Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) description | Cytology description | Cytology images | Peripheral smear description | Peripheral smear images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Liu H. AML M6. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/leukemiam6.html. Accessed August 14th, 2025.
Definition / general
- Acute erythroid leukemia (AEL) or pure erythroid leukemia (PEL)
- Neoplastic proliferation of erythroid precursors with markedly increased proerythroblasts and defect in erythroid differentiation and maturation
Essential features
- Rare aggressive acute myeloid leukemia (AML) (Am J Hematol 2017;92:292)
- Erythroid precursors ≥ 80% and proerythroblasts ≥ 30% of the bone marrow cells
- Myeloblasts are not increased in number but frequently show an aberrant immunophenotype
Terminology
- Acute myeloid leukemia, M6 type
- Acute erythroid leukemia
- Erythroleukemia
- Pure erythroid leukemia M6b
ICD coding
- ICD-10: C94.00 - acute erythroid leukemia, not having achieved remission
Epidemiology
- Extremely rare, < 1% of all AML (Am J Hematol 2017;92:292)
- Any age, can be congenital and incidence peaks in 70 - 80 year old patients (Int J Hematol 2017;106:711, Cancers (Basel) 2023;15:3941)
- Both de novo and secondary (more often, either postexposure to cytotoxic therapy or progression of a prior myeloid neoplasm; cases of acute erythroid leukemia arising after cytotoxic therapy should be designated as myeloid neoplasm postcytotoxic therapy)
Sites
- Bone marrow or peripheral blood (Am J Hematol 2017;92:292)
- Mass lesion (erythroblastic sarcoma) in tissue such as central nervous system, orbit, liver, ovary, etc. (Haematologica 2020;105:e194)
Pathophysiology
- Marked clonal expansion of proerythroblasts and differentiation block in erythroid lineage due to genetic mutations
Etiology
- Unknown
Clinical features
- Anemia (Am J Hematol 2017;92:292)
- Circulating erythroblasts
- Extramedullary mass (Haematologica 2020;105:e194)
Diagnosis
- Erythroblasts ≥ 80% in bone marrow or peripheral blood with proerythroblasts ≥ 30%
- Myeloblasts are not increased
- For extramedullary mass lesion, sheets of erythroid precursor cells with markedly increased proerythroblasts
- Note: in current ICC classification, PEL cases with any somatic TP53 mutations (variant allele frequency ≥ 10%) are diagnosed as AML with mutated TP53 (Virchows Arch 2023;482:27)
