Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Song S. Dysgerminoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumordysgerminoma.html. Accessed May 9th, 2024.
Definition / general
- Malignant primitive germ cell tumor with no specific type of differentiation
Essential features
- Most common malignant ovarian germ cell tumor; female counterpart to testicular seminoma
- Most common in children and young women
- Excellent prognosis with chemotherapy
- Composed of sheets or nests of uniform cells with clear or eosinophilic cytoplasm and distinct cell membranes; nuclei are rounded, often with angulated edges; tumor often separated by fibrous septae containing cytotoxic T cells and epithelioid histiocytes that can extend into tumor
- Positive for SALL4, OCT3/4, D2-40, CD117, PLAP
Epidemiology
- Constitutes 1 - 2% of all malignant ovarian tumors (Am J Surg Pathol 2021;45:1009)
- Most common malignant germ cell tumor of ovary (50%)
- Most common in children and young women
Sites
- Ovary
- Rarely, extraovarian sites, including abdomen, fallopian tube and uterus (J Pediatr Adolesc Gynecol 2021 May 11 [Epub ahead of print], Curr Probl Cancer 2021;45:100667, Indian J Pathol Microbiol 2018;61:590)
Pathophysiology
- Unknown
Etiology
- Arises from primordial germ cells of the ovary
Clinical features
- Most common in children and young women
