Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Umphress B, Maniar KP. Mural nodules in mucinous cystic neoplasms. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumormuralnodules.html. Accessed August 26th, 2025.
Definition / general
- Grossly circumscribed nodules, most associated with primary ovarian mucinous neoplasms (less frequently other ovarian tumor types)
- May be microscopically invasive but still separate / distinct from the associated mucinous tumor (Int J Gynecol Pathol 1994;13:62)
Essential features
- May be reactive (sarcoma-like), benign neoplastic (leiomyomatous) or malignant (anaplastic carcinoma, sarcoma, carcinosarcoma)
- Associated mucinous tumor may be benign, borderline or malignant
- Can present a diagnostic challenge as the discrimination between truly malignant versus reactive mural nodules can be difficult
Terminology
- General term: ovarian mucinous neoplasm with mural nodule
- Various classification schema used (Int J Gynecol Pathol 1994;13:62, Cancer 1979;44:1332, Am J Surg Pathol 2008;32:383):
- Reactive (sarcoma-like mural nodules)
- Pleomorphic and epulis-like
- Pleomorphic and spindle celled
- Giant cell histiocytic
- Benign neoplastic
- Malignant neoplastic
- Anaplastic carcinoma: rhabdoid, spindled or pleomorphic
- Sarcoma
- Carcinosarcoma
- Reactive (sarcoma-like mural nodules)
ICD coding
Epidemiology
- Females of varying ages and parity
- Sarcomatous nodules generally in older patients compared to sarcoma-like nodules (Am J Surg Pathol 2002;26:1467)
- Sarcoma-like mural nodules: 18 - 83 years (mean 39 years) (Cancer 1979;44:1332, Am J Surg Pathol 2002;26:1467)
- Sarcomatous mural nodules: 49 - 72 years (mean 61 years) (Int J Gynecol Pathol 1994;13:62)
- Anaplastic carcinoma mural nodules: 15 - 93 years (mean 44 years) (Am J Surg Pathol 2008;32:383)
- Carcinosarcoma mural nodules: 27 - 44 years (mean 33 years) (Int J Gynecol Pathol 1994;13:62)
Sites