Prognostic factors
- Usually poor for adult patients with median overall survival of 3 - 6 months (Mod Pathol 2018;31:705, Mod Pathol 2011;24:375, Cancers (Basel) 2023;15:3941)
- Prognosis is controversial for children and adolescent groups due to rarity; one study showed poor prognosis and the largest case studies showed relatively better prognosis with median overall survival of 69 months (Blood Adv 2020;4:6000, Cancers (Basel) 2023;15:3941)
Case reports
- 4 month old boy with fatigue, irritability, regurgitation, high fever, hepatosplenomegaly, anemia, leukocytosis, thrombocytopenia and pure erythroid leukemia (PLoS One 2013;8:e63663)
- 2 year old girl presented with headache, vomiting and a de novo erythroid sarcoma in third ventricle (Haematologica 2020;105:e194)
- 3 year old boy suddenly presented with epileptic seizures and postcritic left hemiplegia and erythroblastic sarcoma (Acta Neuropathol Commun 2024;12:12)
- 44 year old woman with progressive fatigue, pancytopenia and pure erythroid leukemia (Clin Case Rep 2019;7:1829)
- 48 year old man with shortness of breath, weight loss and pure erythroid leukemia (Hematol Rep 2015;7:5674)
Treatment
- AML treatment protocol (Am J Hematol 2017;92:292)
- Radiation therapy can be considered for localized mass lesion in orbit or CNS (Haematologica 2020;105:e194)
- Bone marrow transplant
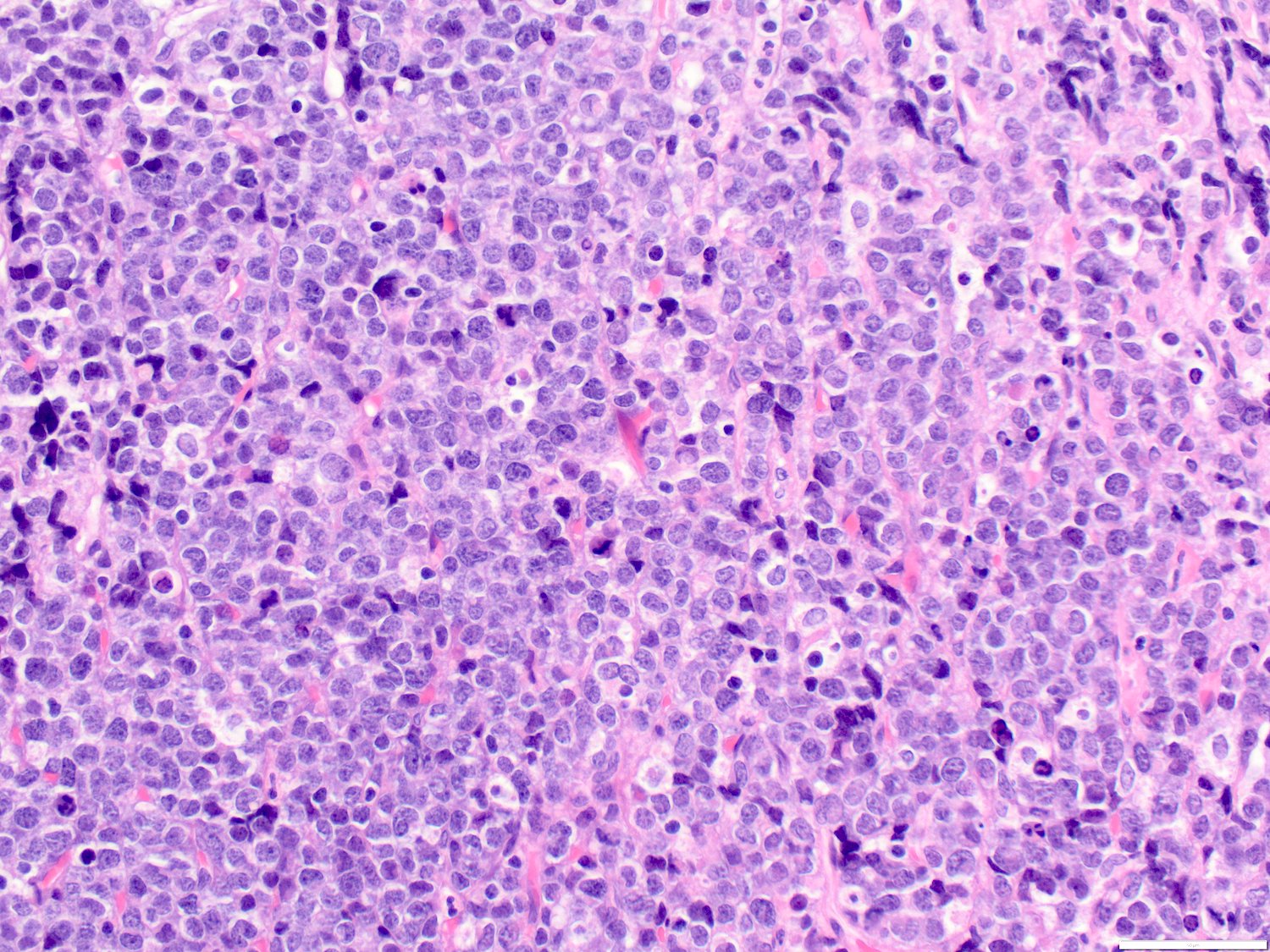
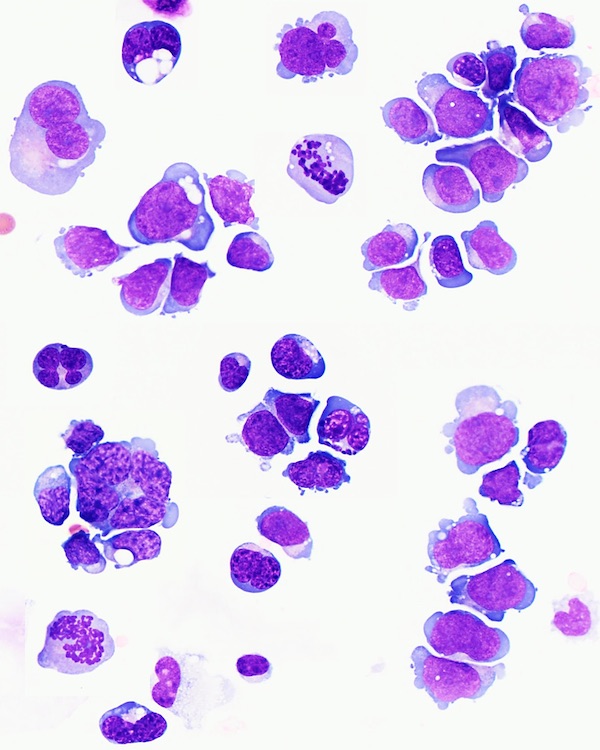
Microscopic (histologic) description
- Bone marrow biopsy: sheets or clusters of immature cells, tumor cells may show intrasinusoidal growth pattern (Am J Hematol 2017;92:292)
- Bone marrow aspirate: erythroid precursors ≥ 80% and proerythroblasts ≥ 30% of bone marrow cells
- Proerythroblasts have centrally located round nuclei, fine chromatin and 1 or more prominent nucleoli, deeply basophilic cytoplasm with vacuoles, often agranular
- Ring sideroblasts are common
- Myeloblasts are not increased
- Dysmegakaryopoiesis is common and dysgranulopoiesis is infrequent
- Mass in tissue: poorly differentiated tumor cells (Haematologica 2020;105:e194)
Microscopic (histologic) description
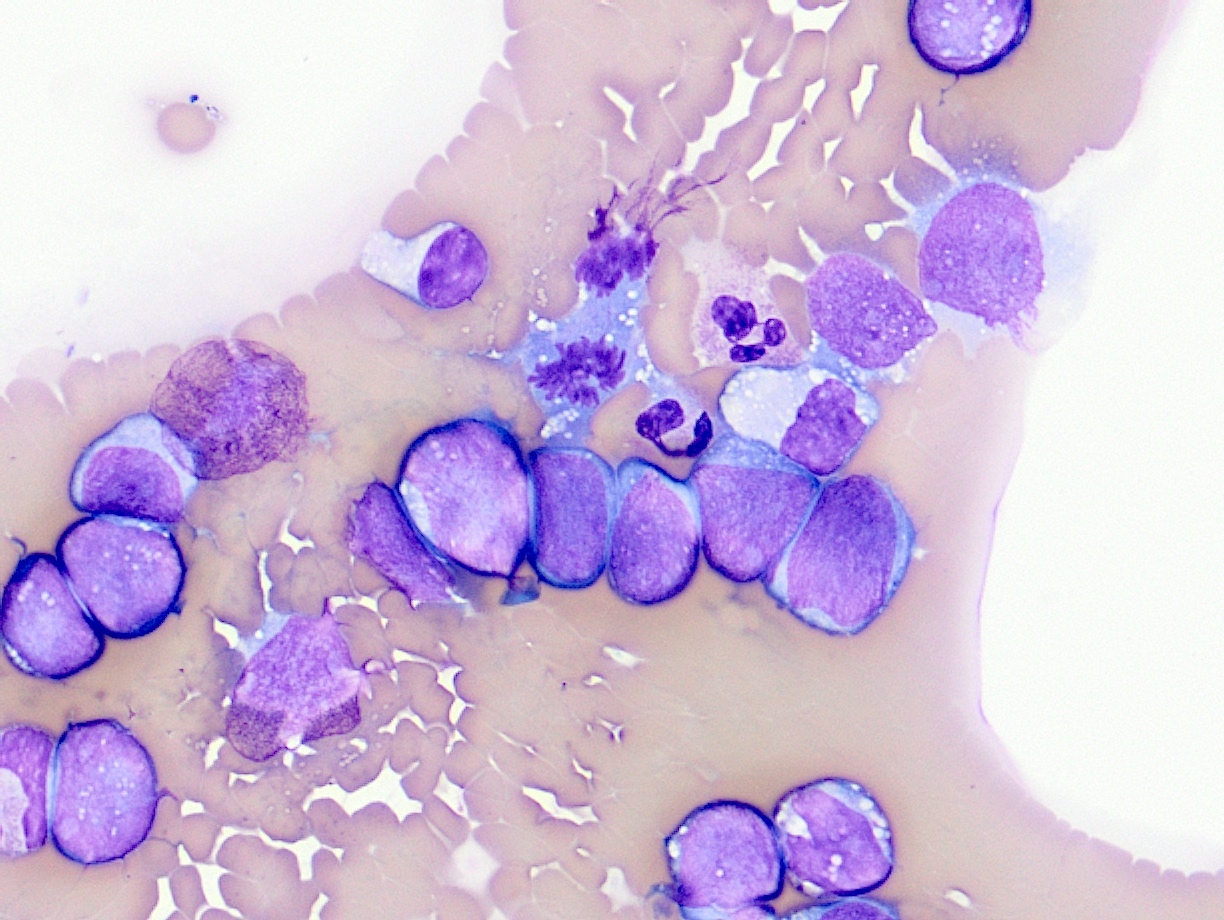
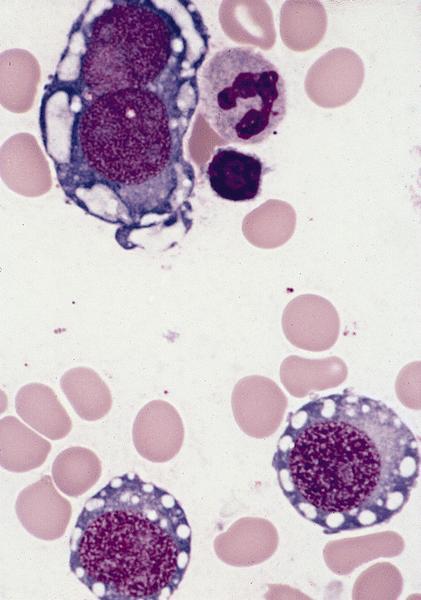
Cytology description
- Proerythroblasts are of medium to large size, with scant to moderate basophilic cytoplasm and dispersed chromatin; some have prominent nucleoli
