Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Diagrams / tables | Clinical features | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosisCite this page: Ellis C, Rollins M. Clear cell sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumorclearcellsarcoma.html. Accessed April 26th, 2024.
Definition / general
- Clear cell sarcoma of the kidney (CCSK) is composed of uniform, small round cells with a clear appearance and evenly distributed fine chromatin separated by a delicate vascular network (eMedicine)
- First described in 1978 by three distinct groups: Beckwith and Palmer (Cancer 1978;41:1937), Morgan and Kidd (Cancer 1978;42:1916), and Marsden and coworkers (Cancer 1978;42:1922); it was initially named "bone metastasizing renal tumor of childhood" since it has predilection for skeletal metastasis (J Neonatal Surg 2014;3:35)
- Most frequently misdiagnosed renal tumor in children, as it is unusual, has varied morphology and there are no specific diagnostic markers (J Neonatal Surg 2014;3:35)
Essential features
- Typically a male child, half are diagnosed at 2 - 3 years of age
- Many histological variants exist (see below), but the classic histological appearance is nests or cords of small, plump cells separated by networks of delicate vascular septa
- Clear cells occur in only 20% of cases, despite its name
- Immunohistochemistry has limited use: it is usually only positive for vimentin, although Cyclin D1 may be useful (as of 2015, see below)
- The most important drug treatment is Doxorubicin (Adriamycin®)
- Recent molecular advances in CCSK tumorigenesis have implicated the BCOR gene (see below)
ICD coding
- ICD-10: C64.9 - malignant neoplasm of unspecified kidney, except renal pelvis
Epidemiology
- Rare (20 cases per year); 3% - 5% of all pediatric renal tumors
- Mean age of diagnosis is 36 months (range, 2 months - 14 years), half are diagnosed at 2 - 3 years of age (Am J Surg Pathol 2000;24:4)
- Rarely diagnosed in adolescents / adults (Am J Surg Pathol 1999;23:1455)
- 2 / 3 male
Clinical features
- Bone metastases occur in 17% - 40% of patients with CCSK, vs. <2% in Wilm tumor (J Neonatal Surg 2014;3:35)
- 5% of patients have metastatic disease at presentation including bone, lung, brain and liver