- Ovary (almost always unilateral)
Pathophysiology / etiology
- Unclear histogenesis; however, may evolve through divergent differentiation of mucinous neoplasm or through a collision phenomenon (Int J Gynecol Pathol 2015;34:19)
- Sarcoma-like mural nodules: likely common histogenesis for different subtypes, favored to be reactive and of histiocytic origin (Cancer 1979;44:1332, Am J Surg Pathol 2002;26:1467)
- Malignant mural nodules clonally related to accompanying mucinous tumor and may represent dedifferentiation (Am J Surg Pathol 2017;41:1261)
- Targeted next generation sequencing has shown a clonal relationship between carcinomatous mural nodules and the ovarian mucinous tumor, indicating a dedifferentiation process (Am J Surg Pathol 2017;41:1261)
Clinical features
- Majority of patients present with abdominal enlargement or pain (Cancer 1979;44:1332, Cancer 1979;44:1327, Am J Surg Pathol 2008;32:383)
- Less common presentations: menometrorrhagia, vomiting, intestinal obstruction, vaginal bleeding (Cancer 1979;44:1332, Am J Surg Pathol 2002;26:1467, Am J Surg Pathol 1991;15:1055)
- Stage at presentation:
- Sarcoma-like mural nodules: all FIGO stage Ia (Cancer 1979;44:1332, Am J Surg Pathol 2002;26:1467)
- Anaplastic carcinoma mural nodules: 68% stage I (Ia or Ic), 32% stage II or higher (Am J Surg Pathol 2008;32:383)
- Sarcomatous mural nodules: 60% stage I, 40% stage III or IV (Int J Gynecol Pathol 1994;13:62)
- Carcinosarcoma mural nodules: 75% stage I, 25% stage III (Int J Gynecol Pathol 1994;13:62)
Prognostic factors
- Sarcoma-like mural nodules behave in benign fashion with no effect on prognosis of associated mucinous tumor (Cancer 1979;44:1332, Am J Surg Pathol 2002;26:1467)
- Overt sarcoma and anaplastic carcinoma carry a much worse prognosis:
- For malignant mural nodules overall: 39% mortality (3 months to 1.5 years) (Am J Surg Pathol 2002;26:1467)