- Erythroblasts are smaller with more condensed chromatin and polychromatic cytoplasm; some erythroblasts may be binucleated or multinucleated or with nuclear budding
- Cytoplasmic vacuoles, cytoplasmic blebbing or pseudopods are frequent
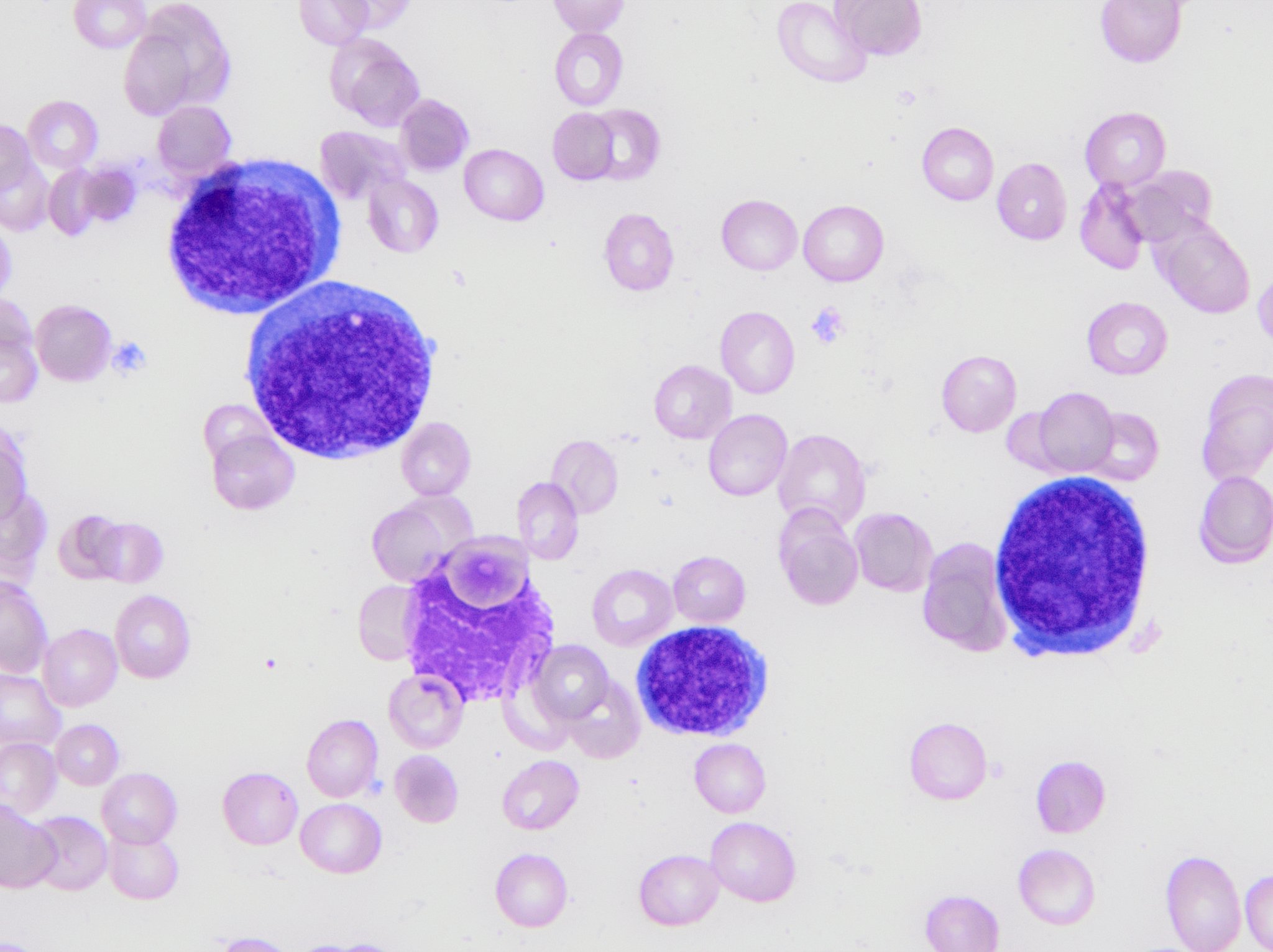
Peripheral smear description
- Anemia, thrombocytopenia or pancytopenia (Am J Hematol 2017;92:292)
- Circulating erythroblasts
Peripheral smear images
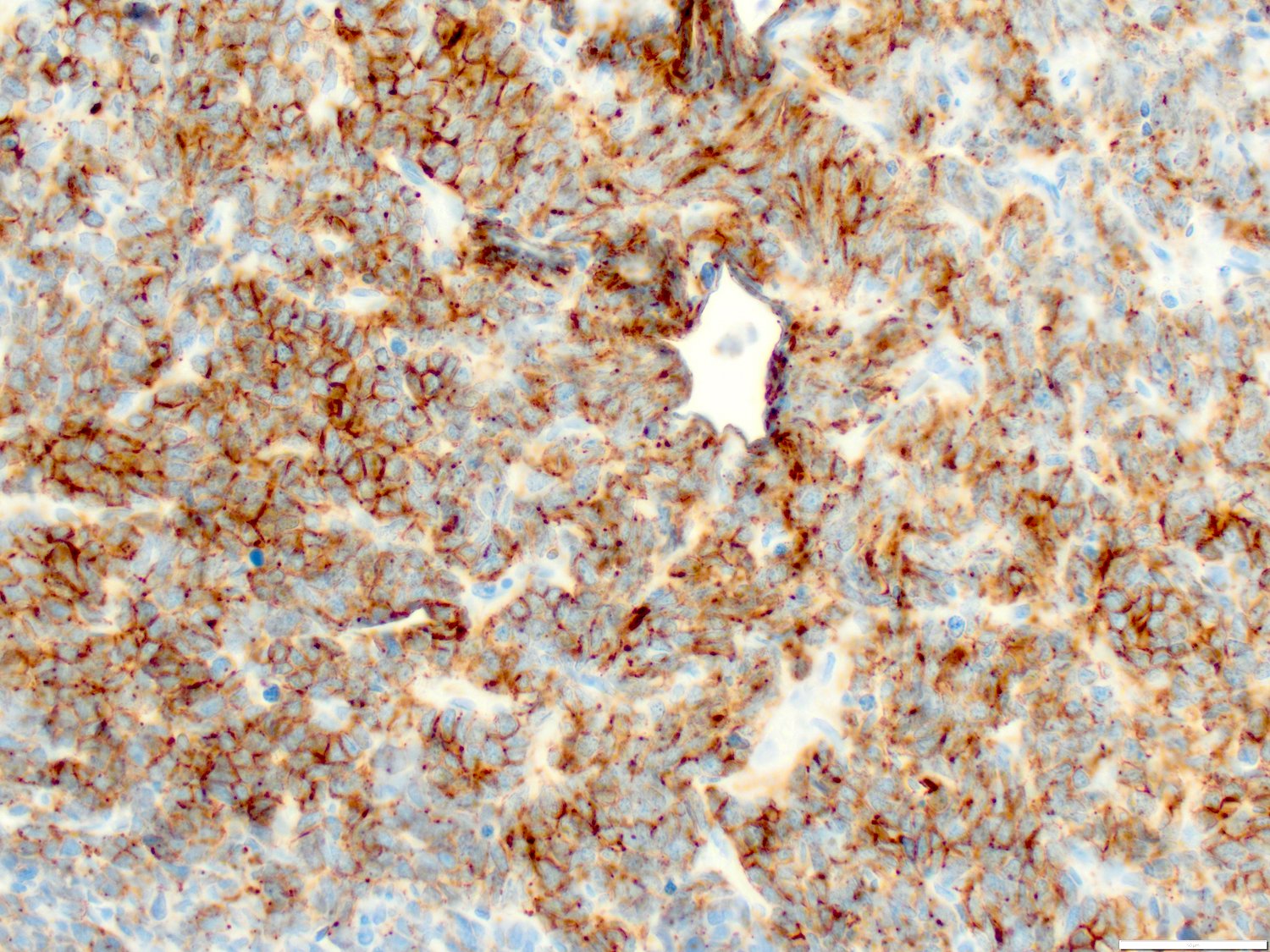
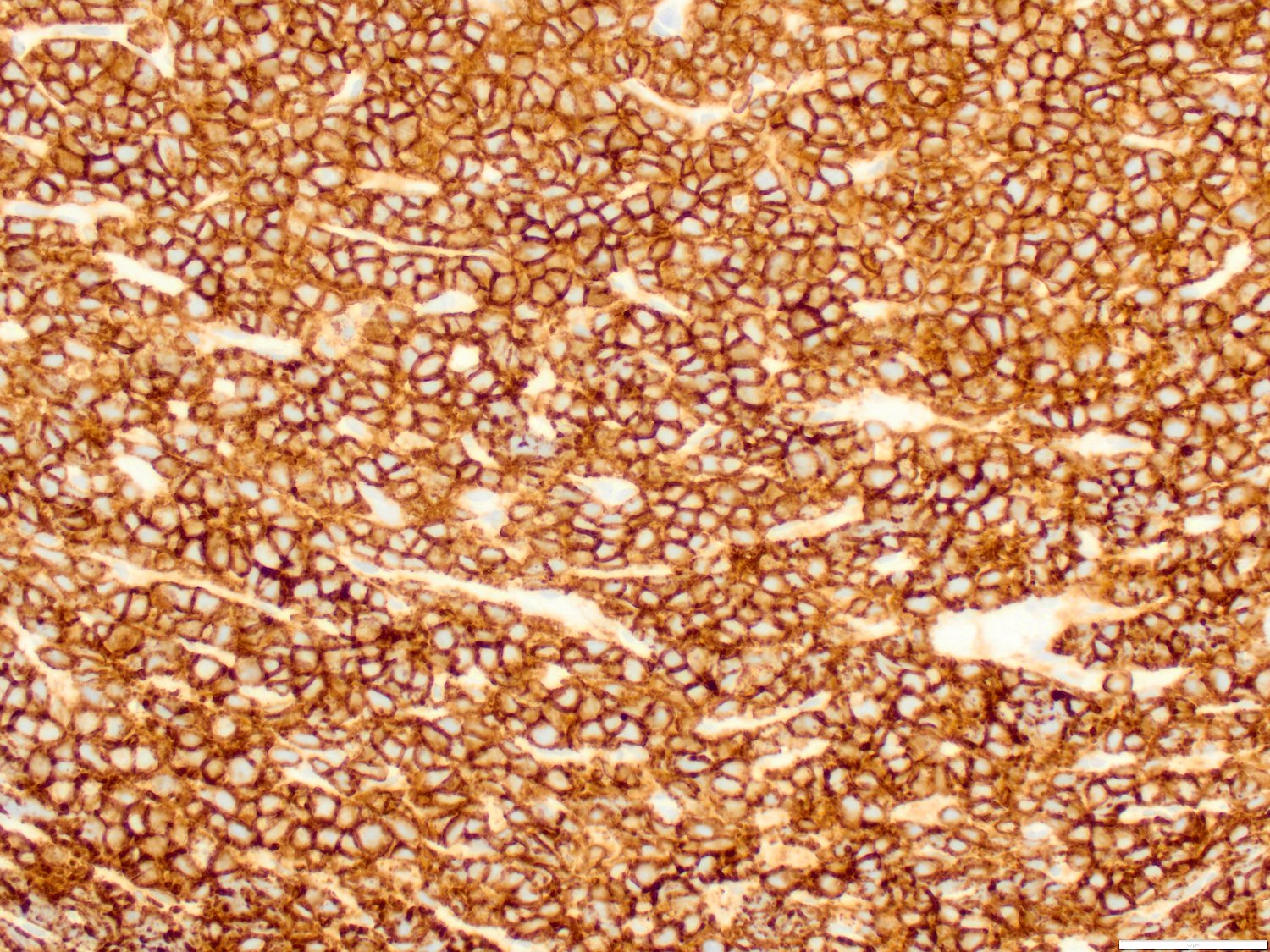
Positive stains
- Erythroid specific markers: E-cadherin (positive in majority of cases), hemoglobin A and glycophorin A (usually positive but can be negative in poorly differentiated erythroblasts) (Am J Hematol 2017;92:292)
- Nonlineage specific markers: CD36, CD43, CD71, CD117, GATA1, ferritin H
- These markers are unusually positive; however, they can be positive in other types of hematopoietic neoplasms
- CD36 is commonly positive in monocytic leukemia and acute megakaryocytic leukemia as well
- CD43 is positive in most AML, T cell acute lymphoblastic leukemia (T ALL) as well as some B cell ALL; it is a very useful marker for extramedullary poorly differentiated tumor to confirm hematopoietic lineage
