Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Turashvili G. Follicle cyst. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarynontumorfollicularcysts.html. Accessed September 15th, 2025.
Definition / general
- Benign cyst measuring at least 3 cm and lined by an inner layer of granulosa cells with an outer layer of theca cells
Essential features
- Benign cyst lined by an inner layer of granulosa cells with an outer layer of theca cells
- Measures ≥ 3 cm, as opposed to cystic follicle, which measures < 3 cm
- Should be differentiated from cystic granulosa cell tumor
- May occur at any age, with a variable clinical presentation depending on age and etiology
Terminology
- Follicular cyst
ICD coding
Epidemiology
- Most common in nonpregnant women of reproductive age, especially near menarche or menopause
- May occur at any age, including neonates and children (Acta Paediatr Scand 1987;76:91, Int J Gynecol Pathol 1984;3:318)
- Affects 1 in 2,500 live female births (Obstet Gynecol Surv 1991;46:407)
- Relatively rare in postmenopausal women and may present with hyperestrogenism
- May be associated with McCune-Albright syndrome (Radiology 1988;168:817, Ann Endocrinol (Paris) 2016;77:7, Semin Pediatr Surg 2005;14:78)
Sites
- Ovary
Pathophysiology
- Physiologically:
- Ovarian follicle matures during proliferative phase of menstrual cycle, mature oocyte gets released due to luteinizing hormone (LH) surge at midcycle and follicle transforms to corpus luteum
- If no fertilization, corpus luteum atrophies and forms corpus albicans
- Follicle may become cystic via 2 mechanisms:
- Gonadotropin independent:
- McCune-Albright syndrome (N Engl J Med 1985;312:65)
- Primary hypothyroidism
- Isosexual pseudoprecocity
- Idiopathic central precocious puberty
- Gonadotropin dependent due to hypothalamic pituitary gonadal axis dysfunction:
- Central precocious puberty
- No luteinizing hormone (LH) surge
- Elevated follicle stimulating hormone (FSH)
- No ovulation
- Treatment with gonadotropin releasing hormone analogues, low dose phasic oral contraceptives and tamoxifen (Am J Obstet Gynecol 1987;156:1538, Fertil Steril 1990;53:1091, Gynecol Oncol 1999;72:202)
- Gonadotropin independent:
- Cyst usually disappears within 2 - 3 menstrual cycles but may persist
Clinical features
- Usually asymptomatic and incidental
- May form adnexal or pelvic mass
- Pelvic / abdominal pain, rarely hemoperitoneum, due to rupture or torsion (Am J Obstet Gynecol 1984;149:5)
- May be multiple or bilateral and present with symptoms related to hyperestrogenism (isosexual precocity, pseudoprecocity, menstrual disturbances including amenorrhea and postmenopausal bleeding, endometrial hyperplasia) when associated with McCune-Albright syndrome
