Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Navale P, Savari O, Tomashefski JF, Vyas M. Solid pseudopapillary neoplasm. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pancreassolidpseudo.html. Accessed September 25th, 2025.
Definition / general
- Low malignant potential tumors with unclear cell of origin and pathogenesis
- May be derived from pluripotent stem cells of the genital ridges that become attached to the pancreas during embryogenesis (Semin Diagn Pathol 2014;31:484)
- First described by V.K. Frantz in 1959; incorporated into the WHO classification in 1996 (Br J Surg 1959;47:334)
Essential features
- Presents in younger women, classically as solitary body / tail mass
- Variable amount of solid and cystic areas grossly
- Papillary fronds on myxoid or hyalinized vascular stalk lined by poorly cohesive, uniform cells with nuclear grooves comprising solid and cystic areas beta catenin nuclear / cytoplasmic positive
Terminology
- Also known as solid pseudopapillary tumor, papillary epithelial neoplasm, papillary cystic neoplasm, solid and papillary neoplasm, low grade papillary neoplasm and Hamoudi or Frantz tumor
Epidemiology
- Represents 1 - 2% of pancreatic neoplasms
- F:M = 10:1 (accounts for 30% tumors in < 40 year old women) (Arch Pathol Lab Med 2020;144:829)
- Usually presents in the third to fourth decade of life (mean age 35 years)
- In men, tends to occur at an older age with more aggressive behavior (Surgery 2008;143:29)
- Occasional cases have been reported in patients with familial adenomatous polyposis (Intern Med 2015;54:1349, Surg Case Rep 2021;7:35)
Sites
- Located throughout the pancreas but more frequently in the body or tail in adults, while more frequent in the head of pancreas in children (Arch Surg 2008;143:1218)