- Anaplastic carcinoma mural nodules: 33% mortality (median 8 months) (Am J Surg Pathol 2008;32:383)
- Sarcoma mural nodules: 67% mortality (within 4 years) (Int J Gynecol Pathol 1994;13:62)
- Among anaplastic carcinomas, FIGO stage is the only significant prognostic factor (stage Ia tumors do not necessarily carry an adverse prognosis) (Am J Surg Pathol 2008;32:383)
Case reports
- 18 and 34 year old women, both with osteosarcomatous mural nodules (Int J Gynecol Pathol 2015;34:369)
- 29 year old woman with solid mural leiomyoma associated with mucinous cystadenoma (Sultan Qaboos Univ Med J 2013;13:127)
- 30 year old woman with borderline mucinous tumor and sarcoma-like mural nodule (J Midlife Health 2014;5:192)
- 36 year old woman with anaplastic carcinoma mural nodule associated with rapid and fatal outcome (Int J Gynecol Pathol 2016;35:348)
- 45 year old woman with mural nodule of anaplastic spindle cell carcinoma within a mucinous borderline tumor (J Ovarian Res 2013;6:86)
- 48 year old woman with multifocal anaplastic carcinoma and sarcoma-like mural nodules (Int J Clin Exp Pathol 2013;6:1688)
- 48 year old woman with anaplastic carcinoma nodule and 60 year old woman with sarcomatous mural nodule (Medicine (Baltimore) 2017;96:e8636)
- 53 year old woman with borderline ovarian seromucinous cystic tumor and anaplastic carcinoma mural nodule (J Ovarian Res 2018;11:77)
Treatment
- Appropriate treatment depends on nature of mural nodule (benign / reactive versus malignant) as well as type of associated mucinous tumor and stage at presentation
- Tumors with sarcoma-like nodules can be followed after oophorectomy
- Staging surgery can be considered in malignant mural nodules, as well as systemic treatment (particularly in patients with extra-ovarian tumor spread)
- Reported cases have been variably treated (Cancer 1979;44:1332, Am J Surg Pathol 2002;26:1467, Am J Surg Pathol 2008;32:383)
