Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Lee JTH, Gupta R. Oncocytoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsoncocytoma.html. Accessed September 17th, 2025.
Definition / general
- Benign tumor of salivary gland origin
- Exclusively or predominantly composed of oncocytes
- Accounts for 1 - 2% of salivary gland neoplasms
Essential features
- Rare, benign salivary gland neoplasm
- Usually unilateral and mostly occurs in parotid
- Tumor is composed exclusively or predominantly of oncocytes
- Cytoplasm is eosinophilic and granular due to the presence of abundant mitochondria within the cytoplasm
- Can be positron emission tomography (PET) avid
- Treated with local excision
Terminology
- Oncocytic adenoma, oxyphilic adenoma
ICD coding
Epidemiology
- Rare; constitutes < 2% of all salivary gland neoplasms (Head Neck Pathol 2024;18:126)
- Age group: 60 - 80 years old
- No sex predilection
Sites
- Most (> 80%) occur in the parotid; ~10% occur in the submandibular gland
- The rest occur in the sublingual gland, minor salivary glands and respiratory tract
Pathophysiology
- Pathogenesis remains unclear; could be neoplastic / hyperplastic or metaplastic growth
- Oncocytoma may arise in the background of multinodular oncocytic hyperplasia
- Eosinophilic granular cytoplasm of oncocytes is due to the presence of increased intracytoplasmic mitochondrial content
- Reference: Ann Maxillofac Surg 2018;8:330
Etiology
- Associated with radiation exposure or radiotherapy
- Smoking
- Older age
- Reference: Head Neck Pathol 2024;18:126
Clinical features
- Usually presents as a unilateral, slow growing, painless and solitary mass
- Rarely bilateral (Cancer Diagn Progn 2024;4:814)
- Rarely presents with obstructive symptoms if occurring in the nasal or respiratory tract
- Rarely occurs in Birt-Hogg-Dubé syndrome (BHD) (Case Rep Radiol 2018;2018:6265175, Head Neck Pathol 2024;18:52)
Diagnosis
- Typically requires histopathologic examination for definitive diagnosis
- Fine needle aspiration cytology along with clinical and radiologic correlation can often suggest the diagnosis
Radiology description
- Ultrasound: sonographic features are nonspecific and include (J Ultrasound 2021;24:241)
- Ovoid mass, usually homogeneously hypoechoic but can be heterogeneous
- Typically well defined, occasionally lobulated
- Vascular
- Computed tomography (CT): often seen as a well defined mass showing homogeneous enhancement (AJNR Am J Neuroradiol 2010;31:1413)