- May present in pure form or as a component of a malignant mixed germ cell tumor
- Present with abdominal pain or distention
- Bilateral ovarian involvement in 10 - 15% of patients; involvement of contralateral ovary may be microscopic (Cancer Treat Rev 2008;34:427)
- Extraovarian spread in 33% of cases
- One of the most common neoplasms in pregnancy (Cancer Treat Rev 2008;34:427)
- Rare association with gonadal dysgenesis and chromosome Y abnormalities; may arise from gonadoblastoma
- Rare estrogenic manifestations
Diagnosis
- Diagnosis informed by patient's age, radiology and laboratory values (e.g. elevated lactate dehydrogenase [LDH] levels) but ultimately made based on histologic examination of surgical specimen
Laboratory
- Serum LDH often elevated (95%)
- 3 - 5% show low level hCG production related to the presence of multinucleated syncytiotrophoblastic giant cells that are not associated with cytotrophoblasts (Cancer Treat Rev 2008;34:427)
- Serum placental alkaline phosphatase (PLAP) may be elevated (Cancer Treat Rev 2008;34:427)
- Hypercalcemia may develop as a paraneoplastic syndrome, due to tumor production of 1,25-dihydroxyvitamin D3 (active form of vitamin D) (Cureus 2019;11:e6097)
Radiology description
- On ultrasound, tends to appear as a highly vascularized, large, solid, lobulated adnexal mass with irregular internal echogenicity (Ultrasound Obstet Gynecol 2011;37:596)
