Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Dutta R, Mannan R. Low grade nasopharyngeal papillary adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalpapillaryadenocarcinoma.html. Accessed September 5th, 2025.
Definition / general
- Low grade primary adenocarcinoma of nasopharynx
Essential features
- Relatively rare nasopharyngeal tumor
- No known etiologic agents; lacks Epstein-Barr virus (EBV) association
- Morphologically, an adenocarcinoma with predominant papillary architecture and hyalinized cores
- Mimics papillary thyroid carcinoma; may be TTF1+, however, PAX8- and thyroglobulin-
- Excellent prognosis with no known metastases
Terminology
- Thyroid-like low grade nasopharyngeal papillary adenocarcinoma
- Low grade nasopharyngeal papillary adenocarcinoma
ICD coding
- ICD-10: C11.9 - malignant neoplasm of nasopharynx, unspecified
Epidemiology
- Uncommon tumor of nasopharynx (Ear Nose Throat J 2017;96:456)
- < 1% of nasopharyngeal malignancies
- Median age of 37 years but occurs over a wide age range (reported range: second - seventh decade)
- No gender predilection
Sites
- May occur anywhere in nasopharynx but common locations are roof, posterior wall and lateral wall of nasopharynx
Pathophysiology
- Exact pathogenesis is unclear
Etiology
- No known etiologic agents
- Not associated with wood dust exposure or other known factors
