Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Brown ML, Tretiakova M. Microcystic. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladdermicrocystic.html. Accessed May 13th, 2024.
Definition / general
- Invasive urothelial carcinoma with deceptively bland architecture and cytology, consisting of slit-like or tubular microcysts lined by cuboidal / flattened cells with minimal atypia and intraluminal granular eosinophilic material (Mod Pathol 2009;22:S96)
Essential features
- Very rare, predominantly case reports and small series (Histopathology 2014;64:872)
- Main biologic significance is deceptively benign features, which may be mistaken for cystitis cystica or glandularis on small biopsies but is usually deeply invasive
- Histologically may be distinguished by infiltrative growth pattern, as well as variability in cyst size and shape
Terminology
- Also known as urothelial carcinoma with gland-like lumens (Arch Pathol Lab Med 2007;131:1244)
- Recommended to have at least 25% microcystic component to designate as microcystic urothelial carcinoma (Arch Pathol Lab Med 2007;131:1244)
- First described in 1991, in bladder (Am J Clin Pathol 1991;96:635)
ICD coding
- Location based ICD-10 coding:
- Renal pelvis, including pelviureteric junction and renal calyces
- Ureter, including ureteric orifice of bladder
- Bladder
- C67.0 - malignant neoplasm of trigone of bladder