- CD71 can be positive in other leukemic blasts, although its expression levels in PEL should be very bright
- CD117 is positive in most AML and some T ALL
- GATA1 is a transcription factor for erythroid development and it is positive in both PEL and acute megakaryocytic leukemia (Am J Clin Pathol 2017;147:420)
- Ferritin H is expressed in erythroid precursors as well as macrophages
- Special stains: PAS (usually in block-like pattern), alpha naphthyl acetate esterase, acid phosphatase
Negative stains
- CD34 and myeloperoxidase (Am J Hematol 2017;92:292)
- Megakaryocytic markers (CD41 and CD61), myeloid markers (CD13, CD33), CD45 and HLA-DR, usually negative but may be partially expressed in some cases (Am J Hematol 2017;92:292)
Flow cytometry description
Molecular / cytogenetics description
- Often complex karyotype, frequently -5/del(5q) and -7/del(7q) (Am J Hematol 2017;92:292)
- Biallelic (or multihit) TP53 loss of function mutation, including del17p (Nat Genet 2019;51:694)
- Pediatric PEL has distinctive molecular genetic changes that include relatively enriched NUP98 fusion, t(1;16)(p31;q24) NFIA::CBFA2T3 rearrangement, NFIA::CBFA2T1 fusion and t(11;20)(p11;q11) / ZMYND8::RELA (Haematologica 2020;105:e194, Leukemia 2013;27:980, PLoS One 2013;8:e63663, Blood Adv 2020;4:6000, Acta Neuropathol Commun 2024;12:12)
Sample pathology report
- Bone marrow, right, biopsy, clot section, aspirate smears, touch imprint and peripheral blood smear:
- Pure erythroid leukemia, blasts 95% of total nucleated cells (see comment)
- Comment:
- Peripheral blood:
- Red blood cells: normocytic normochromic anemia with slight anisopoikilocytosis
- White blood cells: Leukopenia with few large proerythroblasts. The blasts have scant basophilic cytoplasm, round nuclei and open chromatin and few have prominent nucleoli. Cytoplasmic vacuoles are noted in some blasts.
- Platelets: decreased with rare giant forms
- Bone marrow biopsy:
- Decalcification procedures performed to allow for histological assessment of submitted tissue
- Gross measurement: 0.5 cm
- Quality: adequate
- Cellularity: 100%
- Megakaryocytes: rare
- Infiltrate: The marrow is nearly completely replaced by sheets of immature cells with a high N:C ratio, open chromatin and some with prominent nucleoli.