- Overall, survival varies with stage (5 year survival is 97% for stage I vs. 50% for stage IV, Am J Surg Pathol 2000;24:4)
Prognostic factors
- Four important prognostic factors are:
- Doxorubicin treatment
- Stage
- Age at diagnosis
- Presence of tumor necrosis (J Postgrad Med 2001;47:206)
- Stage IV disease and young age are significant adverse prognostic factors for event free survival (Eur J Cancer 2013;49:3497)
Case reports
- Congenital tumor with metastases (Virchows Arch 2005;446:566)
Treatment
- Total nephrectomy followed by postoperative chemotherapy and flank radiation therapy (RT) (Eur J Cancer 2013;49:3497)
- Highly responsive to combination treatment with doxorubicin, vincristine and actinomycin, with doxorubicin the most important (eMedicine)
- The essential role of doxorubicin in therapy emphasizes the need for pathologists to accurately identify CCSK (Am J Surg Pathol 2000;24:4)
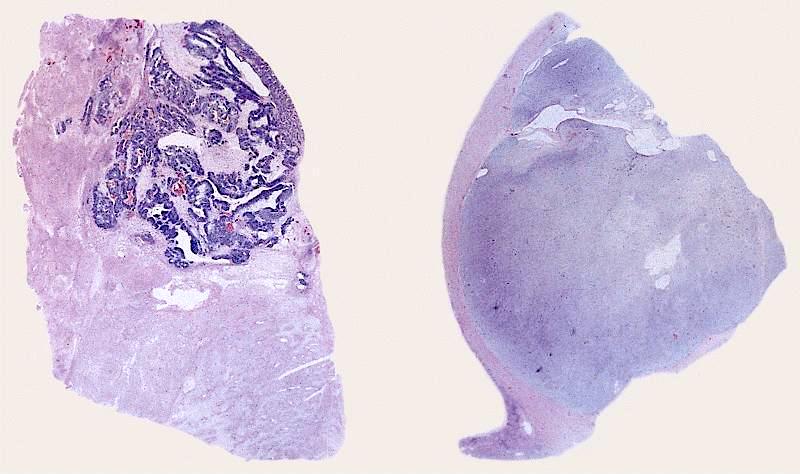
Gross description
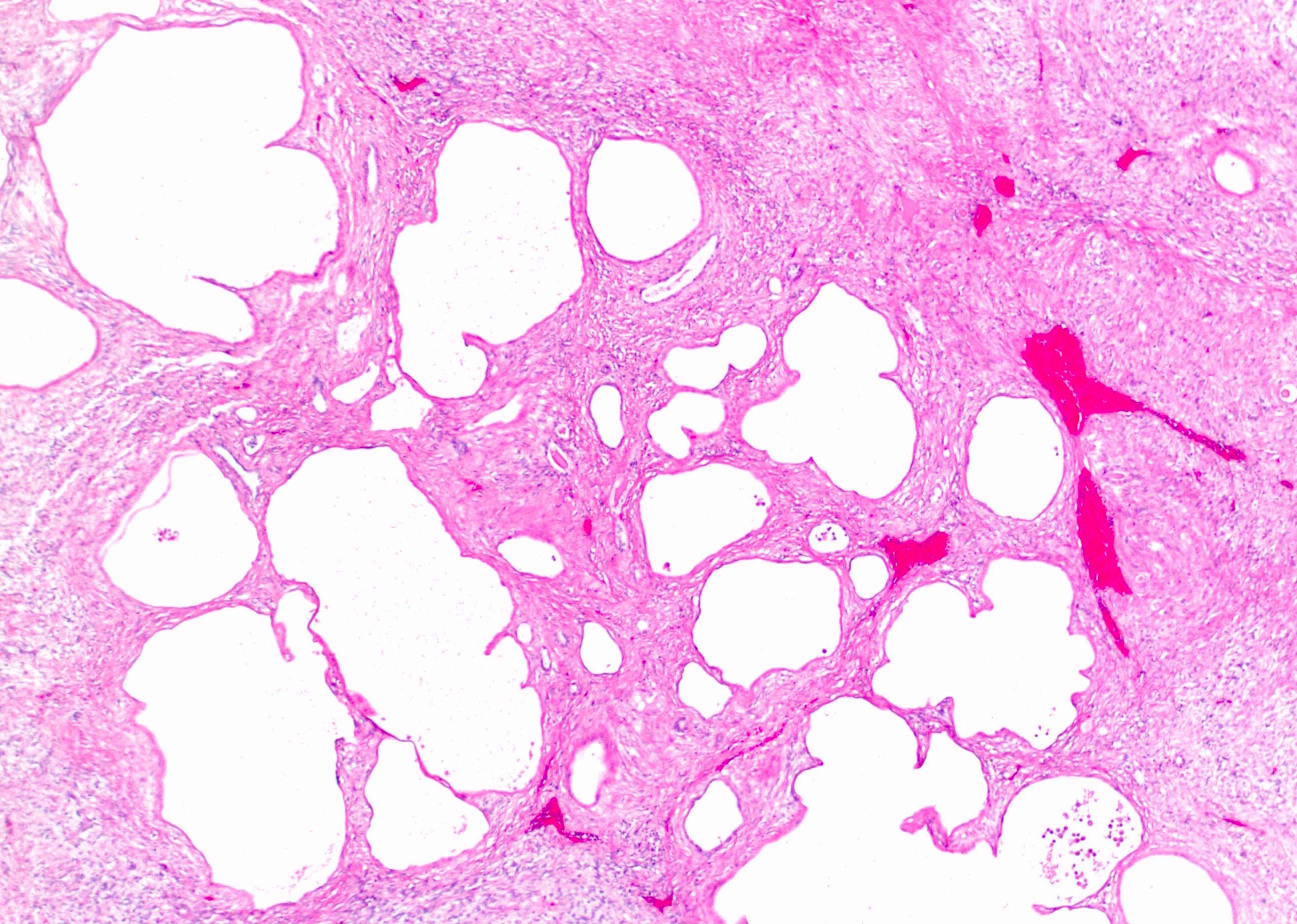
- Unilateral and unicentric mass with irregular but sharp tumor / kidney interface
- Large (mean 11 cm); centered in central kidney or medulla
- Cut surface is homogenous tan / gray or gelatinous and firm with occasional cysts