- Surgical treatment: unilateral salpingo-oophorectomy, bilateral salpingo-oophorectomy or bilateral salpingo-oophorectomy with hysterectomy
- Subset of patients also underwent omentectomy, appendectomy or lymphadenectomy
- Subset of patients treated with adjuvant chemotherapy, especially in cases of malignant nodules
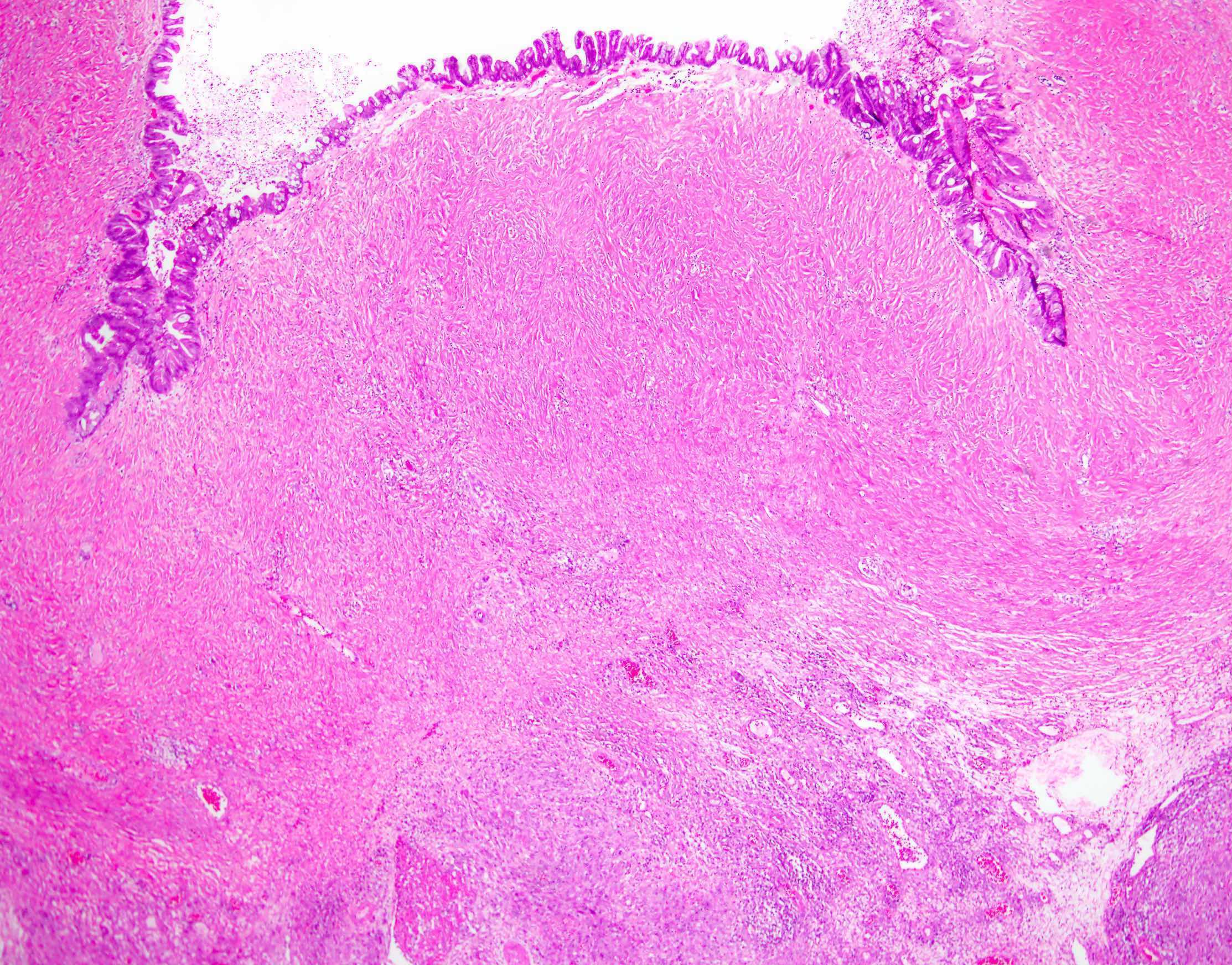
Gross description
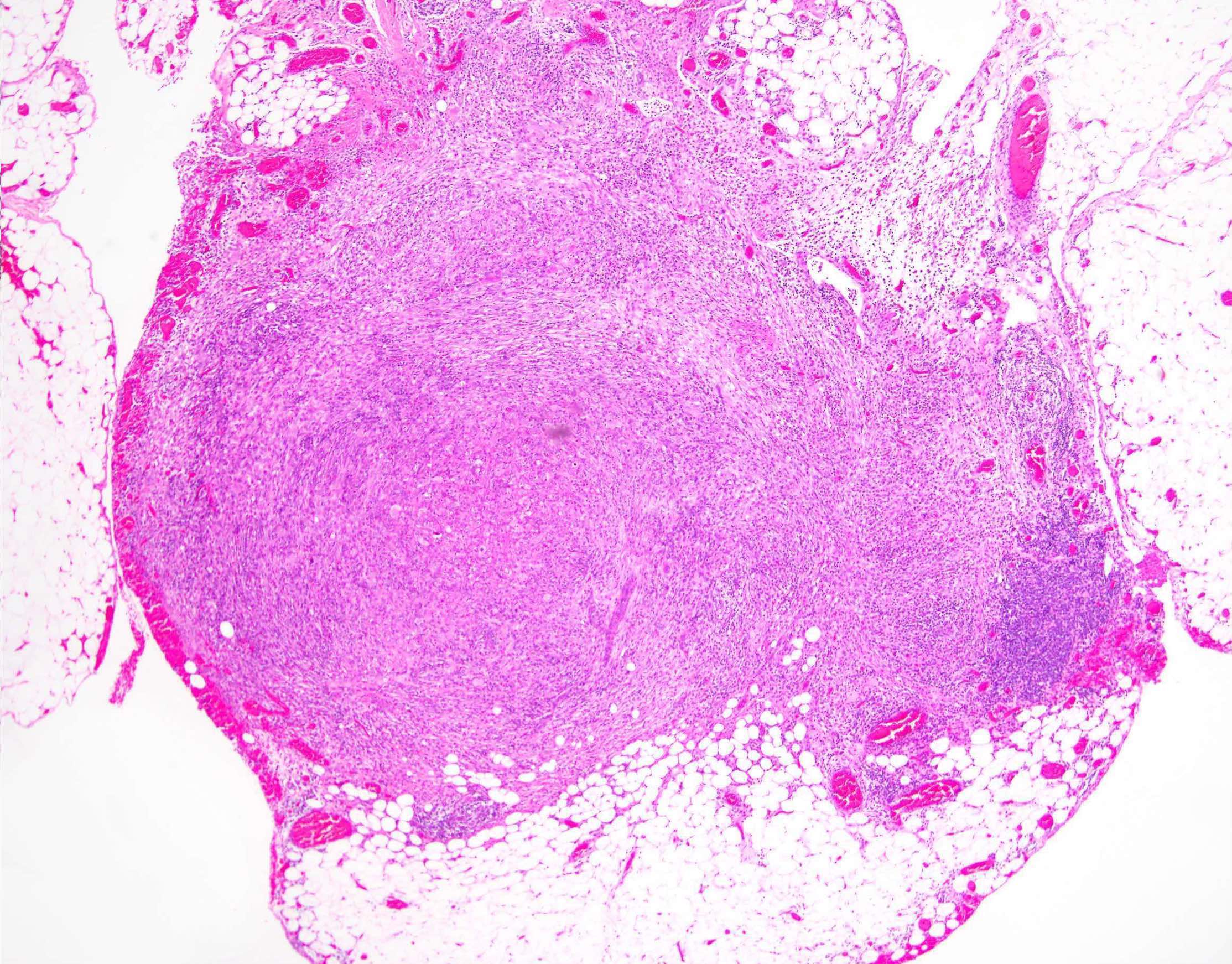
- Typically unilateral, large, unilocular or multilocular cystic mass with smooth external surface (7 - 62 cm, mean ~20 cm) (Am J Surg Pathol 2008;32:383, Cancer 1979;44:1332, Am J Surg Pathol 2002;26:1467)
- 1 or more well circumscribed nodules protruding into lumen
- May be dark brown, hemorrhagic and soft, or firm and yellow-tan; can have necrosis (Am J Surg Pathol 2008;32:383, Cancer 1979;44:1332, Cancer 1982;50:300)
Gross images
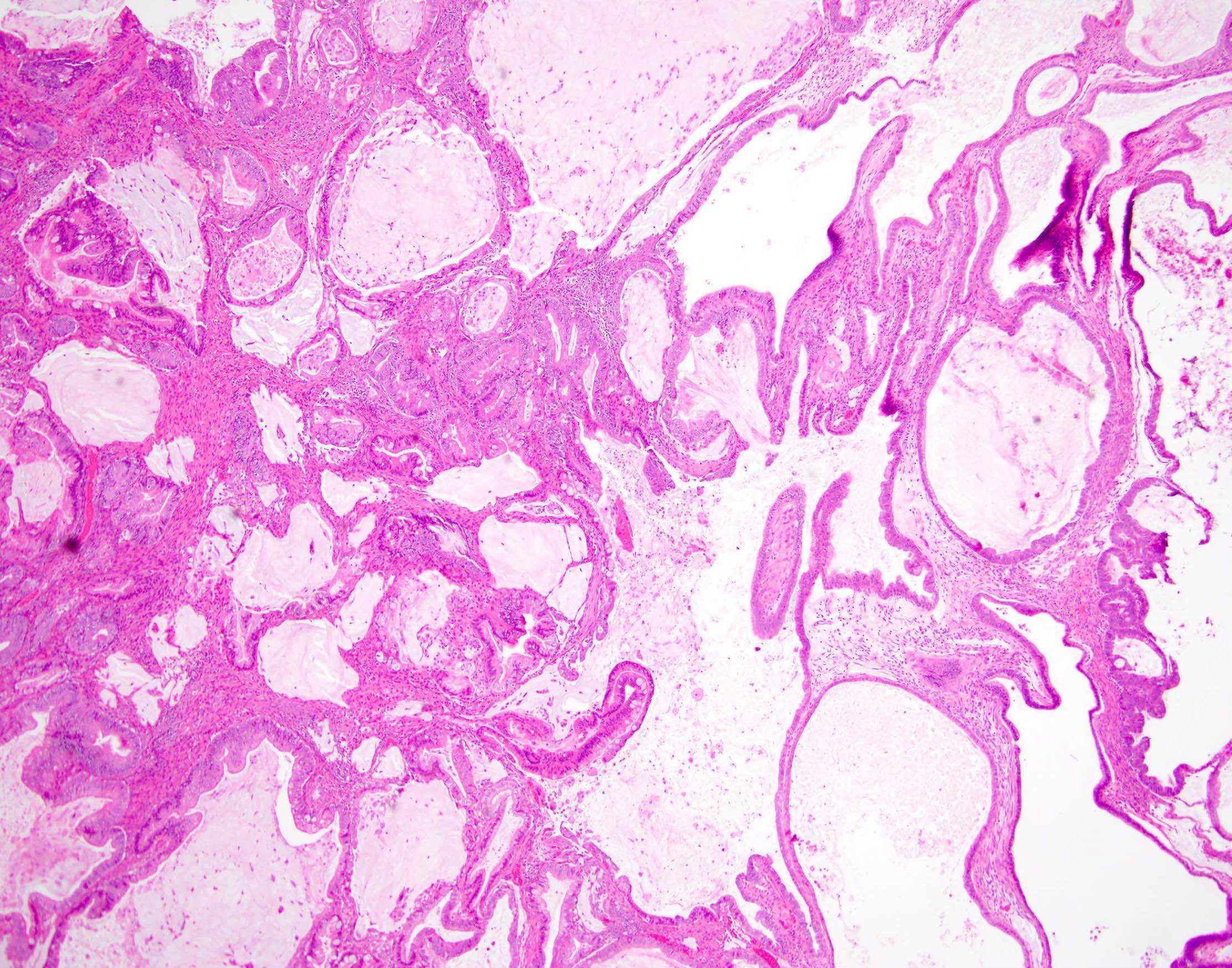
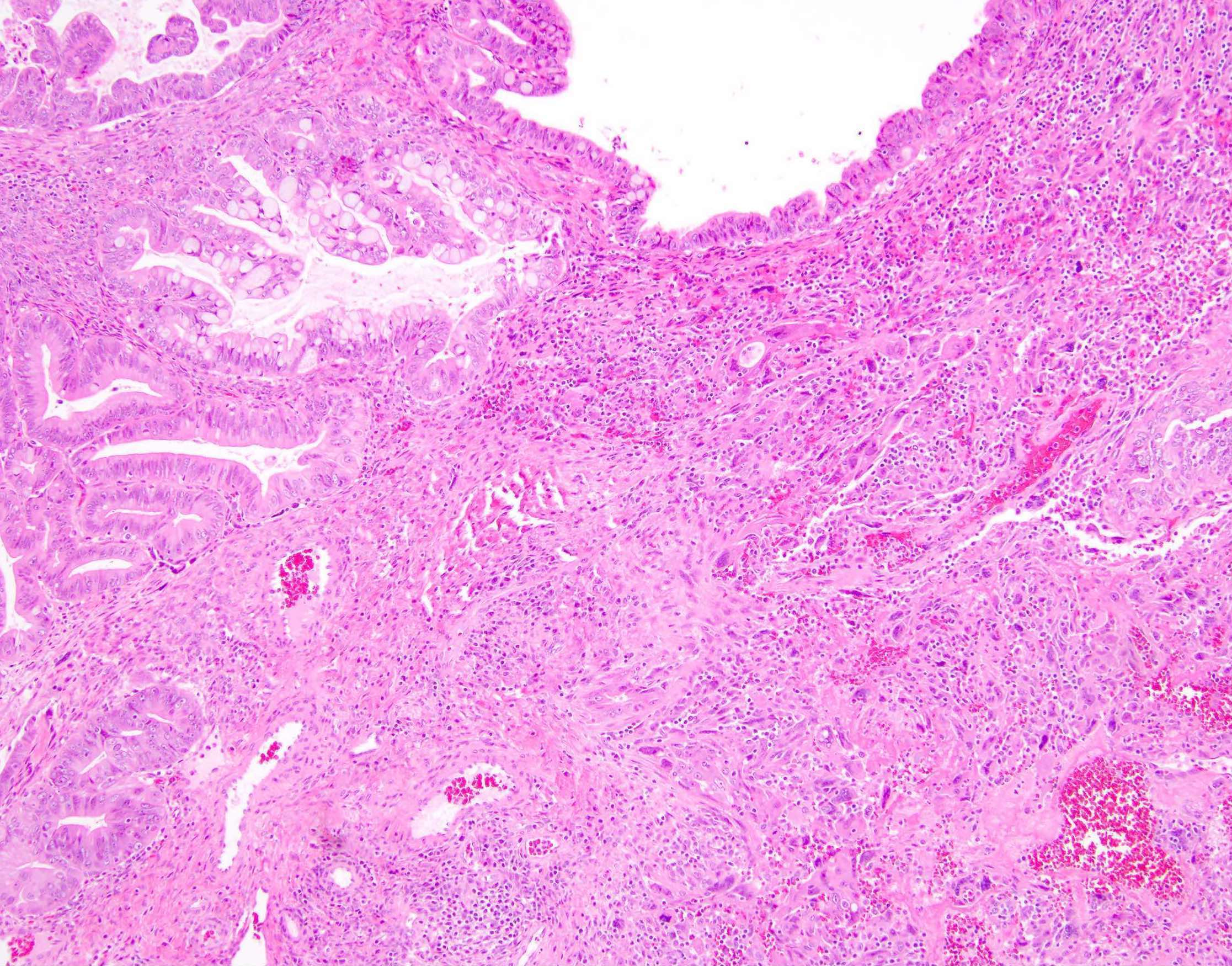
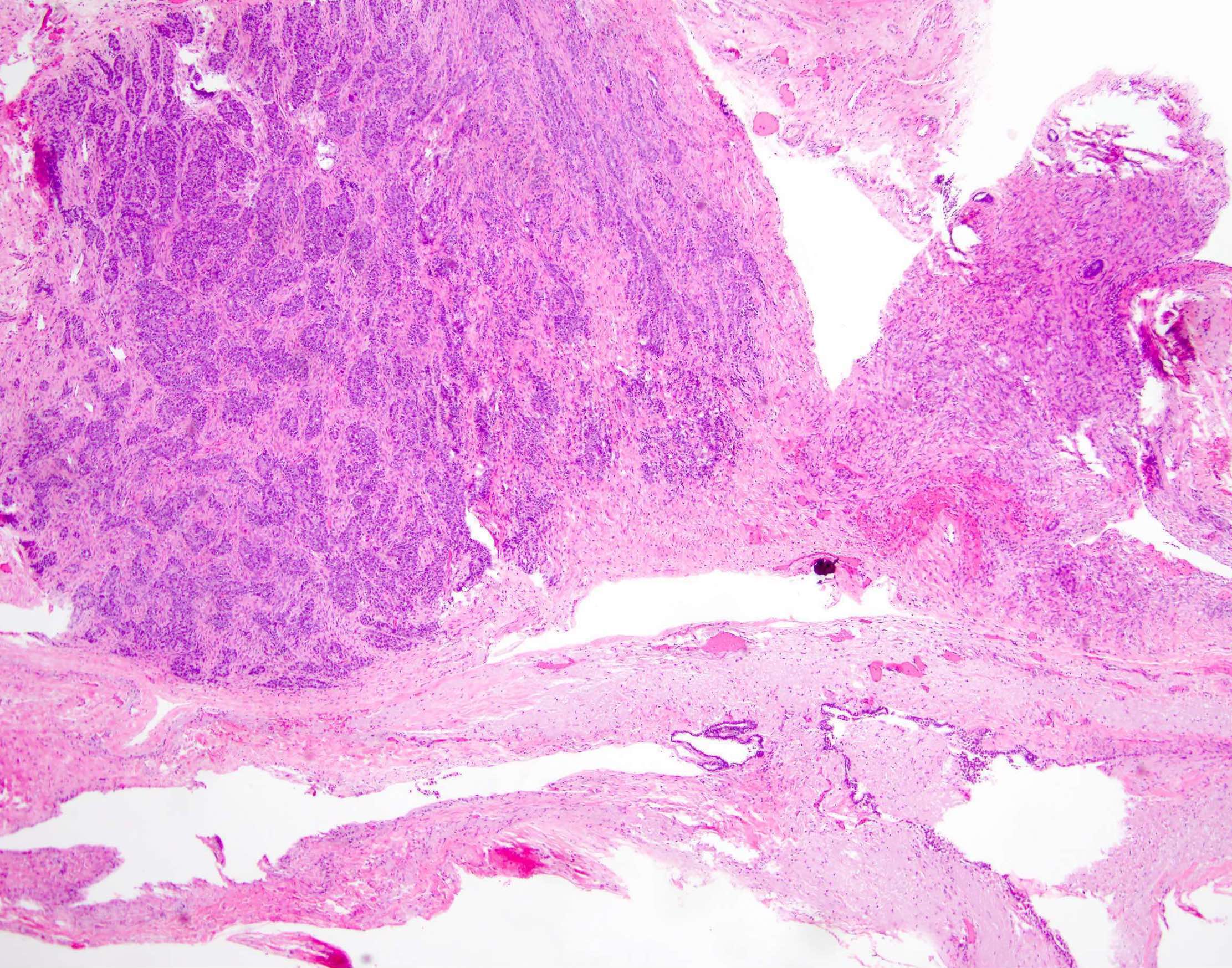
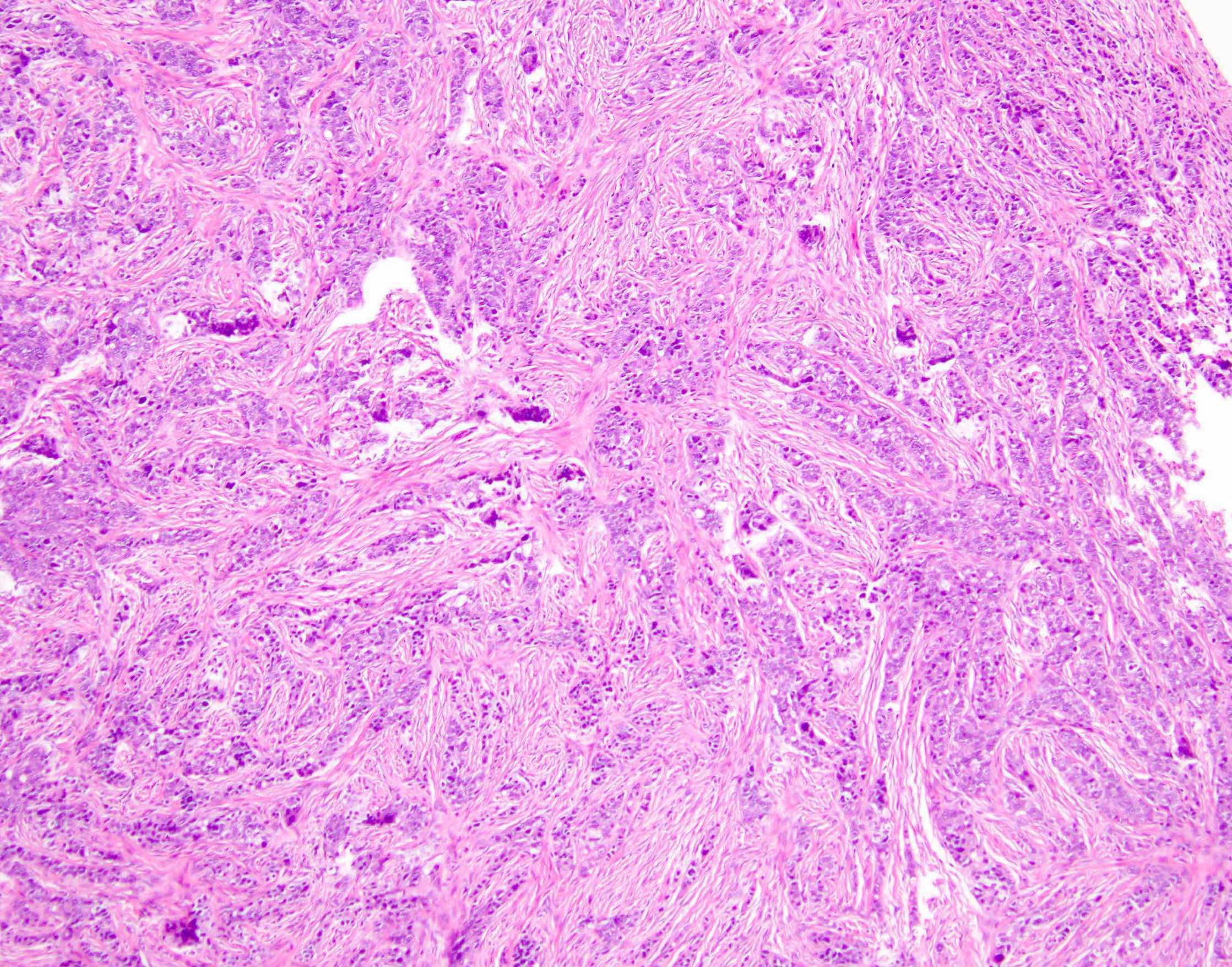
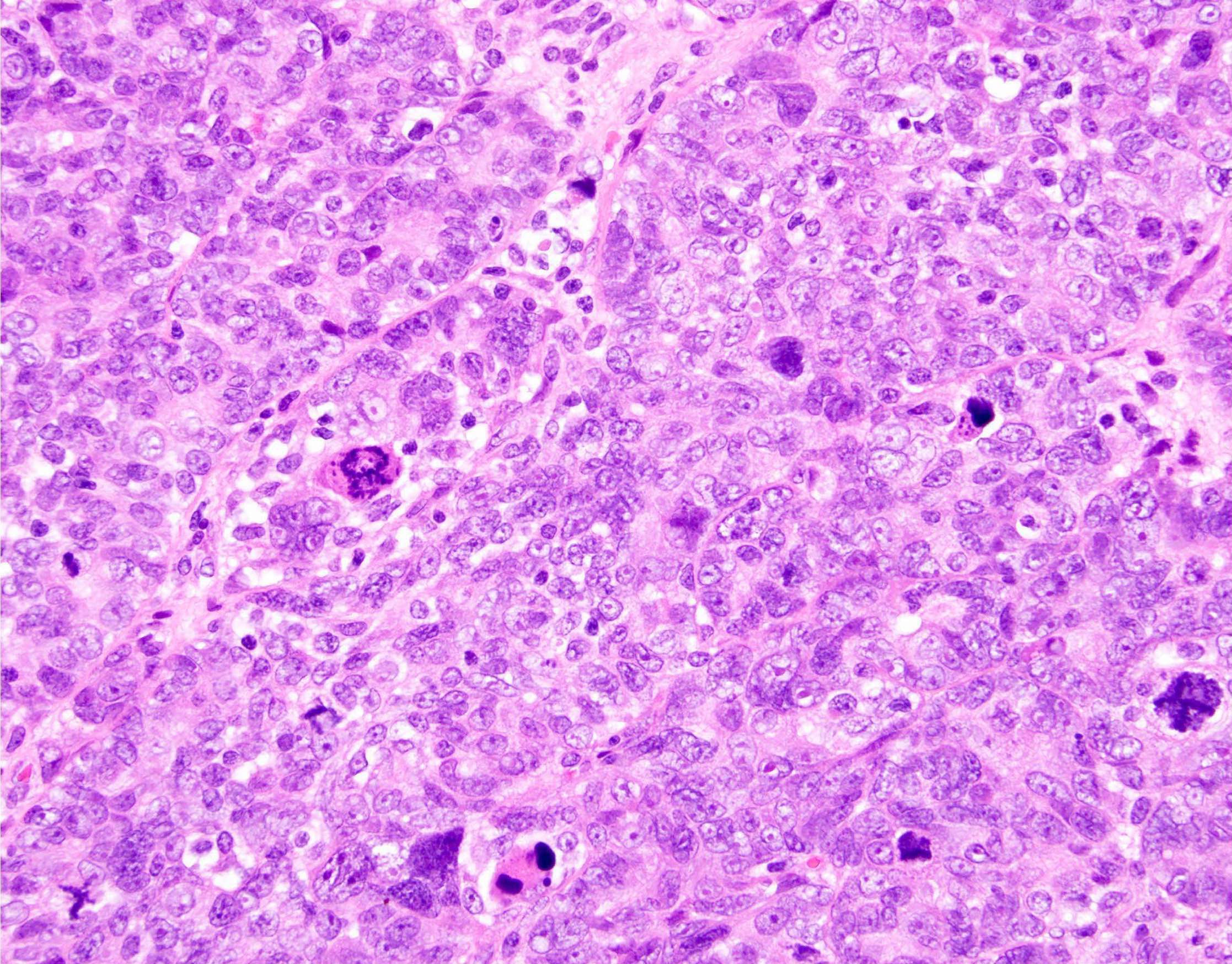
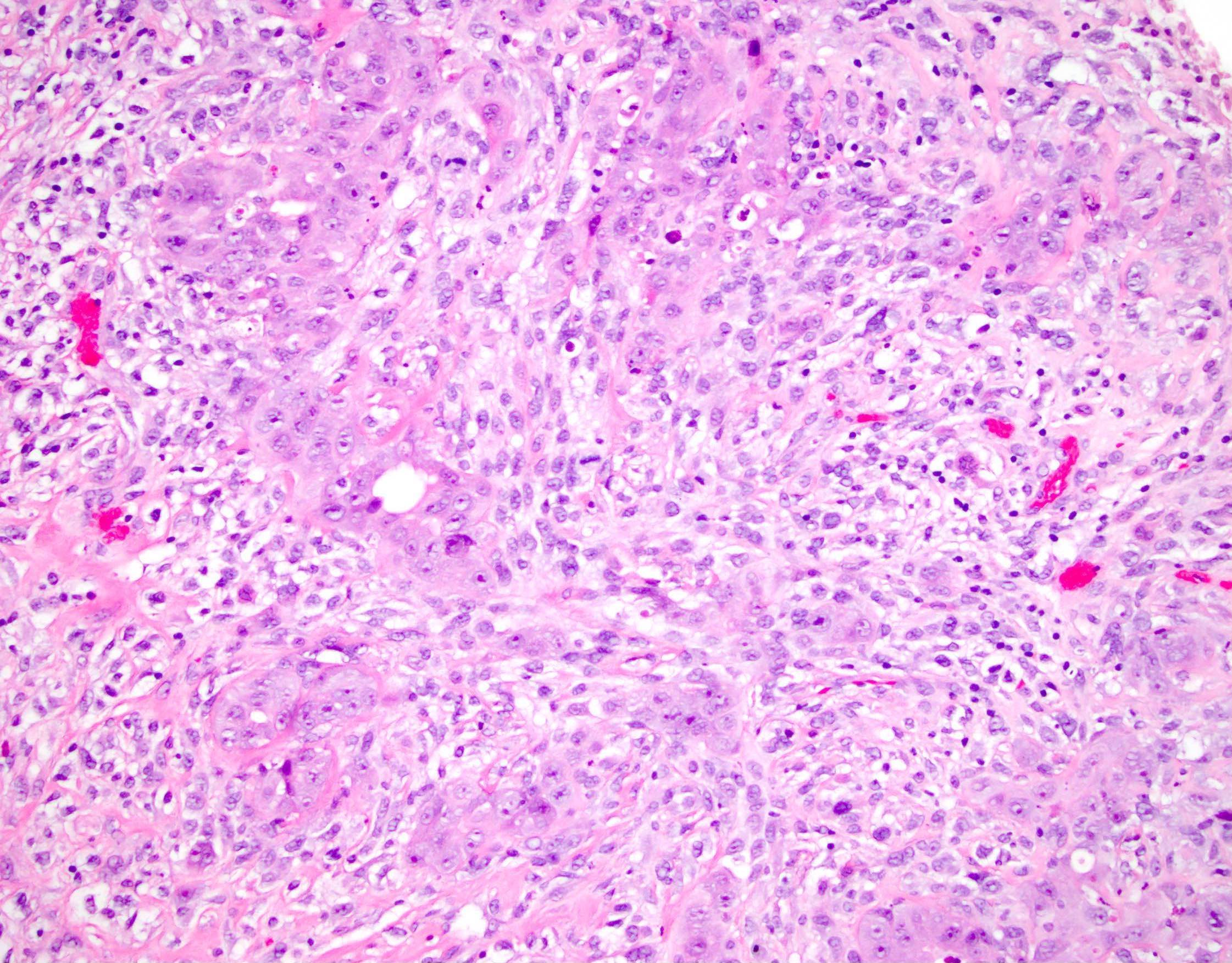
Microscopic (histologic) description
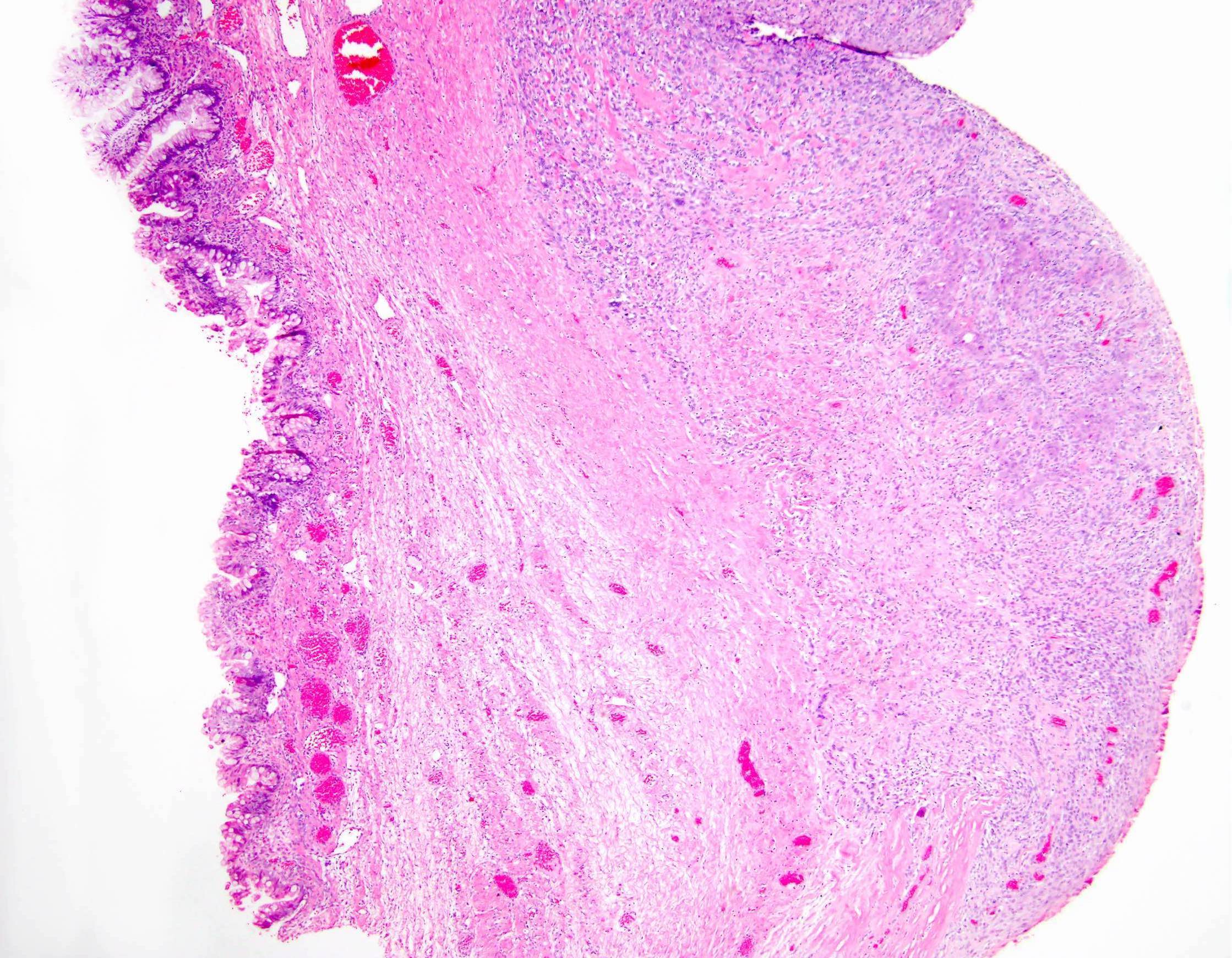
- Associated mucinous tumor: endocervical or intestinal type; cystadenoma, borderline tumor or carcinoma (Am J Surg Pathol 2002;26:1467, Cancer 1979;44:1332)
- Mural nodules: sharply circumscribed, separated from overlying cyst lining by a layer of hypocellular stroma (Am J Surg Pathol 2002;26:1467)
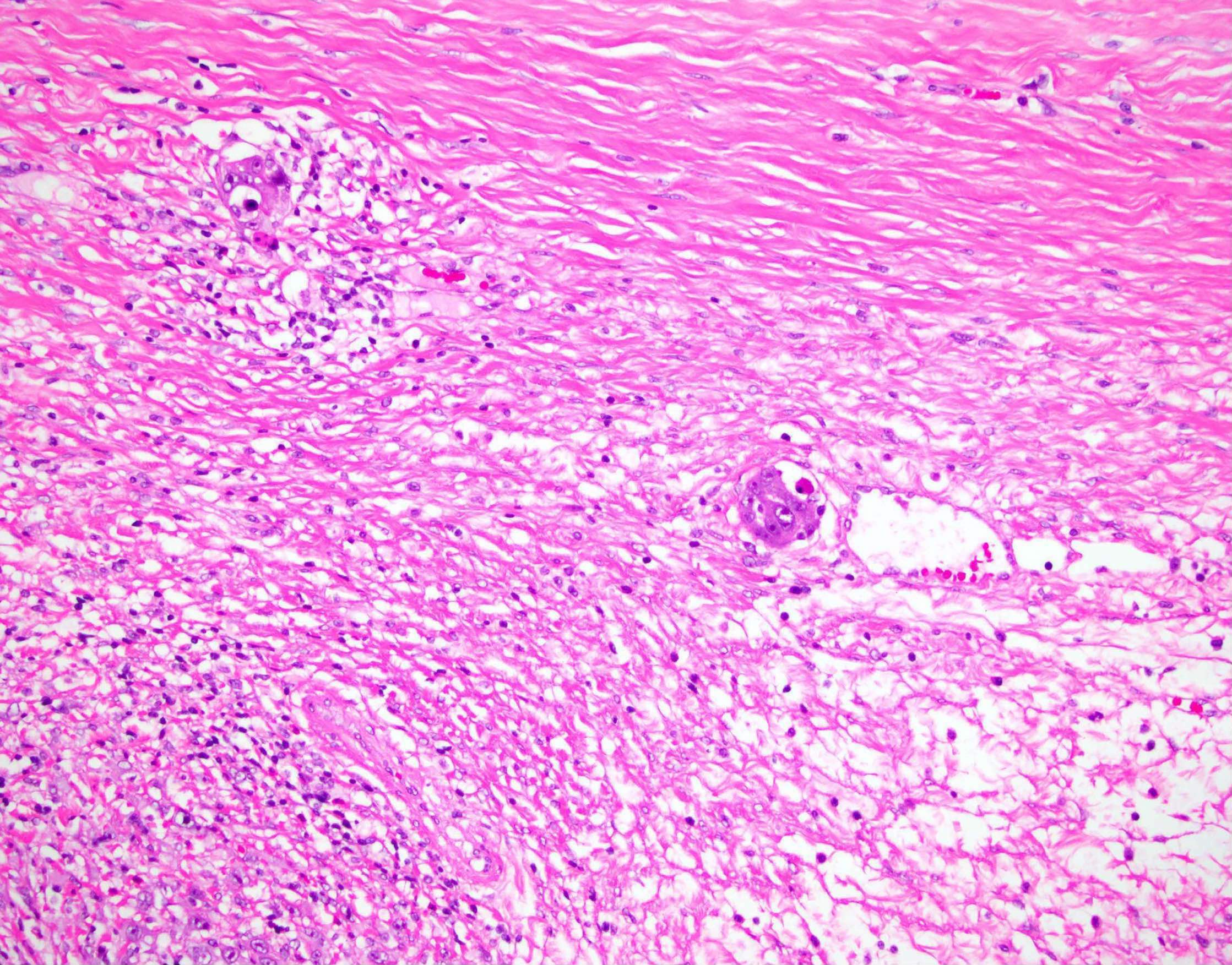
- Sarcoma-like mural nodules: 3 types (Cancer 1979;44:1332, Am J Surg Pathol 2002;26:1467)
- Pleomorphic and epulis-like type (resemble giant cell reparative granuloma / giant cell epulis of gingiva):
- Loose network of oval to spindled mononucleate cells with marked nuclear pleomorphism
- Uniformly distributed, multinucleated osteoclast-like giant cells, some with phagocytized red blood cells and debris
- Blood filled spaces