- Lacks any EBV or human papillomavirus (HPV) association
- Association with Turner syndrome in a rare case (Med J Malaysia 1998;53:104)
Clinical features
- Nasal obstruction is the most common presenting symptom (Am J Clin Pathol 2019;152:582)
- Tumors usually remain confined within the nasopharynx
- Subset of patients with tumor involving the posterior and lateral nasopharyngeal walls present with otitis media or postnasal drip
- Slow growing and indolent
Diagnosis
- Imaging followed by biopsy
Radiology description
- Nasopharyngeal endoscopy typically reveals polypoid or pedunculated masses
- Sinus computed tomography (CT) images show circular or nodular mass at the nasopharynx or the edge of the nasal septum, moderately to strongly enhancing on contrast enhanced CT (CECT) with no bone destruction (Cancer Manag Res 2021;13:1271)
- Sinus magnetic resonance imaging (MRI) reveals masses with moderate signals in plain T1 weighted images and strong signals in T2 weighted images
Prognostic factors
- Excellent prognosis with complete surgical excision
- Rarely recurs (if incomplete excision)
- No metastases reported to date (Ear Nose Throat J 2017;96:456)
Case reports
- 22 year old woman with nasopharyngeal papillary adenocarcinoma harboring a ROS1::GOPC fusion (Medicine (Baltimore) 2021;100:e24377)
