Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Pineda Reyes JP, Ma L. Basal cell carcinoma-vulva. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvabasalcellcarc.html. Accessed October 4th, 2025.
Definition / general
- Basal cell carcinoma (BCC) arises from epithelial cells of either epidermis or hair follicle stem cells
- Vulvar BCC is rare
- Histologic features are identical to that of BCC occurring elsewhere on the skin
Essential features
- Characterized by the presence of nests of basaloid / hyperchromatic nuclei with minimal cytoplasm
- Predominantly seen in older (mean: seventh decade) White women
- Occurs most commonly in the labium majus but can involve any other area of vulva
- Excellent prognosis with up to 21% rate of local recurrence and very rare metastasis
Terminology
- Not recommended: basalioma of the vulva, basal cell epithelioma of the vulva
ICD coding
Epidemiology
- Accounts for < 5% of all vulvar cancers and < 1% of all basal cell carcinomas (J Am Acad Dermatol 2001;45:68, Gynecol Oncol 2005;97:192)
- Mean patient age is ~70 years (Gynecol Oncol 2005;97:192, Dermatol Surg 2023;49:13)
- Predominantly seen in White women
Sites
- Cutaneous epithelium of the vulva but may involve mucosal epithelium as well
- Most common location: labium majus followed by clitoris (Int J Dermatol 2019;58:892)
Pathophysiology
- Arises from skin epithelial cells or hair follicle stem cells (Cell Stem Cell 2015;16:400)
- Inactivating mutations in PTCH1 may contribute to BCC genesis in the absence of ultraviolet irradiation (Cancer Cell 2018;33:229)
- Mutations in TP53
- Activating mutations of SMO
- HPV independent
Etiology
- Unclear; etiology might differ from that of BCC in sun exposed skin
- Proposed risk factors include
- Chronic vulvar irritation
- History of pelvic radiation therapy (J Am Acad Dermatol 2001;45:68)
- Advanced age
- White race
- Basal cell nevus syndrome (Gorlin syndrome) due to germline PTCH1 mutations
- Xeroderma pigmentosum
- Immunosuppression (Gynecol Oncol 2005;97:192)
- Exposure to arsenic (TJ Obstet Gynaecol Br Emp 1956;63:697)
