Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Peripheral smear description | Positive stains | Flow cytometry description | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Tam I, Torlakovic EE. Dermatopathic lymphadenopathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesdermatopathiclymphadenitis.html. Accessed August 20th, 2025.
Definition / general
- Reactive lymphadenopathy characterized by paracortical expansion with increased interdigitating dendritic cells, Langerhans cells and histiocytes / macrophages, typically including melanophages
- Typically associated with chronic skin irritation, inflammation or infection
Essential features
- T cell mediated immune response to persistent cutaneous antigenic stimulation
- Paracortical expansion, often overall nodular in arrangement, with numerous interdigitating dendritic cells, Langerhans cells and histiocytes / macrophages
- Macrophages containing melanin pigment are typically present but vary widely in extent
- Classically associated with dermatologic disorders but can also present without any clinical evidence of skin disease
Terminology
- Lipomelanotic reticular hyperplasia
- Lipomelanotic reticulosis
- Dermatopathic lymphadenitis
- Pautrier-Woringer disease (Am J Dermatopathol 2004;26:499)
ICD coding
- ICD-10: I88.9 - nonspecific lymphadenitis, unspecified
Epidemiology
- Limited studies available
- Sex: initial case series suggested predilection for males, while recent case series included more women than men (Calif Med 1967;106:170, Mod Pathol 2020;33:1104)
- Age: any age, with peak in fifth to sixth decades (Calif Med 1967;106:170)
Sites
- Most commonly affects superficial axillary or inguinal lymph nodes
- Can be bilateral
- Generalized lymphadenopathy can occur uncommonly
- References: Medeiros: Ioachim's Lymph Node Pathology, 5th Edition, 2021, Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017
Pathophysiology
- Persistent cutaneous antigenic stimulation leading to local cytokine release, which mediates migration of Langerhans cells to regional lymph nodes (J Exp Med 2002;196:417)
- Partially through tumor necrosis factor alpha mediated downregulation of epithelial adhesion molecules (e.g., E-cadherin) in skin
- Antigen processing and presentation by dendritic cells and Langerhans cells, leading to a T cell mediated immune response
- Presence of melanophages in part due to pigment incontinence, melanophagocytosis and migration from skin to lymph node (Mod Pathol 2020;33:1104, Int Immunol 2001;13:695)
