Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Hulme K, Gupta R. HPV independent. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityHPVunrelatedoropharyngeal.html. Accessed May 14th, 2024.
Definition / general
- A subset of oropharyngeal squamous cell carcinomas that are not associated with high risk human papillomaviruses (HPV)
Essential features
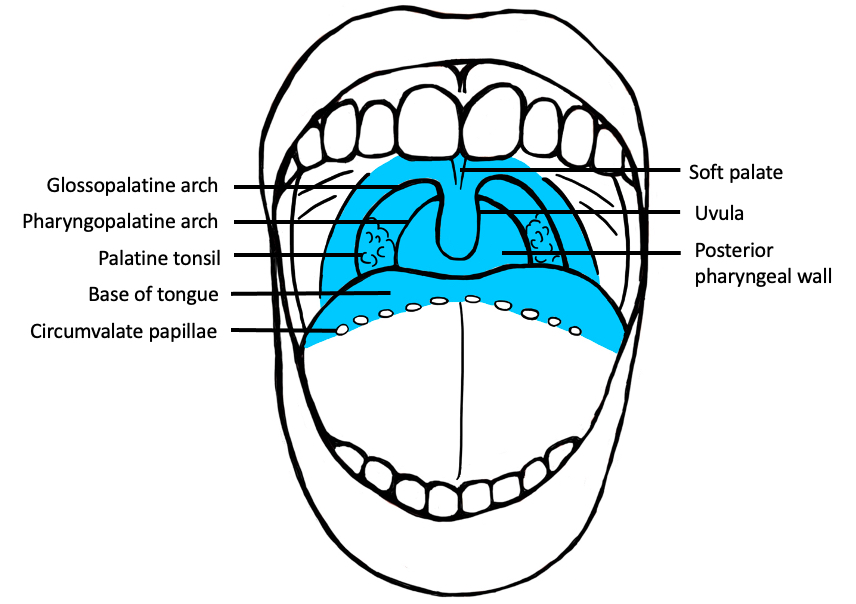
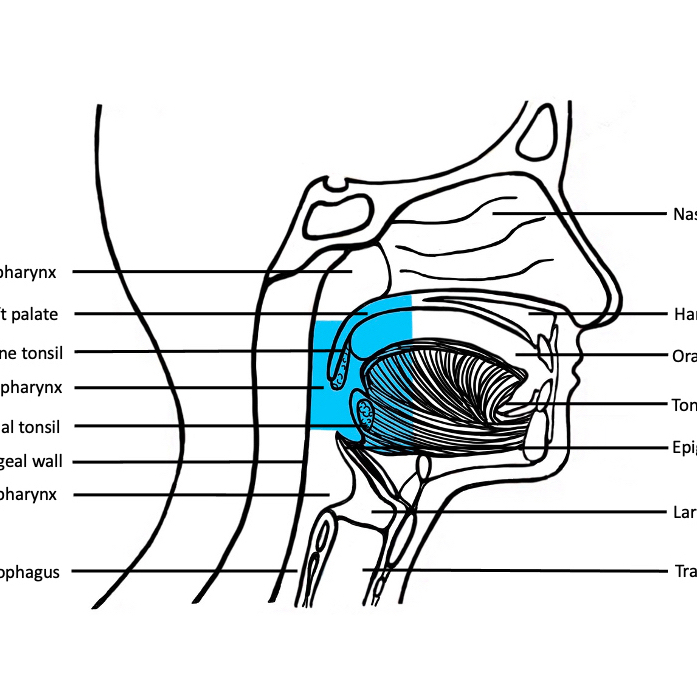
- Squamous cell carcinoma involving the oropharynx
- Oropharynx includes the soft palate, uvula, palatine tonsils, posterior third (base) of the tongue and posterior wall of the pharynx
- Associated with smoking and alcohol
- Not associated with HPV
- Resembles squamous cell carcinoma (SCC) and its morphologic variants observed in other head and neck mucosal sites; can show surface dysplasia, keratinization and desmoplasia
Terminology
- Keratinizing squamous cell carcinoma
ICD coding
Epidemiology
- Age: mean 61 years (standard deviation 10.49) (Cancer 2019;125:761)
- M:F = 3.2:1 (Cancer 2019;125:761)
- Higher incidence in Indian subcontinent, French Polynesia, New Caledonia and Papua New Guinea, Eastern Europe, North America, Australia and Brazil
Sites
- Oropharynx
- Most commonly soft palate
- Arises in the surface mucosa and invades neighboring structures with metastases to draining regional nodes