- Syphilis infection (TJ Obstet Gynaecol Br Emp 1956;63:697)
- Local trauma (Gynecol Oncol 2005;97:192, J Am Acad Dermatol 2001;45:68)
Clinical features
- Frequently asymptomatic
- In symptomatic patients, pruritus is the most frequent symptom (Int J Gynecol Pathol 2023;42:327, Gynecol Oncol 2016;142:440)
- Vulvar lump sensation, palpable vulvar mass, erythema, ulceration, irritation, pain, bleeding (Gynecol Oncol 2005;97:192)
- Clinical appearance ranges from erythematous papules and patches to plaques or nodules with or without ulceration or pigmentation (J Am Acad Dermatol 2001;45:68)
- Dermoscopy findings are identical to BCC in other body areas
- Presence of arborizing vessels and blue globules, shiny white structures (Dermatol Pract Concept 2018;8:68, Arch Dermatol 2007;143:426, J Eur Acad Dermatol Venereol 2017;31:e180)
Diagnosis
- Definite diagnosis requires biopsy / excision
Prognostic factors
- Overall prognosis is excellent
- Local recurrence rates range from 0% to 21% in different case series (Int J Gynecol Pathol 2022;41:86, Cancer 1969;24:460, Int J Dermatol 2019;58:892)
