Search By Subspecialty:
Search By Chapter:
Number of Questions in Database: 4718
Question 1
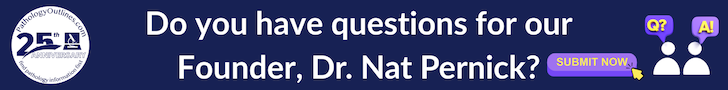
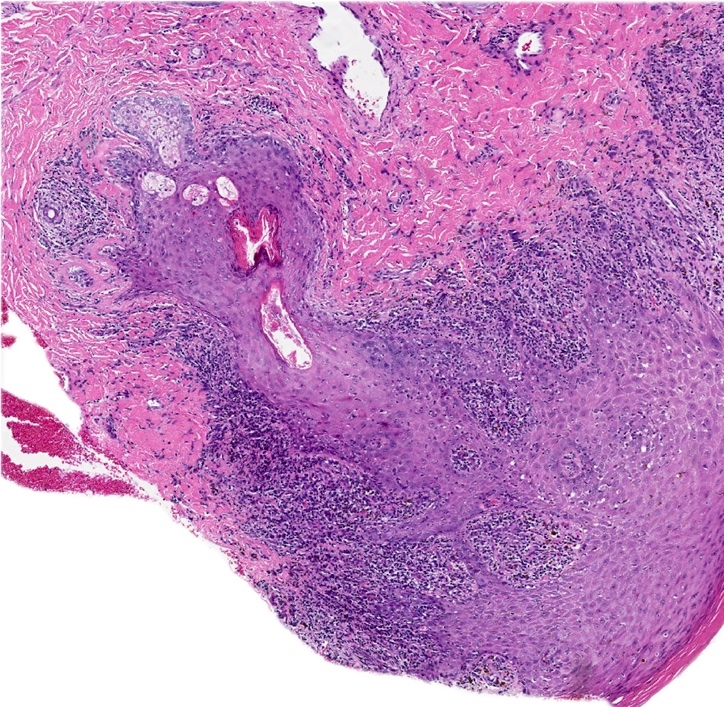
A 42 year old woman presents with a painful cystic swelling along the right posterolateral vulva, near the vaginal introitus. The cyst is excised and sent to pathology, where a benign appearing cystic lesion lined by simple cuboidal epithelium with areas of denudation and surrounding inflammation are seen. These findings, along with the image shown above, best describe which of the following vulvovaginal cysts?
- Bartholin cyst
- Epidermal inclusion cyst
- Gartner duct cyst
- Urothelial cyst
Answer 1
Question 2
Which of the following represents a physiological remnant of the mesonephric duct in adult females?
- Bartholin cyst
- Epidermal inclusion cyst
- Gartner duct cyst
- Urothelial cyst
Answer 2
Question 3
Answer 3
D. HPV6
HPV6 is a low risk HPV and is most often found in condyloma as shown in several studies. The frequency of HPV16 is lower than that of HPV6. HIV is only predisposing, not found in the epithelium. There is no association with HHV8 and HSV. (Am J Surg Pathol 2006;30:1513)
Comment Here
Reference: Condyloma
HPV6 is a low risk HPV and is most often found in condyloma as shown in several studies. The frequency of HPV16 is lower than that of HPV6. HIV is only predisposing, not found in the epithelium. There is no association with HHV8 and HSV. (Am J Surg Pathol 2006;30:1513)
Comment Here
Reference: Condyloma
Question 4
Which diagnostic test is useful to differentiate between verrucous carcinoma and a large condyloma?
- HPV IHC
- HPV ISH
- Ki67
- p16
- p53 IHC
Answer 4
B. HPV ISH
HPV ISH has high sensitivity and specificity while HPV IHC has low sensitivity. Both entities are p53 wildtype, p16 patchy / negative and have elevated Ki67 indices.
Comment Here
Reference: Condyloma
HPV ISH has high sensitivity and specificity while HPV IHC has low sensitivity. Both entities are p53 wildtype, p16 patchy / negative and have elevated Ki67 indices.
Comment Here
Reference: Condyloma
Question 5
A 31 year old woman presents with a 2 cm solid mass protruding from the vagina. A local resection is performed and shows a submucosal, well circumscribed but unencapsulated lesion composed of predominantly bland spindle cells with sparse glands and squamous metaplasia (see image shown above). Electron microscopy of the spindle cells shows abundant tonofilaments and desmosomes but no pinocytotic vesicles. Which of the following is true regarding these spindle cells?
- They are derived from mesonephric rests
- They are derived from normal myoepithelial cells found in the vagina
- They are likely keratin+, CD10+ and SMA+
- They are the malignant component of this biphasic tumor
Answer 5
C. They are likely keratin+, CD10+ and SMA+. This lesion represents a benign spindle cell epithelioma (mixed tumor of vagina). Electron microscopy of the spindle cells of this lesion shows epithelial cell features and a lack of contractile elements. A differential diagnosis of this lesion is a tubulosquamous polyp, which is thought to be derived from mesonephric rests. Myoepithelium does not normally occur in the vagina; a multipotent progenitor cell is thought to give rise to this lesion.
Comment Here
Reference: Mixed tumor of vagina
Comment Here
Reference: Mixed tumor of vagina
Question 6
A 67 year old woman was recently diagnosed with vulvar melanoma of the right labium majus. What is the most likely molecular alteration in this lesion?
- ALK fusion
- BRAF mutation
- KIT mutation
- NTRK 1/3
- PRKAR1A loss
Answer 6
C. KIT mutation. KIT mutations are more common in vulvar melanomas compared with cutaneous melanomas. Answers A and D are incorrect as ALK fusions and NTRK rearrangements are common in Spitz nevi. Answer E is incorrect as PRKAR1A loss is characteristic of pigmented epithelioid melanocytoma. Answer B is incorrect as BRAF mutations are more common in cutaneous melanomas and are only rarely encountered (< 10%) in vulvovaginal melanomas; however, nevi in genital areas, including atypical melanocytic nevi of genital type, frequently have a driver mutation in BRAF.
Comment Here
Reference: Melanoma
Comment Here
Reference: Melanoma
Question 7
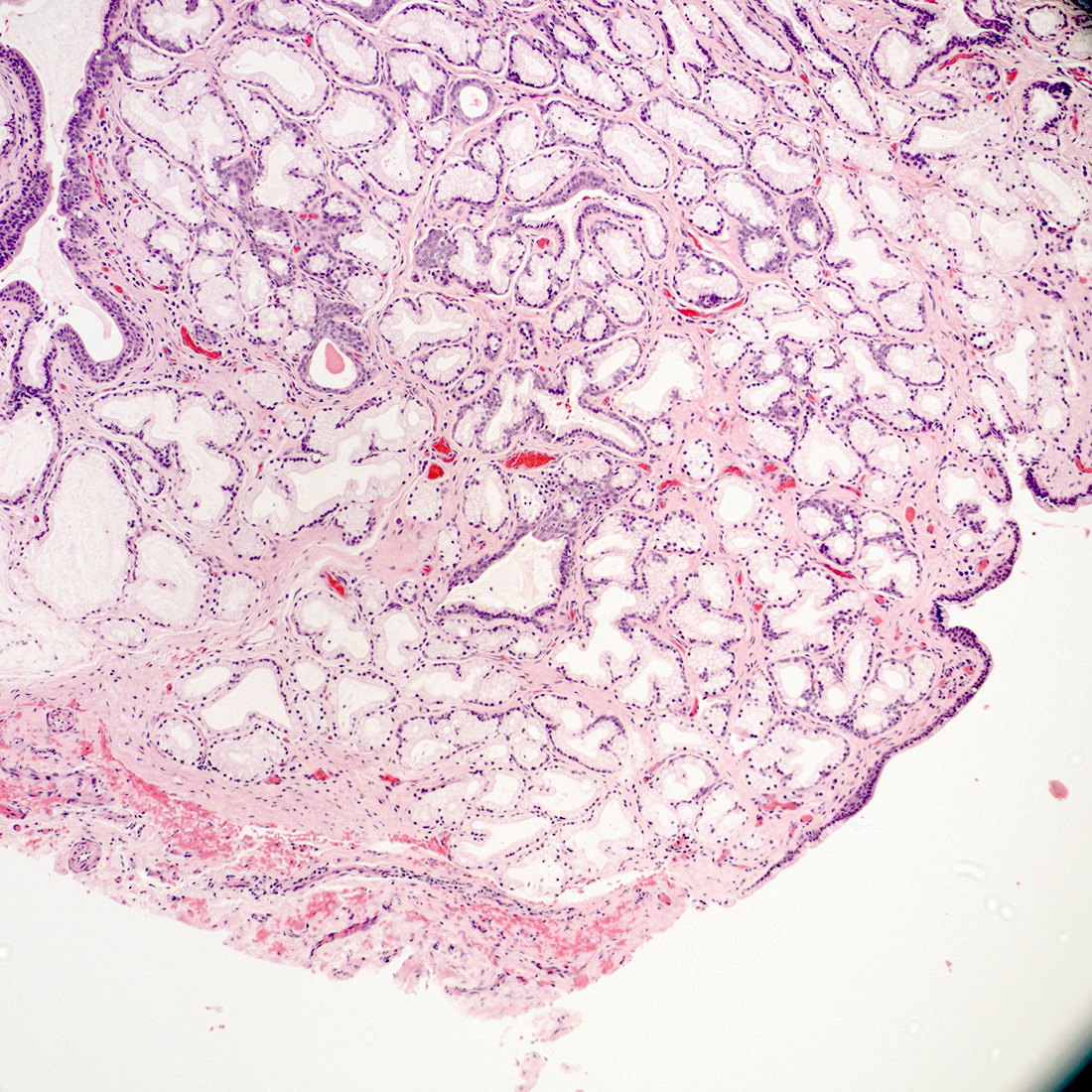
A 69 year old woman presented to the OBGYN clinic with severe pruritis. Clinical exam showed a 12 x 15 mm asymmetric, dark brown patch on the right labia minora extending into the clitoral hood. Biopsy demonstrated a broad, asymmetric, junctional melanocytic proliferation with dense lichenoid infiltrate. What is most likely to be demonstrated by the immunohistochemical stains for this patient’s lesion?
- HMB45 showing diffuse nuclear expression
- Loss of PRAME expression
- MelanA highlighting invasive melanoma cells
- p16 demonstrating strong nuclear expression
- SOX10 highlighting increased number of melanocytes with focal pagetoid spread
Answer 7
E. SOX10 highlighting increased number of melanocytes with focal pagetoid spread. The histologic features are consistent with melanoma in situ, lentiginous growth pattern. SOX10 and MelanA will highlight increased melanocytes and pagetoid growth in melanoma. Answer C is incorrect as there is no evidence of invasive melanoma on H&E section. Answers A, B and D are incorrect as HMB45 is a cytoplasmic stain, PRAME is usually diffusely positive in melanoma and p16 typically demonstrates loss of nuclear expression in melanoma.