- Enhancing septa and areas of cystic change that may represent necrosis or hemorrhage may be seen; calcifications may manifest as a speckled pattern (Radiographics 2014;34:777)
Prognostic factors
- Most tumors are stage I at diagnosis
- Recurrence rate is low
- KIT mutations associated with advanced stage at presentation (Cancer 2011;117:2096)
- With treatment, excellent prognosis and overall survival > 90%
- Dysgerminoma patients have the most favorable outcomes compared with those with other malignant germ cell tumors; young age, low grade and surgery are significant predictors for improved survival (Oncol Res Treat 2021;44:145)
Case reports
- 16 year old girl with Swyer syndrome underwent prophylactic bilateral gonadectomy and salpingectomies and was found to have dysgerminoma solely within the fallopian tube (J Pediatr Adolesc Gynecol 2021 May 11 [Epub ahead of print])
- 19 year old woman with 29 cm dysgerminoma and pseudo-Meigs syndrome (Medicine (Baltimore) 2021;100:e26319)
- 22 year old woman with uncommon vaginal metastasis by dysgerminoma (Medicina (Kaunas) 2021;57:534)
- 26 year old pregnant woman with extraovarian (abdominal) dysgerminoma (Curr Probl Cancer 2021;45:100667)
- 27 year old woman with Swyer syndrome and stage IIA dysgerminoma in streak gonad (Gynecol Endocrinol 2018;34:464)
Treatment
- Radiosensitive but responds very well to cisplatin based chemotherapy, with overall survival > 90% (Cancer Treat Rev 2008;34:427)