- Lymph node and distant metastasis can occur but is rare
- Features with increased risk for recurrence and metastasis
- Size > 5 - 20 mm, tumor thickness, extension into the subcutis, perineural invasion, aggressive histological subtype (morpheaform, infiltrative, basosquamous) and surgical margins < 3.0 mm (Obstet Gynecol 1997;90:765, Int J Gynecol Pathol 2022;41:86)
Case reports
- 51 year old woman with a 1.5 cm firm vulvar lesion with shallow red ulcerations at the lower mons pubis (Cureus 2021;13:e20791)
- 51 year old woman with a history of incompletely resected vulvar basal cell carcinoma, now with bilateral lung nodules and inguinal lymphadenopathy (Gynecol Oncol Rep 2016;18:32)
- 70 year old woman with vulvar basal cell carcinoma and bilateral inguinal lymph node metastases (Case Rep Oncol 2019;12:573)
- 80 year old woman with a history of repeated exposure to perineal heat lamps presents with a 1.8 cm pink pearly eroded plaque on the left vulva (JAAD Case Rep 2020;6:103)
- 83 year old woman with a history of lichen sclerosus presents with a tender, 5 mm eroded papule on the right labium majus (Int J Dermatol 2019;58:892)
Treatment
- Primary treatment is wide local excision or vulvectomy with margin assessment (Gynecol Oncol 2016;142:440)
- Surgical excision by Mohs micrographic surgery or PDEMA (peripheral and deep en face margin assessment) (J Natl Compr Canc Netw 2023;21:1181)
- Radiotherapy for nonsurgical candidates
- If not feasible, systemic therapy with HHIs (hedgehog pathway inhibitors) may be recommended (J Natl Compr Canc Netw 2023;21:1181)
Clinical images
Gross description
- Pink, pearly nodule, with or without elevated borders and telangiectasias
- Ulceration or dark brown pigment may be present
- Flat, scar-like lesion in superficial BCCs
- Reference: Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019
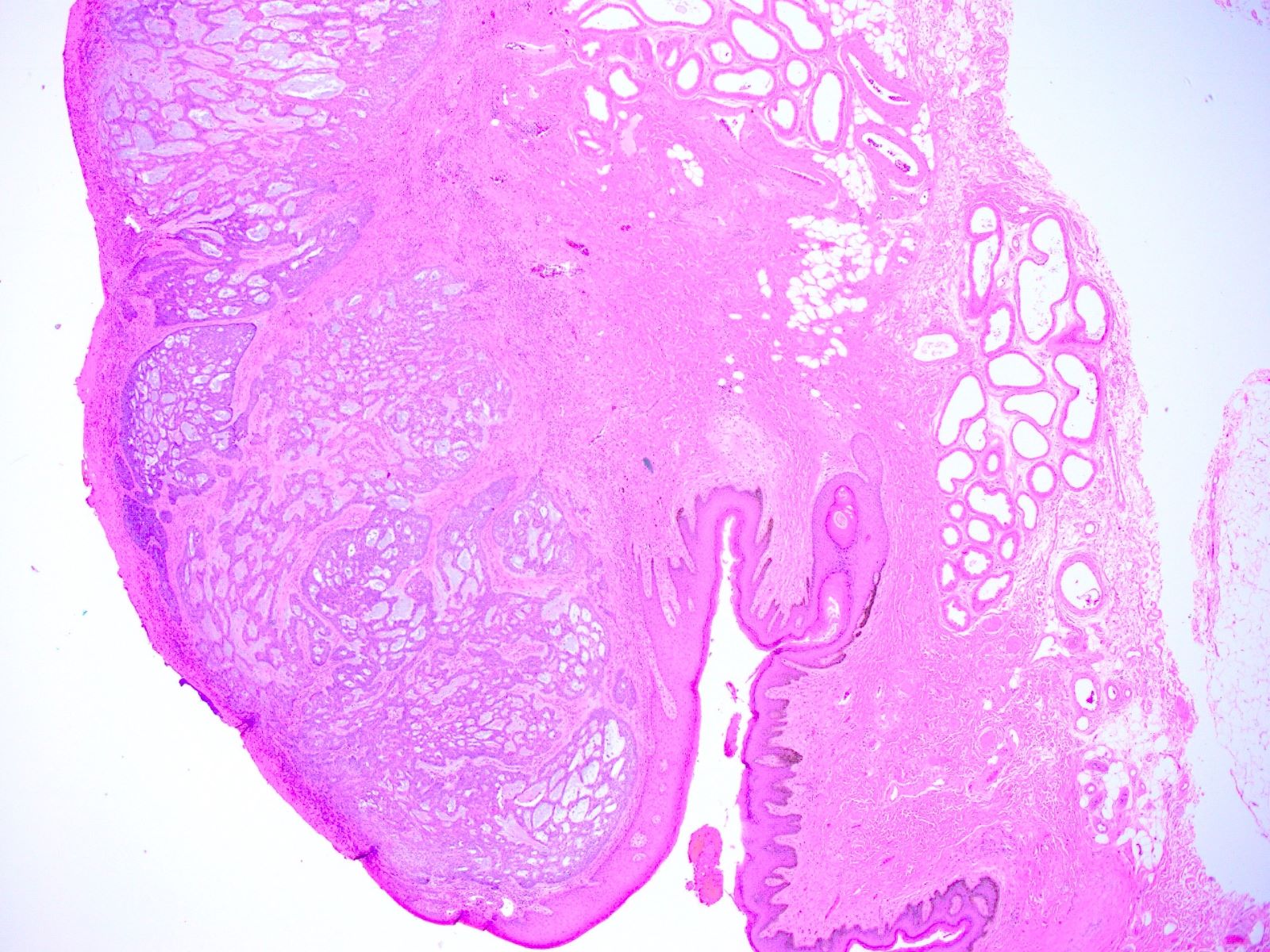
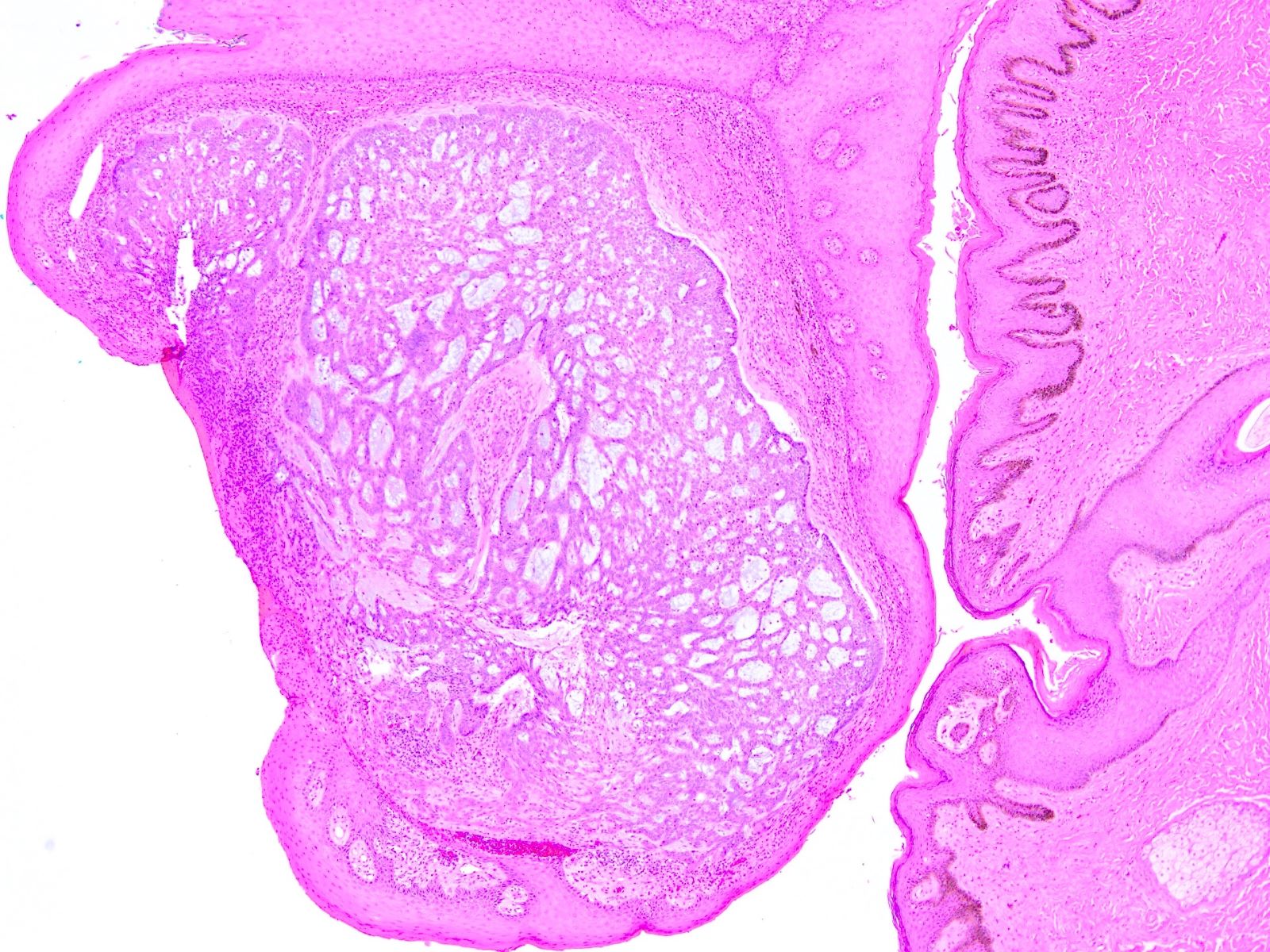
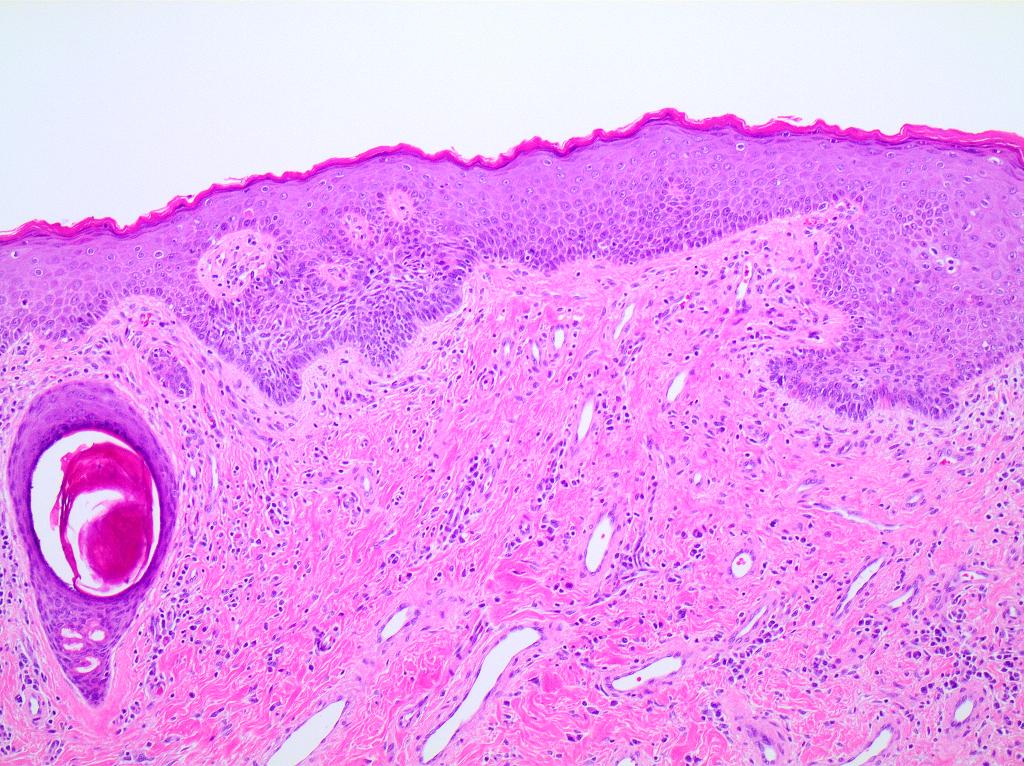
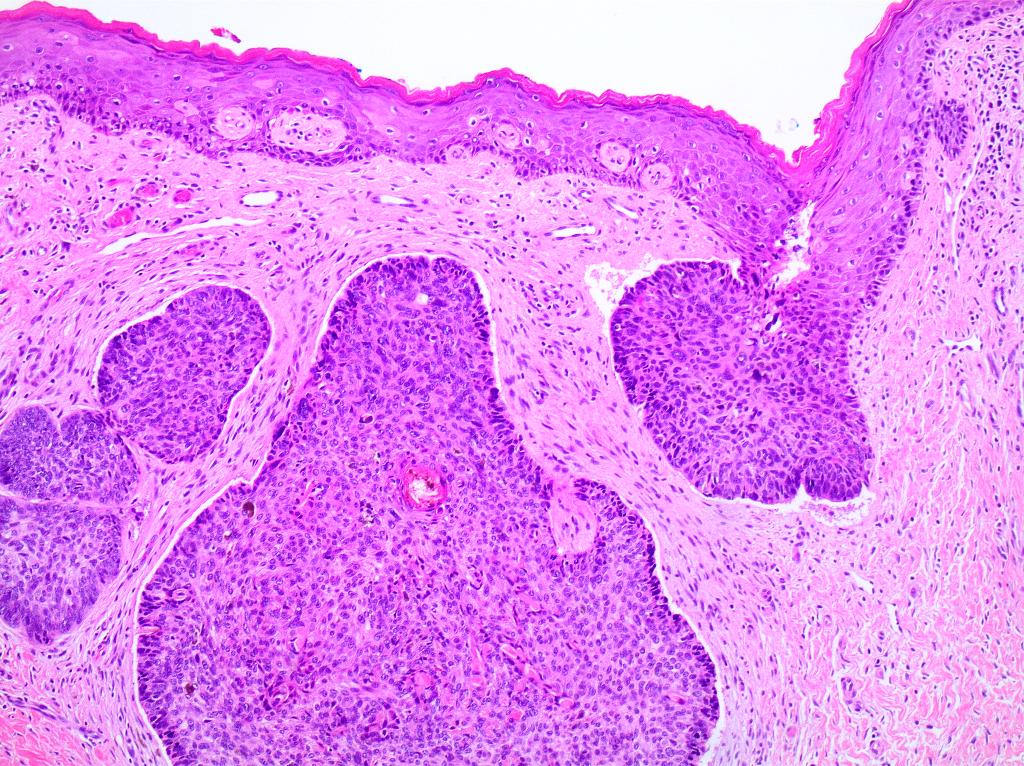
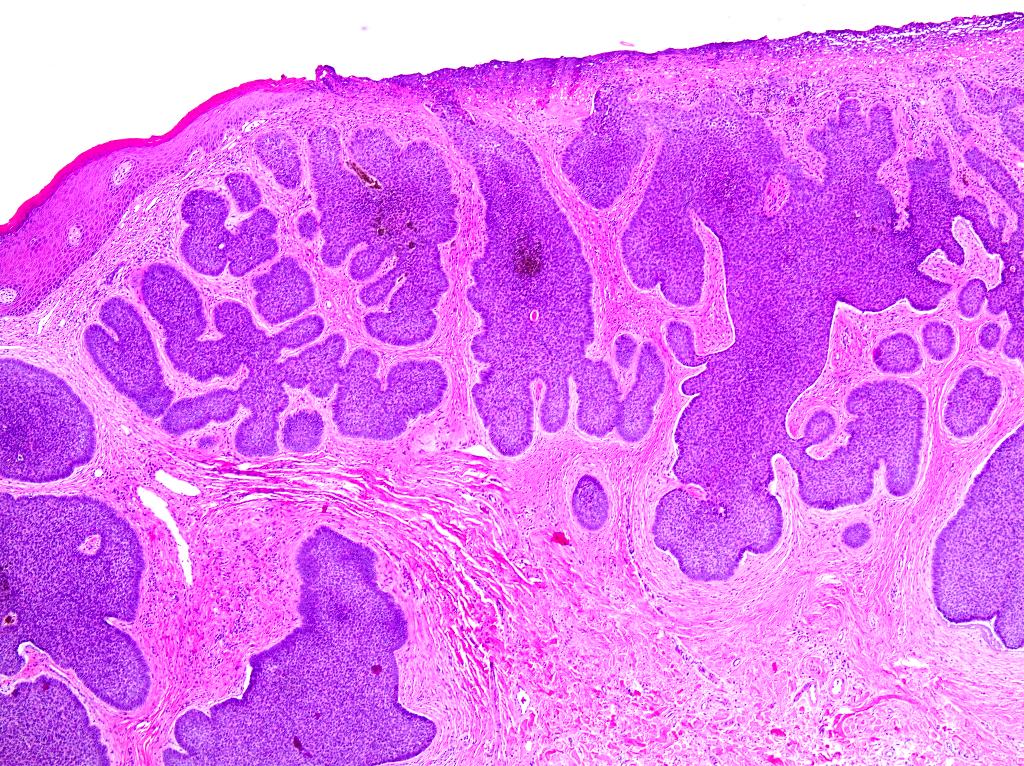
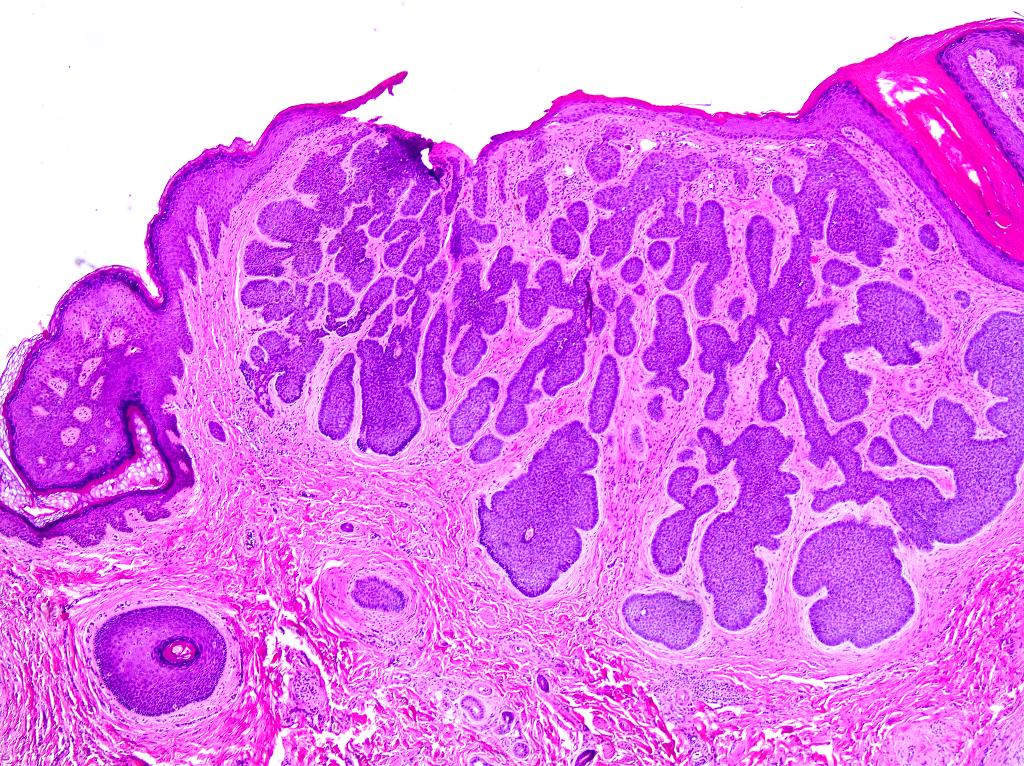