Pathophysiology
- Invasive lesion is typically preceded by progressively severe dysplasia
- Chronic insult with abrogation of DNA repair mechanisms and mutations in tumor suppressor genes, such as gatekeeper p53 (J Oncol 2011;2011:603740)
Etiology
- Most commonly chewing or smoking tobacco, heavy alcohol use and poor oral hygiene (J Natl Cancer Inst 2008;100:407)
- Also reported in association with syphilis, other infections (bacterial, fungal or viral) and Fanconi anemia (Int J Epidemiol 1994;23:381, Sci Rep 2017;7:4036, Arch Otolaryngol Head Neck Surg 2003;129:106)
Diagrams / tables
Clinical features
- Presents as nonhealing mucosal ulcer identified by patient or clinician and confirmed with nasoendoscopy and biopsy
- Difficulty and pain while swallowing
- Metastasis to ipsilateral or bilateral neck nodes may rarely be the initial presenting feature
Diagnosis
- Clinical examination with biopsy of primary lesion
- Biopsy of primary lesion may require examination under anesthesia of the oropharynx
- Cytology of lymph node metastases followed by biopsy of the primary lesion identified on diagnostic CT and PET scan
Radiology description
- Primarily used for staging of nodal drainage sites and distant spread
- PET may identify primary lesion in the rare setting of neck nodal disease of unknown origin
Prognostic factors
- Overall survival at 3 years 57% (N Engl J Med 2010;363:24)
- Prognostic factors
- Clinical
- Tobacco use (N Engl J Med 2010;363:24)
- Overall patient health, comorbidity and lifestyle factors
- Women have worse overall survival and cancer specific survival than men (Expert Rev Anticancer Ther 2020;20:813)
- Histological
- Size
- Depth of invasion
- Perineural invasion (J Surg Oncol 2015;111:352, Head Neck 2019;41:3992)
- Worst pattern of invasion (Am J Surg Pathol 2005;29:167)
- Completeness of resection
- Lymph node involvement
- Extranodal extension
- Stage as per the AJCC 8th edition chapter 11 oropharynx (p16) and hypopharynx (AJCC: Cancer Staging Manual [Accessed 12 December 2020])
- Clinical
Case reports
- 49 year old man with a lymphoepithelial carcinoma in the soft palate and uvula (Head Neck Pathol 2011;5:327)
- 58 year old woman with a spindle cell carcinoma of the palatine tonsil (Am J Otolaryngol 2008;29:123)
- 65 year old man with a basaloid squamous cell carcinoma of the retromolar trigone (J Oral Maxillofac Pathol 2011;15:192)
Treatment
- Surgical resection of the primary along with ipsilateral or bilateral elective neck dissection (N Engl J Med 2015;373:521)