Comment Here
Reference: Melanoma
Comment Here
Reference: Melanoma
Question 8
Answer 8
E. TP53 is most frequently mutated and probably most relevant for pathogenesis. Answer A is incorrect because it is not mutated. Answer B is incorrect because it is infrequently amplified. Answer C is incorrect because it is frequently mutated but probably not the most relevant. Answer D is incorrect because it is frequently mutated but mostly in HPV associated lesions.
Comment Here
Reference: HPV independent VIN-vulva
Comment Here
Reference: HPV independent VIN-vulva
Question 9
Which immunohistochemical stain shows an aberrant pattern in differentiated vulvar intraepithelial neoplasia?
- CK18
- Ki67
- p16
- p53
- SOX10
Answer 9
D. p53 frequently shows a mutation type aberrant staining pattern. Answer A is incorrect because CK18 is not overexpressed in differentiated vulvar intraepithelial neoplasia (dVIN), differentiated exophytic vulvar intraepithelial lesion (DEVIL) or vulvar acanthosis with altered differentiation (VAAD). Answer B is incorrect because Ki67 shows only a variable growth fraction as in many other lesions. Answer C is incorrect because p16 is overexpressed in HPV associated VIN. Answer E is incorrect because it is not aberrantly expressed in dVIN.
Comment Here
Reference: HPV independent VIN-vulva
Comment Here
Reference: HPV independent VIN-vulva
Question 10
Answer 10
D. p16. IHC for p16 shows highest specificity and sensitivity for HPV association. Answers A, B, C and E are incorrect because they are not relevant for verification of HPV association.
Comment Here
Reference: HPV associated squamous cell carcinoma-vulva
Comment Here
Reference: HPV associated squamous cell carcinoma-vulva
Question 11
International Federation of Gynecology and Obstetrics (FIGO) and Union for International Cancer Control (UICC) have decided to use different instructions for measurement of infiltration depth in vulvar carcinomas. Which histomorphological structure is important for the measurement of tumor infiltration depth according UICC?
- Basal cell layer
- Dermal papilla
- Rete ridge
- Surface epidermis
- Tumor surface
Answer 11
B. Dermal papilla. According to UICC, the infiltration depth of vulvar carcinomas should be measured from the top of the nearest dermal papilla to the deepest tumor cell infiltrate. Answer A is incorrect because VIN plays no role in this relation. Answer D is incorrect because the epidermial surface is not relevant for infiltration depth. Answer C is incorrect because rete ridges are important for FIGO staging. Answer E is incorrect because tumor surface is relevant for the measurement of tumor thickness.
Comment Here
Reference: HPV associated squamous cell carcinoma-vulva
Comment Here
Reference: HPV associated squamous cell carcinoma-vulva
Question 12
Answer 12
C. p16 + p53. Simultaneous block-like staining of p16 and a wild type p53 pattern is both sensitive and specific for HPV associated high grade SIL.
Answer A is incorrect because the CK17 staining lacks specificity.
Answer B is incorrect because Ki67 staining is not specific.
Answer E is incorrect because the p53 pattern in basal sparing pattern is inconsistent and the p53 wild type pattern can be found in certain variants of HPV independent vulvar intraepithelial neoplasia.
Answer C is incorrect because, although rare, block-like p16 positivity can occasionally be seen in dVIN as well.
Comment Here
Reference: HPV associated SIL
Comment Here
Reference: HPV associated SIL
Question 13
Answer 13
C. HPV RNA ISH is a sensitive method for visualization of HPV in low risk lesions. Answer A is incorrect because CK17 IHC is not specific for HPV related lesions. Answer B is incorrect because HPV IHC is specific but the sensitivity for HPV is very low. Answer D is incorrect because p16 IHC is mostly negative in low risk HPV types. Answer E is incorrect because p53 typically shows a wild type (nonspecific) expression pattern in seborrheic keratosis and does not aid in determining HPV association.
Comment Here
Reference: HPV associated SIL
Comment Here
Reference: HPV associated SIL
Question 14
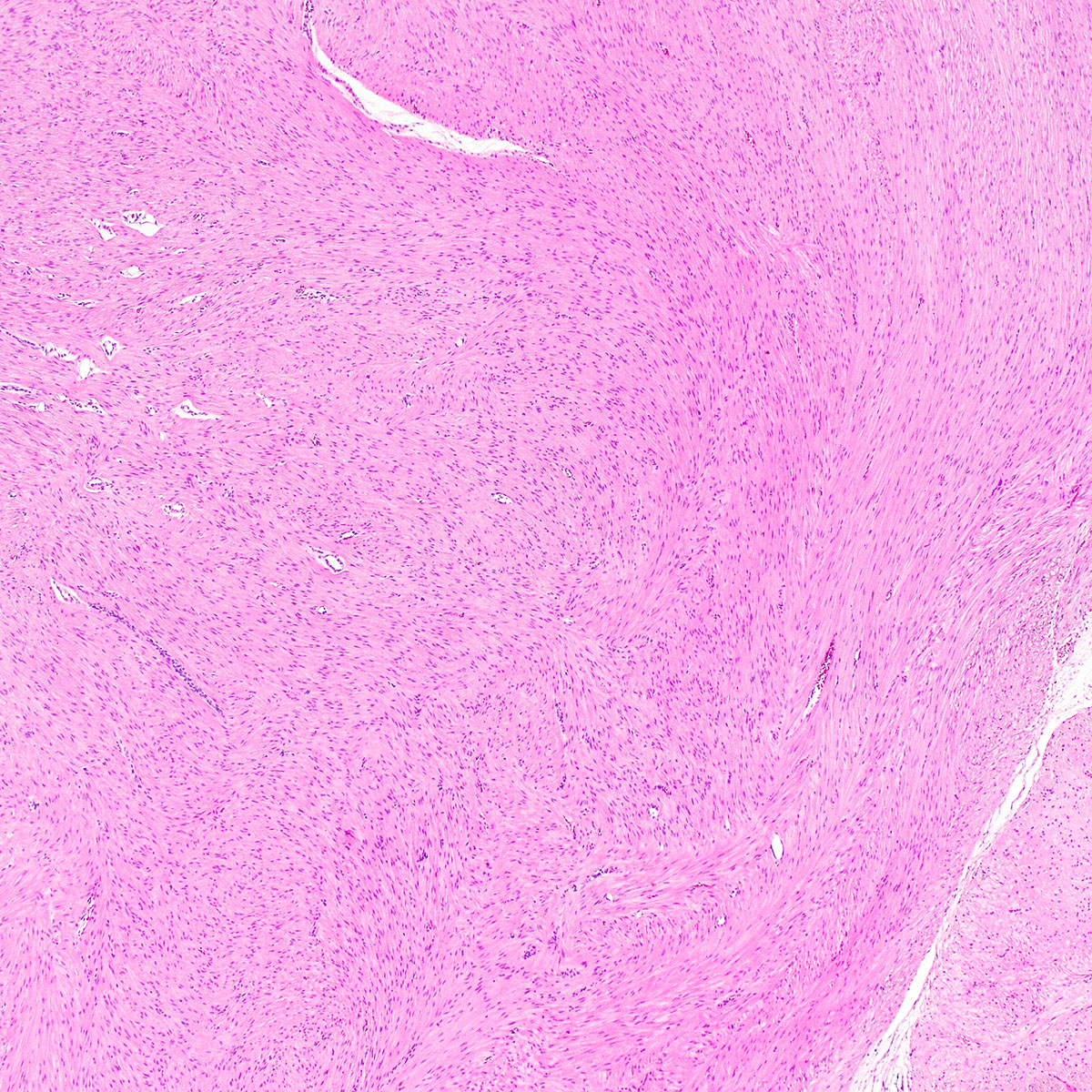
A 48 year old woman presented with a painless 3.5 cm vulvar mass, which had been slowly growing for 18 months. She underwent complete local excision of a rubbery, well circumscribed mass. A representative photomicrograph is shown. Which of the following is true about this lesion?
- Complete local excision is considered curative
- Immunohistochemistry for estrogen receptor and progesterone receptor is typically negative
- Nuclear pleomorphism is associated with an increased risk of distant metastasis
- Rb protein is typically overexpressed
- This lesion occurs exclusively in women
Answer 14
A. Complete local excision is considered curative. This is a cellular angiofibroma.
Comment Here
Reference: Cellular angiofibroma
Comment Here
Reference: Cellular angiofibroma
Question 15
Answer 15
Question 16
A 28 year old woman presents with persistent vaginal discharge and is found to have submucosal mucinous glands on a vaginal biopsy. What is the most likely scenario?
- Maternal grandmother's use of diethylstilbestrol (DES) caused in utero exposure for the patient’s mother
- Maternal use of DES caused in utero exposure for the patient
- The patient had prior treatment for bacterial vaginosis
- The patient had prior treatment for vaginal condyloma acuminata
- Use of DES by the patient
Answer 16
D. The patient had prior treatment for vaginal condyloma acuminata. Vaginal application of 5-fluoruracil and vaginal CO2 laser therapy (common treatments for condyloma acuminata) are 2 known non-DES causes for vaginal adenosis. Answer C is incorrect because these are not common treatments for bacterial vaginosis. Answers A, B and E are incorrect because in utero exposure to diethylstilbestrol (DES) was the most common cause of vaginal adenosis for women born in the middle of the 20th century but DES exposure is not a concern in this patient who was born long after its discontinued use.
Comment Here
Reference: Vaginal adenosis
Comment Here
Reference: Vaginal adenosis
Question 17
Which statement concerning vaginal adenosis is true?
- Inapparent on gross examination
- May be associated with microglandular hyperplasia
- Progresses to adenocarcinoma in a majority of the cases
- Usually manifests in prepubertal age
- Usually related to bacterial vaginosis
Answer 17
B. May be associated with microglandular hyperplasia. Vaginal adenosis commonly appears as red nodules / red granular spots or patches and fails to stain with an iodine solution on colposcopy. Mosaicism and punctation are common findings during colposcopy. It commonly manifests as excessive mucous discharge in postpubertal age. Vaginal adenosis seldom progresses to cancer. Microglandular hyperplasia develops in foci of vaginal adenosis, especially after oral contraceptive use. Microglandular hyperplasia may be confused with clear cell adenocarcinoma (which is also diethylstilbestrol associated).
Comment Here
Reference: Vaginal adenosis
Comment Here
Reference: Vaginal adenosis
Question 18
Answer 18
Question 19
There is an association between lichen sclerosus of the vulva and
- High grade squamous intraepithelial lesion (HSIL / VIN3)
- Human papillomavirus (HPV) independent vulvar intraepithelial neoplasia (VIN)
- Lichen planus
- Psoriasis
Answer 19
B. Human papillomavirus (HPV) independent vulvar intraepithelial neoplasia (VIN)
Comment Here
Reference: Lichen sclerosus
Comment Here
Reference: Lichen sclerosus
Question 20
A 63 year old woman previously diagnosed with lichen planus returns to the clinic with a persistent, well demarcated plaque and suboptimal treatment response. A biopsy shows lichenoid inflammation with minimal basal atypia. What result or clinical information would favor reactive process over neoplastic process?