Microscopic (histologic) description
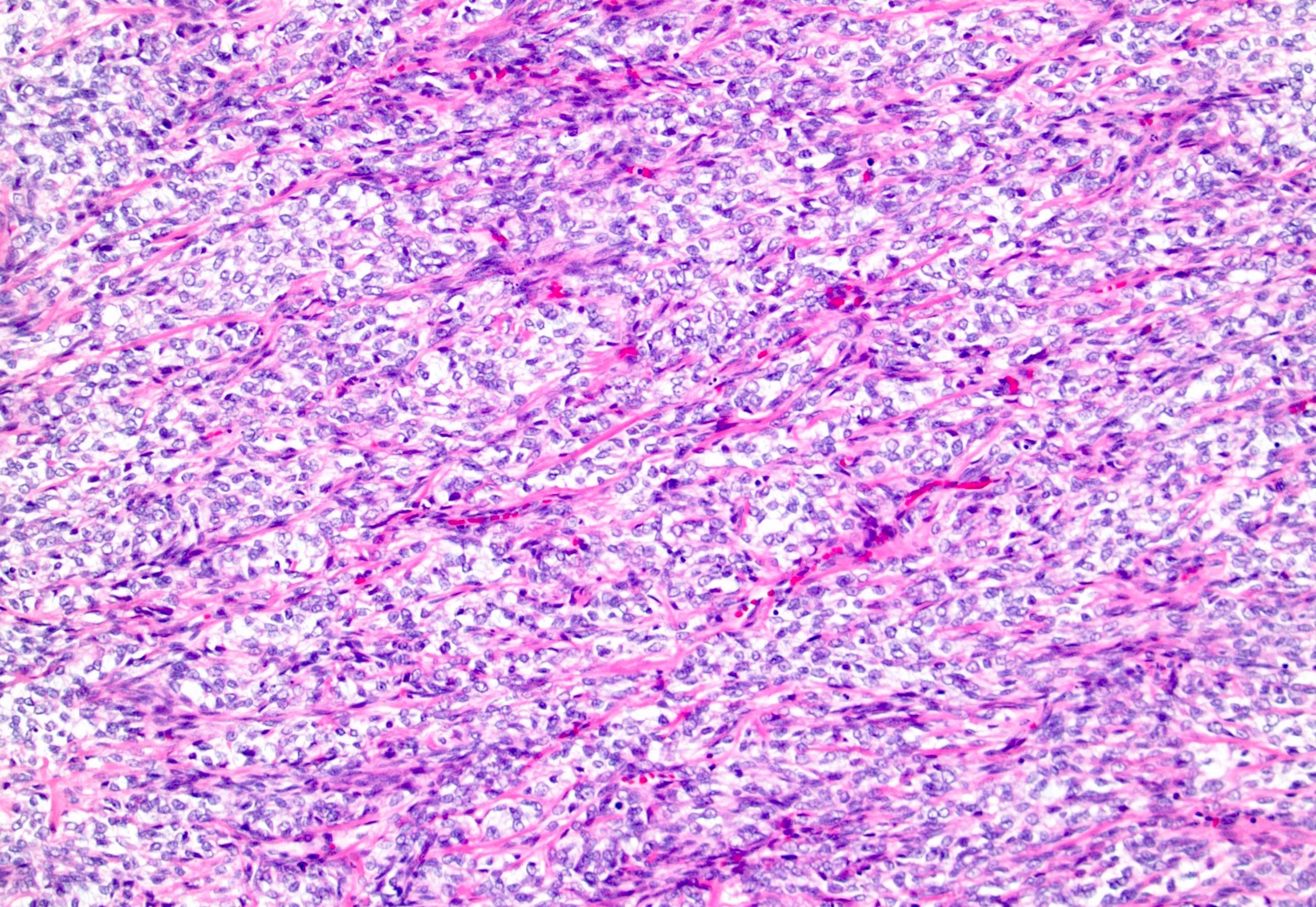
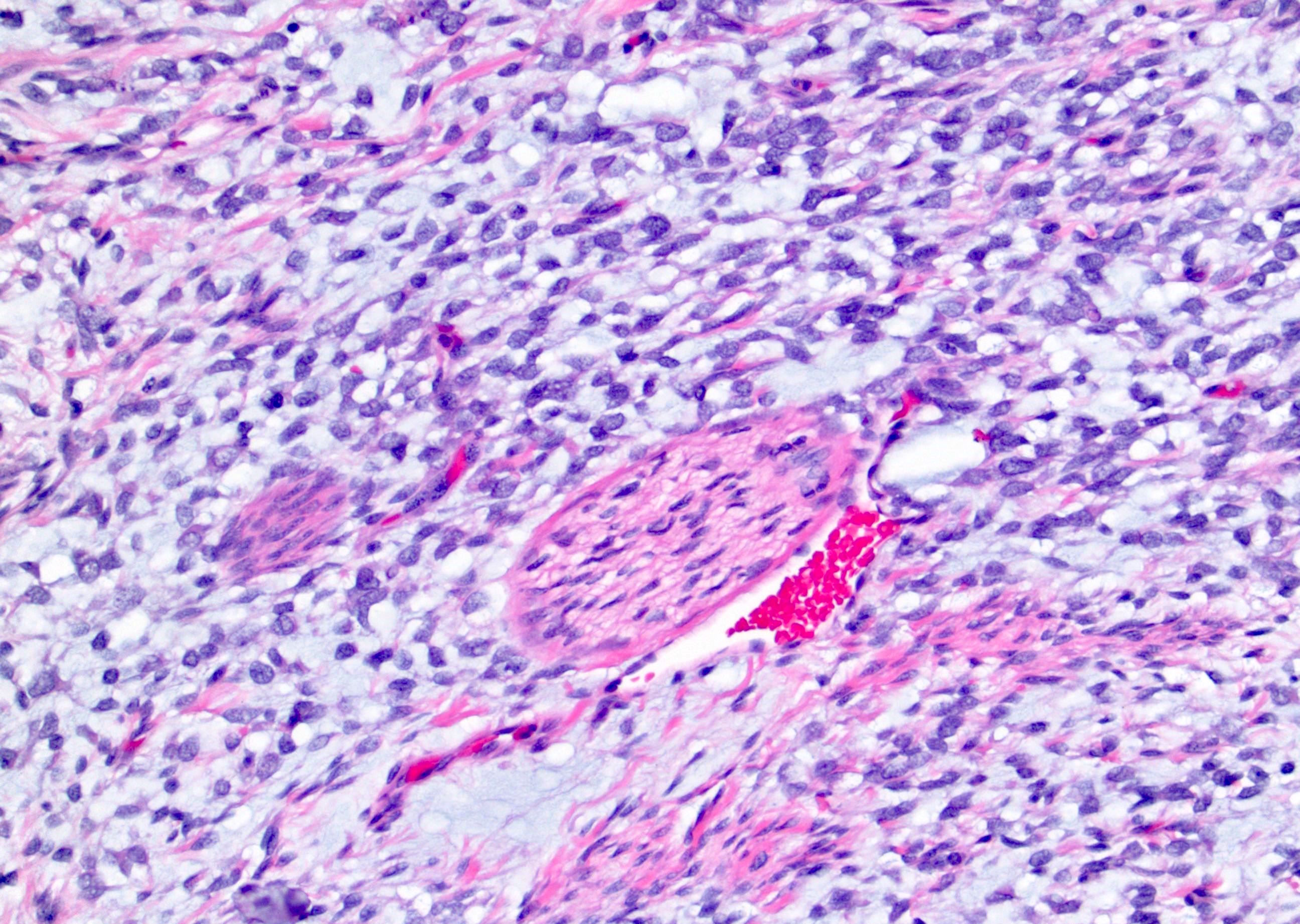
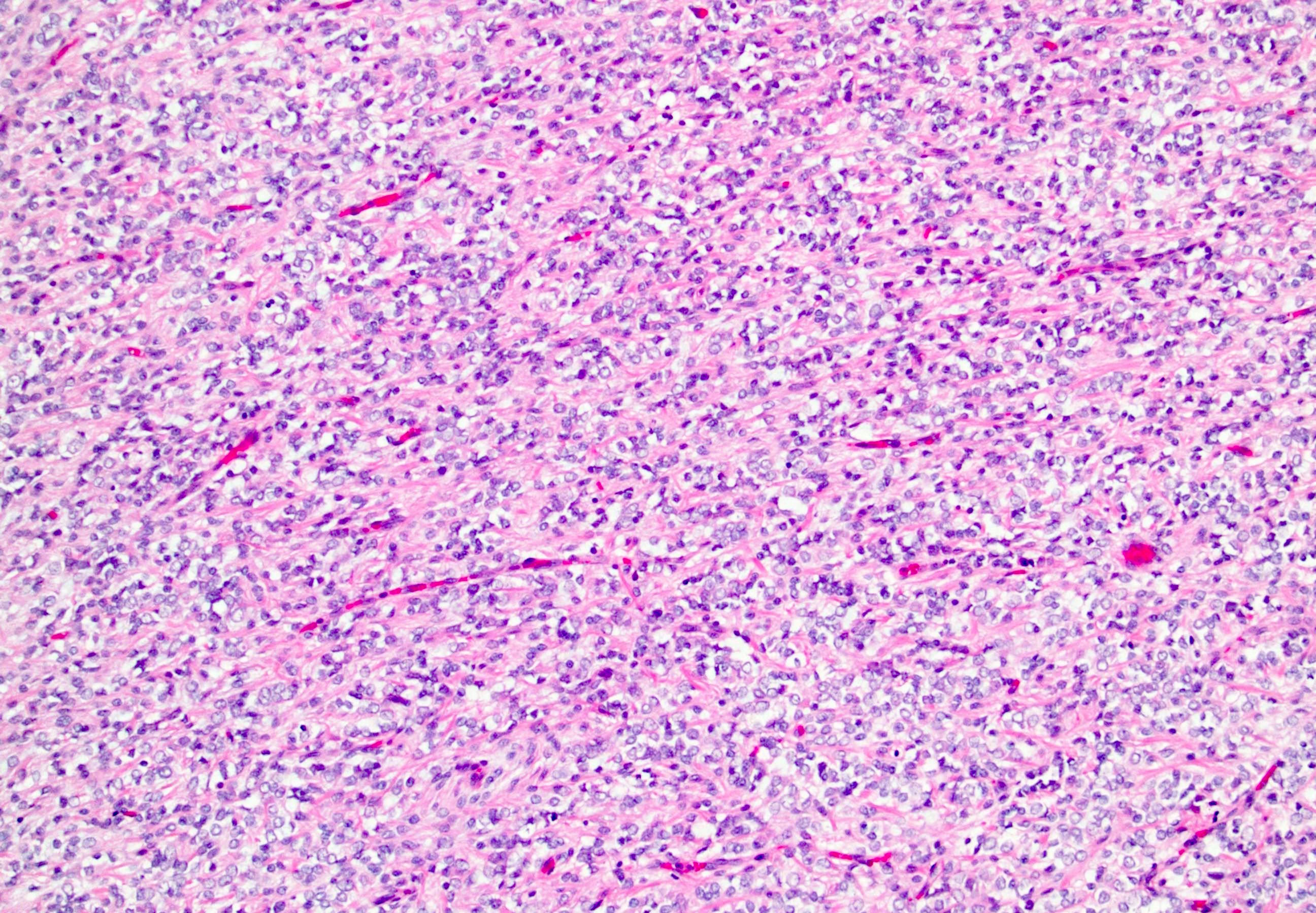
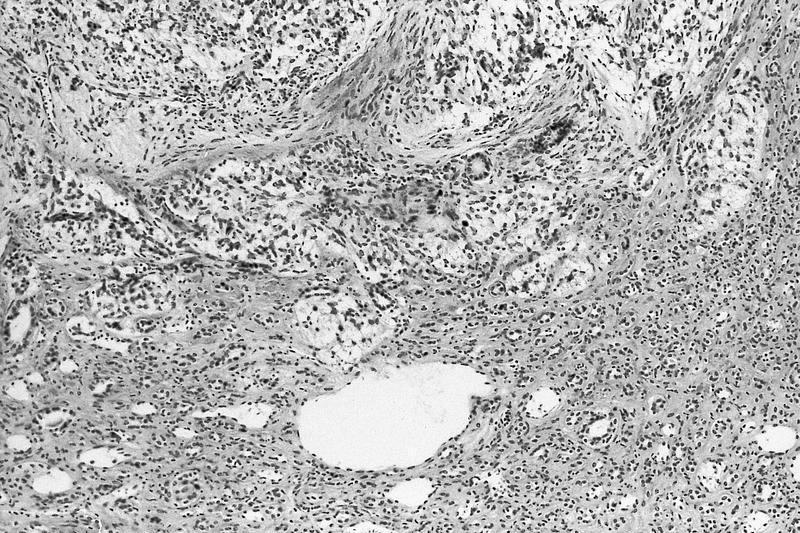
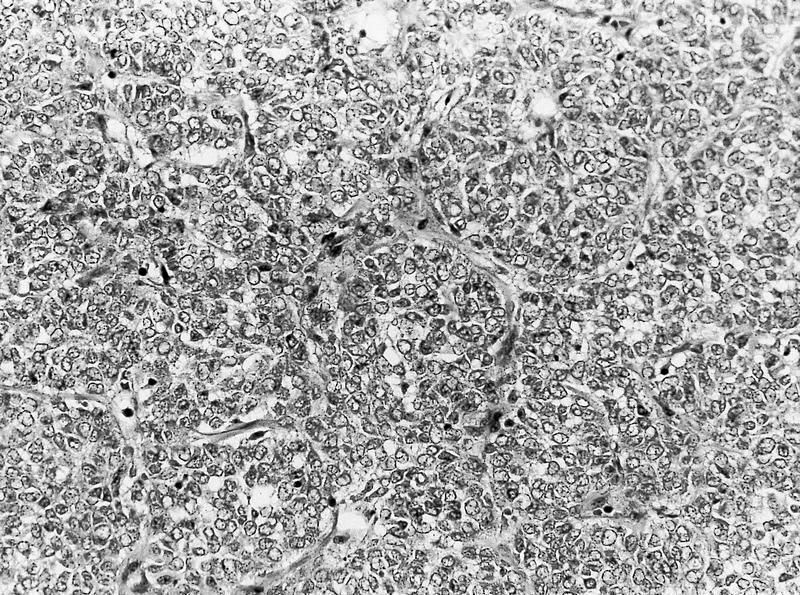
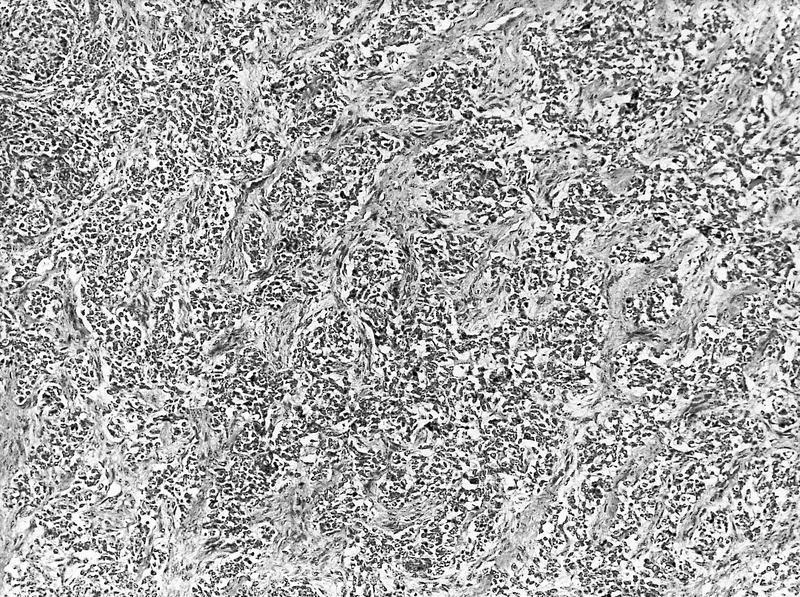
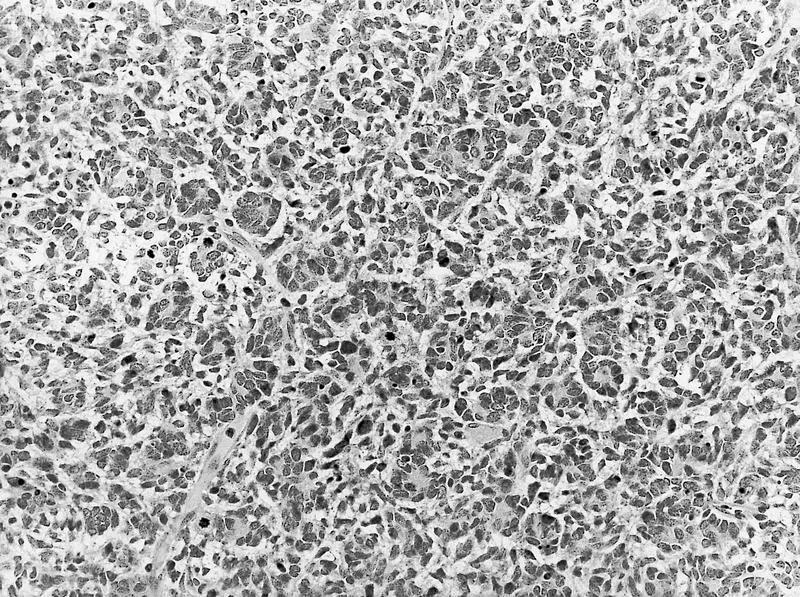
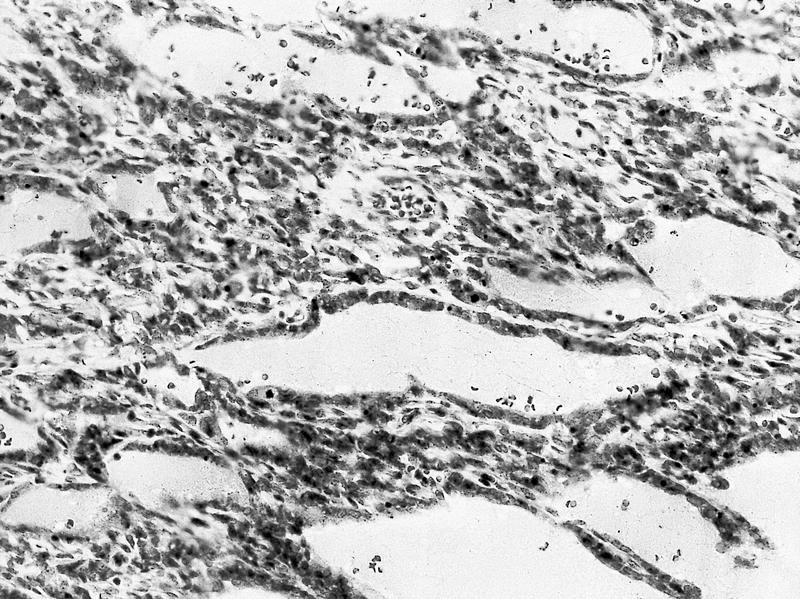
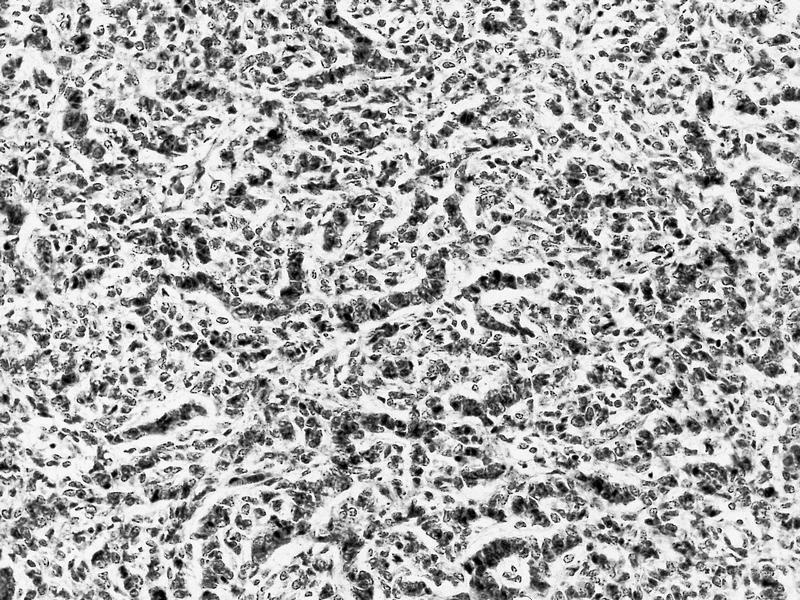
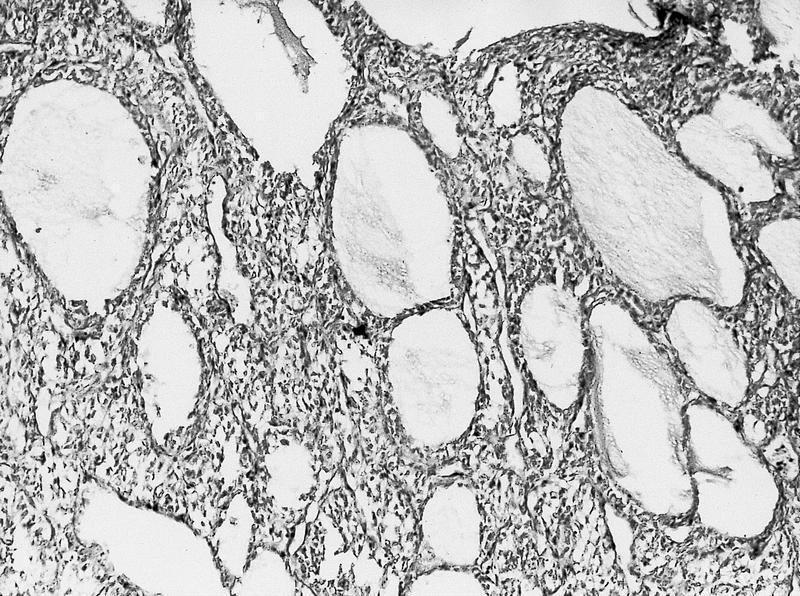
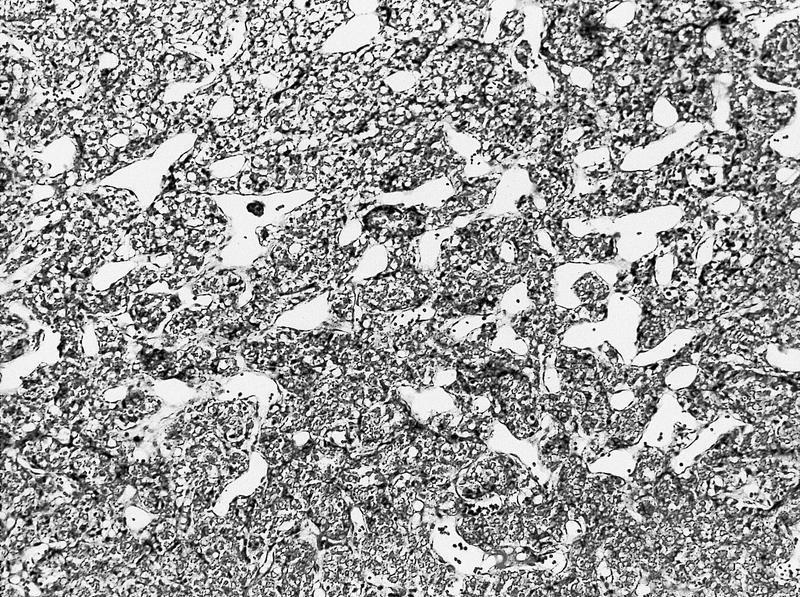
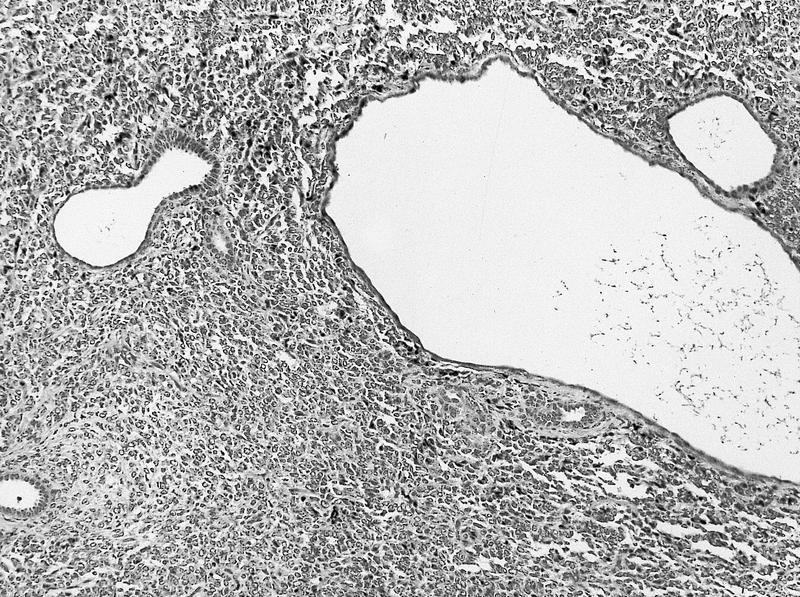
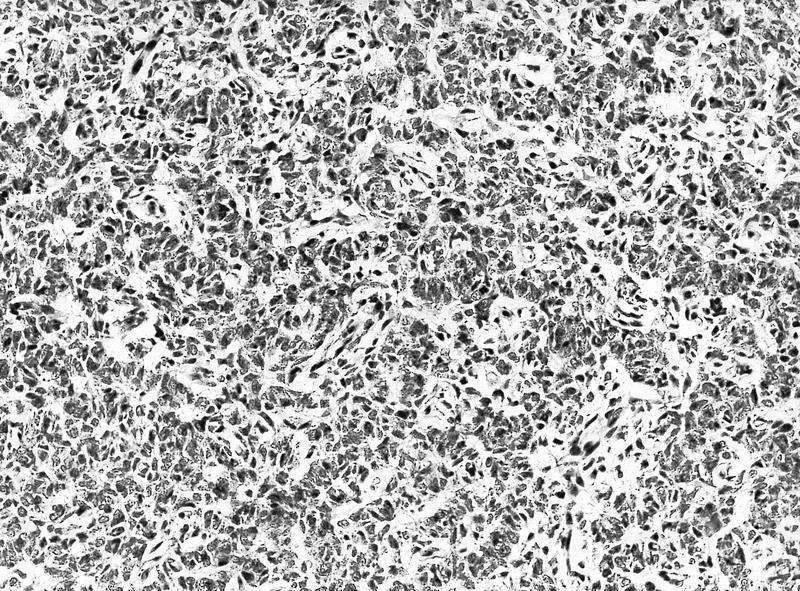
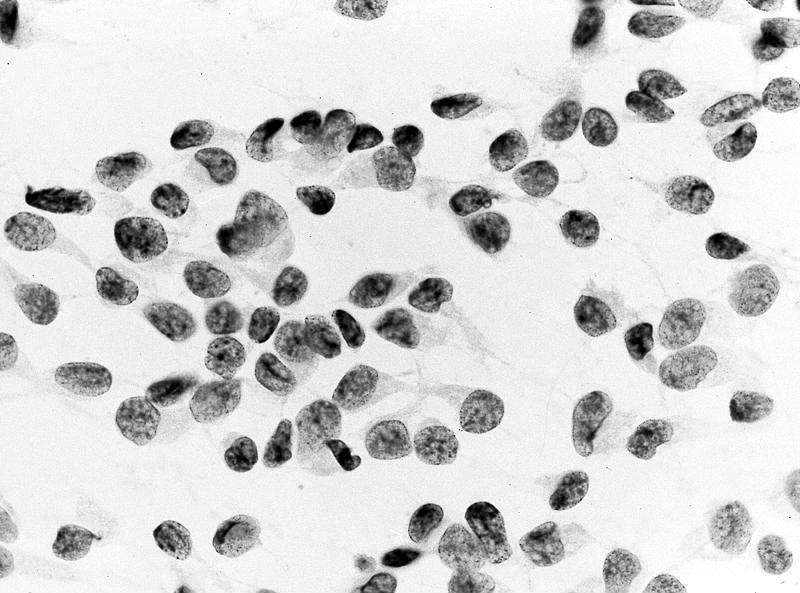
- Classic pattern: nests or cords of small, plump cells separated by network of delicate vascular septa (also called chicken wire capillaries)
- This pattern is almost always focally present, but other patterns may be present
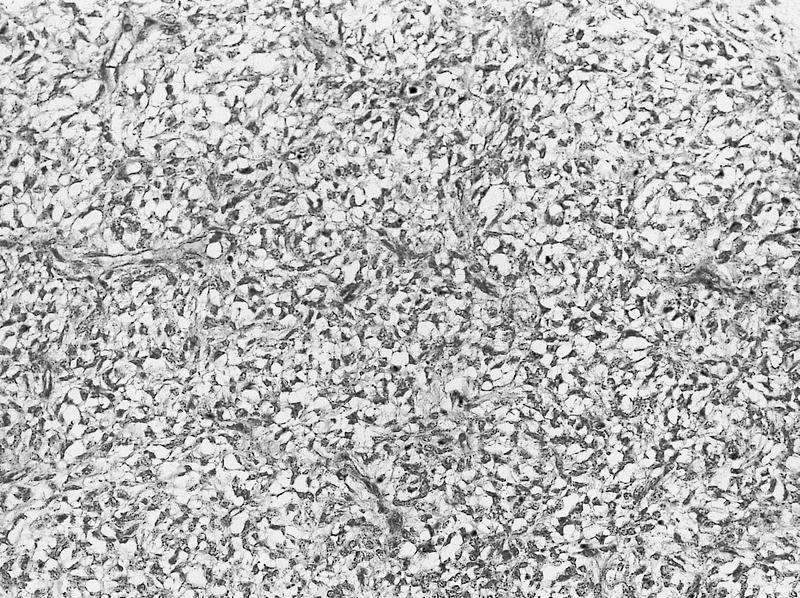
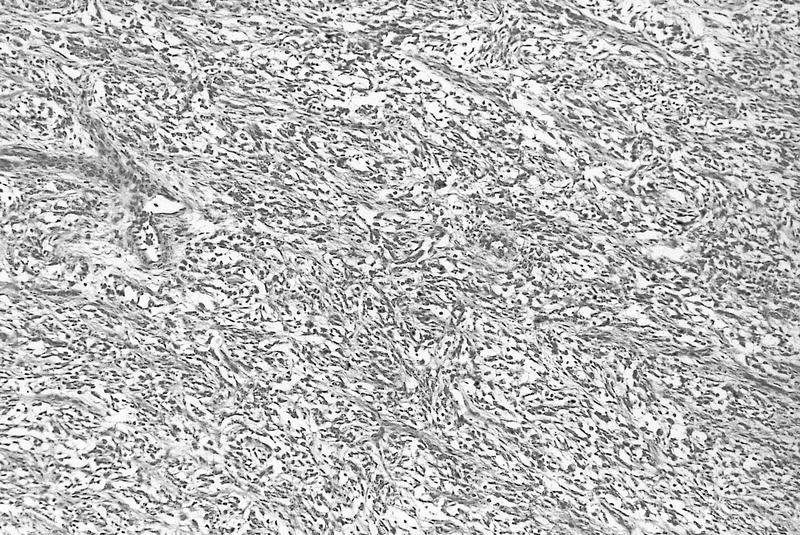
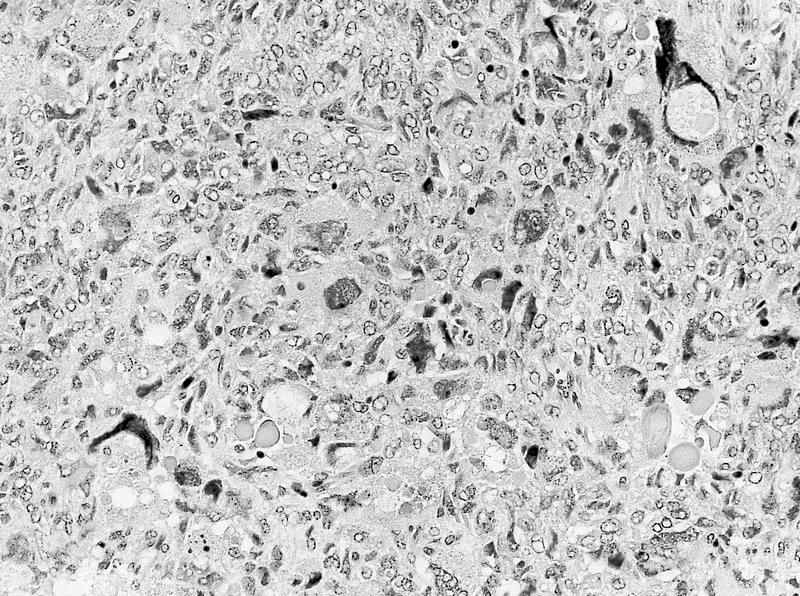
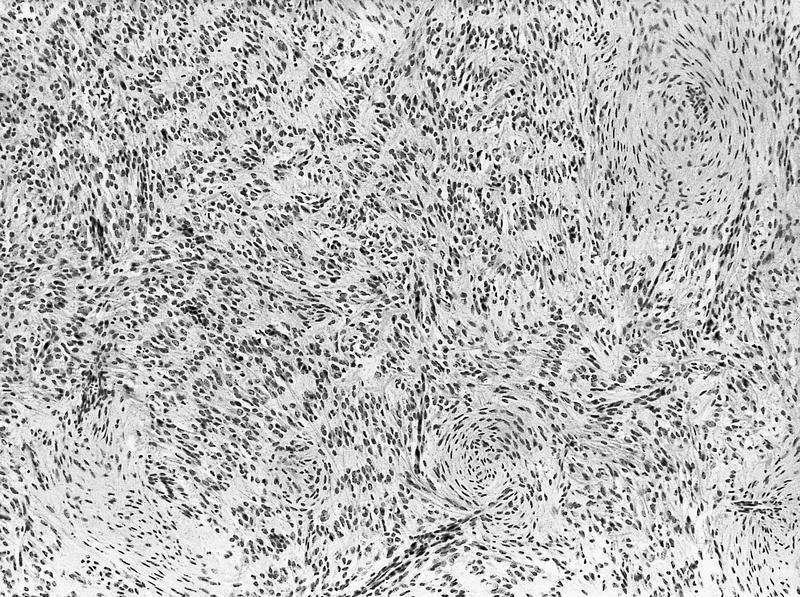
- The 8 variant patterns are myxoid (50%), sclerosing (35%), cellular (26%), epithelioid (trabecular or acinar type) (13%), palisading verocay body (11%), spindle cell (7%), storiform (4%) and anaplastic (2.6%) (Am J Surg Pathol 2000;24:4)