- Rarely, central precocious puberty or isosexual precocity not related to McCune-Albright syndrome (Arch Dis Child 1999;81:53)
- Most cysts regress during the first 4 months of life but may undergo torsion, hemorrhage and rupture during the neonatal period or in utero
- May be associated with symptoms of primary hypothyroidism, including Van Wyk-Grumbach syndrome (juvenile hypothyroidism, precocious puberty with delayed bone age and ovarian cysts)
- May be associated with FSH secreting pituitary adenoma and sometimes precedes clinical presentation of adenoma (Int J Gynecol Pathol 2019;38:562)
- May be associated with ovarian remnant syndrome in 7% of cases (Acta Obstet Gynecol Scand 2012;91:965)
- May be associated with autoimmune oophoritis (Obstet Gynecol 1989;74:492)
Diagnosis
- Histologic examination of tissue
Radiology description
- Ultrasound examination (J Ultrasound Med 1988;7:597):
- Thin walled unilocular cyst measuring at least 3 cm
- Posterior acoustic enhancement
- Absence of internal echoes
- No color flow, nodules or any solid components
- Fluid debris level or internal echoes, if torsion
Prognostic factors
- Usually regress spontaneously (Contraception 2002;66:153, Hum Reprod 2000;15:2567)
- May undergo torsion requiring surgery
- May recur when associated with McCune-Albright syndrome
Case reports
- 6 year old girl with precocious pseudopuberty due to ovarian follicle cyst (BMC Res Notes 2013;6:319)