- Complete loss of p53
- Diffuse, block-like expression of p16
- Prior history of HPV independent squamous cell carcinoma
- Wild type p53 expression
Answer 20
D. Wild type p53 expression. Wild type p53 expression pattern supports the diagnosis of lichen planus, although aberrant expression can be seen in the basal cells of regenerative erosive lichen planus. Answer A is incorrect because the complete loss of p53 constitutes aberrant expression and would be concerning for differentiated vulvar intraepithelial neoplasia. Answer B is incorrect because diffuse block-like expression of p16 is characteristic in HPV associated with a high grade squamous intraepithelial lesion. Answer C is incorrect because prior history of HPV independent squamous cell carcinoma increases a pretest probability in a 63 year old woman with a persistent vulvar plaque and suboptimal treatment response.
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus
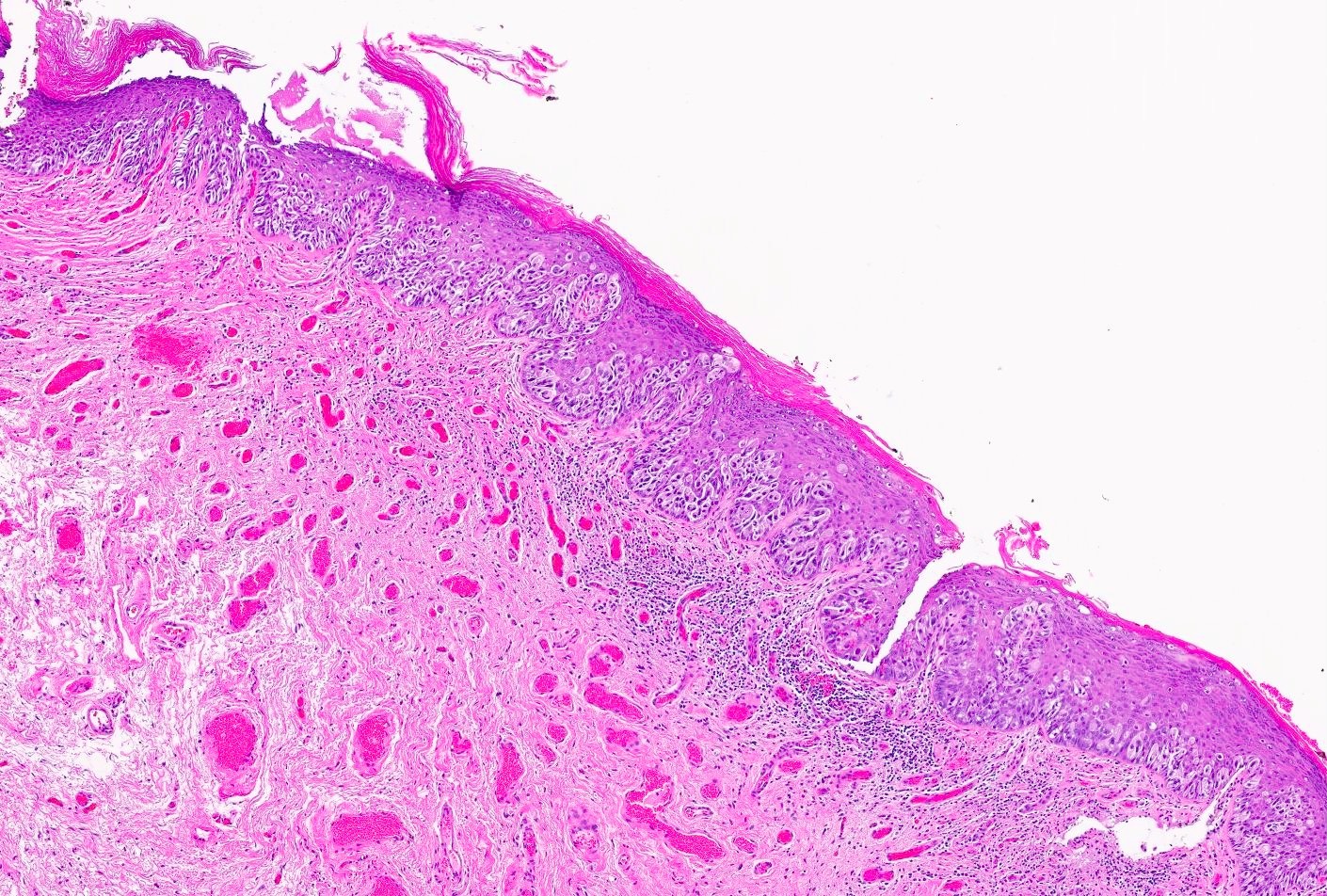
Question 21
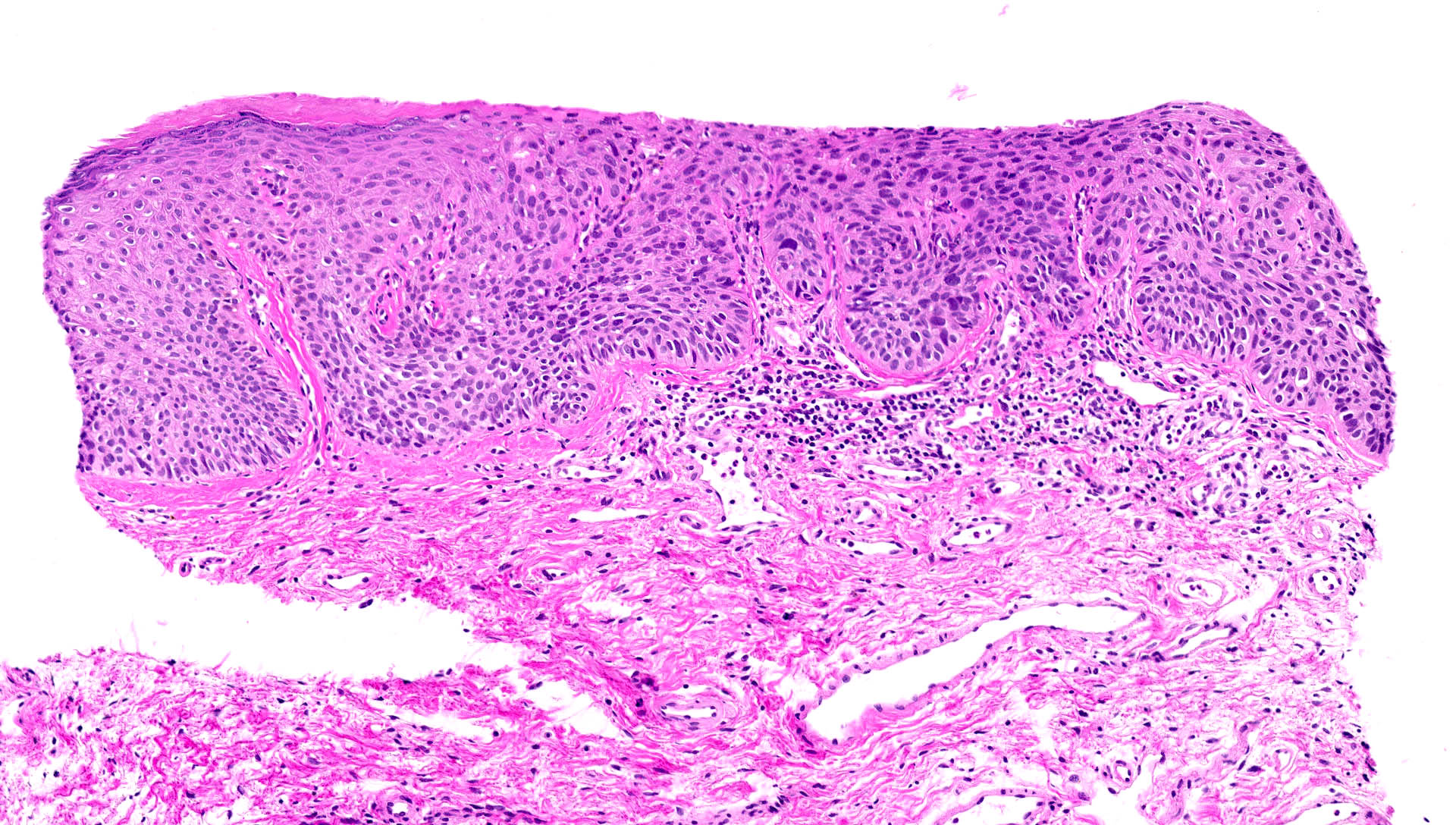
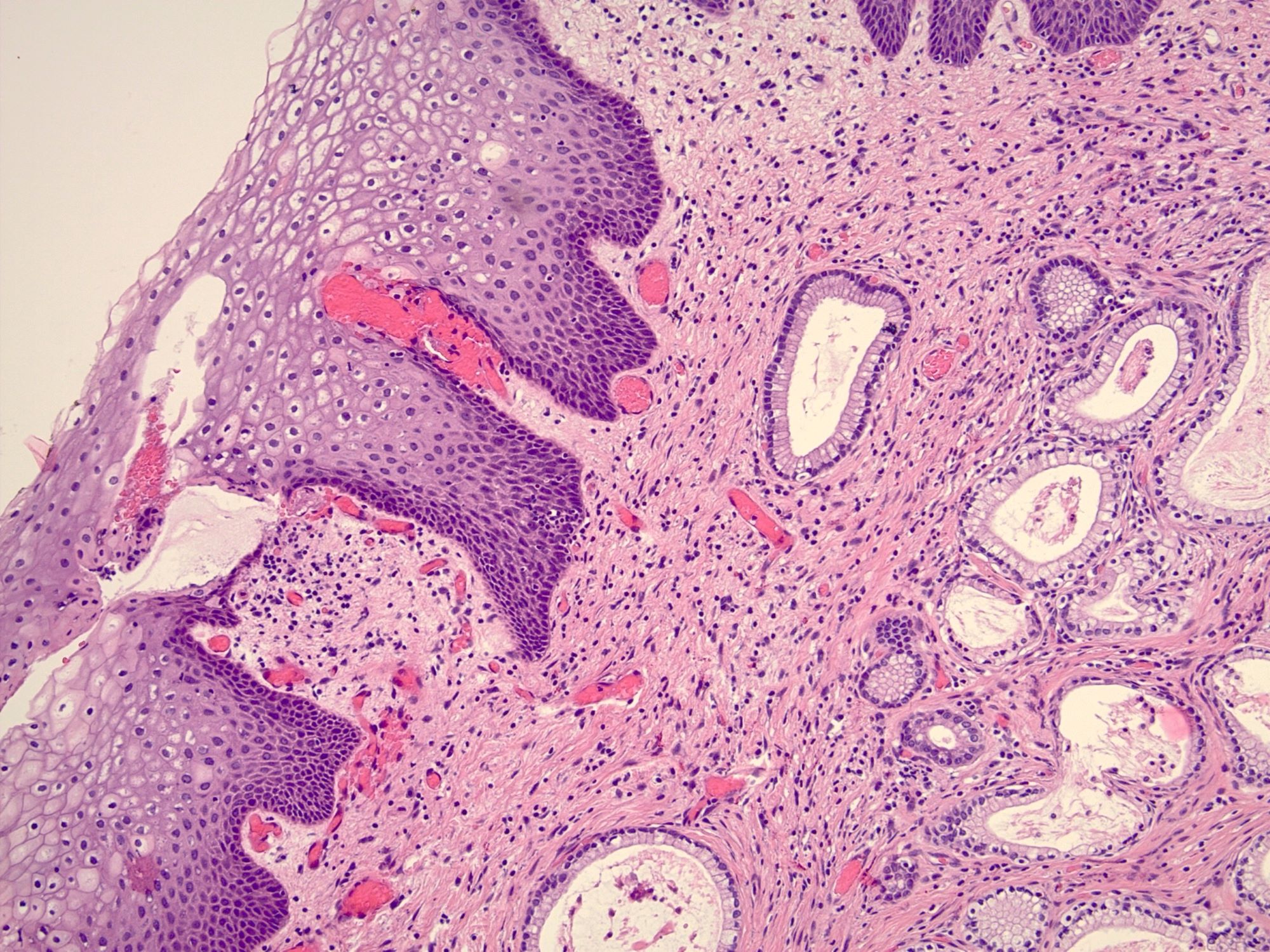
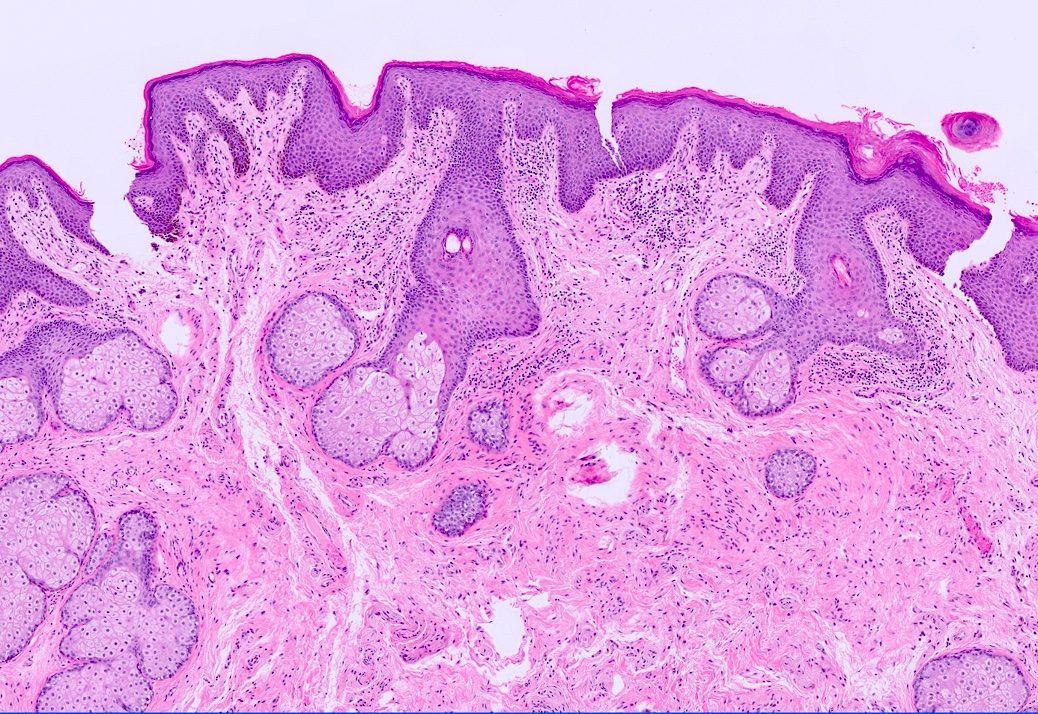
A 45 year old woman with a past medical history of hypothyroidism presents to the clinic with pain and burning discomfort in the vulvar area. On physical examination, a well delineated red plaque in the vaginal introitus is observed extending onto the labia majora. There is no scarring or obvious vaginal inflammation. A punch biopsy was obtained. PASF shows no fungal elements. Based on the microphotograph above and clinical information provided, what is the most likely diagnosis?
- Fixed drug reaction
- High grade squamous intraepithelial lesion (HSIL)
- Syphilis
- Vulvar hypertrophic lichen planus