- Surgical resection can be through transoral robotic surgery (TORS)
- Adjuvant radiotherapy and platinum based chemotherapy
- Immune check point inhibitors have demonstrated response in 25 - 29% patients (Future Oncol 2020;16:1235)
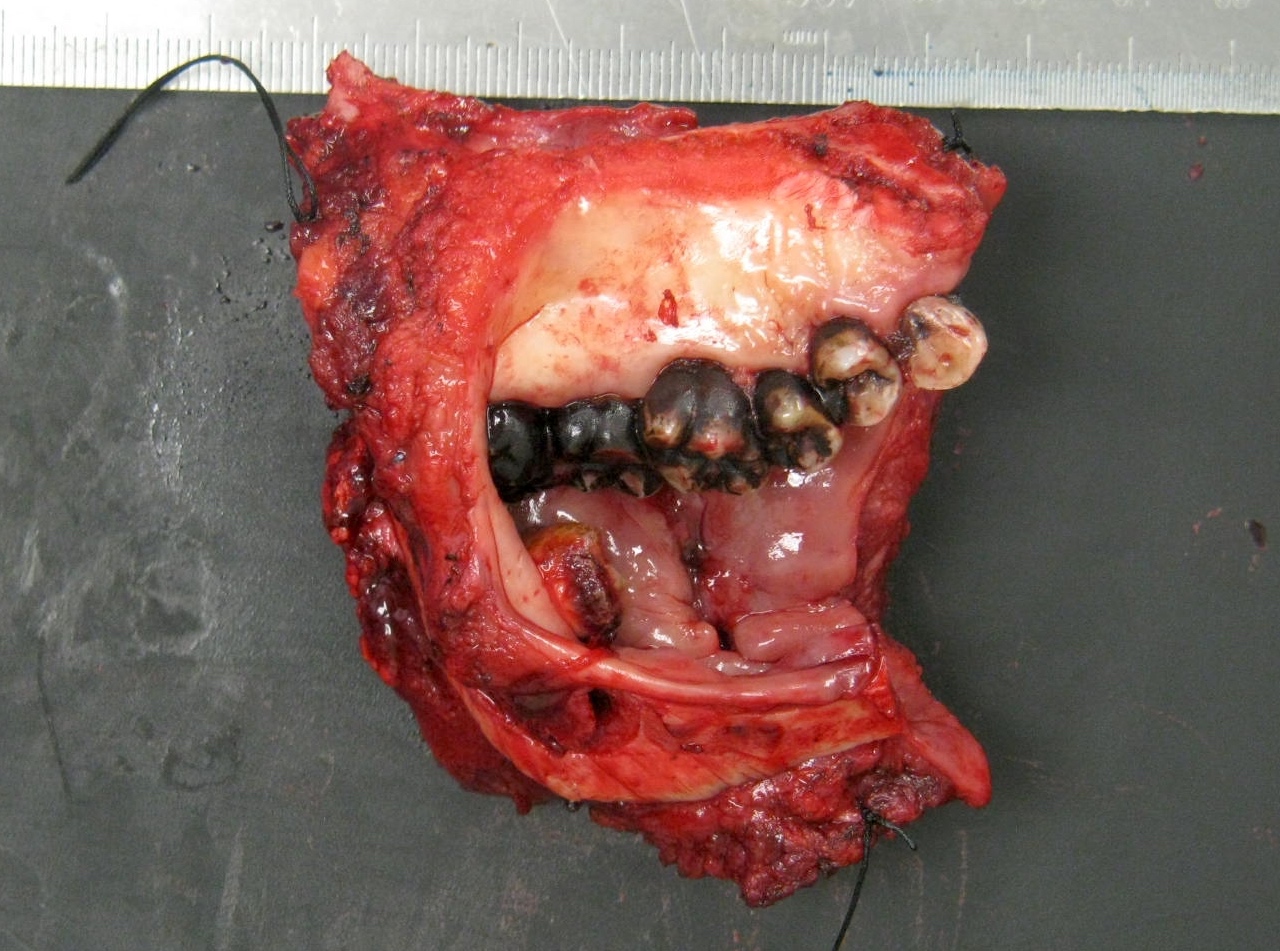
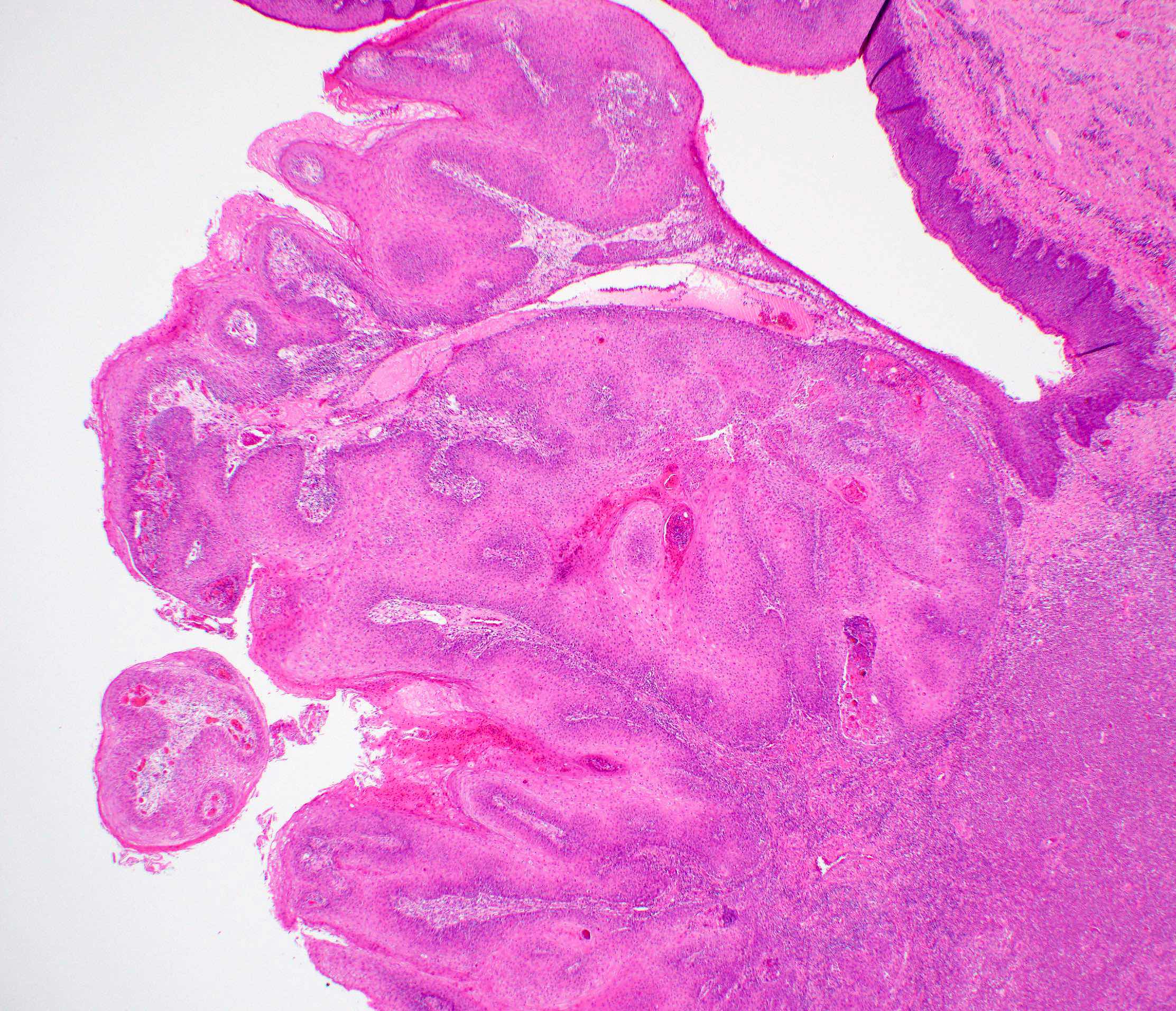
Gross description
- Macroscopic appearance varies with the morphologic type
- Common conventional squamous cell carcinoma shows an ulceroproliferative mucosal lesion with a firm gray-white infiltrative surface
- Verrucous and papillary squamous cell carcinomas demonstrate prominent exophytic, finger-like projections
- Spindle cell carcinoma generally presents as a mucosal polypoid lesion
Gross images
Frozen section description
- Not routinely done
- Value with confirming clearance of margins of primary lesion
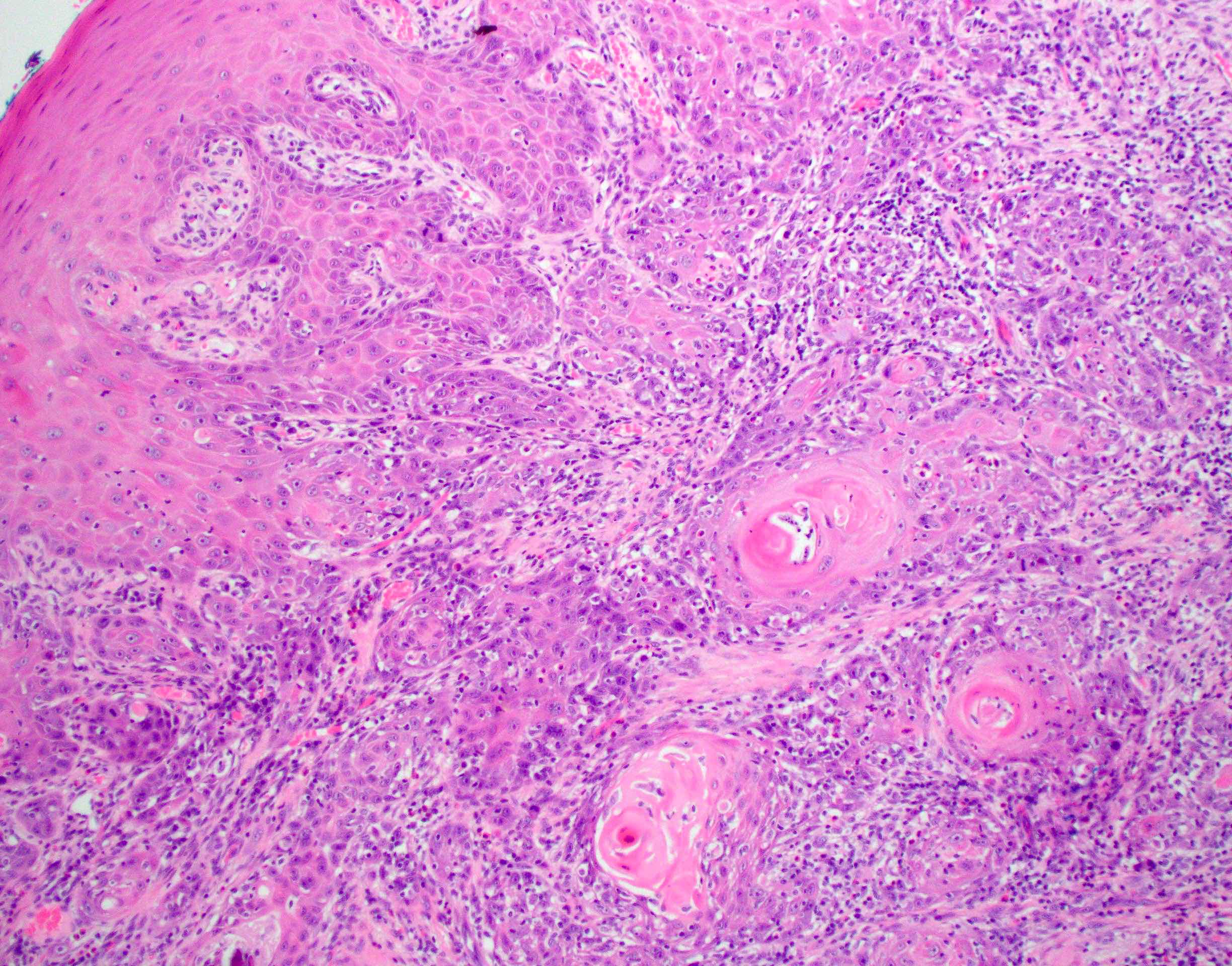
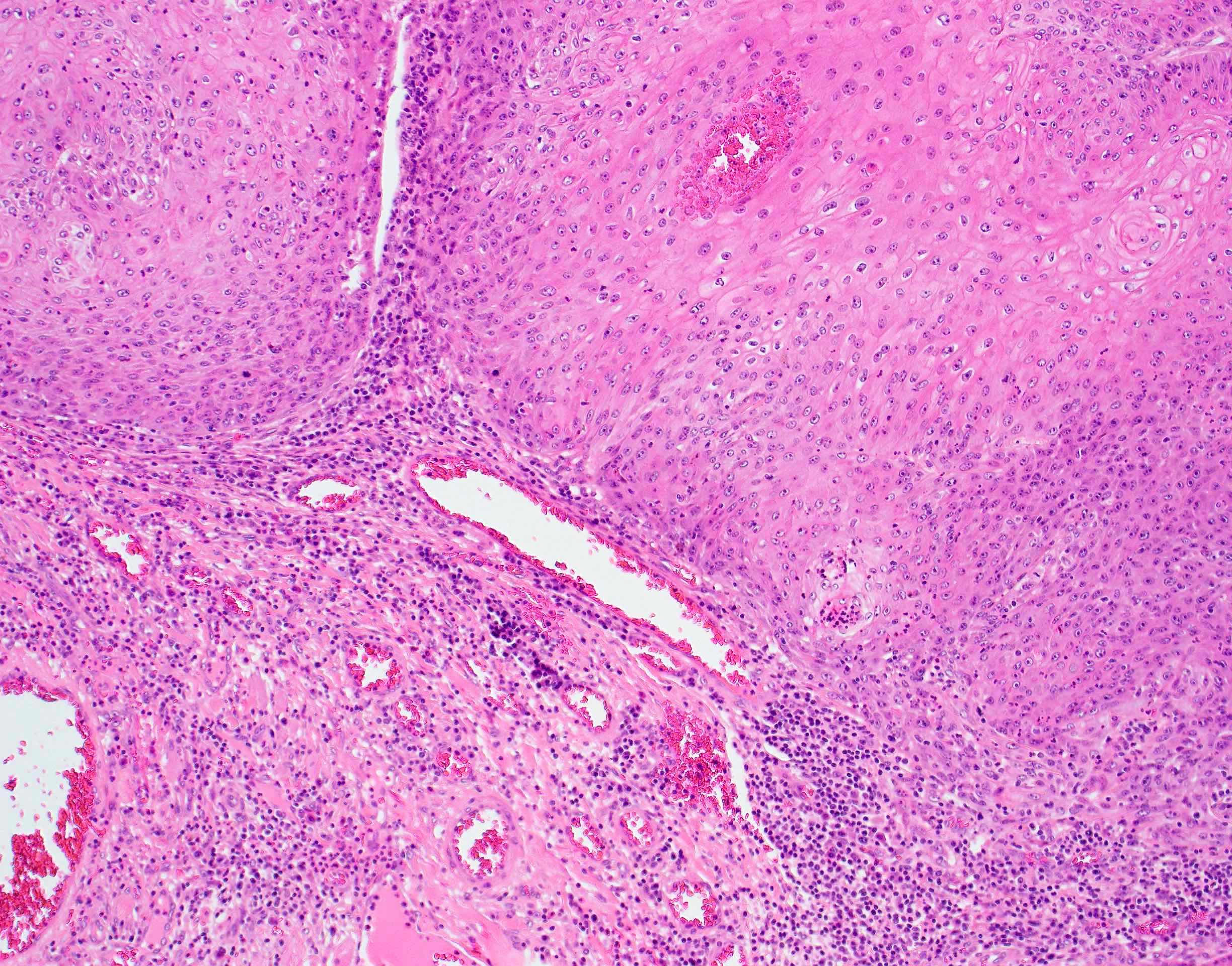
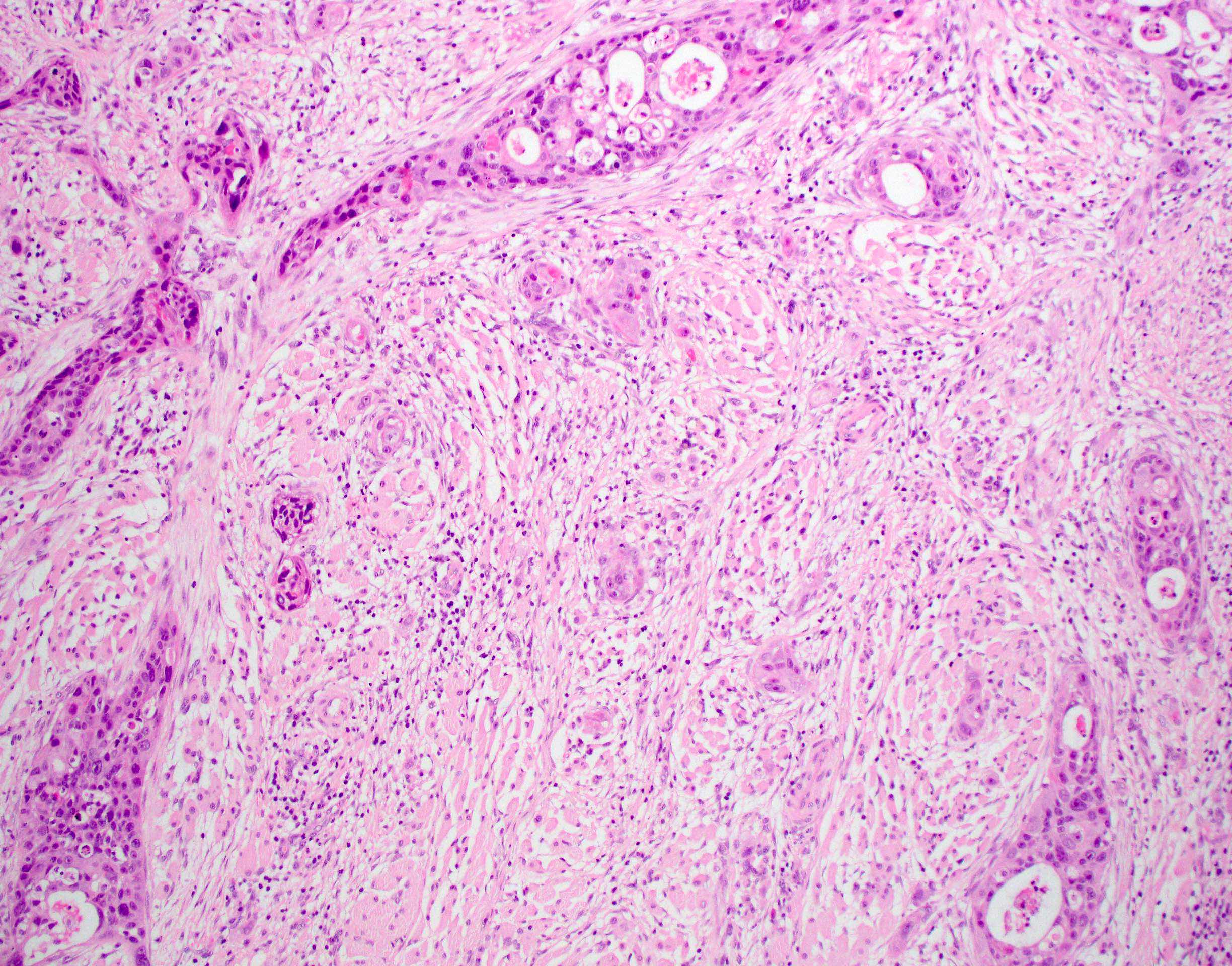
Microscopic (histologic) description
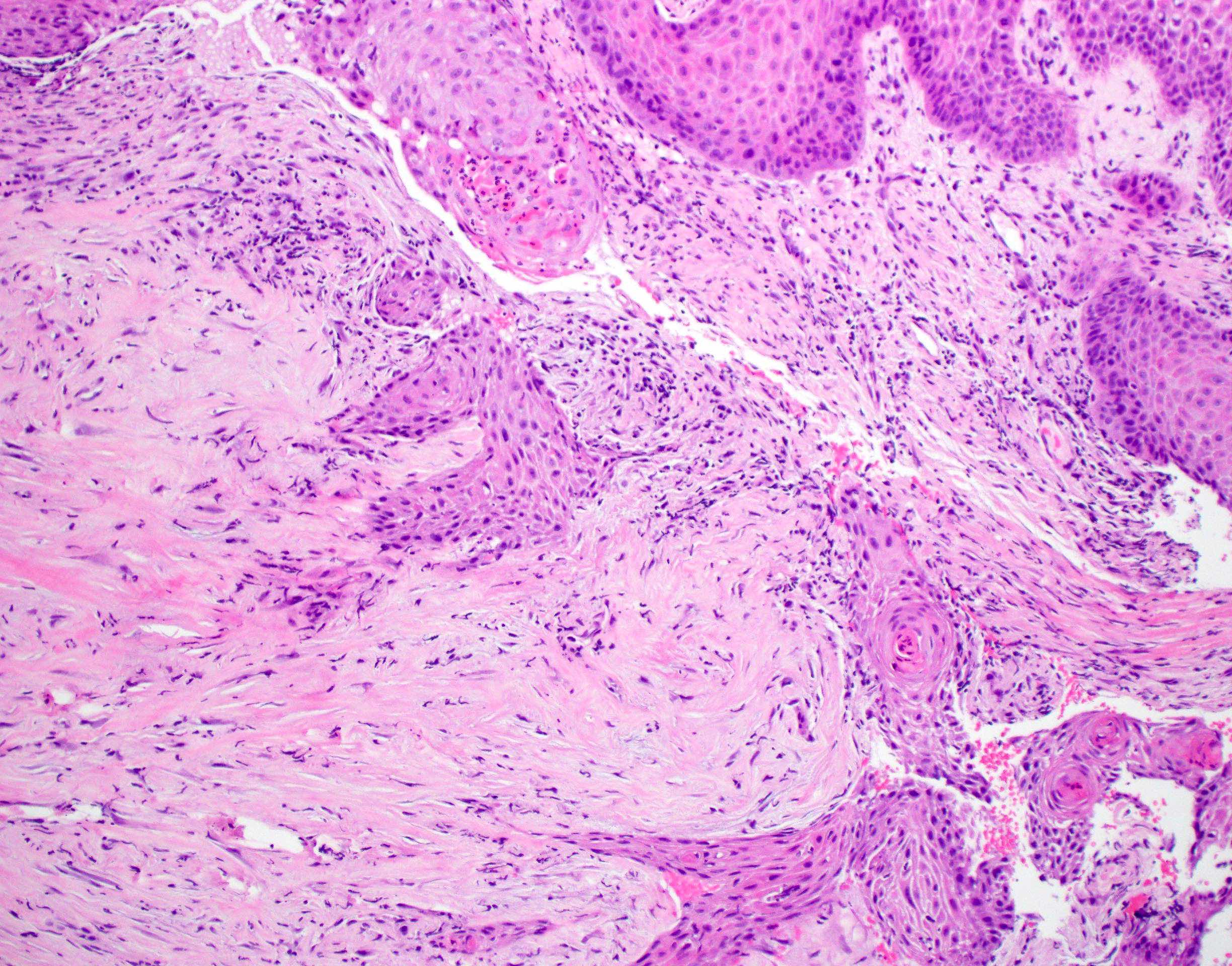
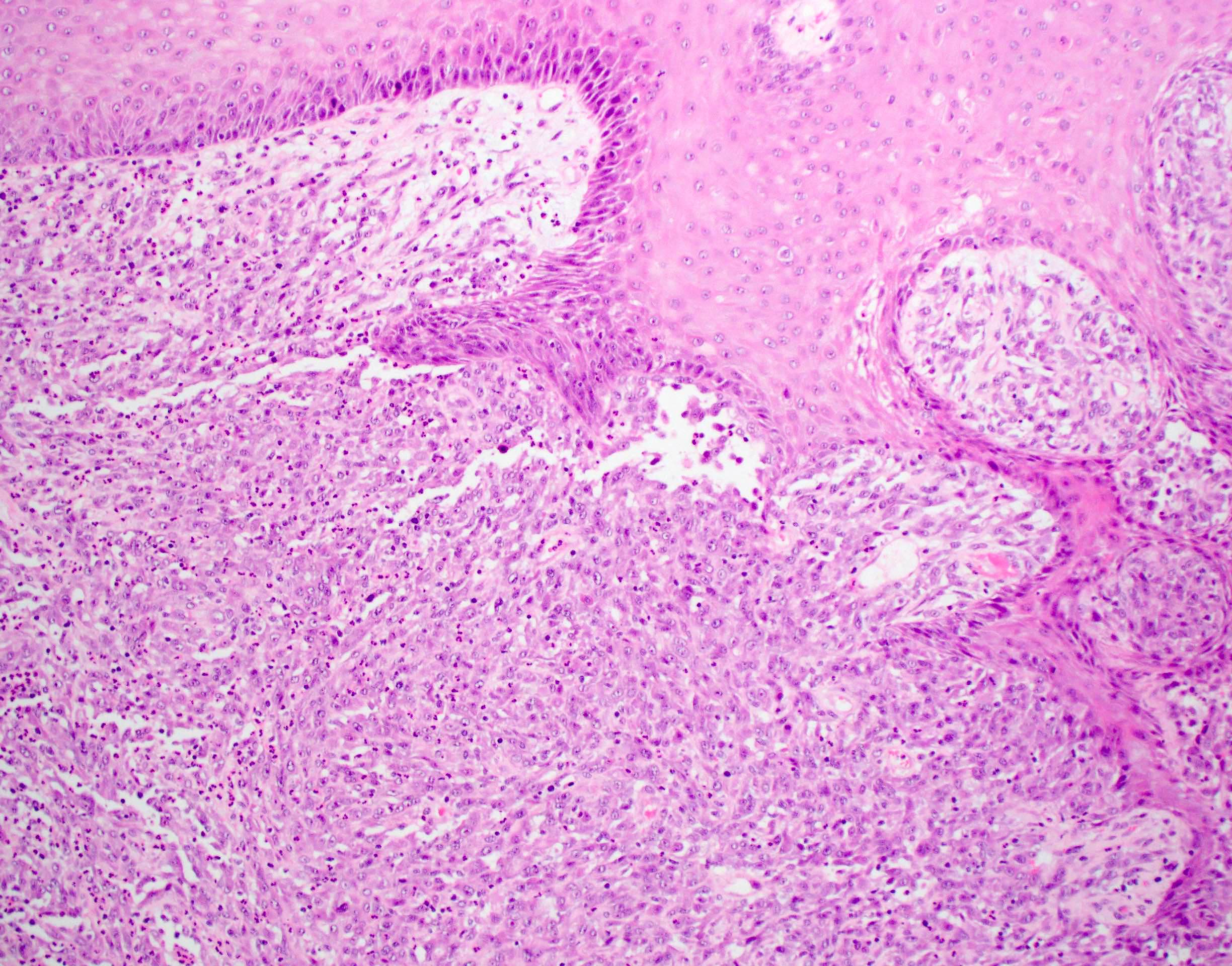
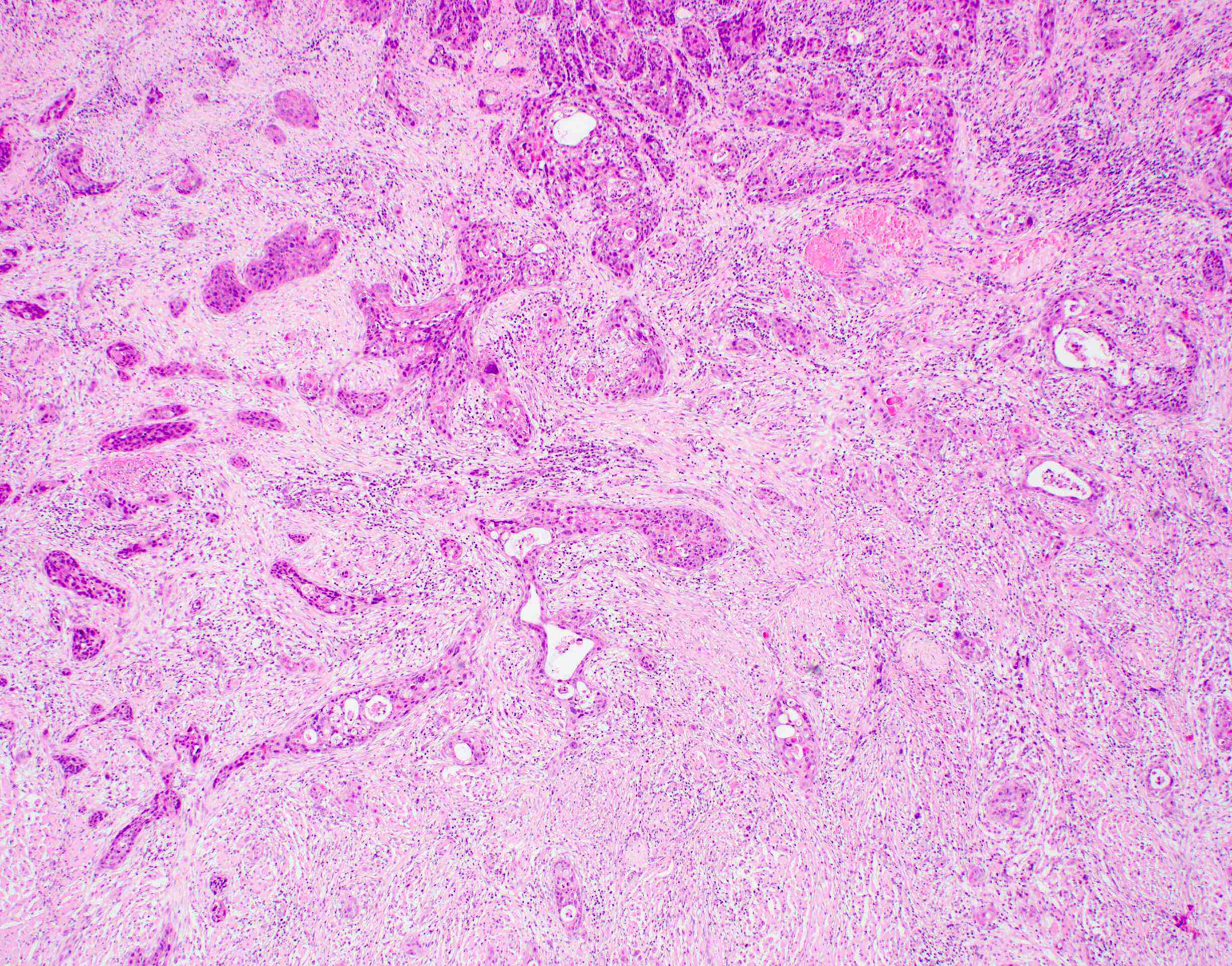
- Squamous cell carcinoma, conventional
- Most common and typical morphology of conventional keratinizing squamous cell carcinoma at any site
- Large polygonal malignant cells with intercellular bridges