Etiology
- Dermatologic disorders
- Benign: atopic dermatitis, chronic contact dermatitis, erythrodermic drug reaction, psoriasis, stasis dermatitis
- Malignant: mycosis fungoides, melanoma, squamous cell carcinoma, Kaposi sarcoma
- No underlying dermatologic disorder can be identified in a subset of cases (12 - 48%) (Calif Med 1967;106:170, Mod Pathol 2020;33:1104)
Clinical features
- Moderately enlarged, firm, moveable and nontender lymph nodes
- Typically associated with chronic dermatologic disorders (Mod Pathol 2020;33:1104)
- Commonly found in patients with mycosis fungoides and Sézary syndrome
- Higher association with severe / florid dermatopathic lymphadenopathy (Mod Pathol 2020;33:1104)
- Can be found in patients with autoimmune disease / presence of autoantibodies (Int J Surg Pathol 2004;12:127)
Diagnosis
- Clinical, radiologic and histologic evaluation of lymph node biopsy
Laboratory
- Peripheral eosinophilia (up to 35%)
- Depending on the underlying condition, if any (e.g., autoimmune dermatitis could be associated with autoantibodies)
- References: Medeiros: Ioachim's Lymph Node Pathology, 5th Edition, 2021, Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017
Radiology description
- Moderately enlarged lymph node(s)