- Magnetic resonance imaging (MRI): appearance can be variable (J Ultrasound 2021;24:241)
- T1: hypointense
- T2: isointense to hypointense
- T1C+: isointense
- PET FDG: high fluorodeoxyglucose (FDG) uptake (due to mitochondrial accumulation) (J Ultrasound 2021;24:241)
Prognostic factors
- Favorable prognosis of a benign tumor following removal
- Low risk for local recurrence
- Malignant transformation is extremely rare
- Reference: Head Neck Pathol 2024;18:126
Case reports
- 73 year old man with right parotid swelling for 35 years (J Oral Maxillofac Pathol 2023;27:S41)
- Case series of submandibular gland swelling (J Maxillofac Oral Surg 2023;22:127)
Treatment
- Complete surgical removal is the treatment of choice (Head Neck Pathol 2024;18:126)
Gross description
- Usually tumor presents as well circumscribed, lobulated, reddish brown nodules
- Mean tumor size is 19.8 mm (AJNR Am J Neuroradiol 2010;31:1413)
- Major salivary glands: tumor is usually encapsulated and solid
- Minor salivary glands: tumor is unencapsulated and less well delineated; cystic change may be present
Gross images
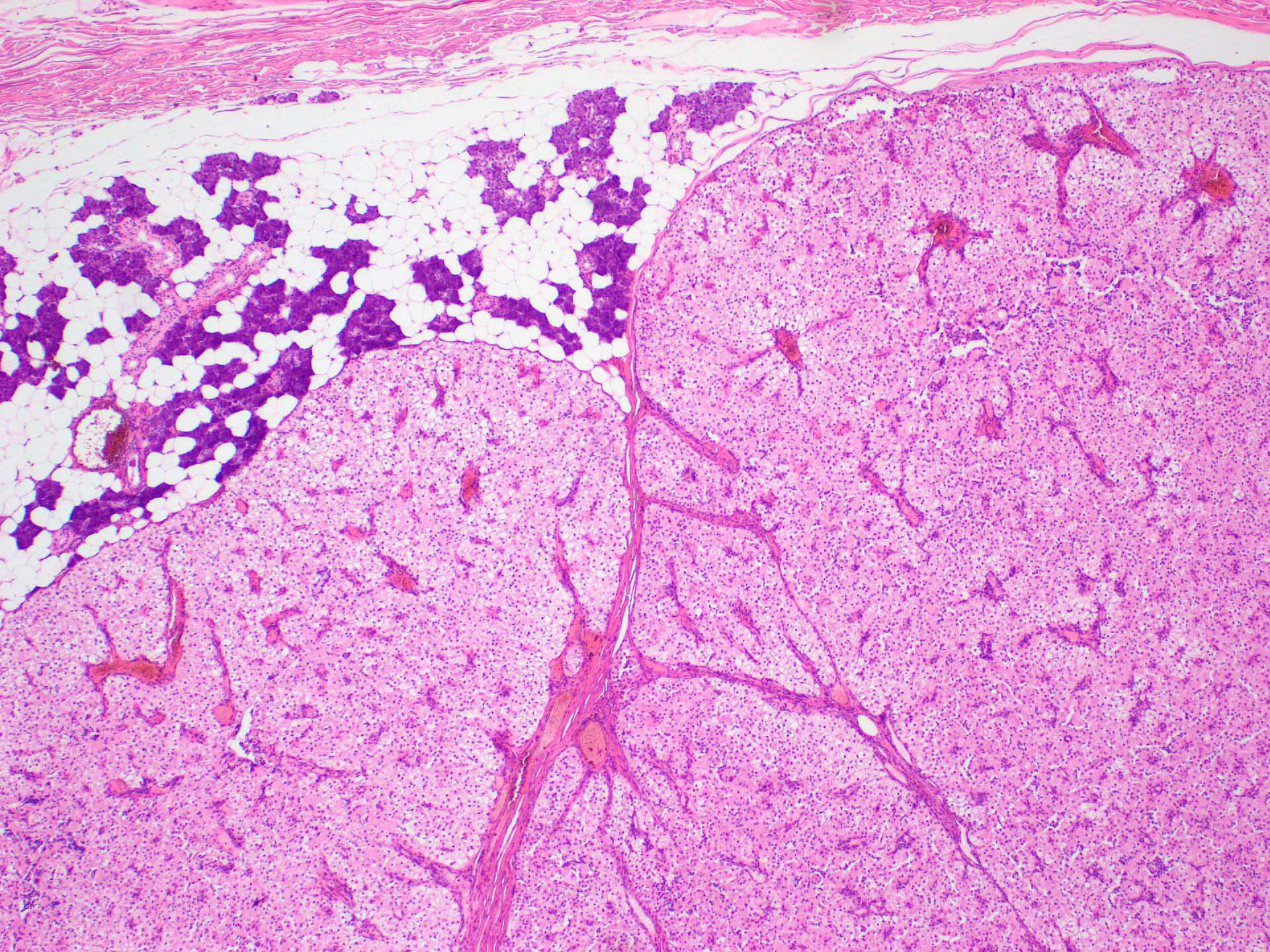
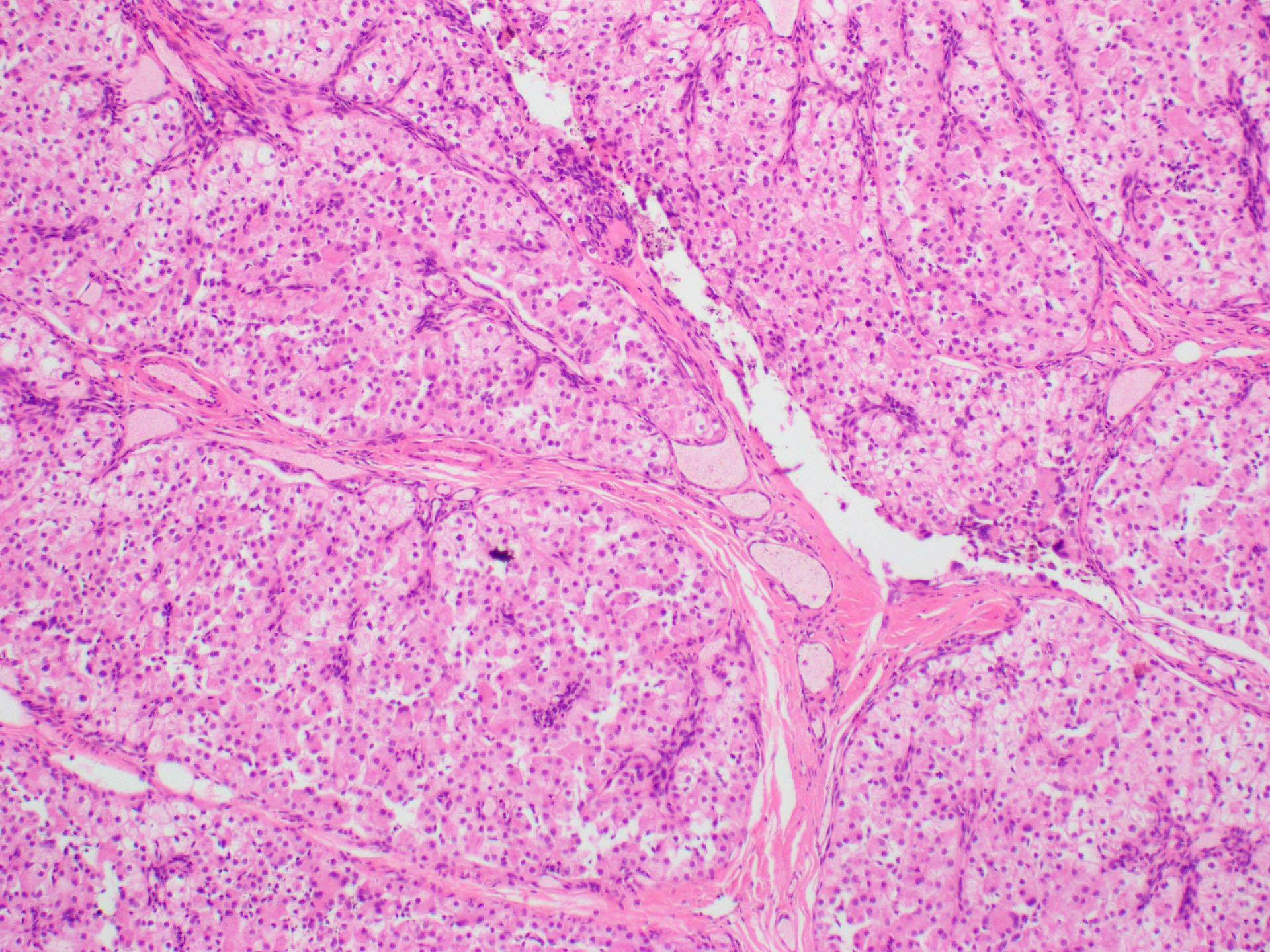
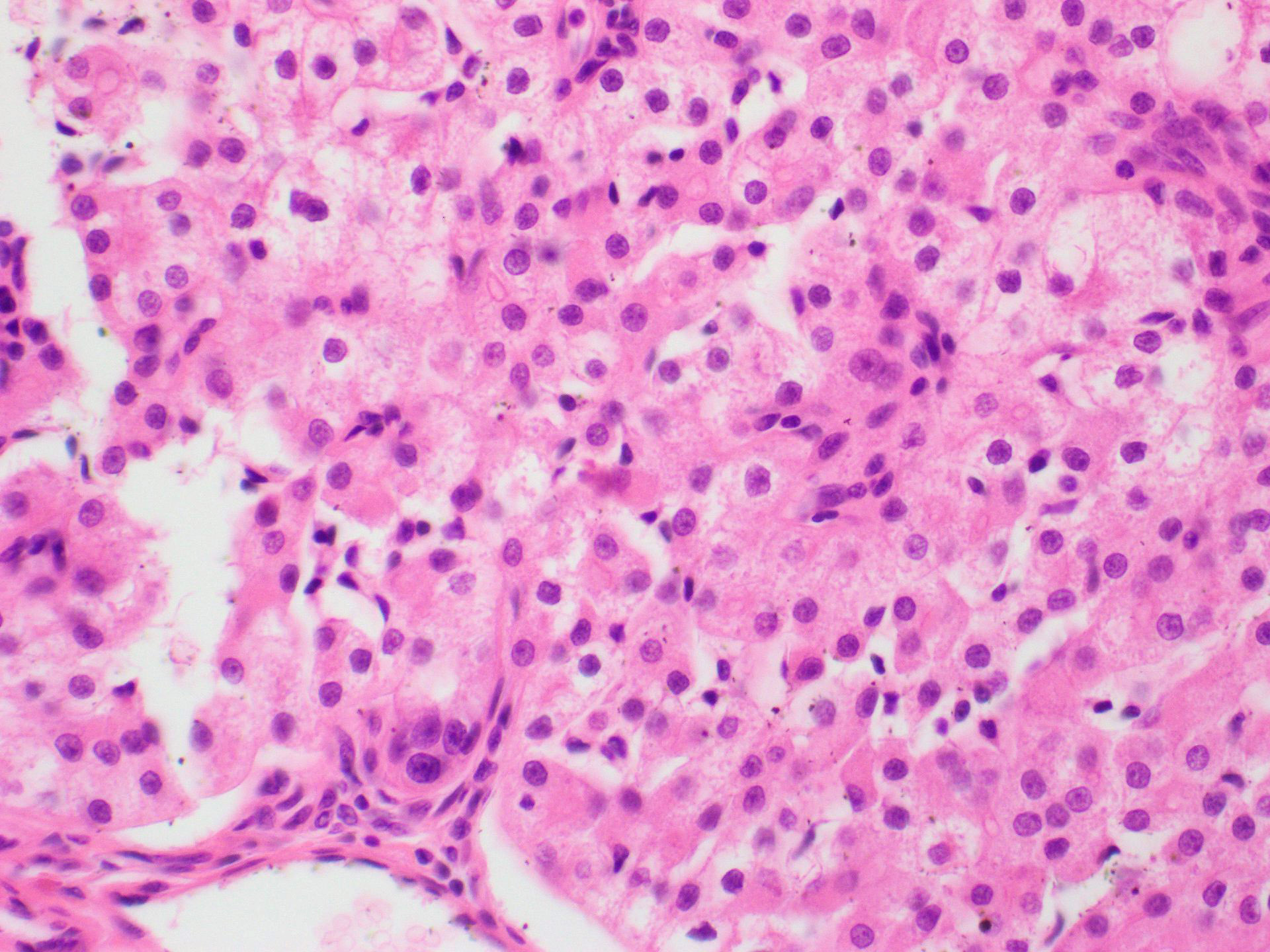
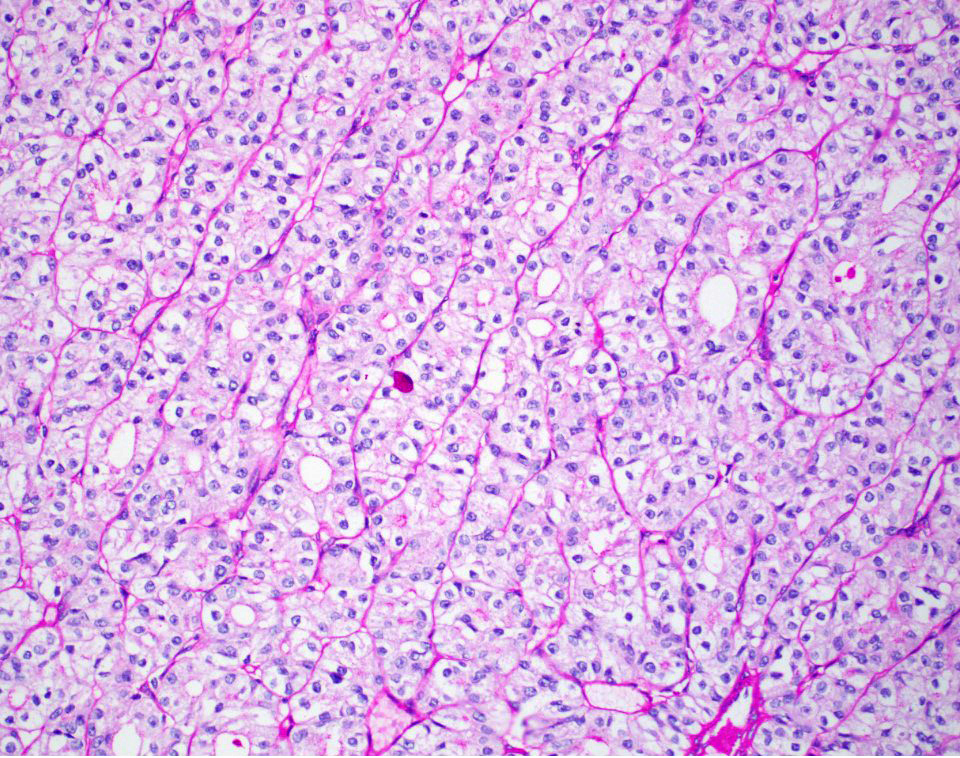
Microscopic (histologic) description