- 42 year old nonsmoking woman presented with foreign body sensation in pharynx and dry throat for 1 month (Transl Cancer Res 2020;9:4457)
- 50 year old woman harboring biphasic thyroid-like low grade nasopharyngeal papillary adenocarcinoma with a prominent spindle cell component (Diagnostics (Basel) 2020;10:323)
Treatment
- Complete surgical excision is usually curative
- Some patients may receive radiation, though role of radiotherapy is unclear
Gross description
- Soft, exophytic mass with papillary, polypoidal or nodular appearance (Ear Nose Throat J 2017;96:456)
- Size can vary from a few millimeters to 3 cm
- Consistency may be soft or gritty
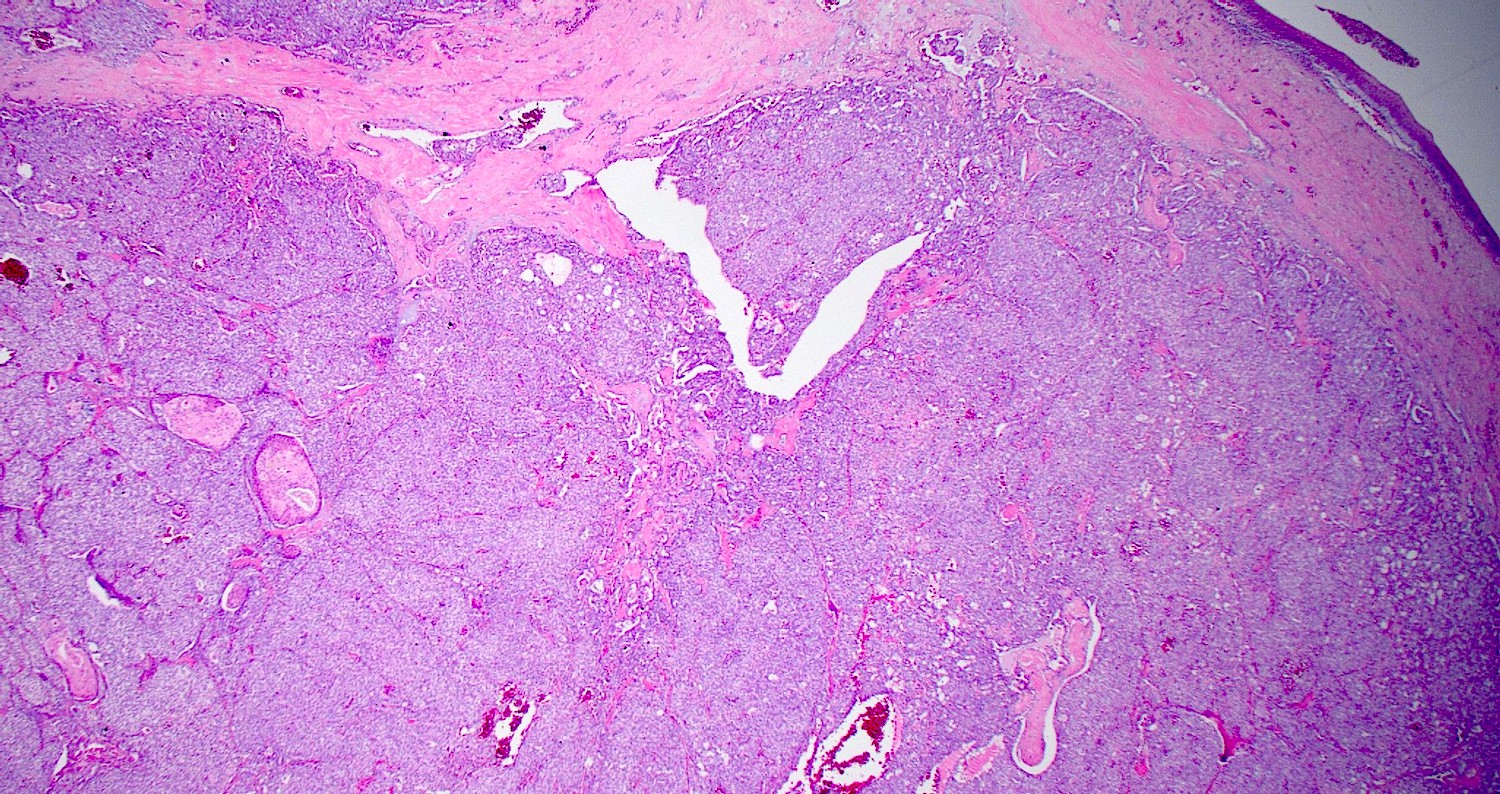
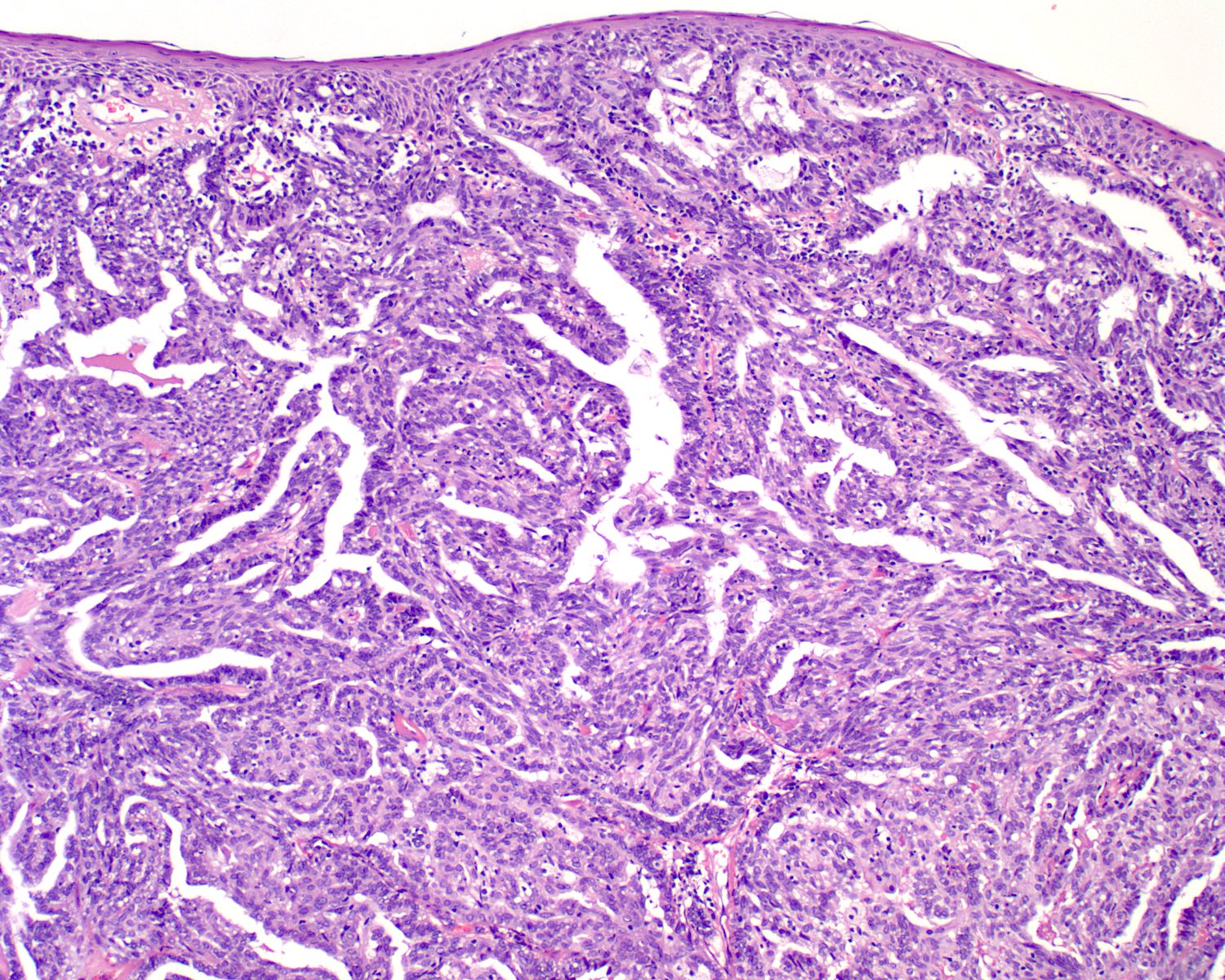