- Anaplasia is defined as nuclear hyperchromasia, atypical mitoses and giant nuclei (Am J Surg Pathol 2000;24:4)
- Cells may take on a spindle appearance, particularly near the vascular septae, these cells are termed "septal cells" (Zhou: Uropathology, 1st Edition, 2012)
- Although the border appears sharp at low power, high power reveals subtle infiltration of the cells into the normal parenchyma at the periphery
- Nuclei have smooth chromatin and appear washed out, similar to papillary thyroid carcinoma
- Nucleoli are not prominent; rare mitoses
- Only 20% have clear cells, and origin of clear cells varies per source: the clear nature of the cells is due to intracytoplasmic vacuoles or an extracellular mucopolysaccharide matrix that imparts a clear cell appearance (Bostwick: Urologic Surgical Pathology, 3rd Edition, 2014, Zhou: Uropathology, 1st Edition, 2012)
- Vascular invasion common
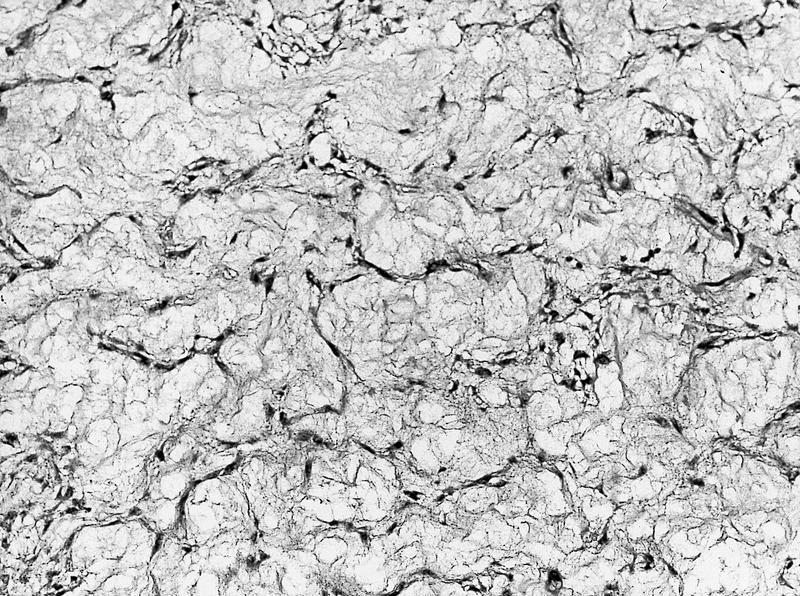
Microscopic (histologic) images
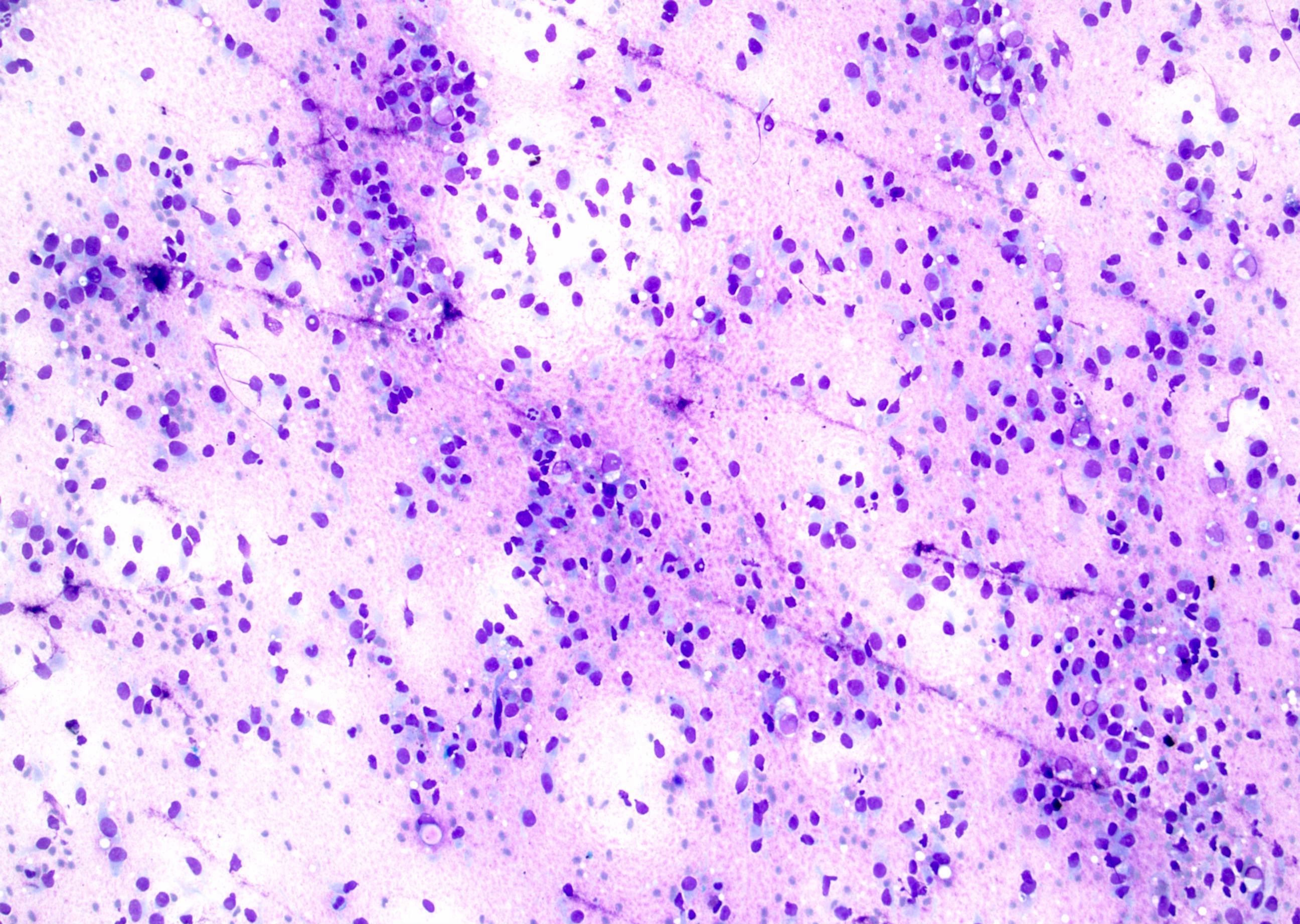
Cytology description