- Cytoplasmic or extracellular eosinophilic keratin
- Dyskeratotic cells and squamous pearls
- Nuclear size, pleomorphism, hyperchromasia and mitoses increase with increasing grade
- Other morphological types
- Verrucous carcinoma
- Pronounced exophytic growth of well differentiated squamous epithelium
- Bulbous enlargement of the rete ridges with elephant foot appearance
- Broad pushing border
- Does not metastasize; good prognosis
- Carcinoma cuniculatum
- Well differentiated exophytic verruciform lesion with broad front of burrowing invasion
- Generally involves mucoperiosteal sites; rare in the oropharynx
- Papillary squamous cell carcinoma
- Well differentiated keratinocytes forming exophytic organized papillary structures with fibrovascular cores
- 70% of tumor must show papillary architecture
- Better prognosis than conventional squamous cell carcinoma
- Acantholytic squamous cell carcinoma (Head Neck Pathol 2012;6:438)
- Keratinocytes with loss of adhesion molecules appear "falling apart"
- May have pseudolumina mimicking glands or vessels but no mucin
- Adenosquamous carcinoma (Head Neck Pathol 2016;10:486)
- True glandular and squamous differentiation close but distinct and separate
- Poor prognosis with frequent metastases
- Basaloid squamous cell carcinoma (J Oral Maxillofac Pathol 2011;15:192)