- Bone marrow clot:
- Quality: inadequate, blood only, no particles with many immature cells
- Bone marrow smears:
- Quality / cellularity: adequate
- Granulocytes: markedly decreased
- Erythrocytes: markedly increased erythroid precursors with increased proerythroblasts
- Megakaryocytes: not seen
- Lymphocytes: decreased, few small and mature cells
- Bone marrow differential count: 500 total cells counted
- Blasts percentage: 95% (normal: 0 - 5%)
- Promyelocytes percentage: 0 (normal: 2 - 8%)
- Myelocytes percentage: 0 (normal: 5 - 20%)
- Metamyelocytes percentage: 0 (normal: 13 - 32%)
- Granulocytes percentage: 2% (normal: 7 - 30%)
- Monocytes percentage: 0 (normal: 0 - 5%)
- Lymphocytes percentage: 3% (normal: 3 - 17%)
- Plasma cells percentage: 0 (normal: 0 - 2%)
- Eosinophils percentage: 0 (normal: 0 - 4%)
- Basophils percentage: 0 (normal: 0 - 1%)
- Pronormoblasts percentage: 80% (normal: 1 - 8%)
- Normoblasts percentage: 15% (normal: 7 - 32%)
- M:E ratio (2 - 4): N/A
- Bone marrow touch imprint:
- Quality: adequate, similar to smear with increased erythroid blasts
- Flow cytometric analysis:
- Aberrant erythroid blasts, 95.2% of total nucleated cells (F19 - 160)
- Pending tests:
- Cytogenetic karyotype and FISH
- Peripheral blood:
Differential diagnosis
- Other types of acute leukemia, especially acute megakaryocytic leukemia:
- Other poorly differentiated malignancy or small blue round cell tumor:
- Immunophenotyping can aid in diagnosis of other poorly differentiated malignancies
- Tumor cells positive for cytokeratin suggest carcinoma, while those expressing neuroendocrine markers may indicate a sarcoma or small round cell tumor
- Additionally, tumor cells typically grow in sheets and exhibit adhesion to one another
- Immunophenotyping can aid in diagnosis of other poorly differentiated malignancies
- Reactive erythroid hyperplasia:
- Diagnosis of exclusion
Additional references
Practice question #1
Which of the following markers is most useful in diagnosing pure erythroid leukemia?
- CD34
- CD71
- CD117
- E-cadherin
- Myeloperoxidase (MPO)
Practice answer #1
D. E-cadherin is specific for pure erythroid leukemia (PEL) because it is only expressed in early erythroid precursors in hematopoietic cells. Answers A and E are incorrect because CD34 and MPO are negative in PEL. Answers B and C are incorrect because CD117 and CD71 are not lineage specific and can be expressed in other types of AML.
Comment Here
Reference: Acute erythroid leukemia (AML M6)
Comment Here
Reference: Acute erythroid leukemia (AML M6)
Practice question #2
A 7 year old boy presented with leukocytosis (55k/µL), anemia (Hb 7.5 g/dL) and thrombocytopenia (52k/µL). Peripheral blood smear (see image above) shows many mononucleated cells of variable sizes with high N:C ratio, round nuclei, open chromatin and deep blue cytoplasm. Some large cells have conspicuous nucleoli. By flow cytometric immunophenotyping, these cells are positive for CD36 and CD117 (heterogeneous) and negative for CD34, CD45, HLA-DR and all other lymphoid, myeloid and monocytic markers. Which of the following sentences is correct regarding this disease?
- ≥ 20% of these cells in blood or bone marrow are required for diagnosis as pure erythroid leukemia
- Cells are positive for CD61
- Cells most likely have a normal karyotype (46, XY)
- Cells show reactivity with alpha naphthyl acetate esterase, acid phosphatase and PAS
- Prognosis for this patient is good
Practice answer #2
D. Cells show reactivity with alpha naphthyl acetate esterase, acid phosphatase and PAS. These cells are consistent with proerythroblasts and the diagnosis is pure erythroid leukemia (PEL). Proerythroblasts are positive for alpha naphthyl acetate esterase, acid phosphatase and PAS. Answer B is incorrect because CD61 is a marker for megakaryocytic cells, although it may be positive on proerythroblastic leukemia cells occasionally. Answer C is incorrect because PEL normally has a complex karyotype. Answer A is incorrect because the diagnosis of PEL requires at least 30% proerythroblasts. Answer E is incorrect because the prognosis of PEL is generally poor.
Comment Here
Reference: Acute erythroid leukemia (AML M6)
Comment Here
Reference: Acute erythroid leukemia (AML M6)