Answer 21
D. Vulvar hypertrophic lichen planus. The patient presented with a circumferential red plaque over the hairless and hair bearing skin of the vulva. The microphotograph shows marked acanthosis with deep and irregular rete ridges, hypergranulosis and dense, band-like lymphocytic infiltrate in the superficial dermis, with apoptotic bodies squamatization and superficial perivascular inflammation. Taken together with the clinical presentation, the findings are consistent with vulvar hypertrophic lichen planus. Answer A is incorrect because although it is important to evaluate medication history, there are no conspicuous eosinophils in the epidermis and superficial dermis, which makes a fixed drug reaction less likely. Answer B is incorrect because high grade squamous intraepithelial lesion can be ruled out based on the absence of full thickness epithelial atypia and increased suprabasal mitotic activity. Answer C is incorrect because syphilis is typically associated with minimal dyskeratosis and neutrophilic infiltrate in the early stages and granulomatous inflammation later in the disease, usually with deep perivascular inflammation.
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus
Question 22
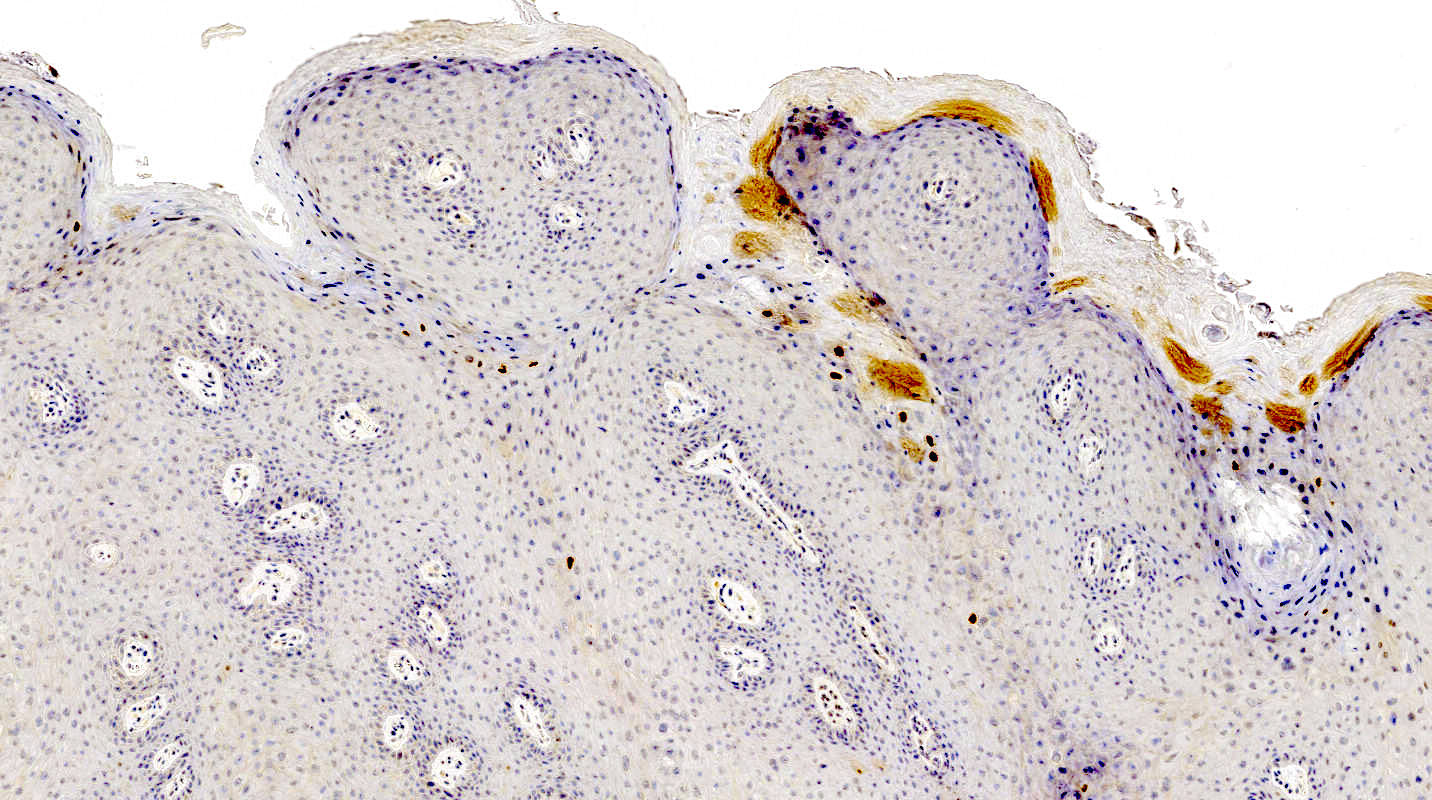
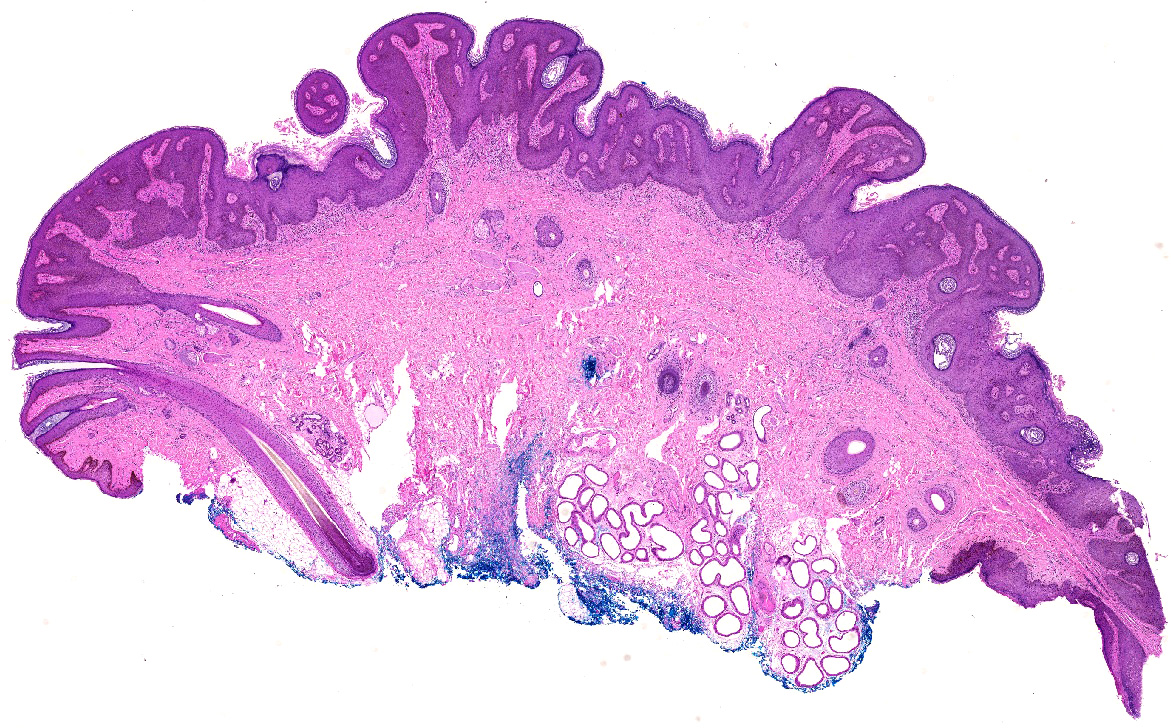
A 36 year old woman undergoes excision of a 3 cm, slow growing, painless vulvar mass. The lesion is well circumscribed and microscopic examination reveals no nuclear atypia, necrosis or mitotic activity. A representative photomicrograph is shown above. Immunostains for smooth muscle actin, desmin and caldesmon are positive. Which of the following statements is true regarding the depicted tumor?