- 13 year old girl with giant ovarian follicle cyst (J Clin Diagn Res 2014;8:OD03)
- 36 year old woman with pituitary adenoma and recurrent ovarian follicle cysts (BMC Res Notes 2013;6:408)
- 47 year old woman with IgG4 related disease associated with ovarian follicle cyst (Am J Case Rep 2020;21:e926803)
Treatment
- Observation
- High dose, combined estrogen progestogen preparations
- LH releasing hormone agonists
- Excision if symptomatic or persistent (Arch Pediatr 1994;1:903)
- Cyst puncture if associated with isosexual pseudoprecocity
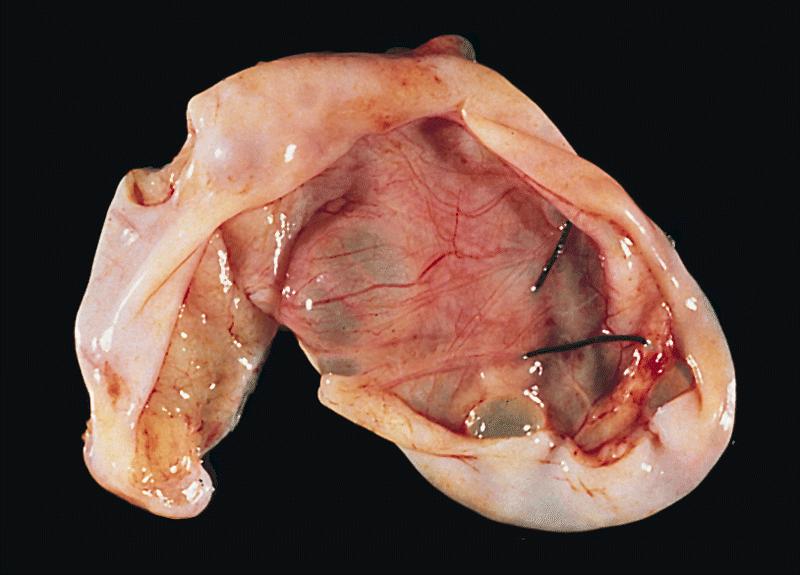
Gross description
- Usually solitary
- Ranging from at least 3 cm to up to 18.5 cm (Int J Gynecol Pathol 2021;40:359)
- Larger size during pregnancy and puerperium
- Thin walled cyst with smooth inner surface
- Usually unilocular
- No solid component
- Clear to straw colored fluid contents
- Serosanguinous or hemorrhagic fluid contents or clotted blood if torsion
- Multiple or bilateral if associated with McCune-Albright syndrome
Frozen section description
- Benign cystic structure lined by an inner layer of granulosa cells with an outer layer of theca cells
- Either cell type may be luteinized
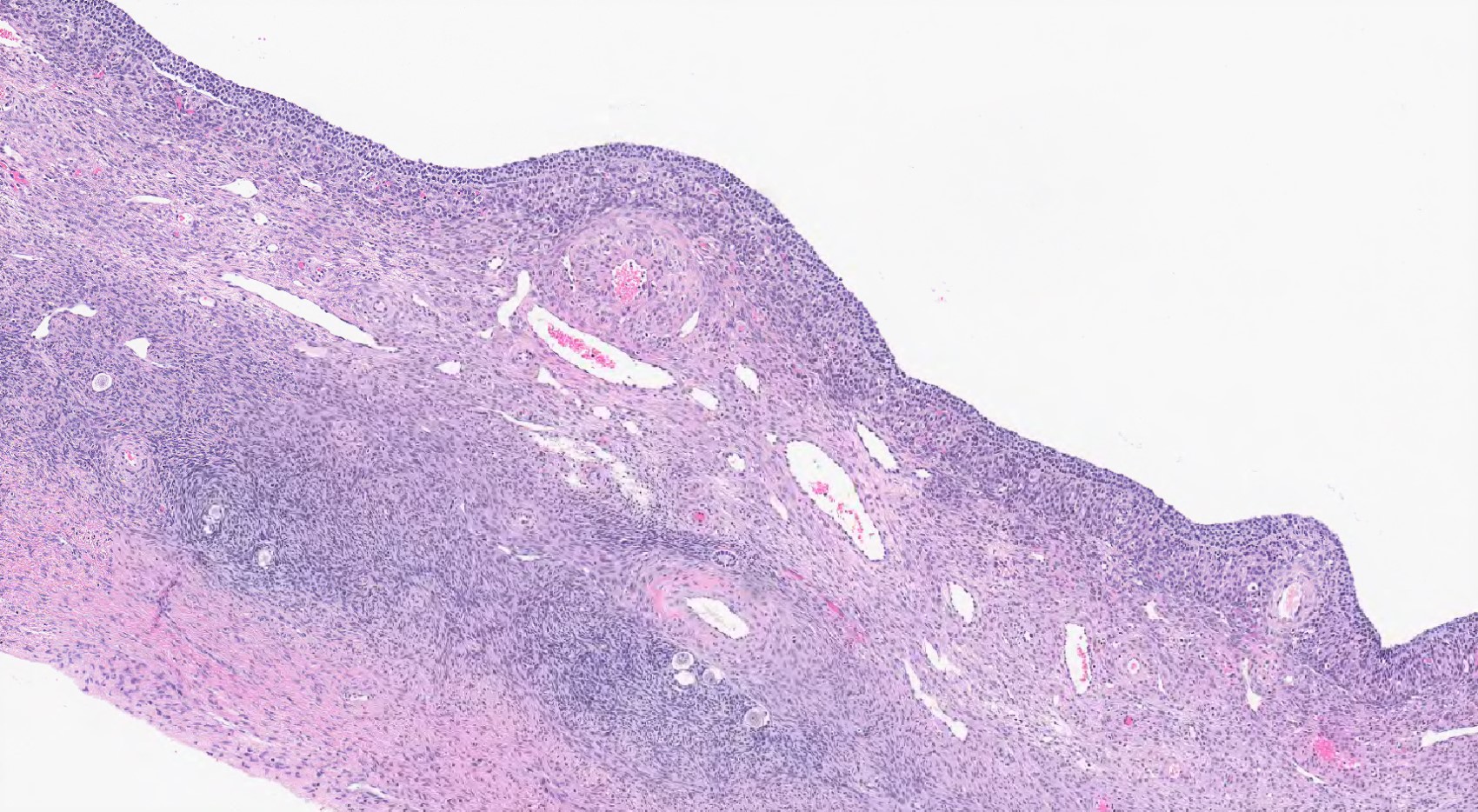
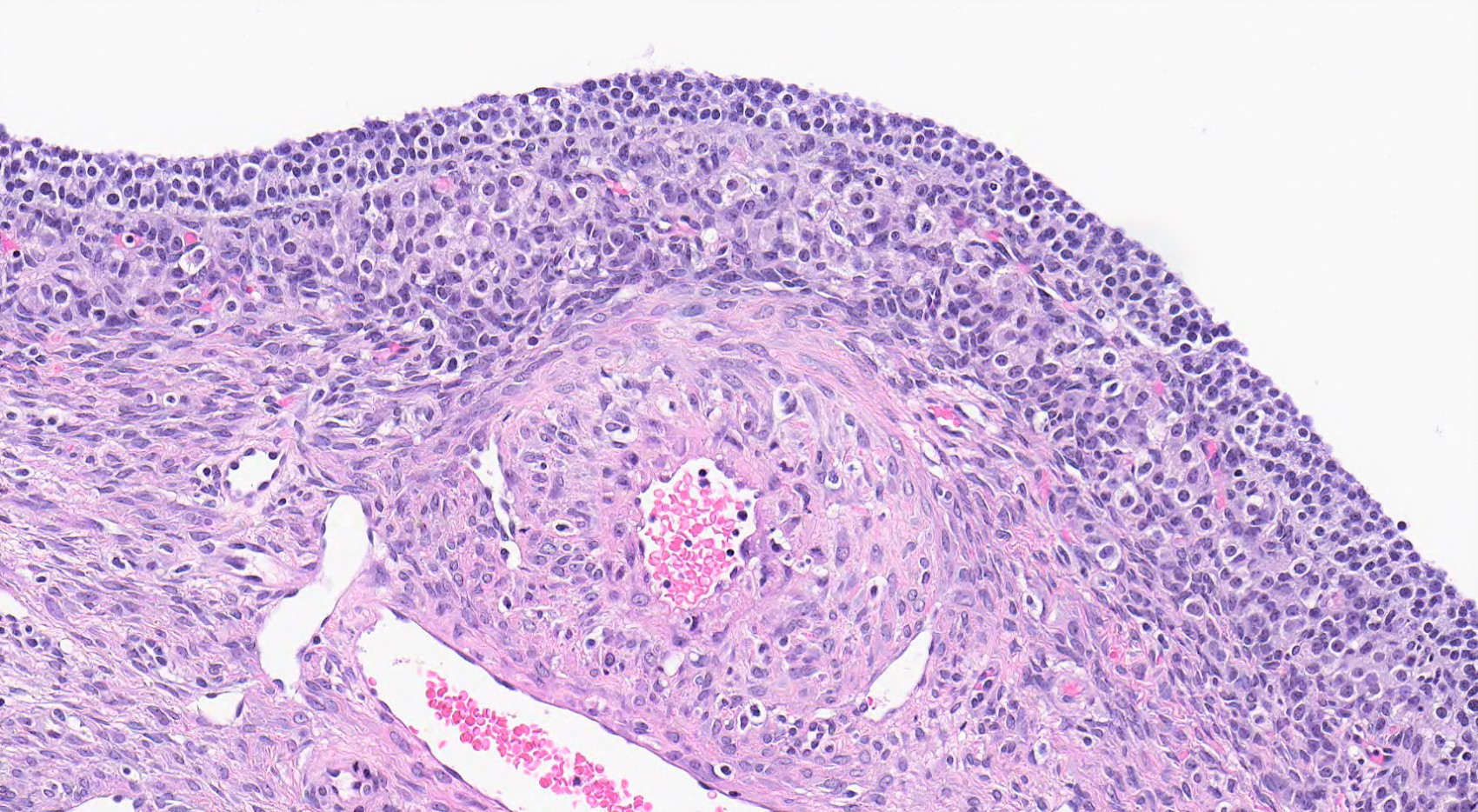
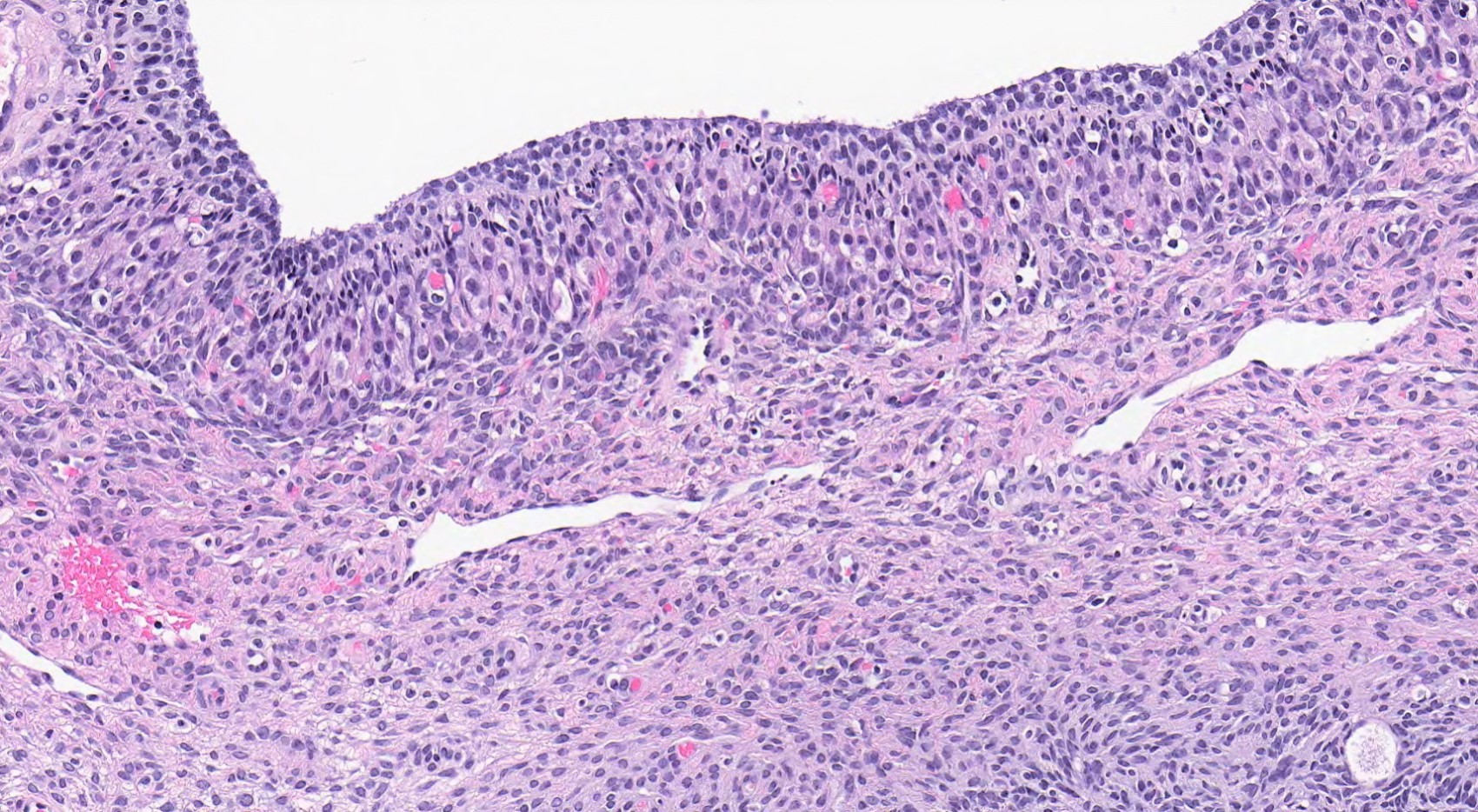
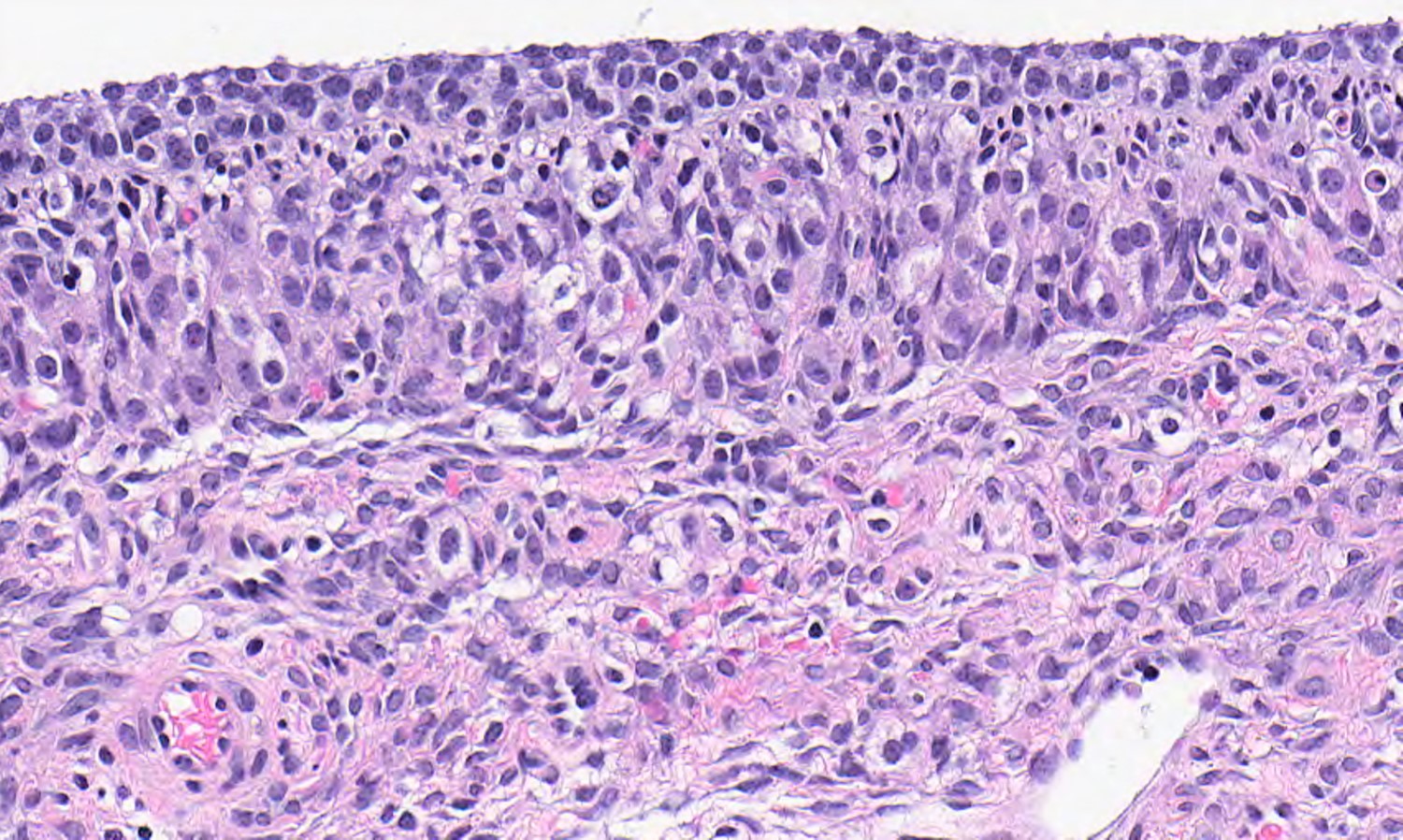