- Cells with minimal cytoplasm
- Enlarged, angulated, hyperchromatic nuclei
- Basement membrane-like matrix
- Solid pattern with lobular configuration
- May have prominent peripheral palisading
- May have comedo type necrosis
- May have abrupt change to differentiated component
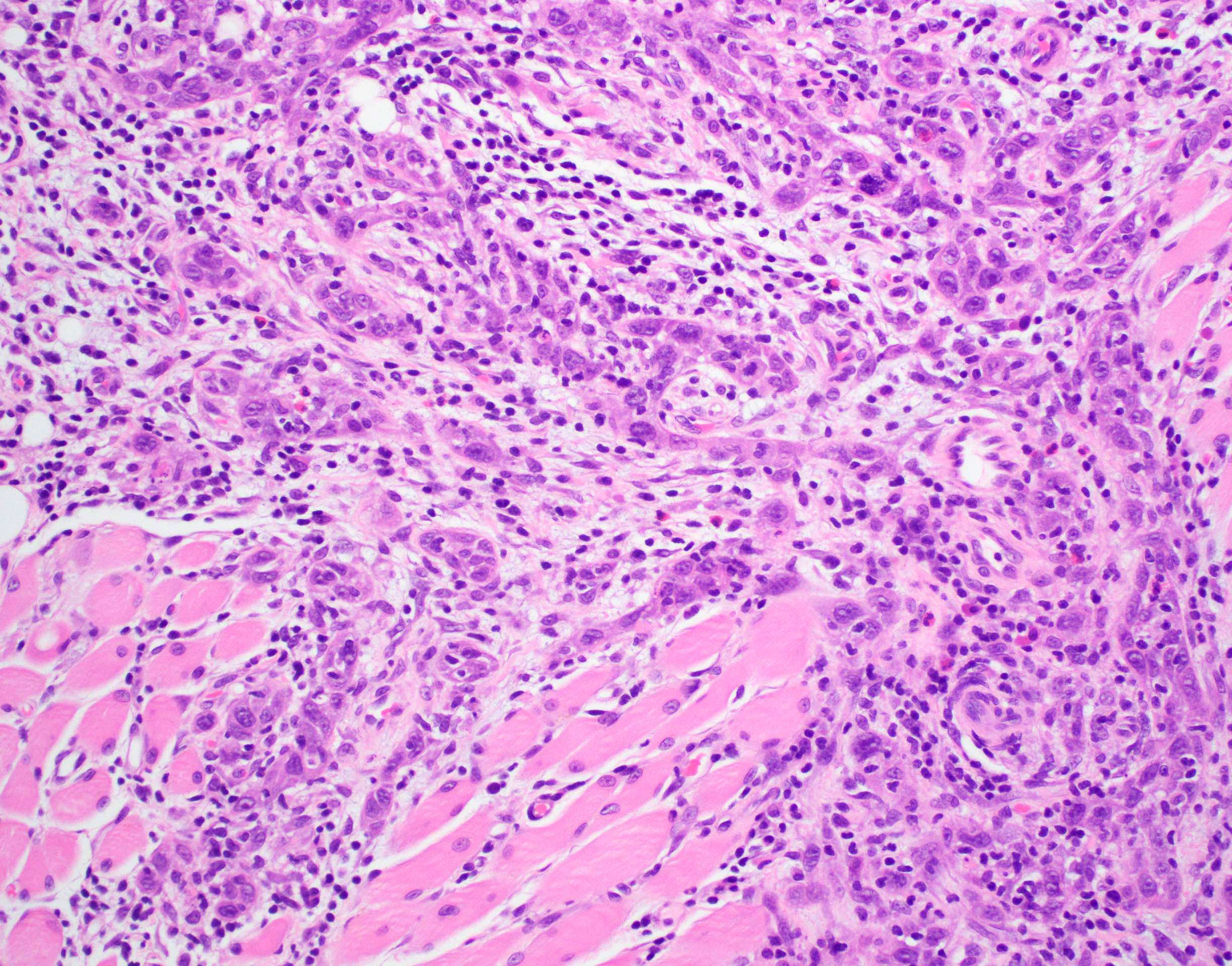
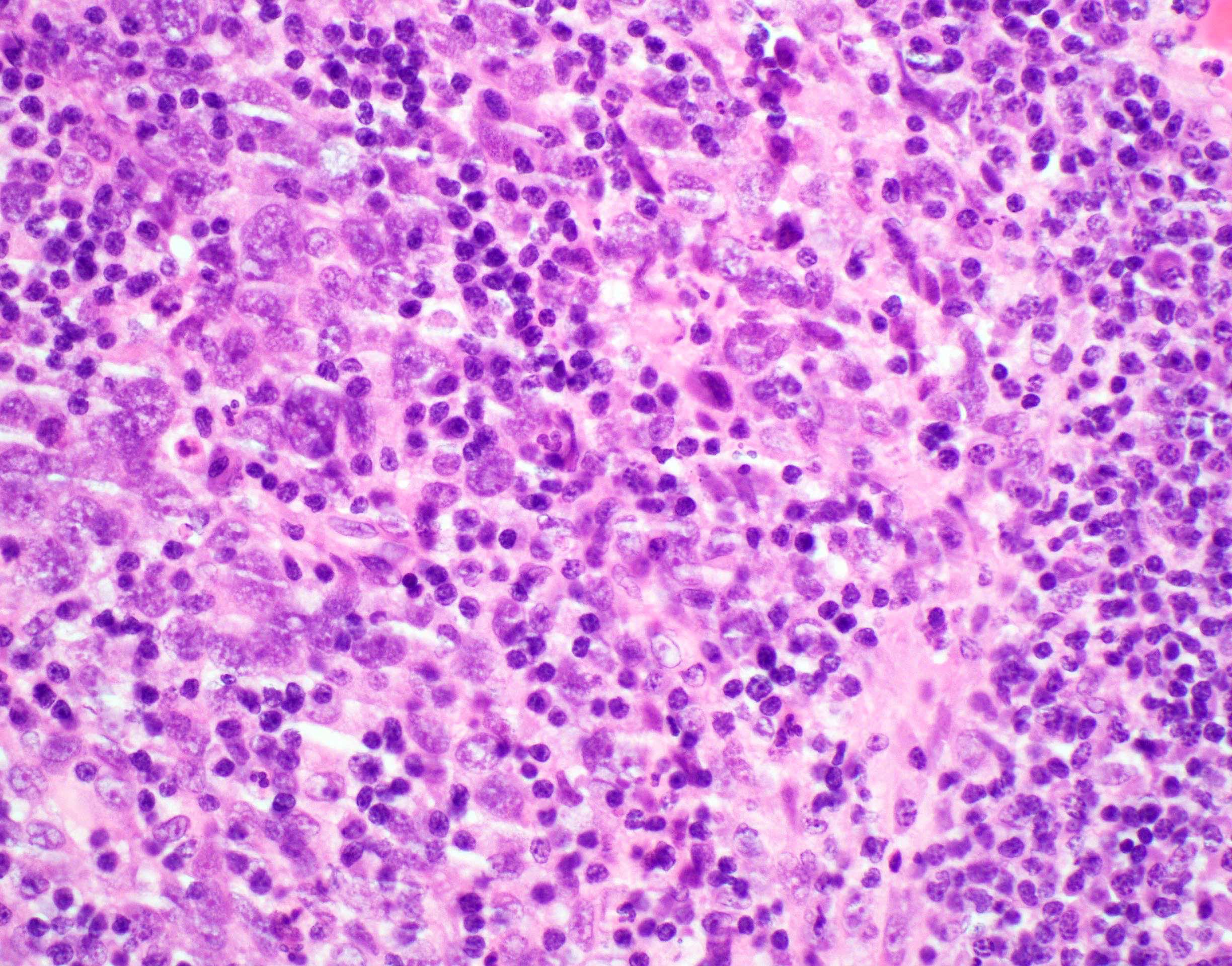
- Lymphoepithelial carcinoma (nonnasopharyngeal) (Head Neck Pathol 2011;5:327)
- Cohesive tumor nests of nonkeratinising epithelioid cells with prominent intermixed reactive lymphoplasmacytic infiltrate
- Present at high stage with metastases
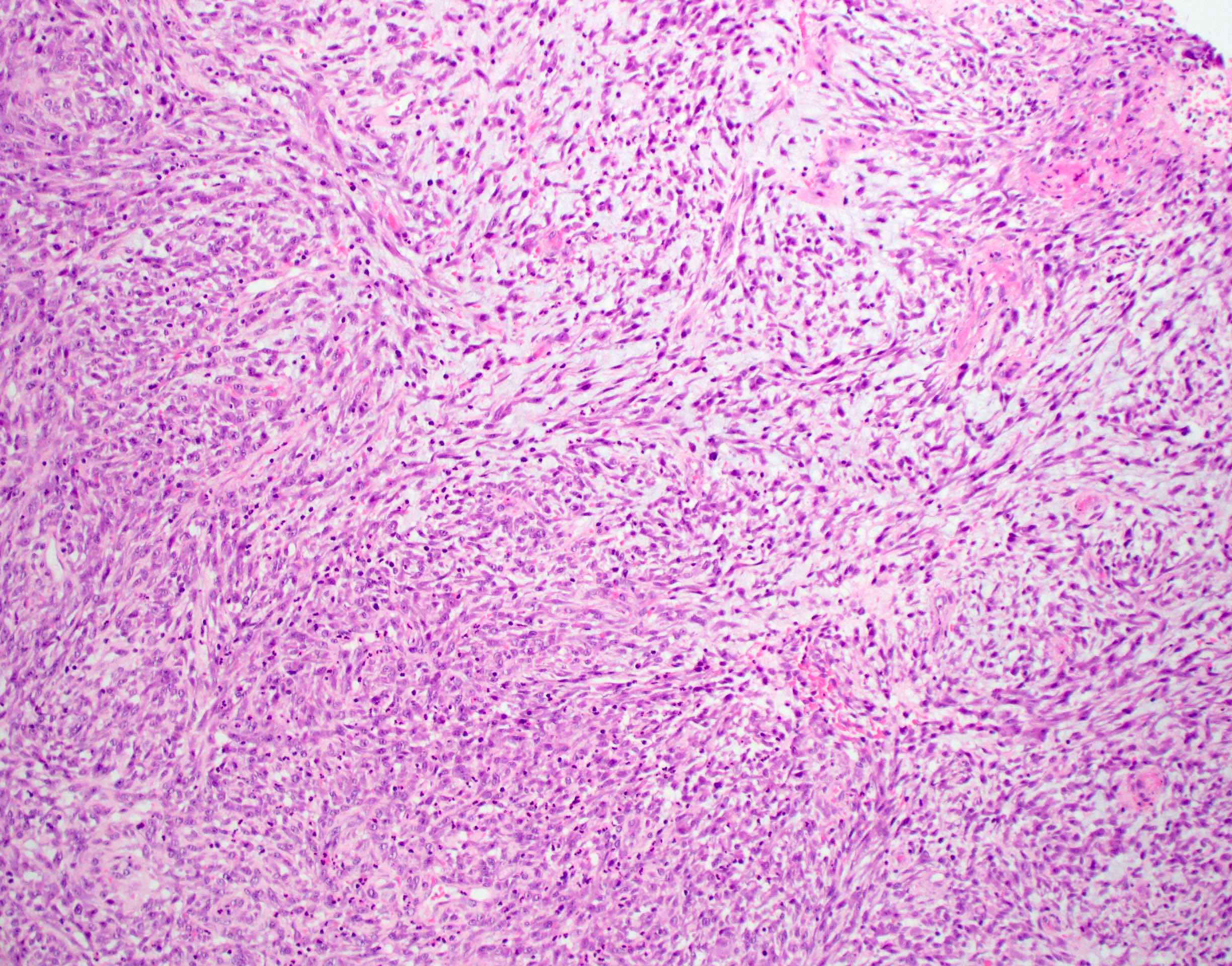
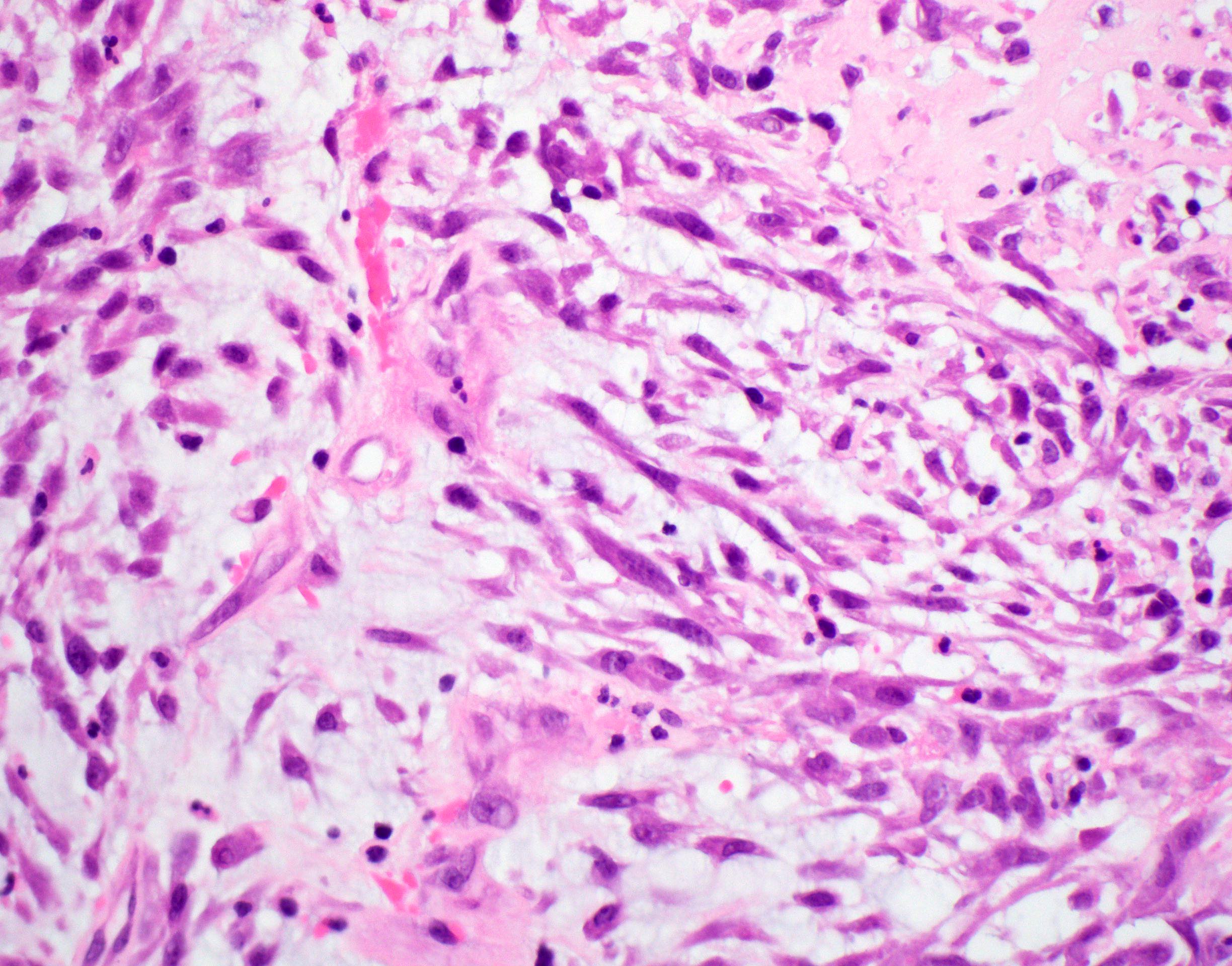
- Spindle cell / sarcomatoid squamous cell carcinoma (Am J Otolaryngol 2008;29:123)
- Most commonly occurs postradiotherapy or as second primary
- Mesenchymal in appearance
- Atypical plump spindled cells arranged in fascicles or storiform pattern
- May have metaplastic or neoplastic cartilage or bone
- Verrucous carcinoma
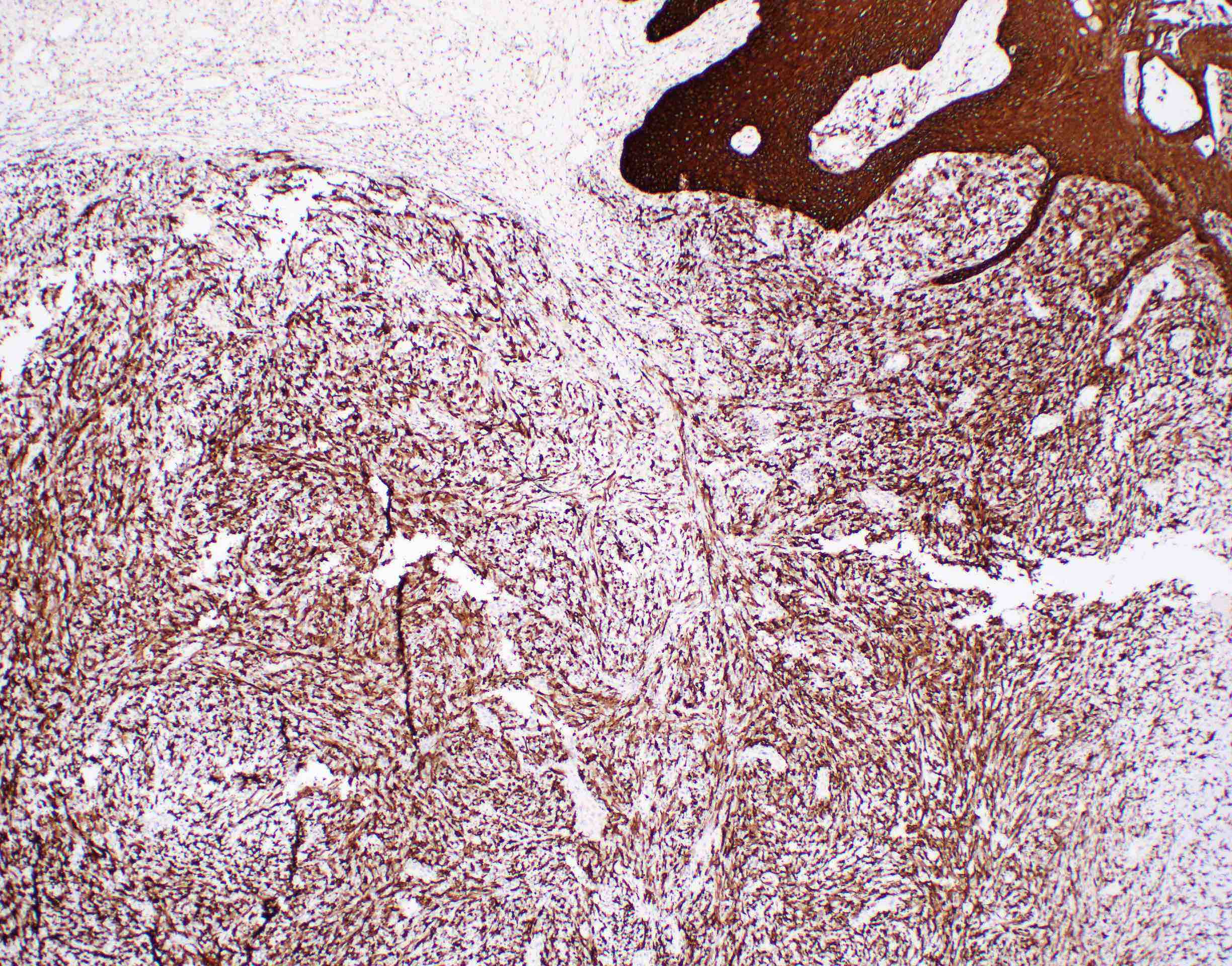
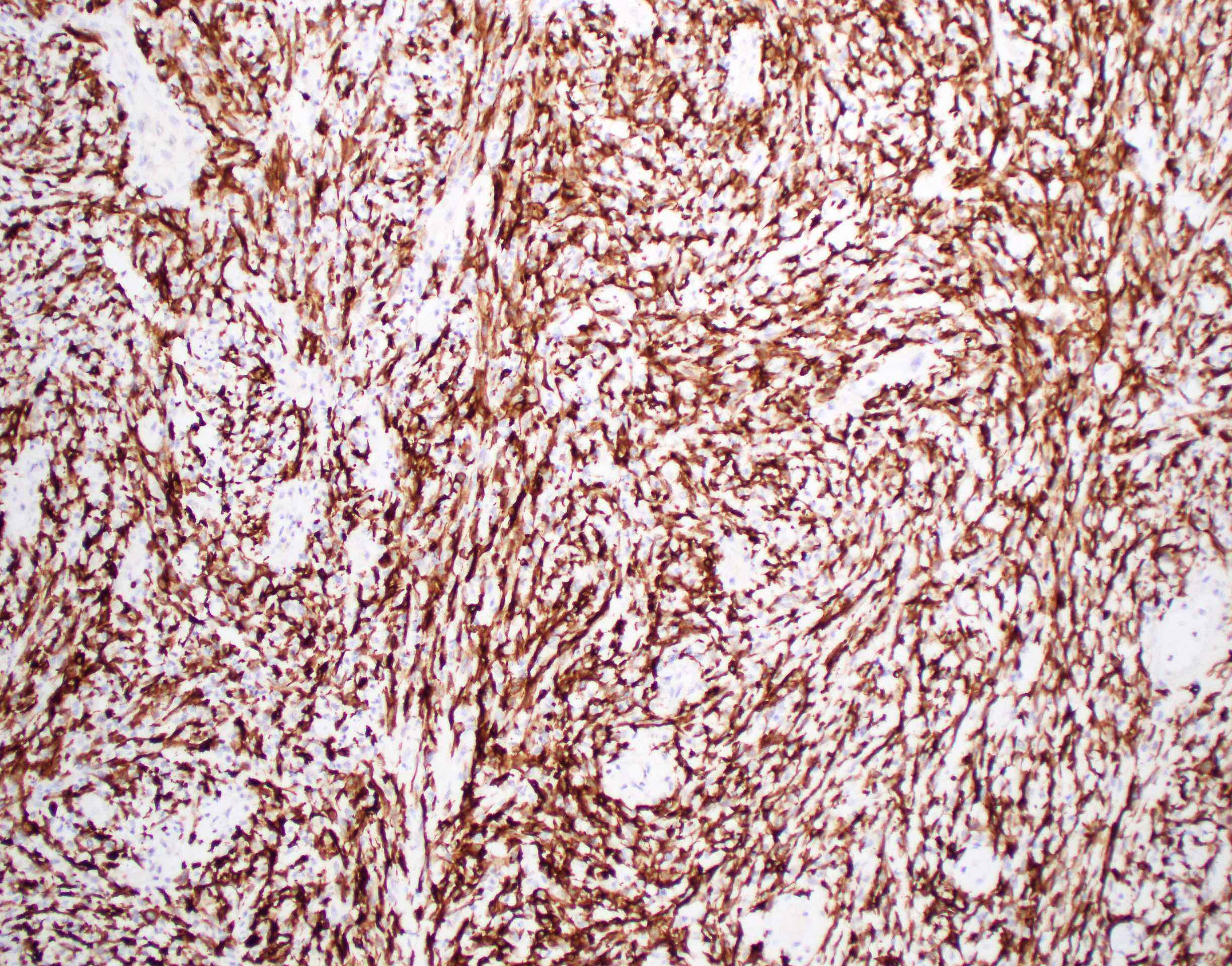
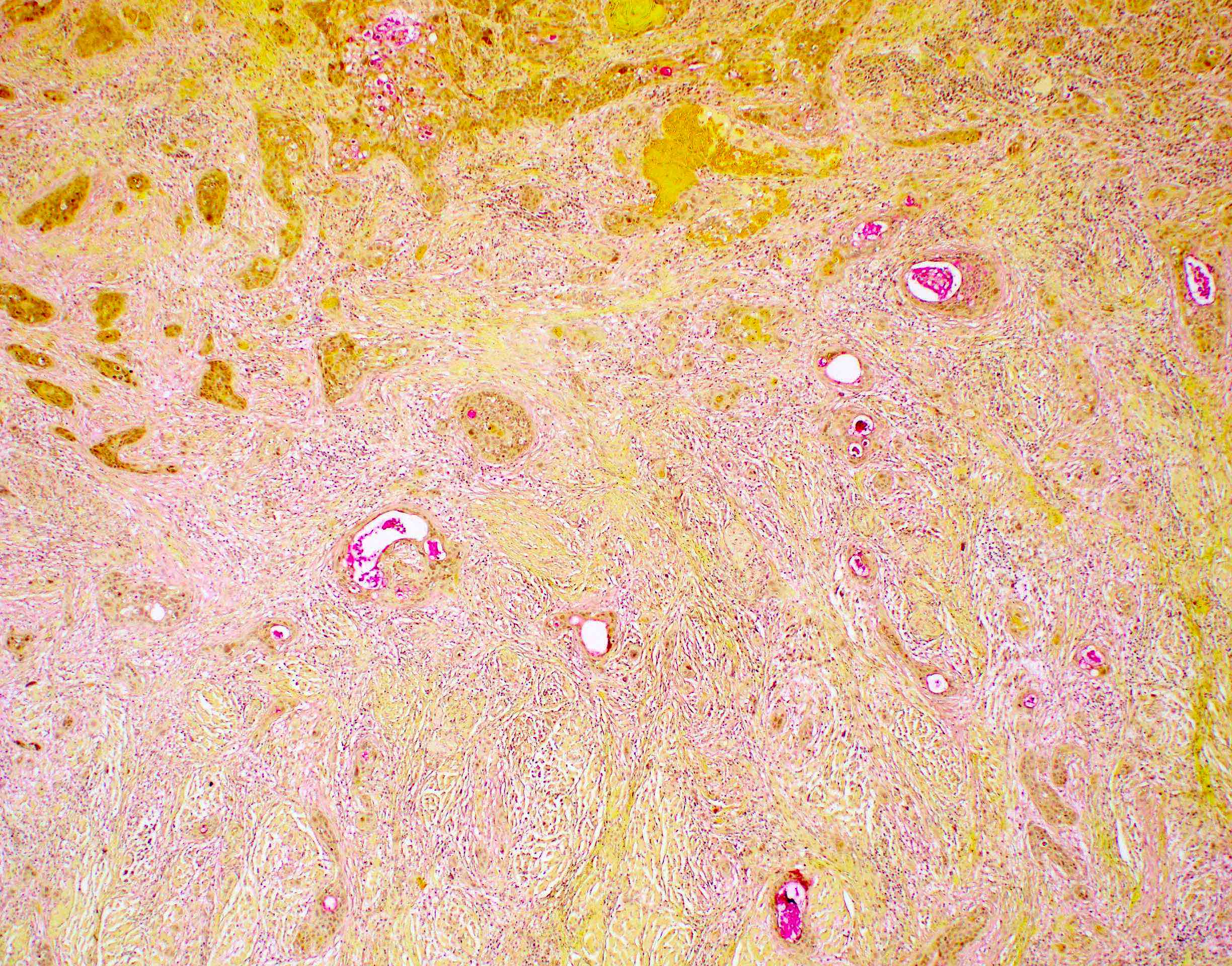
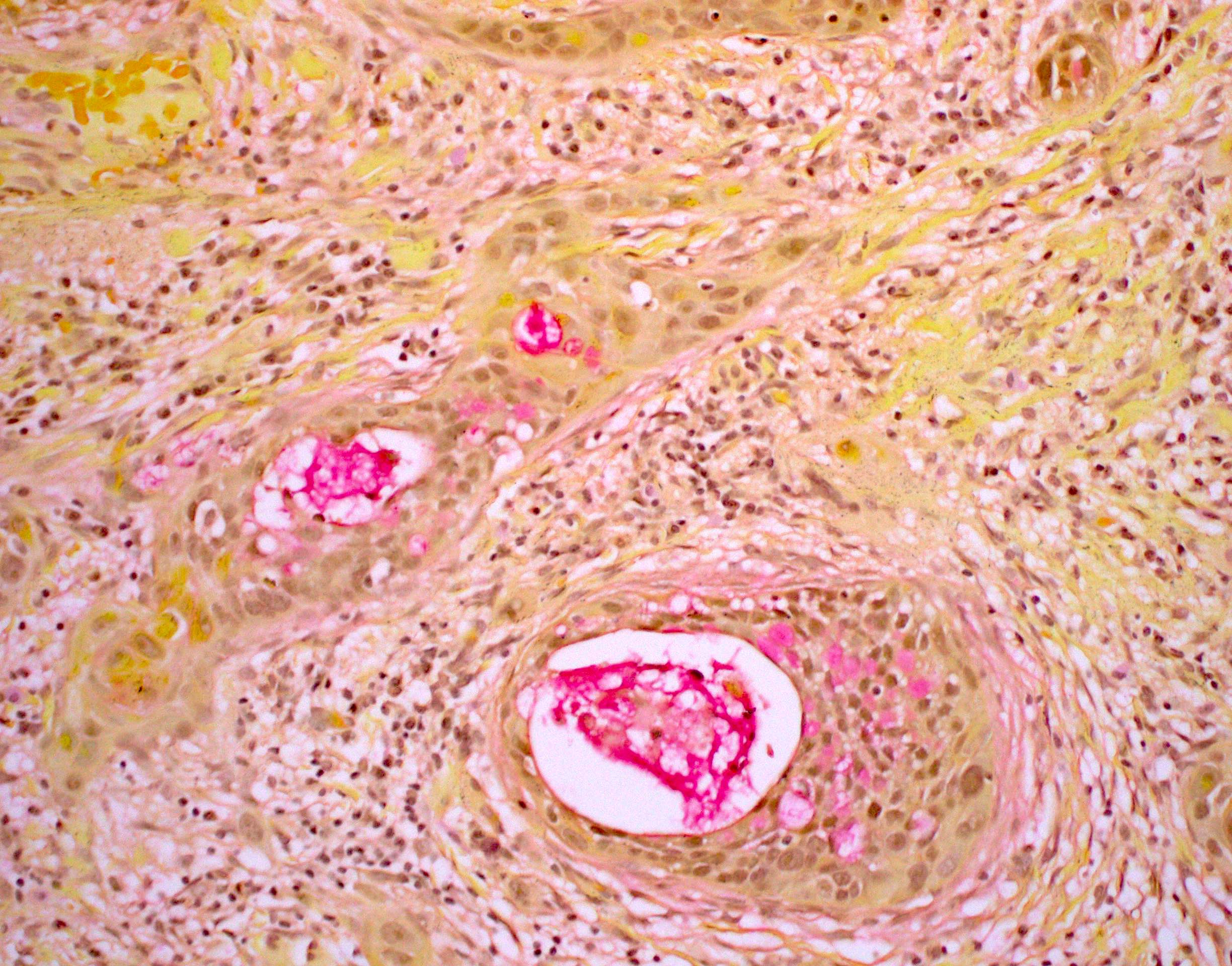
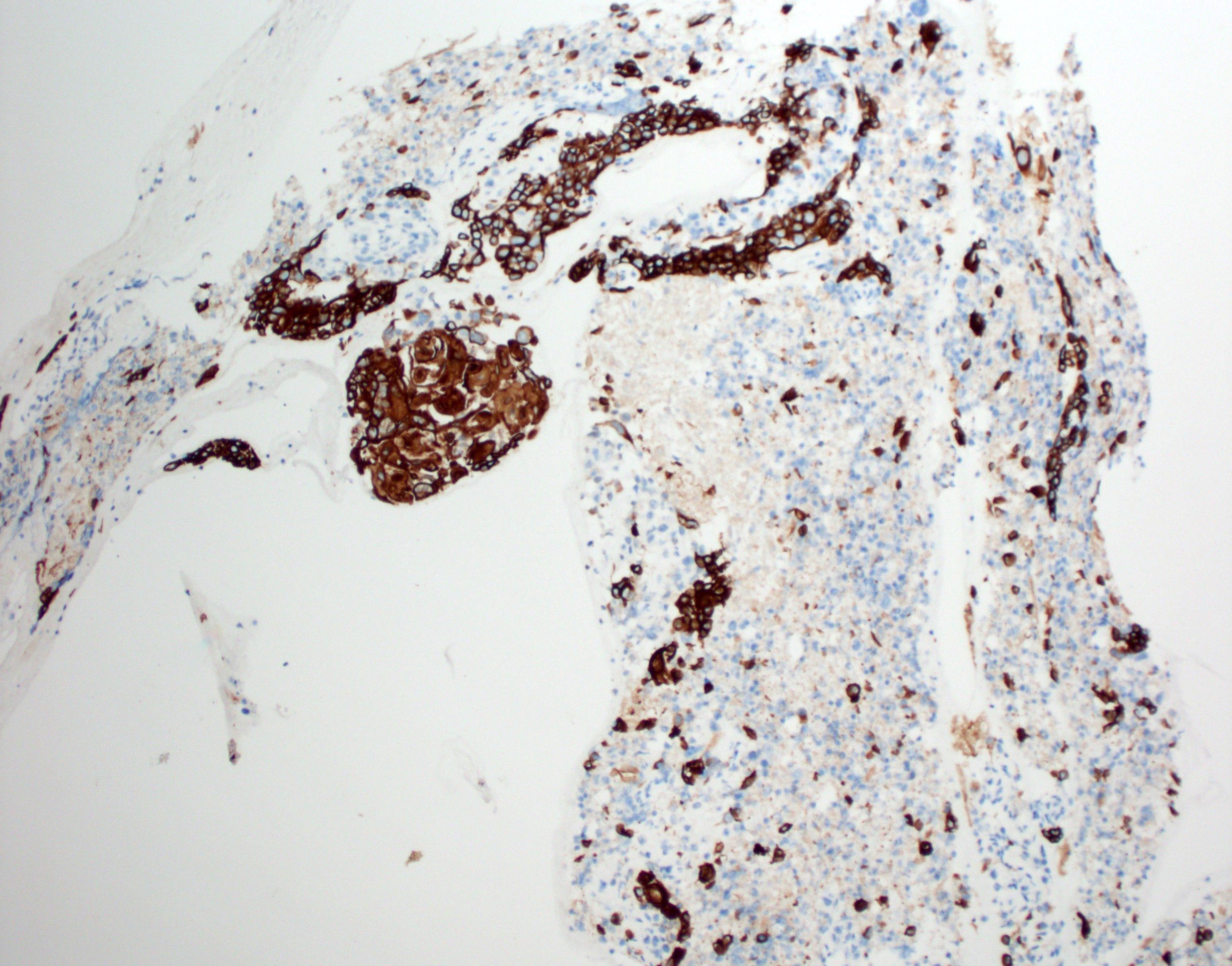
Microscopic (histologic) images
Contributed by Ruta Gupta, M.B.B.S., M.D.