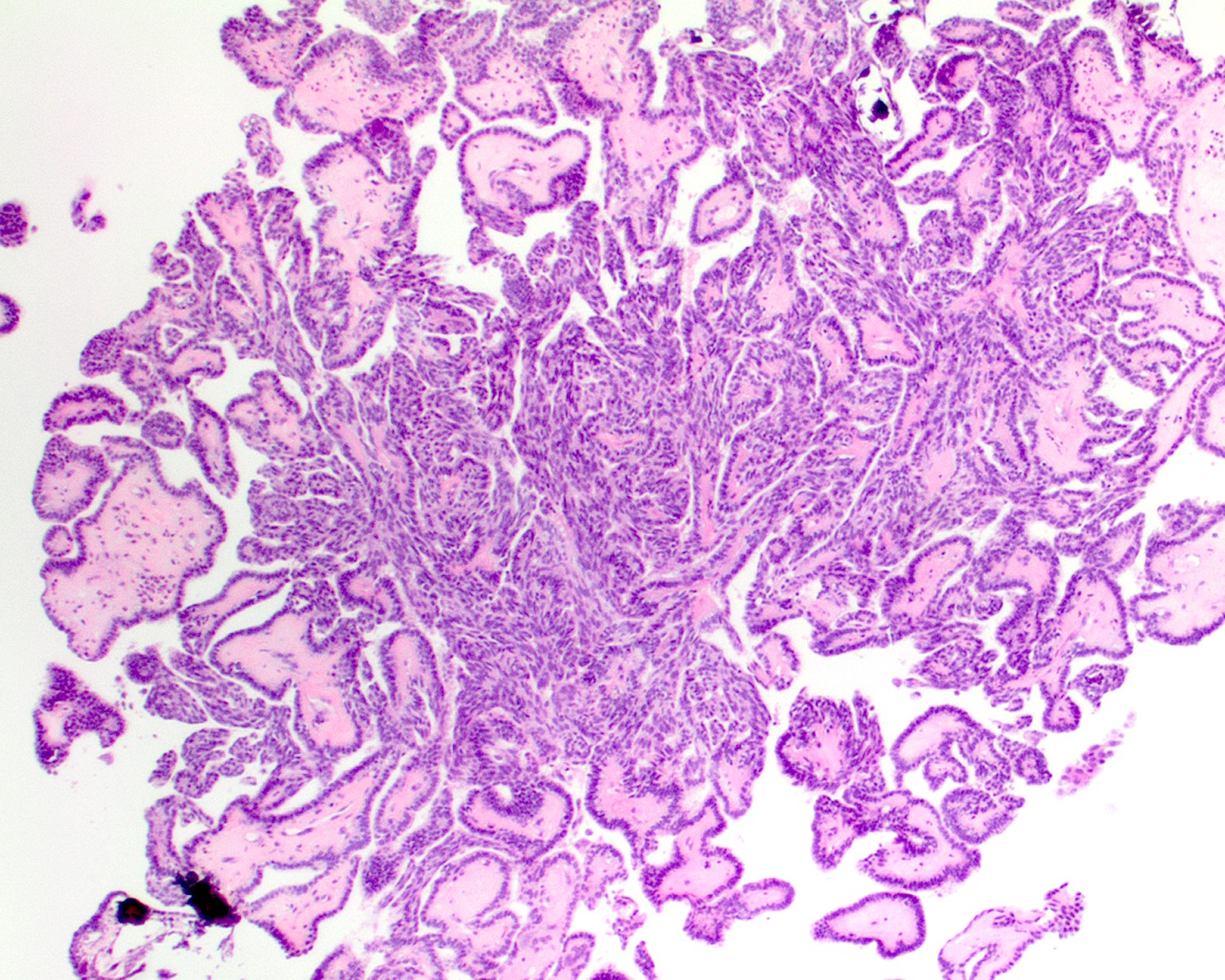
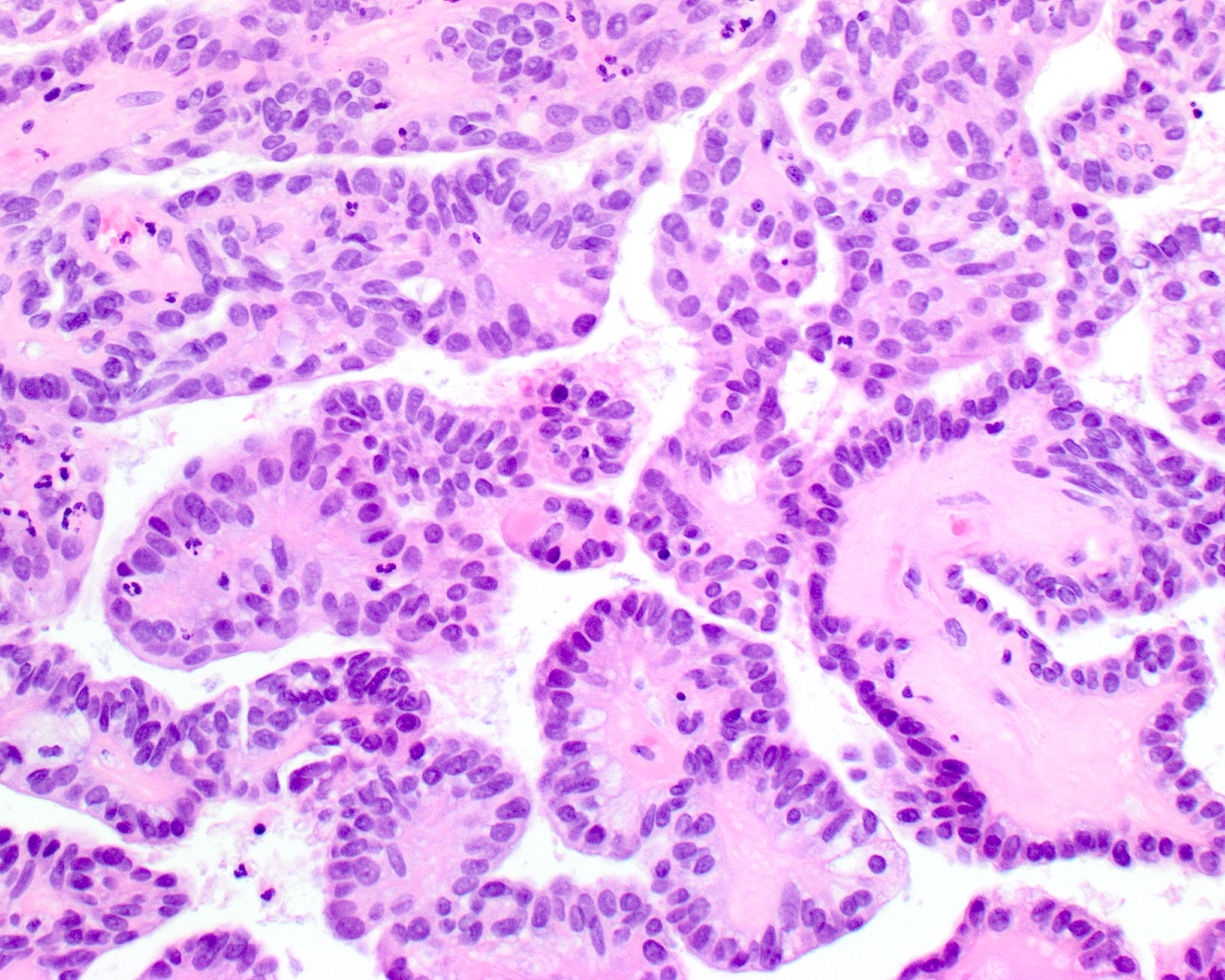
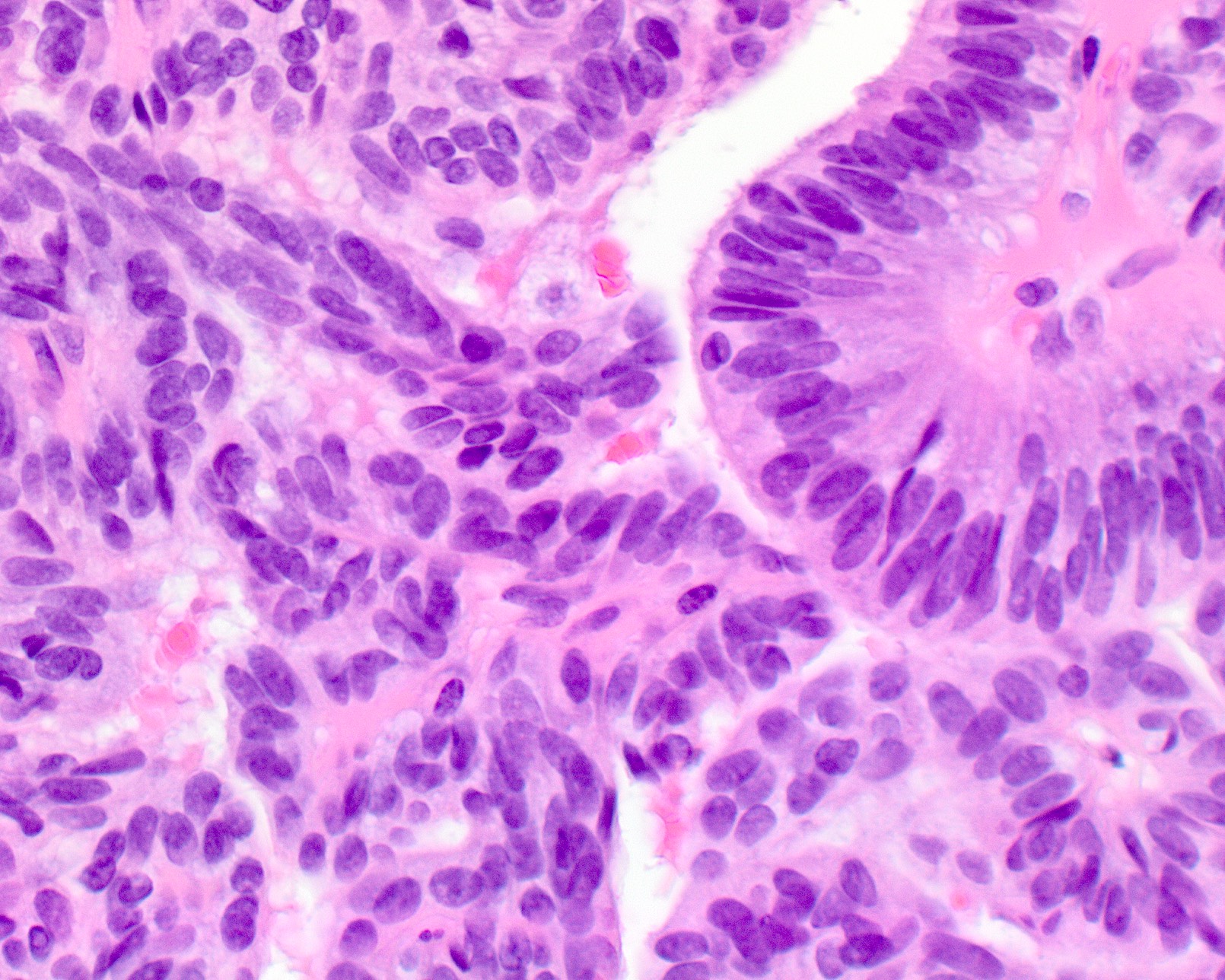
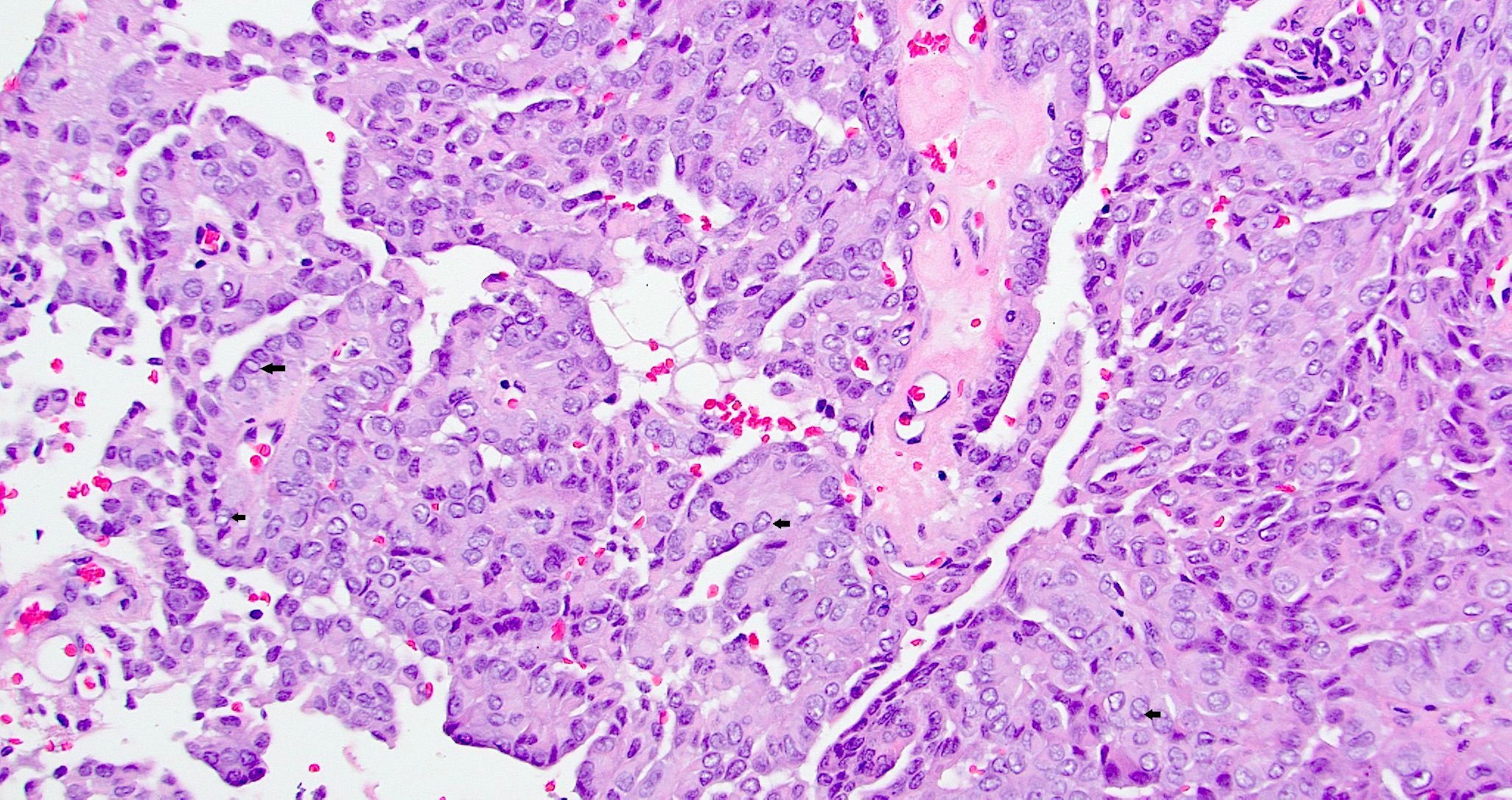
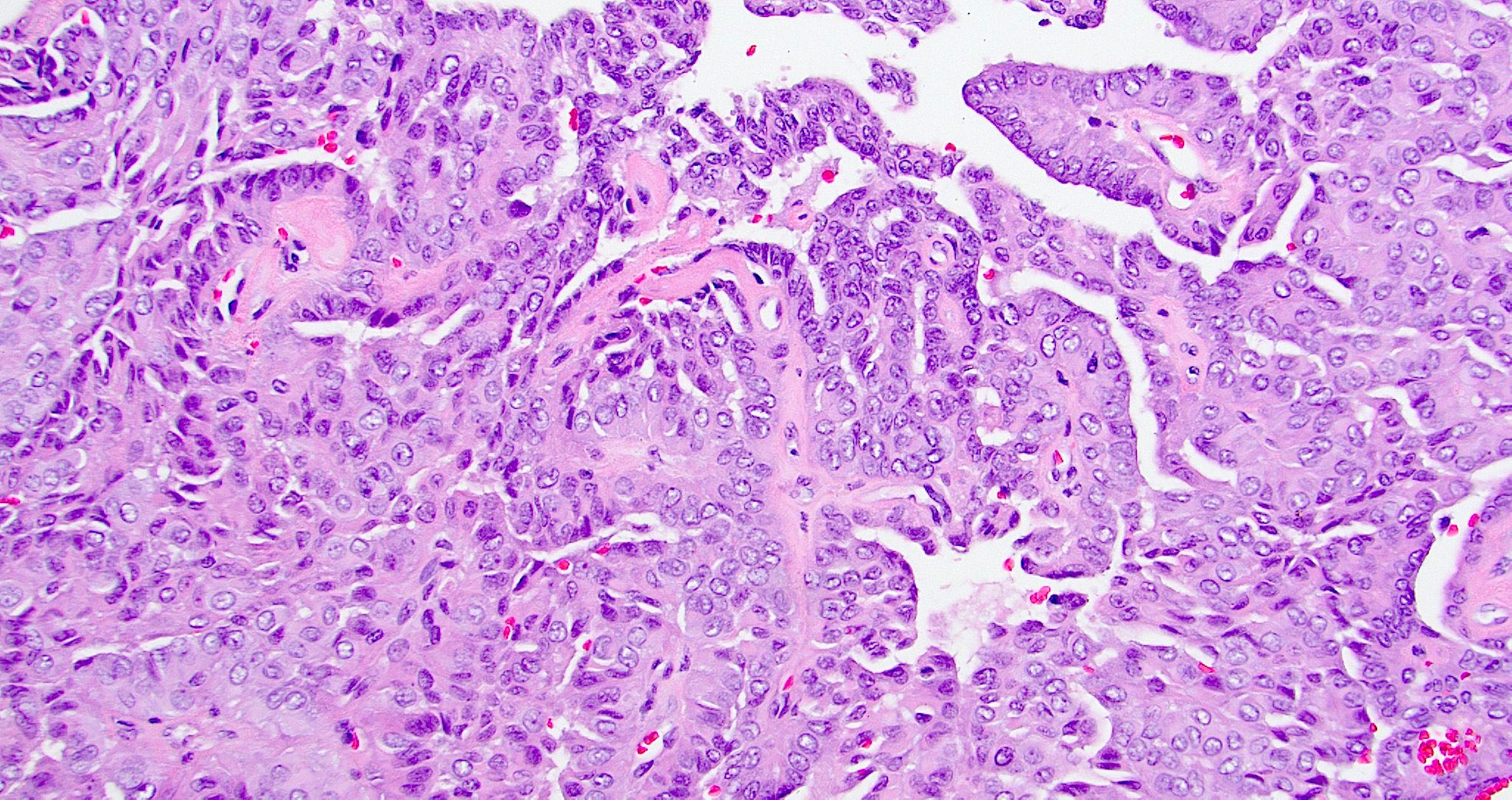
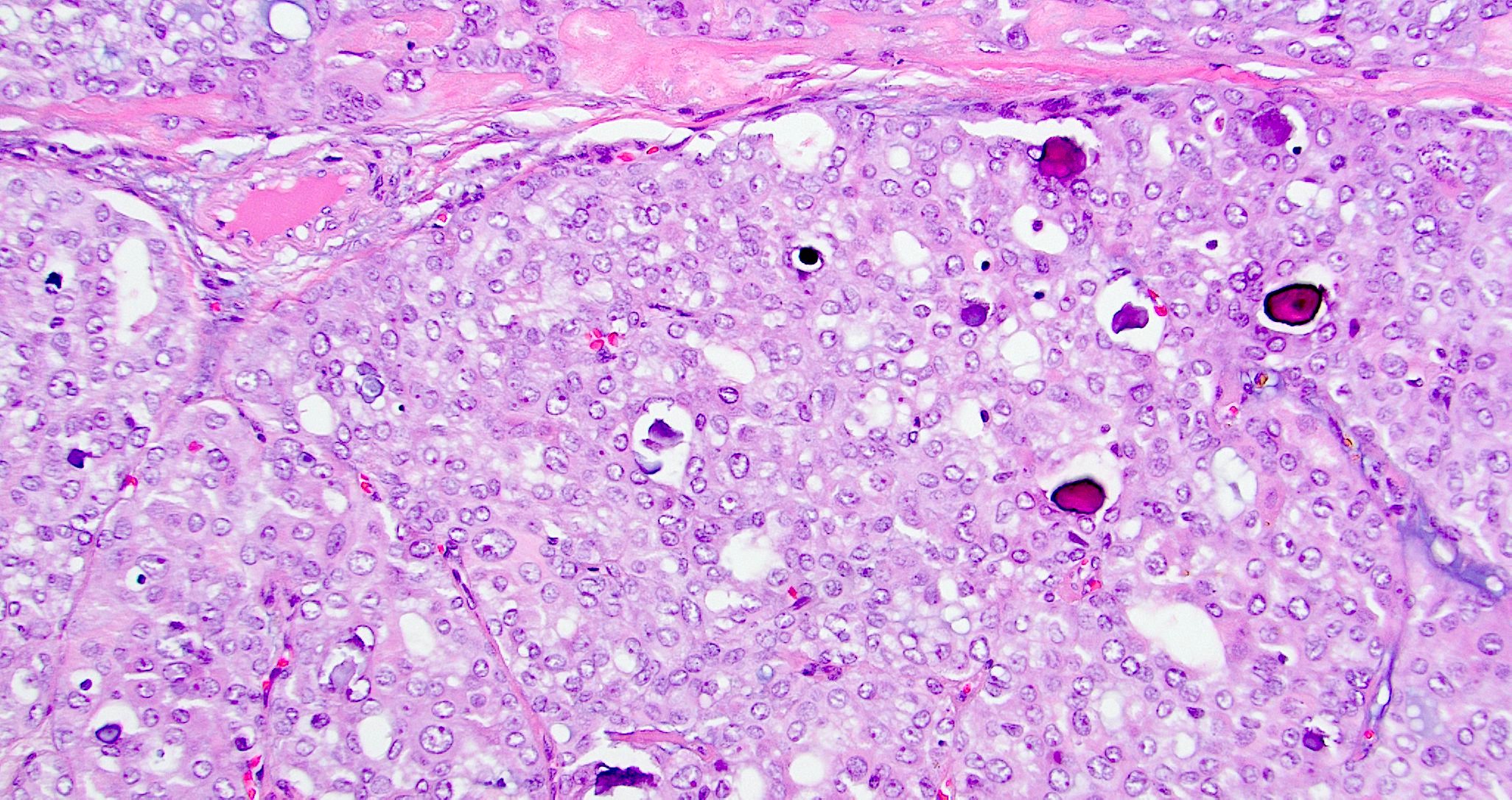
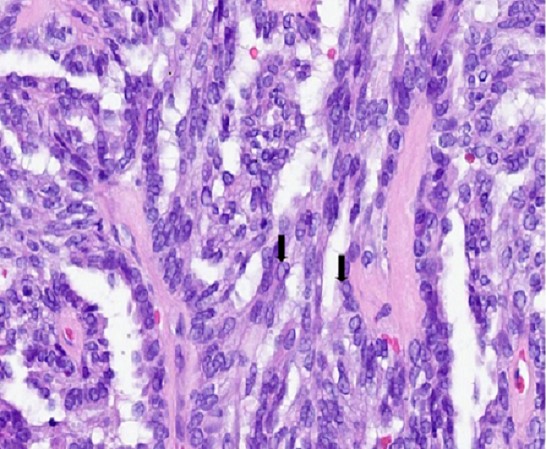
Microscopic (histologic) description
- Invasive tumor involving surface epithelium, at times merging with adjacent nonneoplastic epithelium
- Papillary and glandular growth patterns (Cancer Manag Res 2021;13:1271)
- Papillary structures are complex with arborization and hyalinized fibrovascular cores
- Glandular growth pattern has cribriform or back to back glands