- C67.1 - malignant neoplasm of dome of bladder
- C67.2 - malignant neoplasm of lateral wall of bladder
- C67.3 - malignant neoplasm of anterior wall of bladder
- C67.4 - malignant neoplasm of posterior wall of bladder
- C67.5 - malignant neoplasm of bladder neck
- C67.6 - malignant neoplasm of ureteric orifice
- C67.7 - malignant neoplasm of urachus
- C67.8 - malignant neoplasm of overlapping sites of bladder
- C67.9 - malignant neoplasm of bladder, unspecified
Epidemiology
- Approximately 1% of urothelial carcinomas (Eur Urol Focus 2020;6:653)
- 42 cases reported in genitourinary tract (Urol Case Rep 2020;33:101369)
Sites
- Bladder, renal pelvis
Pathophysiology
- TERT promotor mutations (Histopathology 2019;74:77)
Etiology
- No specific risk factors for development of microcystic variant reported
- General risk factors for urothelial carcinoma: smoking, aromatic amine exposure, arsenic exposure
Clinical features
- Usually deeply invasive
- High recurrence rate (Int J Clin Exp Pathol 2020;13:2778)
Diagnosis
- Cystoscopy
- CT scan
Laboratory
- Hematuria (Int J Clin Exp Pathol 2020;13:2778)
Radiology description
- Bladder wall thickening or mass protruding into lumen (Int J Clin Exp Pathol 2020;13:2778)
Prognostic factors
- Independent prognostic significance has not been established (Mod Pathol 2009;22:S96)