- Generally a well circumscribed nodule; may lack circumscription in the minor salivary glands
- Solid sheets, nested, trabecular or ductular architecture; microcysts and macrocysts are rare
- Exclusively or predominantly composed of oncocytes and separated by thin fibrovascular septae
- Oncocytes are large, polyhedral shaped with distinct cell membranes and abundant granular eosinophilic cytoplasm (Head Neck Pathol 2024;18:126)
- Nuclei are centrally located, round, vesicular with prominent nucleoli
- Absence of significant nuclear pleomorphism, increased mitoses and necrosis
- Absence of infiltrative growth
- Psammoma bodies and tyrosine-like crystals may be present
- Other cell types that may present in limited quantity within the tumor, especially following a fine needle aspiration: mucous cells, squamous cells or sebaceous cells
- Basal cells can be seen at the periphery of the tumor
- Clear cell oncocytoma is a histologic variant that consists entirely or predominantly of clear cells
- Reasons for clear cytoplasm
- Fixation and tissue processing artifact
- Accumulated glycogen content that displaces the mitochondria to the periphery of cells
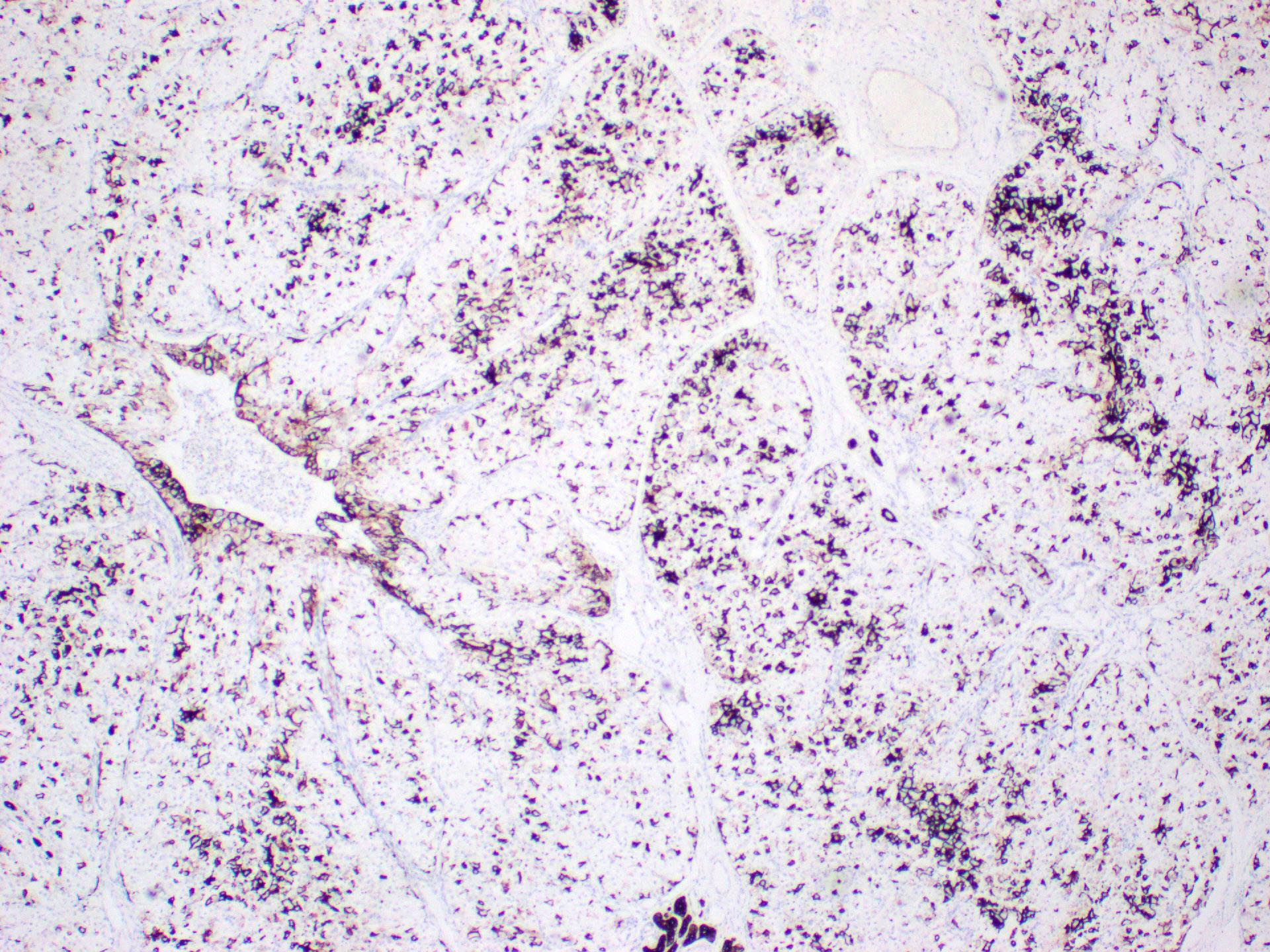
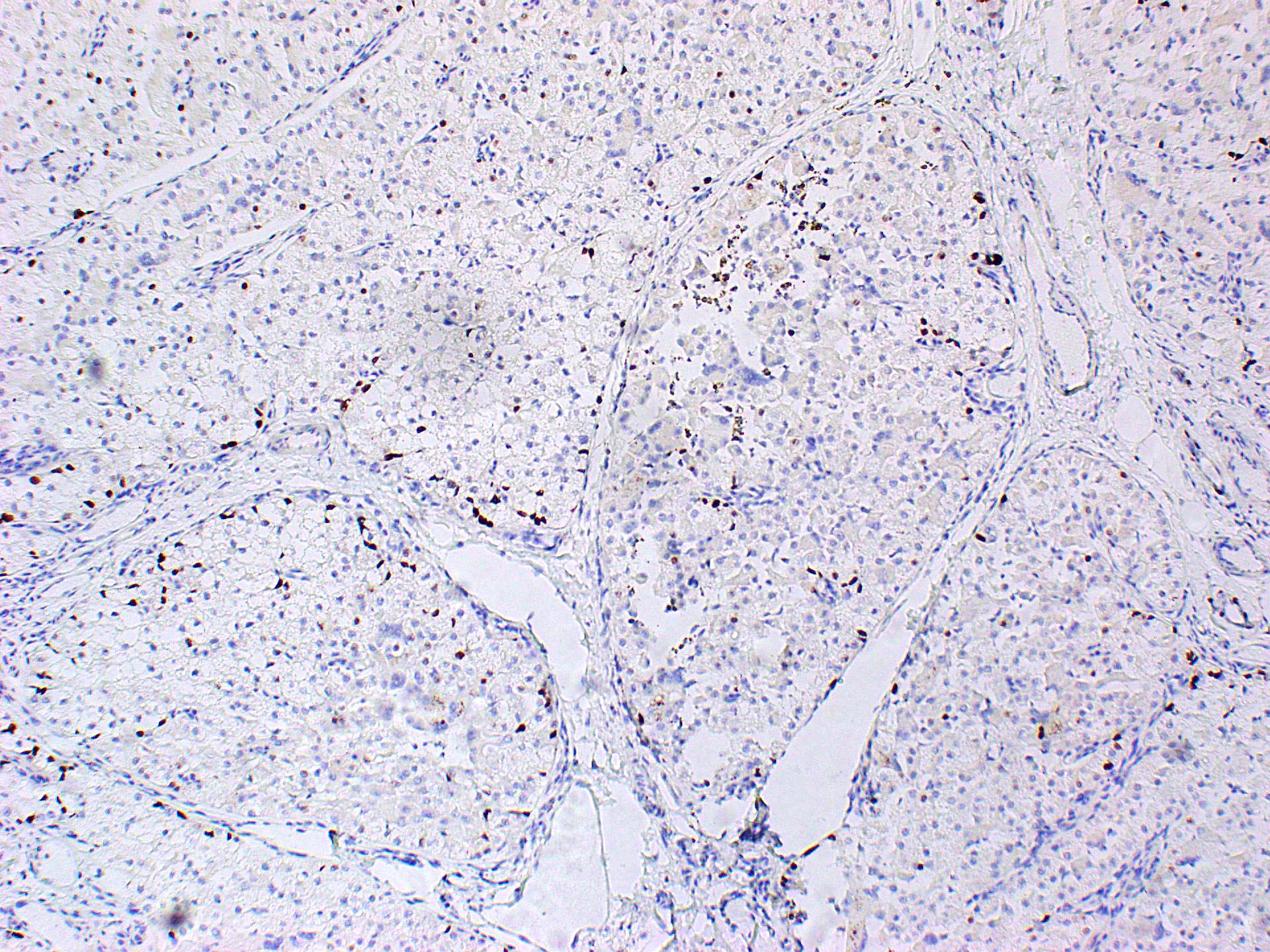