- Approximately 50% recur after simple local excision
- CD34 immunohistochemistry is positive in > 90% of cases
- Estrogen and progesterone receptor are expressed in < 10%
- Plexiform architecture merits a malignant diagnosis
- This is the most common vulvar mesenchymal neoplasm
Answer 22
E. Leiomyoma is the most common mesenchymal neoplasm of the vulva.
Comment Here
Reference: Smooth muscle tumors
Comment Here
Reference: Smooth muscle tumors
Question 23
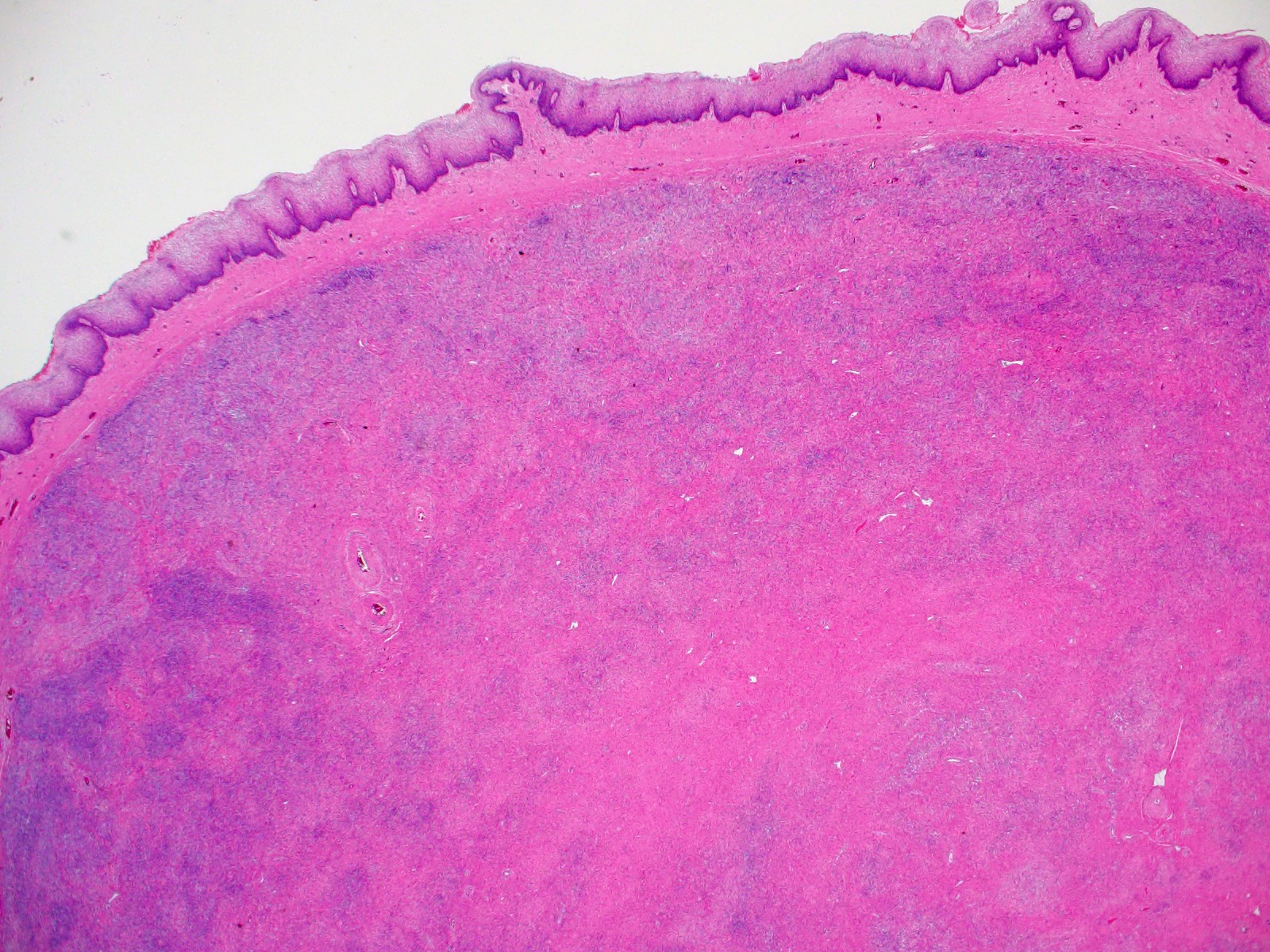
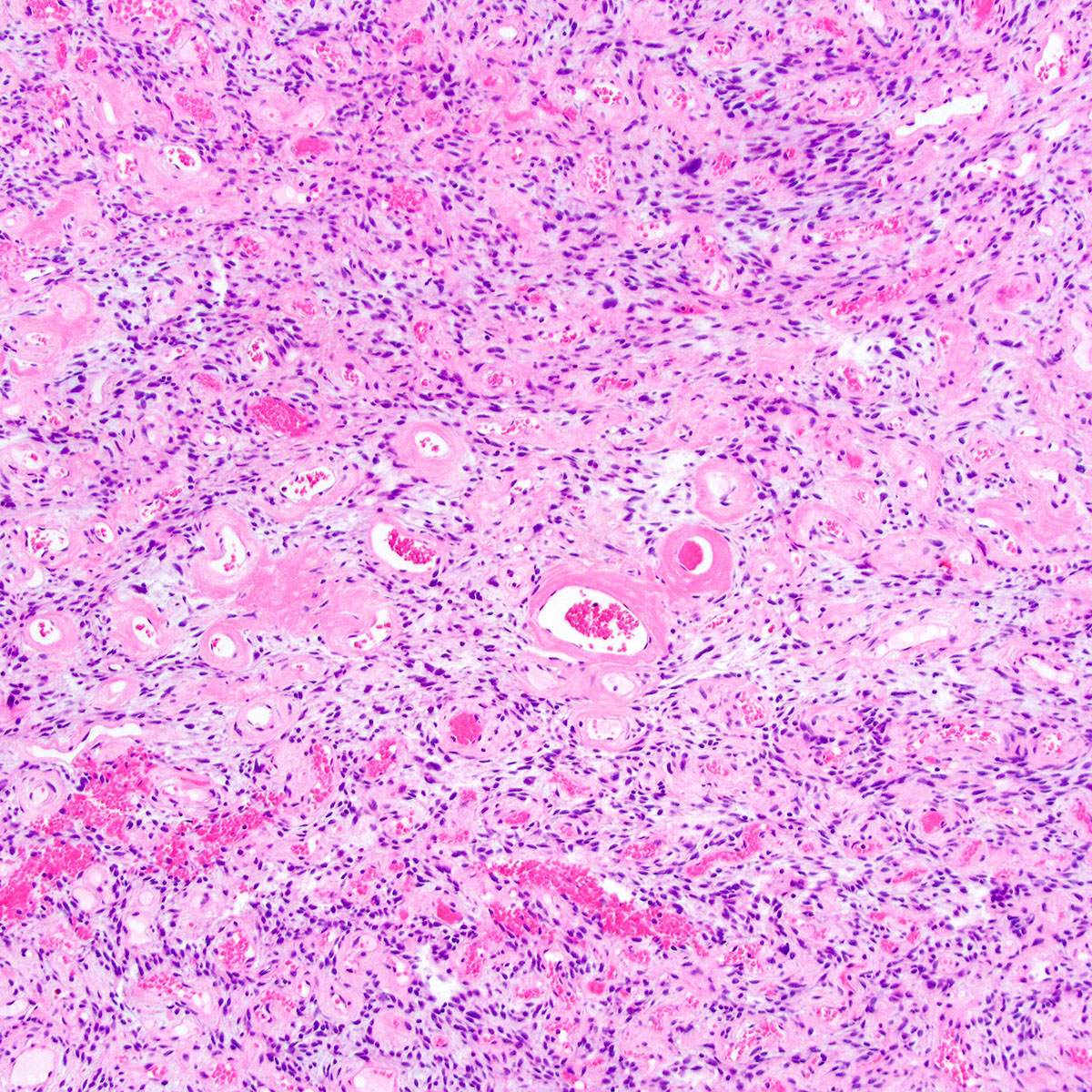
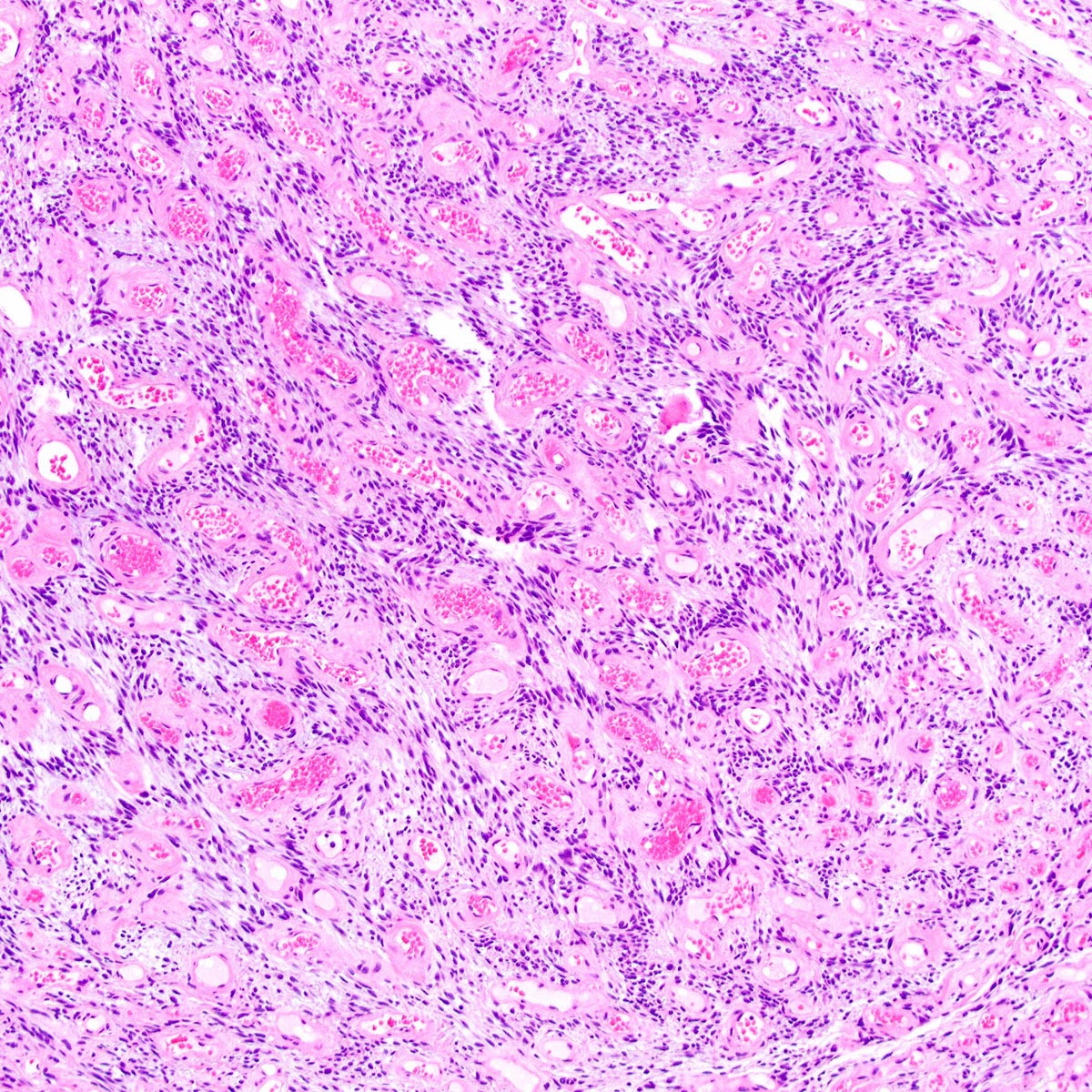
A 60 year old woman presents with vaginal bleeding and is found to have a 7 cm prolapsing mass. A preoperative MRI shows infiltration of the rectovaginal septum. A core biopsy is obtained, showing atypical spindle cells with brisk mitoses (up to 12 per 10 high power fields) and coagulative necrosis. A representative photomicrograph is shown above. Immunostains for desmin and caldesmon are positive. Which of the following statements is true regarding the depicted tumor?