- Variable mitotic activity, can have atypical forms
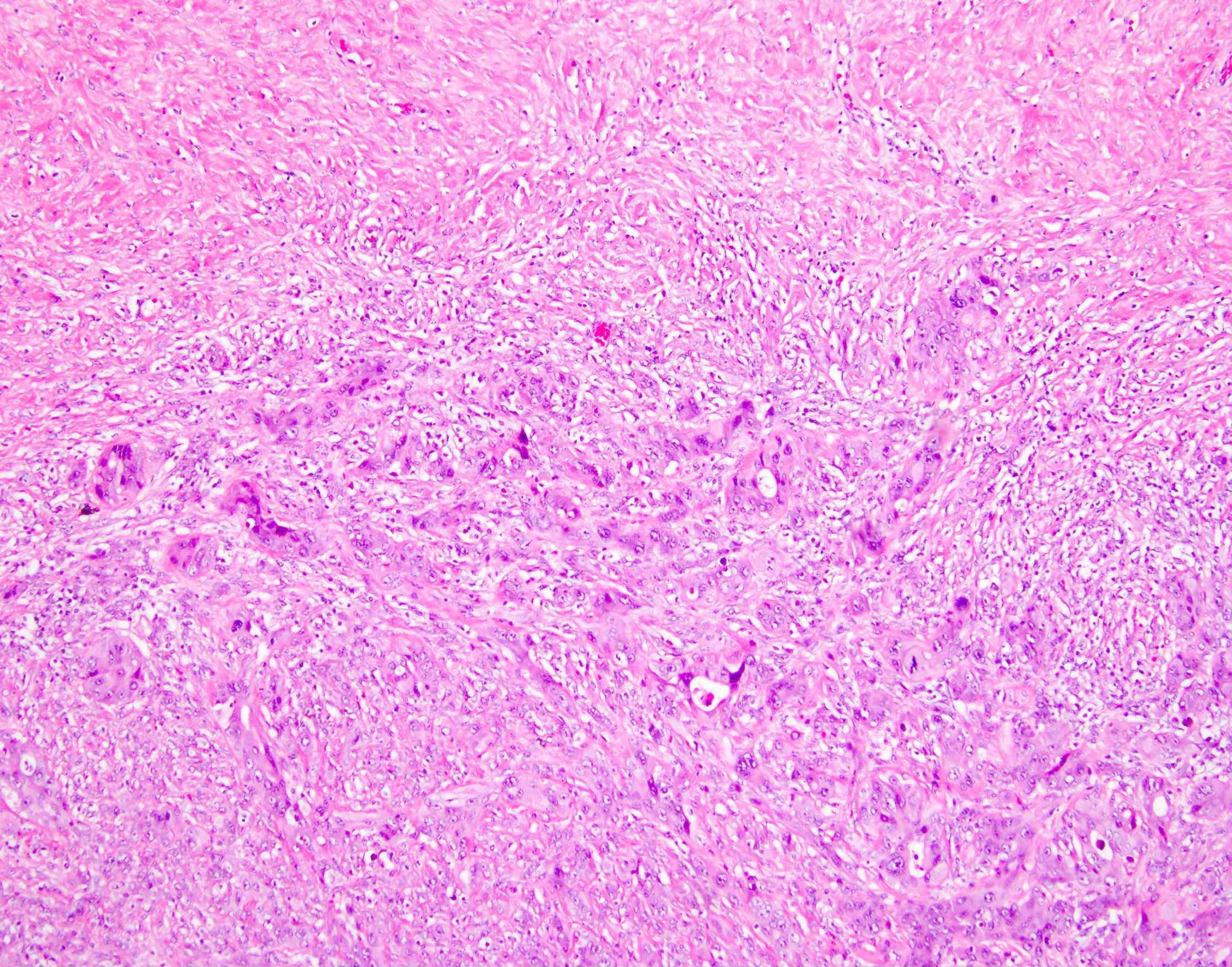
- Pleomorphic and spindle cell type:
- Fascicles of spindle cells with elongated hyperchromatic nuclei and prominent nucleoli
- Multinucleated giant cells similar to epulis-like type
- Diffuse extravasation of red blood cells; blood filled spaces
- Variable mitotic activity, can have atypical forms
- Mitotic index ranges from 5 to 10/10 HPF (usually in the most cellular areas)
- Giant cell histiocytic type:
- Round mononucleate giant cells in closely packed aggregates separated by delicate fibrous septa
- Cells with vesicular nuclei, ill defined borders, abundant ground glass eosinophilic cytoplasm and minute vacuoles
- No multinucleated giant cells as in other types
- Mitoses rare
- Variable but often marked mixed inflammatory infiltrate in all types of nodules
- Some nodules contain scattered cuboidal epithelium lined glands (likely entrapped)
- Most cases have multiple nodules within the tumor
- Associated mucinous tumor is carcinoma in 50% of cases, the rest being benign and borderline in nature
- Pleomorphic and epulis-like type (resemble giant cell reparative granuloma / giant cell epulis of gingiva):
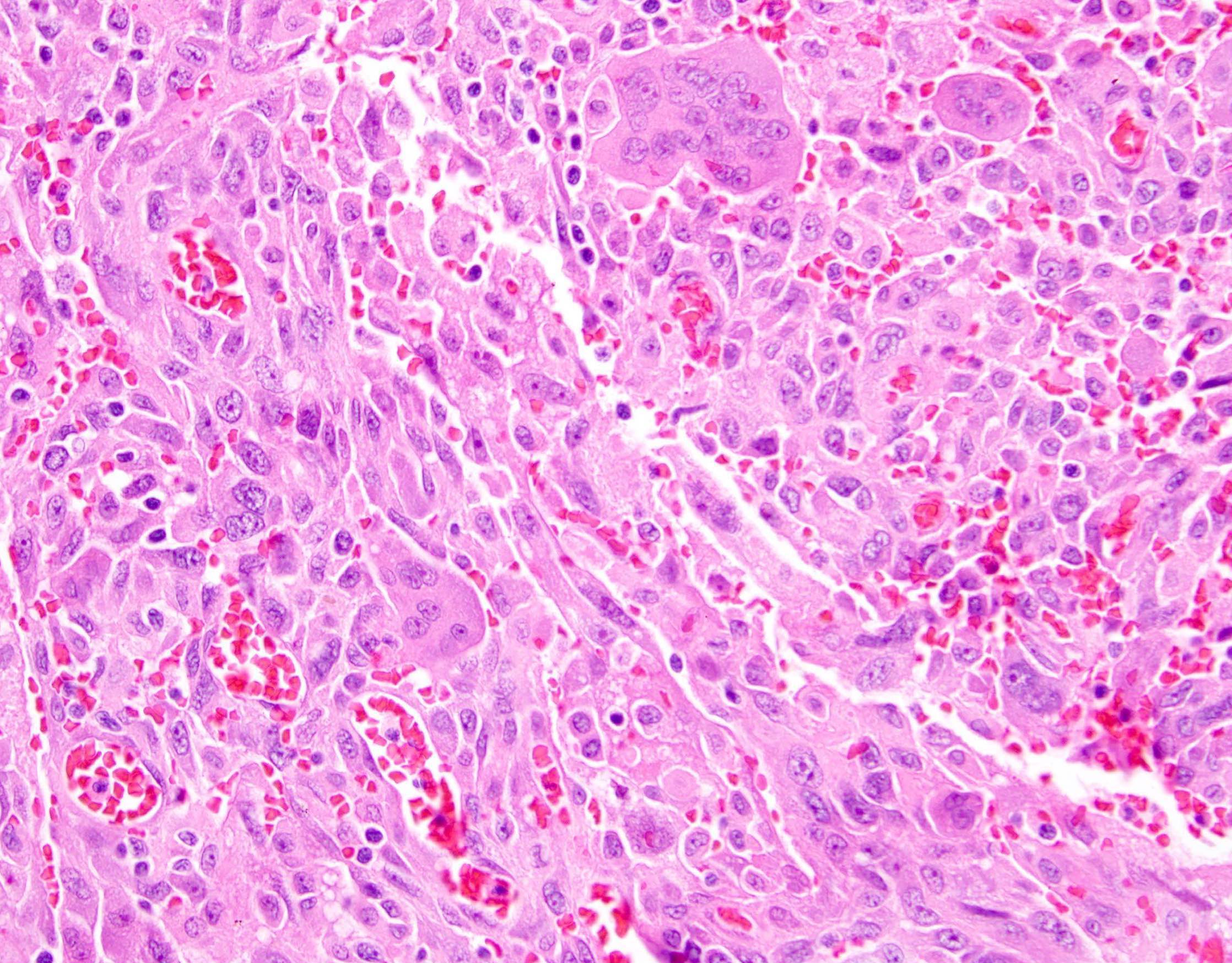
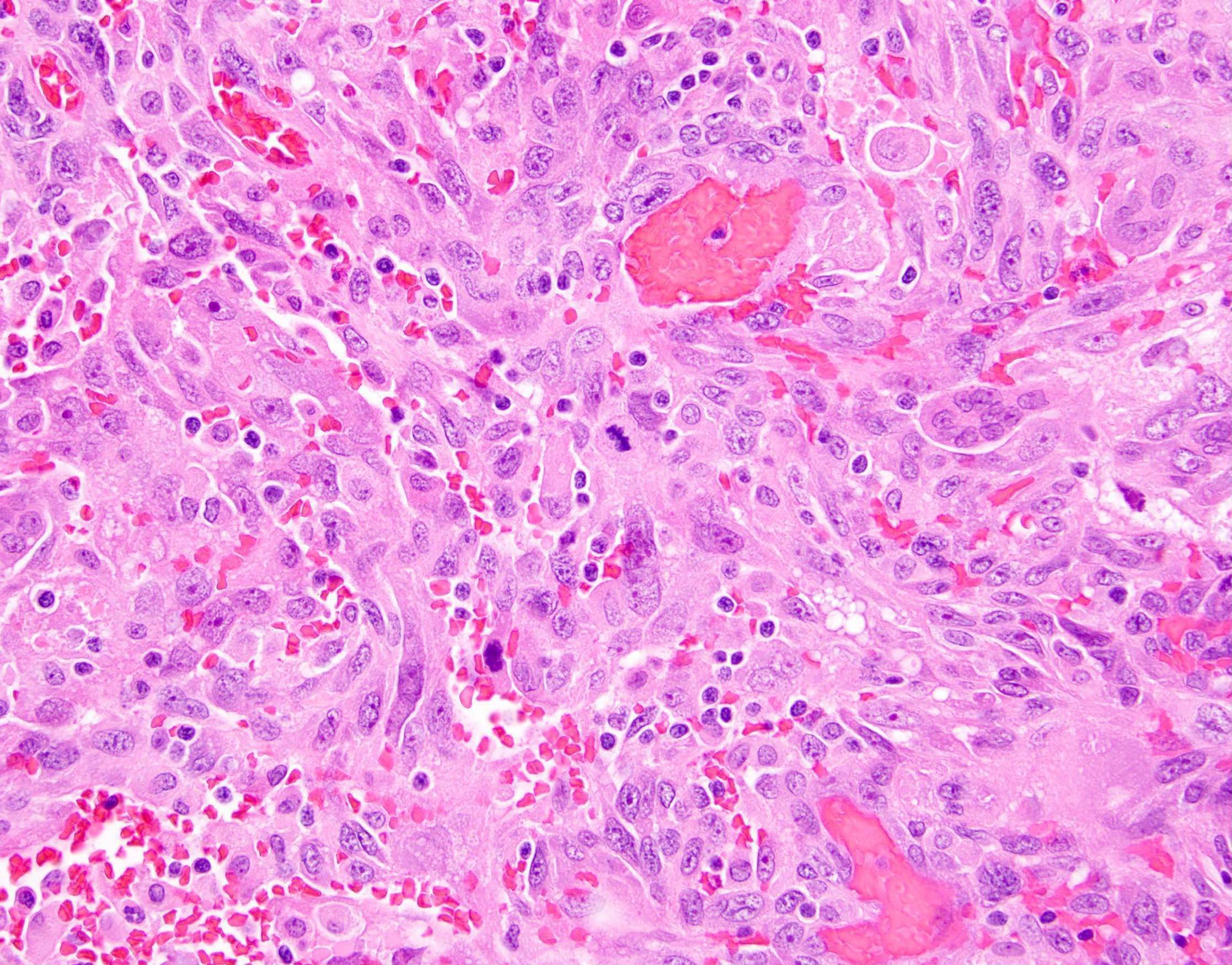
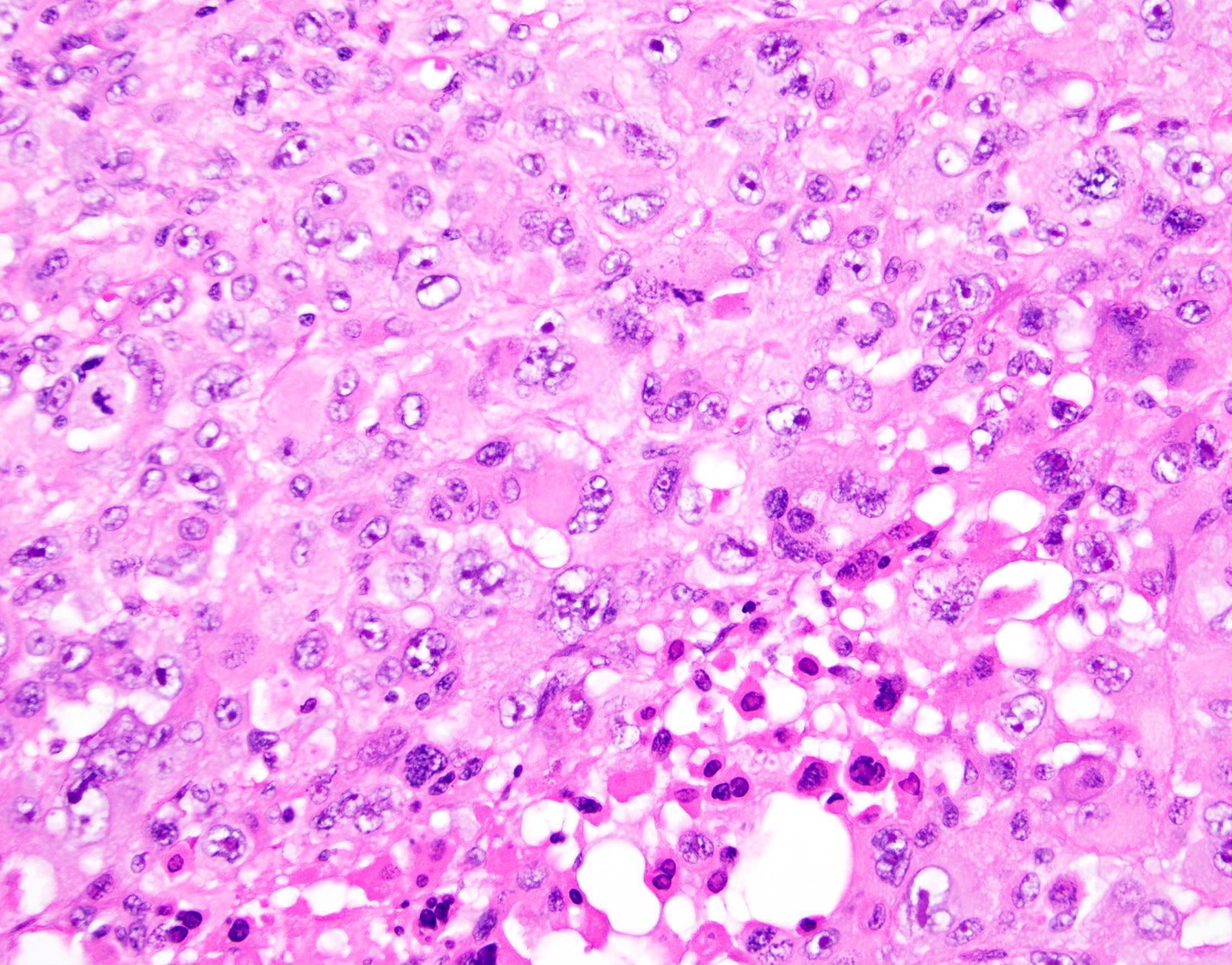
- Anaplastic carcinoma mural nodules (Am J Surg Pathol 2008;32:383):
- In general, characterized by poor circumscription, tumor infiltration into adjacent stroma and vessels, and necrosis
- Can have scattered multinucleated giant cells of epulis type
- Divided into 3 types:
- Rhabdoid: diffusely arranged cells with abundant bright pink cytoplasm and atypical, eccentrically placed nuclei
- Spindled: spindle cells with atypical vesicular nuclei and moderate eosinophilic cytoplasm, often in herringbone pattern; areas of obvious epithelial differentiation
- Pleomorphic: admixture of above types, more variegated