- Rarely reported in extrapancreatic sites, such as mesocolon, omentum, ovary and testis (Virchows Arch A Pathol Anat Histopathol 1991;418:179, Am J Surg Pathol 2010;34:1514, Int J Gynecol Pathol 2011;30:539, Ann Diagn Pathol 2018;35:42)
Clinical features
- Most common symptoms are abdominal pain and a palpable, nontender, upper abdominal mass
- Also symptoms related to an intra abdominal mass effect, such as discomfort, nausea, vomiting and early satiety
- However, most cases are incidentally discovered on imaging
- Reference: Arch Pathol Lab Med 2017;141:990
Diagnosis
- Solid / solid cystic mass in the tail of pancreas on imaging, especially in young women (Diagn Interv Radiol 2017;23:94)
- Cyst fluid chemistry shows low CEA and amylase (Ann Gastroenterol 2013;26:122)
- Cytology / histology are necessary for confirmation of diagnosis
Laboratory
- Cyst fluid is often bloody with low CEA and low amylase (Ann Gastroenterol 2013;26:122)
Radiology description
- Well circumscribed, encapsulated, heterogeneous pancreatic lesion with cystic degeneration on CT or MRI
Radiology images
Prognostic factors
- Poor prognostic factors include: size > 5 cm, male gender, necrosis, cellular atypia, vascular invasion, perineural invasion and invasion into adjacent structures (Dig Liver Dis 2013;45:703)
Case reports
- 14 year old Hispanic girl with silent presentation of a solid pseudopapillary neoplasm of the pancreas (Am J Case Rep 2017;18:656)
- 16 year old boy with tonic convulsions (J Clin Res Pediatr Endocrinol 2017;9:375)
- 40 year old man with subsequent multiple metastases (World J Gastrointest Oncol 2017;9:497)
- 45 year old woman with situs invertus (Medicine (Baltimore) 2018;97:e0205)
- 62 year old woman with IgG4 related pancreatitis (Int J Surg Pathol 2017;25:271)
Treatment
- Surgical resection is curative in > 95% of cases
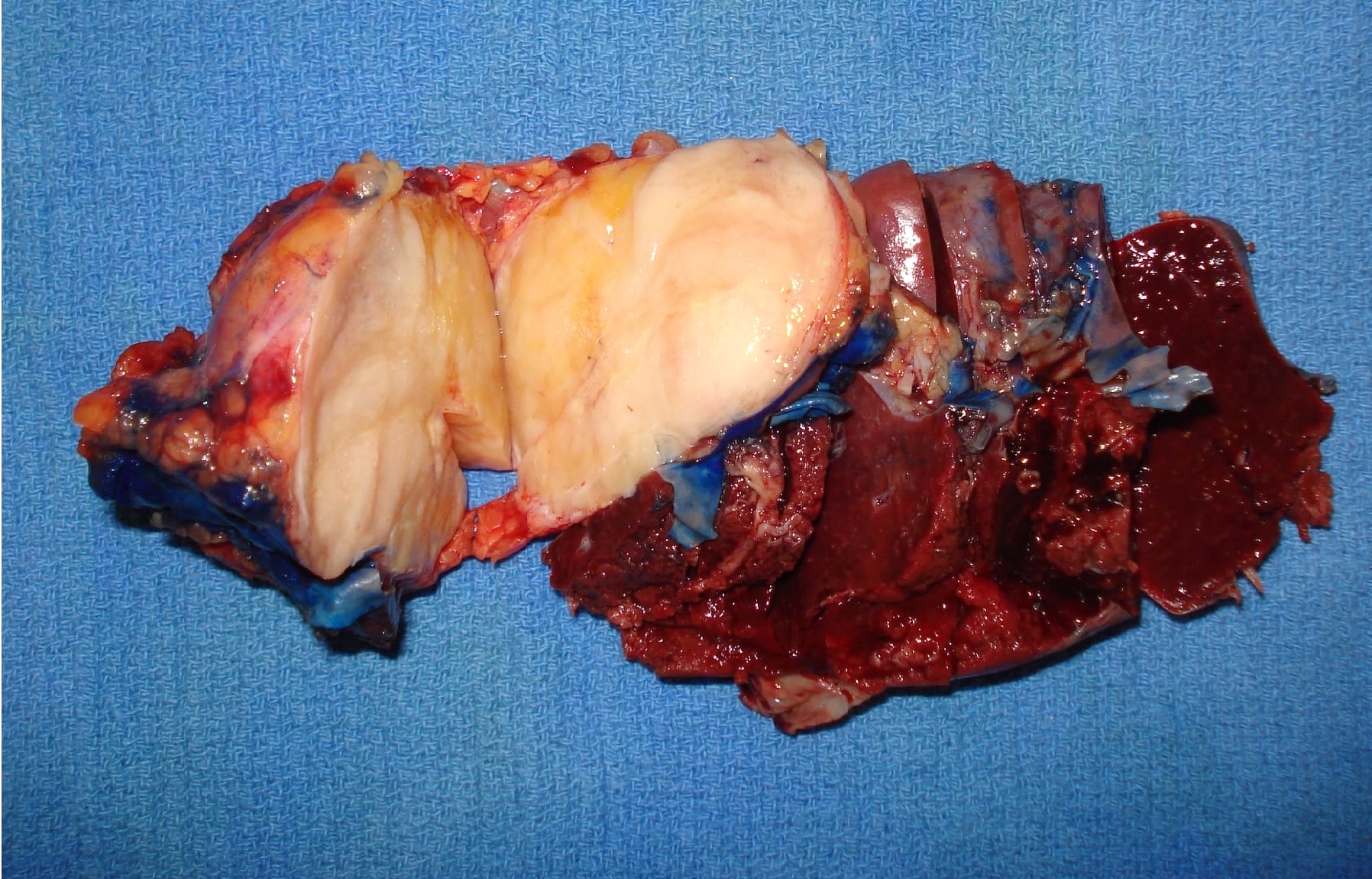
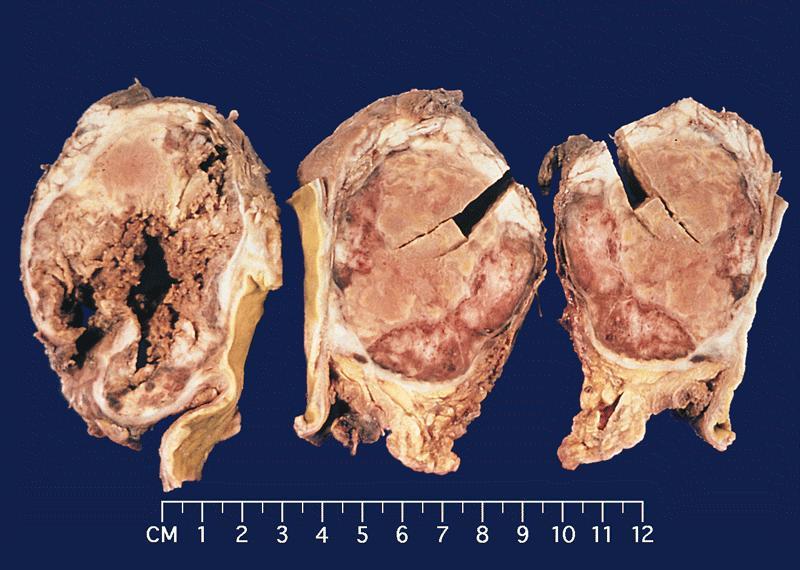
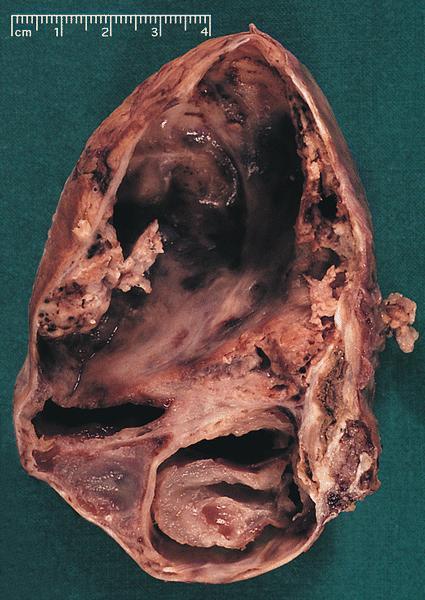