- Local recurrence or distant metastasis occur in > 50%
- Most are grossly and microscopically well circumscribed
- Most cases show predominantly epithelioid morphology
- MyoD1 immunohistochemistry is strongly and diffusely positive
- Positive surgical margins are not associated with increased risk of local recurrence
Answer 23
A. Primary vulvovaginal leiomyosarcoma is associated with > 50% risk of local recurrence or distant metastasis.
Comment Here
Reference: Smooth muscle tumors
Comment Here
Reference: Smooth muscle tumors
Question 24
What are the most helpful auxiliary analysis methods for categorization of vulvar carcinomas in HPV associated and HPV independent carcinomas?
- HPV immunohistochemistry
- HPV RNA in situ hybridization
- p16 immunohistochemistry
- p16 and p53 immunohistochemistry
- TP53 next generation sequencing
Answer 24
D. p16 and p53 immunohistochemistry (IHC). Combined IHC for p16 and p53 shows the highest specificity and sensitivity for HPV association. Answer B is incorrect because the sensitivity of HPV RNA in situ hybridization is lower than p16 IHC. Answer C is incorrect because there are rare vulvar carcinomas with p16 overexpression without HPV association and these can be recognized because they show mutant pattern p53 expression. Answer E is incorrect because rare HPV associated vulvar carcinomas harbor TP53 mutations. Answer A is incorrect because the sensitivity for verification of HPV association is very low.
Comment Here
Reference: HPV independent squamous cell carcinoma-vulva
Comment Here
Reference: HPV independent squamous cell carcinoma-vulva
Question 25
Answer 25
A. Basal mutation type. There is a strong basal overexpression of p53. Answer B is incorrect because the p53 staining pattern is not diffuse. Answer D is incorrect because p53 is overexpressed. Answer E is incorrect answer because the p53 expression is not heterogeneous. Answer C is incorrect because p53 expression is never membranous.
Comment Here
Reference: HPV independent squamous cell carcinoma-vulva
Comment Here
Reference: HPV independent squamous cell carcinoma-vulva
Question 26
A 28 year old woman presented to the clinic with a 0.6 cm, flat, dark brown lesion with an irregular border on the labia majora. The histologic findings of the shave biopsy demonstrated a relatively symmetric, broad melanocytic proliferation with large oval nests with retraction perpendicular to the dermal epidermal junction, focal fusion and mild cytologic atypia. Dermal maturation is evident. What is the most likely molecular alteration in this lesion?
- ALK fusion
- BRAF mutation
- Homozygous deletion of CDKN2A
- PTEN mutation
Answer 26
B. BRAF mutation. The majority of atypical melanocytic nevi of genital type (AMNGT) have a driver mutation in BRAF. Answer A incorrect because ALK fusion is more characteristic of Spitz nevi. Answers C and D are incorrect because those alterations are specific to superficial spreading melanoma.
Comment Here
Reference: Atypical melanocytic nevi of genital type-vulva
Comment Here
Reference: Atypical melanocytic nevi of genital type-vulva
Question 27
A 16 year old girl presented with her parents to the OBGYN clinic with an irregular, dome shaped, dark pigmented papule on the mons pubis. A biopsy demonstrated large, ill defined nests with focal retraction. What is the most likely interpretation of the immunohistochemical stains for this patient's lesion?
- Diffuse expression of PRAME
- Gradient pattern of HMB45
- High Ki67 proliferation index in the dermal component
- SOX10 highlighting pagetoid and extensive lentiginous growth
Answer 27
B. Gradient pattern of HMB45. The histologic features are consistent with atypical melanocytic nevi of genital type (AMNGT). Although HMB45 expression varies in nevi, the stain can be useful to highlight the maturation (zonation) pattern (diminished or loss of expression from epidermal to dermal component). Answers A, C and D are incorrect because PRAME is usually diffusely positive in melanoma, SOX10 helps to highlight the increase of melanocytes and pagetoid growth in melanoma and Ki67 is expected to be low in the dermal component of genital nevi.
Comment Here
Reference: Atypical melanocytic nevi of genital type-vulva
Comment Here
Reference: Atypical melanocytic nevi of genital type-vulva
Question 28
Which HPV subtype is the most common driver of VAIN 2 - 3 / vaginal high grade squamous intraepithelial lesion (HSIL)?
- HPV 16
- HPV 18
- HPV 31
- HPV 33
- HPV 35
Answer 28