- Variable prognosis, from highly aggressive to similar to conventional invasive urothelial carcinoma (Adv Urol 2013;2013:654751, Arch Pathol Lab Med 2007;131:1244, Histopathology 2014;64:872)
- No survival differences when compared with conventional urothelial carcinoma (Histopathology 2019;74:77)
Case reports
- 37 year old man with microcystic transitional cell carcinoma of the urinary bladder (Pathologica 2017;109:151)
- 55 year old man with microcystic urothelial cell carcinoma (Virchows Arch 2009;454:223)
- 62 year old woman and 73 year old man with microcystic transitional cell carcinoma (Arch Pathol Lab Med 2002;126:859)
- 71 year old man with microcystic urothelial carcinoma of bladder (Urol Case Rep 2020;33:101369)
- 71 year old woman with microcystic urothelial carcinoma of bladder and left lower ureter (Int J Clin Exp Pathol 2020;13:2778)
Treatment
- Managed the same as urothelial carcinoma of the same stage (Eur Urol Focus 2020;6:653)
Gross description
- Thickened bladder wall
Frozen section description
- Not usually diagnosed on frozen section
- Deceptively bland appearance; depth of invasion is key to distinguish from benign mimics, such as cystitis cystica glandularis, on the rare occurrence of frozen diagnosis (Eur Urol Focus 2020;6:653)
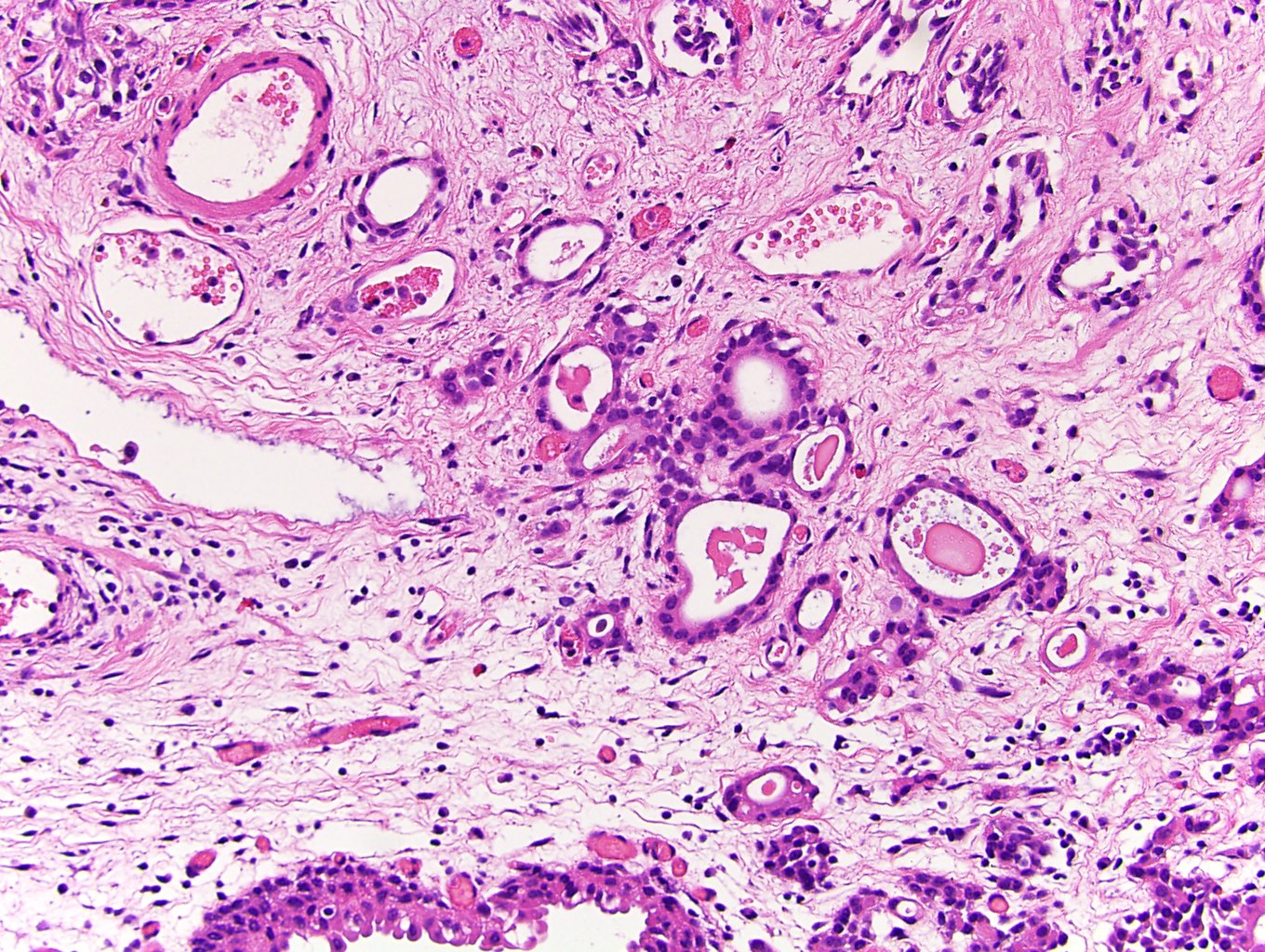
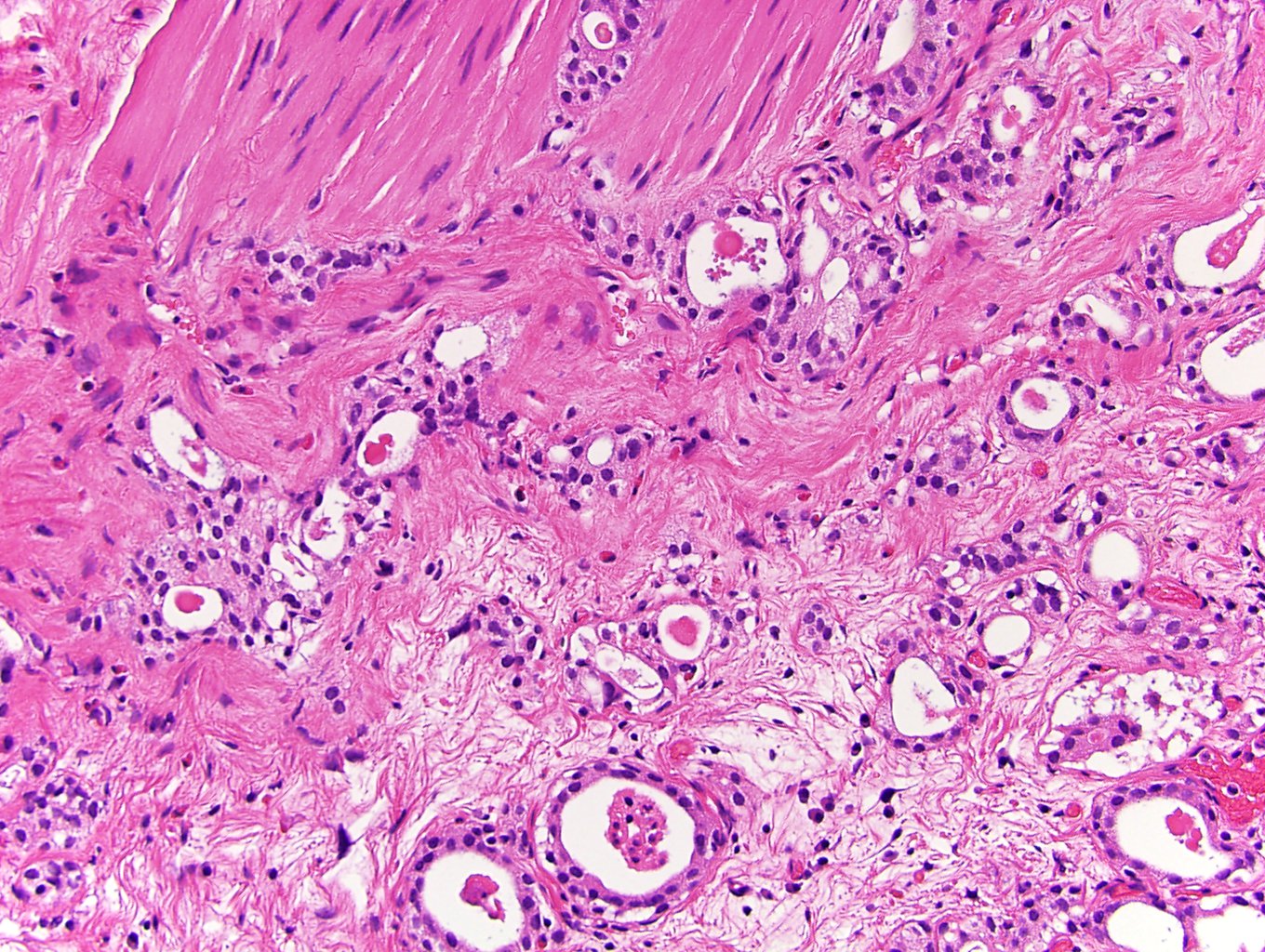
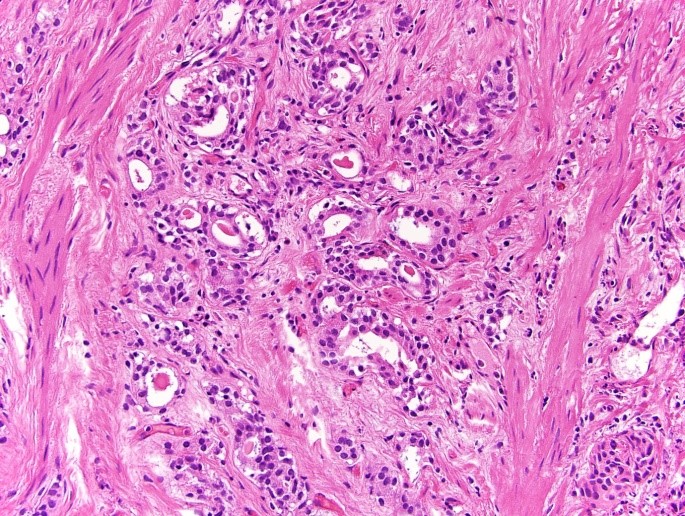
Microscopic (histologic) description