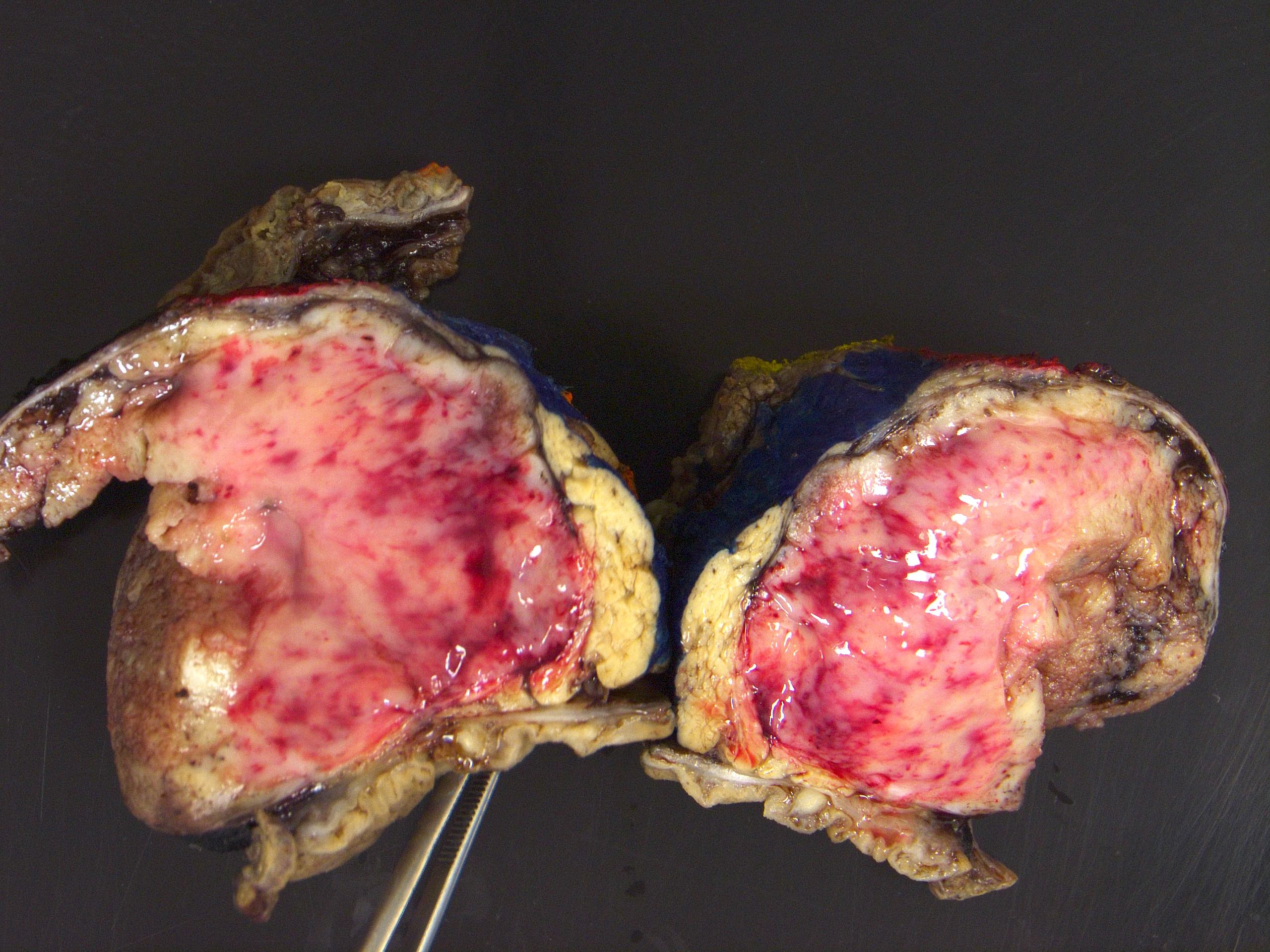
Gross description
- Range from 0.5 to 34.5 cm, with a mean diameter of 6 cm
- Well defined, encapsulated, with variable amount of solid and cystic patterns
- Smaller lesions tend to be more solid but less sharply circumscribed
- Larger tumors demonstrate a fibrous pseudocapsule and have a variegated and friable cut surface
- Cystic degeneration and hemorrhage are common findings in larger specimens
- Rarely, may extend into adjacent structures, such as duodenum
- Reference: Arch Pathol Lab Med 2020;144:829
Gross images
Contributed by Omid Savari, M.D., Dr. Andreas Schulz, Manfred Stolte, M.D., Dr. Helmut Luchtrath, Wei Chen, M.D., Ph.D., Nakul Anush Ravish, M.B.B.S. and Case #121
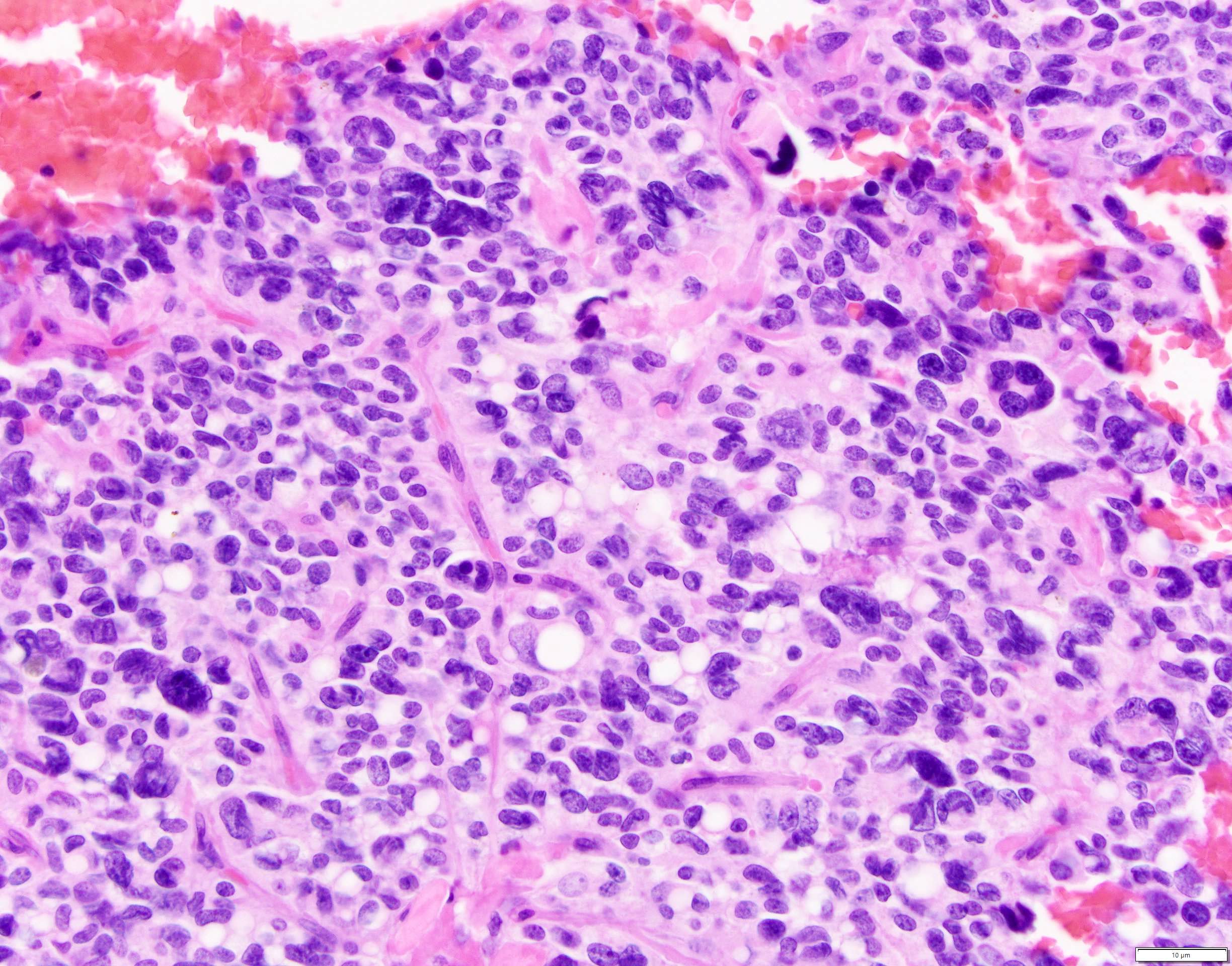
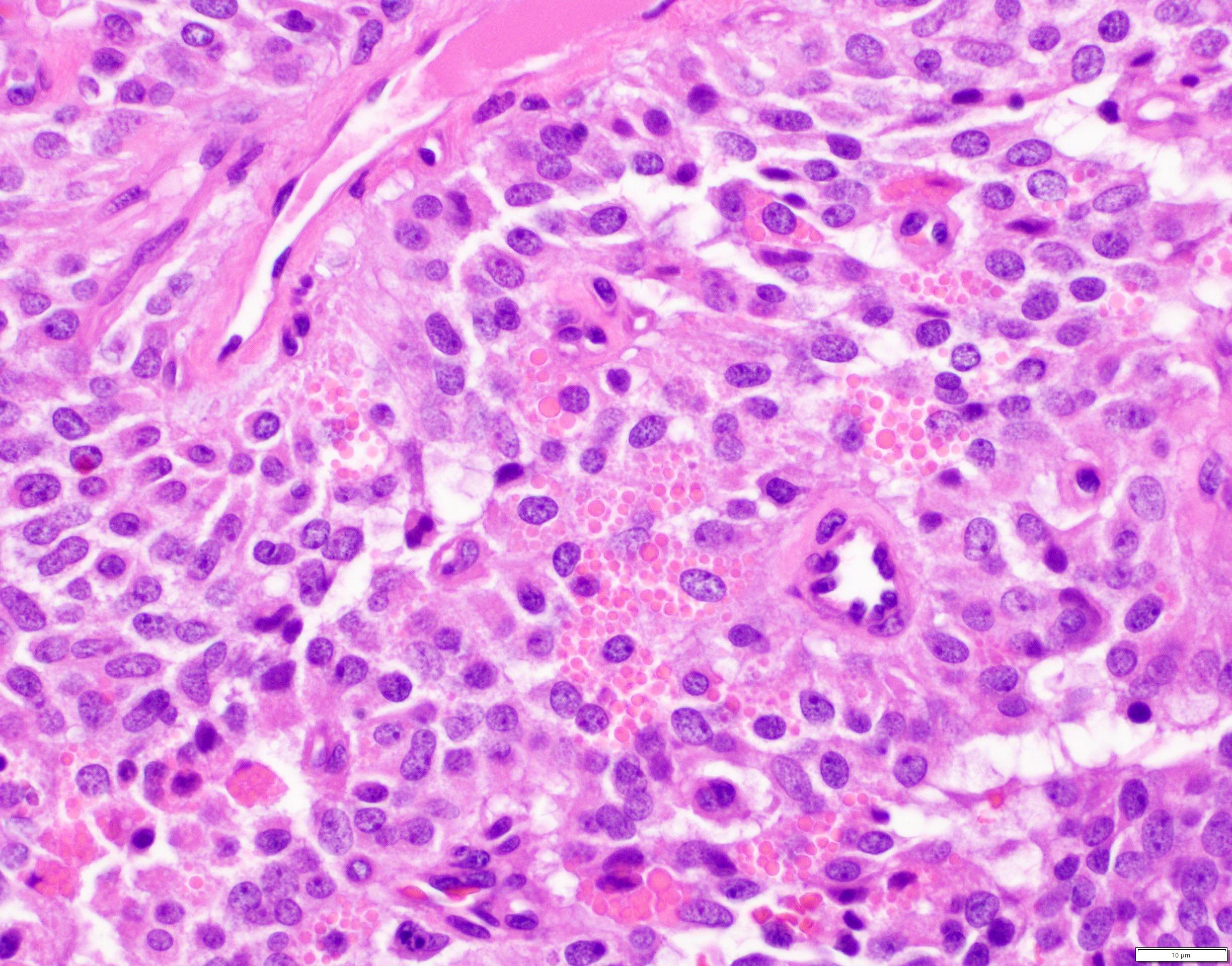
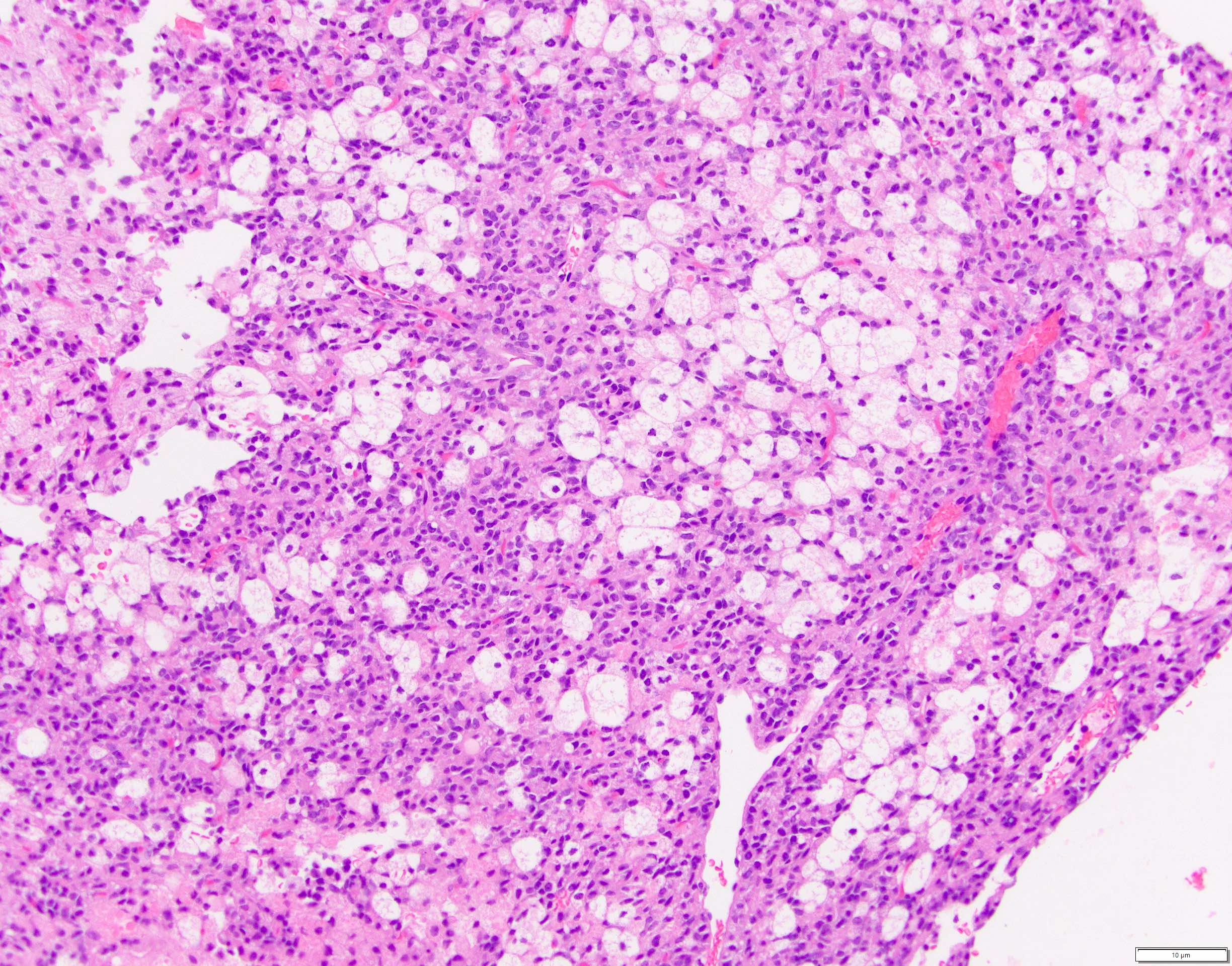
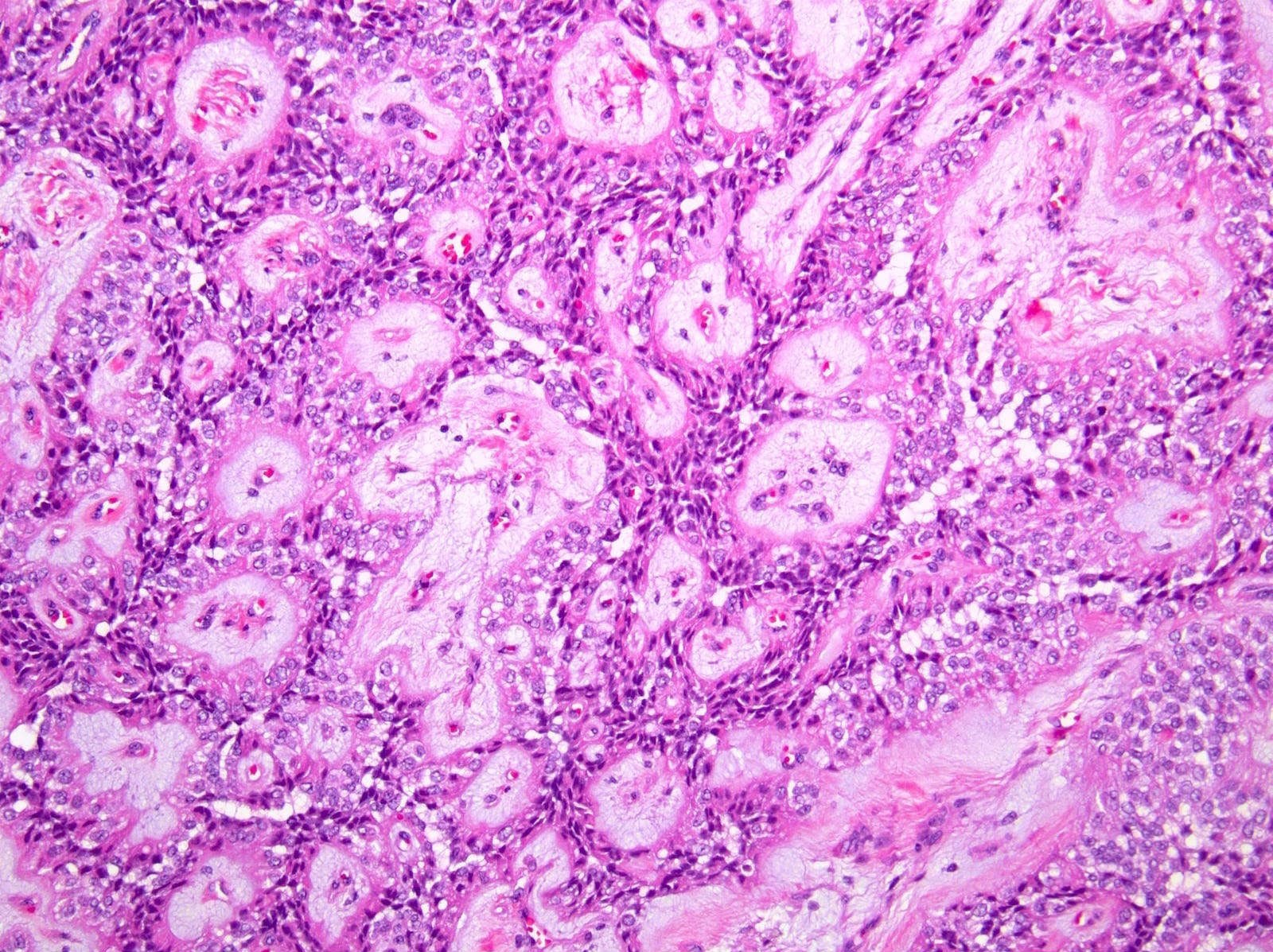
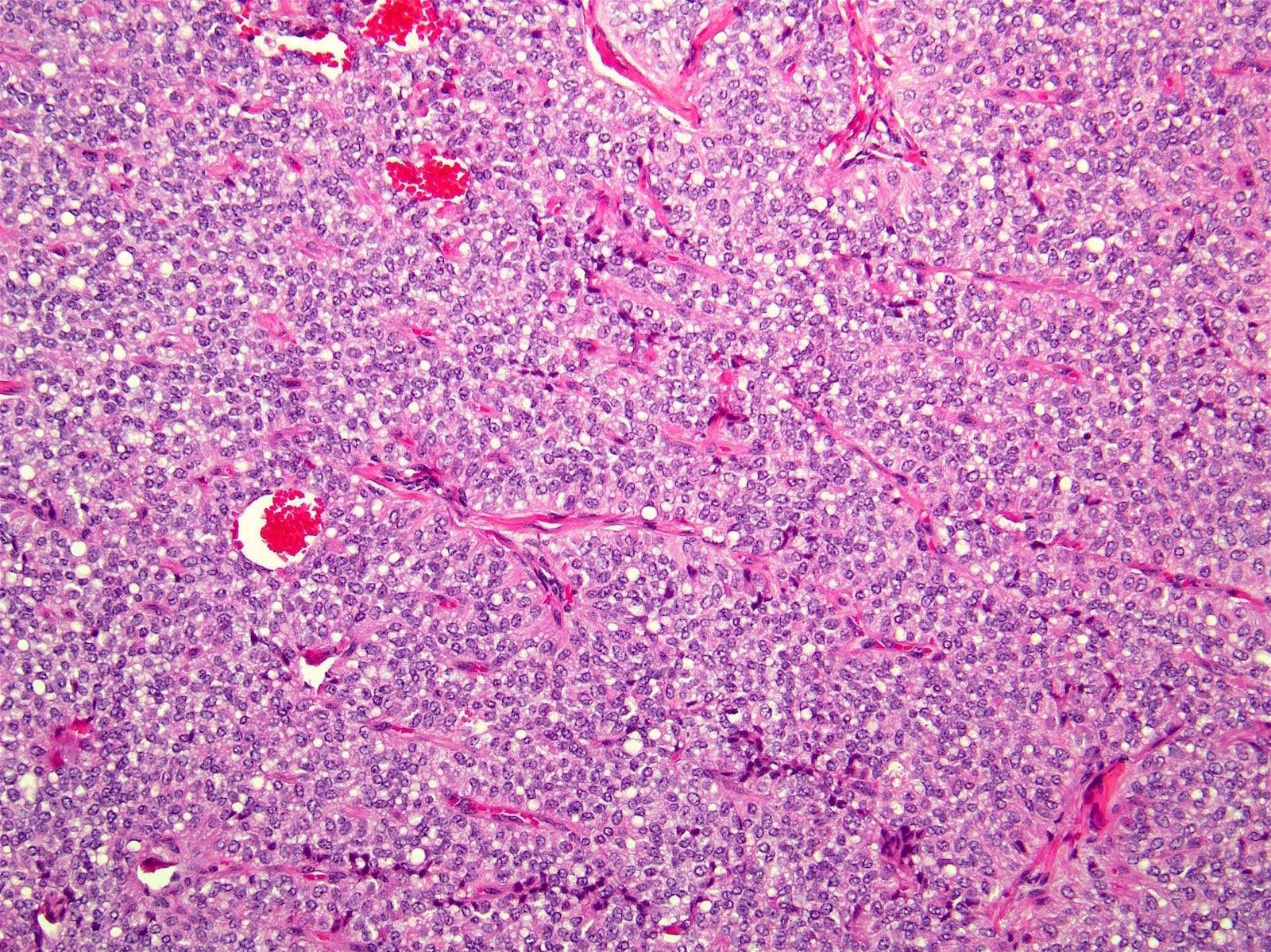