- Fertility sparing surgery in patients with pure ovarian dysgerminoma with additional staging surgery, including retroperitoneal lymph node dissection to determine stage IA patients exempt from adjuvant chemotherapy (J Adolesc Young Adult Oncol 2021;10:303)
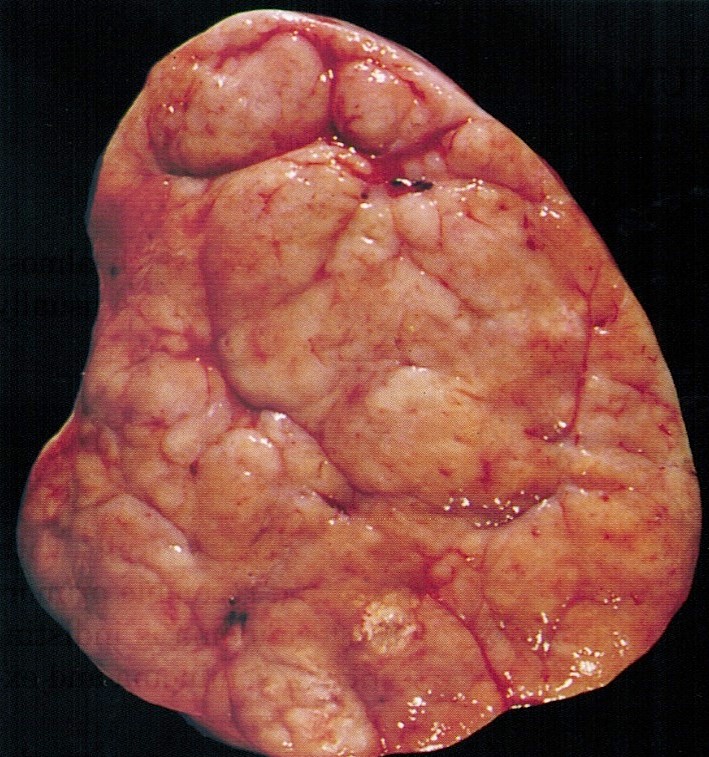
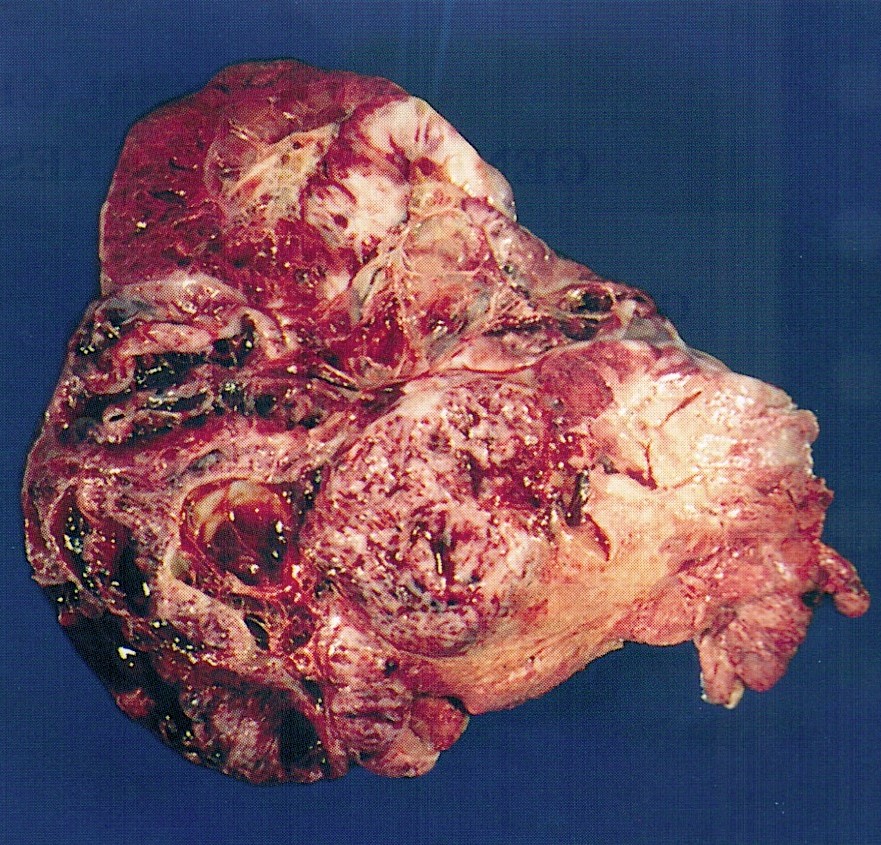
Gross description
- Usually > 10 cm
- Solid and lobulated with fleshy tan-white cut surface (Am J Surg Pathol 2021;45:1009)
- Hemorrhage and necrosis with cystic degeneration may be present
- Presence of calcifications may suggest an associated component of gonadoblastoma but not specific
Gross images
Frozen section description
- May favor diagnosis of high grade malignant germ cell tumor or malignant epithelioid neoplasm on frozen section; however, final diagnosis should be deferred to permanent sections
- Clear cytoplasm or distinct cell membranes may not be appreciated on frozen section due to artifact
- May mimic large cell lymphoma, both of which share similar gross appearance, large neoplastic nuclei and infiltrating background lymphocytes (Int J Gynecol Pathol 2020;39:79, Int J Surg Pathol 2019;27:387)
- Features favoring dysgerminoma include presence of fibrous septae and squared off nuclei
- Thickening of the fallopian tube is more suggestive of lymphoma (Int J Gynecol Pathol 2008;27:353)