A. HPV 16 is the most common high risk HPV subtype associated with VAIN 2 - 3 / HSIL. Answers B, C, D and E are incorrect because although they are all high risk HPV subtypes, they are less common.
Comment Here
Reference: Vaginal intraepithelial neoplasia (VAIN)
Comment Here
Reference: Vaginal intraepithelial neoplasia (VAIN)
Question 29
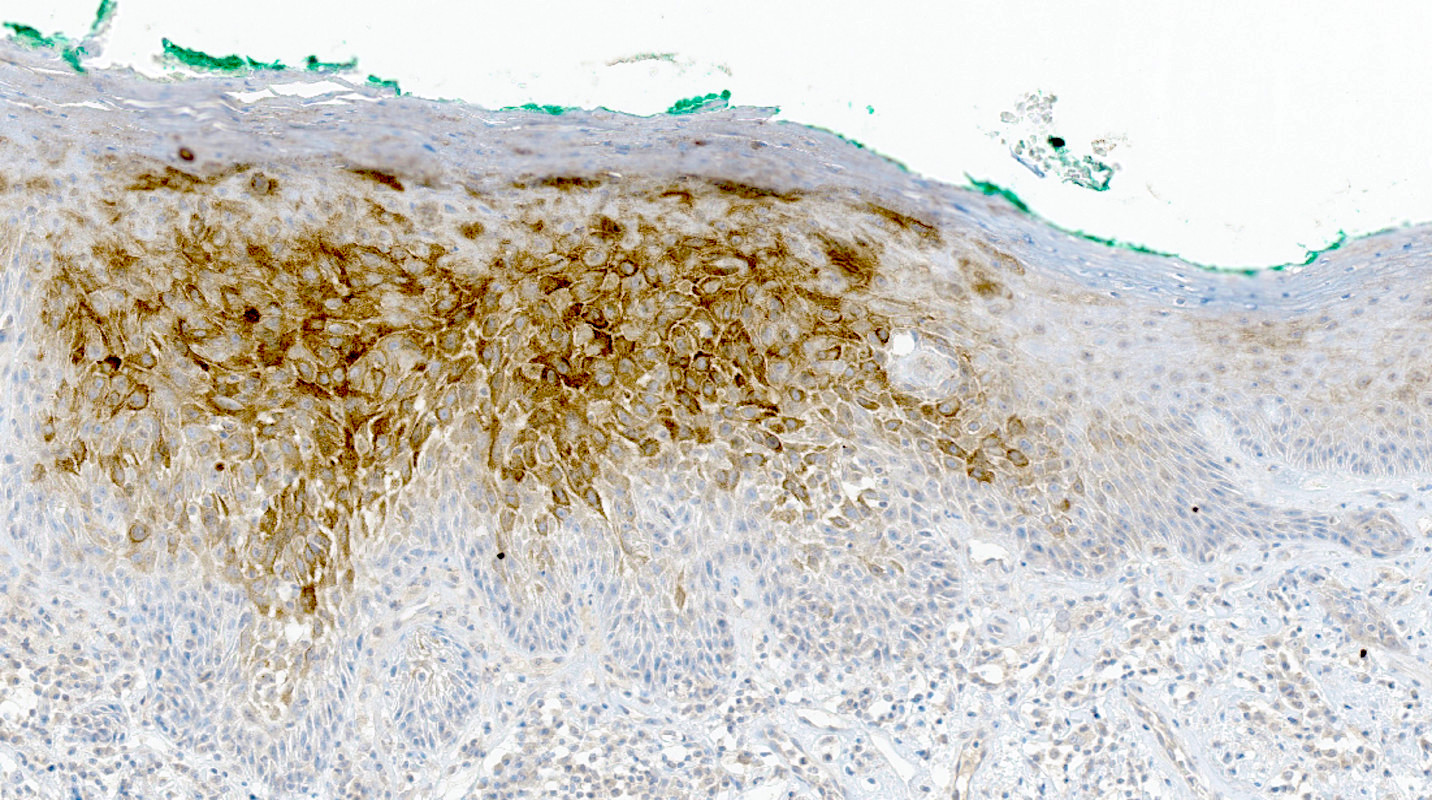
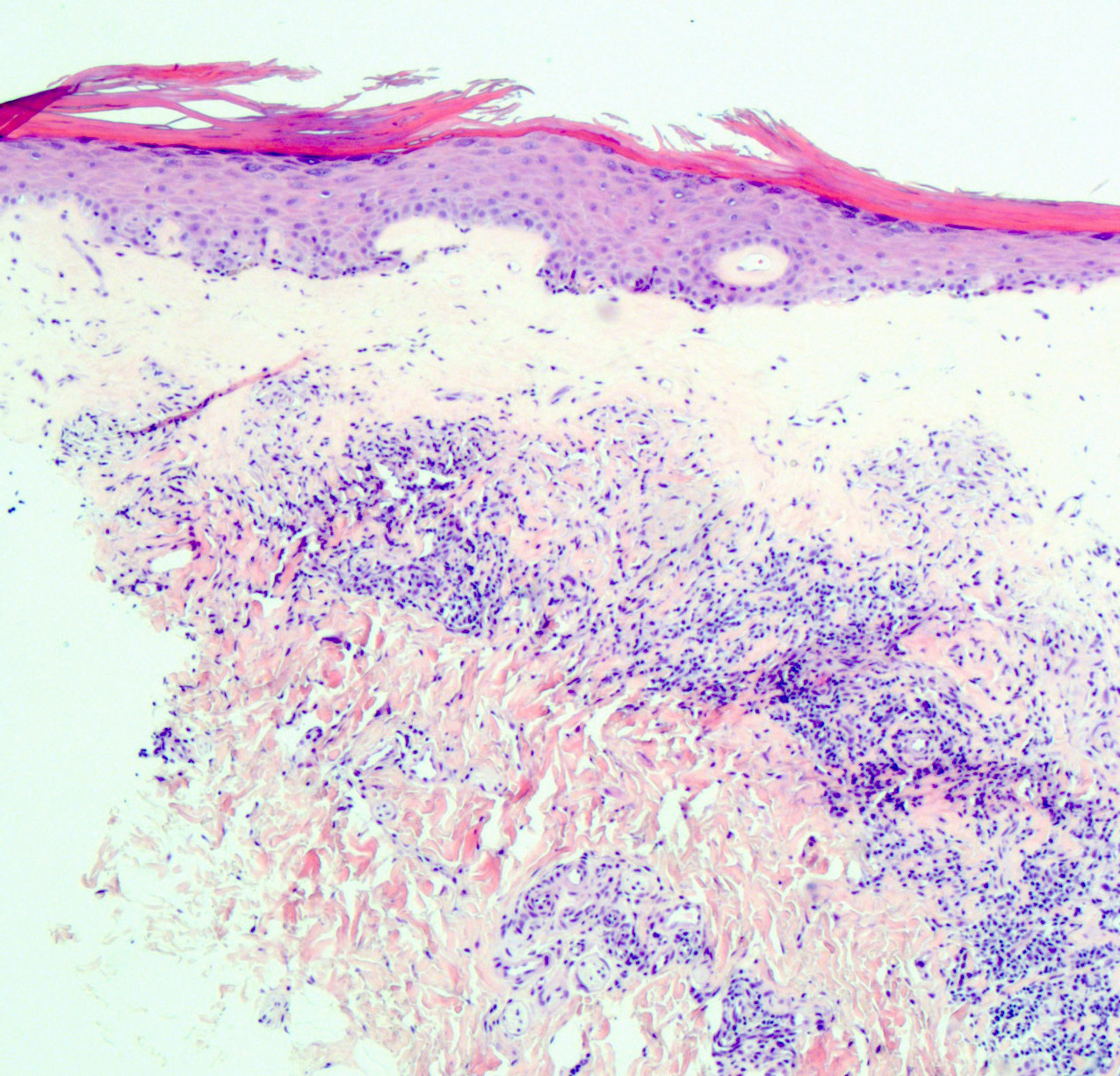
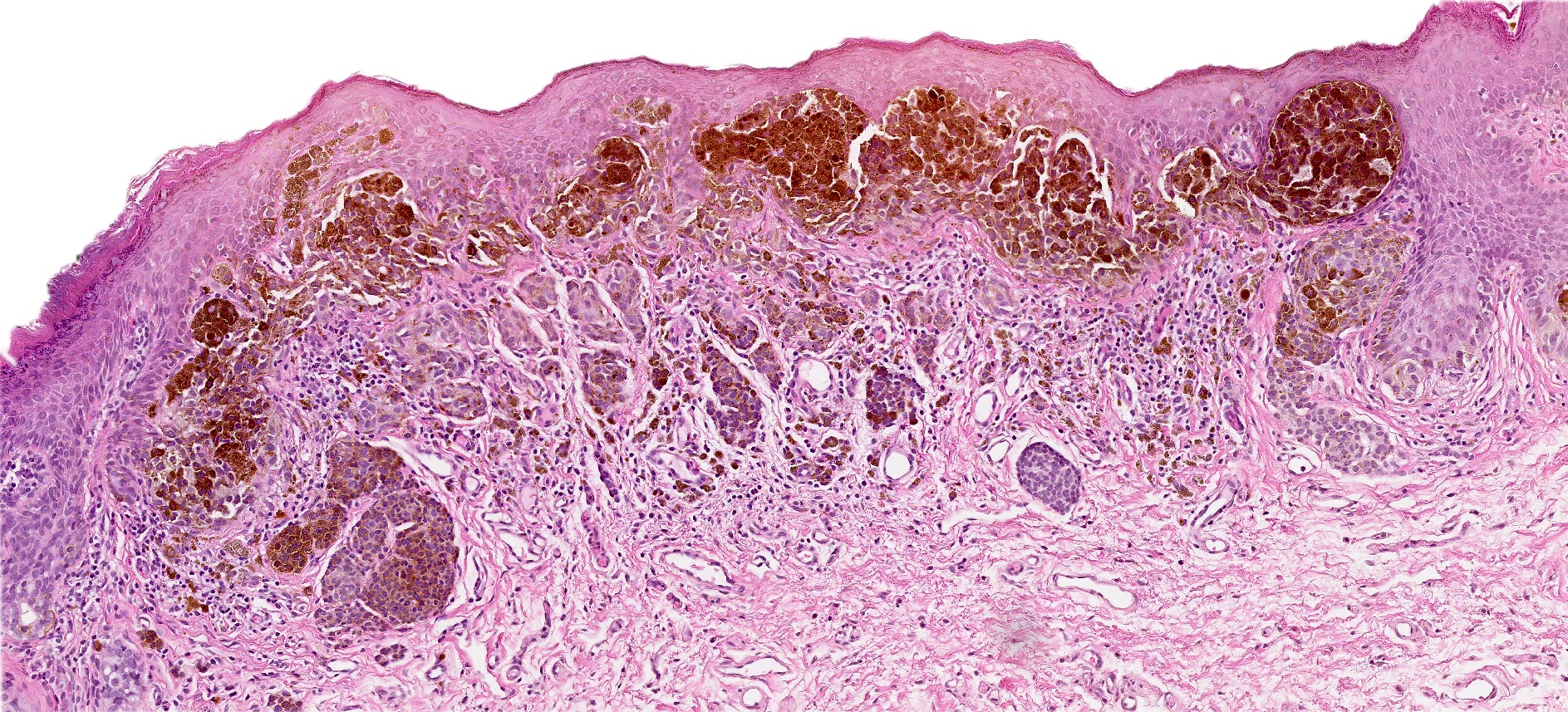
A raised vaginal lesion in a 52 year old woman was biopsied and demonstrated features shown in the image above. What is your diagnosis?
- High grade squamous intraepithelial lesion (HSIL) / vaginal intraepithelial neoplasia (VAIN) 2
- High grade squamous intraepithelial lesion (HSIL) / vaginal intraepithelial neoplasia (VAIN) 3
- Low grade squamous intraepithelial lesion (LSIL) / vaginal intraepithelial neoplasia (VAIN) 1
- Reactive changes, no dysplasia is identified
Answer 29
C. Low grade squamous intraepithelial lesion (LSIL) / vaginal intraepithelial neoplasia (VAIN) 1. The biopsy shows papillomatous architecture, increased cellularity, koilocytic change, increased mitotic activity, hyperkeratosis and parakeratosis, which are all features consistent with the diagnosis of LSIL / VAIN 1. Answers A and B are incorrect because the dysplastic changes do not extend beyond one - third of the epithelium. Answer D is incorrect because the combination of morphological changes shown (including increased mitotic figures and koilocytic changes) is beyond dysplastic changes.
Comment Here
Reference: Vaginal intraepithelial neoplasia (VAIN)
Comment Here
Reference: Vaginal intraepithelial neoplasia (VAIN)
Question 30
The most important tumor related feature for staging early vaginal carcinoma (confined to the vagina) is:
- Depth of invasion
- Involvement of paravaginal adipose tissue
- Lymphovascular space invasion
- Multifocality
- Tumor size
Answer 30
E. Tumor size. Staging of vaginal cancer is mostly clinical (with aid from pathology or radiology data, if available). Tumor size divides early stage tumors in 1a (≤ 2 cm) and 1b (> 2 cm in size). Unlike vulva and cervix, depth of invasion is not required for staging purposes. Lymphovascular invasion and multifocality are prognostic factors but do not influence staging. Involvement of paravaginal adipose tissue is, by definition, extension outside the vagina and qualifies as stage II.
Comment Here
Reference: Staging-vagina carcinoma
Comment Here
Reference: Staging-vagina carcinoma
Question 31
Answer 31
B. Labia majora. Labia majora is composed of keratinized stratified squamous epithelium with hair follicles and eccrine, apocrine and sebaceous glands. Answer A is incorrect because the ectocervix is lined by stratified squamous epithelium overlying fibrous stroma and endocervix is lined by simple, columnar mucinous epithelial cells. Answer C is incorrect because labia minora is lined by keratinized stratified squamous epithelium, without any adnexa. Answer D is incorrect because uterus is lined by endometrial glands, stroma, myometrium and serosa. Answer E is incorrect because vagina has nonkeratinized stratified squamous epithelium and is composed of basal, parabasal, intermediate and superficial cell layers.
Comment Here
Reference: Anatomy & histology - vulva, vagina & female urethra
Comment Here
Reference: Anatomy & histology - vulva, vagina & female urethra
Question 32
What is the epithelium of the labia minora classified as?
- Keratinized stratified squamous epithelium with adnexa
- Keratinized stratified squamous epithelium without adnexa
- Nonkeratinized stratified squamous epithelium with adnexa
- Simple, columnar mucinous epithelial cells
Answer 32
B. Keratinized stratified squamous epithelium without adnexa. This describes the lining of labia minora. Answer A is incorrect because it describes the lining of the labia majora. Answer C is incorrect because the epithelium of labia minora is keratinized and without adnexa. Answer D is incorrect because this describes the lining of endocervix.
Comment Here
Reference: Anatomy & histology - vulva, vagina & female urethra
Comment Here
Reference: Anatomy & histology - vulva, vagina & female urethra
Question 33
A 19 year old patient presented with a 1.2 cm dark brown to black papule with irregular borders on the left labia minora. Histologic examination showed nearly contiguous large oval nests with striking atypia, nearly obscuring the dermal epidermal junction. What would be the most concerning feature?