- Sarcomatous mural nodules: various types of sarcoma described, including fibrosarcoma, rhabdomyosarcoma, undifferentiated sarcoma (Cancer 1979;44:1327, Int J Gynecol Pathol 1994;13:62)
- Other mural nodule types described:
- Multiple or mixed types of nodules may occur in same tumor (Am J Surg Pathol 2002;26:1467)
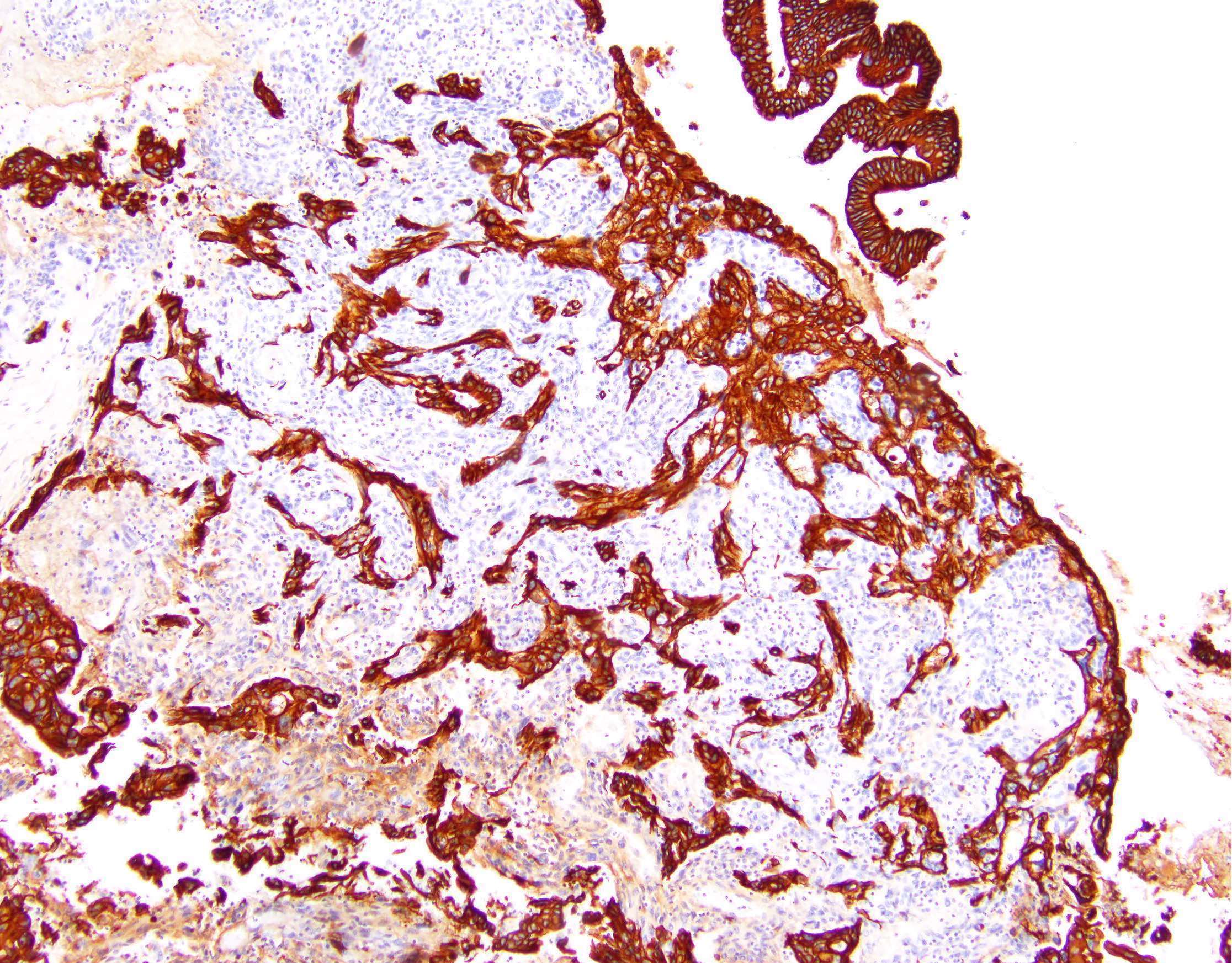
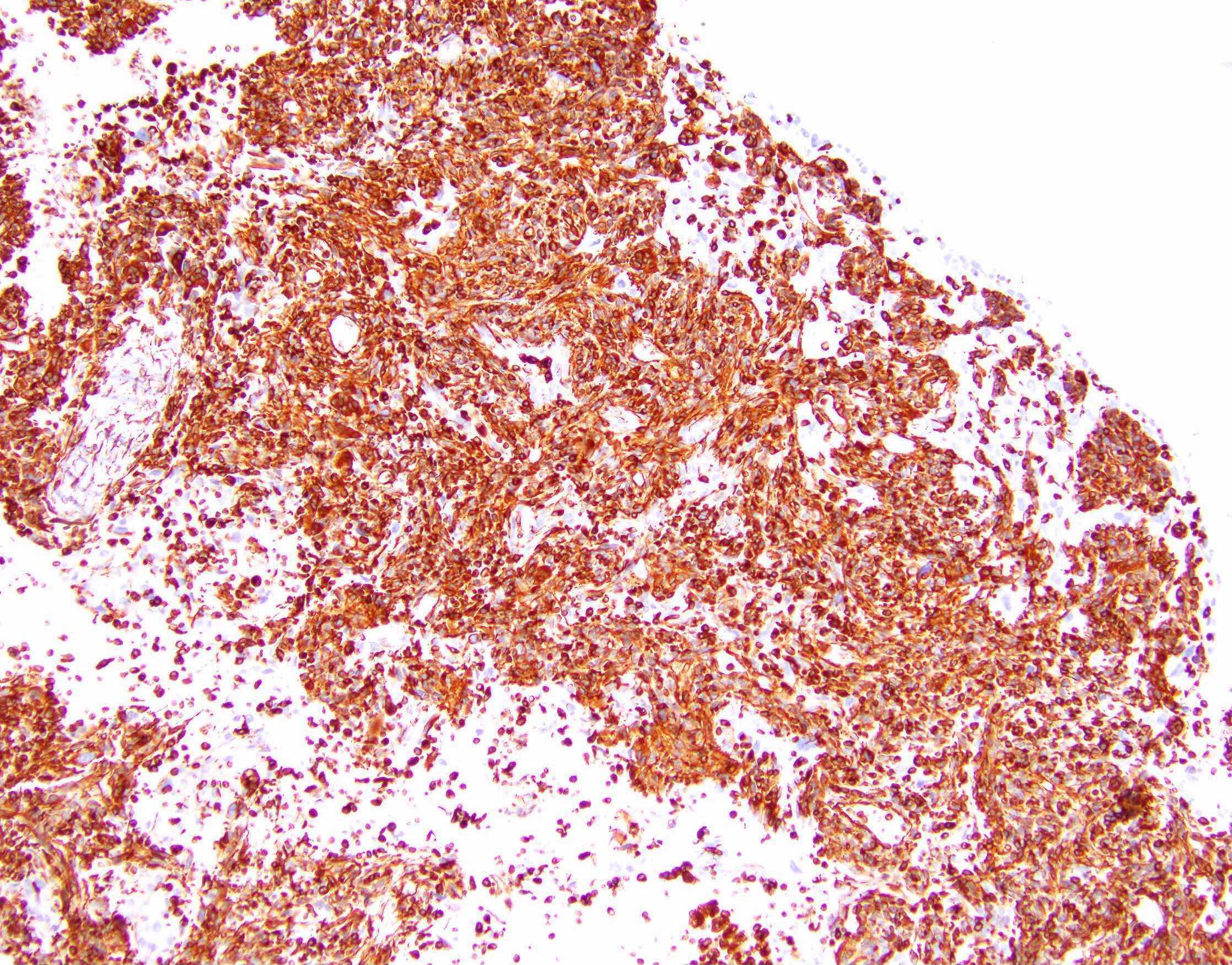
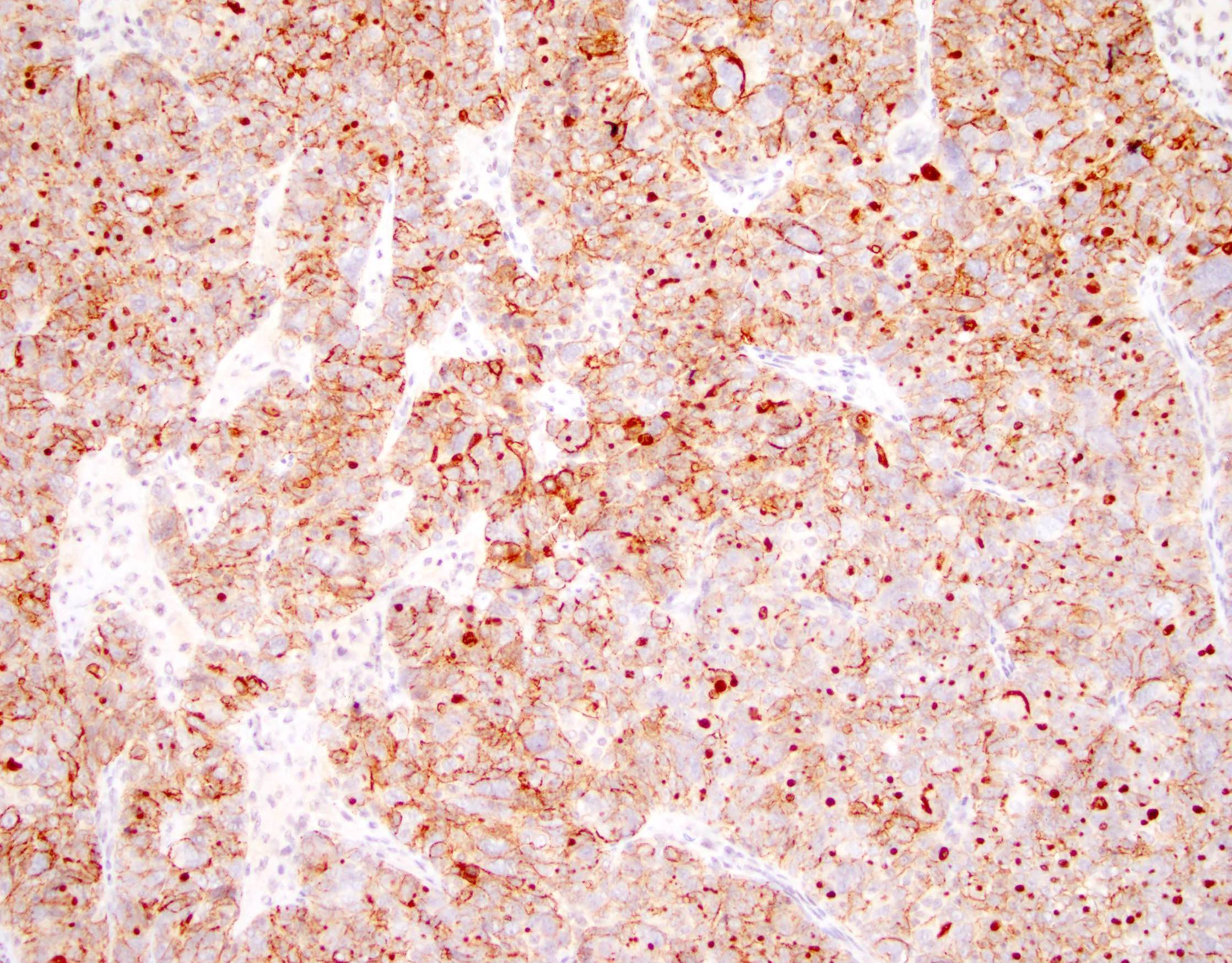
Microscopic (histologic) images
Contributed by Kruti P. Maniar, M.D. and Jian-Jun Wei, M.D.
Images hosted on other servers:
Positive stains
- Sarcoma-like mural nodules (Am J Surg Pathol 2002;26:1467):
- Vimentin
- CD68 (in most)
- Variable calretinin, smooth muscle actin, muscle specific actin
- Sarcomatous mural nodules: vimentin (Int J Gynecol Pathol 1994;13:62)
- Anaplastic carcinoma mural nodule:
- Pankeratin is positive in many cases (Int J Gynecol Pathol 1994;13:62)
- However, staining can be focal
- Moreover, a negative result does not exclude anaplastic carcinoma
- Leiomyomatous mural nodule: vimentin, desmin, smooth muscle actin, muscle specific actin (Int J Gynecol Pathol 1990;9:80, Am J Surg Pathol 1991;15:1055)
Negative stains
- Sarcoma-like mural nodules (Am J Surg Pathol 2002;26:1467):
- Pankeratin (but can have focal / weak expression)
- ALK, CD34, desmin
- Sarcomatous mural nodule: pankeratin (Int J Gynecol Pathol 1994;13:62)
- Leiomyomatous mural nodule: pankeratin (Int J Gynecol Pathol 1990;9:80, Am J Surg Pathol 1991;15:1055)
Molecular / cytogenetics description
- Recent next generation sequencing study found identical KRAS mutations in paired mucinous tumors and carcinomatous mural nodules (Am J Surg Pathol 2017;41:1261, Int J Gynecol Pathol 2015;34:19)
- Identical CDH1 and p53 mutations may also be seen in both components
- Unpaired p53 and PTEN mutations detected in 2 mural nodules