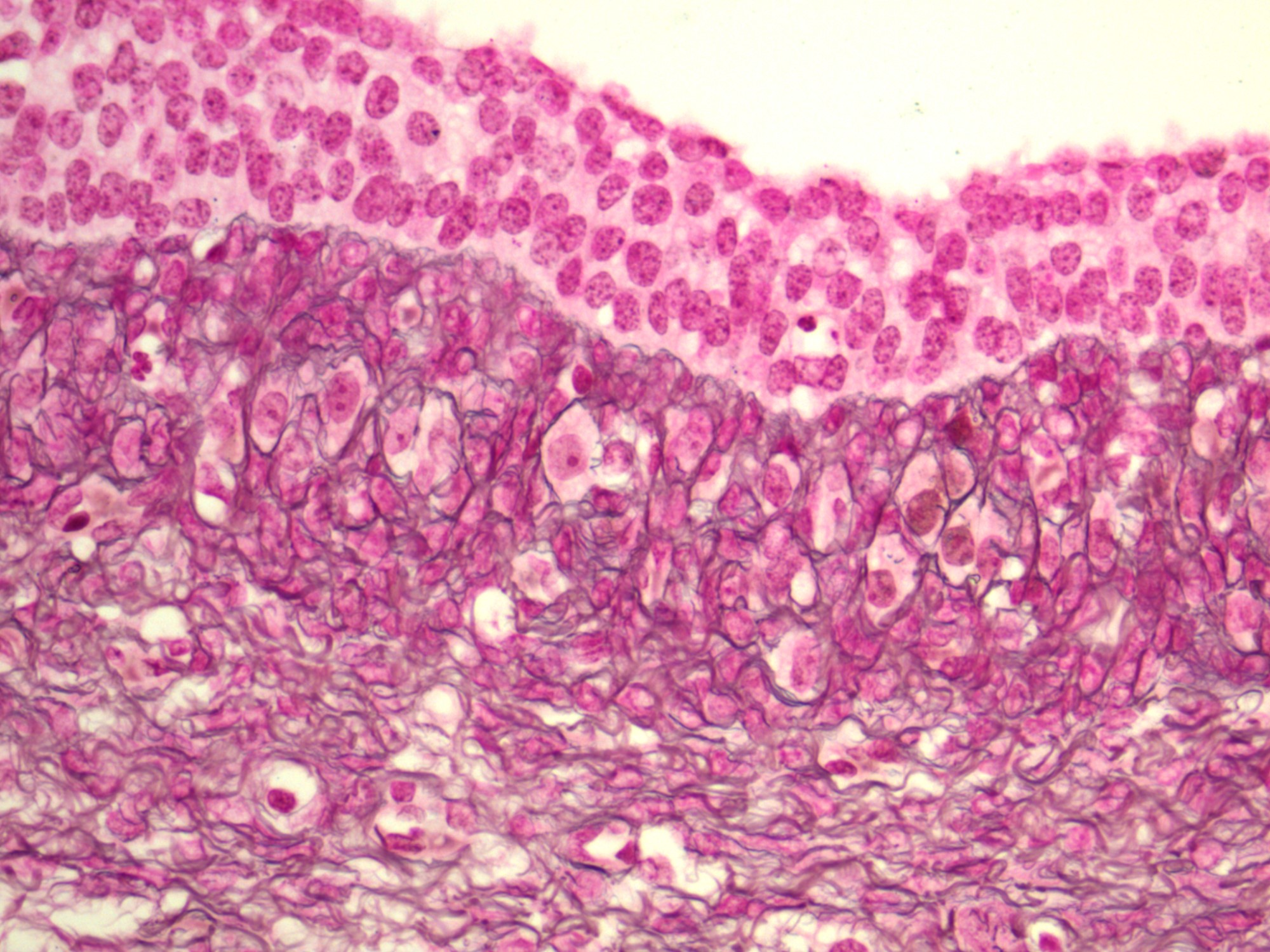
Microscopic (histologic) description
- Inner layer (1 to several) of granulosa cells with or without luteinization
- May be focally denuded
- Uniform round nuclei lacking grooves (Int J Gynecol Pathol 2021;40:359)
- Moderate amounts of eosinophilic cytoplasm
- Variable mitotic activity ranging from 1 - 36 per 10 high power fields (Int J Gynecol Pathol 2021;40:359)
- Sparse or absent reticulum on reticulin stain
- Outer layer of theca cells with or without luteinization
- Dense reticulum on reticulin stain
- Luteinized cells have eosinophilic to clear cytoplasm and round nuclei with central nucleoli
- Nonluteinized cysts are more common in patients with precocious puberty (Int J Gynecol Pathol 2021;40:359)
- Dystrophic calcifications in neonatal cysts (Int J Gynecol Pathol 2021;40:359)
- Multiple follicle cysts may be associated with eosinophil rich infiltrate (so called eosinophilic perifolliculitis) in autoimmune oophoritis (J Reprod Med 2006;51:141, Int J Gynecol Pathol 2021;40:359)
Microscopic (histologic) images
Positive stains
- Inhibin (J Clin Endocrinol Metab 1993;77:859)
- Calretinin
- SF1
- Immunohistochemistry usually not required for diagnosis
Negative stains
Sample pathology report
- Right ovary, cystectomy:
- Follicle cyst
Differential diagnosis
- Cystic adult type granulosa cell tumor:
- May be virilizing
- Usually larger than follicular cysts
- Multiple layers of granulosa cells
- Typical architectural patterns within cyst wall (Call-Exner bodies, trabecular, corded)
- With or without invagination of granulosa cells into cyst wall (Int J Gynecol Pathol 2021;40:359)
- Nuclear grooves (may be inconspicuous in luteinized forms)
- Extensive sampling may be required
- Cystic juvenile granulosa cell tumor:
- Pale to vacuolated cytoplasm
- Typical noncystic foci usually present
- Cystadenoma:
- Usually 1 layer of epithelial cells with serous, mucinous, clear cell or endometrioid morphology
- Negative for inhibin and calretinin, positive for EMA
- Endometriotic cyst:
- At least focally lined by endometrial-type epithelium
- Surrounded by endometrial stroma with or without hemorrhage or hemosiderin laden macrophages within wall
- Cystic follicle:
- Considered physiologic
- Morphology identical to follicle cyst but measuring < 3 cm
- Simple cyst:
- Denuded cyst without obvious lining or flattened lining
- No theca cells
- Large solitary luteinized follicle cyst (Am J Surg Pathol 1980;4:431):
- Occurs during pregnancy or puerperium
- Larger than follicular cyst (median size 25 cm)
- 1 to several layers of markedly luteinized granulosa cells and theca cells that are usually indistinguishable