- Adnexal spread
- Dense fibrosis in papillary dermis
- Lack of a mature dermal component
- Pagetoid spread to granular layer in the center of the lesion
Answer 33
C. Lack of a mature dermal component. Atypical melanocytic nevus of genital type is usually a symmetric, well delineated lesion that can be associated with a common dermal component. Answers B and D are incorrect because atypical melanocytic nevus is characterized by dense fibrosis in the papillary dermis and focal pagetoid spread to the granular layer is usually present in the center of the lesion. Answer A is incorrect because adnexal spread and mature dermal component are also common features of atypical melanocytic nevus of genital type. Hence, the lack of maturation is the most concerning feature in this patient.
Comment Here
Reference: Pigmented lesions-vulva
Comment Here
Reference: Pigmented lesions-vulva
Question 34
A 65 year old woman presented with a dark brown macule with irregular borders measuring 0.7 cm in the largest dimension, located at the mucosal junction of right labia majora (left image). Shave biopsy is shown (right image). Which of the following is true for this patient's condition?
- HPV test will help to diagnose the lesion
- p63 will highlight neoplastic cells
- PRAME will highlight an in situ component
- SOX10 may demonstrate slight increase in density of the isolated melanocytes at the dermal - epidermal junction
Answer 34
D. SOX10 may demonstrate a slight increase in density of isolated melanocytes at the dermal epidermal junction. Melanocytic macules with hyperpigmentation in basal keratinocytes may show a slight increase in melanocytes at the dermal - epidermal junction, with no confluence. Hence, SOX10 may demonstrate a slight increase in density of isolated melanocytes at the dermal - epidermal junction. Answer C is incorrect because PRAME is typically positive in melanoma. Answer B is incorrect because p63 is positive in squamous epithelial cells. Answer A is incorrect because pigmented HPV associated lesions demonstrate koilocytic changes, hyperplastic squamous epithelium and a lack of basal layer maturation.
Comment Here
Reference: Pigmented lesions-vulva
Comment Here
Reference: Pigmented lesions-vulva
Question 35
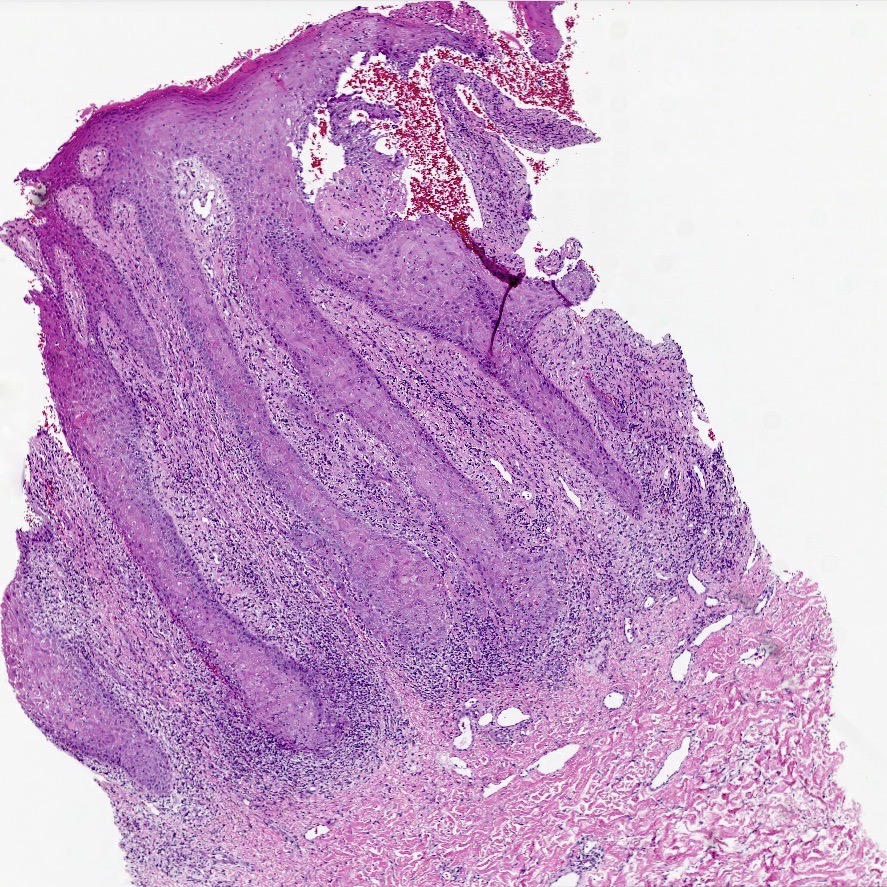
A 78 year old woman presents with a 2 cm pearly pink nodule in the right labium majus. Dermoscopy of the lesion reveals ovoid nests and arborizing fine blood vessels. A biopsy is performed and shows the image above. Which of the following is true?
- Genes usually mutated in this cancer include TP53 and NOTCH1
- Human papillomavirus (HPV) plays a major role in disease pathogenesis
- The tumor is also positive for CK20 perinuclear dot-like staining
- This neoplasm has a high rate of metastatic disease
Answer 35
A. Genes usually mutated in this cancer include TP53 and NOTCH1. TP53 and NOTCH1 are mutated in about half of basal cell carcinomas (BCCs). Answer D is incorrect because metastatic disease from BCC is rare. Answer B is incorrect because BCCs are HPV independent. Answer C is incorrect because the described staining pattern is seen in Merkel cell carcinomas.
Comment Here
Reference: Basal cell carcinoma-vulva
Comment Here
Reference: Basal cell carcinoma-vulva
Question 36
An 83 year old woman presents with a slightly erythematous and ulcerative lesion in the left vulva. A biopsy is performed and is positive for basal cell carcinoma. Which of the following immunohistochemical stains is positive in this tumor?
- BCL2
- CEA
- CK20
- EMA
Answer 36
A. BCL2. Basal cell carcinomas (BCCs) stain diffusely positive for BCL2. Answer D is incorrect because BCCs usually stain negative for EMA. Answer C is incorrect because BCCs usually stain negative for CK20. Answer B is incorrect because BCCs usually stain negative for CEA.
Comment Here
Reference: Basal cell carcinoma-vulva
Comment Here
Reference: Basal cell carcinoma-vulva
Question 37
A vulvar biopsy reveals large polyhedral cells with large nuclei and pale cytoplasm trickling through the epidermis. Immunohistochemistry reveals that the tumor cells are positive for CK7, CK20, uroplakin III and p63. The tumor cells are negative for GCDFP-15, ER and PR. What is the best diagnosis?
- Primary extramammary Paget disease
- Secondary Paget disease, likely associated with breast carcinoma
- Secondary Paget disease, likely associated with rectal carcinoma
- Secondary Paget disease, likely associated with urothelial carcinoma
Answer 37
D. Secondary Paget disease, likely associated with urothelial carcinoma. Vulvar Paget disease secondary to urothelial carcinoma is positive for CK7, CK20, uroplakin III and p63. Answer A is incorrect because primary Paget disease of the vulva would be negative for uroplakin III and CK20. It is, however, positive for CK7. Answer C is incorrect because vulvar Paget disease secondary to anorectal carcinoma is generally negative for CK7 and uroplakin III. It is, however, positive for CK20. Answer B is incorrect because vulvar Paget disease secondary to breast carcinoma would be exceedingly rare. If such an entity were to occur, it would not be positive for uroplakin III and it would be unlikely for it to be positive for CK20; it could be CK7 positive.
Comment Here
Reference: Vulva & vagina - Paget disease
Comment Here
Reference: Vulva & vagina - Paget disease
Question 38
A 66 year old woman presents with a pruritic plaque on the right labia majora of 2 years duration. She has no significant oncologic history. As her symptoms have not improved, a punch biopsy is performed (image shown above). A mucicarmine stain is positive within the tumor cells. Which of the following ancillary stains would also likely be positive in this tumor?
- CK5/6
- CK7
- High risk HPV in situ hybridization
- HMB45
Answer 38
B. CK7. Given the history of a pruritic lesion of years in duration, along with the microscopic image of mucicarmine positive cells percolating through the epidermis, the diagnosis is most likely extramammary Paget disease, which is strongly CK7 positive. Answer D is incorrect because while melanoma is certainly in the differential diagnosis given the microscopic image, it would not be consistent with mucicarmine positivity; therefore, HMB45, a melanoma marker, is incorrect. Answer C is incorrect because while in theory high risk HPV ISH could potentially be positive in Paget disease of the vulva secondary to a HPV dependent cervical adenocarcinoma, primary vulvar Paget disease is far more common. Answer A is incorrect because CK5/6 is a high molecular weight cytokeratin, which stains squamous cells, not glandular cells.
Comment Here
Reference: Vulva & vagina - Paget disease
Comment Here
Reference: Vulva & vagina - Paget disease
Question 39
A 42 year old woman presented to the clinic with a 0.8 cm flat, dark brown lesion with an irregular border on the mons pubis. The histologic findings of the shave biopsy demonstrated a broad junctional atypical melanocytic proliferation with central dermal component, focal bridging of adjacent junctional nests, focal pagetoid spread, moderate cytologic atypia, rare dermal mitoses (2 mitoses/2 mm2) and dense lymphocytic infiltrate. The lesion is transected at the deep dermis. What is the most important histological finding that questions the diagnosis of a dysplastic nevus?
- Cytologic atypia, grade 1
- Dermal mitotic activity (2 mitoses/2 mm2)
- Focal fused junctional nests
- Focal pagetoid spread
Answer 39
B. Dermal mitotic activity (2 mitoses/2 mm2). When considering a dysplastic melanocytic nevus, any dermal mitotic figures, especially atypical mitosis, should warrant additional work up. Answer C is incorrect because unless there is confluent architectural atypia, the focal fusion of junctional nests is not a concerning feature by itself and part of the diagnostic criteria for dysplastic nevus. Answer D is incorrect because it is permissible for dysplastic nevus to demonstrate focal pagetoid spread that does not exceed the lower part of epidermis. The concerning features include extensive wide pagetoid spread of melanocytes, especially if it extends past the epidermis and laterally beyond the underlying junctional component. Answer A is incorrect because cytologic atypia, grade 1 (see Table 3) is the least concerning feature in this lesion and without the presence of architectural atypia would not be enough for diagnosis of dysplastic nevus.
Comment Here
Reference: Dysplastic nevi
Comment Here
Reference: Dysplastic nevi
Question 40
A 38 year old woman presented to the OBGYN clinic with a 0.9 cm, irregular, dome shaped, dark pigmented papule on the right labium majus. A biopsy demonstrated symmetric melanocytic proliferation, with maturation, adjacent bridges of rete ridges and focal pagetoid spread mostly confined to the lower level of the epidermis. What is the most likely molecular alteration in this lesion?
- ALK fusion
- BRAF V600E mutation
- Homozygous deletion of CDKN2A
- NRAS mutation
Answer 40
B. BRAF V600E mutation. Most dysplastic melanocytic nevi have a driver mutation in BRAF V600E. Answer A is incorrect as ALK fusion is more characteristic of Spitz nevus. Answers C and D are incorrect as those alterations are specific to superficial spreading melanoma.
Comment Here
Reference: Dysplastic nevi
Comment Here
Reference: Dysplastic nevi