- Lined by single layer of cuboidal to columnar cells with moderate amount of eosinophilic cytoplasm and round to oval nuclei
- Nuclei are vesicular or optically clear showing grooves or membrane irregularities mimicking papillary thyroid carcinoma
- Mild to moderate nuclear pleomorphism, no / rare nucleoli
- Mitotic figures are inconspicuous
- Psammoma bodies may be present in 33% of cases
- Necrosis is rare and usually absent
- No angiolymphatic invasion or perineural invasion
Microscopic (histologic) images
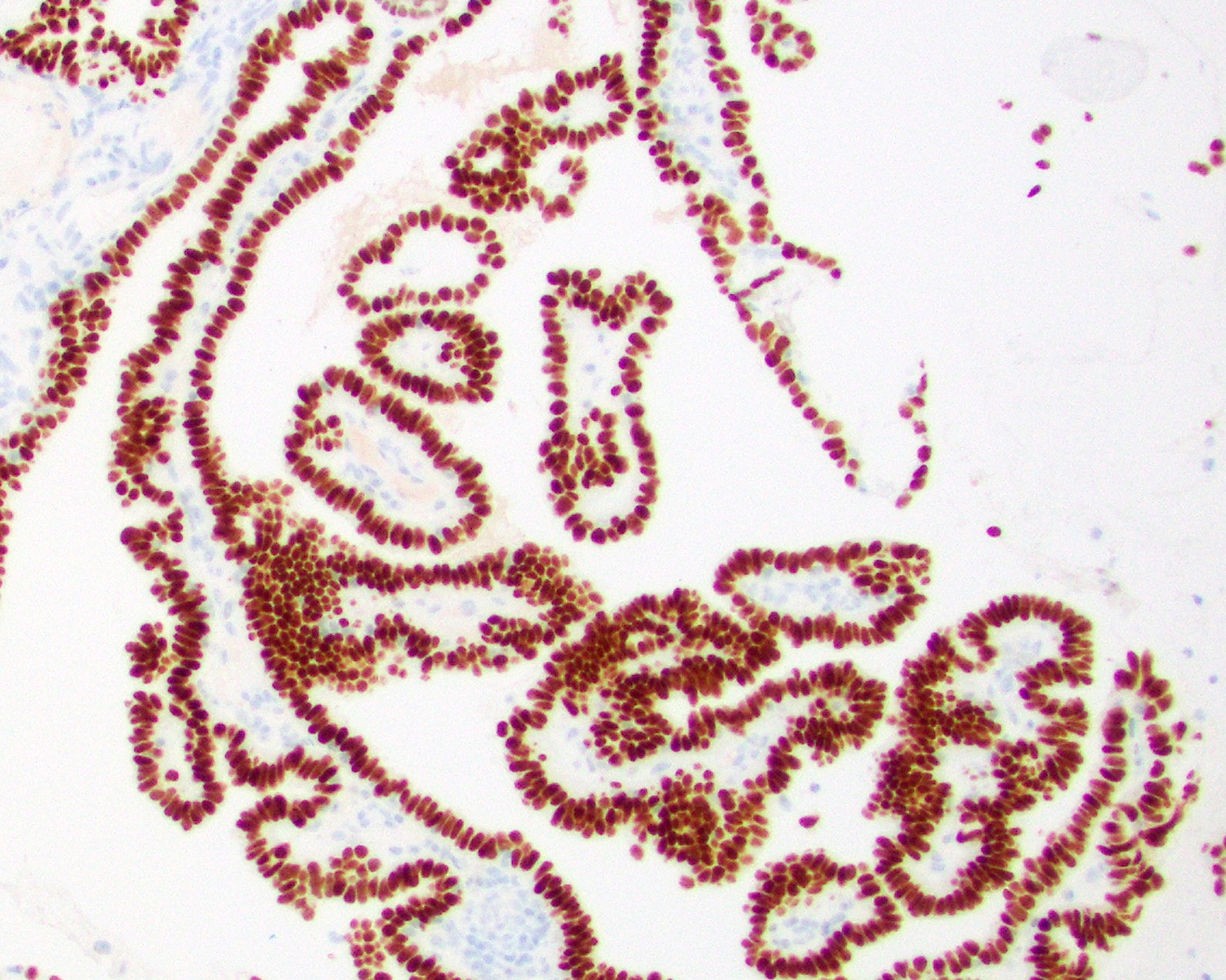
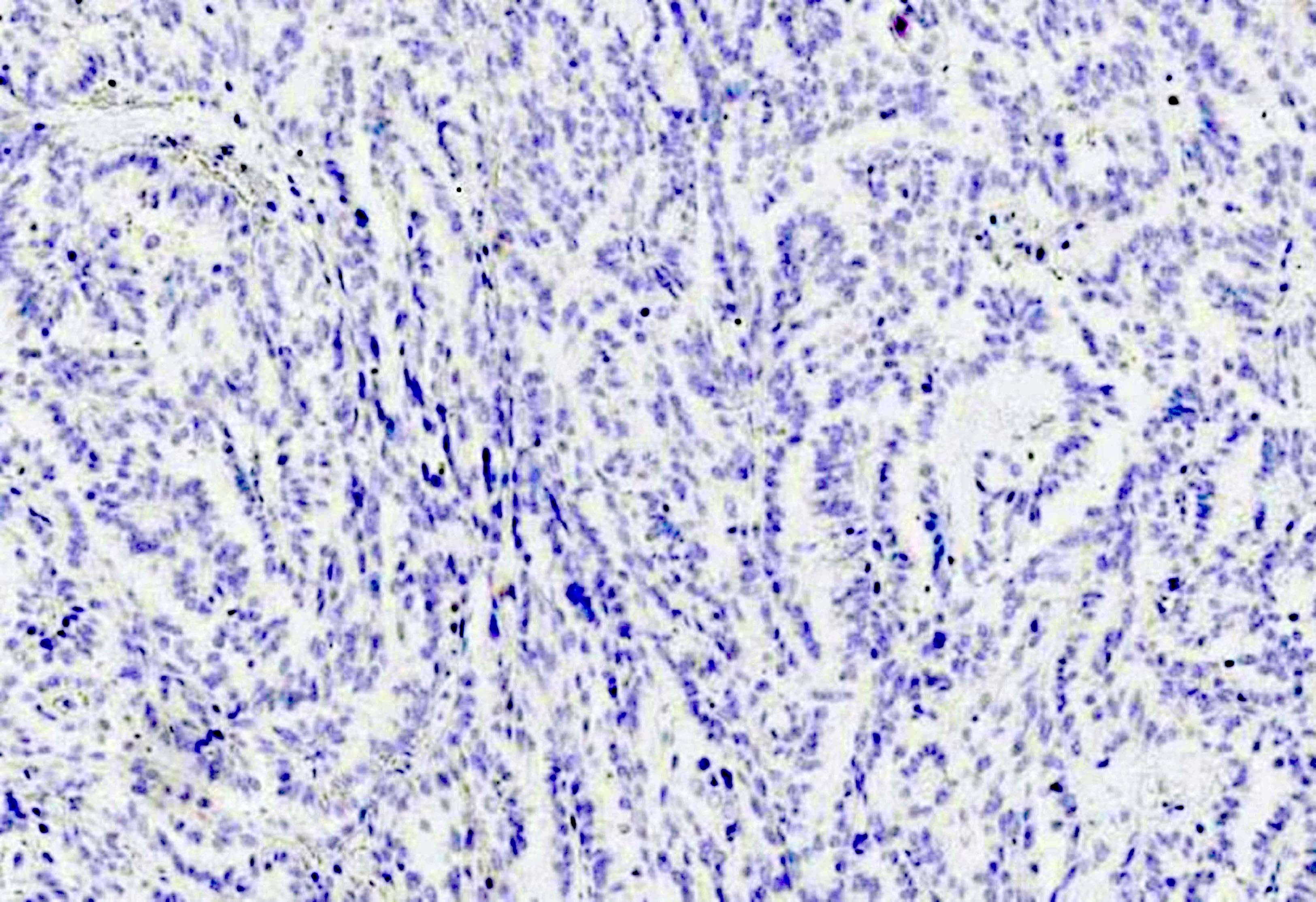
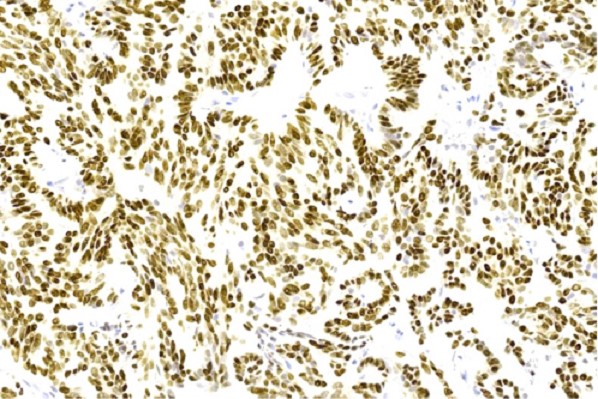
Contributed by Diana Bell, M.D. and Lester Thompson, M.D.