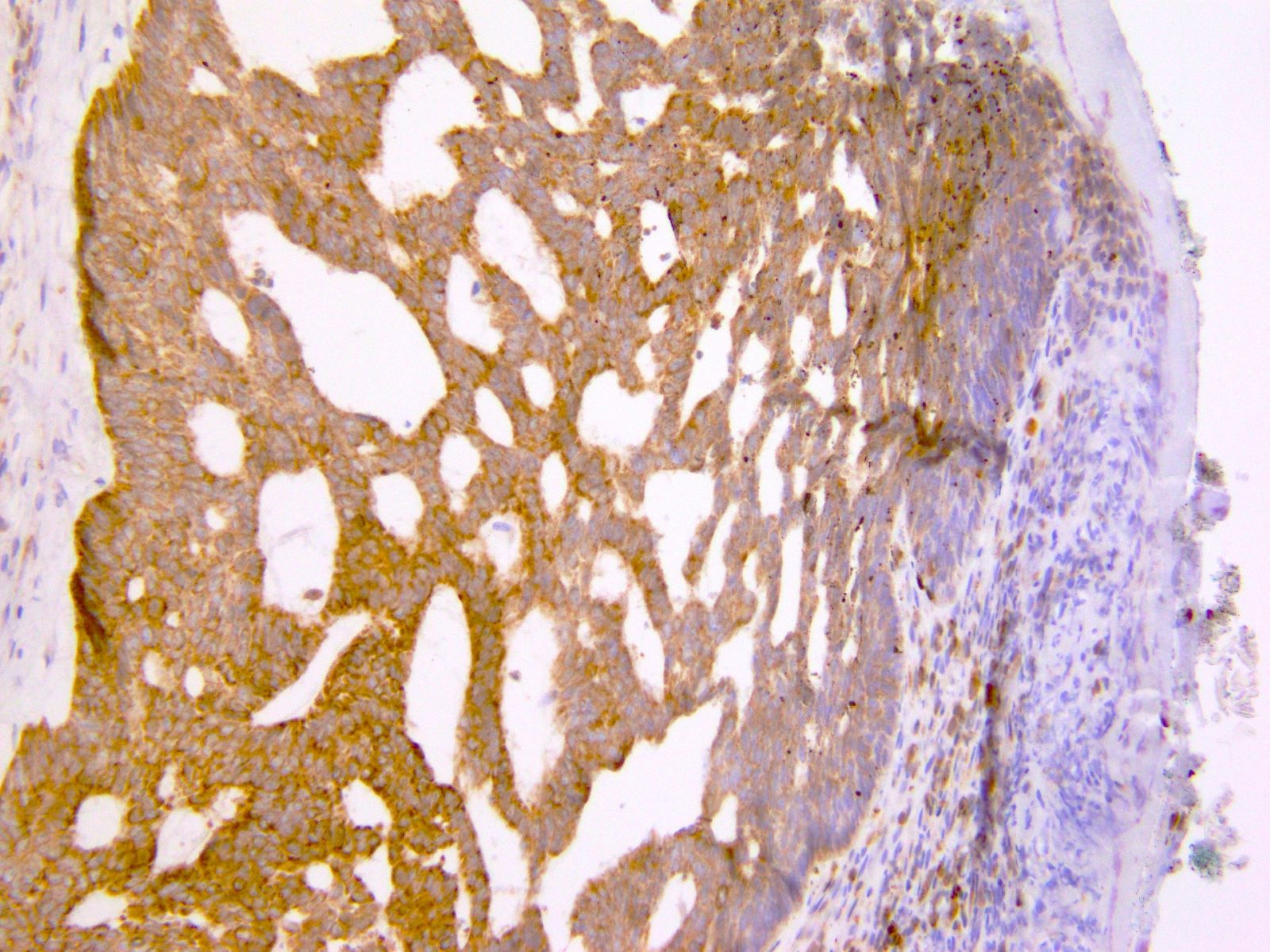
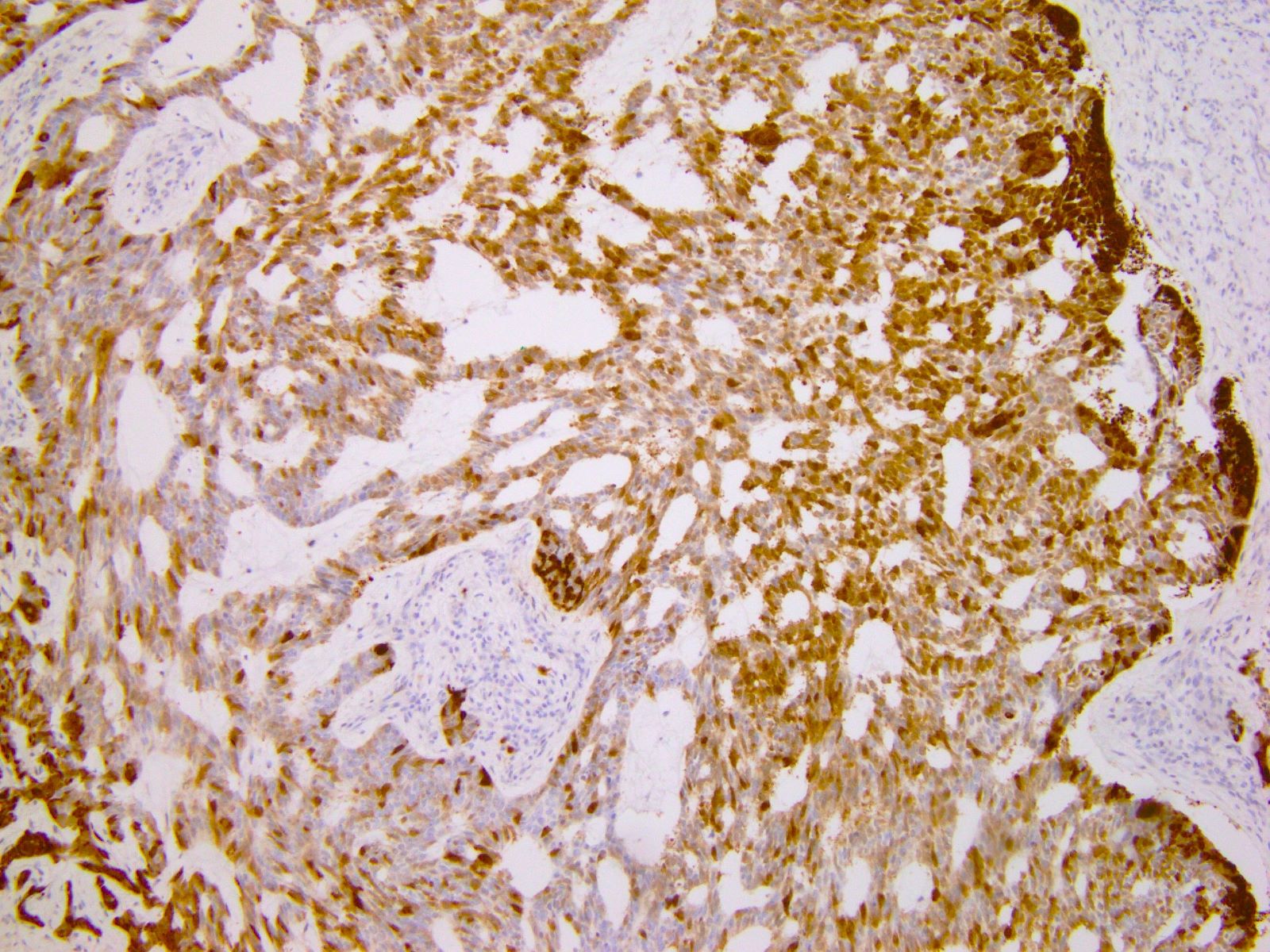
Microscopic (histologic) description
- Identical diagnostic criteria to BCC occurring elsewhere on the skin
- Basaloid tumor cells with uniform hyperchromatic / basophilic nuclei and scant cytoplasm
- Peripheral palisading of tumor cells with variety of architectural patterns
- Retraction artifact of tumor nests from surrounding stroma (also known as clefting)
- Stromal changes
- Fibromyxoid change, calcification, amyloid deposition
- May be colonized by nonneoplastic melanocytes and may contain melanin pigment
- With or without squamous differentiation
- Most frequent histologic subtype is nodular, followed by superficial and infiltrative
- References: Calonje: McKee’s Pathology of the Skin, 5th Edition, 2019, Kurman: Blaustein's Pathology of the Female Genital Tract, 7th Edition, 2019
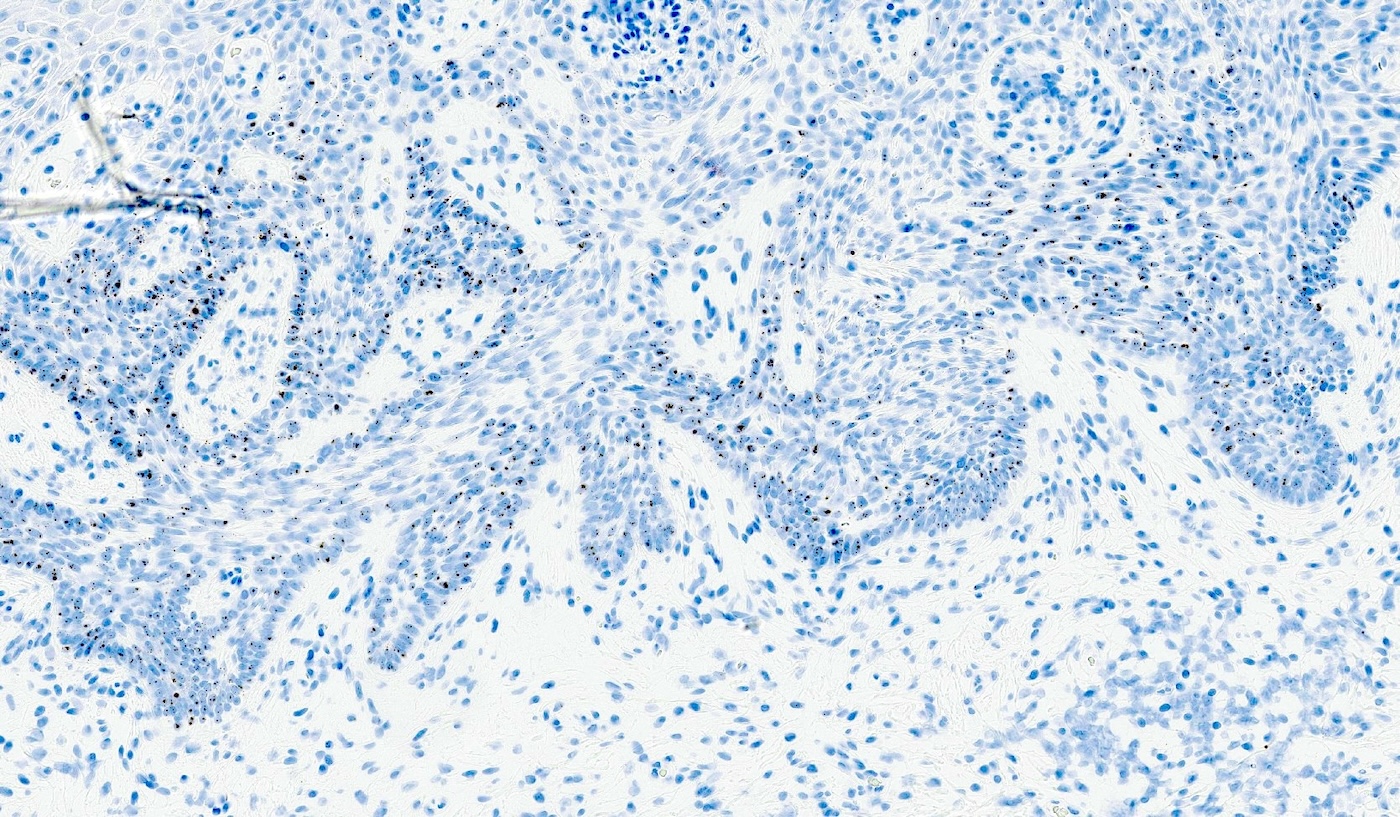
Microscopic (histologic) images
Contributed by Lucy Ma, M.D., Priya Nagarajan, M.D., Ph.D. and Stephanie L. Skala, M.D.