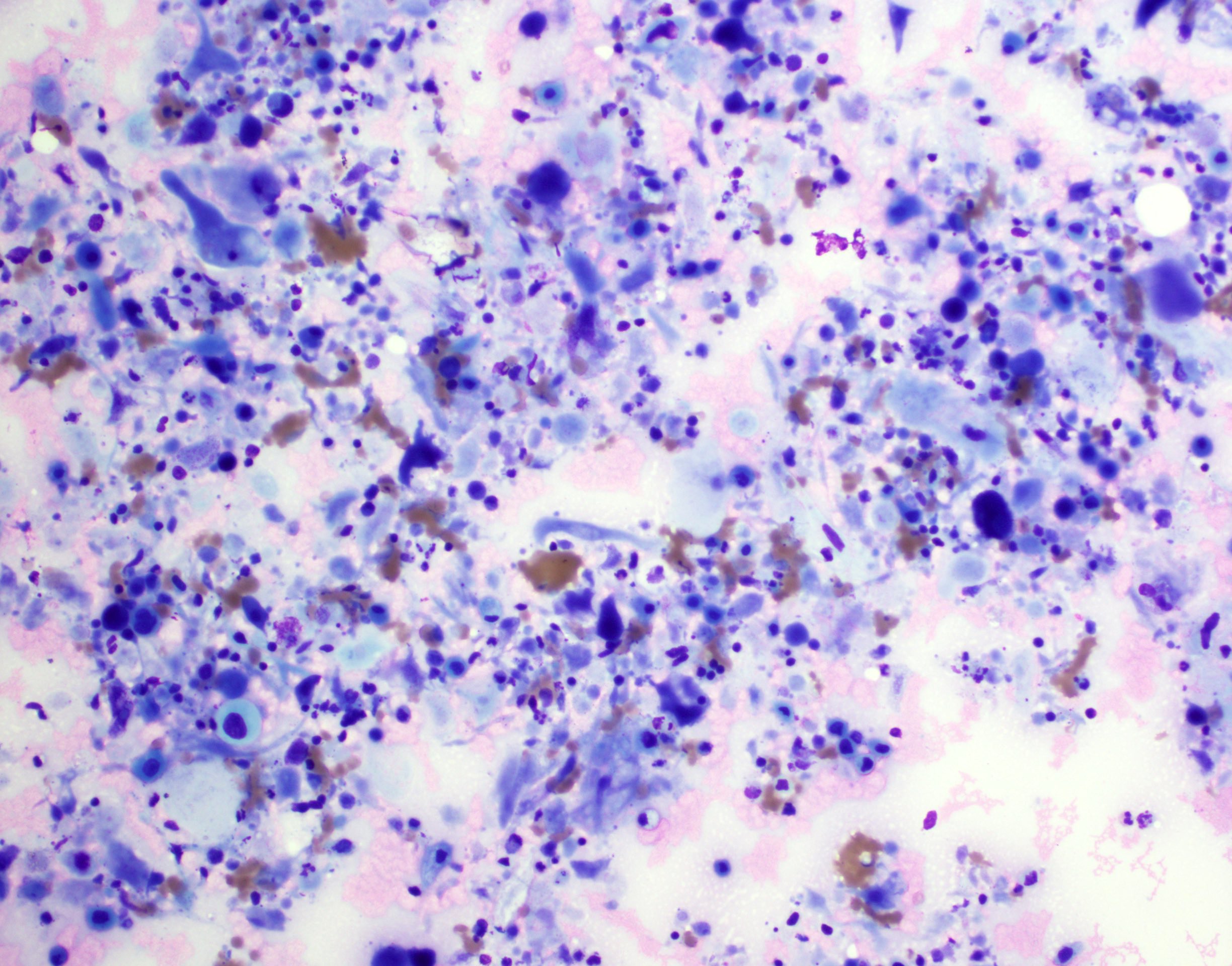
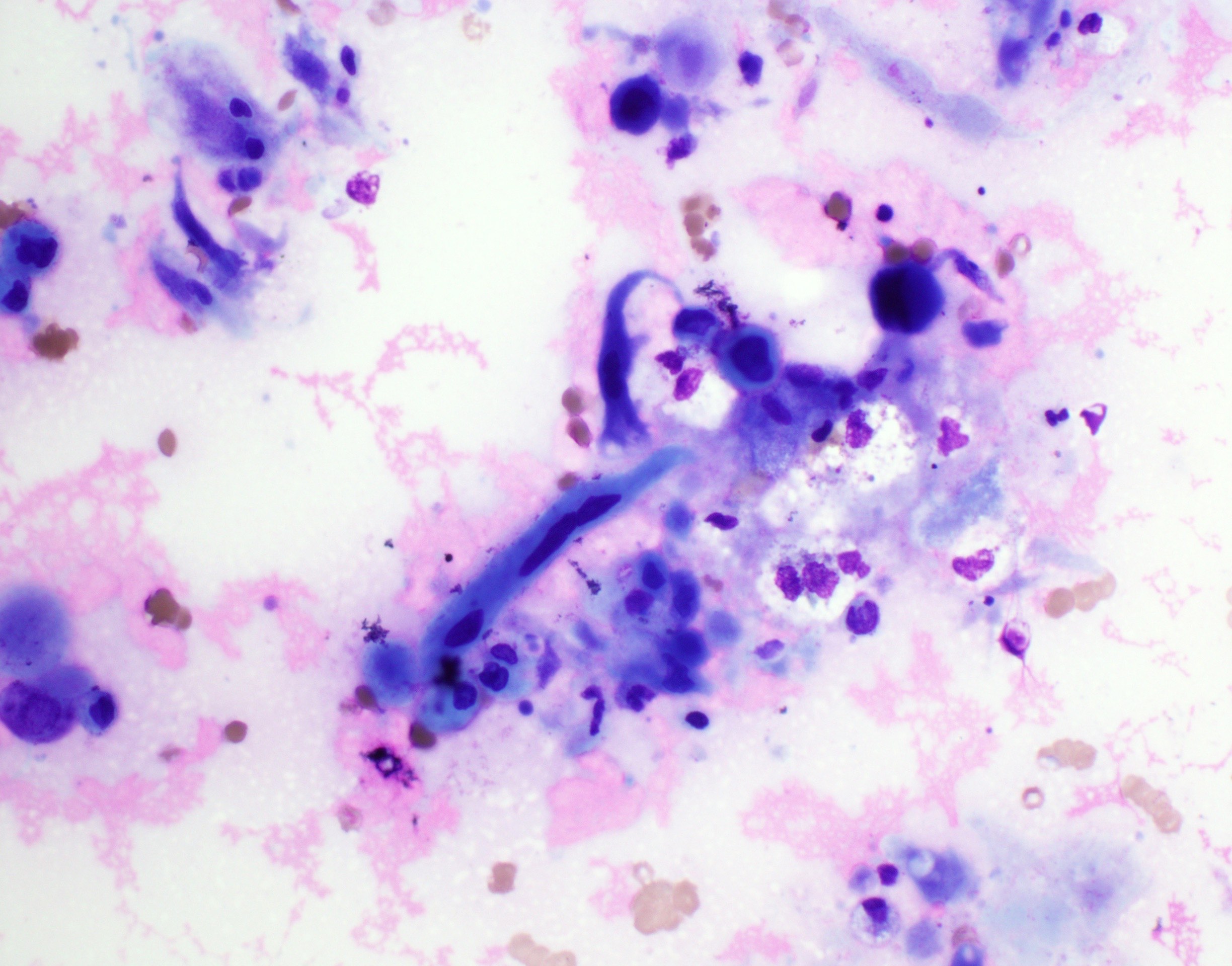
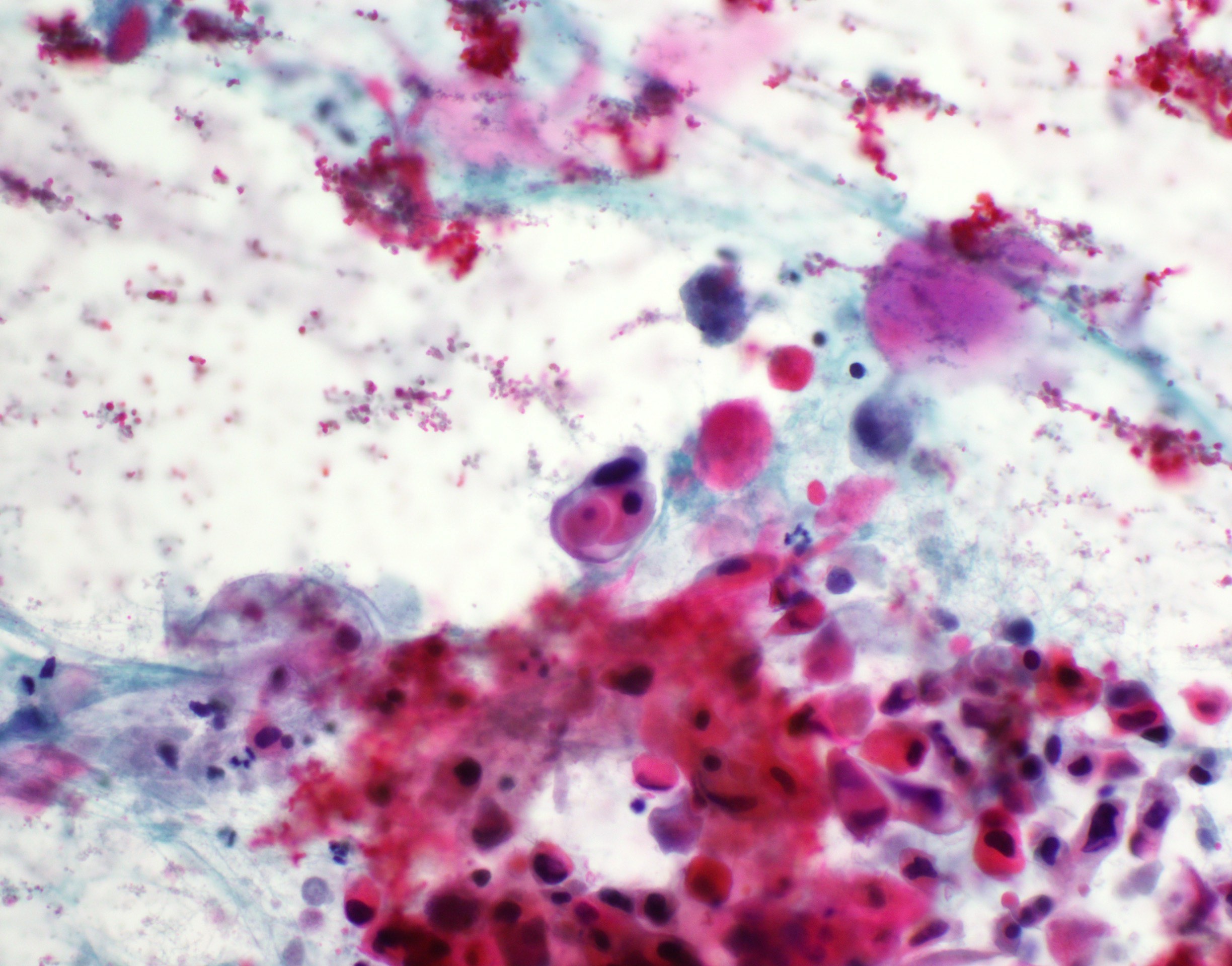
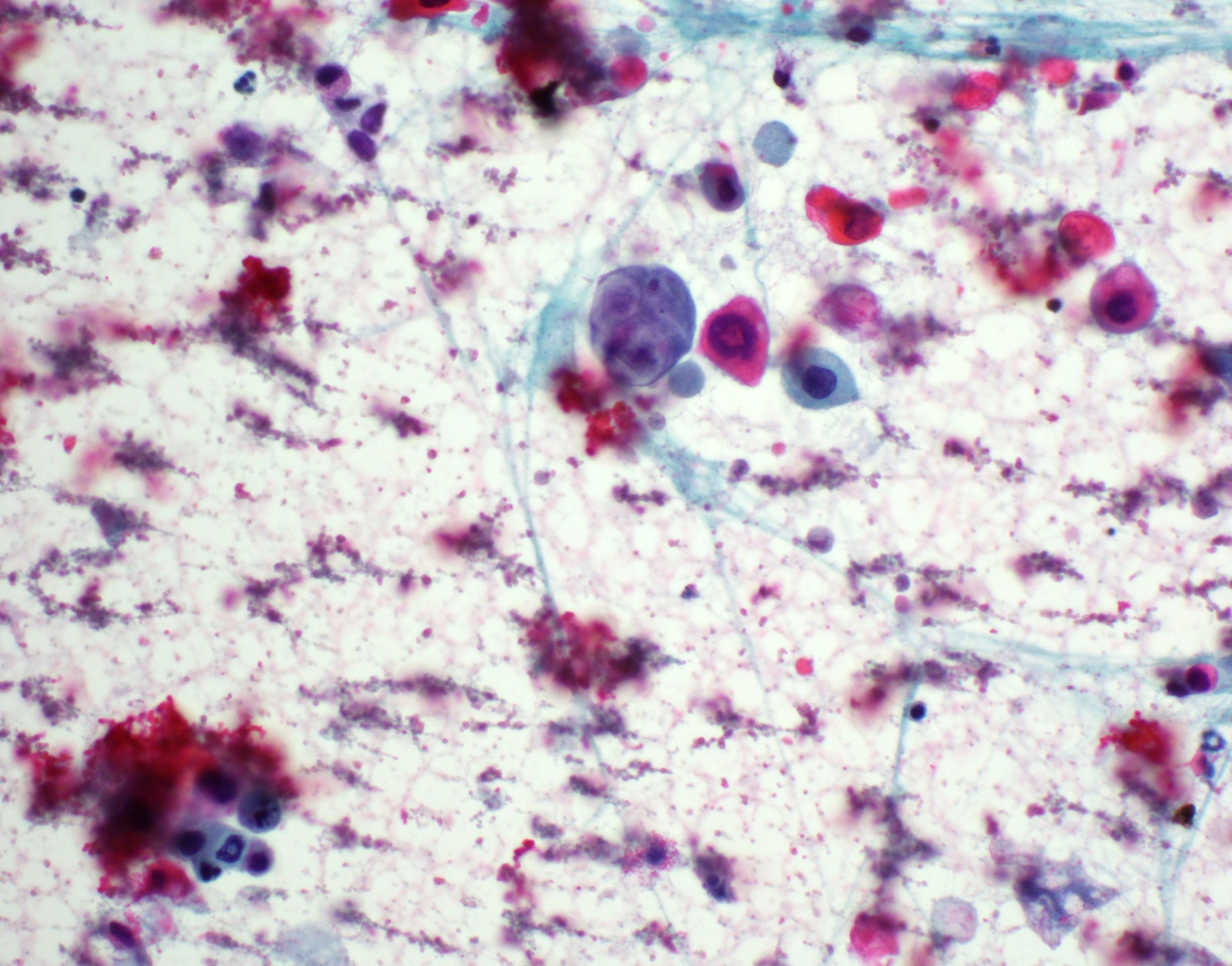
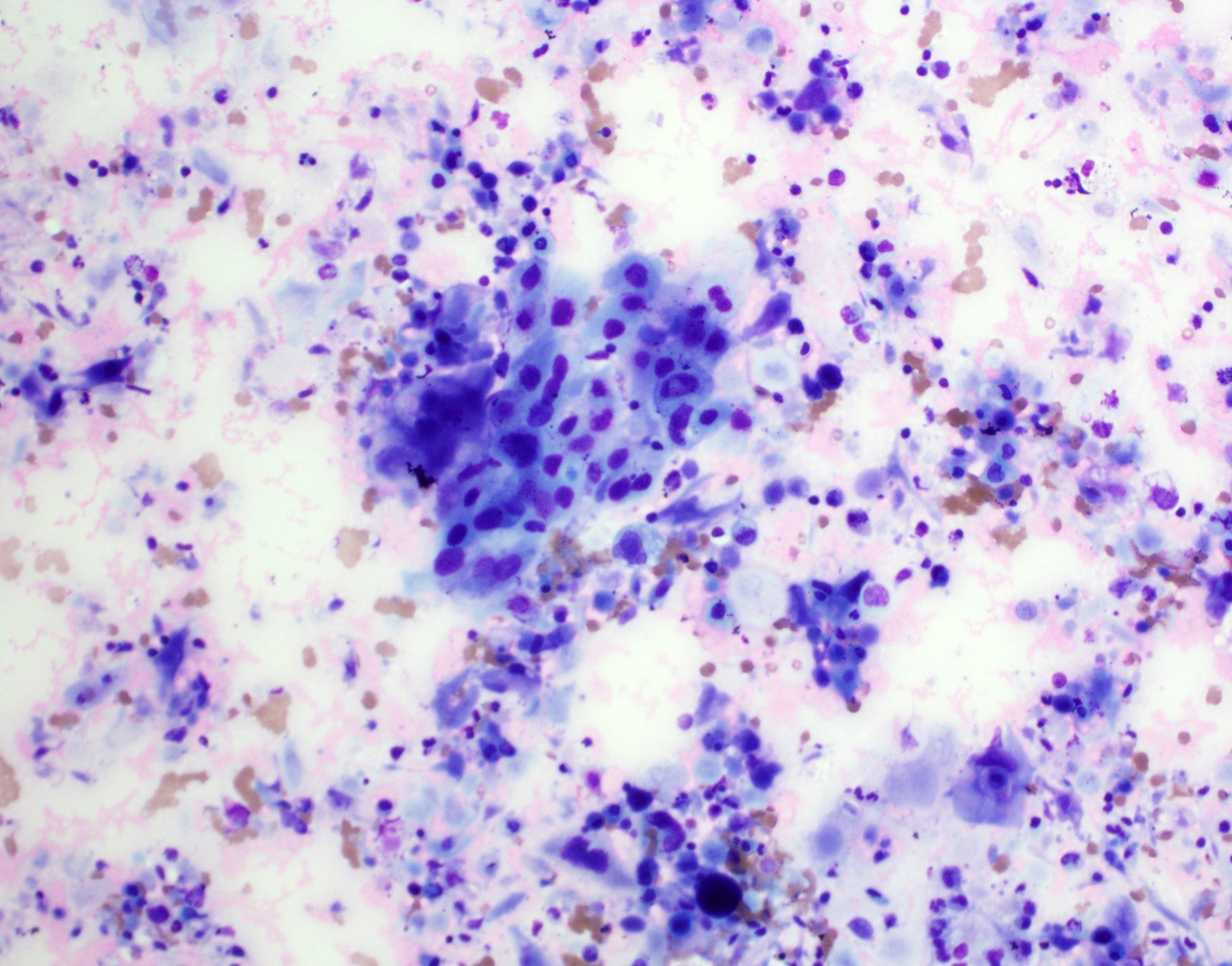
Cytology description
- Role of cytology only in investigation of regional or distant metastases
- Appearance depends on type and differentiation
- Conventional squamous cell carcinoma shows sheets and small clusters of large polygonal malignant cells with intercellular bridges and cytoplasmic or extracellular eosinophilic keratin
Cytology images
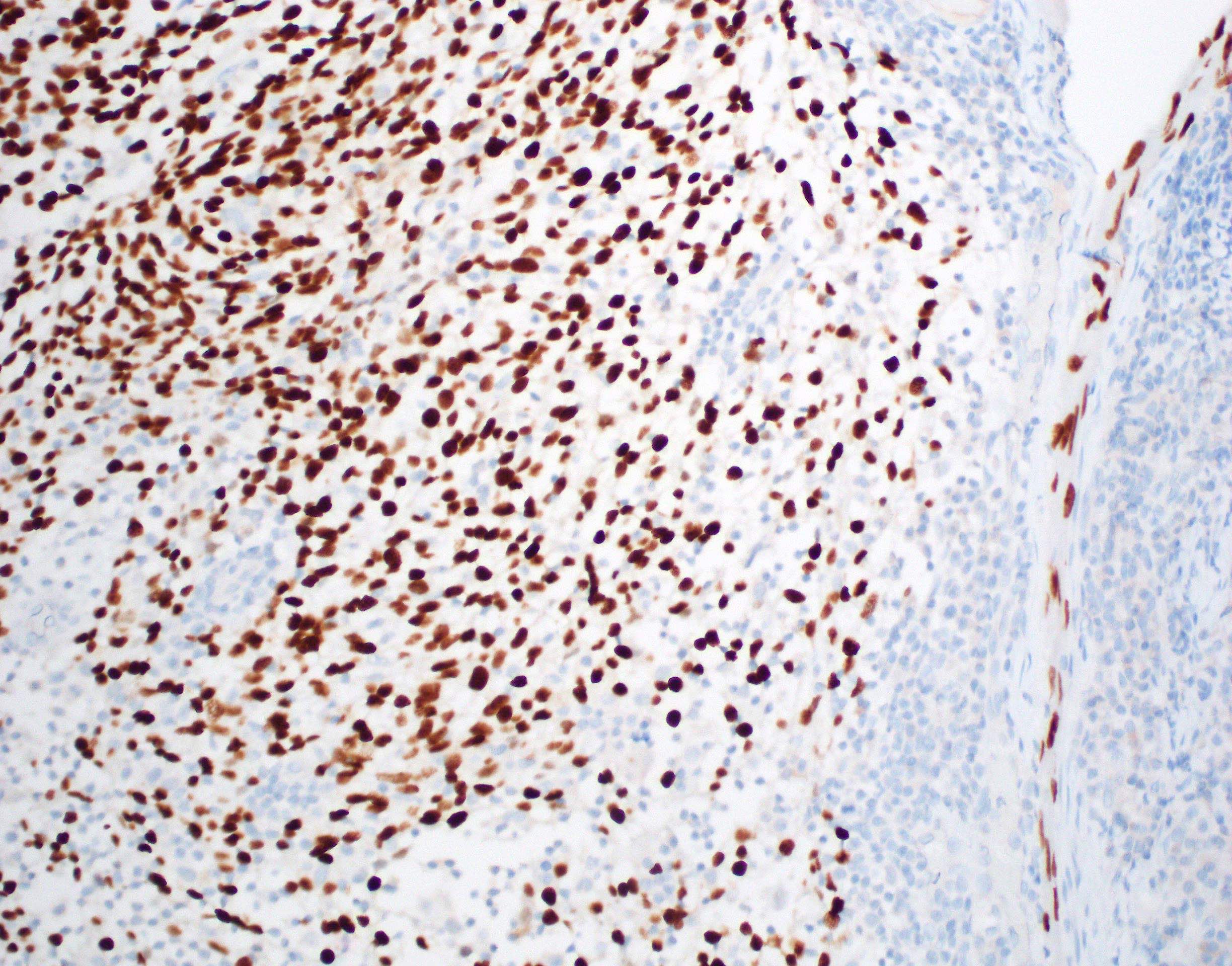
Positive stains
- Diffusely and strongly positive:
Negative stains
Molecular / cytogenetics description
- Negative for presence of high risk HPV DNA / RNA
- EBV ISH negative
Sample pathology report
- Right soft palate and uvula and bilateral neck dissection levels I - IV, excision:
- Moderately differentiated squamous cell carcinoma (T = 28 mm, pT2) arising on a background of carcinoma in situ (see comment)
- Comment: Extensive perineural involvement is present. Local excision complete, closest margin: anterior mucosal 3 mm away. Bilateral neck dissection shows 2/66 lymph nodes with metastatic squamous cell carcinoma. The larger involved node is present in the right neck, measures 25 mm and shows extranodal extension (pN3b). AJCC 8th Ed pT2pN3b group stage 4. The tumor cells lack immunostaining with p16 excluding an HPV related oropharyngeal squamous cell carcinoma. HPV negative oropharyngeal squamous cell carcinoma is frequently associated with smoking and alcohol and does not carry the good prognosis described in HPV related oropharyngeal squamous cell carcinoma.
Differential diagnosis
- HPV+ oropharyngeal squamous cell carcinoma:
- HPV related oral diseases: squamous papilloma, verruca vulgaris, condyloma acuminatum
- Usually low risk HPV+
- Nasopharyngeal carcinoma:
- Arising in the nasopharynx
- Usually EBV+
- Verrucous hyperplasia / proliferative verrucous leukoplakia:
- Exophytic growth only
- Mature keratinocytes with marked acanthosis
- Can be multifocal and widespread
- Squamous dysplasia:
- No invasive component
- Dysplastic keratinocytes with variable level of thickness involvement
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2