- May mimic small cell carcinoma, hypercalcemic type, both of which typically occur in young women and show overlapping features, including paraneoplastic hypercalcemia (Semin Diagn Pathol 2019;36:246)
- Features favoring dysgerminoma include elevated LDH levels, moderately abundant cytoplasm
- In small cell carcinoma, hypercalcemic type, tumor cells usually have scant cytoplasm unless admixed component of large cell variant present
Frozen section images
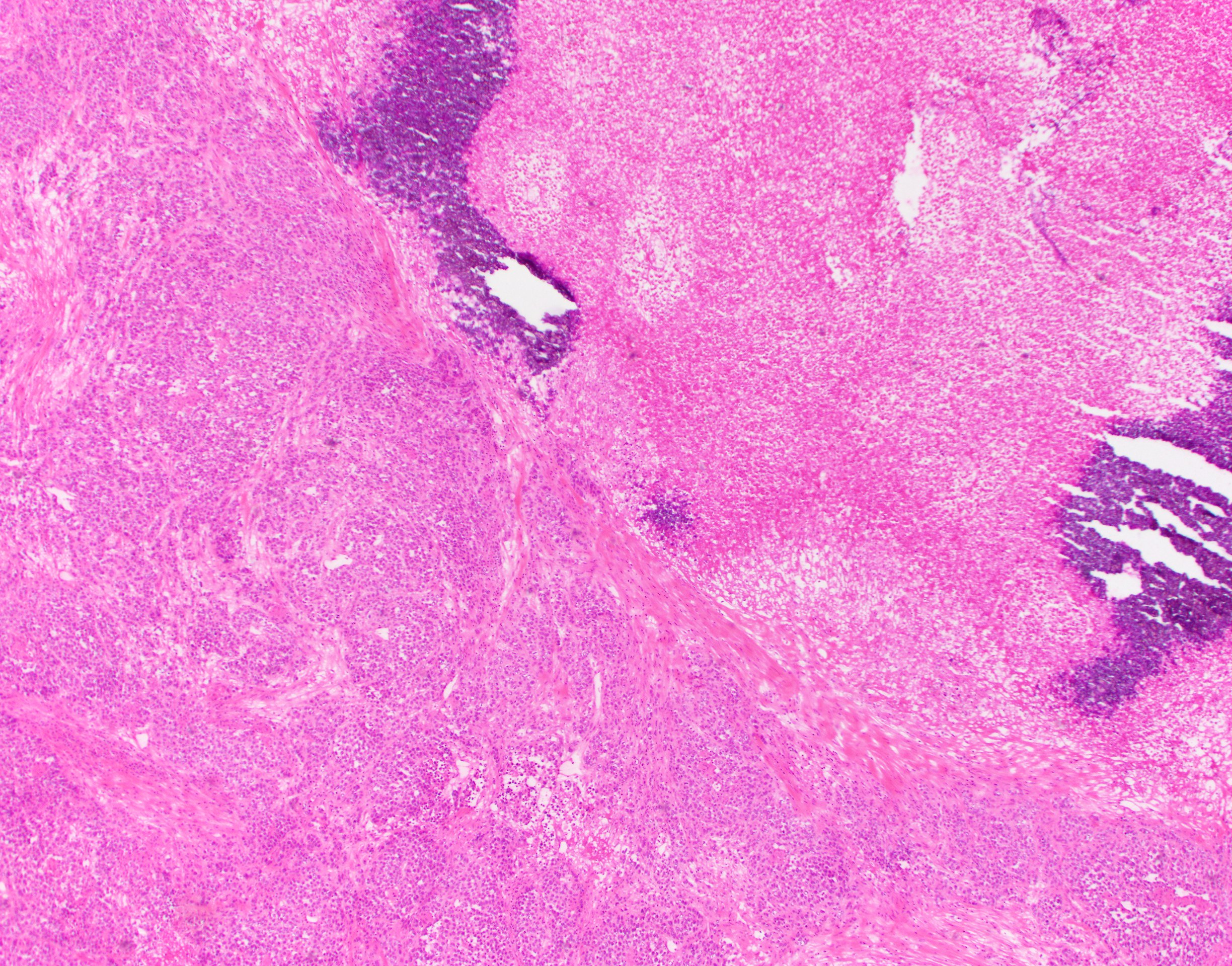
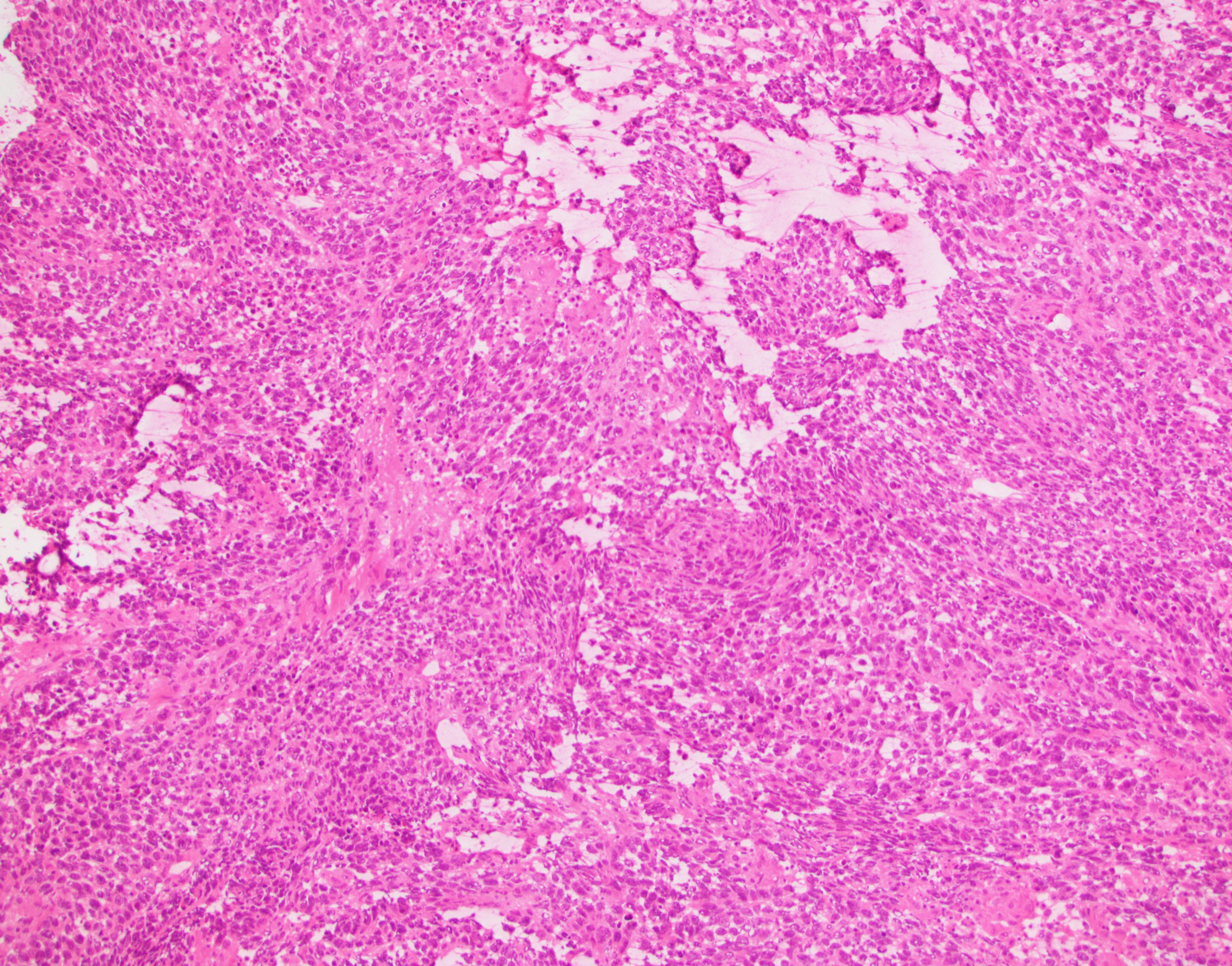
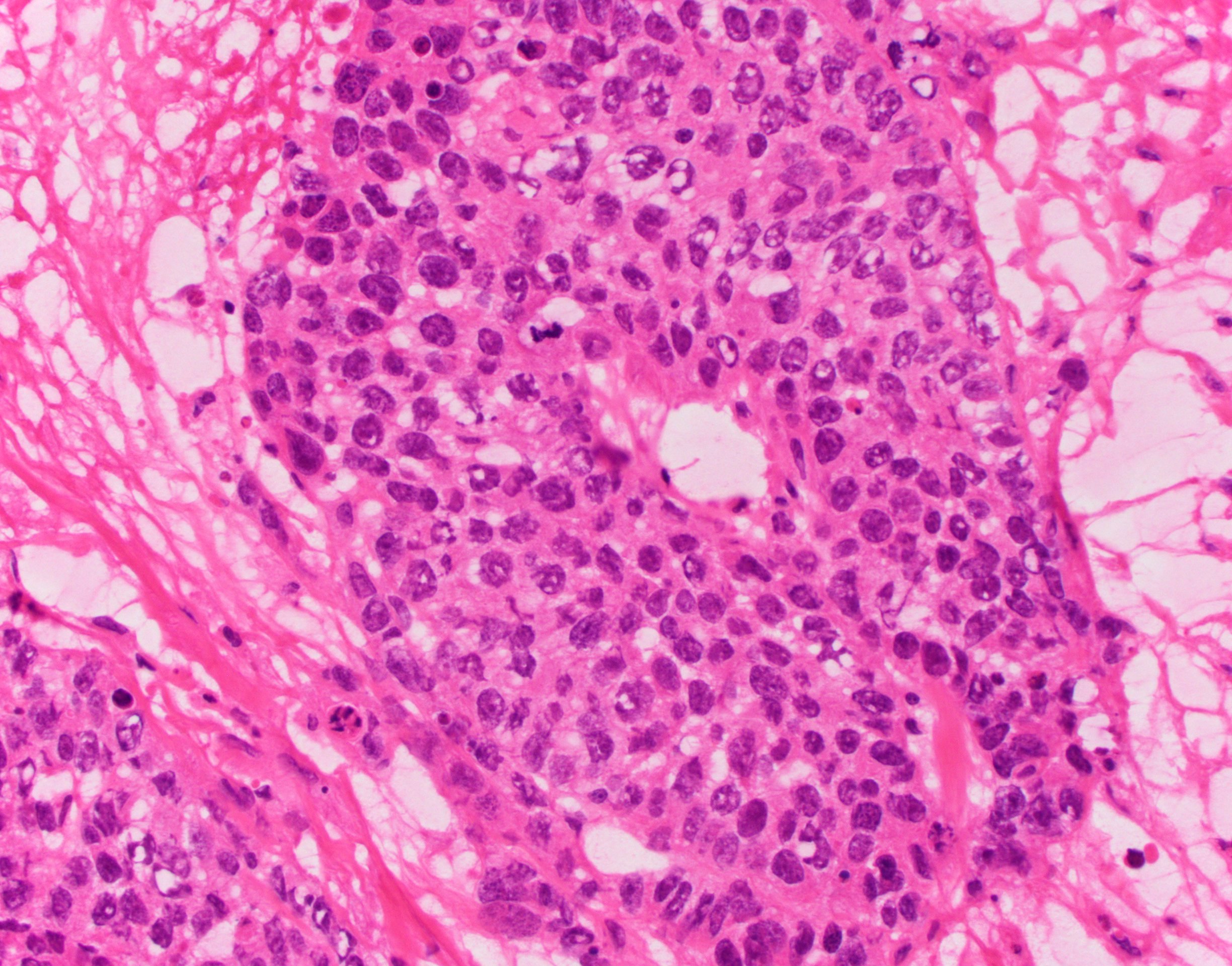
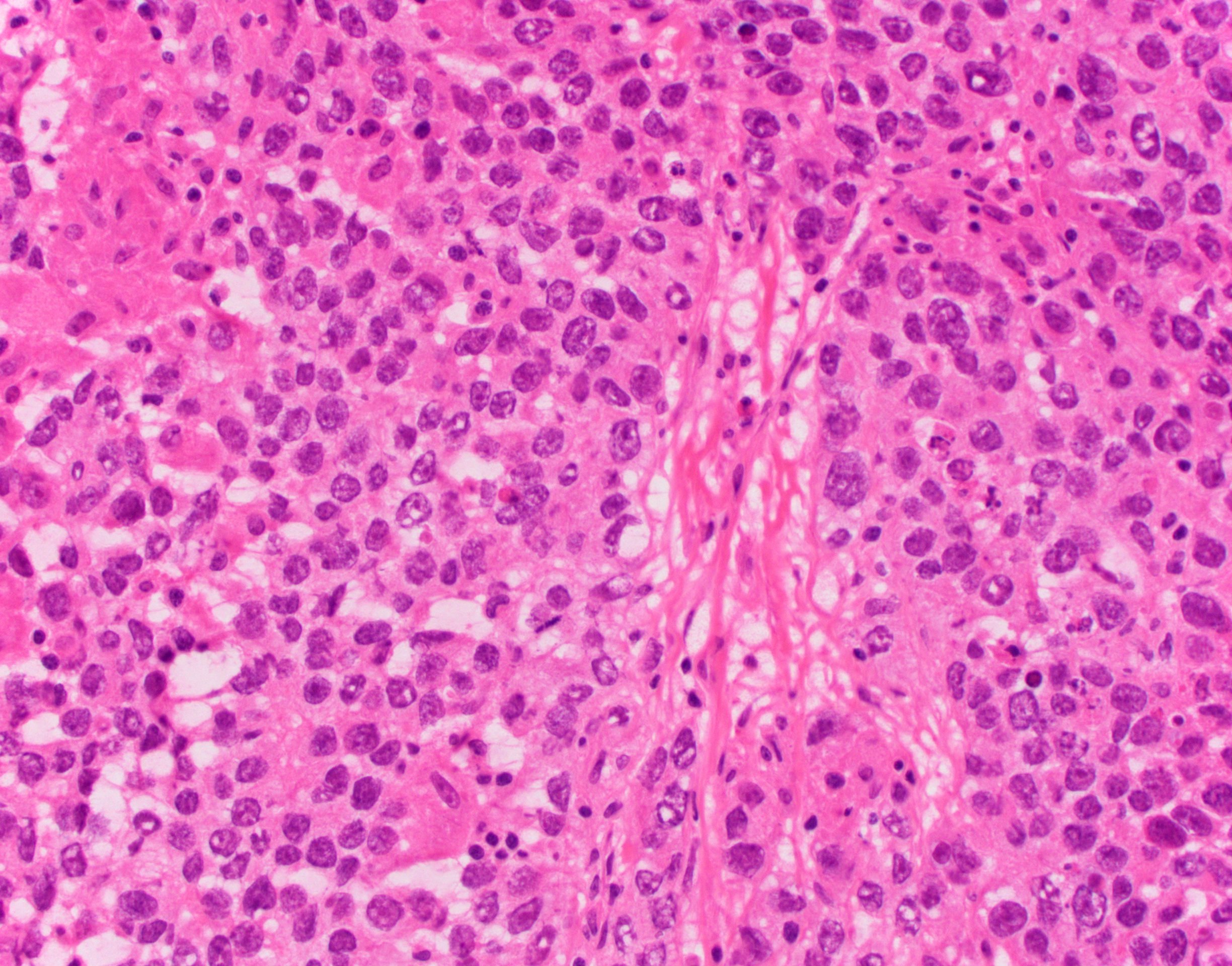
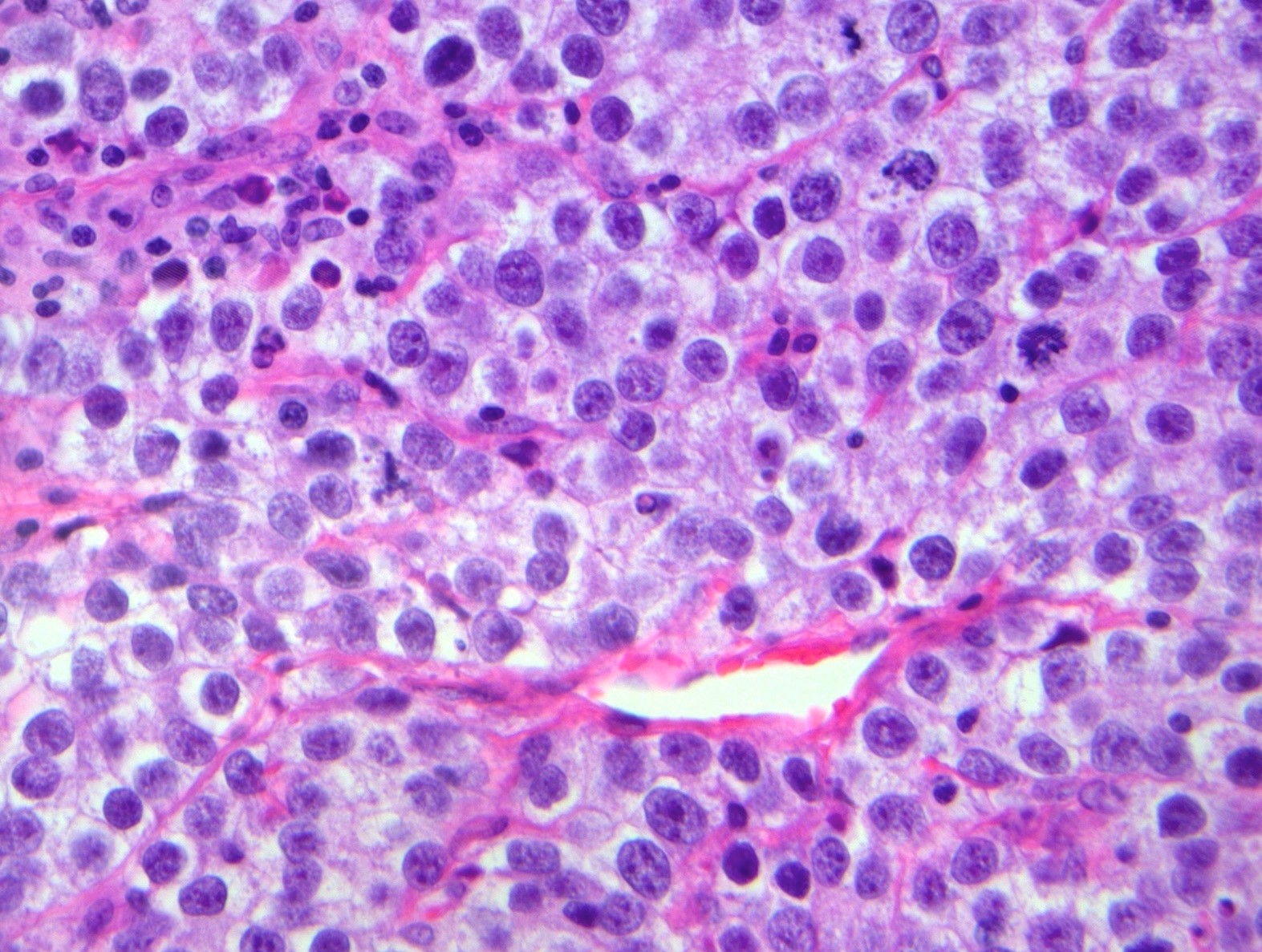
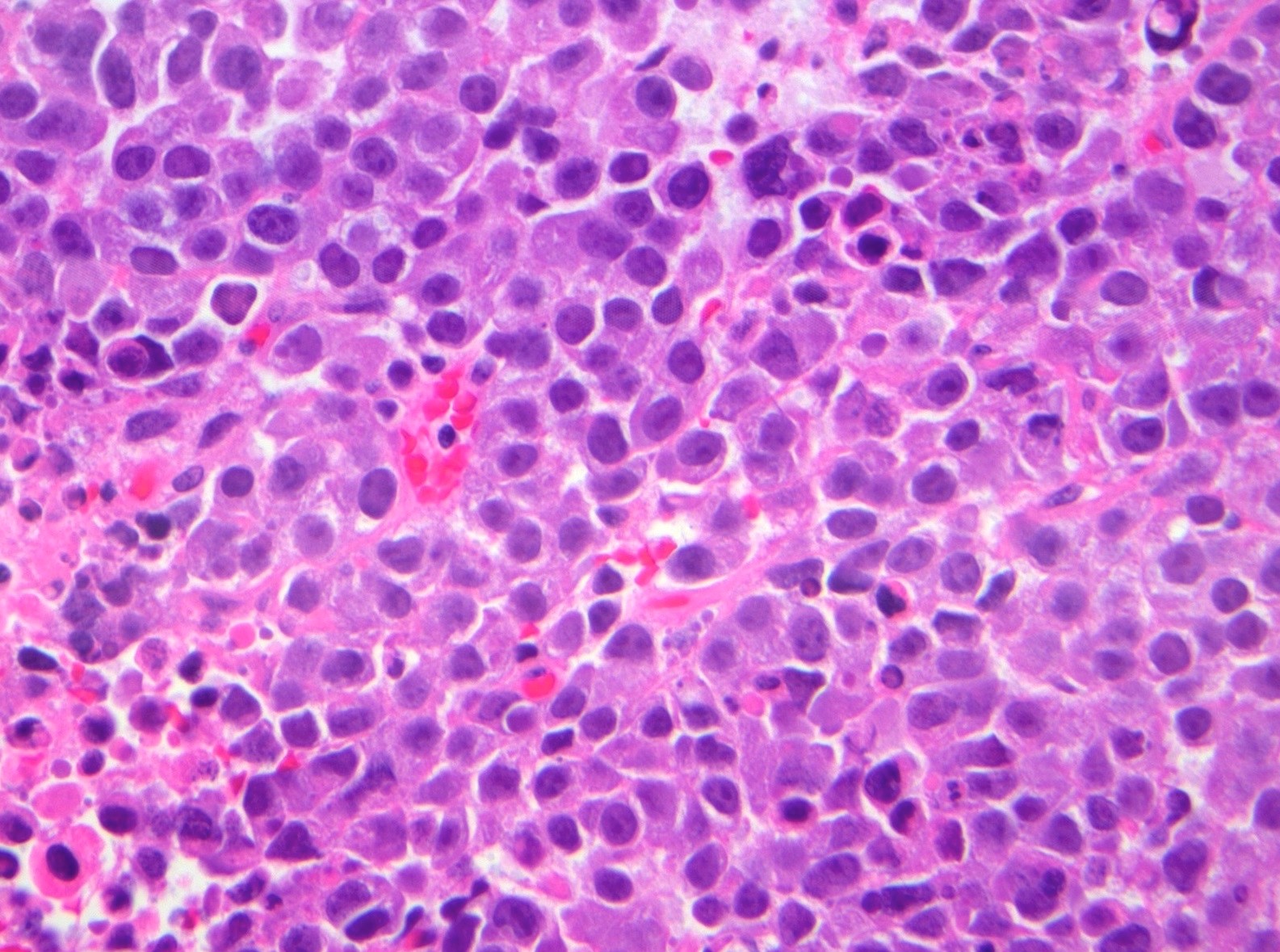
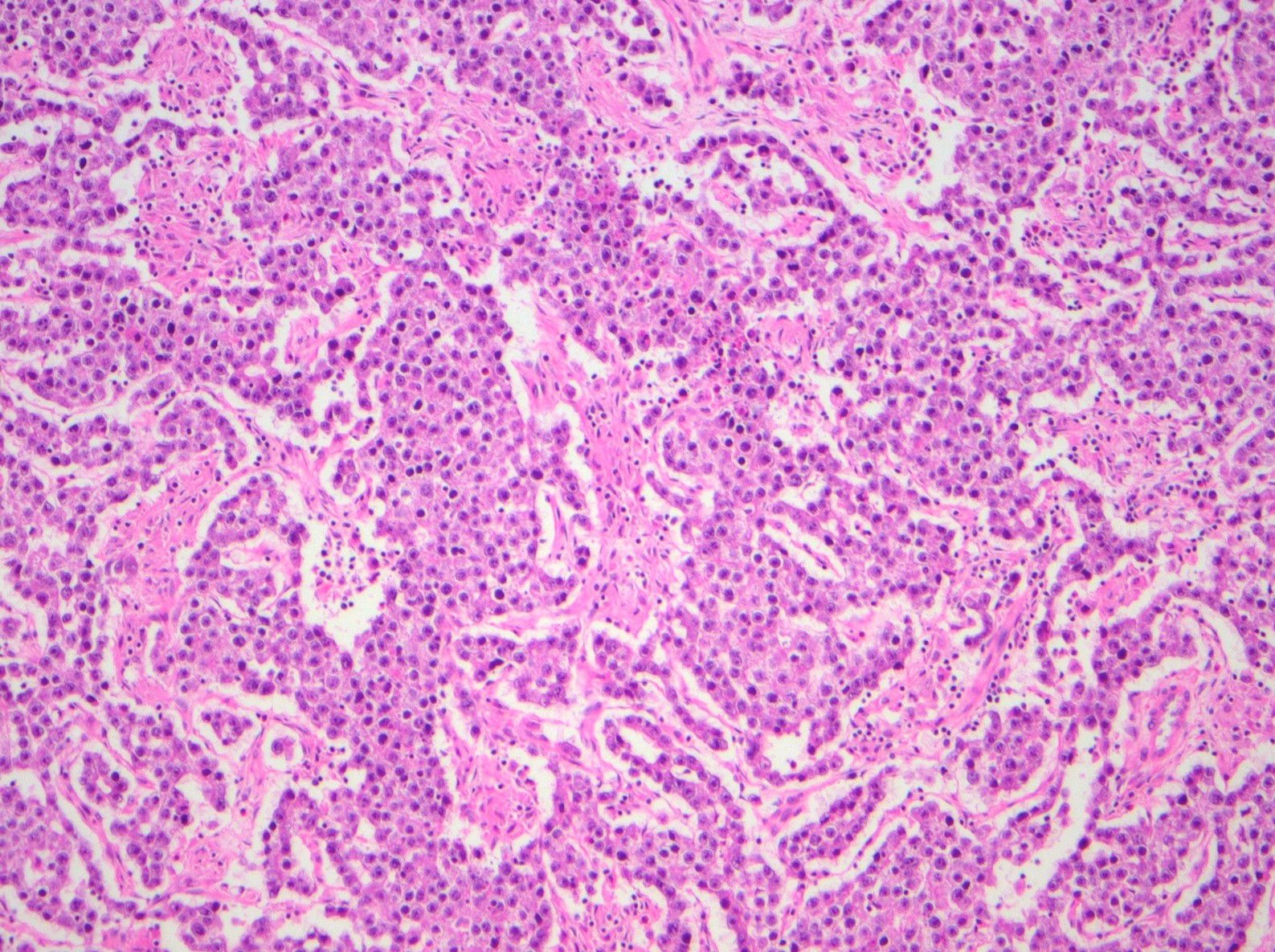
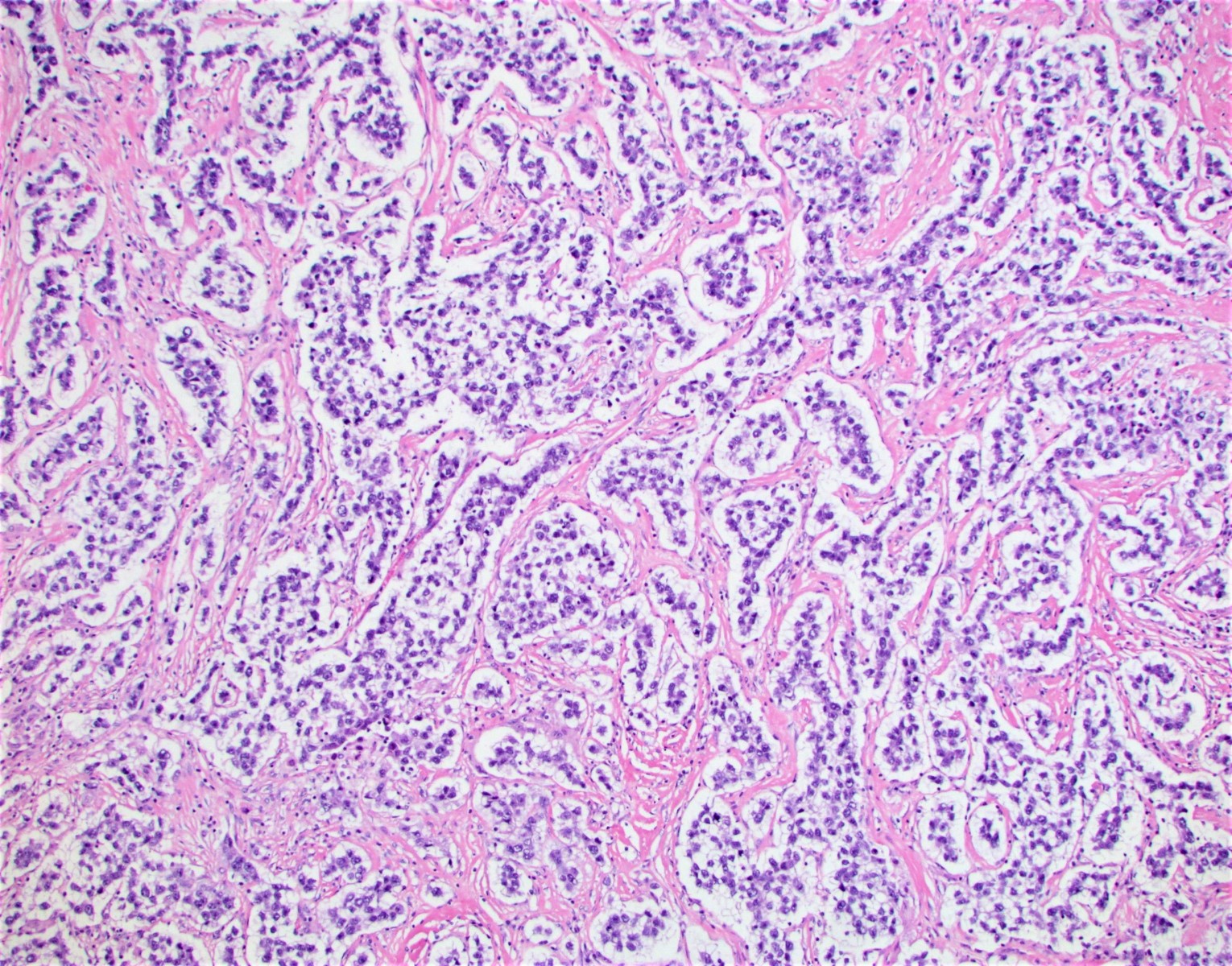
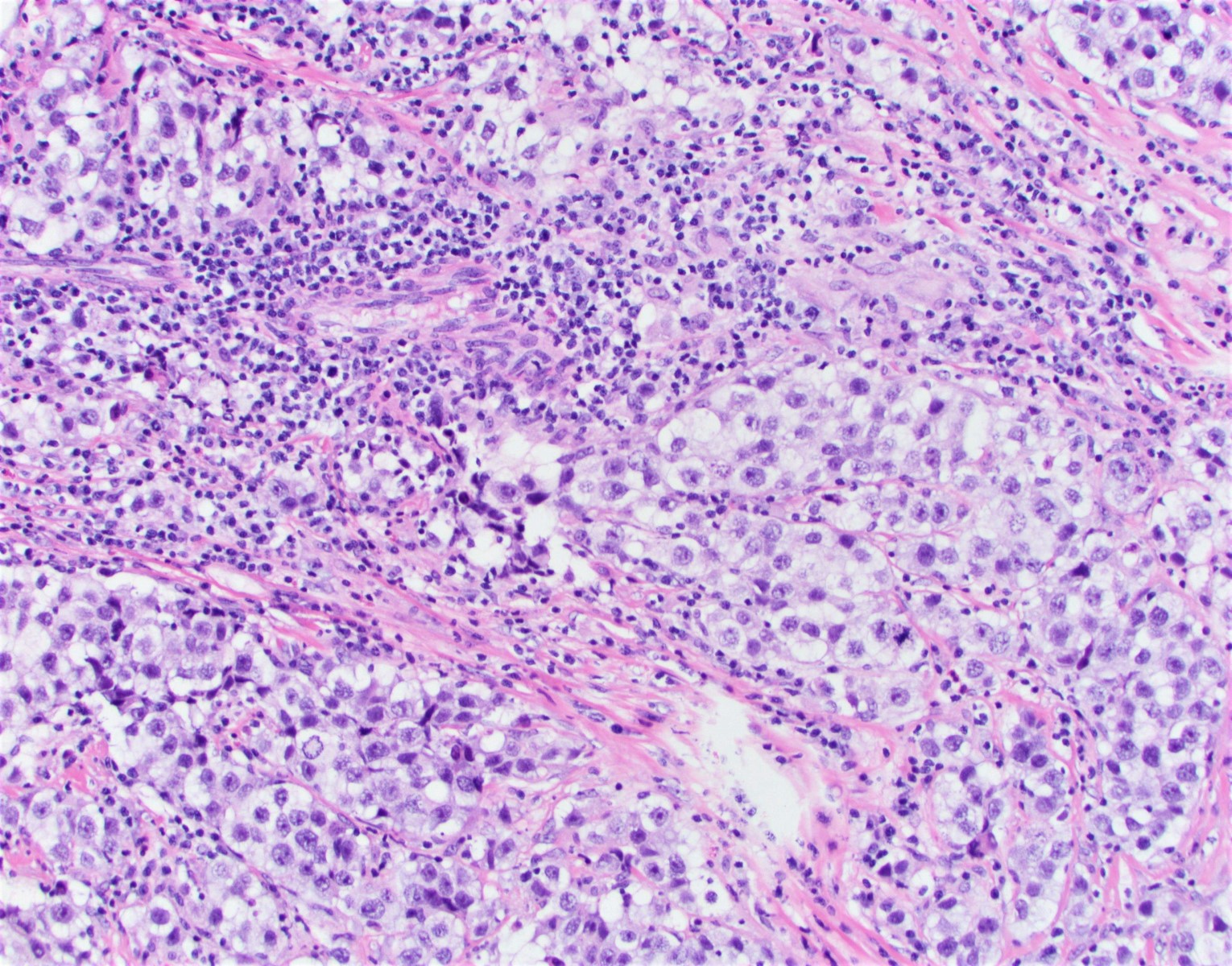
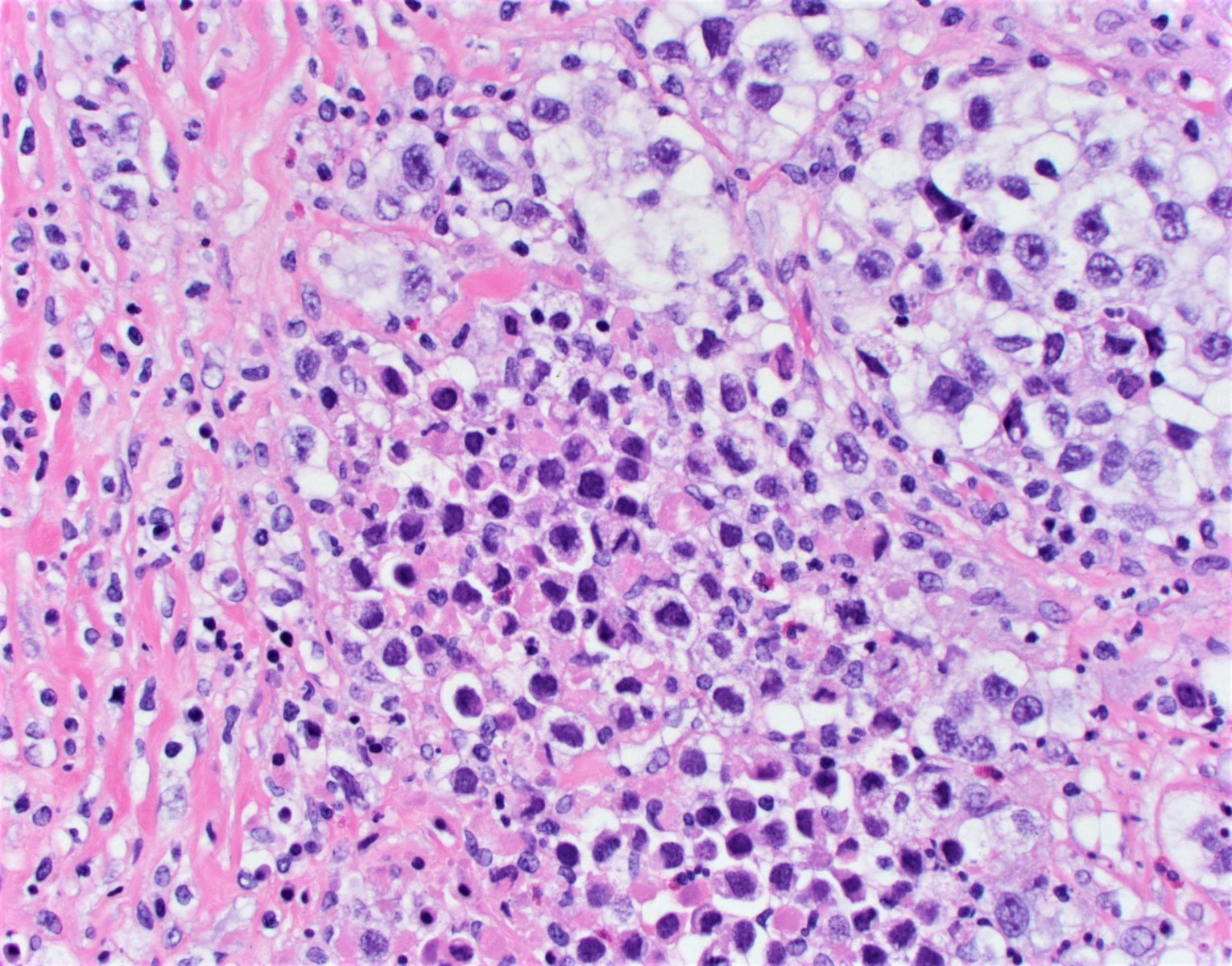
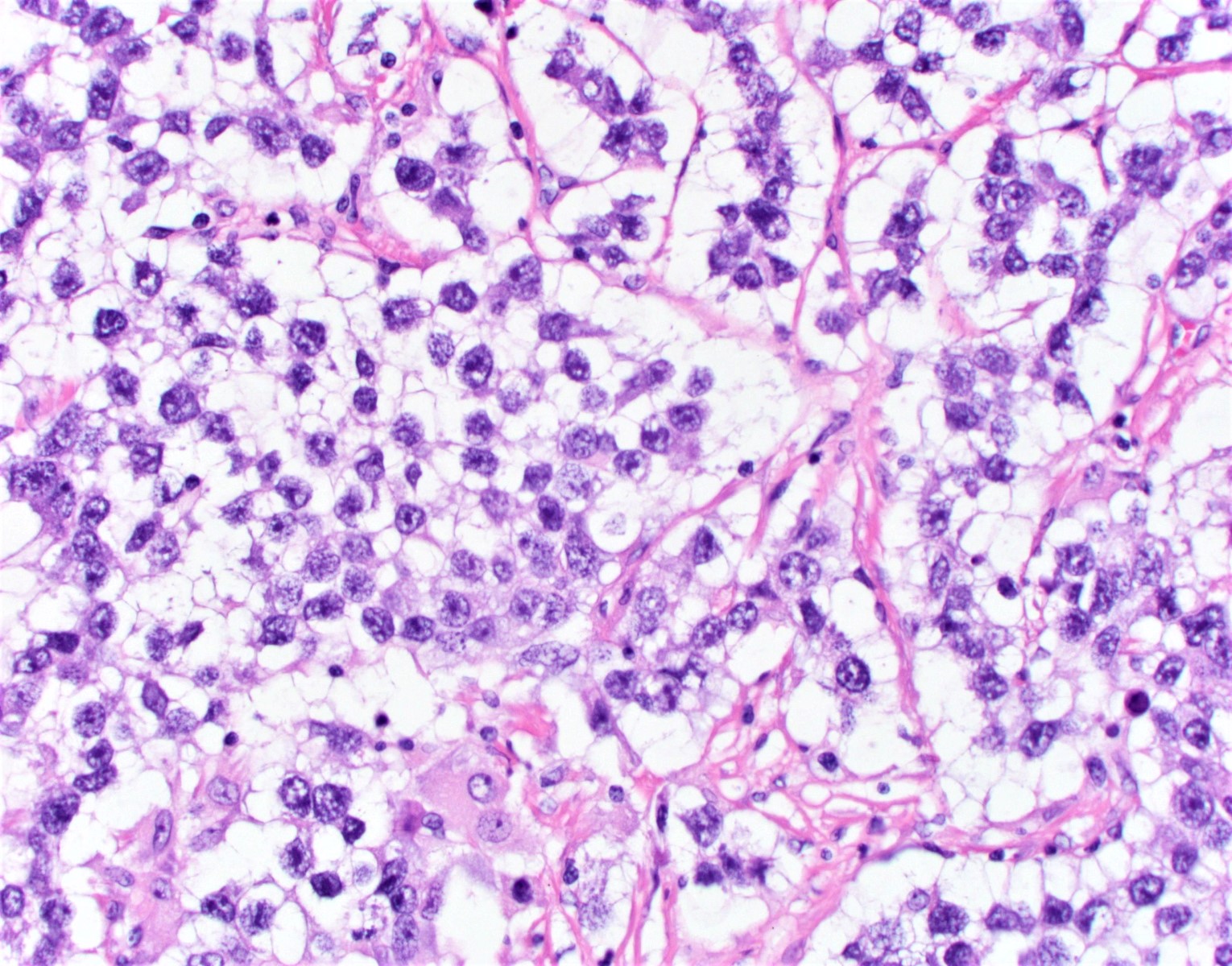
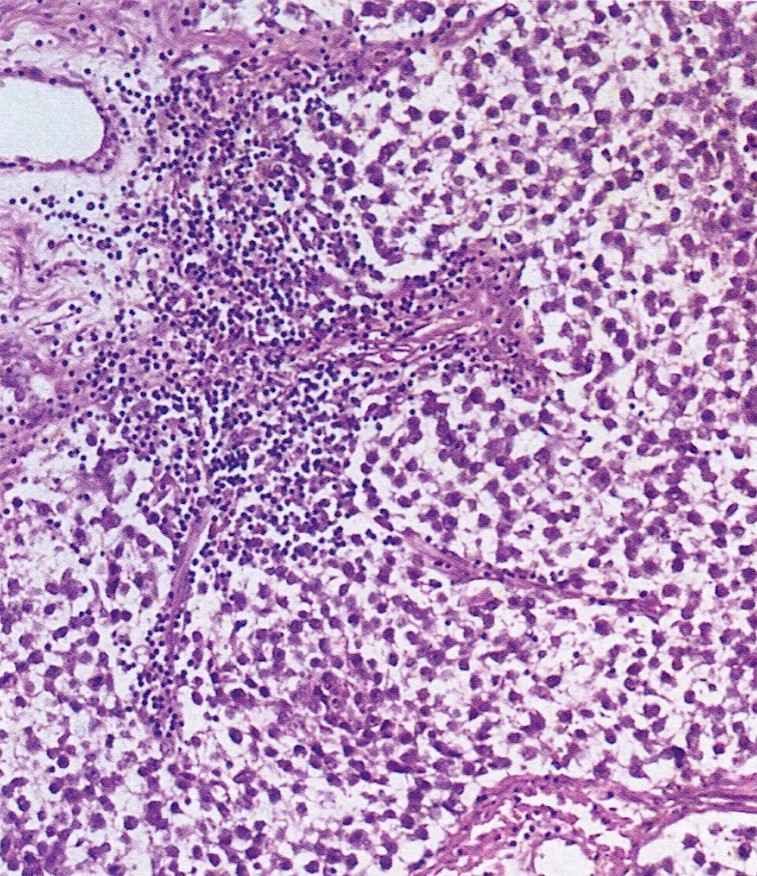
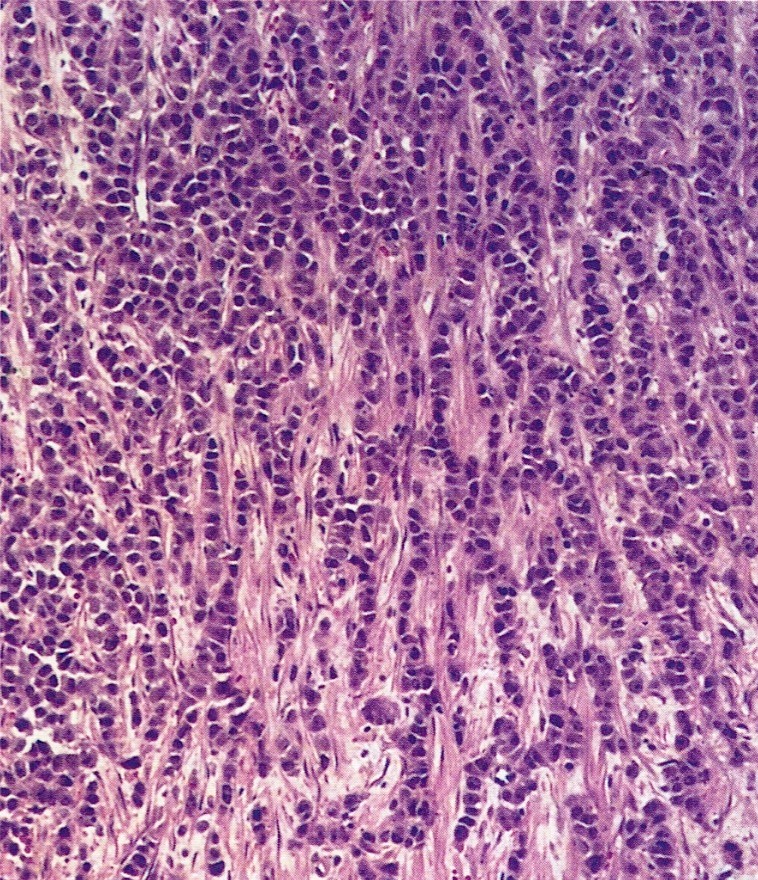
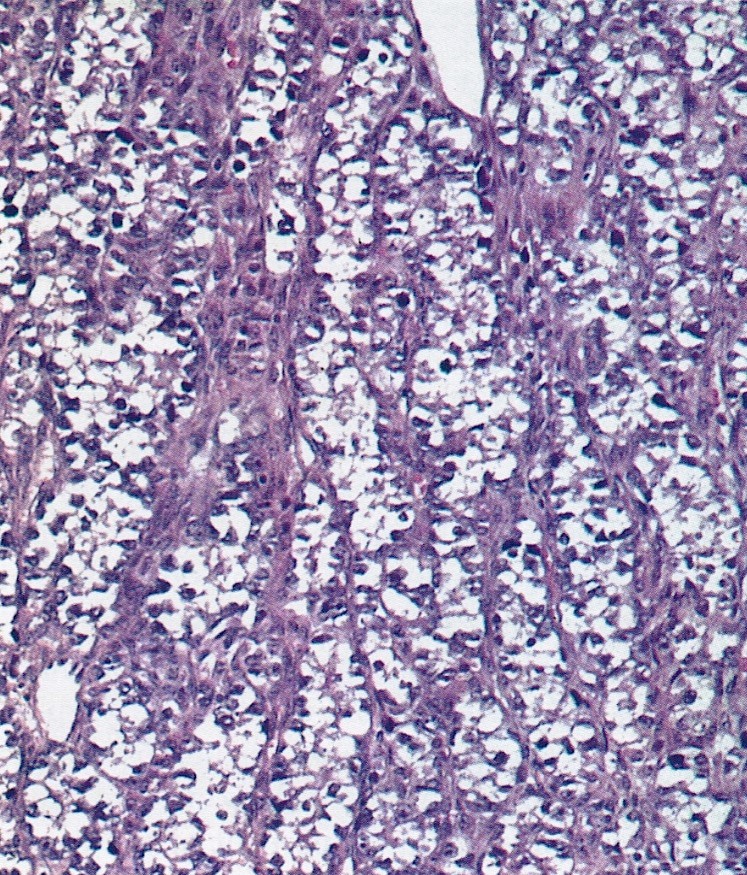
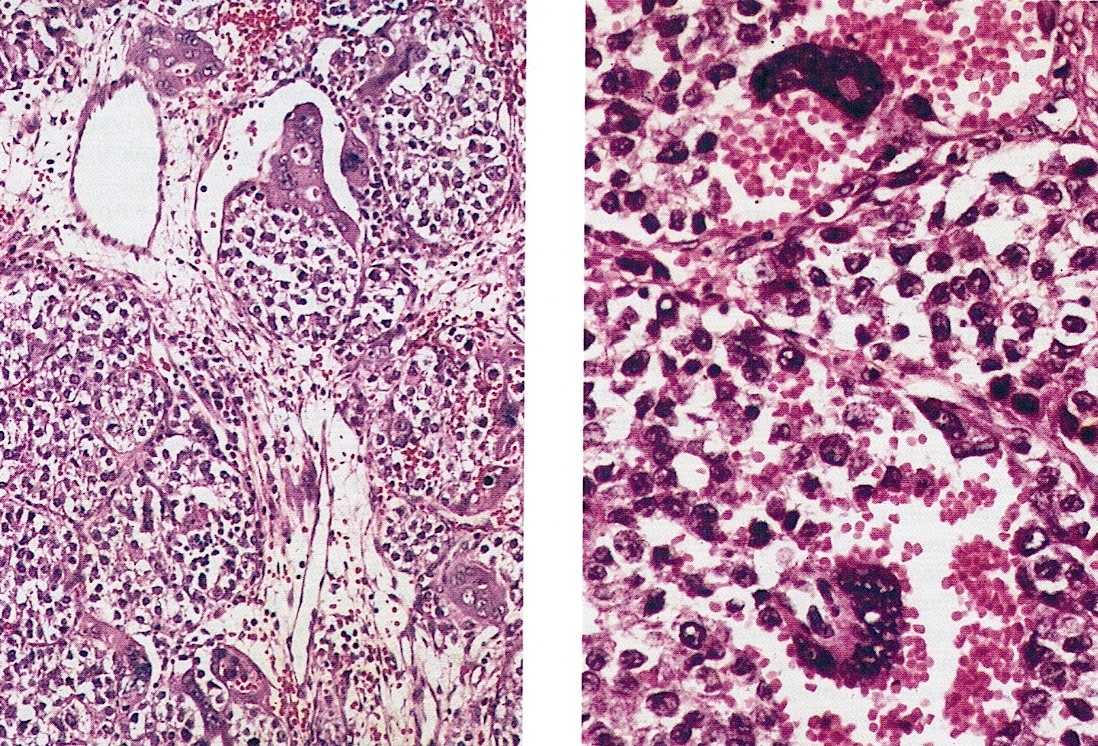
Microscopic (histologic) description
- Histomorphology identical to that of testicular seminoma
- In a well preserved specimen, characteristic appearance of nests of large, uniform polygonal cells with clear or eosinophilic cytoplasm and distinct cell membranes (alveolar pattern)