- Can be FDG avid on 18F-FDG PET / CT (World J Nucl Med 2020;20:205, Chin Med J (Engl) 2015;128:3121)
Radiology images
Prognostic factors
- Usually self resolving, depending on underlying condition
Case reports
- Newborn boy with chromosome 22q11.2 deletion syndrome and generalized skin rash (Am J Case Rep 2020;21:e924961)
- 21 year old man with fever, pruritis and nonblanching rash (Clin Case Rep 2018;6:1637)
- 50 year old woman without skin disease (J Cytol 2016;33:49)
- 56 year old woman with a history of breast carcinoma in remission (Am J Case Rep 2017;18:1330)
Treatment
- Treatment of the underlying dermatologic disorder
Gross description
- Enlarged lymph node (usually > 1.5 cm in greatest dimension)
- Yellow to tan with occasional brown pigmented foci
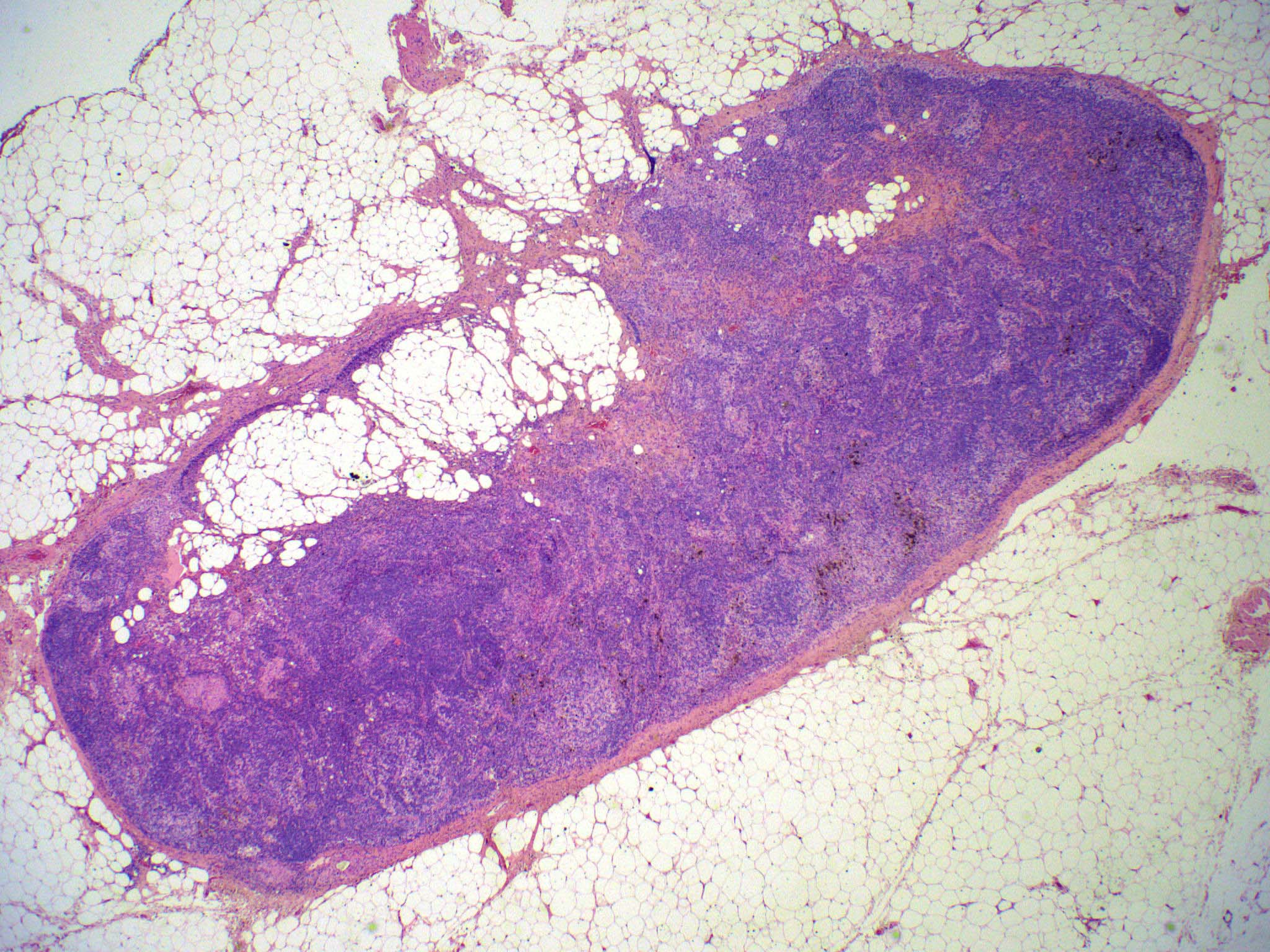
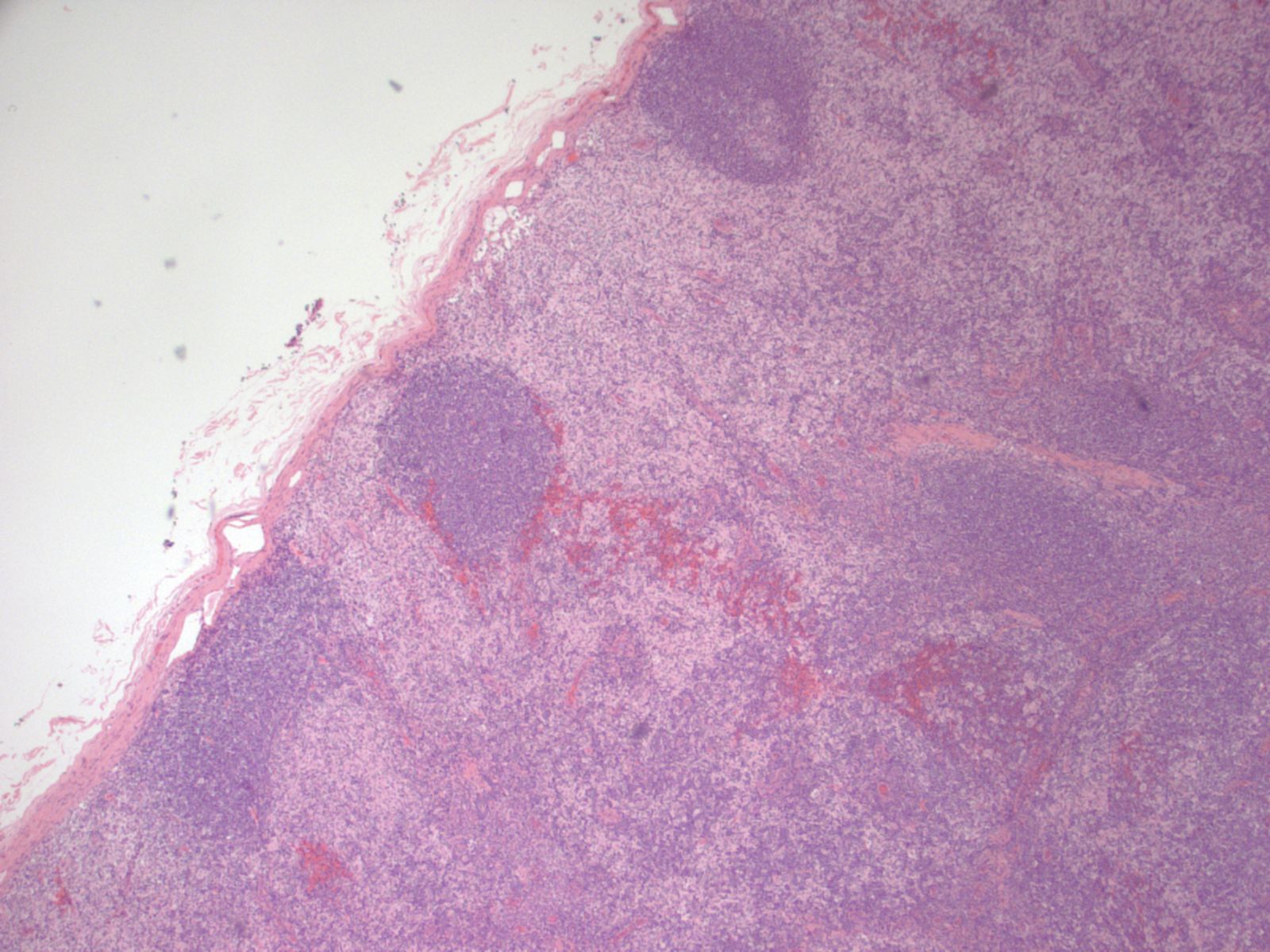
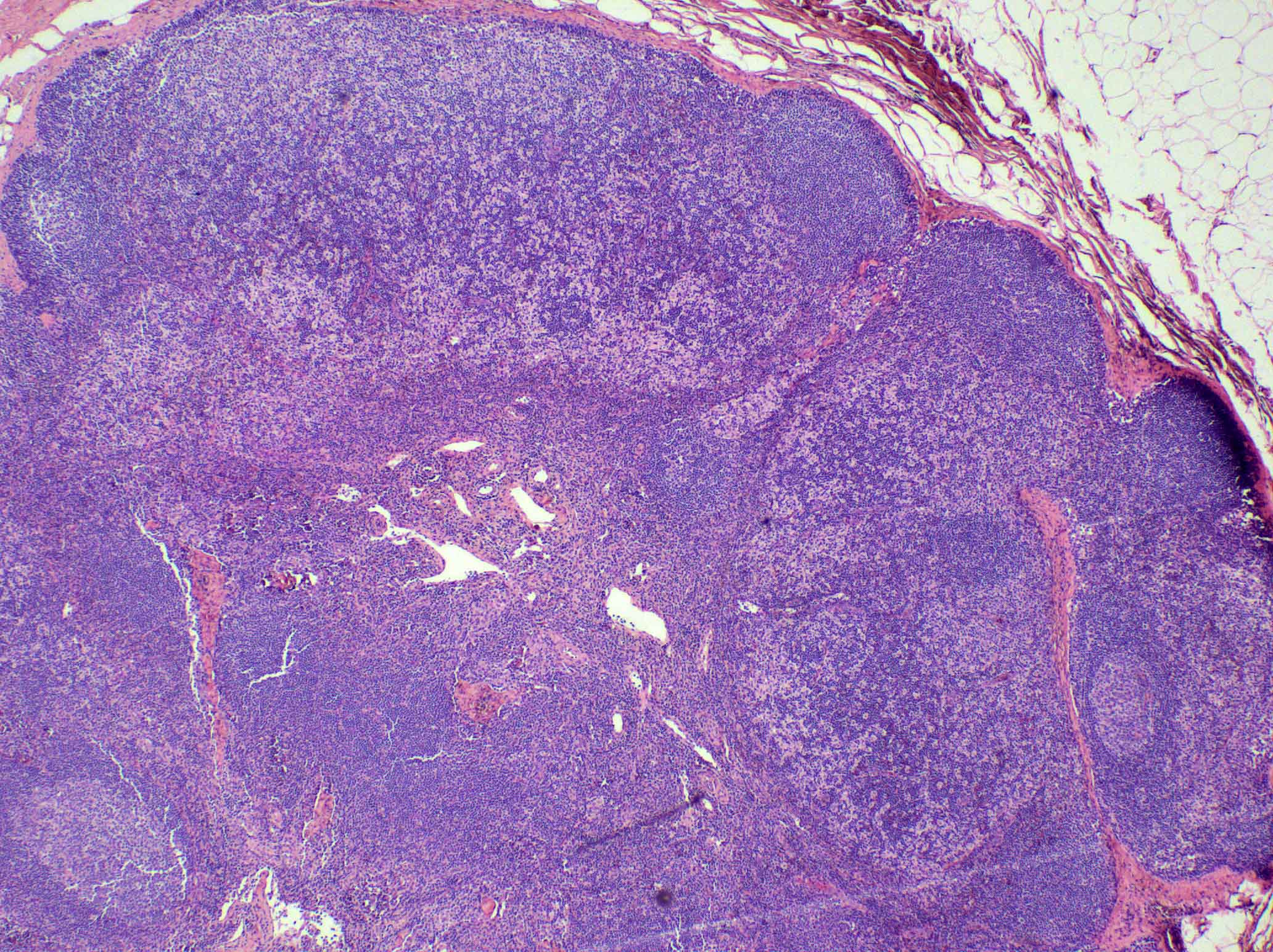
Microscopic (histologic) description
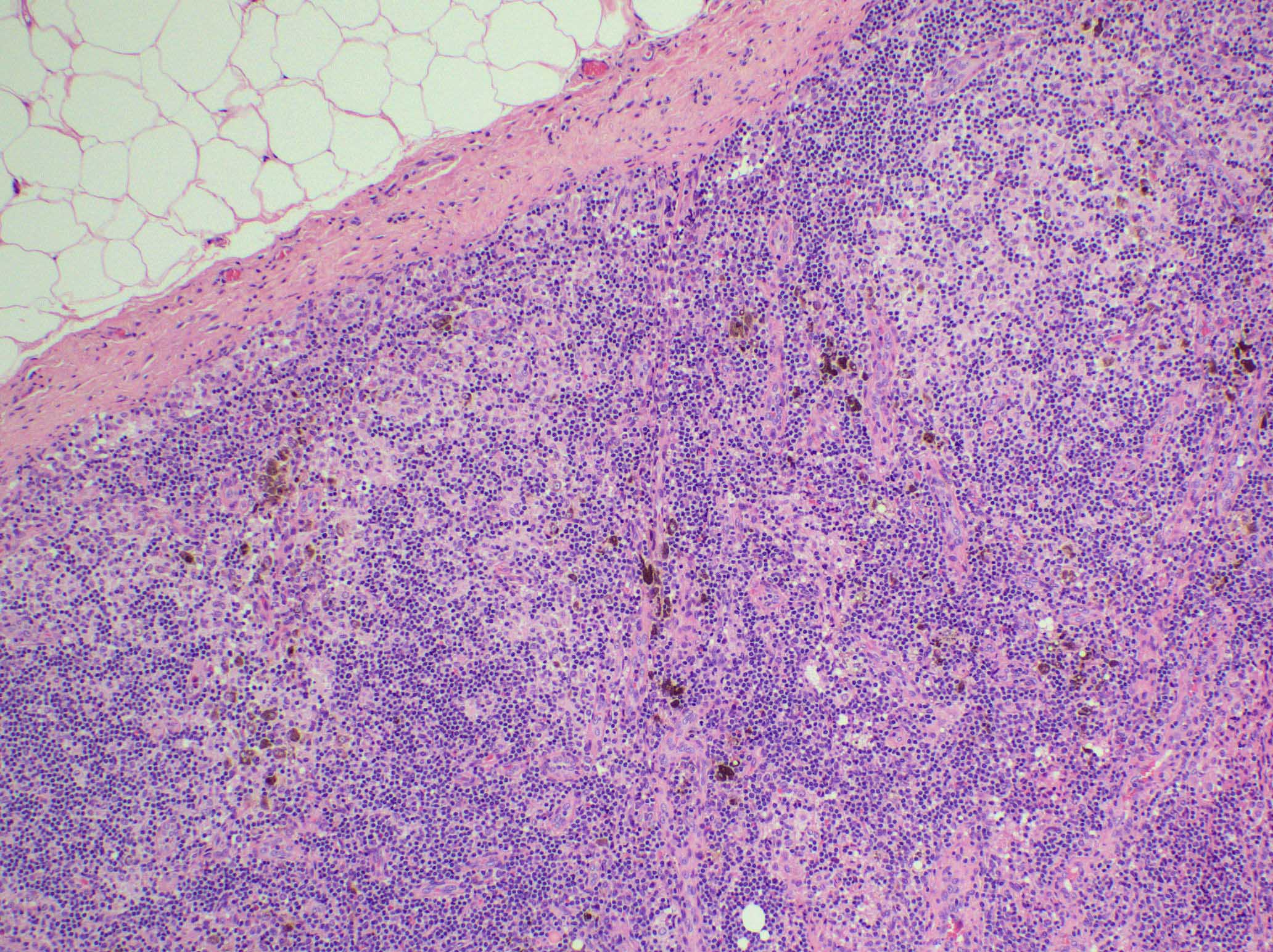
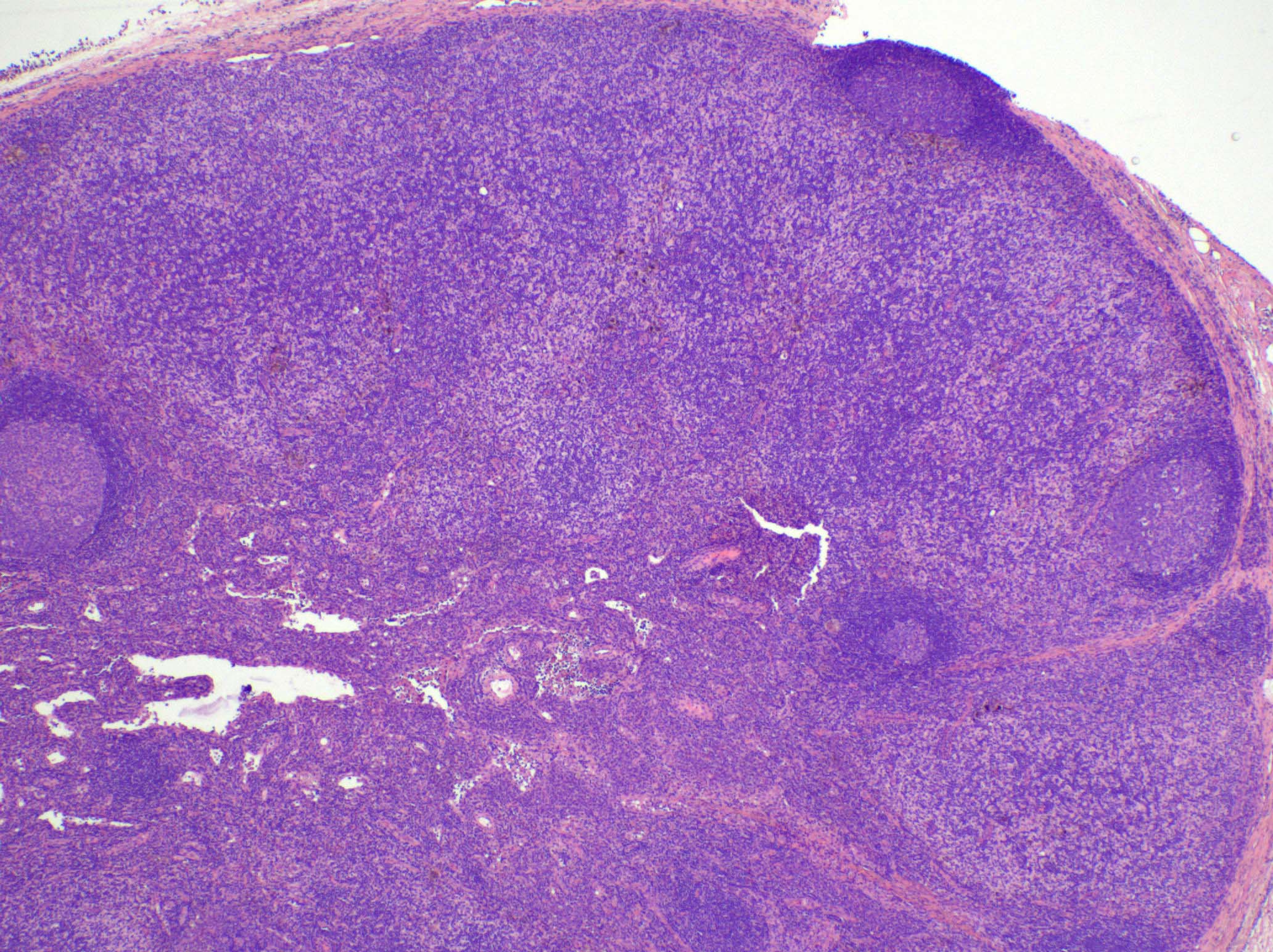
- There is always preserved nodal architecture with intact capsule
- Follicular hyperplasia may be present but it is usually minimal
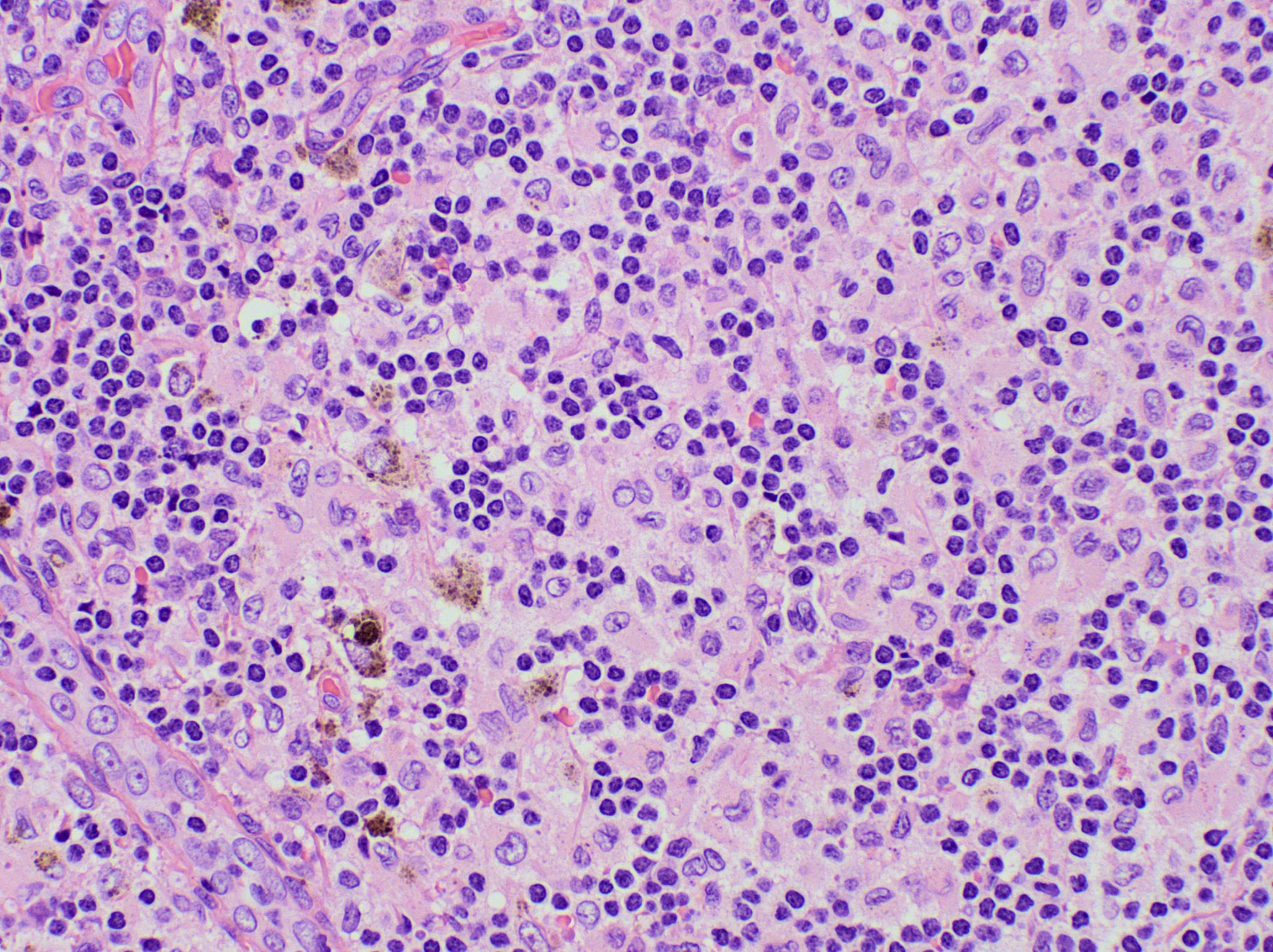