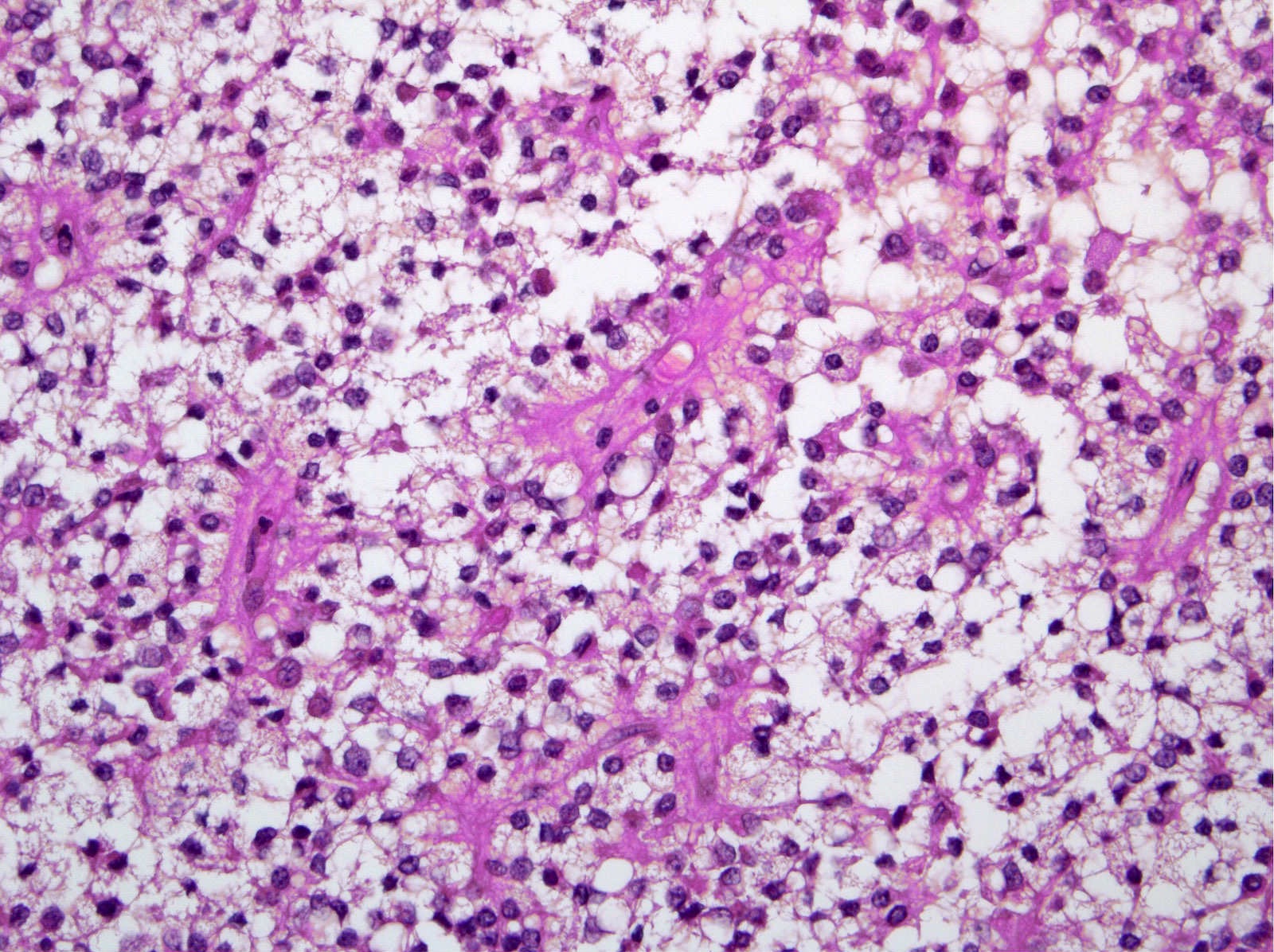
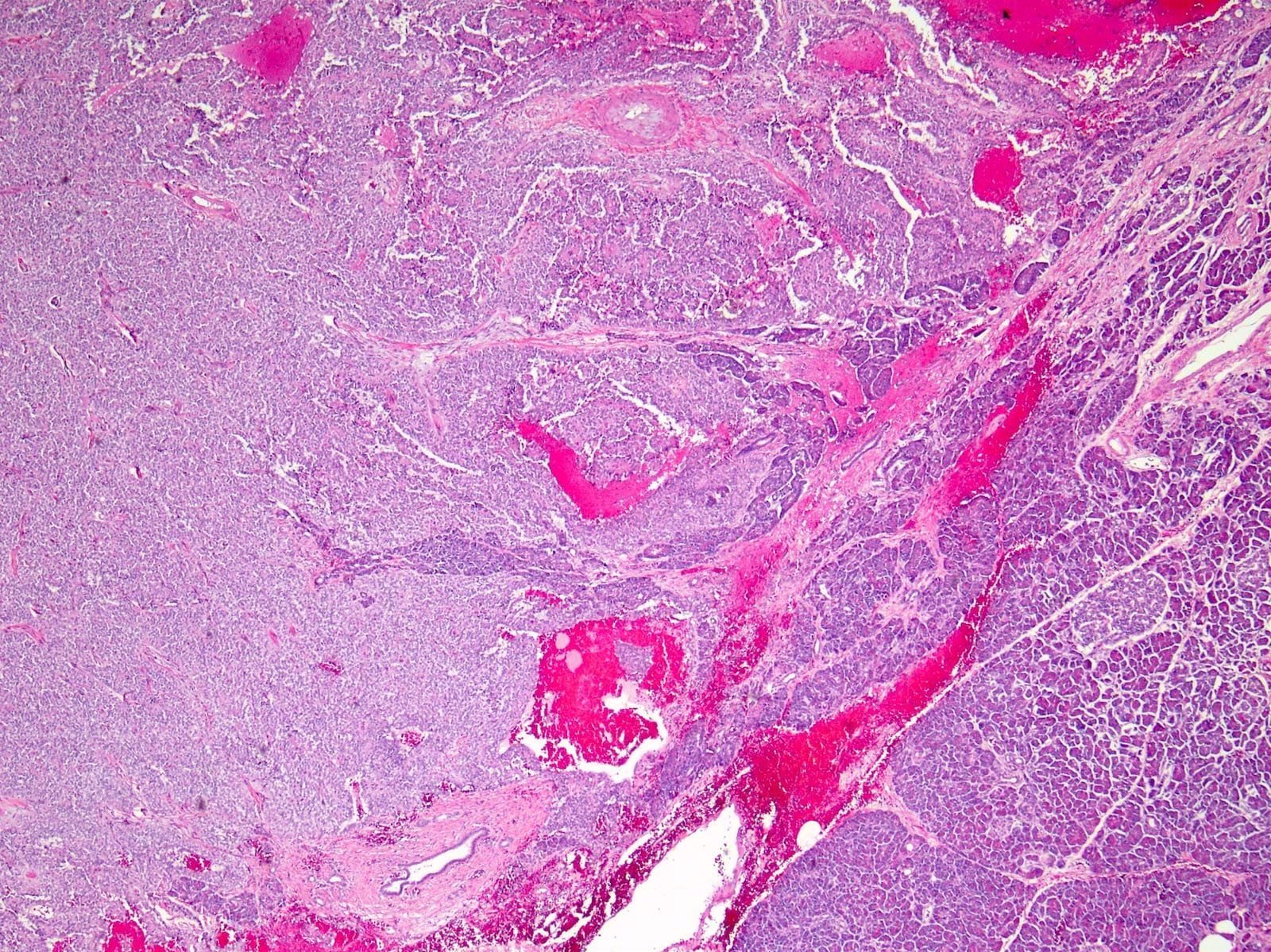
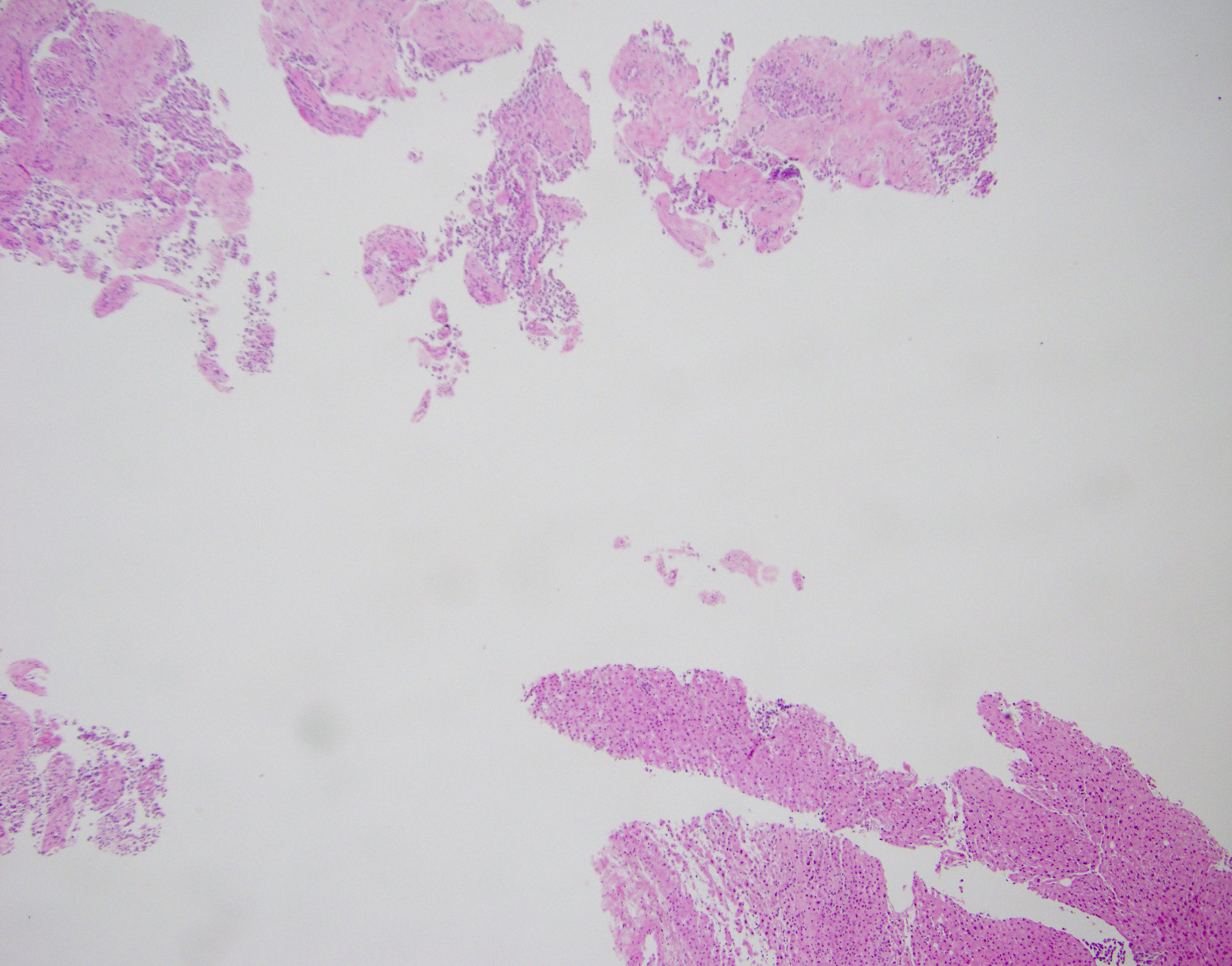
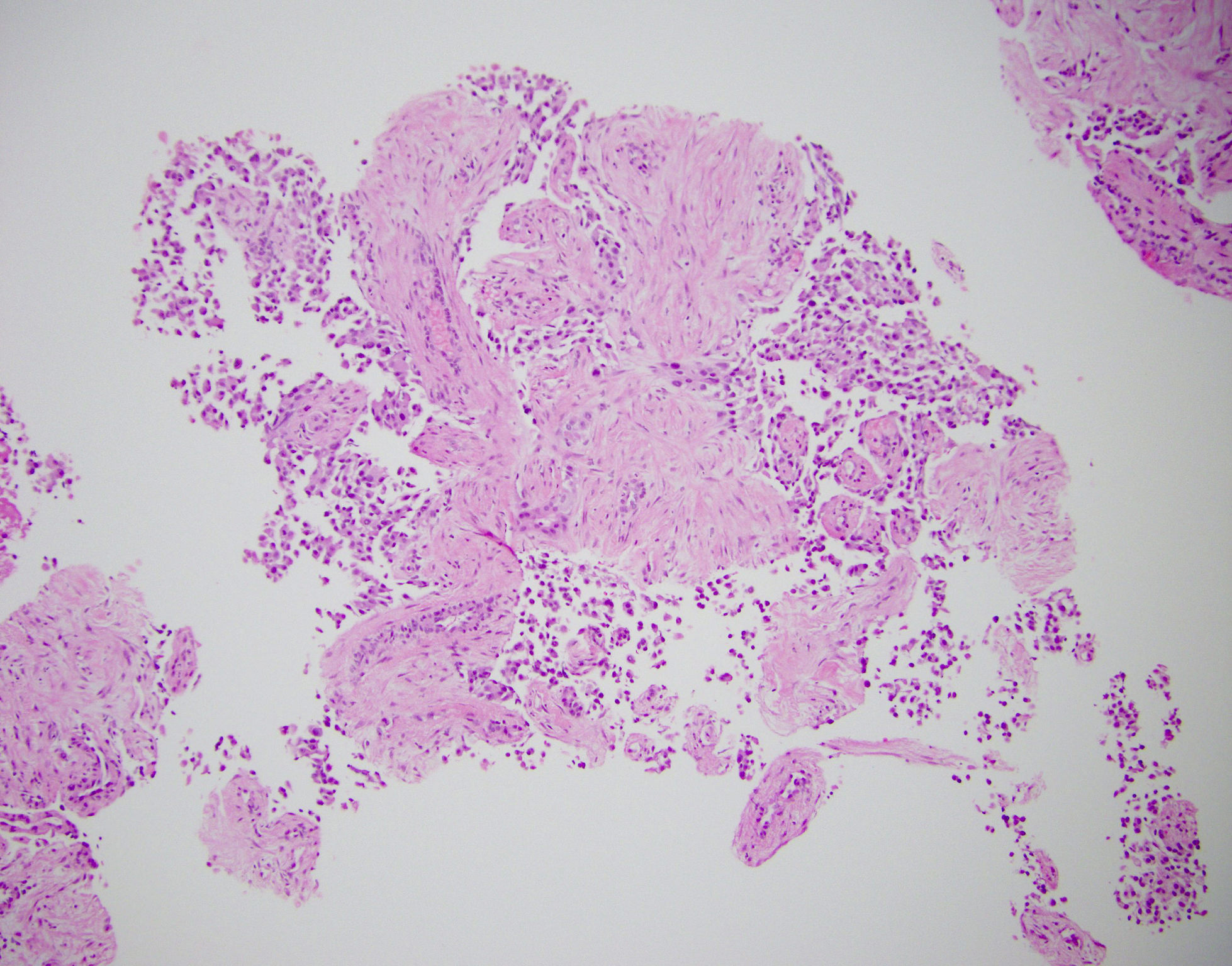
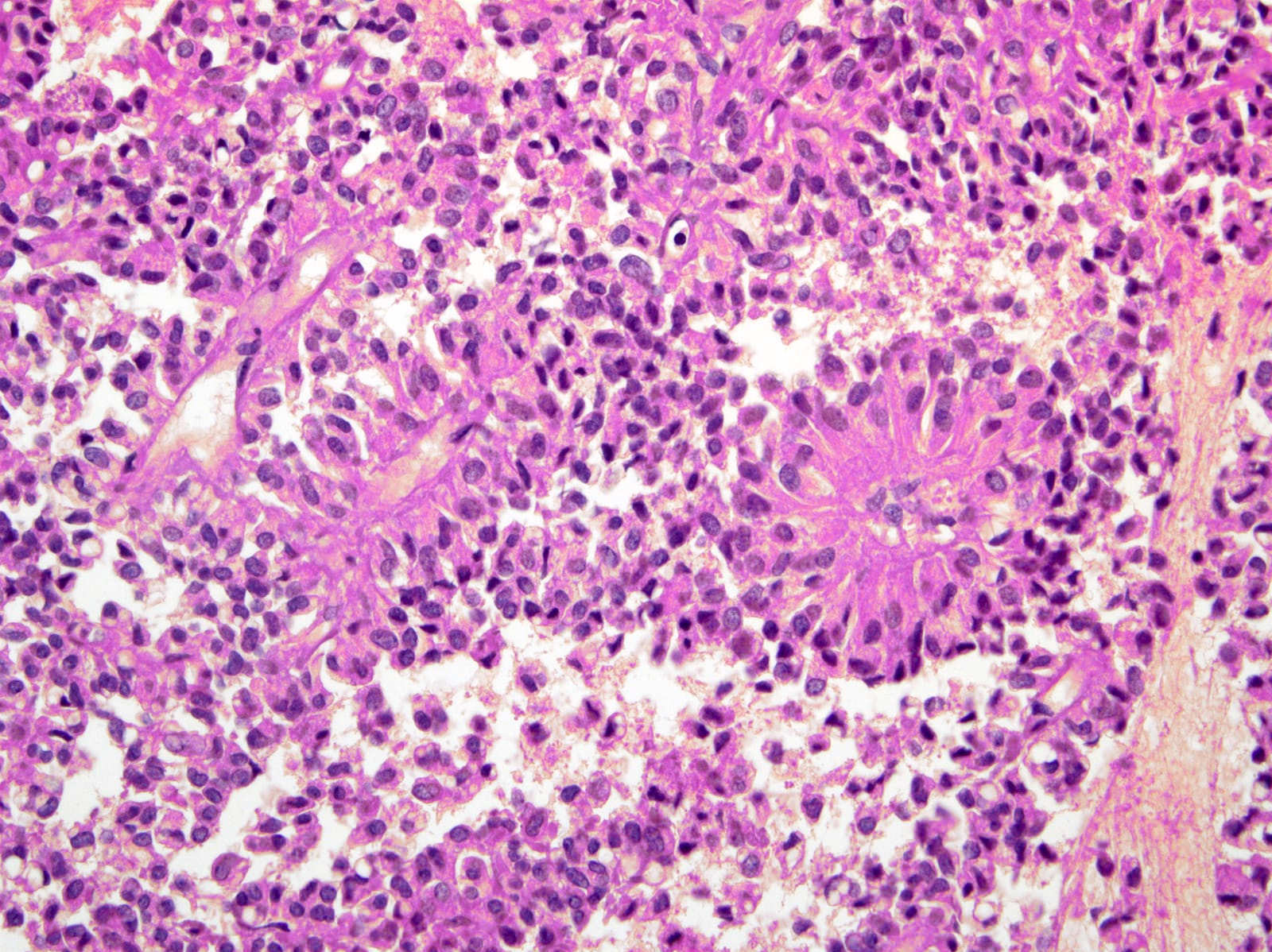
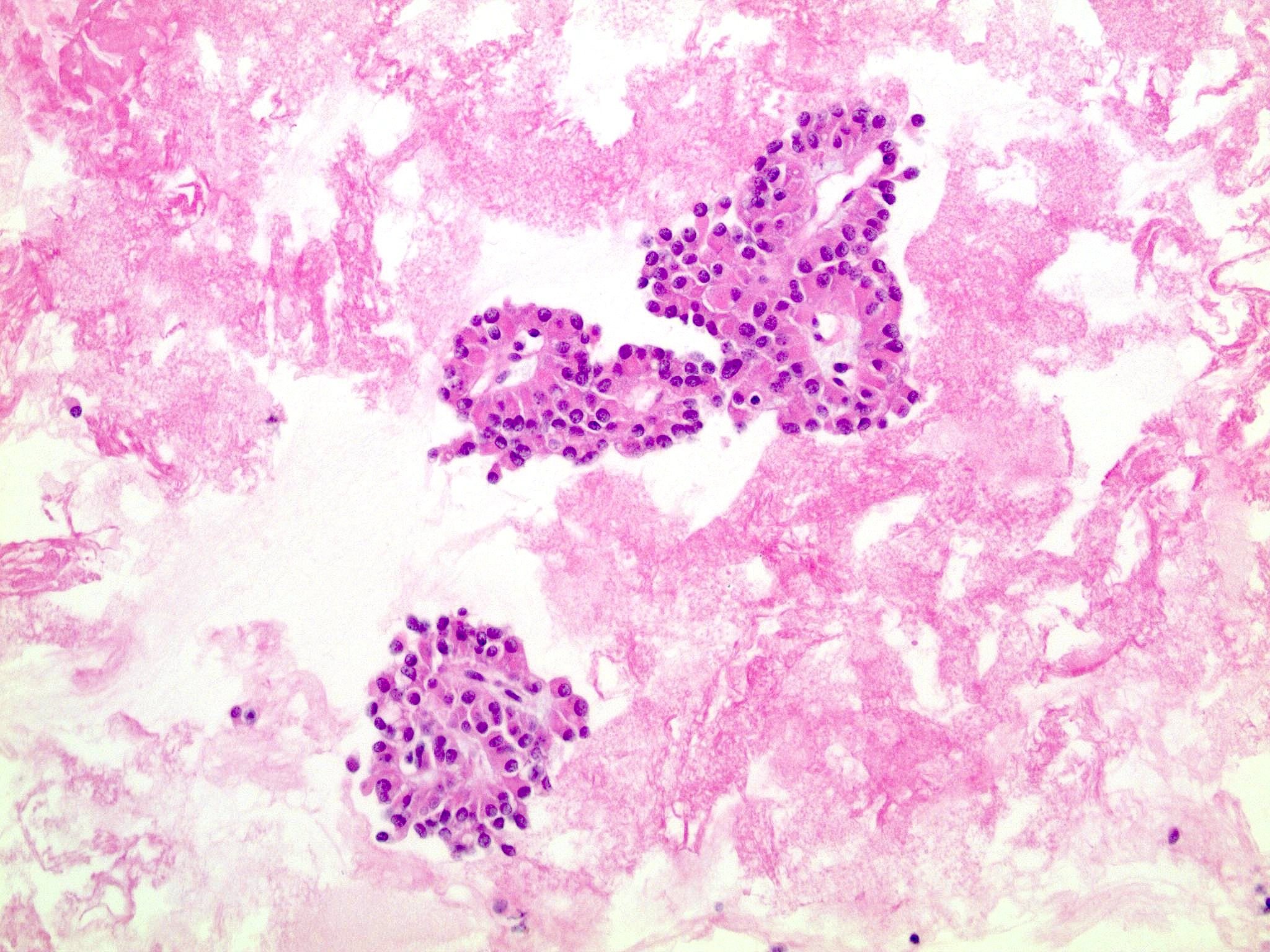
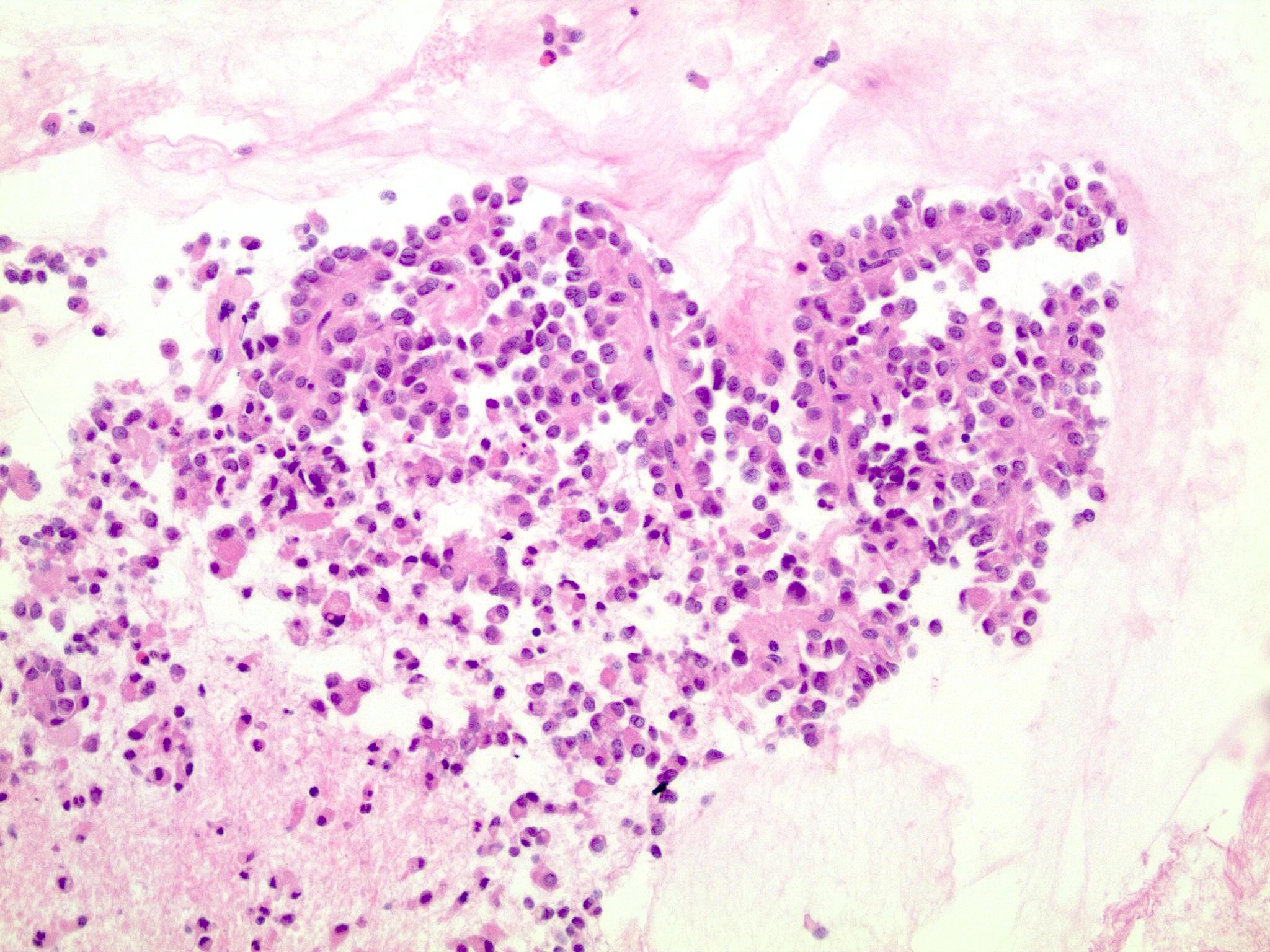
Microscopic (histologic) description
- Tumors are heterogeneous, with variable admixture of solid and pseudopapillary areas
- Solid areas are comprised of uniform cells admixed with capillary sized blood vessels
- Pseudopapillae are formed due to tumor cells getting detached from blood vessels forming fibrovascular stalks or rosette-like structures (Arch Pathol Lab Med 2020;144:829)
- Stroma usually shows various degrees of hyalinization or evidence of degeneration, such as hemorrhage, foamy macrophages, calcification and cholesterol clefts
- Tumor cells usually have a moderate amount of eosinophilic cytoplasm with intracytoplasmic hyaline globules (PAS+ and diastase resistant, positive for alpha-1-antitrypsin) and perinuclear vacuoles (Am J Surg Pathol 2011;35:981)