- May also show sheets, cords, macronodules, insular growth, microcysts, tubules, pseudoglandular spaces or trabeculae (Arch Pathol Lab Med 2014;138:351, Am J Surg Pathol 2021;45:1009)
- Rarely may show pseudopapillary or macrofollicular growth pattern (Iran J Pathol 2018;13:94)
- Tumor separated by fibrous septae containing cytotoxic T cells and epithelioid histiocytes, often with spillover into tumor; plasma cells, eosinophils, Langhans type giant cells, syncytiotrophoblasts, noncaseating granulomas or lymphoid follicles with germinal centers may be present (Am J Surg Pathol 2021;45:1009)
- Stroma usually loose and delicate but in some cases may be hyalinized, myxoid or luteinized
- Numerous mitotic figures
- Rare cases show syncytiotrophoblastic cells, singly or in clusters, without cytotrophoblastic cells; sample tumor thoroughly to exclude choriocarcinoma
- Extensive hemorrhage and necrosis may be present with dystrophic calcification; if large areas of dystrophic calcification seen in the absence of necrosis, may be a gonadoblastoma
- As gonadoblastomas give rise to dysgerminomas, thorough sampling indicated to rule out its presence
Microscopic (histologic) images
Contributed by Sharon Song, M.D.
AFIP images
Cytology description
- Uniform population of medium to large sized cells (Diagn Cytopathol 2020;48:356)
- Centrally located, round to oval nuclei, often with angulated, squared off borders
