bilateral vesicoureteric junction resection and reimplantation for paraganglioma of the bladder trigone (Cent European J Urol 2017;70:378)
- 16 year old girl with hematuria diagnosed with bladder paraganglioma (Pediatr Dev Pathol 2011;14:327)
- 39 year old woman with bladder paraganglioma and gastrointestinal stromal tumor diagnosed with Carney-Stratakis syndrome (Front Oncol 2022:12:1030092)
- 48 year old woman with gross hematuria diagnosed with ureteral paraganglioma (BMC Urol 2023;23:21)
- 53 year old man with aggressive bladder paraganglioma with local recurrence and pelvic metastasis (Pathol Oncol Res 2020;26:2827)
- 58 year old man presented with hematuria and diagnosed with metastatic paraganglioma of the urinary bladder (Pathol Res Pract 2015;211:183)
- 64 year old man with bladder paraganglioma invading the rectum (World J Surg Oncol 2022;20:185)
- 64 year old man with urine cytologic findings of primary bladder paraganglioma (Diagn Cytopathol 2017;45:350)
- 73 year old man with composite paraganglioma ganglioneuroma of the urinary bladder (Pathol Int 2005;55:596)
Treatment
- Medical preparation for treatment: alpha blockade with or without the addition of other antihypertensive drugs as needed
- Primary treatment
- Resection with preference for minimally invasive procedures
- For locally unresectable or metastatic cases, watchful waiting is recommended if the patient is asymptomatic or if the tumor is small and slow growing
