Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Marotti J. Columnar cell change / hyperplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastcolumnarcelllesion.html. Accessed April 26th, 2024.
Definition / general
- Enlarged terminal duct lobular units (TDLUs) with irregularly dilated acini lined by columnar epithelial cells
- Intraluminal secretions and calcifications common
Essential features
- Terminal duct lobular units are lined by columnar epithelial cells
- Lacks low grade cytologic atypia of flat epithelial atypia and architectural atypia of atypical ductal hyperplasia or ductal carcinoma in situ
Terminology
- WHO acceptable:
- Columnar cell change
- Columnar cell hyperplasia
- Not recommended by WHO:
- Blunt duct adenosis
- Columnar alteration of lobules
- Columnar metaplasia
- Hyperplastic unfolded lobules
- Hyperplastic enlarged lobular units
- Enlarged lobular units with columnar alteration
- Lesions with cytologic atypia are flat epithelial atypia (FEA)
ICD coding
Epidemiology
- Columnar cell lesions (columnar cell change / hyperplasia and flat epithelial atypia) seen in as high as 42% of biopsies for calcifications (Am J Surg Pathol 1998;22:1521)
Sites
- Breast terminal duct lobular units
Pathophysiology
- Might represent the earliest nonobligate precursor in low grade breast neoplasia pathway and a marker for potential presence of atypia
Etiology
- Unknown
Clinical features
- No specific clinical features
- Most often detected on screening mammography when associated with microcalcifications
Diagnosis
- Image guided needle core or surgical excisional biopsy with tissue histologic examination
- Diagnosis is reproducible with available histologic diagnostic criteria (Mod Pathol 2006;19:172)
Radiology description
- Heterogeneously dense tissue with clustered, amorphous or fine pleomorphic calcifications on mammography (Radiographics 2007;27:S79)
- Branching microcalcifications are not common (Am J Surg Pathol 1998;22:1521)
Radiology images
Prognostic factors
- Slight increased risk for breast cancer development (relative risk ~1.5) but risk with columnar cell change / hyperplasia not independent of risk associated with concurrent proliferative lesions (Breast Cancer Res 2010;12:R61, Cancer 2008;113:2415)
- Can be associated with other lesions on the low grade breast neoplasia pathway (flat epithelial atypia, atypical ductal hyperplasia, low grade ductal carcinoma in situ, lobular neoplasia) (Surg Pathol Clin 2018;11:177)
Case reports
- 43 year old woman with columnar cell hyperplasia and mucocele-like lesion (J Med Case Rep 2008;2:138)