- Spectrum of changes from mild to severe, characterized by paracortical expansion with pale, irregularly shaped areas containing numerous pale staining histiocytes, interdigitating dendritic cells, Langerhans cells and occasional immunoblasts
- Predominance of interdigitating dendritic cells over Langerhans cells, which are indistinguishable on morphology alone
- Both cell types show ill defined cell borders with fine irregular reniform nuclear contours and occasional nuclear grooves
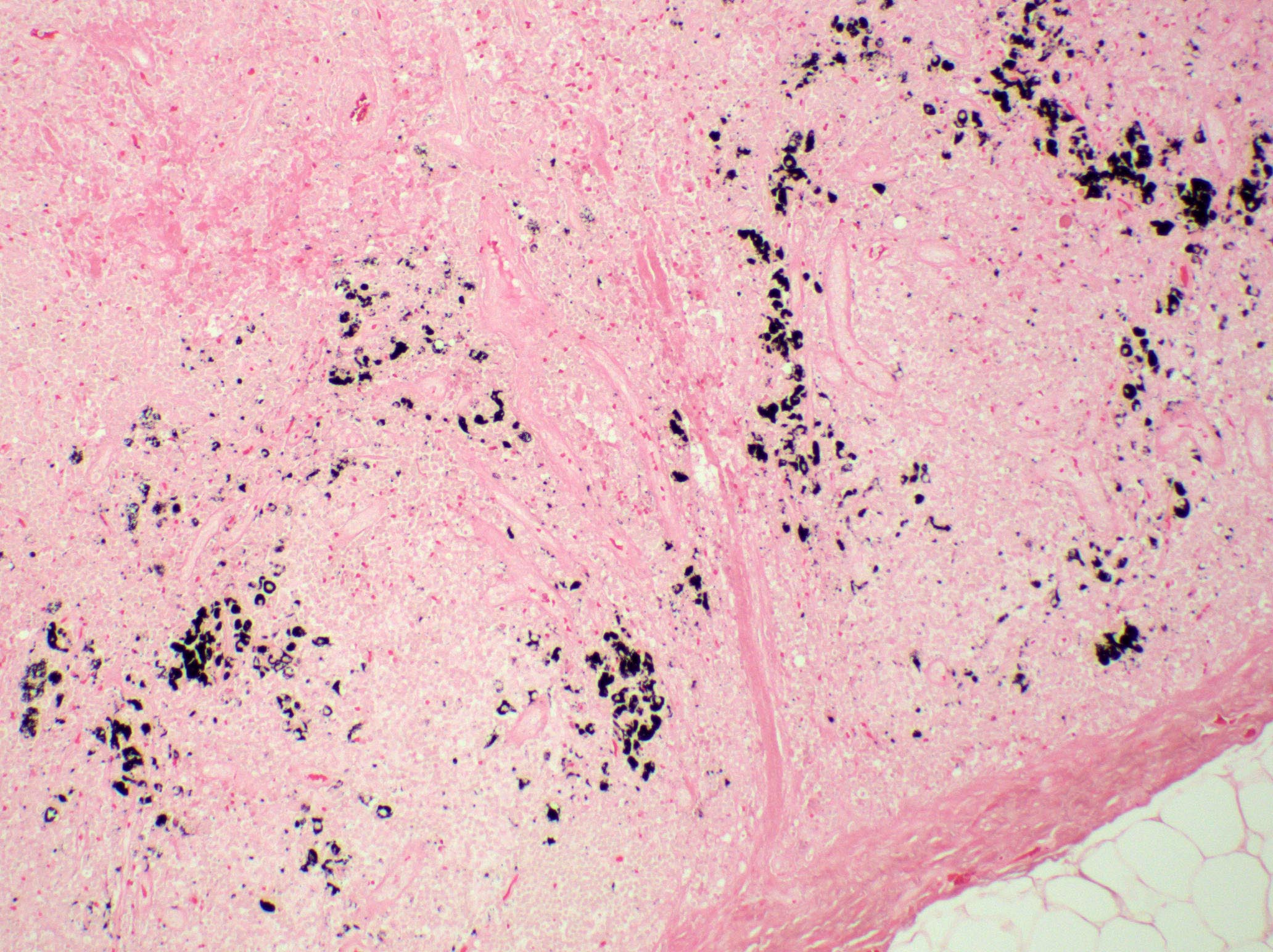
- Paracortical or sinusoidal histiocytes and macrophages often contain cytoplasmic melanin pigment but they also can contain hemosiderin or lipid
- Medullary plasmacytosis is variable
- Distended sinuses with histiocytes, plasma cells and eosinophils can be present
- Variable, usually mild capillary hyperplasia
- Mild / early
- Increased interdigitating dendritic cells that do not form nodules or networks, admixed with Langerhans cells and histiocytes
- Hyperplastic lymphoid follicles
- Severe / florid
- Large vague nodules or sheets of interdigitating dendritic cells that can compress lymphoid follicles
- Rarely, sinuses can be partially compressed
- Severe forms are more frequently seen in patients with mycosis fungoides
- References: Medeiros: Ioachim's Lymph Node Pathology, 5th Edition, 2021, Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017