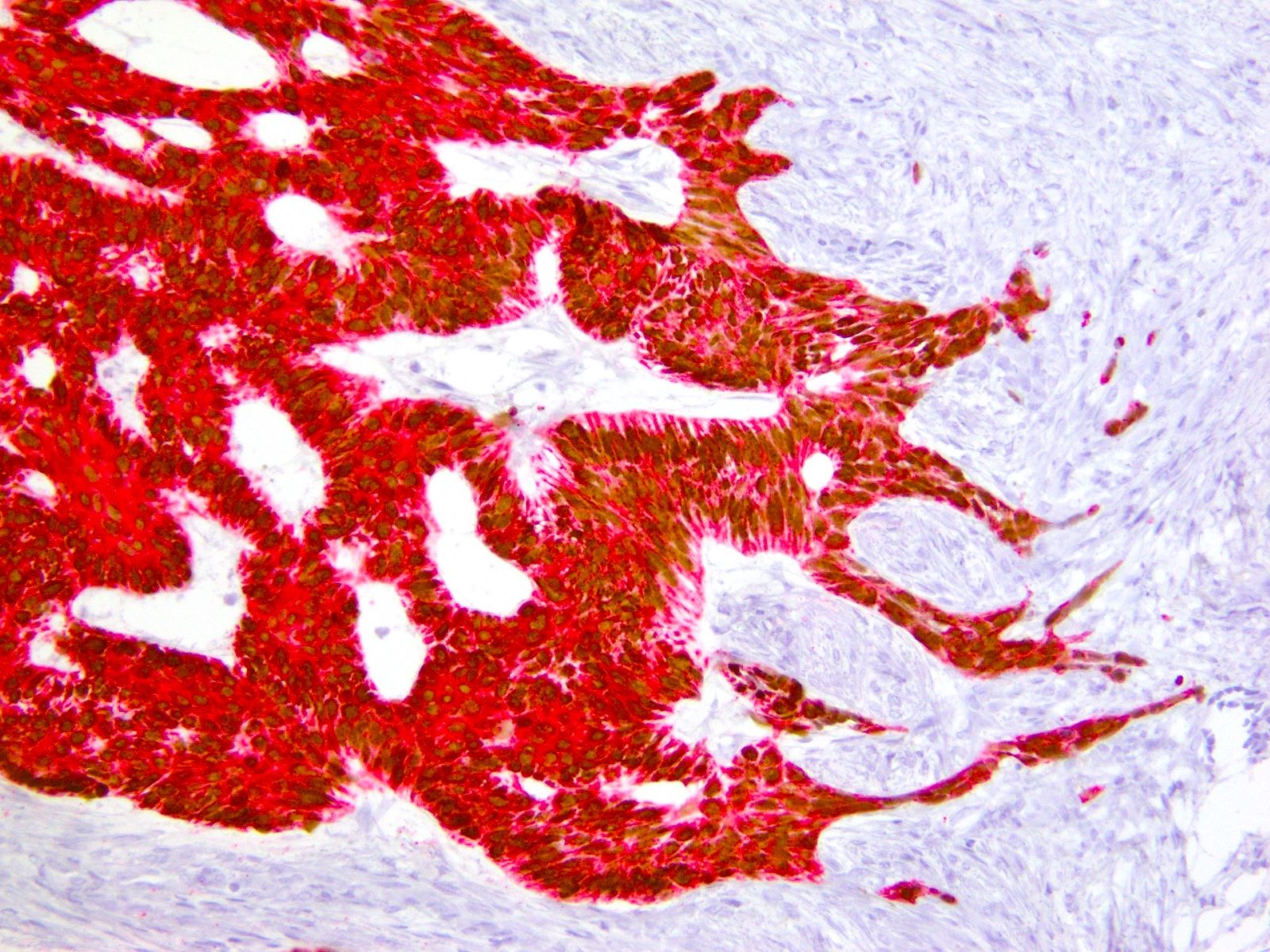
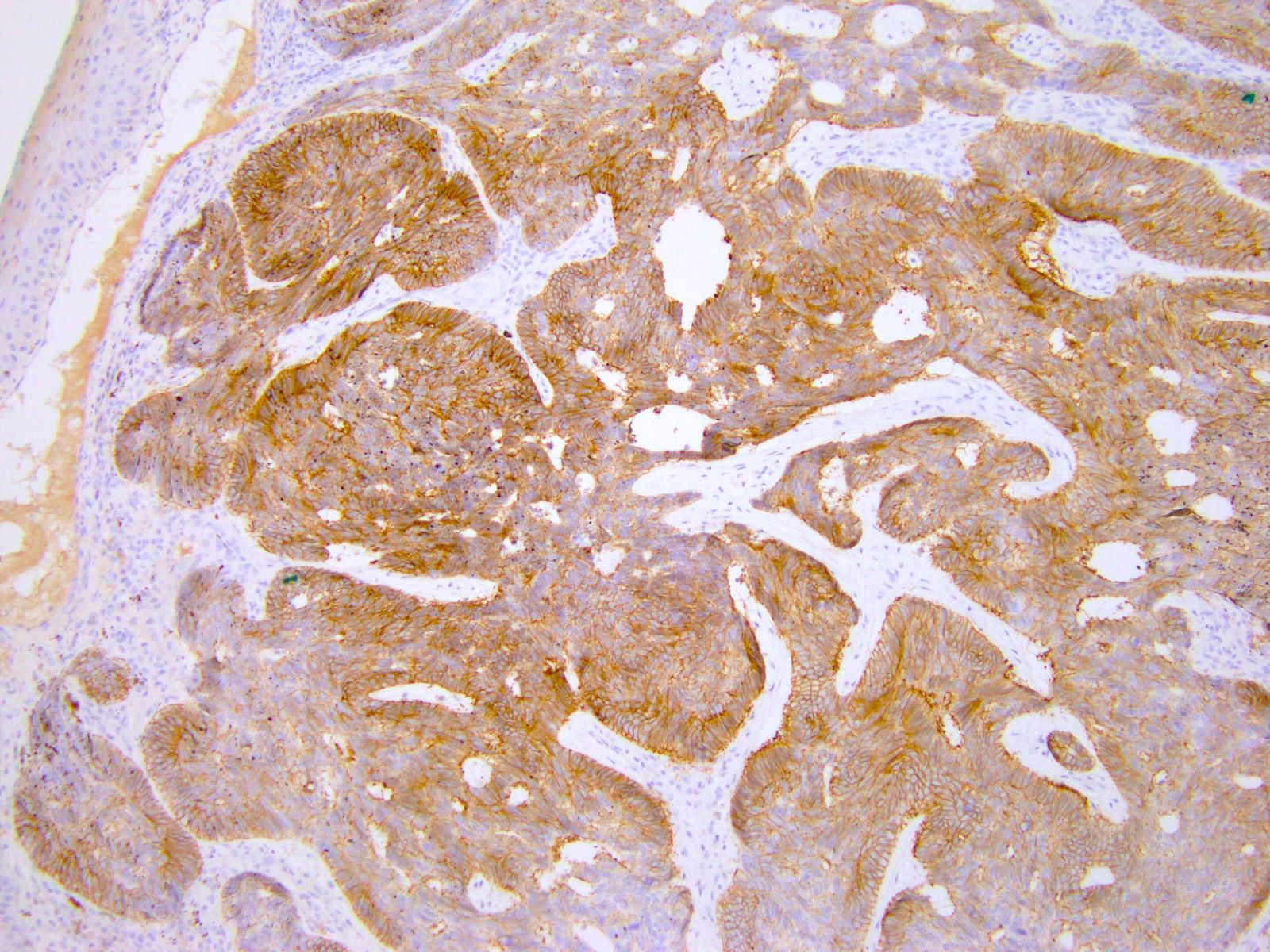
Positive stains
- p40, p63, CK5/6
- BerEP4 (typically diffuse), BCL2 (diffuse), CD10 (tumor and stroma), AR (focal)
- CK7, CK19 (J Cutan Med Surg 2017;21:457)
- CD56 (95%), chromogranin A (28%), and synaptophysin (18%) (Med Oncol 2013;30:444, J Immunoassay Immunochem 2017;38:487)
- GLI1 ISH (Mod Pathol 2023;36:100265)
Negative stains
- EMA, CEA, CK20 (may be positive in colonizing Merkel cells)
- PHLDA1 (TDAG51) (J Cutan Pathol 2011;38:542)
- p16 (negative or patchy), high risk HPV in situ hybridization (Am J Surg Pathol 2014;38:542)
Molecular / cytogenetics description
- See Pathophysiology
Videos
BCC 101 by Dr. Jerad Gardner
Reporting BCC by Dr. Catriona McKenzie, pathCast
Sample pathology report
- Vulva, left (partial vulvectomy):
- Basal cell carcinoma, 1.3 cm
- Depth of invasion: 2 mm
- Margins are negative
Differential diagnosis
- Basaloid squamous cell carcinoma:
- Trichoepithelioma / trichoblastoma:
- Basaloid follicular neoplasm
- Presence of horn / keratin cysts and lack of retraction artifact
- CD10 expression limited to stroma
- PHLDA1 (TDAG51)+
- Merkel cell carcinoma:
- Typically no connection to overlying dermis
- Small, round, blue cell tumor with high N:C ratio, round nuclei, salt and pepper chromatin
- Conspicuous mitoses and apoptotic bodies
- CK20+, perinuclear dot-like staining
- Adenoid cystic carcinoma:
- More deeply situated; no connection to overlying epidermis
- Biphasic neoplasm with ductal and myoepithelial differentiation
- Characteristic cribriform, tubular and solid architectural patterns
- Cribriform spaces filled with basement-like material
- MYB:NFIB fusion
- Differentiated vulvar intraepithelial neoplasia:
- Differential diagnosis of superficial subtype of BCC
- Atypical cells confined to basal layer