- 2 cases (41 and 49 year old Japanese women) in which epithelial detachment artifact of columnar cell lesions was thought to result in pseudomicropapillae mimicking atypia (Virchows Arch 2013;463:93)
Treatment
- Excision not required when columnar cell change / hyperplasia without atypia is the most significant pathology in core biopsy specimens
- No further management required when columnar cell lesions are the most significant pathology in excision specimens
- Reference: Ann Surg 2012;255:259
Gross description
- No specific gross features
Microscopic (histologic) description
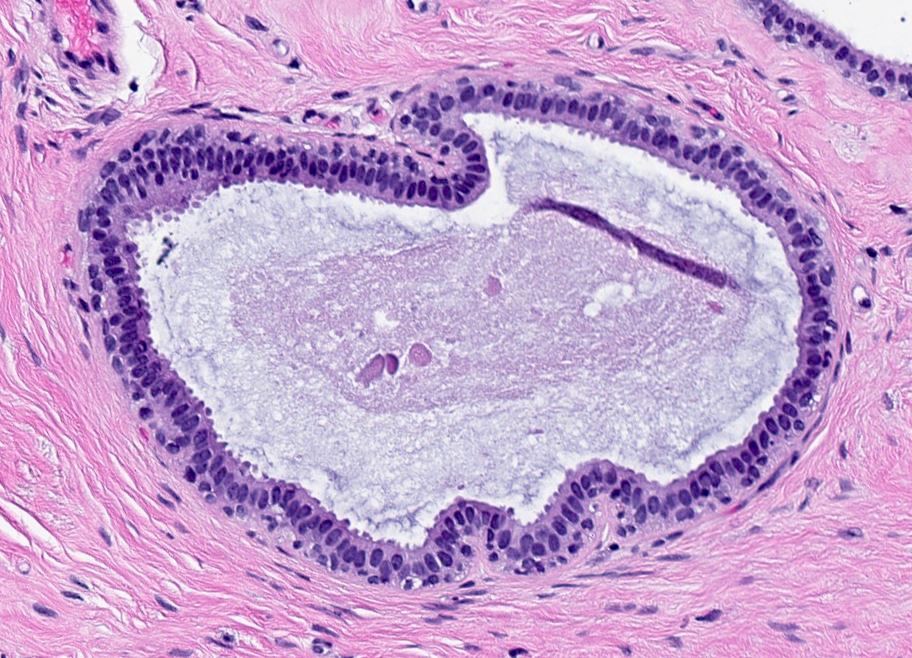
- Columnar cell change:
- Terminal duct lobular units with irregular, variably dilated acini
- Acini lined by 1 - 2 cell layers
- Lining cells have uniform, ovoid to elongated nuclei oriented perpendicular to basement membrane
- Apical snouts are frequently present
- Luminal secretions and calcifications may be present
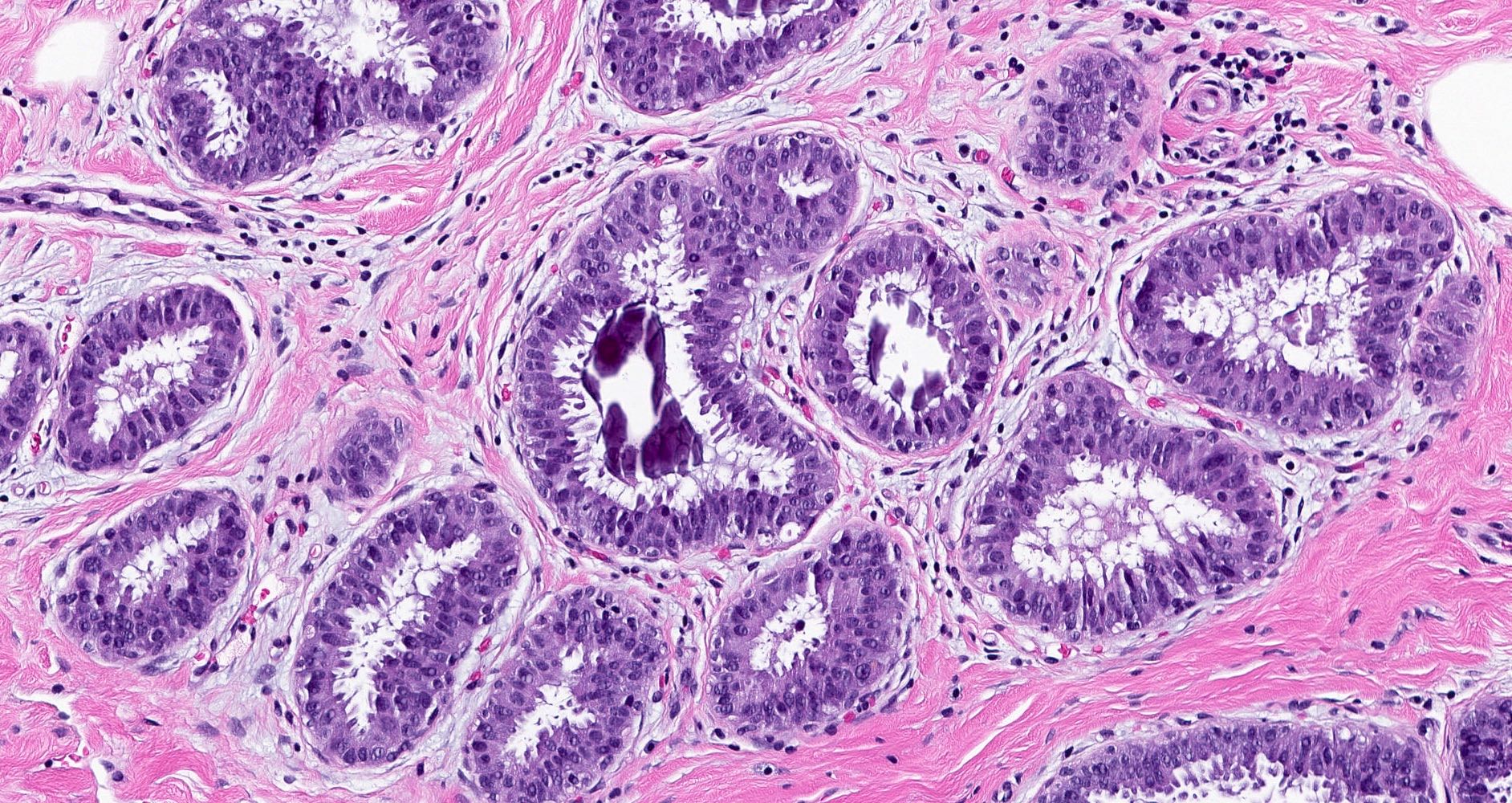
- Columnar cell hyperplasia:
- Terminal duct lobular units with irregular, variably dilated acini
- Acini lined by stratified cells (more than 2 cell layers); may form tufts or mounds
- Lining cells have uniform, ovoid to elongated nuclei that may appear crowded and overlap
- Apical snouts often present
- Luminal secretions and calcifications may be present
- Columnar cell change / hyperplasia with cytologic atypia (high nuclear cytoplasmic ratio, irregular nuclear chromatin, variably prominent nucleoli) can be classified as flat epithelial atypia
- Round nuclei with variably prominent nucleoli and loss of orientation perpendicular to basement membrane is flat epithelial atypia
- Rigid bars, arcades and true micropapillations is atypical ductal hyperplasia or low grade ductal carcinoma in situ
- Reference: Adv Anat Pathol 2003;10:113
Microscopic (histologic) images
Cytology description
- Range of atypia; cannot reliably differentiate from papillary neoplasms or well differentiated adenocarcinoma
- Flat sheets of cells with distinct cell borders, finely granular cytoplasm, enlarged nuclei and few myoepithelial cells (Diagn Cytopathol 2007;35:73)
- 3 dimensional clusters of polygonal epithelial cells mixed with myoepithelial cells; palisading columnar cells peripherally (Diagn Cytopathol 2004;31:370)
Positive stains
Molecular / cytogenetics description
- Loss of 16q (Mod Pathol 2018;31:1816, Am J Surg Pathol 2005;29:734)
- Low prevalence of molecular alterations in columnar cell change; progressive accumulation of allelic damage through columnar cell hyperplasia, atypia and invasive carcinoma (Mod Pathol 2006;19:344)
Sample pathology report