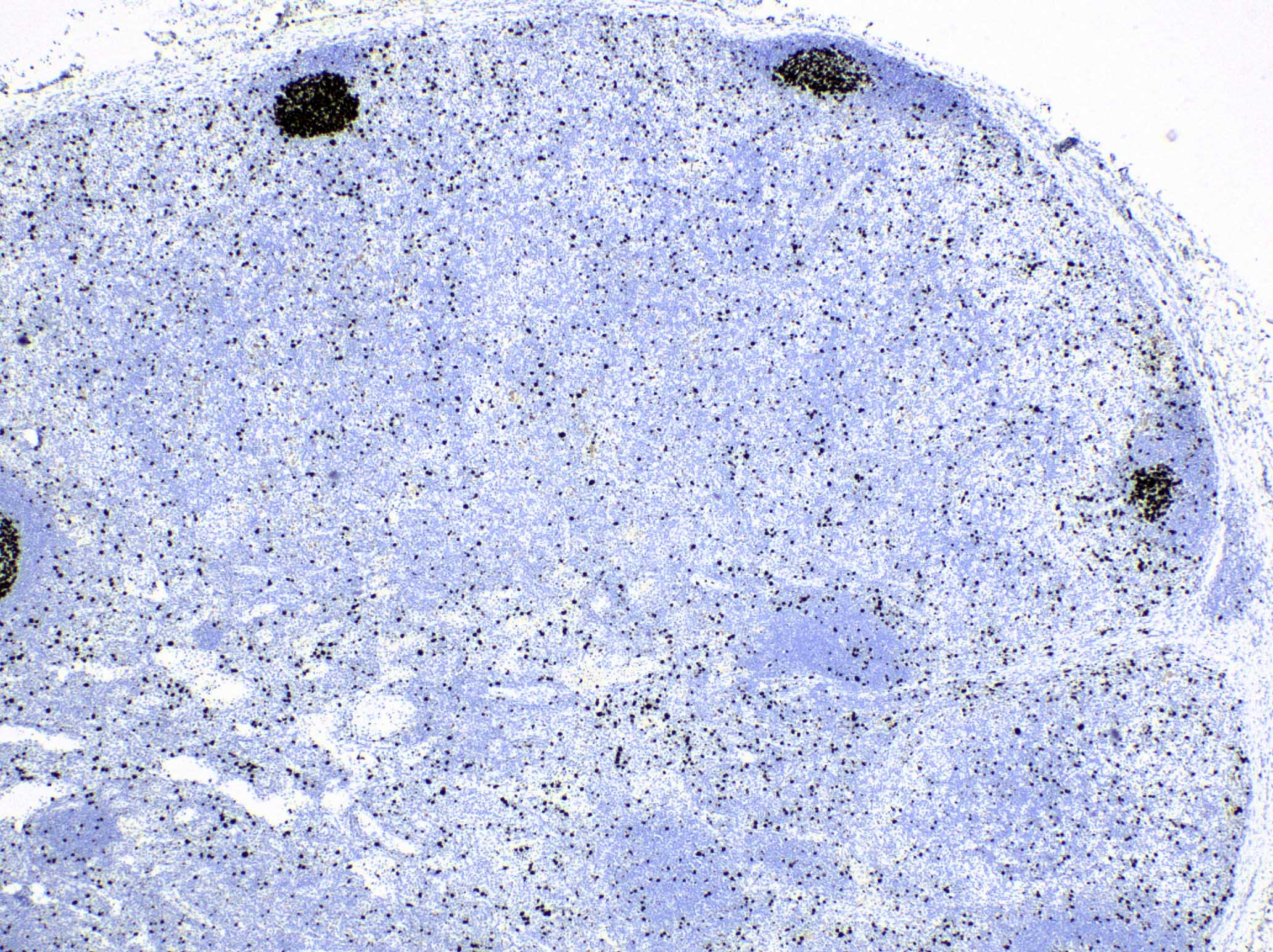
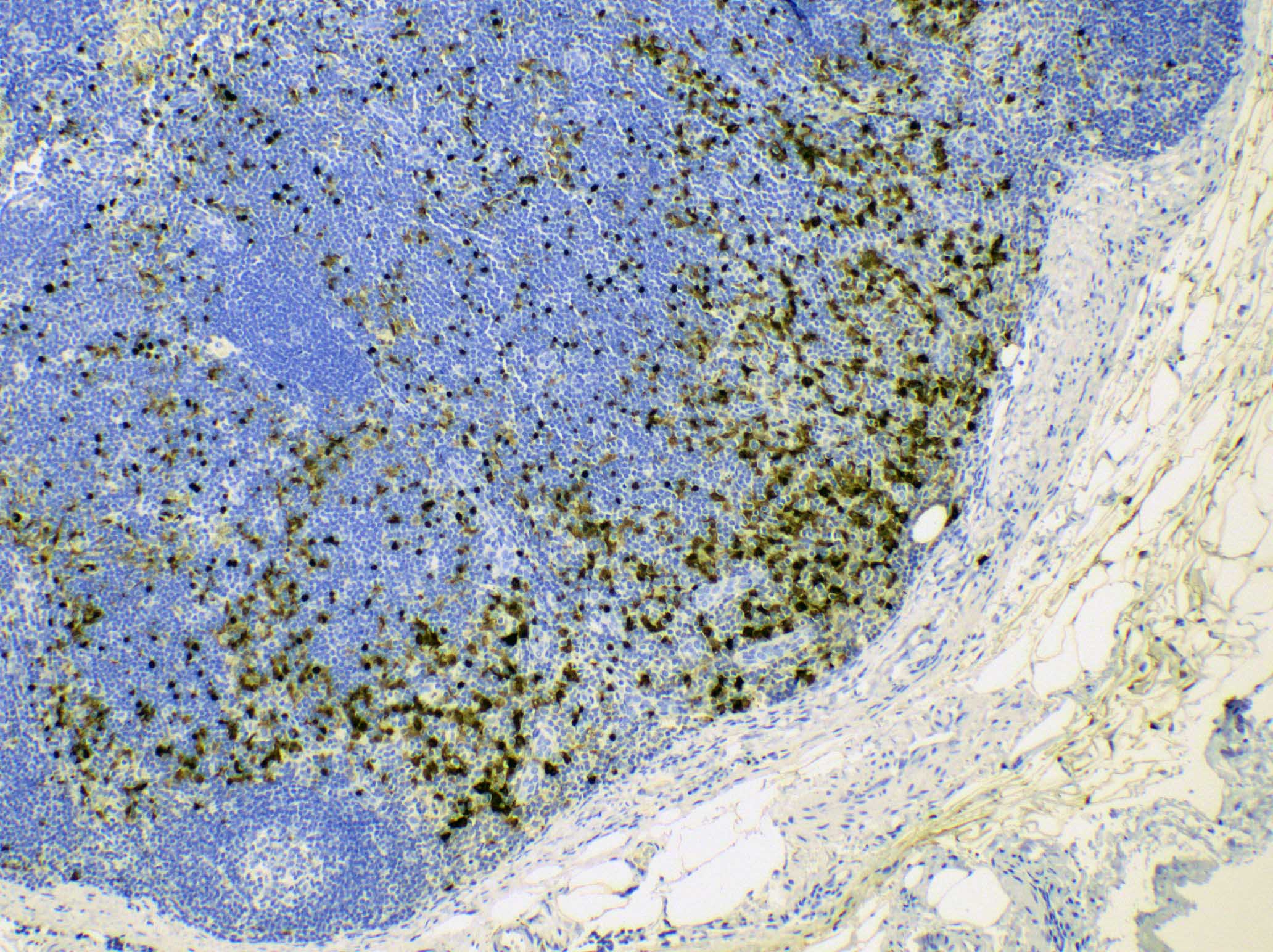
Microscopic (histologic) images
Contributed by Ingrid Tam, M.D., M.Sc., Emina Emilia Torlakovic, M.D., Ph.D. and Nikhil Sangle, M.D. (Case #396)
Peripheral smear description
- Peripheral eosinophilia in up to 35% of cases
Positive stains
- S100, CD1a, CD207 / langerin: Langerhans cells
- CD4 and CD8: typically there is great predominance of CD4+ T cells over CD8
- Fontana-Masson silver stain for melanin; melanin histochemical stain is often positive even when melanin is not readily identified on H&E sections
- S100, MUM1 / IRF4: interdigitating dendritic cells (Am J Surg Pathol 2022;46:1514)
- CD68: histiocytes and dendritic cells
- Prussian blue for hemosiderin: this is less useful as it is not as specific as melanin for this diagnosis
- Pan-T cell markers CD2, CD5 and especially CD7 may be useful if there is a suspicion of involvement by mycosis fungoides or other cutaneous T cell lymphoproliferative disease (e.g., CD7 is typically negative in mycosis fungoides)
- CD30: immunoblasts; CD30+ immunoblasts are not required for diagnosis
Flow cytometry description
- No evidence of aberrant B or T cell populations, except if involved by mycosis fungoides or other primary cutaneous lymphoproliferative disorder
Electron microscopy description
- Predominance of interdigitating cells over Langerhans cells
- Langerhans cells: cytoplasmic Birbeck granules are defining feature
- Both interdigitating cells and Langerhans cells have fine irregular nuclear contours and finger-like cytoplasmic extensions
- References: Medeiros: Ioachim's Lymph Node Pathology, 5th Edition, 2021, Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017
Molecular / cytogenetics description
- No evidence of immunoglobulin or T cell receptor gene rearrangement when associated with benign skin disease
- Monoclonal T cell receptor gene rearrangements when associated with mycosis fungoides / Sézary syndrome or other primary cutaneous lymphoproliferative disorder
Sample pathology report
- Lymph node, left axilla, excision:
- Reactive changes consistent with dermatopathic lymphadenopathy (see comment)
- Comment: The lymphoid architecture is preserved. There is evidence of paracortical hyperplasia with dendritic cells, Langerhans cells and histiocytes. Melanin pigment is noted. There is also mild focal follicular hyperplasia. The overall features are consistent with dermatopathic lymphadenopathy.