- Relatively uniform nuclei with finely textured chromatin, inconspicuous nucleoli and characteristic longitudinal grooves
- Variants include clear cell, oncocytic and pleomorphic
- Rare mitotic figures
- Although grossly well circumscribed, microscopic finding of infiltration to the surrounding pancreatic tissue is not uncommon
- Rare cases of highly aggressive behavior; histological features in those cases included diffuse growth pattern, extensive necrosis, significant nuclear atypia, high mitotic count (35 - 70/50 high power fields) or sarcomatoid features (Am J Surg Pathol 2005;29:512)
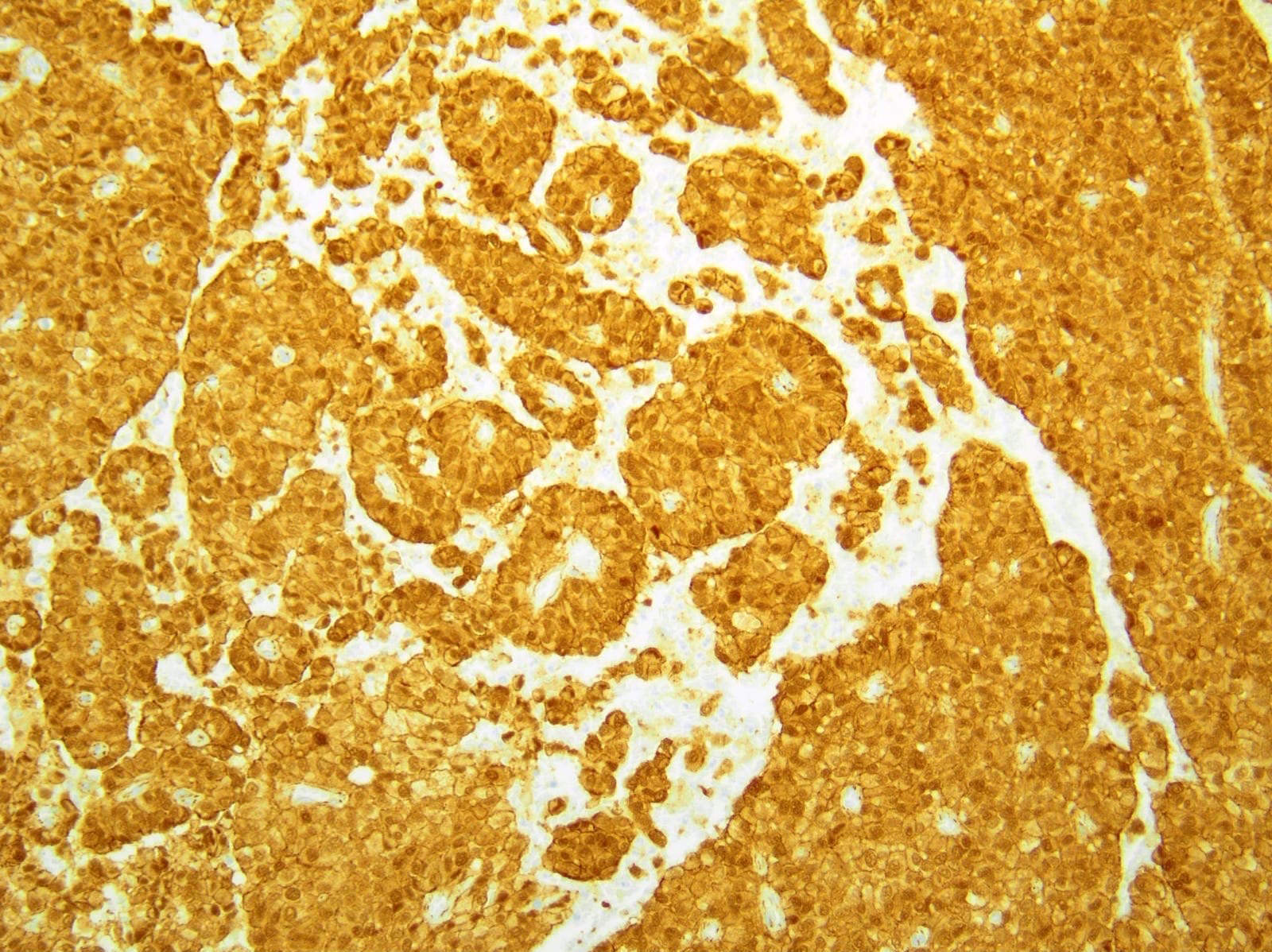
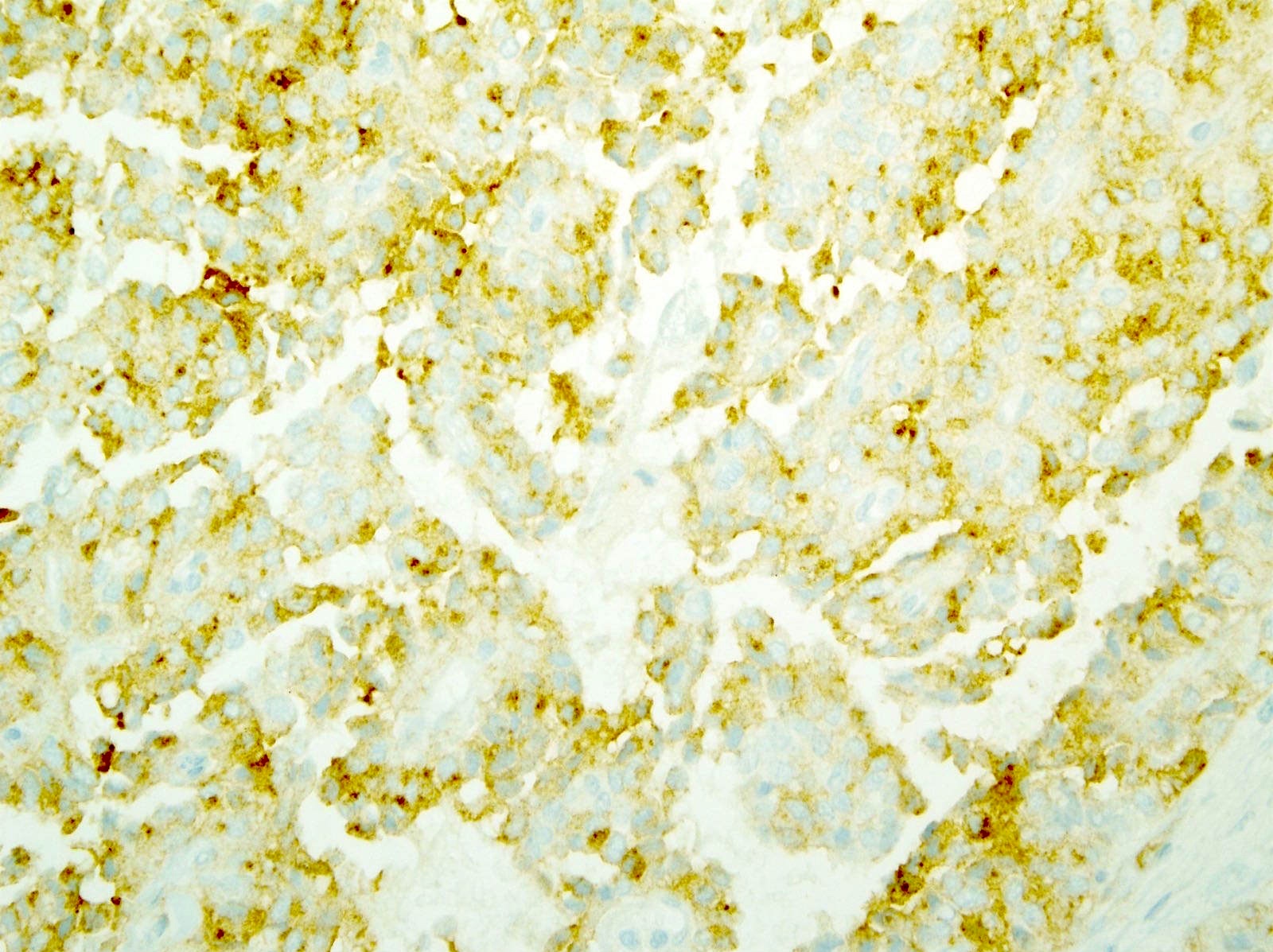
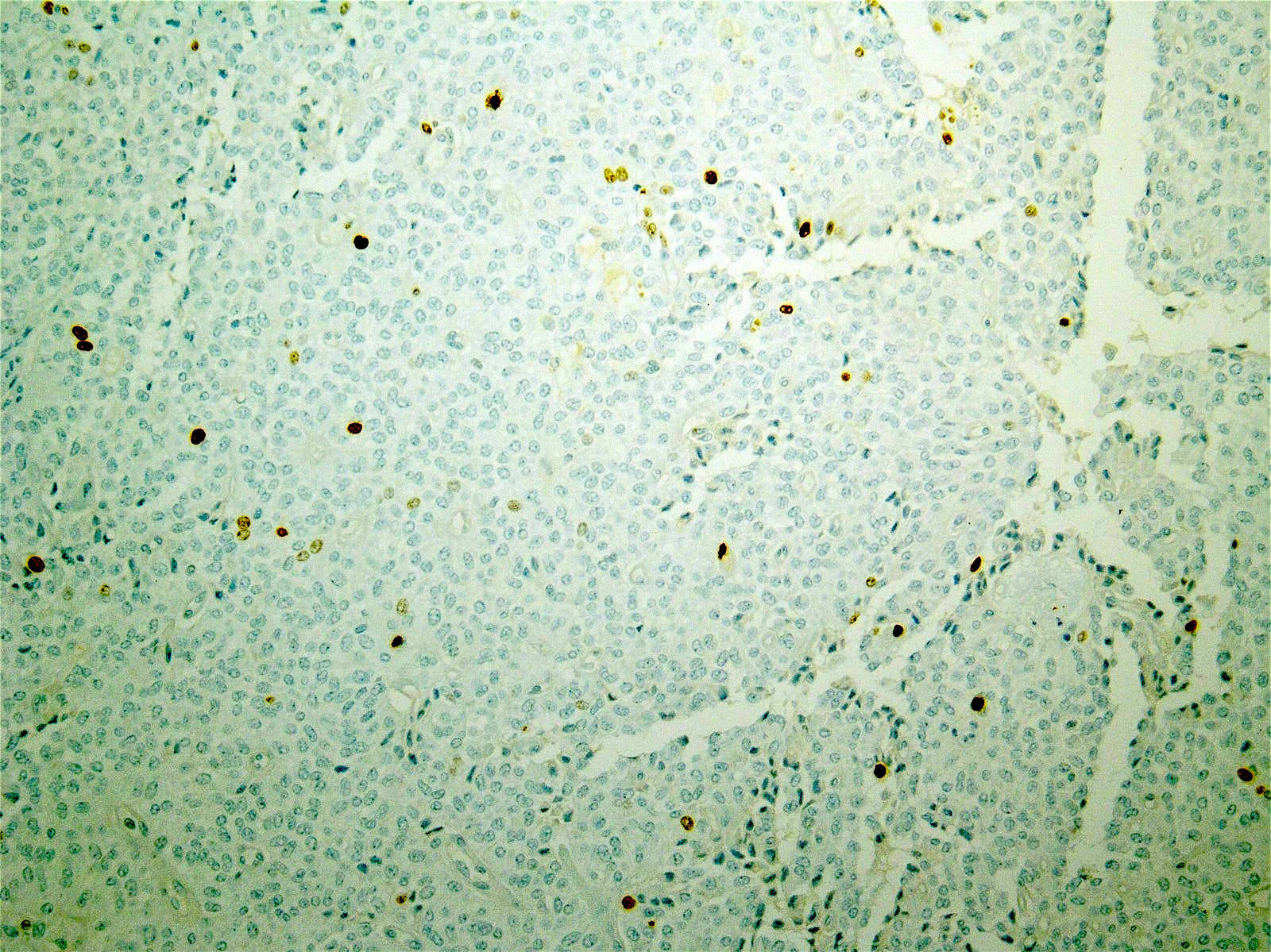
Microscopic (histologic) images
Contributed by Monika Vyas, M.D., Omid Savari, M.D. and Raul S. Gonzalez, M.D.