- For secreting tumors that are unresectable / with distant metastases, the recommendation is to continue alpha blockade with initiation of one of the following modalities as clinically warranted: clinical trial, radiation therapy, cytoreductive resection, MIBG therapy, sunitinib, systemic chemotherapy, peptide receptor radionuclide therapy and somatostatin analogues
- Reference: NCCN: NCCN Guidelines - Neuroendocrine and Adrenal Tumors [Accessed 28 November 2023]
Clinical images
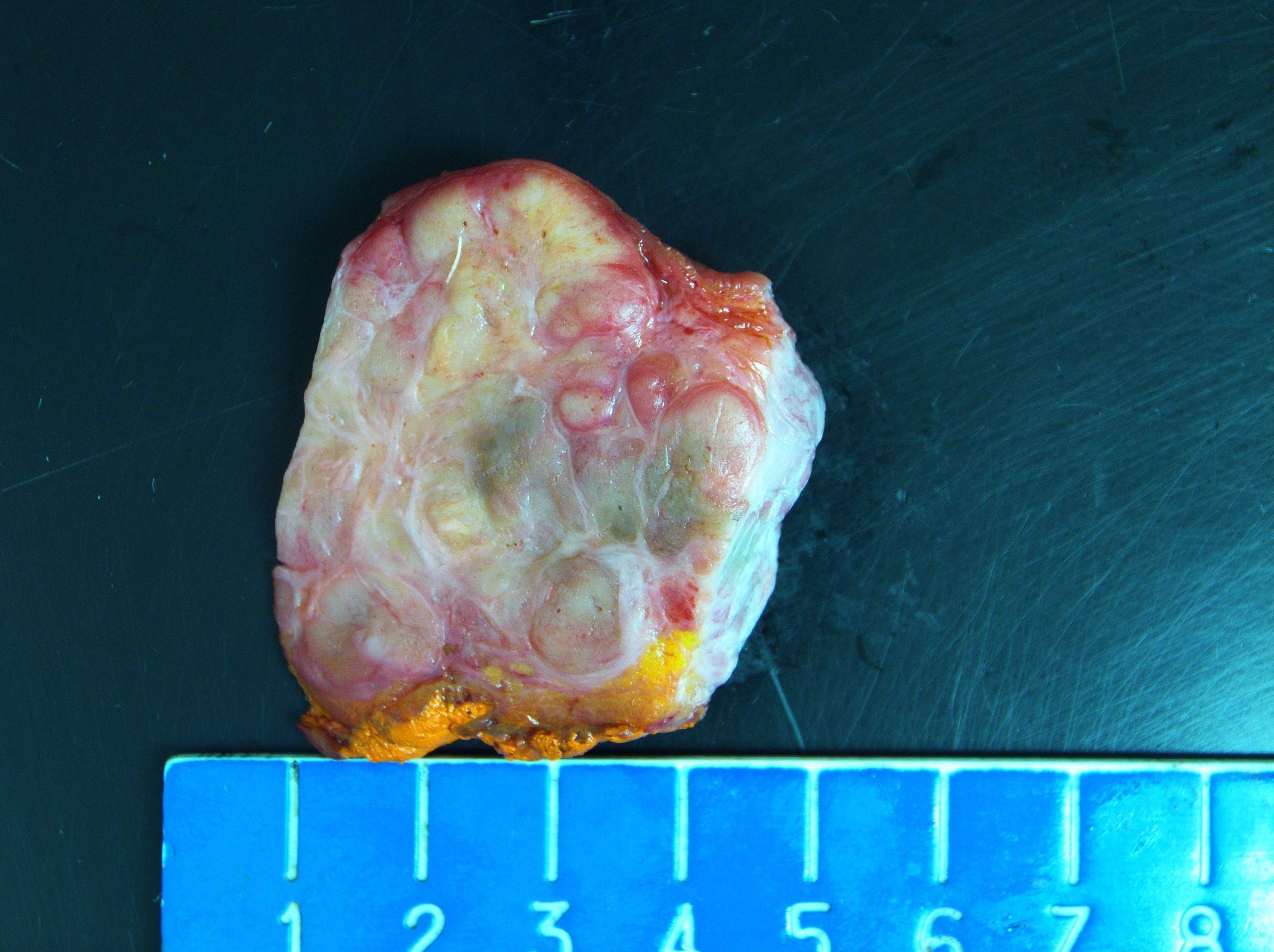
Gross description
- Genitourinary paragangliomas are typically tan-pink to violaceous, encapsulated and firm (Abdom Radiol (NY) 2022;47:1414, Abdom Radiol (NY) 2022;47:4032, BMC Urol 2023;23:21)
- Bladder paragangliomas are often submucosal or intramural and less frequently subserosal, with size at diagnosis up to 9.1 cm (mean: 3.9 cm)
- Small bladder paragangliomas: typically well circumscribed, round ovoid and homogeneous
- Larger bladder paragangliomas: usually more complex appearance with lobulation, peri and intratumoral vascularization and cystic / necrotic / hemorrhagic areas
- Bladder paragangliomas may have calcification (up to 20% of cases) or local invasion of the pelvic side wall, uterus, vagina and ovaries
Gross images
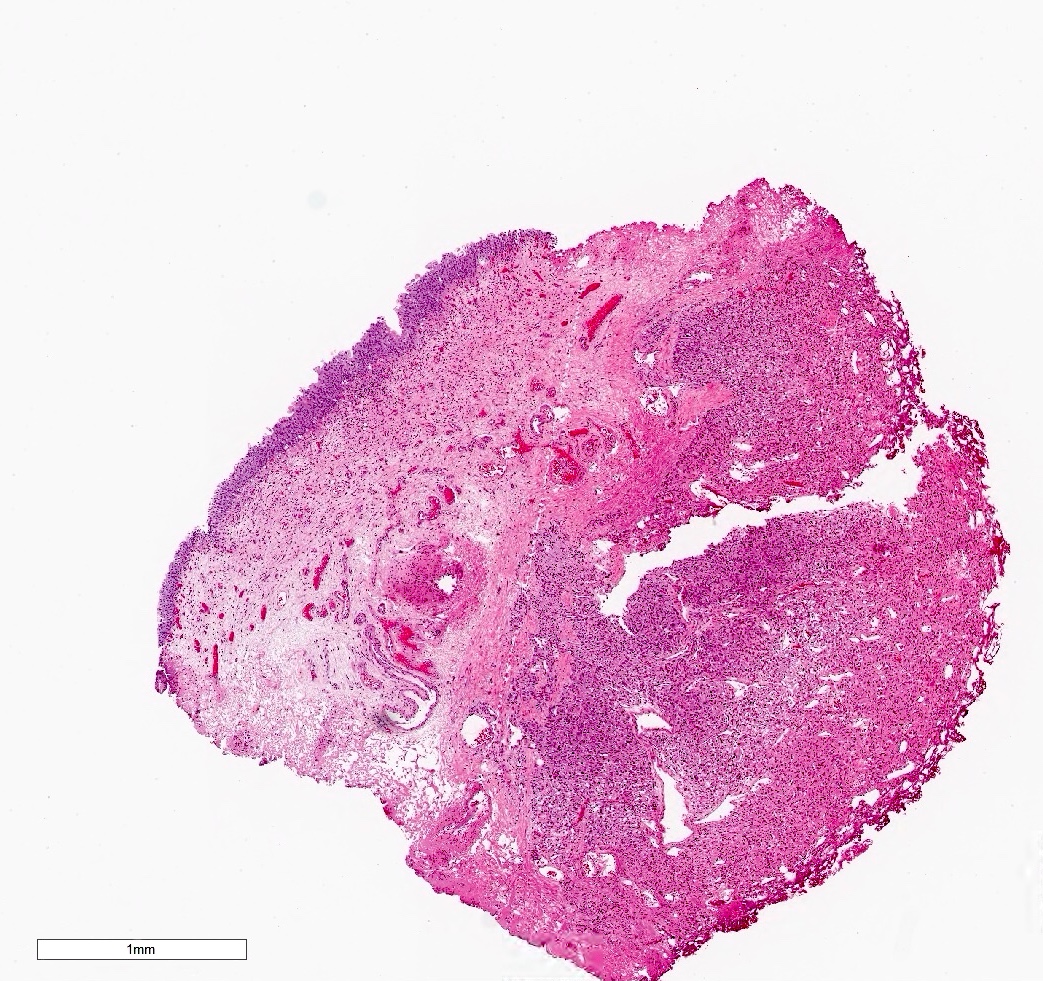
Frozen section description