- Cells with moderate pale blue cytoplasm (Cytopathology 2008;19:80), cord cells with few stromal fragments
- Spindle cell variant has myxoid stromal fragments and septal cells
- Anaplastic variant has bizarre pleomorphic nuclei, coarse chromatin and atypical mitotic figures (Diagn Cytopathol 2005;33:83)
Positive stains
- Vimentin is strongly positive (45 / 45 cases) (Am J Surg Pathol 2000;24:4)
- Cyclin D1 may be useful (14 / 14 cases of CCSK are diffusely and strongly positive) (Histopathology 2015;67:306)
- CD34 highlights septal capillaries (Bostwick: Urologic Surgical Pathology, 3rd Edition, 2014)
- MIB1 (Ki67) had mean staining index of 21% in 22 cases (range among cases: 8% - 32% of cells staining), and no obvious correlation with histologic pattern was noted (Am J Surg Pathol 2000;24:4)
- p53 shows variable staining depending on histologic subtype: 86% (25 / 29 cases) of nonanaplastic CCSKs showed minimal (less than 5% of nuclei) staining; in contrast, 66% (2 of 3 cases) of anaplastic CCSKs showed intense, diffuse (> 75% of nuclei) staining (Am J Surg Pathol 2000;24:4)
Negative stains
Molecular / cytogenetics description