- Variable nuclear atypia ranging from small round nuclei with single nucleolus to enlarged nuclei with focal marked pleomorphism, hyperchromasia and smudgy chromatin (degenerative)
- Absent or rare mitotic figures
- Hyperreactio luteinalis:
- Secondary to elevated human chorionic gonadotropin (hCG) levels due to gestational trophoblastic disease, fetal hydrops, multiple gestations, ovarian hyperstimulation syndrome
- Hyperandrogenism in 15%
- Bilateral, multiple, thin walled follicle cysts with distinct granulosa and theca cells
- More extensive luteinization in theca cells compared with granulosa cells
- Markedly edematous ovarian stroma and groups of luteinized stromal cells between cysts
- Corpora lutea in ovarian hyperstimulation syndrome
- Corpus luteum cyst:
- Undulating border and inner fibrous lining with a zone of small blood vessels with involution (Int J Gynecol Pathol 2021;40:359)
- Markedly luteinized polygonal shaped granulosa cells with abundant eosinophilic cytoplasm
- Cortical inclusion cyst:
- < 1 cm
- Lined by serous type ciliated epithelium or nonciliated nonmucinous flat epithelium
Additional references
Practice question #1
What entities are included in the differential diagnosis of this cystic lesion of the ovary?
- Clear cell carcinoma, cystic follicle and cystic corpus luteum
- Corpus luteum cyst, endometriotic cyst and endometrioid borderline tumor
- Cystic adult type granulosa cell tumor, cystic follicle and corpus luteum cyst