- Vesicular, finely granular or coarse chromatin
- Prominent single or multiple nucleoli
- With poor fixation, cells may show loss of cohesion, nuclei can appear hyperchromatic and cytoplasm may appear scant and eosinophilic, mimicking cells of embryonal carcinoma
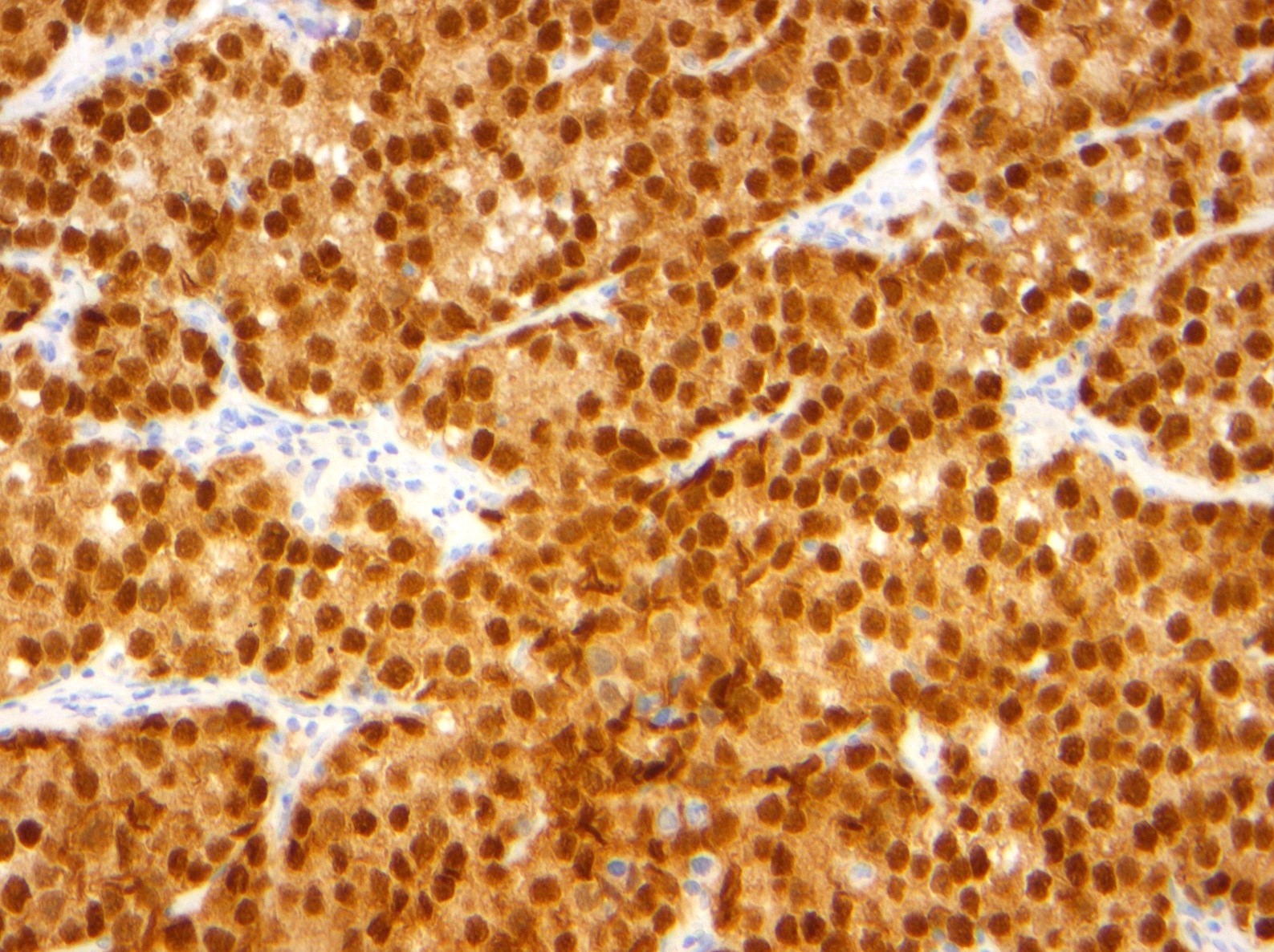
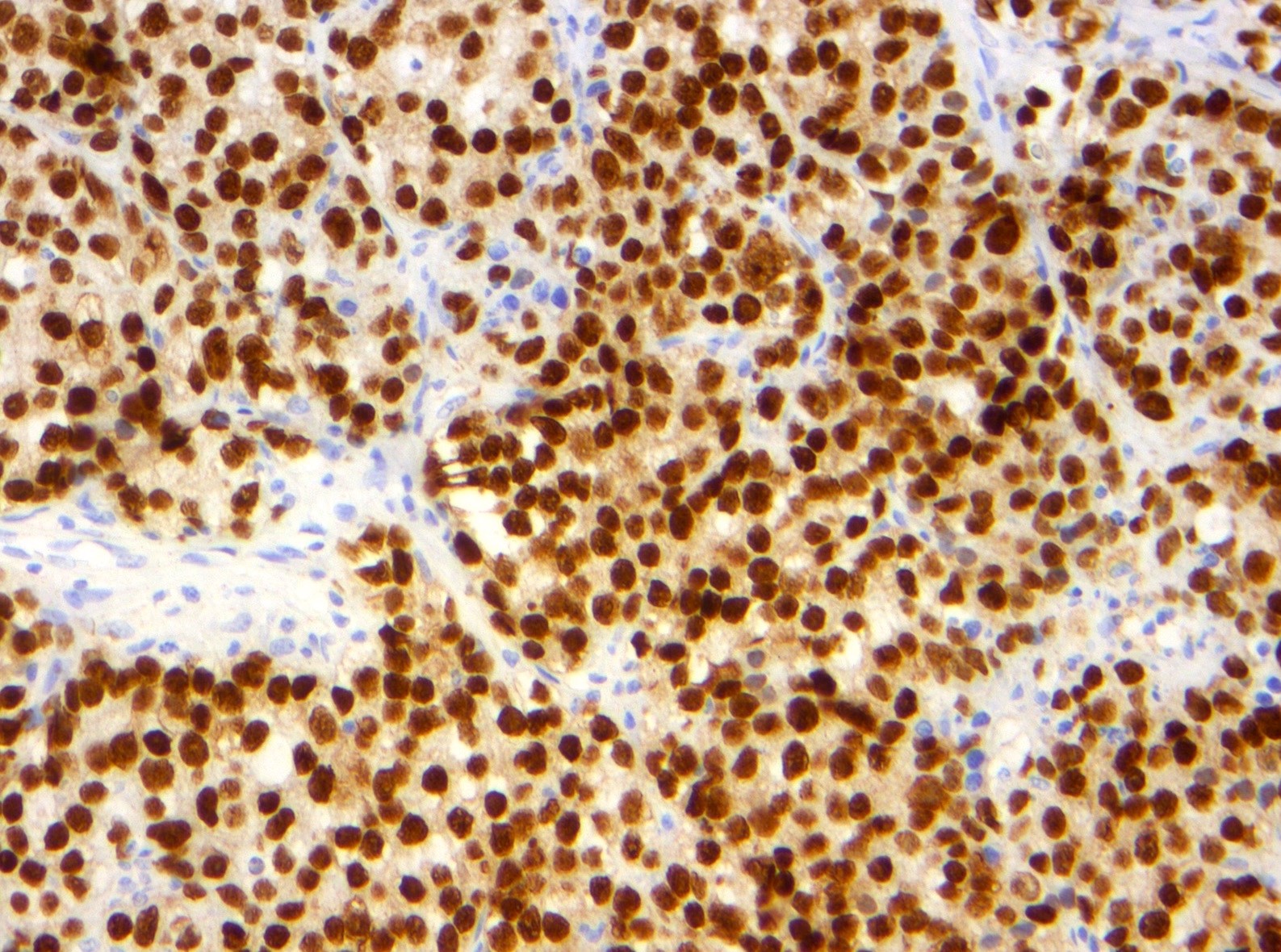
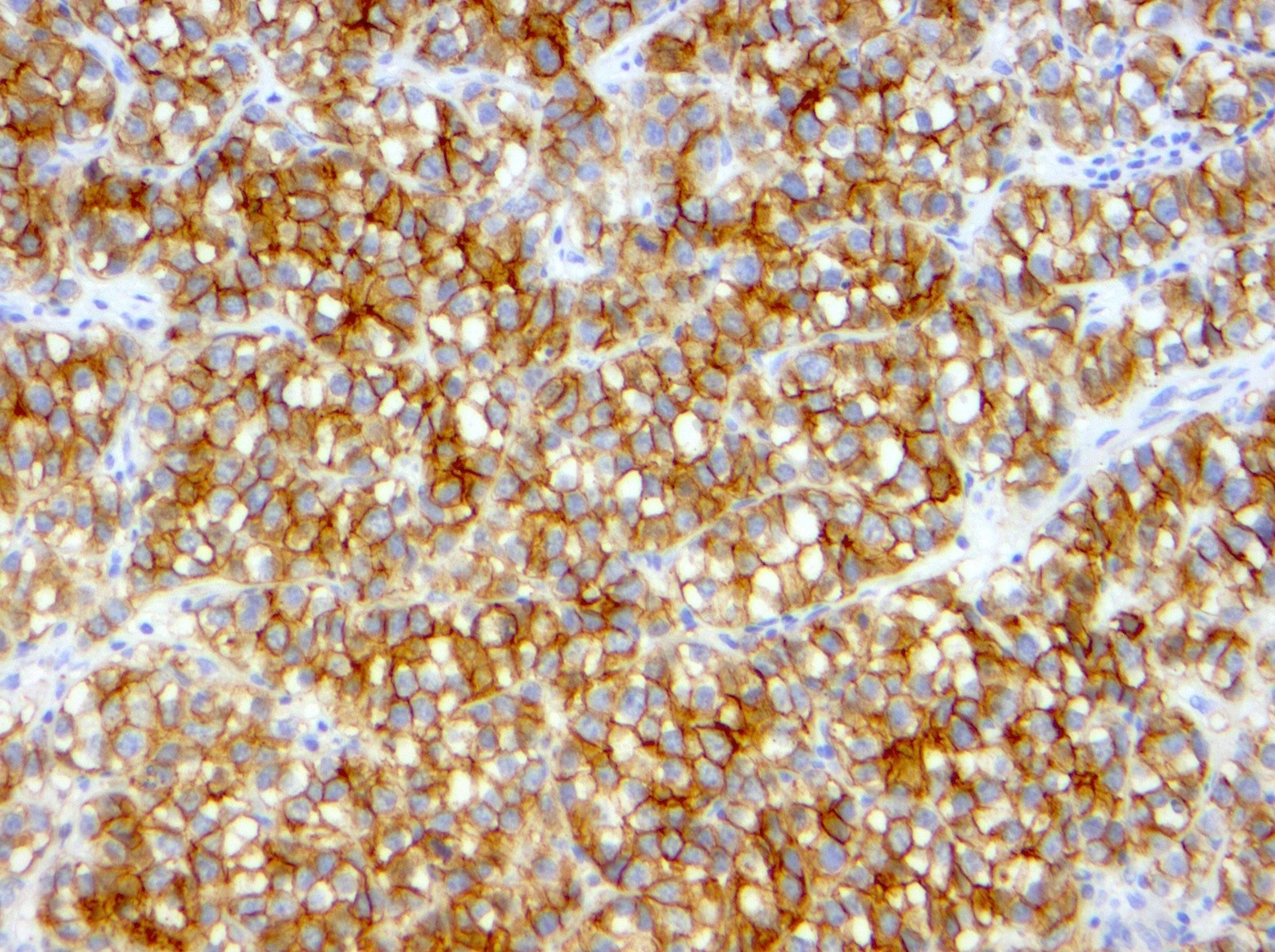
Positive stains
- OCT3/4 (nuclear), CD117 (KIT; membranous), D2-40 (membranous and cytoplasmic) (Histopathology 2013;62:71)
- NANOG (nuclear) and SALL4 (nuclear) stem cell markers
- PLAP (membranous and cytoplasmic)
- May focally express keratins with cytoplasmic dot or rim-like staining: CAM 5.2 (positive in up to 10% of tumor cells in < 50% of dysgerminomas); AE1 / AE3 and CK7 (positive in up to 10% of tumor cells in < 25% of dysgerminomas)
- hCG, inhibin, glypican 3 and CK7 can highlight syncytiotrophoblastic giant cells; can search for these cells in patients with moderate serum hCG elevation (Histopathology 2013;62:71)
Molecular / cytogenetics description
- Isochromosome 12p in 81% (Pathol Res Pract 2012;208:628, Mod Pathol 2006;19:611)
- KIT mutations in exon 17 codon 816 or KIT amplification detected in approximately 33% of cases and associated with advanced stage at presentation (Cancer 2011;117:2096)
- As this KIT mutation involves exon 17, not exon 11 as in gastrointestinal stromal tumors, these cases are not responsive to KIT receptor inhibitors