- Invasive urothelial carcinoma with microcysts, macrocysts or tubular structures, lined by single to multilayered cuboidal or flattened cells with minimal cytologic atypia (Histopathology 2019;74:77)
- Microcysts are irregular in shape, deeply infiltrative and range in size from microscopic to up to 2 mm (Histopathology 2019;74:77)
- Has luminal granular eosinophilic secretions with necrotic cellular debris, sometimes mucinous material or a targetoid appearance (PAS+, Alcian blue+) (Mod Pathol 2009;22:S96, Arch Pathol Lab Med 2007;131:1244)
- May be focally calcified
- May be associated with nested variant of urothelial carcinoma
- May be associated with focal high grade conventional urothelial carcinoma in approximately 40% of cases (Histopathology 2019;74:77)
Microscopic (histologic) images
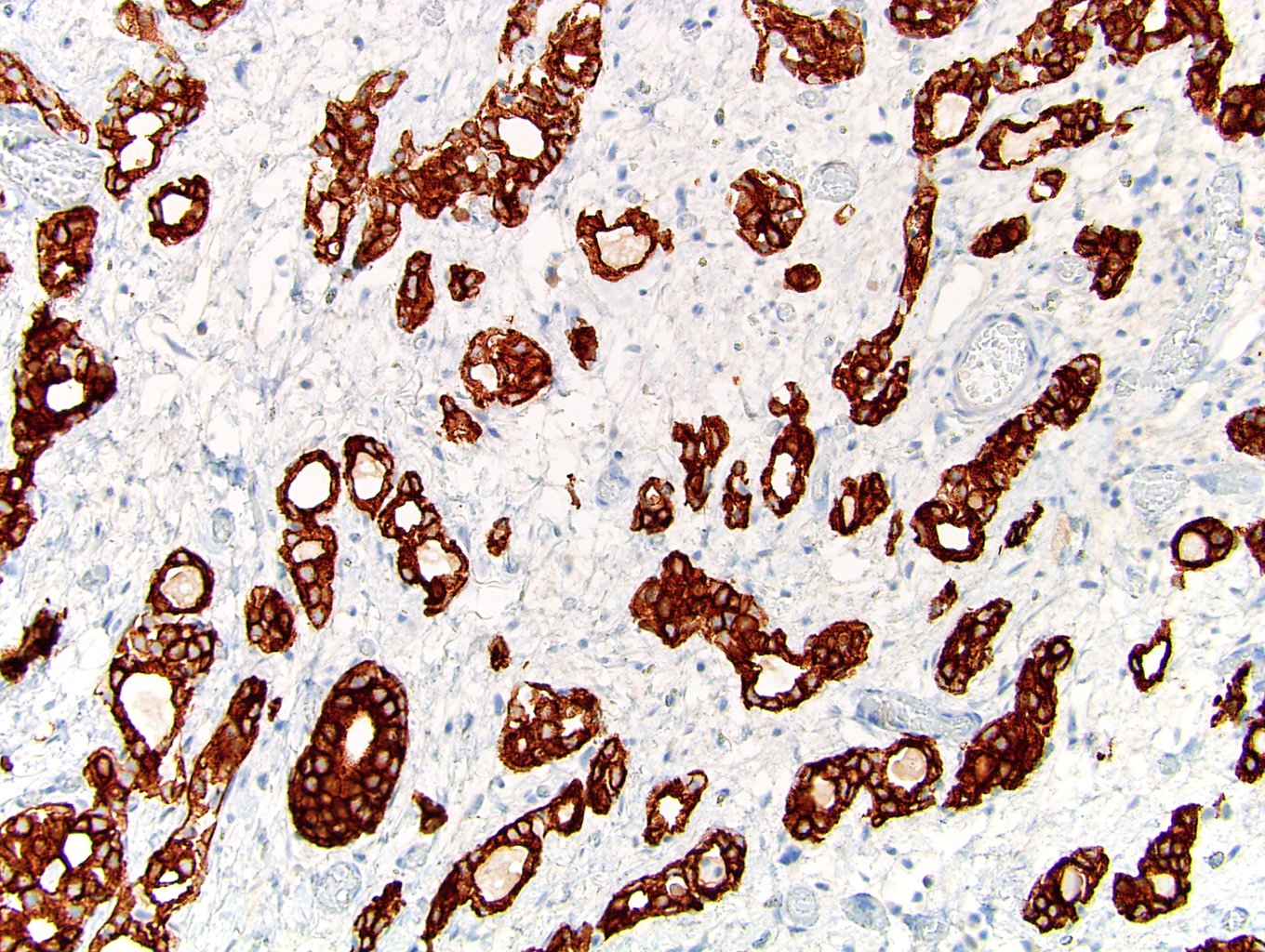
Positive stains
- Similar to other urothelial carcinomas: 34 beta E12, CK7, p63, uroplakin, thrombomodulin, GATA3, MUC5AC, CK20
- Intraluminal granular eosinophilic material may be PAS+ and Alcian blue+
- High p53
- Reference: Histopathology 2019;74:77
Molecular / cytogenetics description
- TERT promotor mutations (Histopathology 2019;74:77)
Sample pathology report
- Bladder, transurethral resection:
- Invasive high grade urothelial carcinoma with microcystic component (40%)
- Invasive of muscularis propria (pT2)
- Angiolymphatic invasion absent
Differential diagnosis
- Cystitis glandularis or cystitis cystica:
- More lobular growth pattern and regularly sized cystic structures rather than an infiltrative growth pattern and marked variability in size and shape of cystic structures
- Also cytologically bland (Mod Pathol 2009;22:S96)
- Adenocarcinoma, primary or metastatic:
- More marked atypia, mitotic activity, necrosis
- Site specific immunoprofile differentiates
- Nephrogenic adenoma:
- Circumscribed growth rather than an invasive growth pattern
- Expresses AMACR, PAX8 and PAX2 (Arch Pathol Lab Med 2007;131:1244, Intensive Care Med 1992;18:S35)
- Does not express p63
- Prostatic adenocarcinoma, Gleason 3 + 3:
Board review style question #1
A 40 year old man presents with gross hematuria, abdominal pain and bladder wall thickening on CT scan. He undergoes transurethral resection of bladder tumor (see above image). Which immunohistochemical profile would support the diagnosis of urothelial carcinoma with microcystic features?
- PAX8- / GATA3- / CK7+ / PSA+
- PAX8- / GATA3+ / CK7+ / p53 wild type / PSA-
- PAX8- / GATA3+ / CK7+ / p53+ / PSA-
- PAX8+ / GATA3- / CK7- / PSA-
Board review style answer #1
C. PAX8- / GATA3+ / CK7+ / p53+ / PSA-. This immunohistochemical profile is one that is classic to conventional urothelial carcinomas and shared by microcystic variant.
Comment Here
Reference: Microcystic urothelial carcinoma-invasive
Comment Here
Reference: Microcystic urothelial carcinoma-invasive