- One case of different KRAS mutations in sarcomatous mural nodule and associated mucinous tumor - suggests different clones of same tumor (Int J Gynecol Pathol 2014;33:186)
- Overall findings support neoplastic nature of carcinomatous mural nodules and clonal relationship with better differentiated mucinous tumor; acquisition of additional mutations within the mucinous neoplasm may result in transformation to anaplastic morphology (Am J Surg Pathol 2017;41:1261)
- Further larger molecular studies still needed to clearly elucidate the mechanisms and molecular alterations underlying the different types of mural nodules
Differential diagnosis
- Distinguishing different types of mural nodules:
- Sarcoma-like mural nodules versus anaplastic carcinoma:
- Irregular borders, epithelioid and cohesive areas are indicative of carcinoma
- Keratins are useful if positive; however, a negative result should be interpreted with caution (Virchows Arch A Pathol Anat Histopathol 1991;419:89)
- Sarcoma-like mural nodules versus true sarcomatous nodules:
- Immunohistochemistry not useful (both keratin-, vimentin+) (Virchows Arch A Pathol Anat Histopathol 1991;419:89)
- Features favoring true sarcoma: irregular or infiltrative nodule borders, monotonous population of spindle cells, significant nuclear atypia, evidence of vascular or stromal invasion, presence of atypical heterologous elements, older patient age, large nodule size (Virchows Arch A Pathol Anat Histopathol 1991;419:89, Int J Gynecol Pathol 1994;13:62)
- Sarcoma-like mural nodules versus anaplastic carcinoma:
- Other differential diagnoses:
- Carcinosarcoma: carcinoma component usually not mucinous; carcinoma and sarcoma elements more intimately admixed
- Pure sarcoma: no associated epithelial component
- Inflammatory myofibroblastic tumor: larger, less circumscribed, often immunohistochemical positivity for ALK
Practice question #1
Which of the following features favors diagnosis as a true sarcomatous mural nodule?