Sample pathology report
- Left ovary, left oophorectomy:
- Dysgerminoma (11 cm) (see synoptic report)
- No ovarian surface involvement identified
Differential diagnosis
- Important to rule out other types of mixed germ cell tumor
- Yolk sac tumor:
- Classically variable morphologic patterns (commonly reticular / microcystic)
- Lacks fibrous septae containing lymphocytes
- Glypican 3+, AFP+, OCT3/4-, CD117-, D2-40-
- Yolk sac tumor:
- Lymphoma:
- Lacks fibrous septae
- May be associated with thickened fallopian tube
- Positive lymphoid markers and IgH clonality
Board review style question #1
Board review style answer #1
B. Dysgerminoma is the most common malignant ovarian germ cell tumor.
Comment Here
Reference: Dysgerminoma
Comment Here
Reference: Dysgerminoma
Board review style question #2
- Which of the following immunostains are typically positive in dysgerminoma and can confirm the diagnosis?
- AFP, SALL4, OCT3/4, hCG
- D2-40, CD117, OCT3/4, SALL4
- OCT3/4, EMA, hCG, SALL4
- PLAP, AFP, hCG, AE1 / AE3
Board review style answer #2
B. D2-40, CD117, OCT3/4, SALL4. SALL4 is positive in germ cell tumors. OCT3/4 positivity narrows the differential of germ cell tumors to dysgerminomas and embryonal carcinomas. Dysgerminomas are positive for CD117 and D2-40.
Comment Here
Reference: Dysgerminoma
Comment Here
Reference: Dysgerminoma