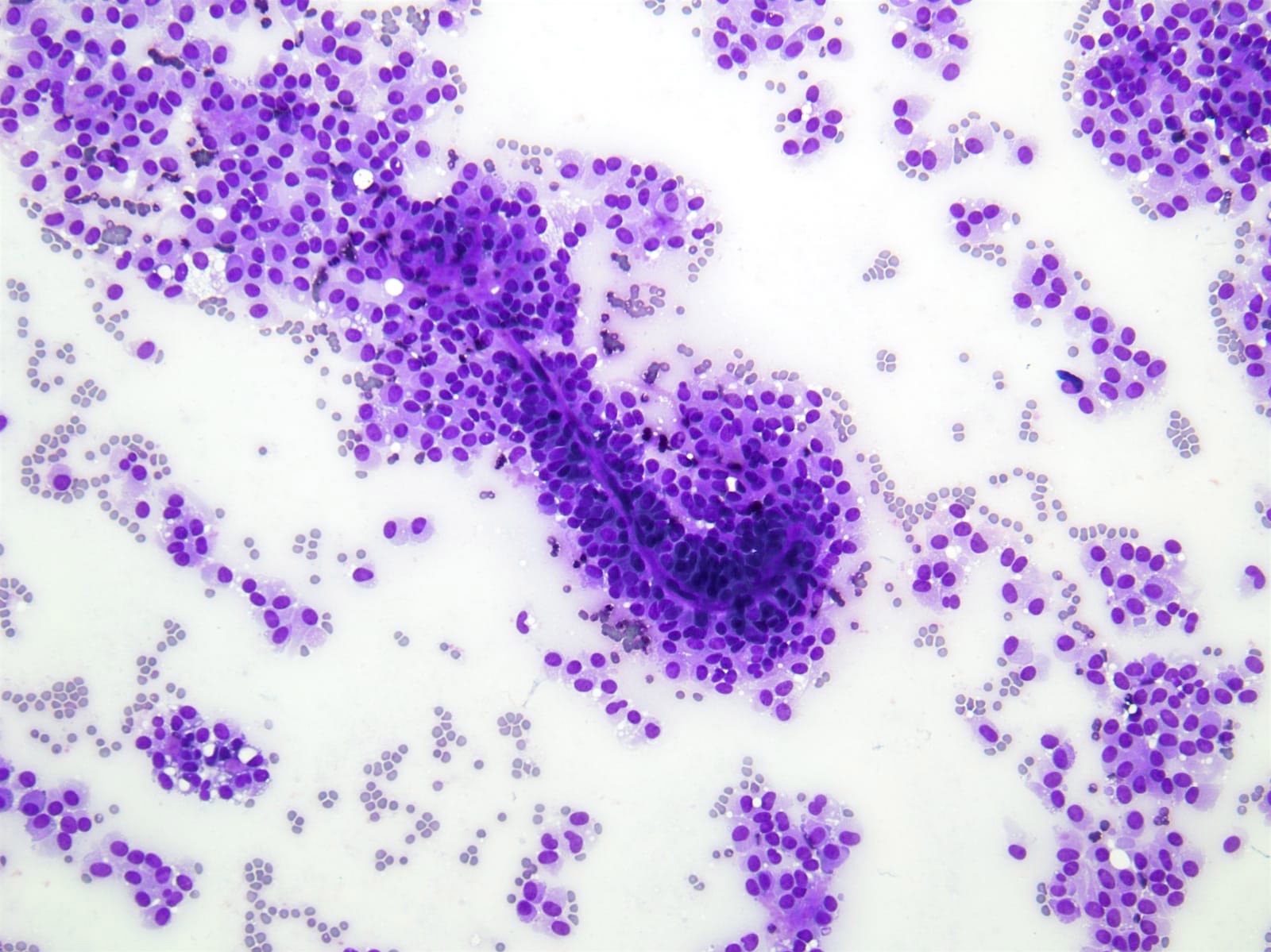
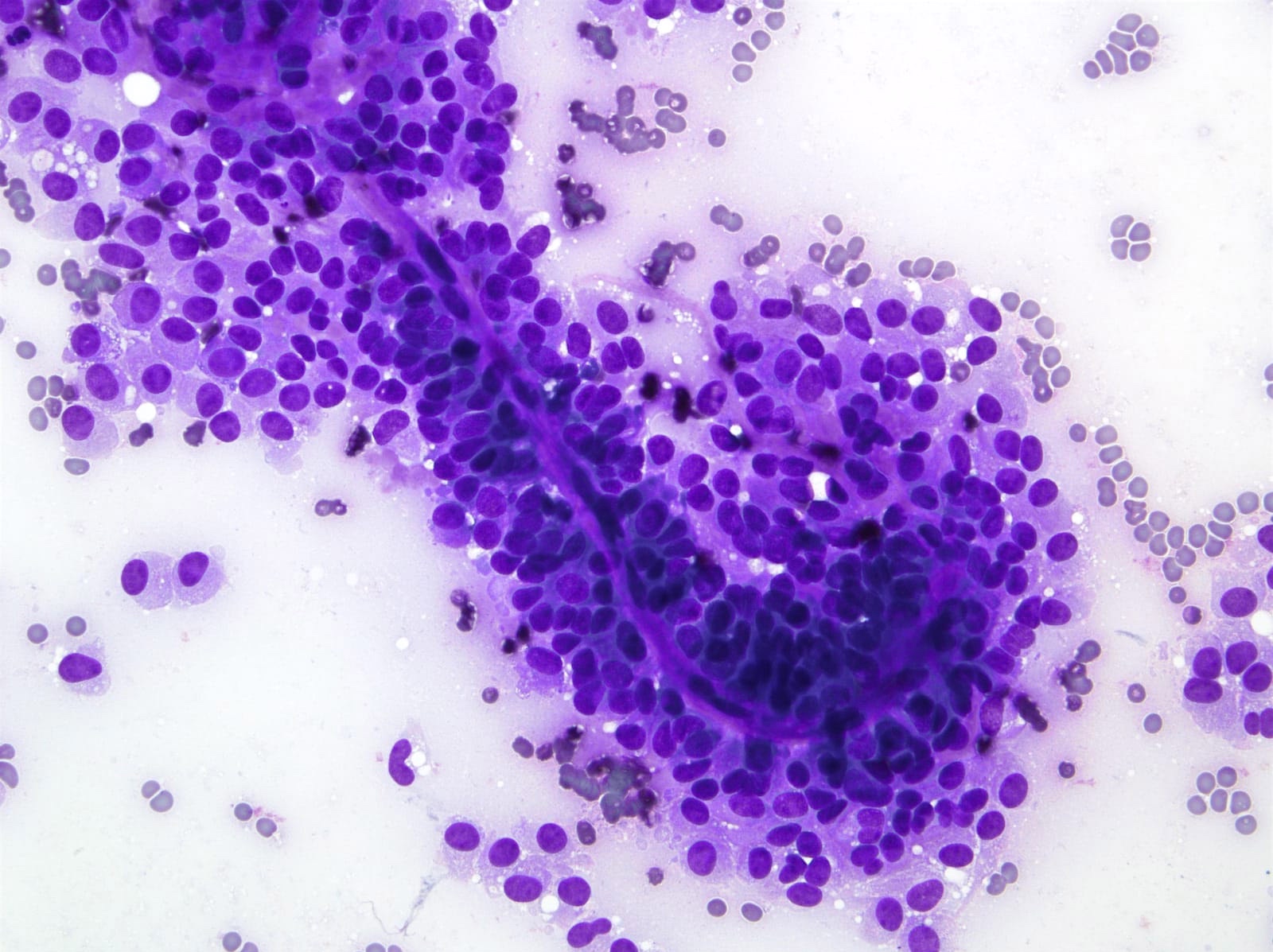
Cytology description
- Cellular smears with delicate papillary fronds
- Tumor cells are usually bland and uniform with a moderate amount of cytoplasm, which usually contains variable sized clear perinuclear vacuoles or cytoplasmic eosinophilic hyaline globules
- Nuclei are round to oval with grooves and finely granular chromatin (J Cytol 2010;27:118, Arch Pathol Lab Med 2017;141:990)
- Cercariform cells, cytoplasmic vacuolation, reniform nuclei, hyaline globules and degenerative features, such as cholesterol crystals, calcifications, foam cells or giant cells, are more commonly seen in solid pseudopapillary neoplasms, compared with acinar cell carcinomas / neuroendocrine tumors (Cancer Cytopathol 2013;121:298)
Cytology images
Positive stains
- Beta catenin (98%): aberrant nuclear expression
- E-cadherin (loss of membranous expression) (Hum Pathol 2008;39:251)
- p120 (cytoplasmic staining with loss / reduction of membranous expression) (Am J Clin Pathol 2008;130:71)
- Alpha-1-antichymotrypsin (95%), alpha-1-antitrypsin (82%)
- Vimentin (88%)
- Cyclin D1
- CD10 (63%)
- SOX11 (100%)
- Androgen receptor (81%), TFE3 (75%), LEF1 (93%), FUS (85%), progesterone receptor (63%), claudin7, claudin5 (Am J Surg Pathol 2009;33:768)
- CD56 (96%), neuron specific enolase (70%), synaptophysin (55%)
- Cytokeratin (52%)
- CD99 (dot-like) (Am J Surg Pathol 2011;35:799)
Negative stains
- Chromogranin A (positive in only 9%)
- CEA
- Estrogen receptor
- Reference: Arch Pathol Lab Med 2017;141:990
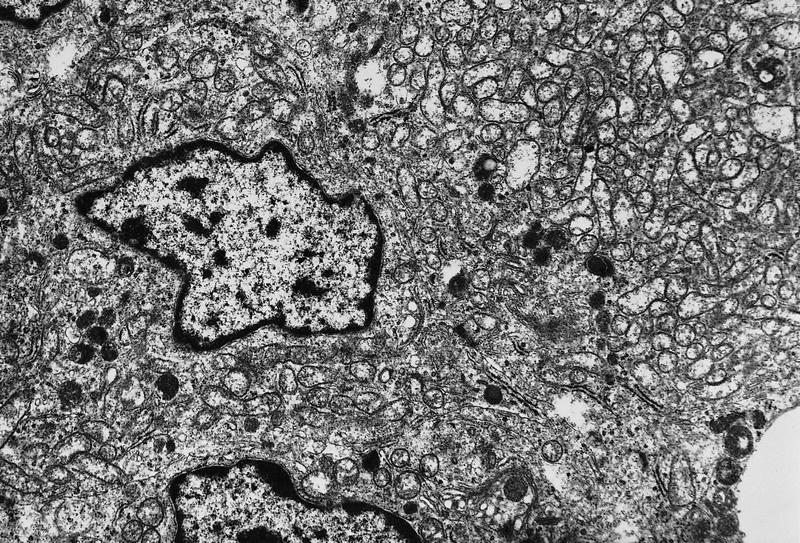
Electron microscopy description
- Mitochondria rich cytoplasm with electron dense granules and rough endoplasmic reticulum
Molecular / cytogenetics description
- Point mutation in exon 3 of β catenin gene (CTNNB1) is present in > 90%
- Gene mutation results in the accumulation of β catenin in the cytoplasm and formation of a β catenin Tcf / Lef complex, through which the Wnt signaling pathway activates several oncogenic genes, such as MYC and cyclin D1 (Am J Clin Pathol 2017;149:67)
- Rarely, mutations in APC gene (also associated with familial adenomatous polyposis) have been described (Pathol Int 2019;69:193)
Sample pathology report
- Pancreas and spleen, distal pancreatectomy and splenectomy:
- Solid pseudopapillary neoplasm (XX cm), confined to pancreas (see comment)
- Resection margins are free of tumor
- Unremarkable spleen, (x g)
- X benign lymph nodes (0/12)
- Comment: Immunohistochemical stains show the neoplastic cells are positive for CD10 and exhibit nuclear expression of beta catenin while negative for synaptophysin and chromogranin.
- Pancreas, mass, biopsy:
- Epithelial neoplasm, most consistent with solid pseudopapillary neoplasm (see comment)
- Comment: By immunohistochemistry, the neoplastic cells are positive for CD56, pancytokeratin (focal) and show rare focal positivity for synaptophysin while being negative for chromogranin. Aberrant nuclear expression of beta catenin is present. The histologic and immunohistochemical findings are in keeping with a solid pseudopapillary neoplasm.
- Pathological staging (AJCC 8th edition) - similar to exocrine pancreatic tumors
Differential diagnosis
- Pancreatic neuroendocrine tumor:
- Small to medium sized cells with uniform nuclei and finely granular chromatin (salt and pepper appearance), arranged in organoid, trabecular or nested patterns
- Positive for neuroendocrine markers and negative for nuclear beta catenin
- Acinar cell carcinoma:
- Prominent acinar formation and cells with finely granular cytoplasm
- Positive for pancreatic enzymes (trypsin, chymotrypsin), BCL10 and variable staining for beta catenin
- Pancreatoblastoma:
- Primitive pancreatic elements with acinar, ductal and neuroendocrine differentiation
- Also squamoid corpuscles; more common in children younger than 10 years
- Positive for beta catenin (80%), neuroendocrine markers and pancreatic enzymes (trypsin, chymotrypsin and lipase) and BCL10
Practice question #1
What is the most common gene mutation in pancreatic solid pseudopapillary neoplasm?
- CTNNB1
- KIT
- PDGFRA
- RAS
Practice answer #1
A. Somatic point mutation of β catenin gene (CTNNB1) is present in > 90% of pancreatic solid pseudopapillary neoplasms
Comment Here
Reference: Solid pseudopapillary neoplasm
Comment Here
Reference: Solid pseudopapillary neoplasm
Practice question #2
Practice answer #2
A. The hyaline globules are immunoreactive for alpha-1-antitrypsin and are also PAS+ and diastase resistant
Comment Here
Reference: Solid pseudopapillary neoplasm
Comment Here
Reference: Solid pseudopapillary neoplasm