- Monotonous spindle cells with infiltration into stroma
- Positivity for CD68
- Positivity for pankeratin AE1 / AE3
- Presence of extravasated red blood cells and blood lakes
- Scattered osteoclast-like multinucleated giant cells
Practice answer #1
A. Monotonous spindle cells with infiltration into stroma
Comment Here
Reference: Mural nodules in mucinous cystic neoplasms
Comment Here
Reference: Mural nodules in mucinous cystic neoplasms
Practice question #2
60 year old patient had a 30 cm mucinous ovarian tumor removed. Gross exam demonstrated a 5 cm mural nodule. Based on the histologic image of the mural nodule (right) and the overlying mucinous tumor (left), which of the following is most likely true regarding tumor behavior?
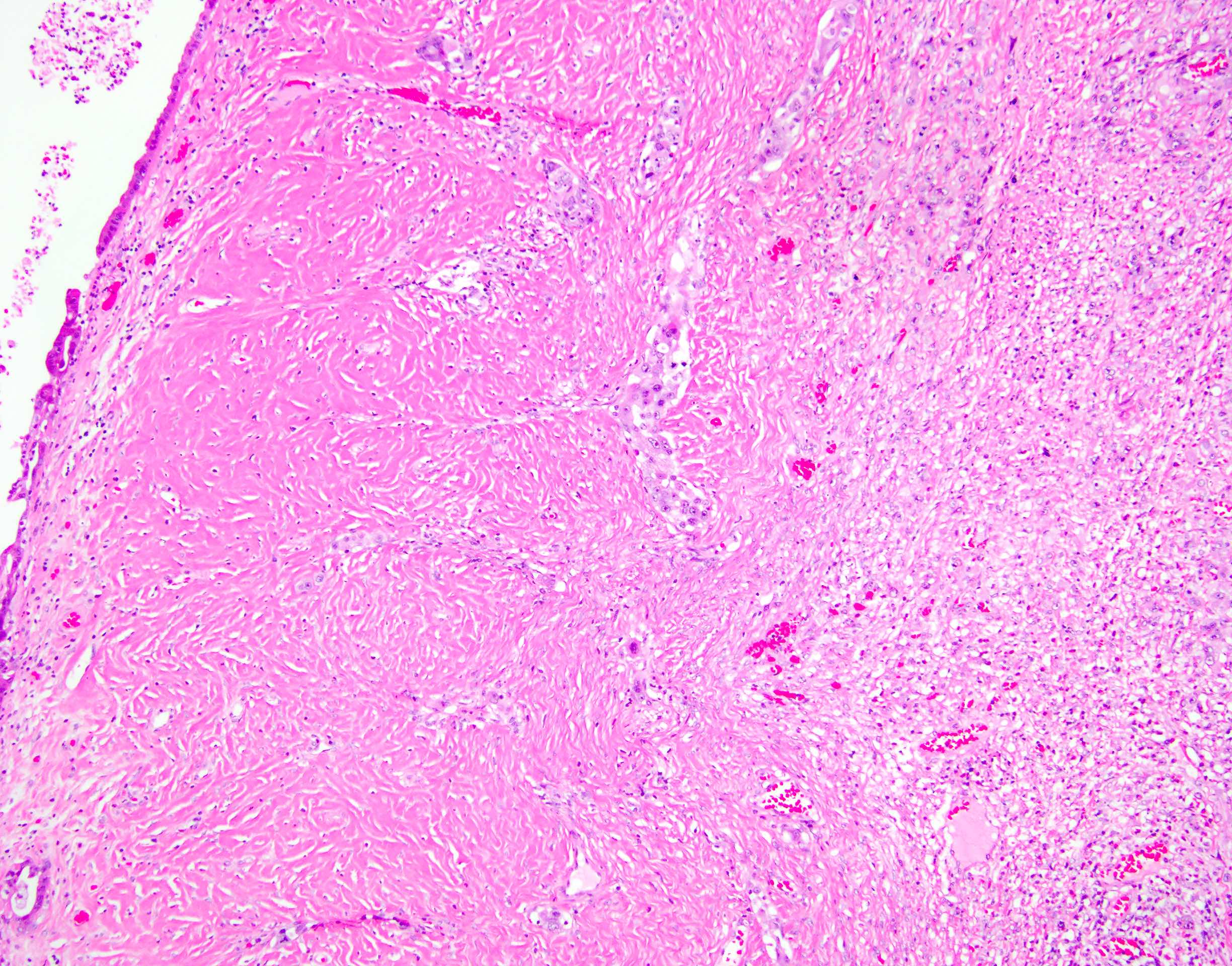
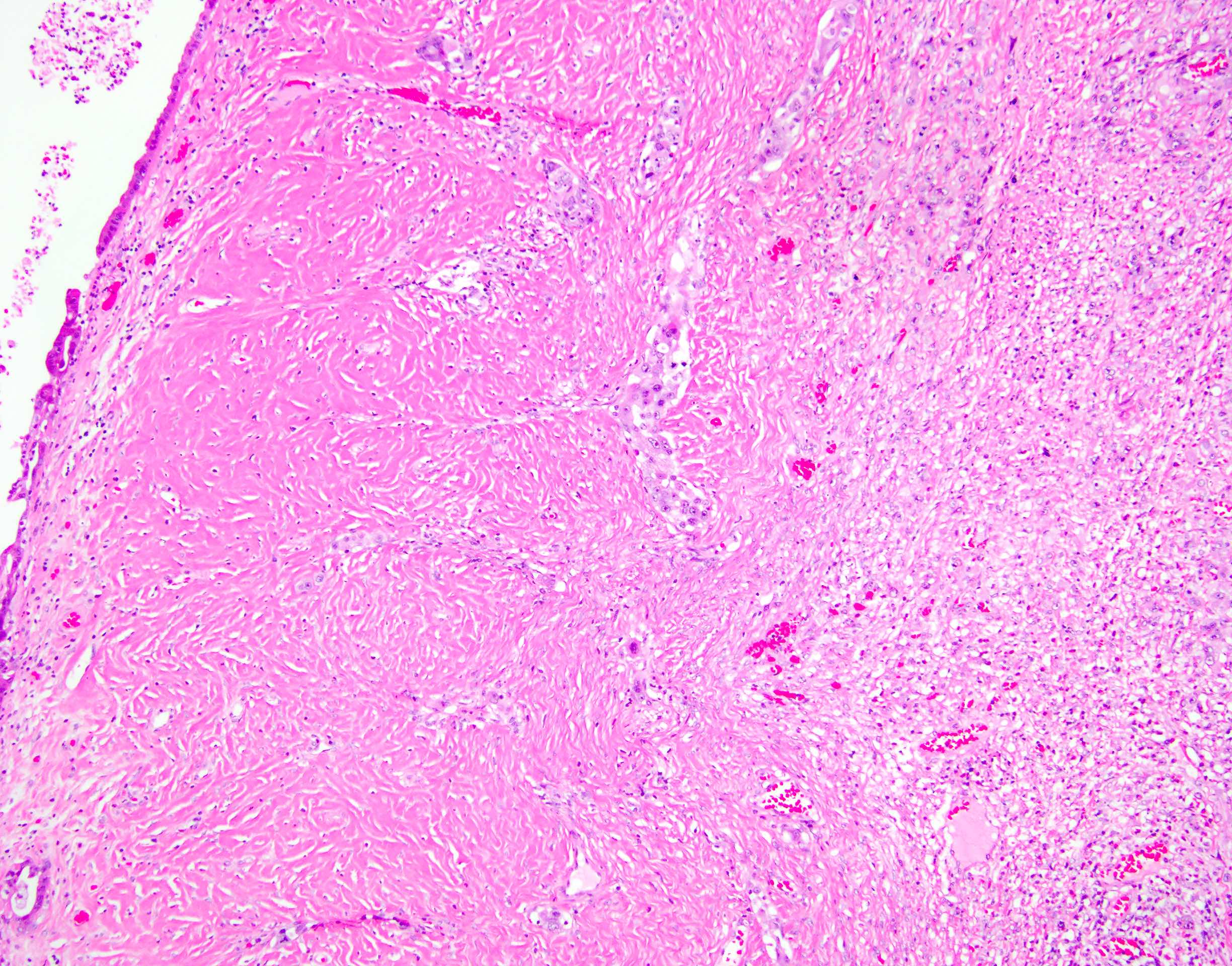
- Absence of vascular invasion indicates that the tumor is benign
- Presence of cytologic atypia within the mural nodule indicates that it is malignant
- Presence of a fibrous layer between the nodule and the mucinous tumor indicates that the mural nodule is benign
- Presence of infiltrative tumor nests between the nodule and the mucinous tumor indicates that the mural nodule is malignant
- Tumor behavior will be driven by the mucinous tumor, which appears benign
Practice answer #2
D. Presence of infiltrative tumor nests between the nodule and the mucinous tumor indicates that the mural nodule is malignant
All mural nodules are characterized by the presence of a fibrous stromal layer between the nodule and the mucinous tumor. However, tumor invasion into this stroma is indicative of malignancy. Vascular invasion may also be seen in malignant mural nodules but is not required for diagnosis as such. Cytologic atypia may be seen in both malignant mural nodules and benign sarcoma-like mural nodules. A malignant mural nodule can be associated with poor prognosis regardless of the benignity of the associated mucinous tumor.
Comment Here
Reference: Mural nodules in mucinous cystic neoplasms
All mural nodules are characterized by the presence of a fibrous stromal layer between the nodule and the mucinous tumor. However, tumor invasion into this stroma is indicative of malignancy. Vascular invasion may also be seen in malignant mural nodules but is not required for diagnosis as such. Cytologic atypia may be seen in both malignant mural nodules and benign sarcoma-like mural nodules. A malignant mural nodule can be associated with poor prognosis regardless of the benignity of the associated mucinous tumor.
Comment Here
Reference: Mural nodules in mucinous cystic neoplasms