Differential diagnosis
- Mycosis fungoides:
- Neoplastic T lymphocytes with cerebriform nuclei that demonstrate partial loss of CD7
- Lymph node may be involved even if it is not possible to confirm the presence of atypical T cells by morphology or immunophenotyping; therefore, TCR clonality assay is always required in patients with primary cutaneous lymphoproliferative disorder where regional lymph nodes show dermatopathic changes (Am J Surg Pathol 1981;5:343)
- Flow cytometry: loss of CD7 is the most frequent finding; other pan-T cell markers including CD2, CD3, CD8 and CD5 may also be altered (low, high, negative, double positive CD4 / CD8, etc.); downregulated CD26 is often seen
- T cell receptor (TCR) clonality assay: monoclonal TCR gene rearrangement
- Langerhans cell histiocytosis:
- Sinusoidal involvement with partial or total effacement of lymph node architecture
- Formation of aggregates and sheets of Langerhans cells is more typical of Langerhans cell histocytosis than dermatopathic lymphadenopathy, even when the latter is florid
- Predominance of large Langerhans cells with abundant eosinophilic cytoplasm
- Often with abundant eosinophils
- Molecular: BRAF V600E in up to 50% of cases; BRAF V600E IHC assay may also be used
- Classic Hodgkin lymphoma:
- Metastatic melanoma:
- Melanoma cells are positive for HMB45 (cytoplasmic), SOX10 (nuclear) or S100 (nuclear / cytoplasmic), MelanA / MART1 (cytoplasmic)
- Ki67 proliferative index often > 10% but this is a nonspecific finding
- Reactive lymphadenopathy with paracortical hyperplasia due to viral infections:
- Positive serology, culture or in situ hybridization studies
- Usually no significant increase in interdigitating dendritic cells or Langerhans cells
- Melanophages are typically absent
- Toxoplasma lymphadenitis:
- Sinuses with monocytoid B cells
- Interfollicular and paracortical epithelioid histiocytes
- Prominent follicular hyperplasia
- No significant increase in interdigitating dendritic cells or Langerhans cells
- Melanophages typically absent
Practice question #1
Which of the following histologic patterns is characteristically seen in dermatopathic lymphadenopathy?
- Florid reactive follicular hyperplasia
- Nonnecrotizing granulomatous inflammation
- Paracortical expansion with a predominance of interdigitating cells admixed with Langerhans cells and histiocytes
- Reactive follicular hyperplasia, interfollicular epithelioid histiocytes and monocytoid B cell hyperplasia
- Sinus expansion with histiocytes showing emperipolesis
Practice answer #1
C. Dermatopathic lymphadenopathy is characterized by a paracortical expansion with increased interdigitating dendritic cells, Langerhans cells and histiocytes / macrophages. Florid reactive follicular hyperplasia (answer A) can be seen in a number of conditions, including HIV lymphadenitis, rheumatoid arthritis and syphilis. A variety of etiologies can lead to nonnecrotizing granulomatous inflammation (answer B), including sarcoidosis, infections and autoimmune conditions. Reactive follicular hyperplasia, interfollicular epithelioid histiocytes and monocytoid B cell hyperplasia describe the triad of Toxoplasma lymphadenitis (answer D). Sinus histiocytosis with emperipolesis (answer E), characterizes Rosai-Dorfman disease.
Comment Here
Reference: Dermatopathic lymphadenopathy
Comment Here
Reference: Dermatopathic lymphadenopathy
Practice question #2
Practice answer #2
E. Polyclonal population by TCR assays. In dermatopathic lymphadenopathy, T cell receptor gene rearrangement assays show a polyclonal population. There is no evidence of B or T cell clonality (answers C and D); however, dermatopathic lymphadenopathy detected in patients with mycosis fungoides may show T cell clonality. This may be the case even without morphologic evidence of involvement by mycosis fungoides (e.g., stage N1b, with histopathology Dutch grade 1). BRAF V600E mutation (answer A) is associated with several hematologic conditions, including Langerhans cell histiocytosis and hairy cell leukemia. MAP2K1 mutations (answer B) can be seen in a subset of Langerhans cell histiocytosis cases as well as in Rosai-Dorfman disease.
Comment Here
Reference: Dermatopathic lymphadenopathy
Comment Here
Reference: Dermatopathic lymphadenopathy