- Highly vascularized tissues showing on histologic examination nests / sheets of polygonal neoplastic cells with eosinophilic or amphophilic cytoplasm, surrounded by stromal cells and blood vessels (Int J Surg Pathol 2018;26:213)
- Focal signet ring features or dilated blood vessels may be seen
Frozen section images
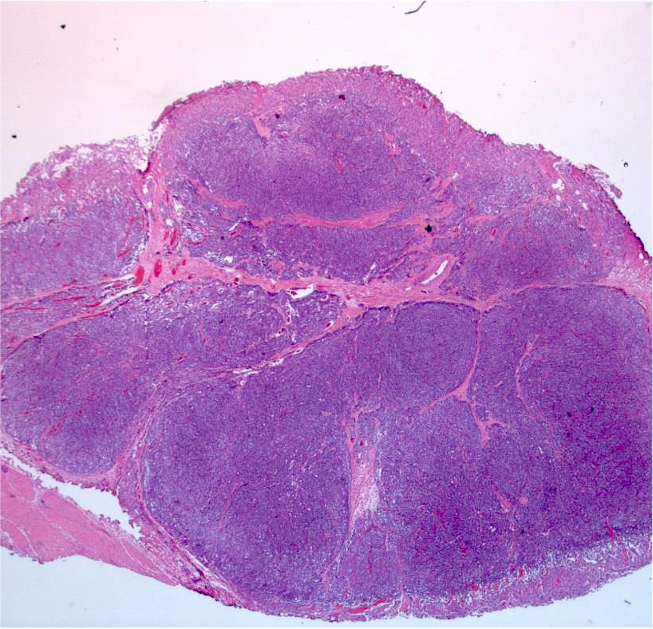
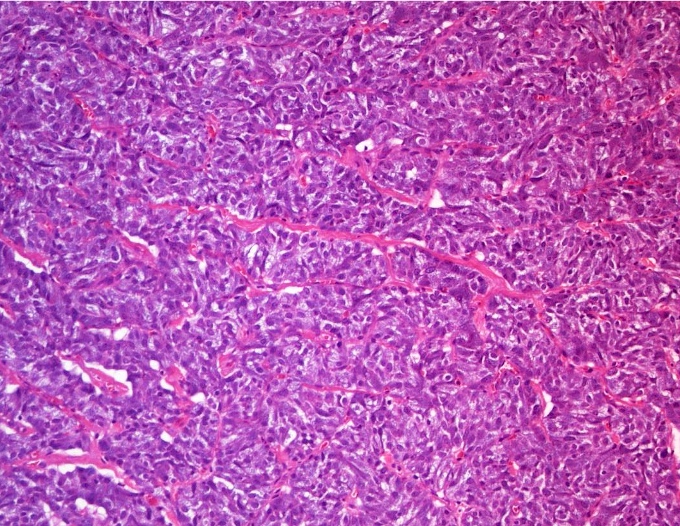
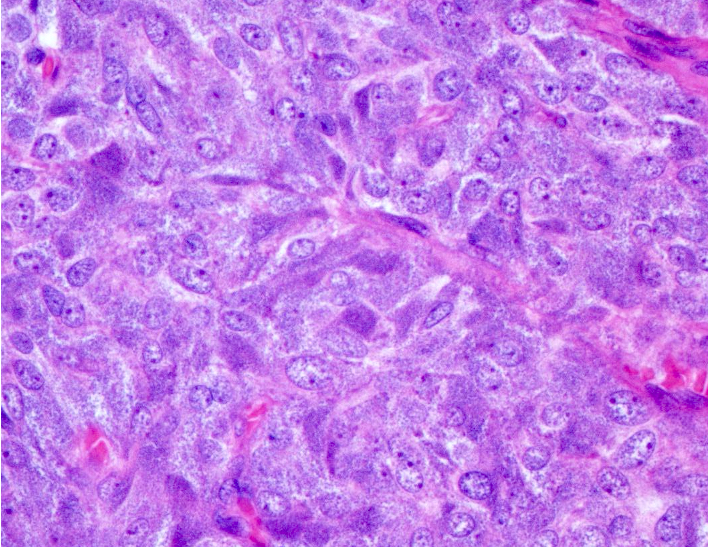
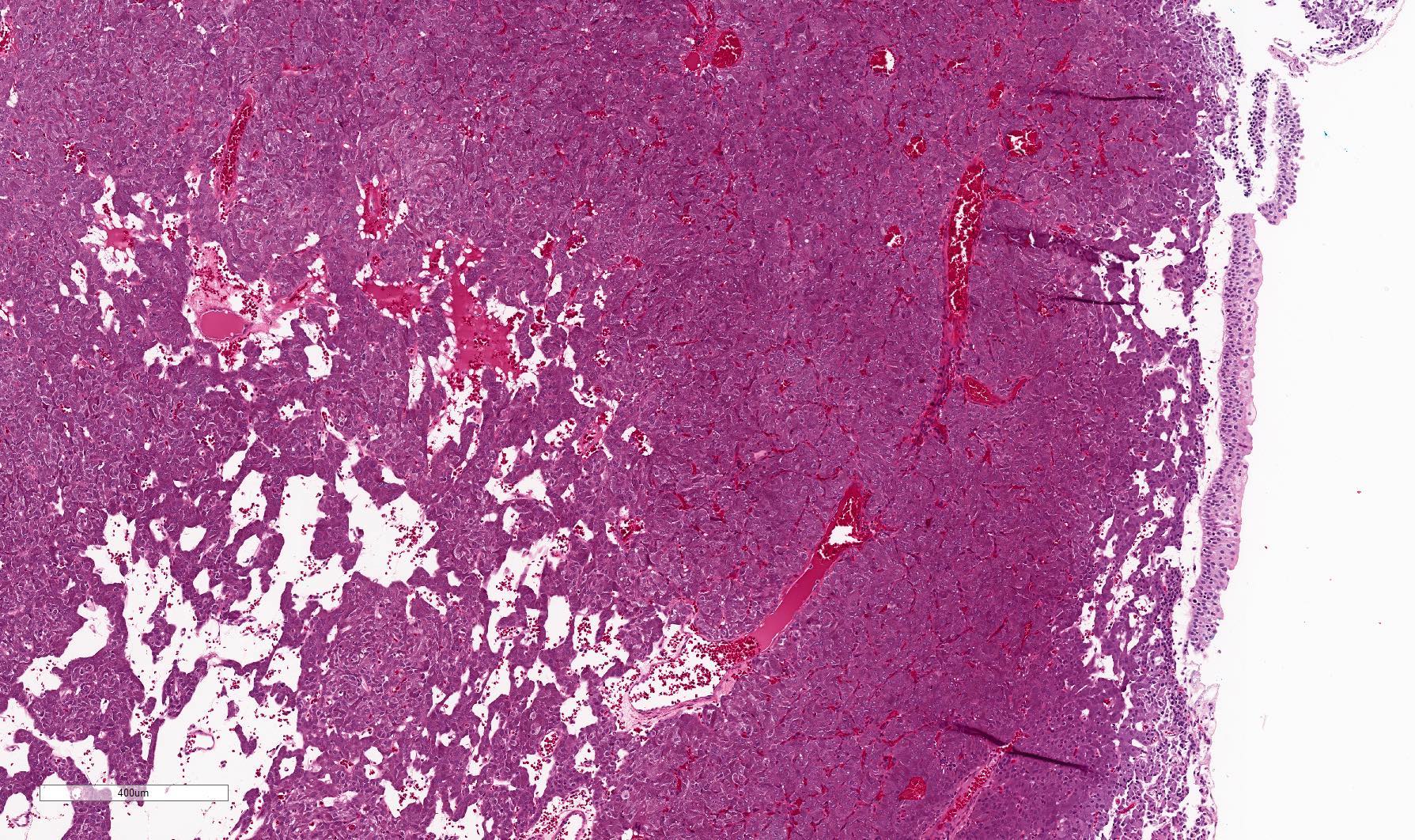
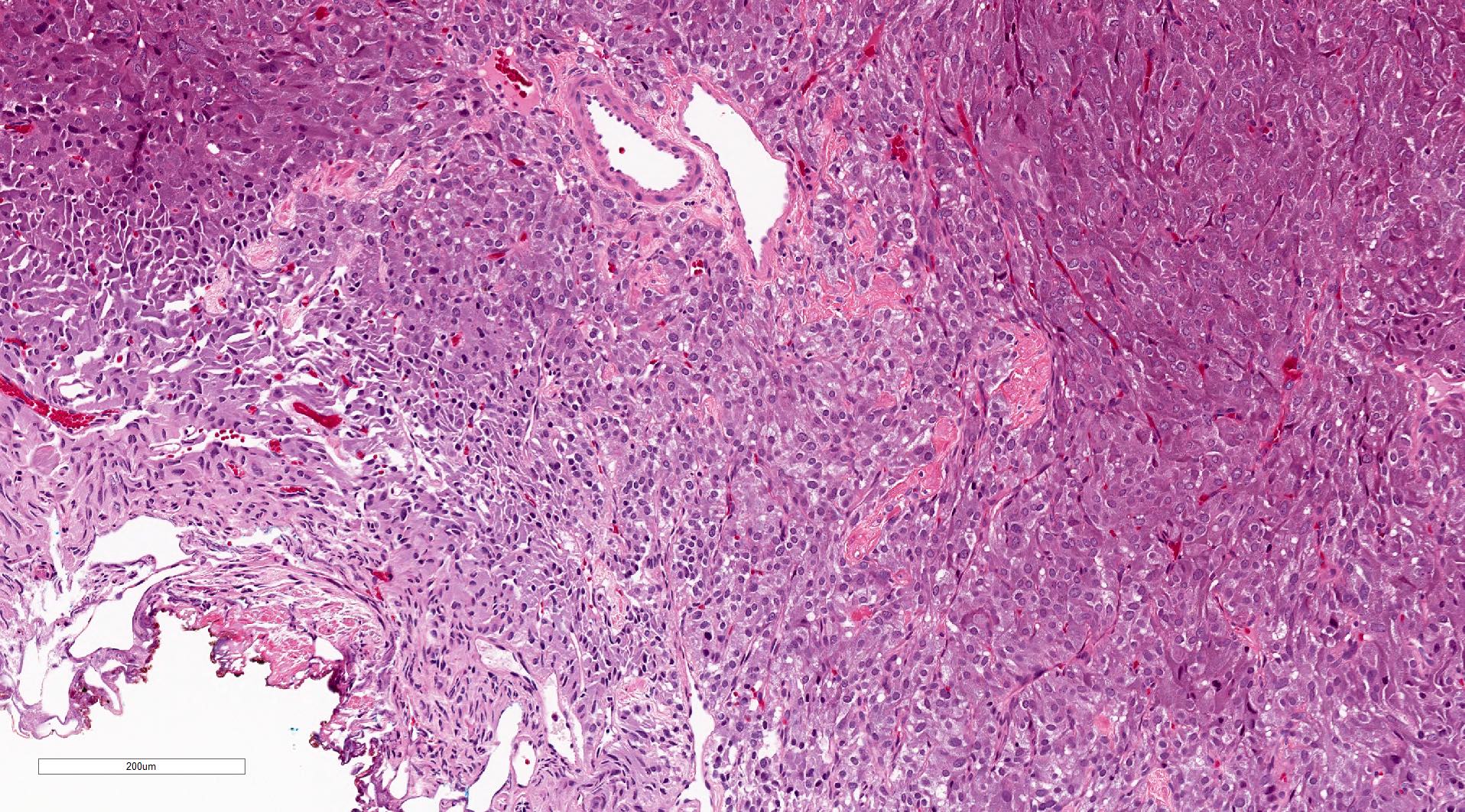
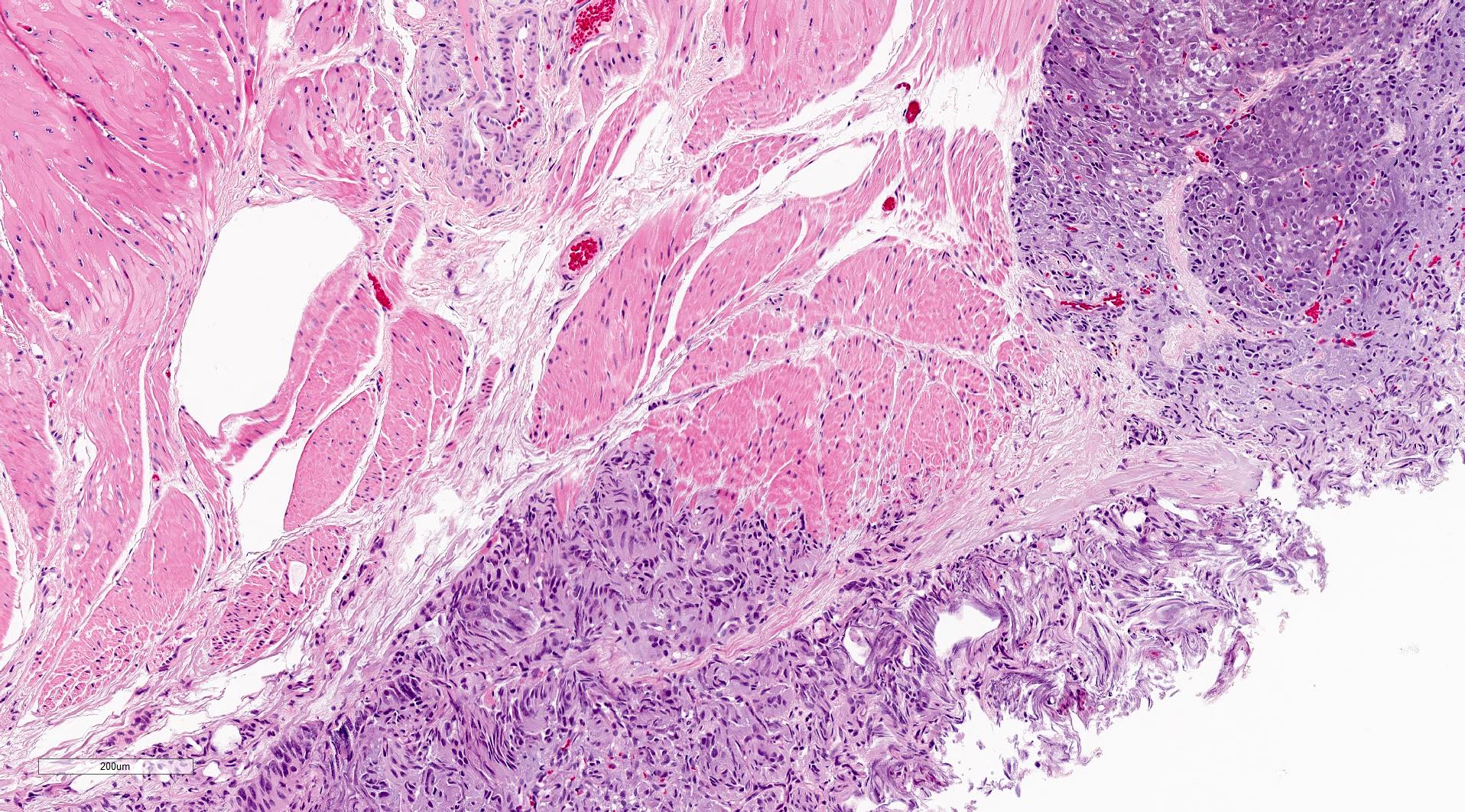
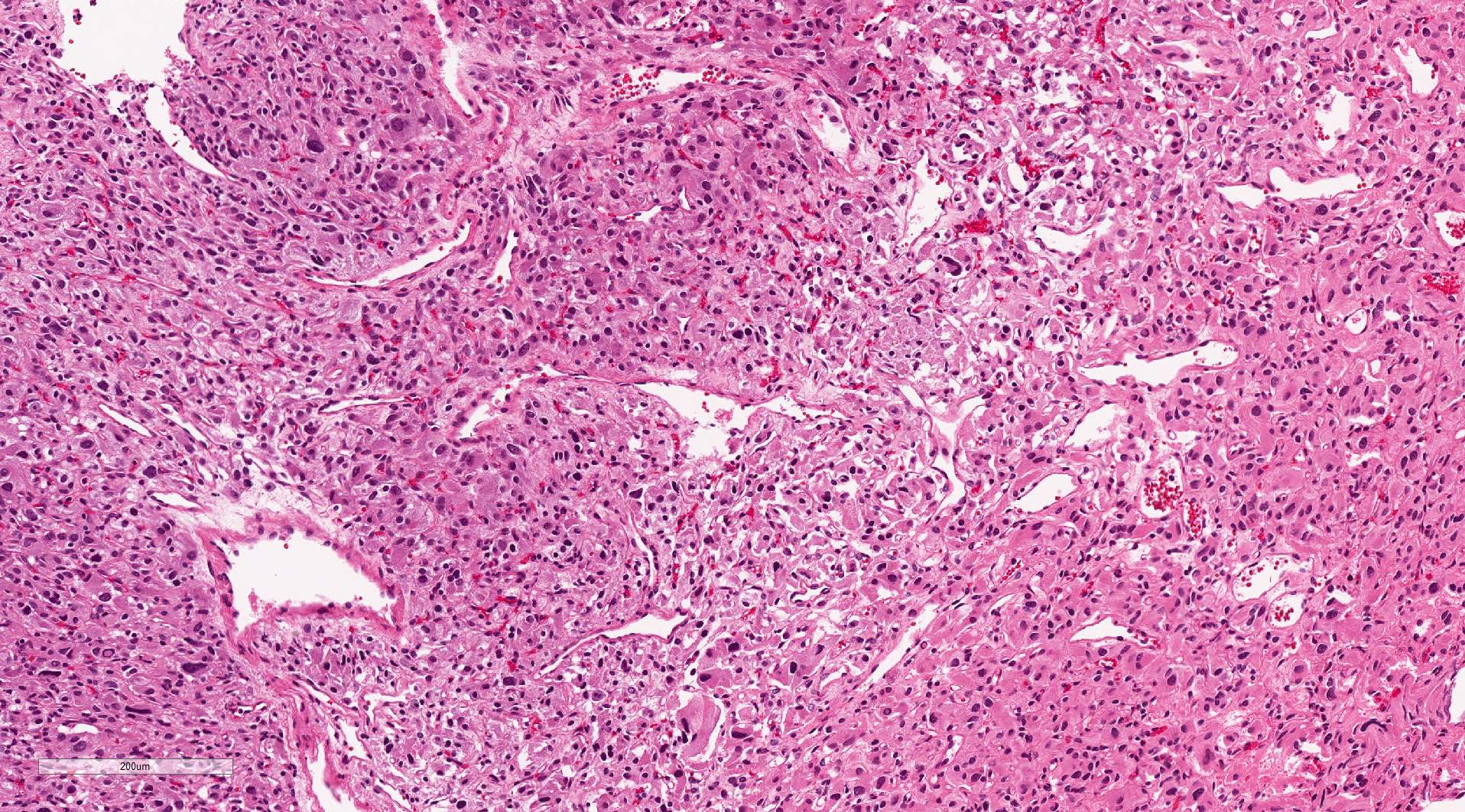
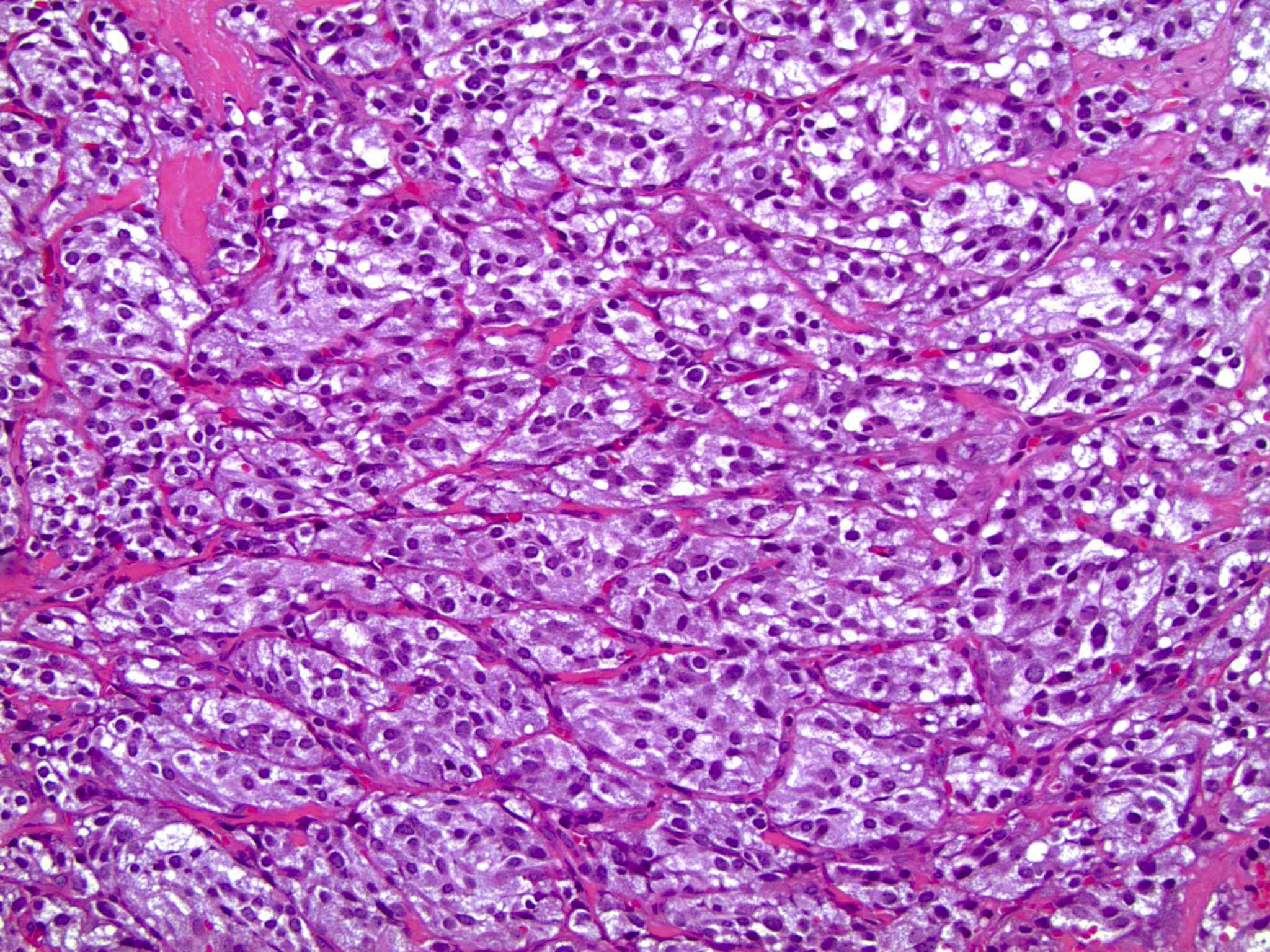
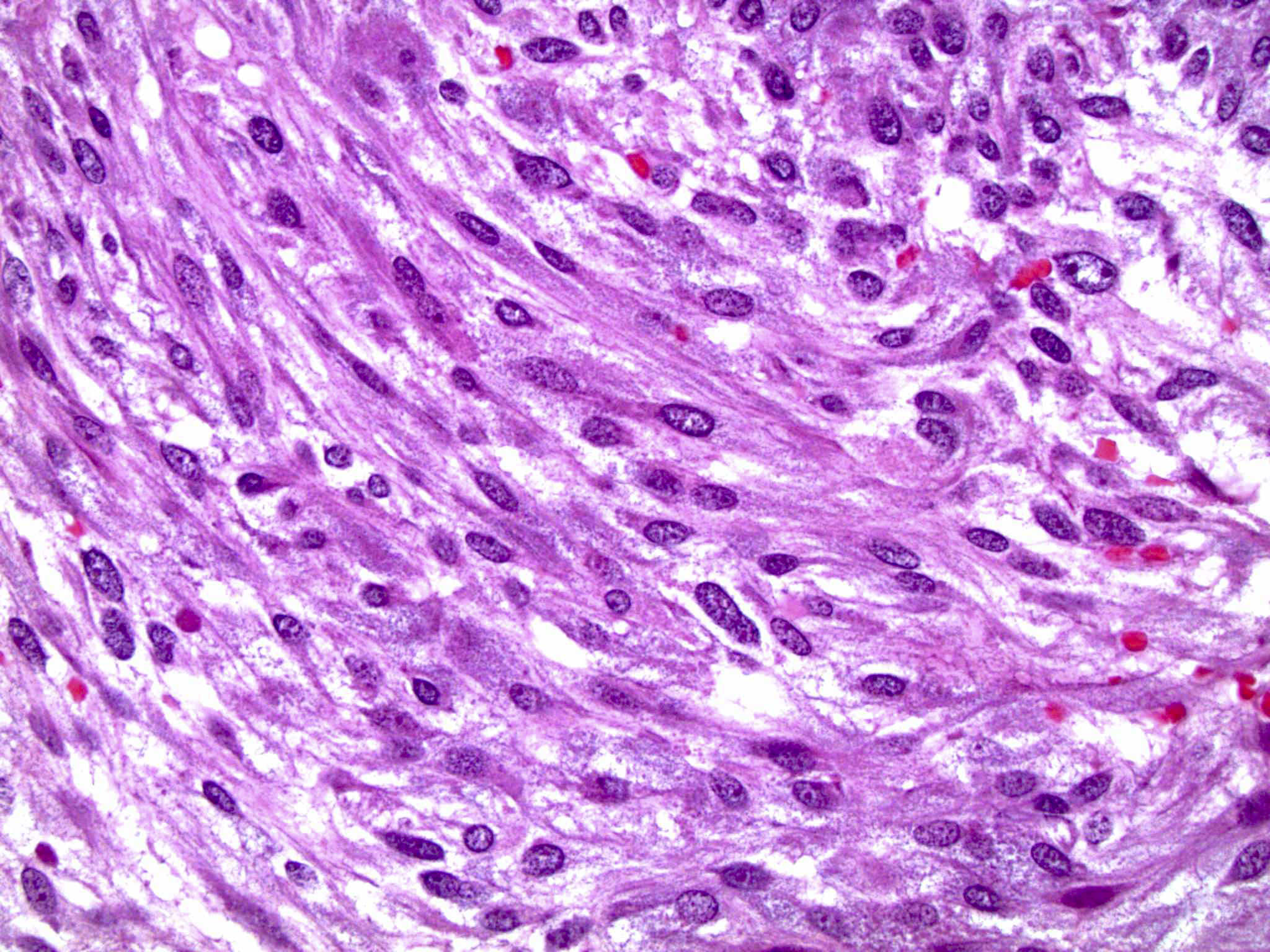
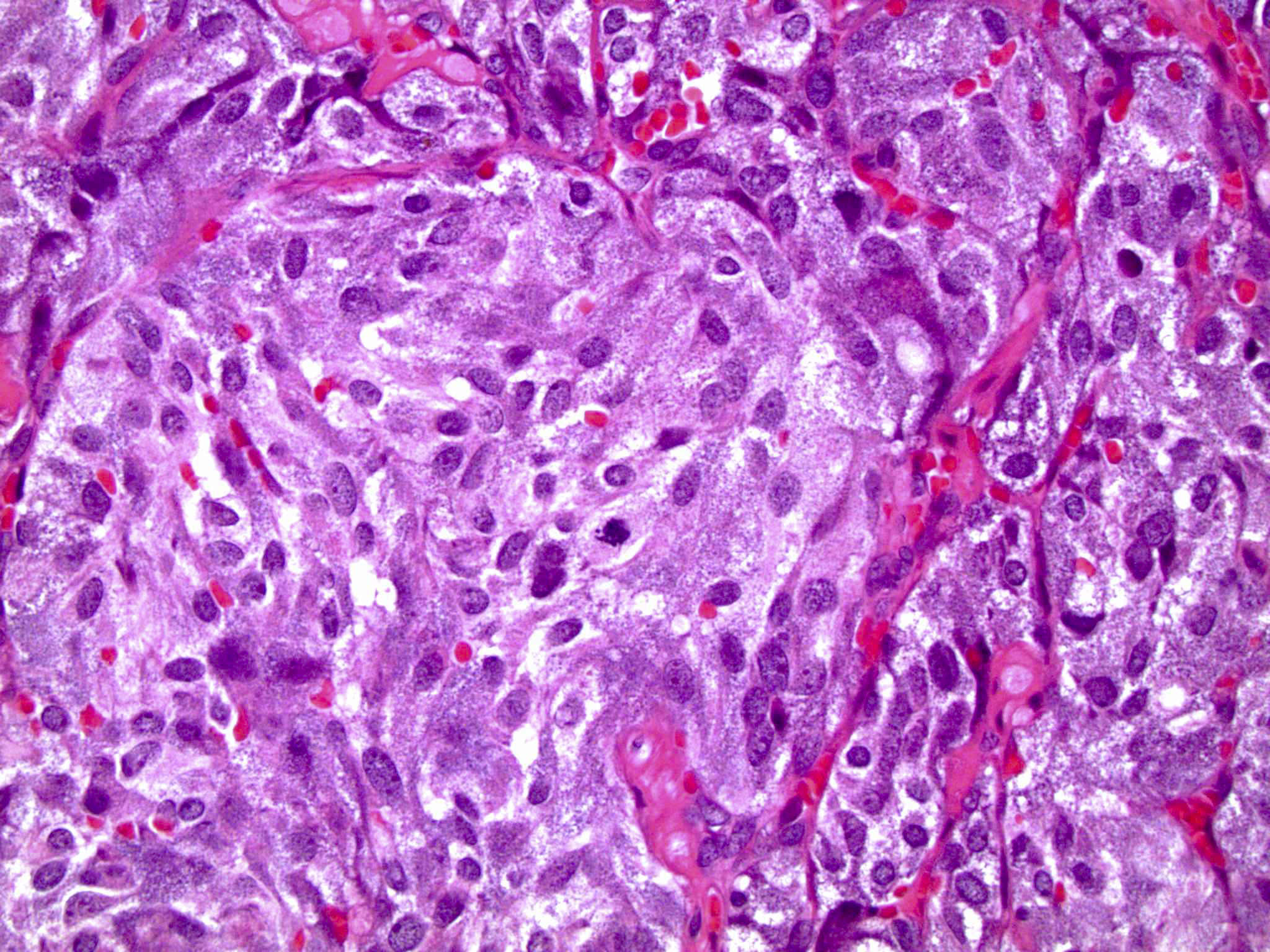
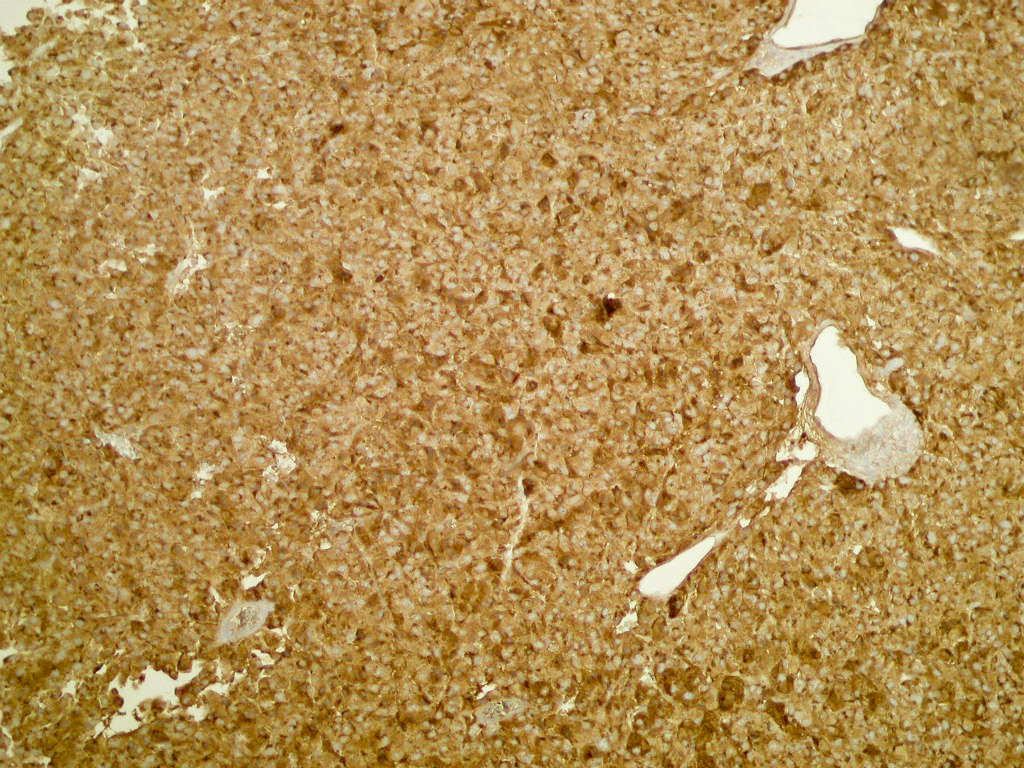
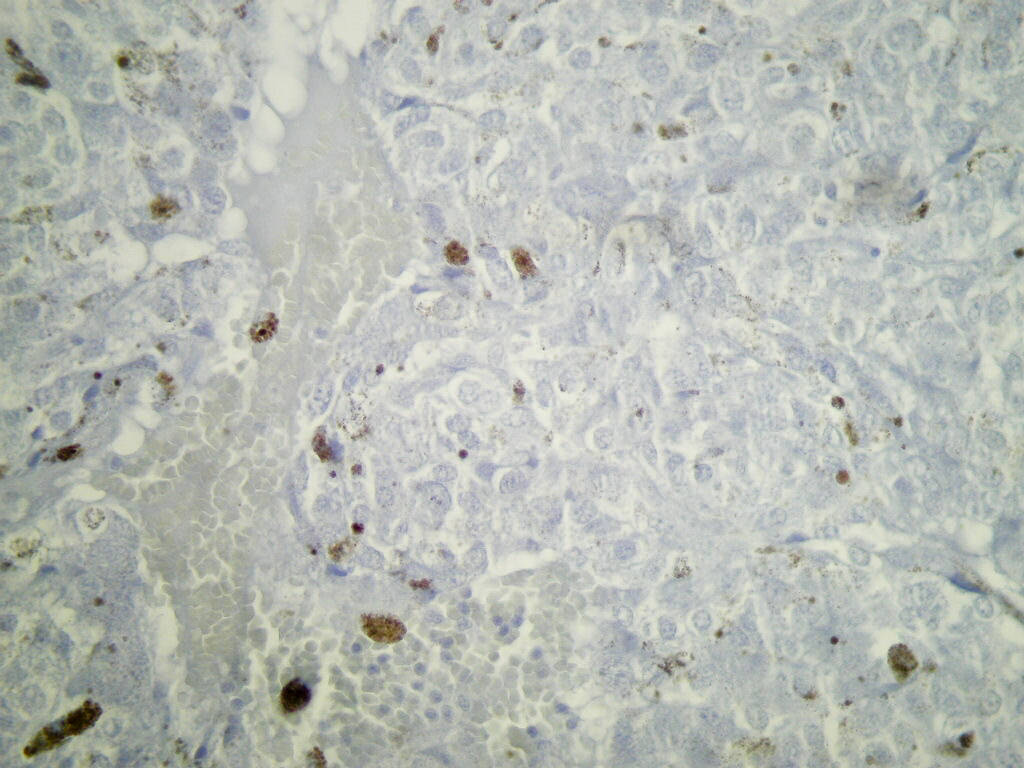
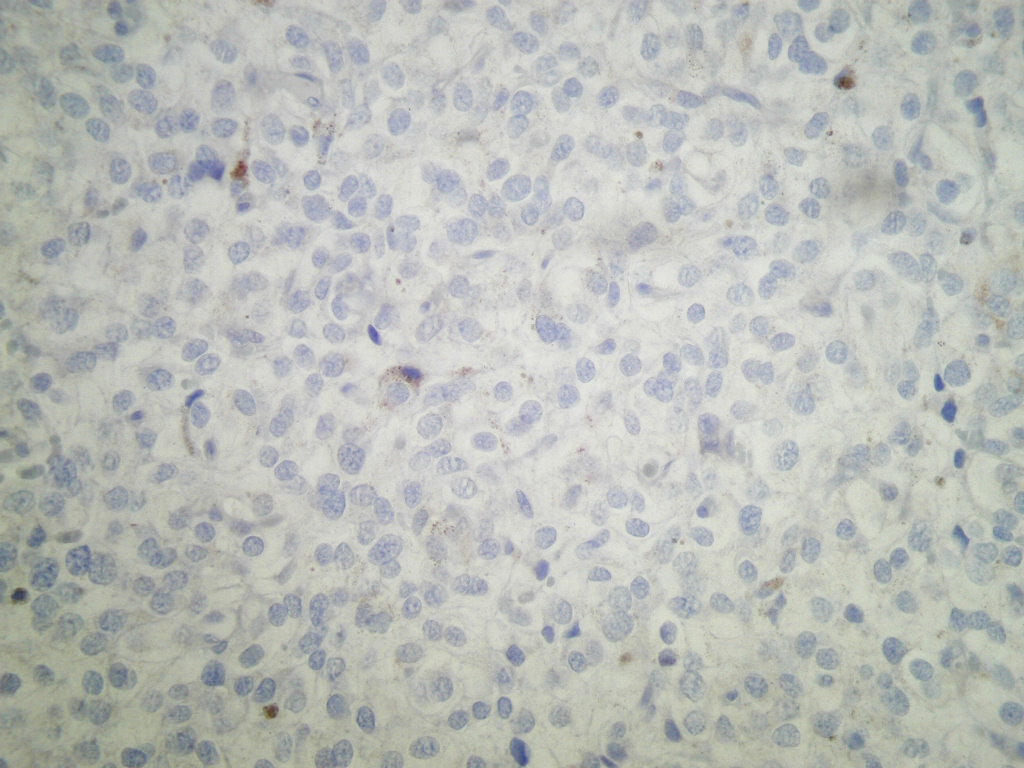
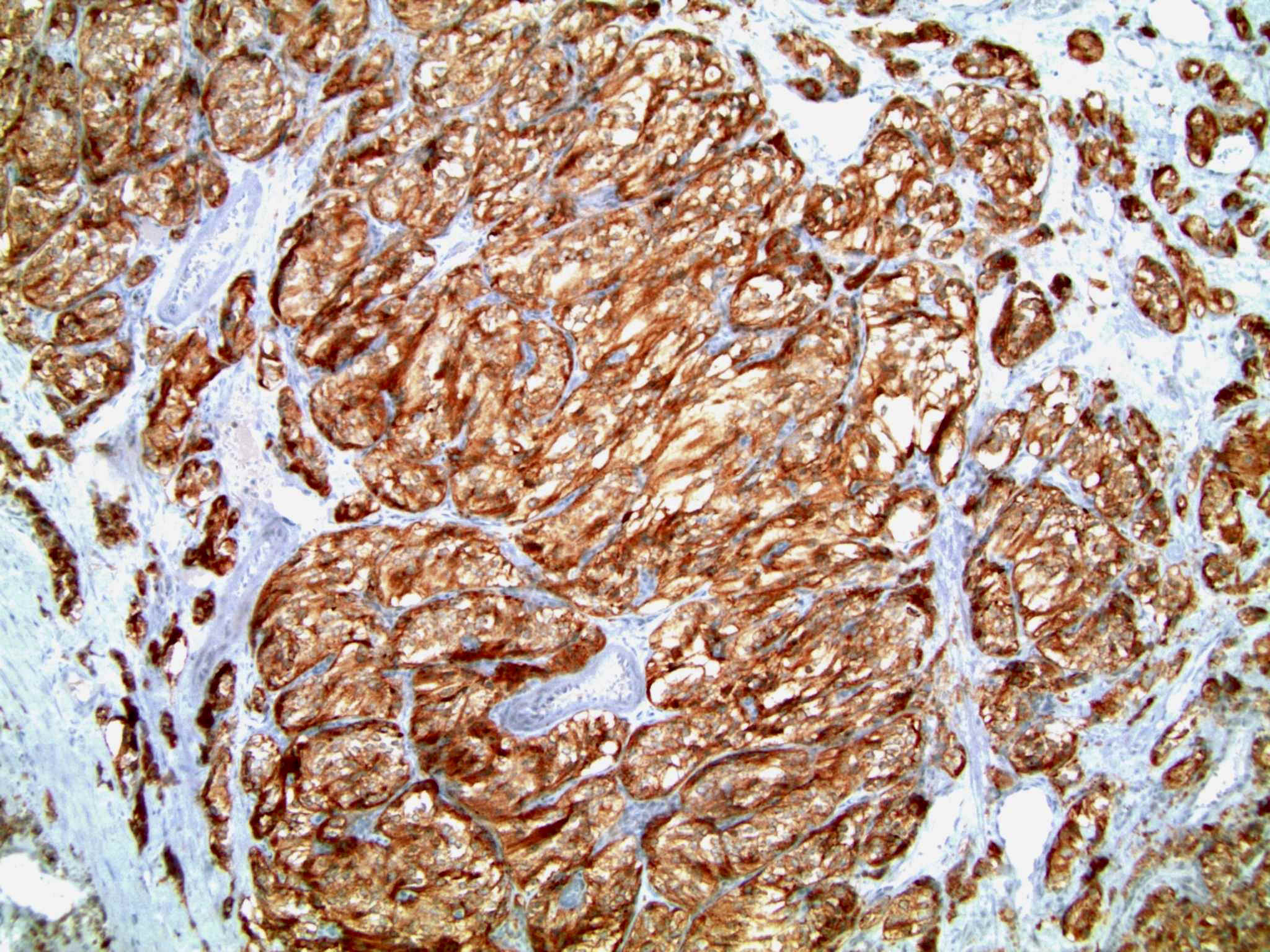
Microscopic (histologic) description
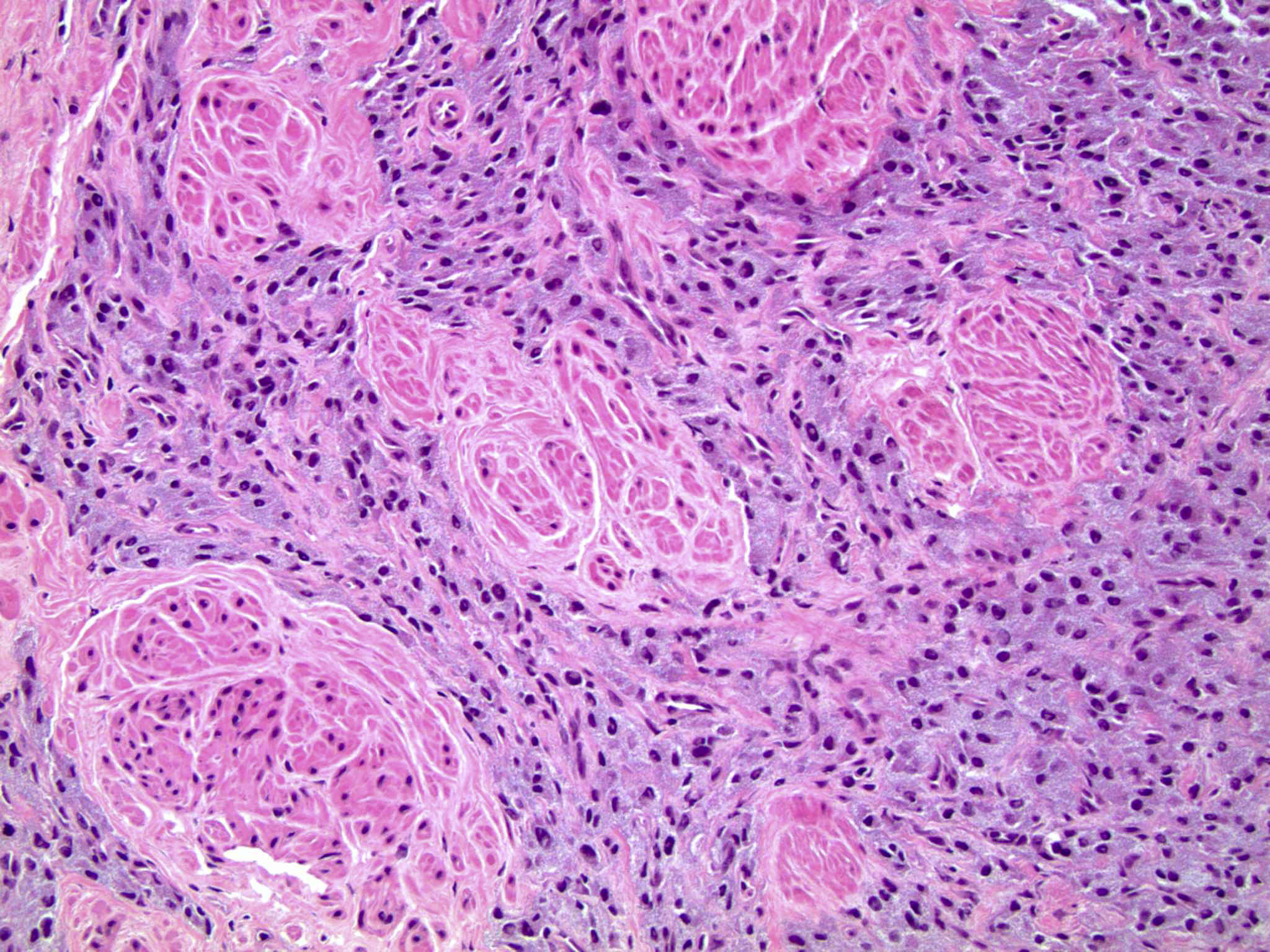
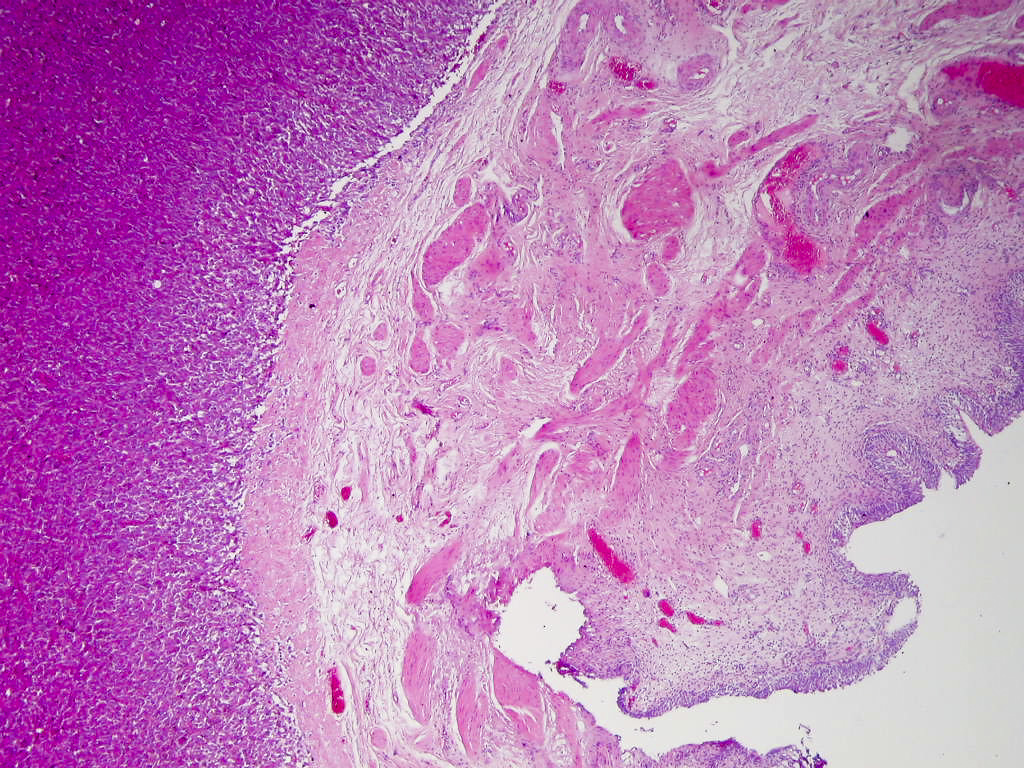
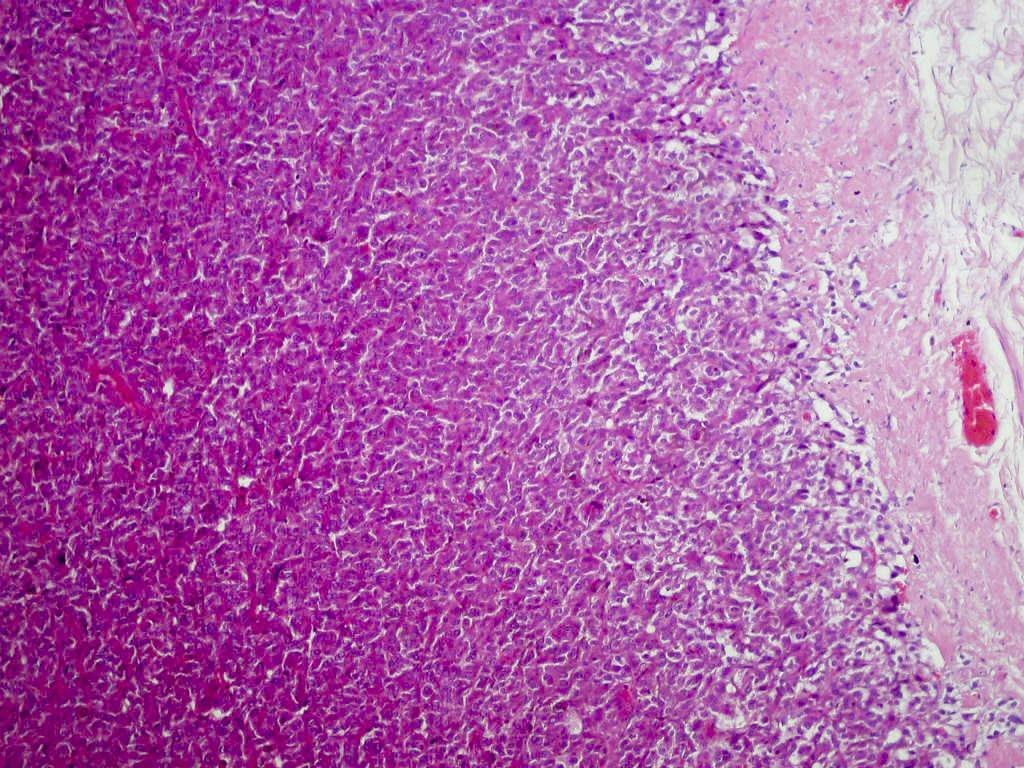
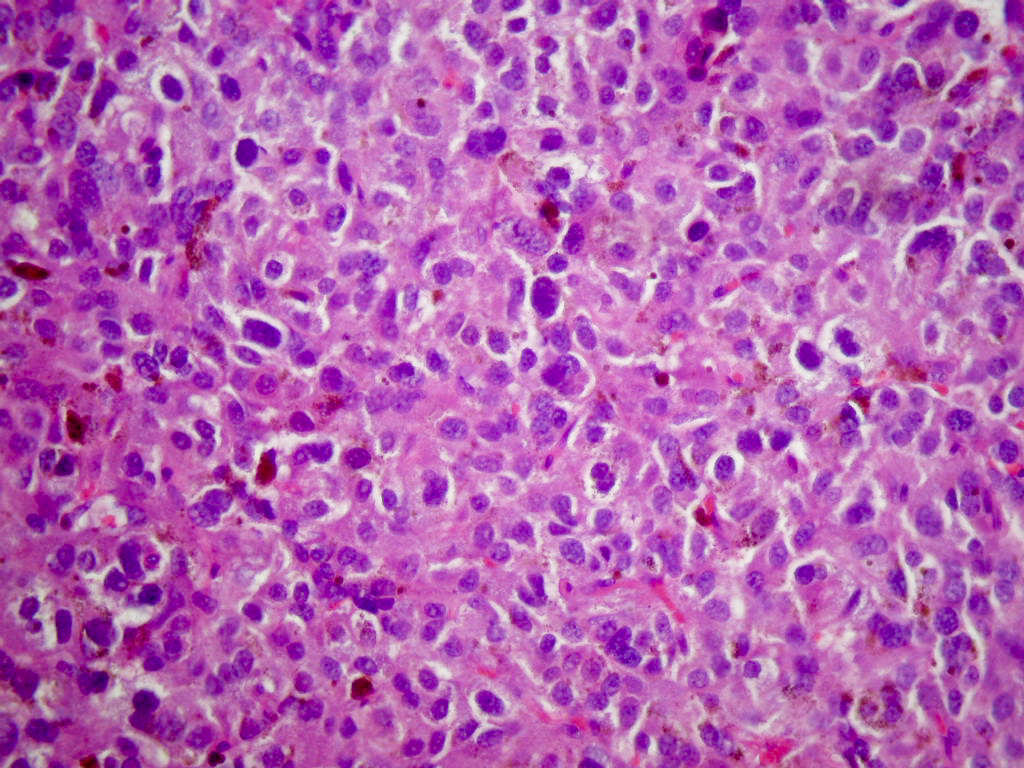
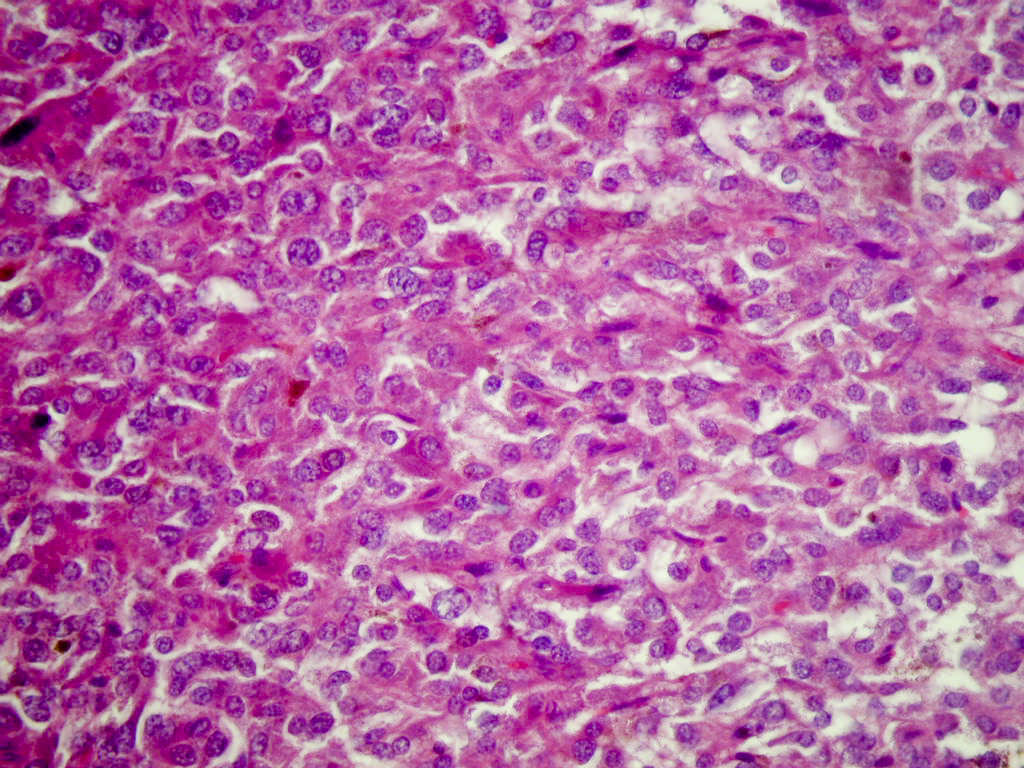
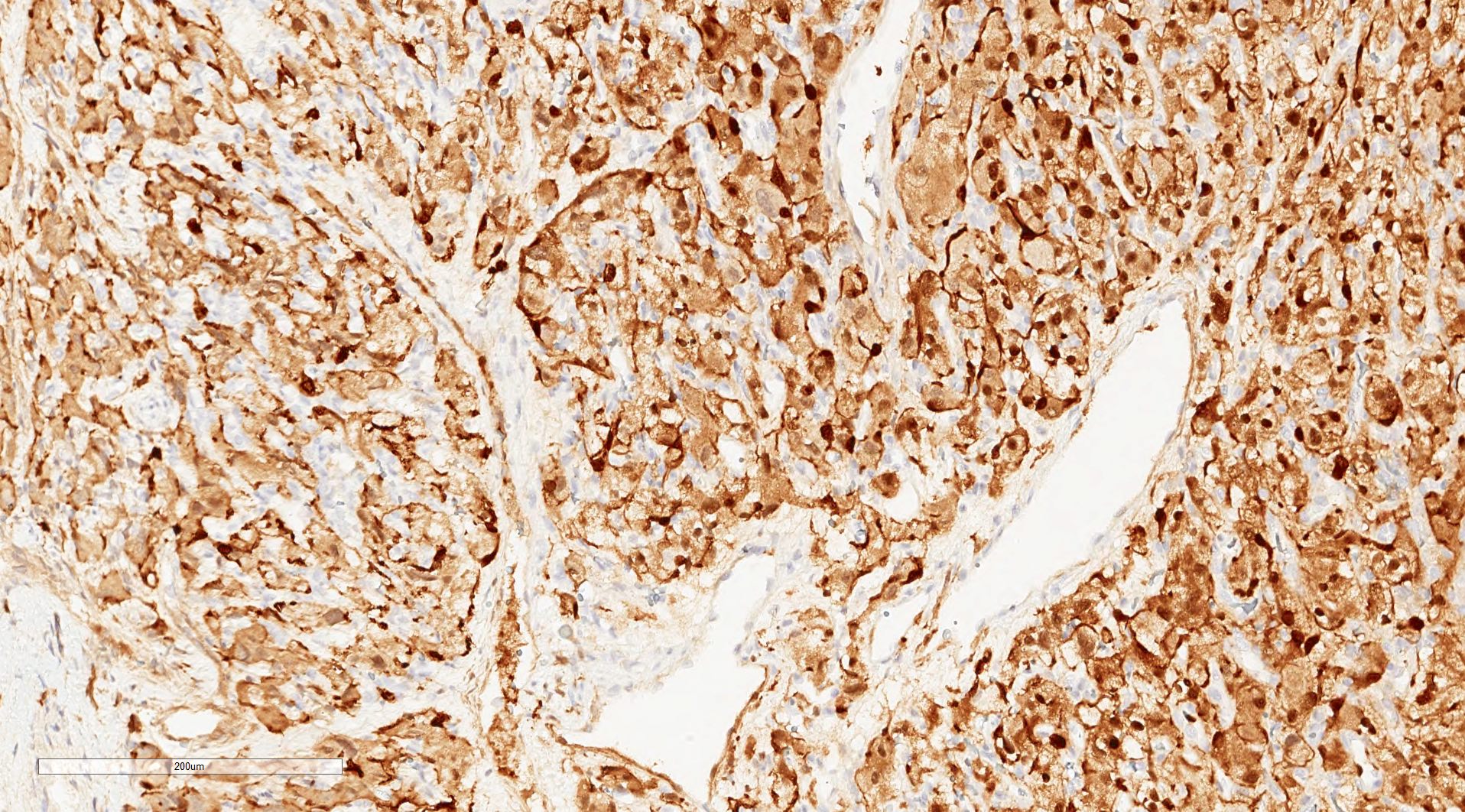
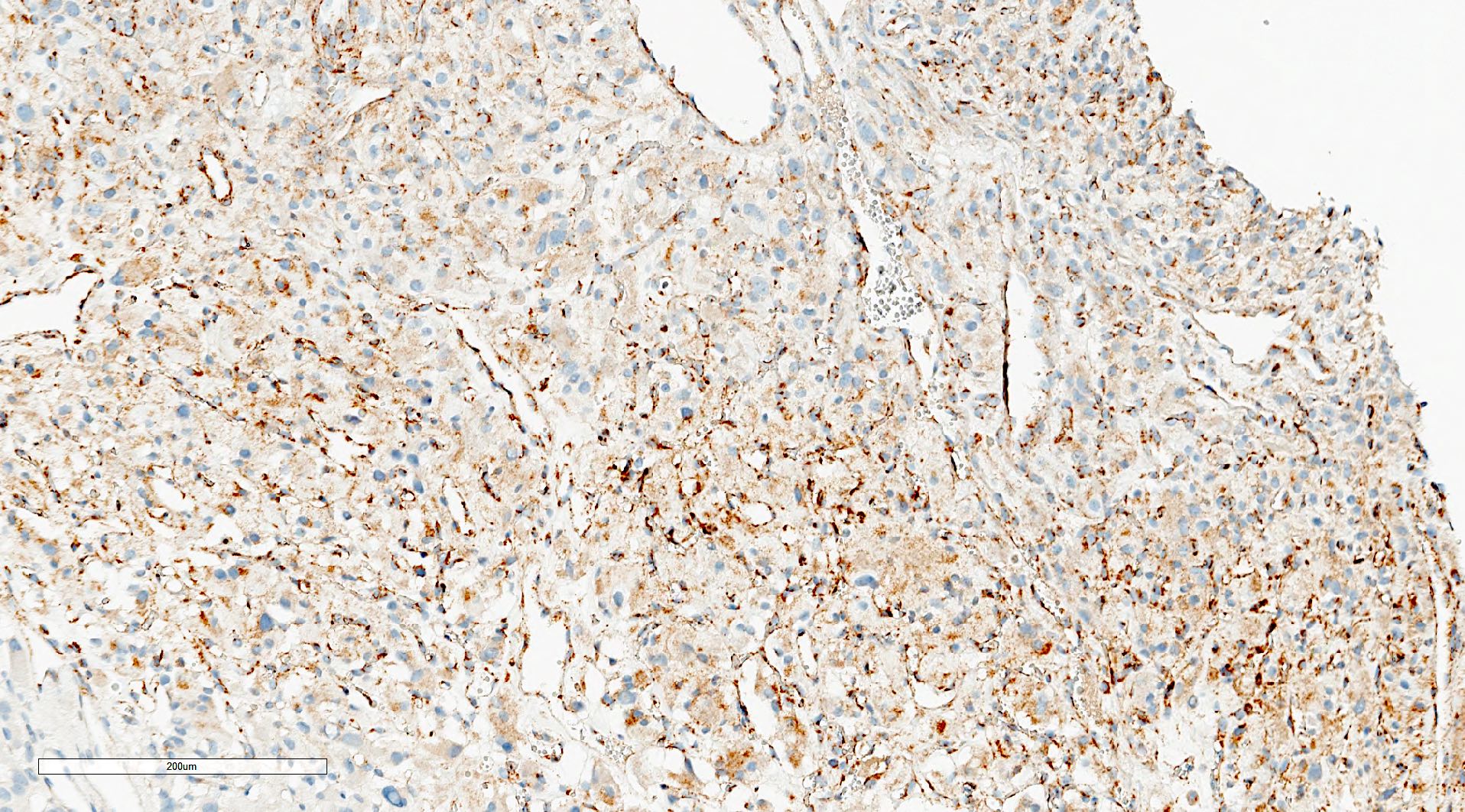
- Typical morphology: epithelioid cells with abundant, eosinophilic / amphophilic, granular cytoplasm and round / ovoid, vesicular / salt and pepper nuclei, arranged in a nested / zellballen pattern and separated by fibrovascular septae with sustentacular cells (Am J Surg Pathol 2004;28:94, World J Clin Cases 2014;2:591, Endocr Pathol 2022;33:90)