- Endometriotic cyst, corpus luteum cyst and clear cell carcinoma
- Serous borderline tumor, cystic adult type granulosa cell tumor and cystic follicle
Practice answer #1
C. Cystic adult type granulosa cell tumor, cystic follicle and corpus luteum cyst
Comment Here
Reference: Follicular cyst
Comment Here
Reference: Follicular cyst
Practice question #2
What features would favor a cystic adult type granulosa cell tumor over a follicle cyst?
- Large size (> 10 cm), 1 - 2 layers of granulosa cells with readily identifiable mitotic figures and without invagination into cyst wall or nuclear grooves
- Large size (> 10 cm), markedly luteinized granulosa cell layer with readily identifiable mitotic figures
- Large size (> 10 cm), thick granulosa cell layer with multiple architectural patterns, invagination into cyst wall and nuclear grooves
- Small size (< 10 cm), 1 - 2 layers of granulosa cells without invagination into cyst wall or nuclear grooves
- Small size (< 10 cm), 1 - 2 layers of granulosa cells without invagination into cyst wall or nuclear grooves and with external layer of luteinized theca cells
Practice answer #2
C. Large size (> 10 cm), thick granulosa cell layer with multiple architectural patterns, invagination into cyst wall and nuclear grooves
Comment Here
Reference: Follicular cyst
Comment Here
Reference: Follicular cyst