- Right breast, needle core biopsy:
- Columnar cell change and columnar cell hyperplasia with associated microcalcifications
Differential diagnosis
- Cysts:
- Attenuated, cuboidal or apocrine epithelium (noncolumnar)
- Apocrine metaplasia:
- Abundant, granular eosinophilic cytoplasm
- Round nuclei with prominent nucleoli
- Prominent apical snouting not typically seen
- Cystic hypersecretory hyperplasia:
- Cystic structures containing dense eosinophilic colloid-like material
- Epithelium can demonstrate spectrum of alterations
- Flat epithelial atypia:
- Dilated terminal duct lobular units with round contours
- Low grade, monomorphic, round to ovoid nuclei with variably prominent nucleoli and increased nuclear cytoplasmic ratio
- Nuclei lose perpendicular orientation to basement membrane
- Atypical ductal hyperplasia (ADH) and low grade ductal carcinoma in situ:
- Architectural features of atypical ductal hyperplasia and low grade ductal carcinoma in situ (arcades, bridges, papillations, round fenestrations) are present
- Ductal carcinoma in situ, clinging type:
- Marked cytologic atypia (typically high grade)
Additional references
Board review style question #1
Board review style answer #1
B. No additional action required. The image demonstrates the histologic features of columnar cell hyperplasia: stratified columnar epithelial cells forming tufts, exaggerated apical snouts and luminal calcifications. If columnar cell hyperplasia is the most significant alteration in the core biopsy sample and assuming adequate radiology and pathology correlation, no further clinical management is required. Surgical excision with negative margins is typically appropriate for ductal carcinoma in situ and invasive carcinomas. Tamoxifen is reserved for patients with higher risk lesions. Breast MRI is not indicated for columnar cell change / hyperplasia.
Comment Here
Reference: Columnar cell change / hyperplasia
Comment Here
Reference: Columnar cell change / hyperplasia
Board review style question #2
Columnar cell change / hyperplasia is often diagnosed because of
- Calcifications seen on mammography
- Large irregular mass seen on ultrasound
- New palpable breast mass
- Nipple discharge
Board review style answer #2
A. Calcifications seen on mammography. Columnar cell change / hyperplasia is often biopsied following identification of calcifications on mammography. Columnar cell change / hyperplasia can also be an incidental finding in core biopsies or surgical excisions.
Comment Here
Reference: Columnar cell change / hyperplasia
Comment Here
Reference: Columnar cell change / hyperplasia