- May have focal pleomorphism, nuclear hyperchromasia, low mitotic activity or clear cytoplasm
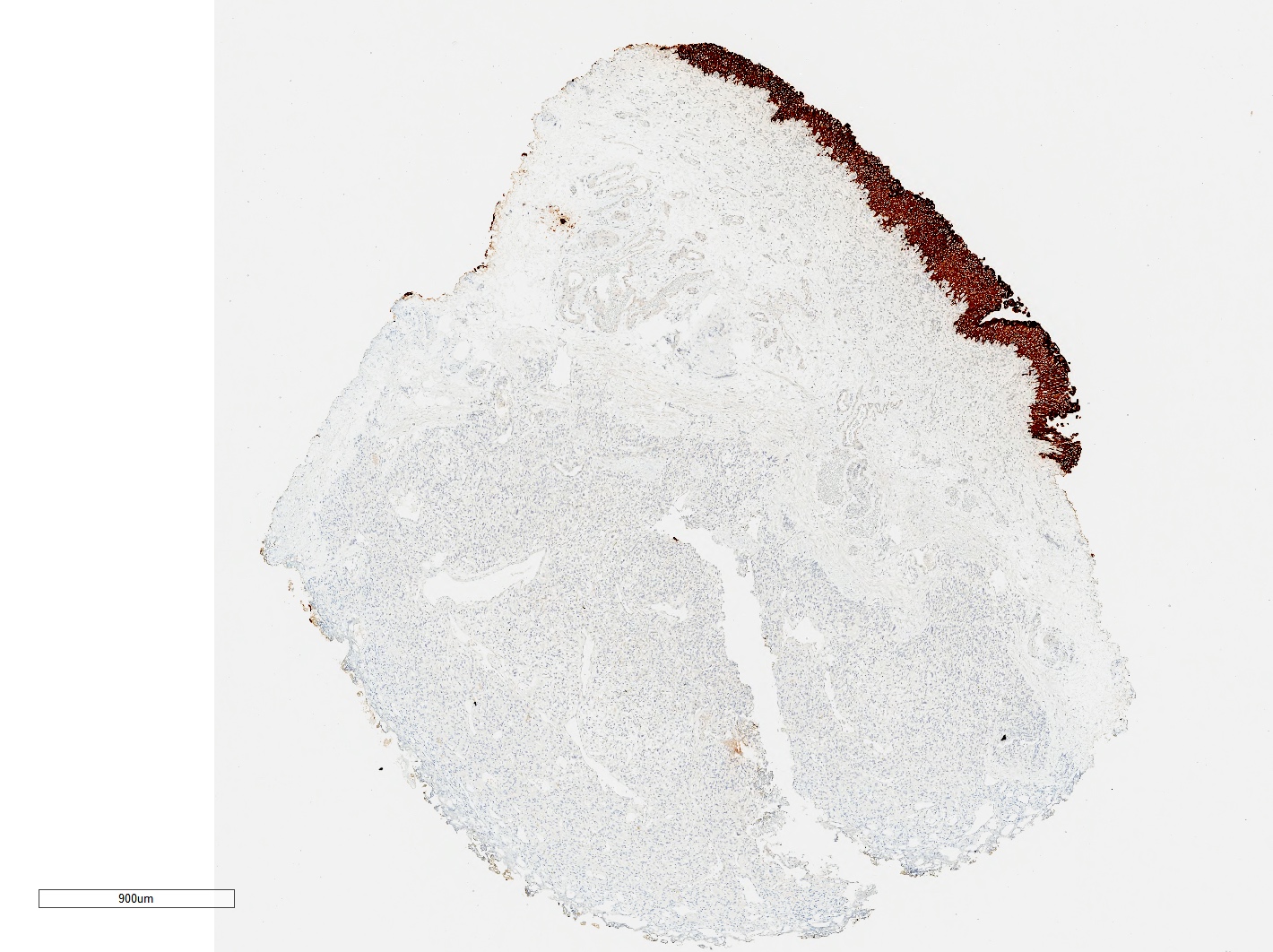
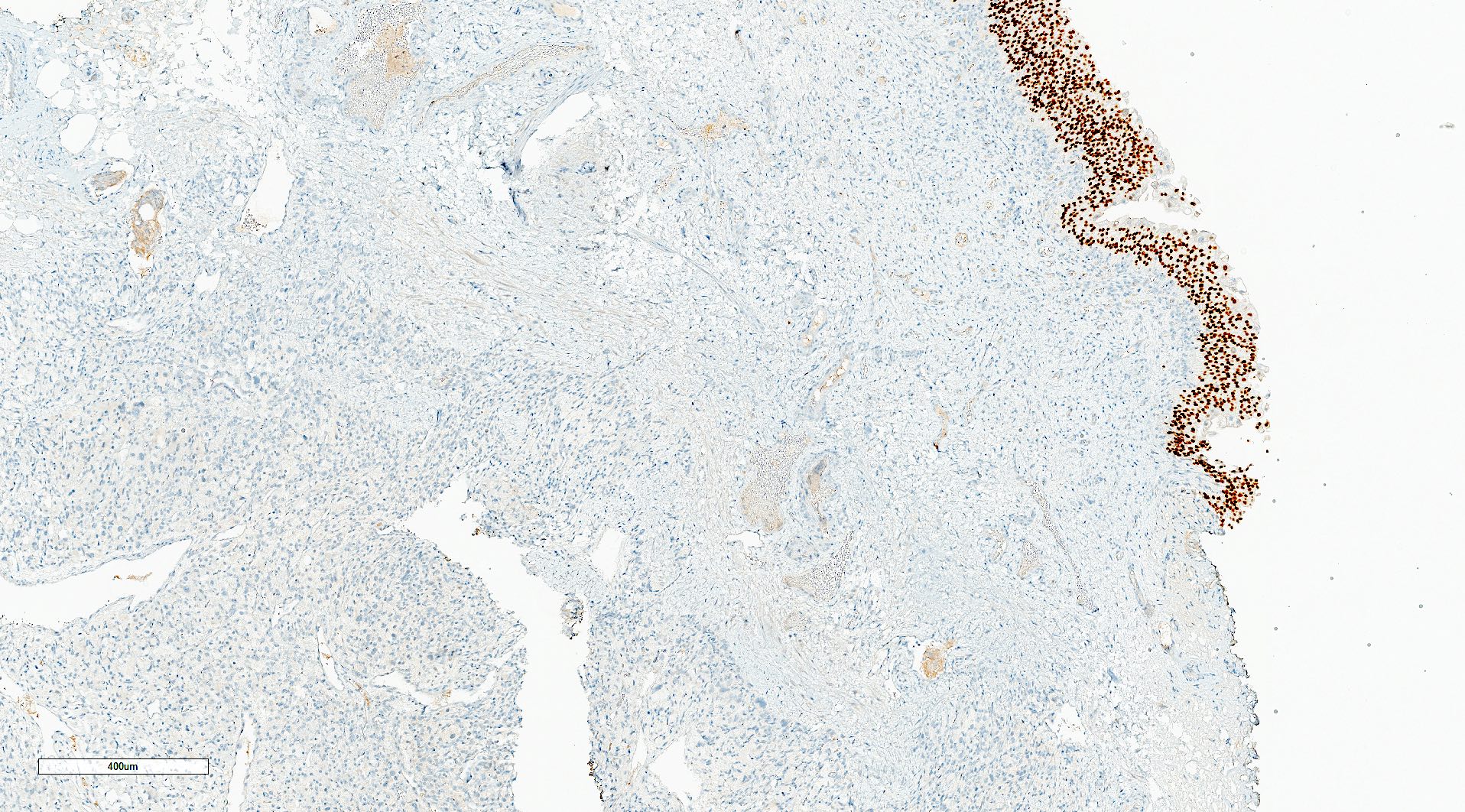
Microscopic (histologic) images
Contributed by Theodorus H. van der Kwast, M.D., Ph.D., Michelle R. Downes, M.D., Debra L. Zynger, M.D. and David Cohen, M.B.B.Ch., M.D.
Cytology description
- Tumor cells arranged in clusters or singly (Diagn Cytopathol 2017;45:350)
- Epithelioid cells with abundant, finely granular, pale cytoplasm
- Ovoid nuclei with smooth contour, fine chromatin and inconspicuous nucleoli
- Occasional spindle sustentacular cells admixed within clusters of tumor cells
- Naked nuclei present
Positive stains
- INSM1 (diffuse), chromogranin A (variable, often diffuse), synaptophysin (variable, usually diffuse) (Endocr Pathol 2022;33:90)
- GATA3
- SSTR2 (Hum Pathol 2019:86:66)
- TH, DBH in functional paragangliomas
- SDHB loss (absence of granular cytoplasmic labeling) if SDHB mutation
- SDHA loss (absence of strong diffuse granular cytoplasmic labeling) if SDHA mutation
- Sustentacular cells: S100, SOX10
Negative stains
Molecular / cytogenetics description
- See Pathophysiology
Sample pathology report
- Bladder, transurethral resection:
- Paraganglioma, SDHB staining intact (see comment)
- Involvement of muscularis propria
- Unremarkable surface urothelium
- Comment: The risk of malignancy in these lesions is estimated at 5 - 15% of cases. Malignant behavior cannot be predicted based on morphology alone and relies on the identification of metastases. Tumors associated with SDHB mutations (loss of SDHB staining) are reported to have an increased risk of metastases.
- Microscopic description: This specimen shows an unencapsulated, monomorphous population of round tumor cells in a nested / zellballen pattern with delicate vascular septa and intervening extravasated red blood cells. It predominantly involves the lamina propria of the bladder but in 1 tissue piece clearly involves muscularis propria. The tumor cells have abundant amphophilic cytoplasm and vesicular chromatin with occasional small nucleoli. There is no necrosis, diffuse growth pattern or vascular space invasion identified. The mitotic count is (maximally) 1/10 high power fields. Immunohistochemistry shows the tumor cells to be positive for GATA3 with strong and diffuse expression of synaptophysin and chromogranin, as well as retention of SDHB staining. The tumor cells are negative for AE1 / AE3, HMWK and p63. The Ki67 proliferation index is < 1%. S100 shows faint nuclear and cytoplasmic staining with occasional sustentacular cells identified.
- Bladder, transurethral resection:
- Paraganglioma extending to the base of the tissue fragment (see comment)
- No muscularis propria sampled
- Comment: Paragangliomas in the bladder can exhibit local recurrence or metastasis in up to 15% of cases (BMC Urol 2013:13:22).
- Microscopic description: Sections show unremarkable surface urothelium with a lesion in the deep lamina propria comprised of large eosinophilic cells with hyperchromatic, focally enlarged nuclei with occasional intranuclear inclusions. A fine vascular plexus is identified in some areas. Necrosis and hemorrhage are not identified. Mitotic rate = 1/10 high power fields (field of view [FOV] = 0.55 mm). The lesion extends to the cauterized base of the specimen. Immunostains confirm the lesion expresses synaptophysin, chromogranin and GATA3. SDHB is retained. AE1 / AE3, CD45, p63 and NKX3.1 are negative.
Differential diagnosis
- Invasive urothelial carcinoma:
- May have stromal reaction
- Positive for cytokeratins, p63 and uroplakin
- Prostatic adenocarcinoma:
- Renal cell carcinoma:
- Well differentiated neuroendocrine tumor:
- Positive for keratins
- Negative for GATA3, TH and GFAP (Hum Pathol 2020:103:72)
- Large cell neuroendocrine carcinoma:
- Focal pleomorphism, frequent prominent nucleoli
- High mitotic activity with high Ki67 labeling index
- Variable expression of cytokeratins
- Melanoma:
- Granular cell tumor:
- Fine vascular plexuses absent
- Positive for nestin, inhibin and calretinin with diffuse expression of S100 and SOX10
- Negative for neuroendocrine markers
Additional references
Practice question #1
A 50 year old woman reported paroxysmal hypertension with episodic headache, palpitations and micturition attacks. Biochemical studies demonstrated elevated 24 hour urine metanephrines and normetanephrine. CT revealed a 2 cm bladder mass lesion which was resected transurethrally. Pathology showed paraganglioma. Regarding this entity, what immunostain can be performed to identify the strongest genetic prognosticator of poor outcomes?
- BRAF
- FH
- p53
- SDHB
Practice answer #1
D. SDHB. SDHB germline mutation is the strongest genetic risk factor for metastatic disease. The diagnosis of SDHB related paraganglioma can be supported by the loss of SDHB immunoreactivity in the tumor cells. Answer A is incorrect because while the presence of BRAF mutation has been described in a small subset of cases, it has not been proven to be associated with an increased risk for metastatic disease. Answer C is incorrect because while TP53 has been suggested to be a disease modifying gene, its association with a more aggressive disease behavior requires further studies. Answer B is incorrect because FH is a novel genetic risk factor for tumor aggressiveness but it is not the strongest genetic prognosticator of poor outcomes in paragangliomas.
Comment Here
Reference: Paraganglioma
Comment Here
Reference: Paraganglioma
Practice question #2
A 45 year old man presented with macroscopic hematuria and underwent cystoscopy, which revealed a 4 cm highly vascularized, pink violaceous, ovoid mass in the posterior bladder wall. Transurethral resection of the bladder tumor was performed. Which stain combination would be most consistent with bladder paraganglioma?
- Keratin negative, GATA3 negative, synaptophysin positive, S100 positive
- Keratin negative, GATA3 positive, synaptophysin positive, S100 positive
- Keratin positive, GATA3 negative, synaptophysin positive, S100 negative
- Keratin positive, GATA3 positive, synaptophysin negative, S100 negative
Practice answer #2
B. Keratin negative, GATA3 positive, synaptophysin positive, S100 positive. In paragangliomas, tumor cells are positive for GATA3 and neuroendocrine markers while negative for keratins; sustentacular cells are positive for S100. Answer D is incorrect because that stain combination is most consistent with urothelial carcinoma. Answer C is incorrect because that stain combination is most consistent with epithelial neuroendocrine neoplasm. Answer A is incorrect because paragangliomas are typically positive for GATA3.
Comment Here
Reference: Paraganglioma
Comment Here
Reference: Paraganglioma