Microscopic (histologic) images
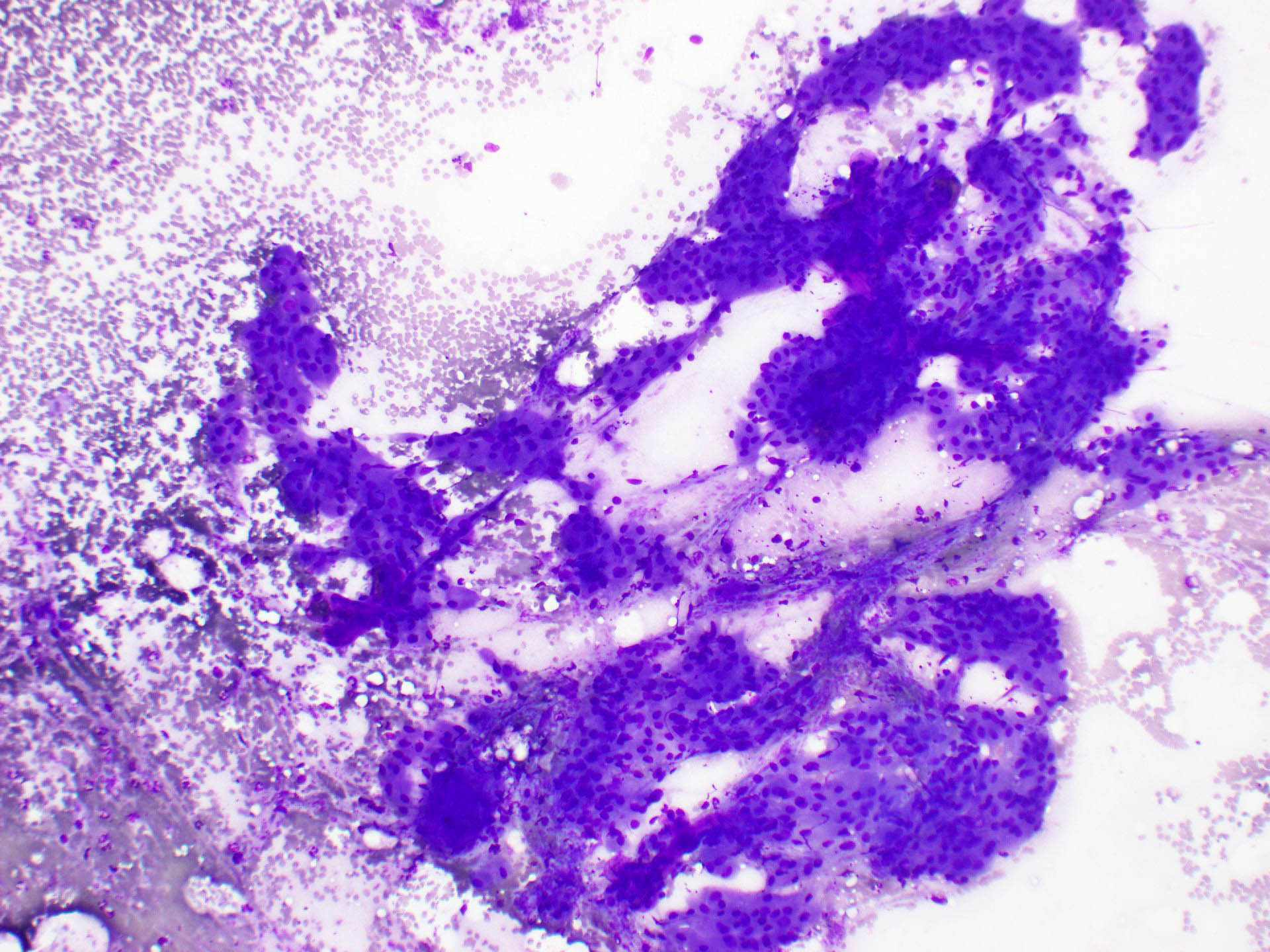
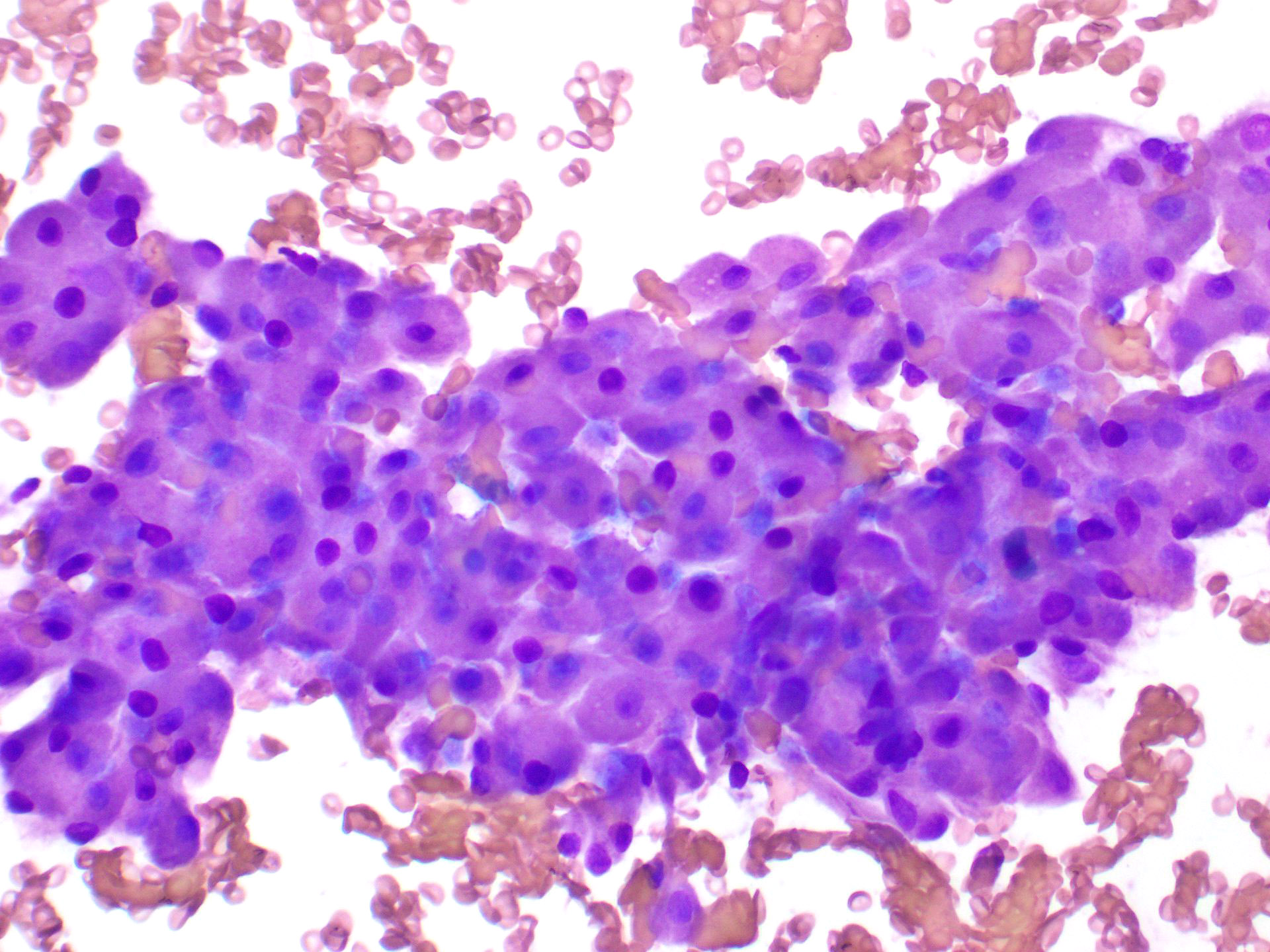
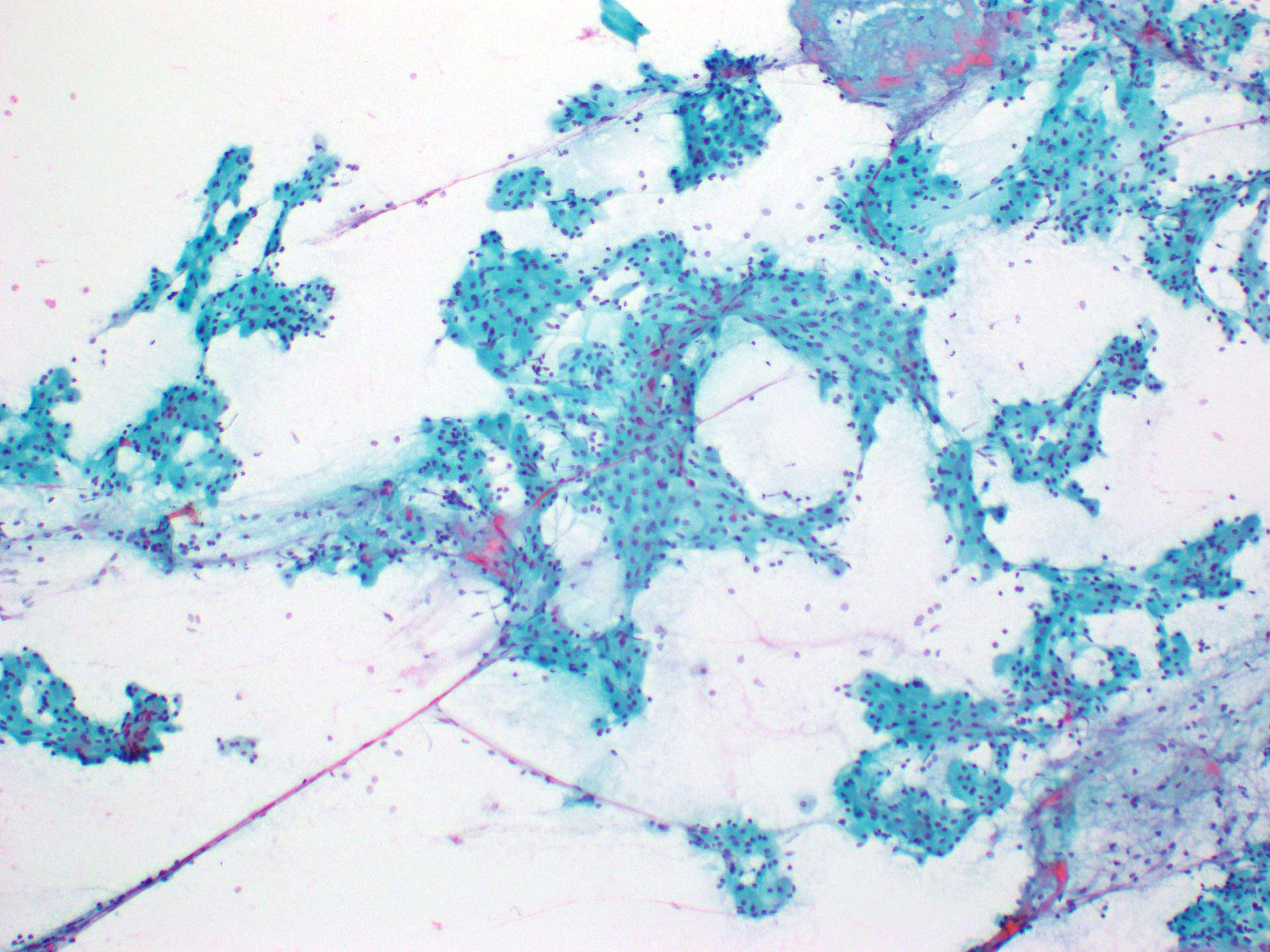
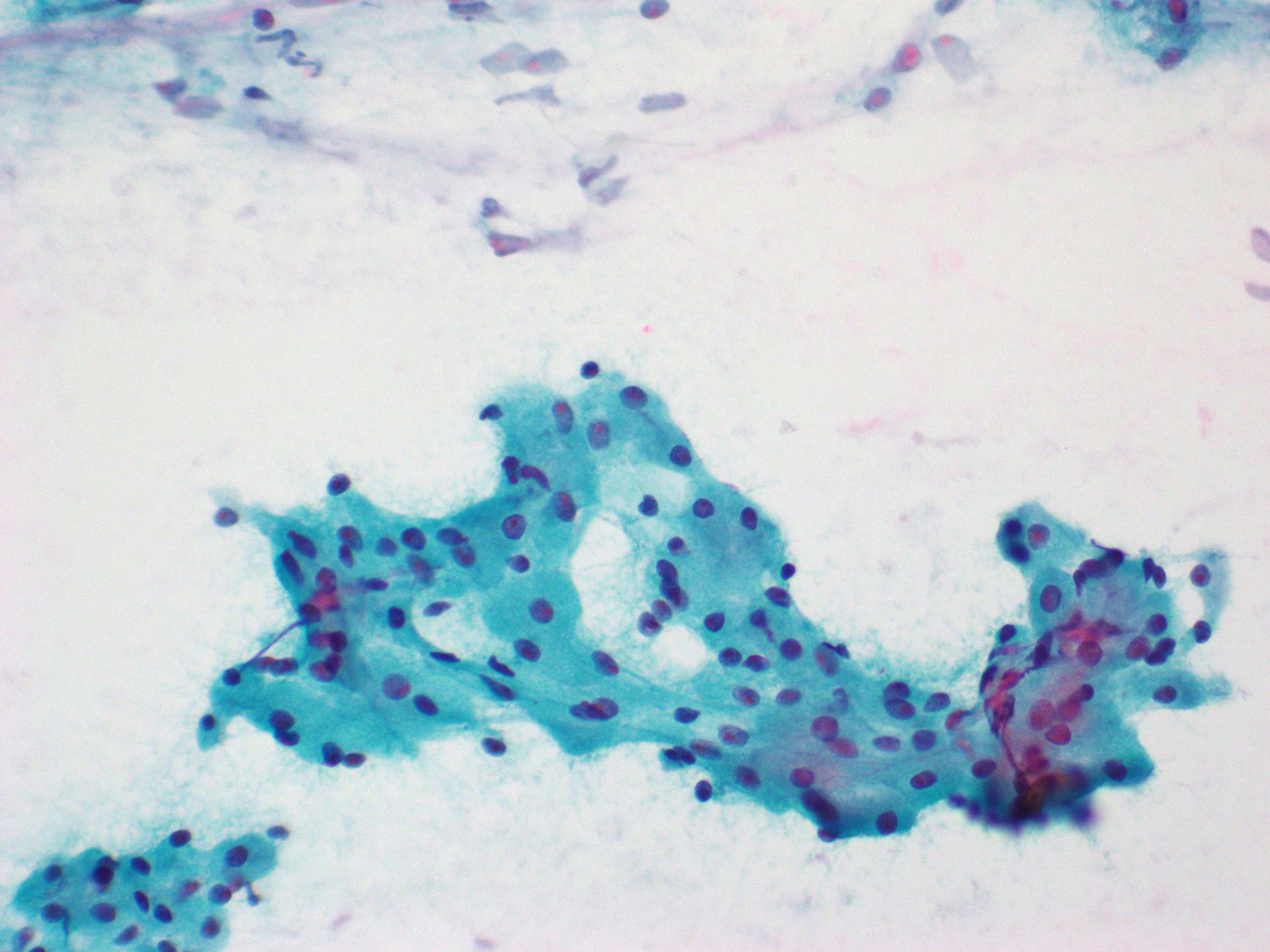
Cytology description
- Smears are usually cellular
- Oncocytes (cells with granular eosinophilic cytoplasm) are arranged in sheets, papillary fragments and individual cells
- Cytologic atypia is absent to minimal
- Absence or very sparse lymphoid component
- Distinction of oncocytoma from oncocytosis or another salivary gland lesion with prominent oncocytic metaplasia may not be possible on cytology alone
- Reference: Head Neck Pathol 2024;18:126
Cytology images
Positive stains
Negative stains
Electron microscopy description
- Cytoplasm of the oncocytes is packed with abundant mitochondria, which are oval or elongated in shape with stacked cristae
- Other organelles, such as endoplasmic reticulum and Golgi complex, are sparse
- Continuous basement membrane around cell clusters
- Reference: Cancer 1976;37:1606
Electron microscopy images
Sample pathology report
- Left parotidectomy:
- Oncocytoma with background multinodular oncocytic hyperplasia (see comment)
- Comment: There is a dominant encapsulated oncocytic nodule. The salivary gland parenchyma shows occasional scattered microscopic oncocytic nodules. There is no evidence of malignancy.