- Despite clear cell sarcoma of the kidney (CCSK) being the second most common renal tumor in children, its mechanism has not yet been fully elucidated
- A 2012 study demonstrated 12% (6 / 50 cases) contain a t(10;17), resulting in YWHAE - NUTM2B/E(FAM22B) fusion, confirming an earlier report (Arch Pathol Lab Med 2007;131:446)
- The prognostic significance of this translocation is unknown (J Pathol 2012;227:72)
- The t(10;17) is the same translocation seen in high grade endometrial stromal sarcoma
- There is a correlation between BCOR gene aberration and CCSK tumorigenesis
- Internal tandem duplications in the BCOR gene (BCL6 corepressor) were identified in 100% (20 / 20) of CCSK vs 0 of 193 other pediatric renal tumors
- None of these 20 cases had the YWHAE – NUTM2 fusion (Nat Genet 2015;47:861)
- In another study, internal tandem duplications in the BCOR gene (BCL6 corepressor) were identified in 85% (23 / 27) of CCSK (Nat Commun 2015;6:8891)
- Internal tandem duplications in the BCOR gene (BCL6 corepressor) were identified in 100% (20 / 20) of CCSK vs 0 of 193 other pediatric renal tumors
- Downregulated vascular endothelial growth factor A (VEGFA) and its interacting genes may initiate clear cell sarcoma of the kidney (CCSK) development by interrupting two different pathways, kinase regulation and protein tyrosine kinase metabolism
- IIn a 2016 gene expression study of 14 CCSK and 3 fetal kidney samples, a total of 2681 differentially expressed genes were identified, of which 2138 genes were downregulated, including VEGFA, and 543 were overexpressed (Oncol Lett 2016;11:953)
Differential diagnosis
- Conventional clear cell carcinoma of kidney: extremely rare in children, tumor cells are cytokeratin+
- Malignant rhabdoid tumor of the kidney: vimentin staining in a dot like pattern; CCSK is negative (Sebire: Diagnostic Pediatric Surgical Pathology, 1st Edition, 2009)
- Mesoblastic nephroma: WT1+, smooth muscle actin (SMA)+
- Wilm tumor (WT):
- Pushing border, more aggressive invasion, nephrogenic rests rule out CCSK; Wilm tumor is WT1+, epithelioid areas are keratin+
- In a pure stromal type WT treated with preoperative chemotherapy, the stroma may show a striking clear cell sarcoma-like appearance, and extensive sampling may be required to find foci with other WT components (Popov: Wilms Tumor, 2016)