- Large nuclei with vesicular chromatin, prominent nuclei
- Retained but abnormal maturation of epithelium
- Aberrant p53 expression
Additional references
Practice question #1
A 78 year old woman presents with a 2 cm pearly pink nodule in the right labium majus. Dermoscopy of the lesion reveals ovoid nests and arborizing fine blood vessels. A biopsy is performed and shows the image above. Which of the following is true?
- Genes usually mutated in this cancer include TP53 and NOTCH1
- Human papillomavirus (HPV) plays a major role in disease pathogenesis
- The tumor is also positive for CK20 perinuclear dot-like staining
- This neoplasm has a high rate of metastatic disease
Practice answer #1
A. Genes usually mutated in this cancer include TP53 and NOTCH1. TP53 and NOTCH1 are mutated in about half of basal cell carcinomas (BCCs). Answer D is incorrect because metastatic disease from BCC is rare. Answer B is incorrect because BCCs are HPV independent. Answer C is incorrect because the described staining pattern is seen in Merkel cell carcinomas.
Comment Here
Reference: Basal cell carcinoma-vulva
Comment Here
Reference: Basal cell carcinoma-vulva
Practice question #2
An 83 year old woman presents with a slightly erythematous and ulcerative lesion in the left vulva. A biopsy is performed and is positive for basal cell carcinoma. Which of the following immunohistochemical stains is positive in this tumor?
- BCL2
- CEA
- CK20
- EMA
Practice answer #2
A. BCL2. Basal cell carcinomas (BCCs) stain diffusely positive for BCL2. Answer D is incorrect because BCCs usually stain negative for EMA. Answer C is incorrect because BCCs usually stain negative for CK20. Answer B is incorrect because BCCs usually stain negative for CEA.
Comment Here
Reference: Basal cell carcinoma-vulva
Comment Here
Reference: Basal cell carcinoma-vulva