Positive stains
- PAS (intracytoplasmic, diastase resistant granules), mucin stains like mucicarmine (intracellular or luminal)
- Pancytokeratin (diffuse), CK7 (diffuse), EMA (diffuse), CK5/6, CEA (focal), CK19 (subset of cases), S100 (focally in few cases) (Cancer Manag Res 2021;13:1271)
- TTF1 (J Formos Med Assoc 2015;114:473)
- Low proliferation indices (Ki67 < 5%)
Negative stains
- PAX8, thyroglobulin, CK20, CDX2, villin, GFAP, BCL2 (Hum Pathol 2023;134:66)
- EBV encoded small nuclear RNA in situ hybridization
Molecular / cytogenetics description
- No defined genetic alterations to date
- No BRAF or NRAS mutations
- One case was reported in a patient with Turner syndrome (Med J Malaysia 1998;53:104)
- ROS1 gene rearrangements with presence of ROS1::GOPC fusion has been described in a patient (Medicine (Baltimore) 2021;100:e24377)
Sample pathology report
- Roof of nasopharynx, endoscopic resection:
- Nasopharyngeal papillary adenocarcinoma (1 cm) (see comment)
- Margins negative
- Comment: Microscopic examination reveals complex, interwoven papillary architecture along with crowded back to back glands. The tumor nuclei are oval and exhibit mild degree of pleomorphism with presence of optically clear chromatin. Lymphovascular or perineural invasion are not identified. On immunohistochemistry, the tumor cells are immunopositive for pan-CK, CK7 and TTF1, while they are negative for PAX8 and thyroglobulin. The findings are consistent with nasopharyngeal papillary adenocarcinoma.
Differential diagnosis
- Metastatic papillary thyroid carcinoma:
- No surface epithelial dysplasia
- PAX8+ and thyroglobulin+
- TTF1+ in both tumor types (Head Neck Pathol 2019;13:661)
- Sinonasal intestinal type adenocarcinoma, papillary variant:
- Nasal cavity and paranasal sinuses
- Usually wood dust exposure
- More papillary and less glandular
- Tall columnar and goblet cells
- Lack of nuclear features of papillary thyroid carcinoma
- Dirty background with hemorrhage and inflammation
- Mitotic activity
- Usually positive for CK20, CDX2, villin and MUC2 (Ann Diagn Pathol 2006;10:215)
- Polymorphous adenocarcinoma of salivary gland origin:
- Papilloma of surface epithelial or minor salivary gland origin:
- Lacks infiltrative growth pattern
Practice question #1
A 45 year old woman presented with a nasopharyngeal mass. Based on the H&E and immunohistochemistry (TTF1) images above, what is the diagnosis?
- Low grade nasopharyngeal papillary adenocarcinoma
- Metastasis from papillary thyroid carcinoma
- Polymorphous adenocarcinoma
- Sinonasal intestinal type adenocarcinoma, papillary variant
Practice answer #1
A. Low grade nasopharyngeal papillary adenocarcinoma. The pictures show a tumor arranged as glands and interwoven papillae with hyalinized cores. The tumor nuclei show pseudoinclusions, nuclear clearing, longitudinal grooves and overlapping. No mitotic figures are identified. Diffuse nuclear immunopositivity for TTF1 is seen. These features are consistent with a low grade nasopharyngeal papillary adenocarcinoma. Though metastasis from papillary thyroid carcinoma is also TTF1 positive and shows similar nuclear features, answer B is incorrect because it does not fit the given clinical history of presence of only a nasopharyngeal mass. However, in case of diagnostic dilemma, other immunohistochemical markers like PAX8 and thyroglobulin can be used, which are immunopositive in papillary thyroid carcinoma but not in low grade nasopharyngeal papillary adenocarcinoma. Answer C is incorrect because polymorphous adenocarcinoma usually shows highly variable architectural patterns in different proportions including solid, trabecular, tubular, reticular, cribiform and papillary arrangements. The tumor cells usually have monotonous pale nuclei and are immunonegative for TTF1. Answer D is incorrect because sinonasal intestinal type adenocarcinoma, papillary variant shows tumor cells arranged in papillary architecture with presence of goblet cells. The tumor cells are immunopositive for CD20 and CDX2, while TTF1 is negative in this tumor.
Comment Here
Reference: Low grade nasopharyngeal papillary adenocarcinoma
Comment Here
Reference: Low grade nasopharyngeal papillary adenocarcinoma
Practice question #2
Regarding low grade nasopharyngeal papillary adenocarcinoma, which of the following statements is true?
- Complete surgical excision is usually curative
- PAX8 is immunopositive in this tumor
- This tumor has EBV association
- This tumor has a high rate of metastasis
Practice answer #2
A. Complete surgical excision is usually curative. This tumor exhibits indolent biological behavior and complete surgical excision is usually curative.
Answer C is incorrect because this tumor does not have any known etiological agent or any viral association.
Answer B is incorrect as PAX8 (which is a transcription factor involved in development of the central nervous system, eye, kidney, thyroid gland, organs derived from the mesonephric [Wolffian] duct and organs derived from the Müllerian duct) is usually immune negative in nasopharyngeal tumors.
Answer D is incorrect because this tumor usually has anexcellent prognosis with no known metastases.
Comment Here
Reference: Low grade nasopharyngeal papillary adenocarcinoma
Comment Here
Reference: Low grade nasopharyngeal papillary adenocarcinoma