Differential diagnosis
- Oncocytic metaplasia:
- Metaplastic change
- No mass forming lesion
- Ductal and acinar epithelium transformed into oncocytes due to metaplastic process in aging
- Oncocytosis:
- Proliferation of oncocytic cells within the salivary glands
- Often presents as multiple microscopic oncocytic nodules (nodular oncocytic hyperplasia)
- Difficulty in differentiating oncocytoma from diffuse oncocytosis with detectable mass
- Nonencapsulation, multiple nodules and presence of entrapped normal salivary gland parenchyma assist in distinction from oncocytoma
- Pleomorphic adenoma with extensive oncocytic cells:
- Primary salivary gland carcinomas predominantly composed of oncocytic cells:
- Oncocytic mucoepidermoid carcinoma:
- Acinic cell carcinoma (zymogen poor variant):
- Tumor cells are PAS positive, PASD resistant
- They are also positive for DOG1, SOX10 and NOR1 / NR4A3
- Salivary duct carcinoma (oncocytic variant):
- Aggressive and infiltrative tumor frequently involving adjacent structures
- Tumor cells have apocrine phenotype: cytoplasm is granular and eosinophilic and nuclei are large, pleomorphic with prominent nucleoli
- Perineural and lymphovascular invasion is present
- Tumor cells are positive for AR; HER2 is positive in about 30% of cases
- Clear cell carcinoma:
- Usually occurs in minor salivary glands, such as soft palate, buccal and floor of mouth
- Tumor is infiltrative, usually composed of tumor cells with clear cytoplasm within densely hyalinized stroma; perineural invasion may be present
- Diffuse staining for p63, p40 and CK5/6
- Positive for EWSR1 gene rearrangement
- Metastatic renal cell carcinoma:
- Thyroid oncocytic carcinoma:
- Positive for thyroglobulin and TTF1
Additional references
Practice question #1
Which of the following statements regarding oncocytoma of the salivary gland is true?
- The tumor is common in young patients
- The tumor is malignant
- The tumor is positive for PAX8
- The tumor is rare and occurs mostly in the parotid gland
Practice answer #1
D. The tumor is rare and occurs mostly in the parotid gland. Oncocytoma constitutes about 1 - 2% of salivary gland neoplasms and mostly occurs in the parotid gland, followed by the submandibular gland and minor salivary gland. Answer A is incorrect because this tumor occurs mostly in middle aged to older people. Answer B is incorrect because oncocytoma is benign. Answer C is incorrect because oncocytoma is PAX8 negative, which is useful in differentiating this tumor from metastatic renal cell carcinoma.
Comment Here
Reference: Oncocytoma
Comment Here
Reference: Oncocytoma
Practice question #2
Which of the following statements about oncocytic cells in oncocytoma of the salivary gland is true?
- Cytology can differentiate oncocytosis from oncocytoma
- FISH analysis is positive for MAML2 rearrangement
- Oncocytic cells are diffusely positive for p63, p40 and CK5/6
- The main organelle in the cytoplasm of oncocytic cells is the mitochondria
Practice answer #2
D. The main organelle in the cytoplasm of oncocytic cells is the mitochondria. The presence of increased intracytoplasmic mitochondrial content contributes to the eosinophilic granular cytoplasm of oncocytes. Answer C is incorrect because oncocytic cells are predominantly positive for cytokeratins such as CK7 and EMA but very focally positive for p63, p40 and CK5/6, which is useful in differentiating this tumor from mucoepidermoid carcinoma. Answer A is incorrect because cytology cannot differentiate oncocytosis from oncocytoma. Answer B is incorrect because MAML2 rearrangement is seen in mucoepidermoid carcinoma.
Comment Here
Reference: Oncocytoma
Comment Here
Reference: Oncocytoma