Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Gustafson DM, Chung CG. Atypical intradermal smooth muscle neoplasm. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticlms.html. Accessed September 10th, 2025.
Definition / general
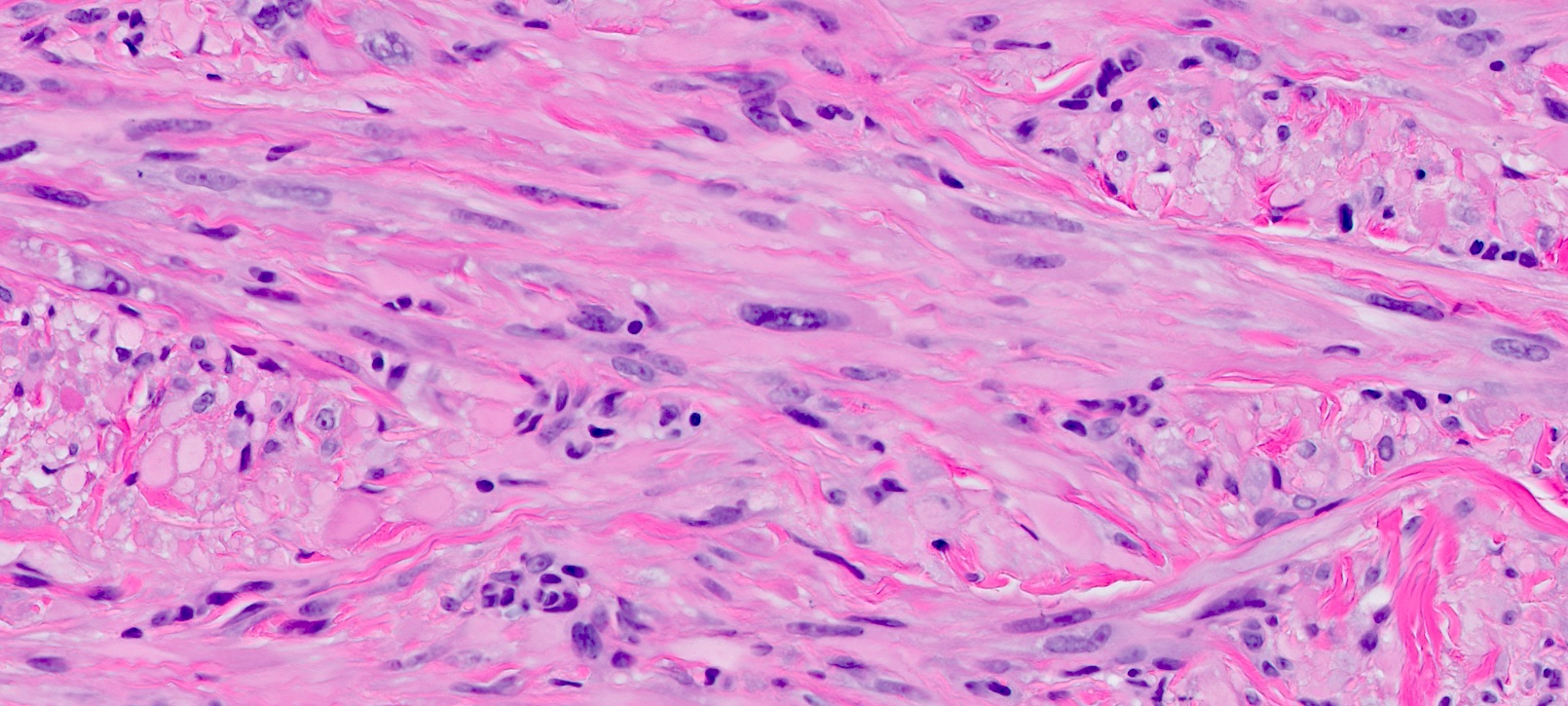
- Rare primary dermal neoplasm composed of well differentiated spindled cells resembling normal arrector pili smooth muscle
- Cells show mild to moderate atypia (nuclear enlargement, hyperchromatism and mitotic activity) (Am J Surg Pathol 2011;35:599)
Essential features
- Dermal based neoplasm with an infiltrative growth pattern
- Fascicles of relatively uniform spindled cells with smooth muscle differentiation and cytologic atypia
- Marked pleomorphism, mitoses and necrosis are rare; if present, other diagnosis should be considered (such as metastasis or extension from a deep leiomyosarcoma)
- Extremely low metastatic potential
Terminology
- Formerly referred to as cutaneous leiomyosarcoma (Appl Immunohistochem Mol Morphol 2013;21:132)
- Listed as intermediate smooth muscle neoplasms in the WHO 5th edition
- WHO lists cutaneous leiomyosarcoma as an accepted alternative term (J Pathol Transl Med 2023;57:337)
ICD coding
- ICD-O: 8897/1 - smooth muscle tumor of uncertain malignant potential
- ICD-11: 2F9C & XH1EN1 - neoplasms of unknown behavior of connective tissue or other soft tissue & smooth muscle tumor of uncertain malignant potential
Epidemiology
- Age of presentation is 22 - 90 years (Appl Immunohistochem Mol Morphol 2013;21:132, Ann Surg Oncol 2024;31:7950)
- Male predominance (Appl Immunohistochem Mol Morphol 2013;21:132, Ann Surg Oncol 2024;31:7950)
Sites
- Lower extremities (44.2%), upper extremities (28.4%), trunk (22.1%) and head and neck (5.2%) (Ann Surg Oncol 2024;31:7950)
- Head and neck and scalp were reported more frequently in other series (Appl Immunohistochem Mol Morphol 2013;21:132)
Pathophysiology
- Smooth muscle origin, arising from the erector pili muscles or dermal vasculature (Appl Immunohistochem Mol Morphol 2013;21:132)
- Less aggressive biology compared to subcutaneous and deep leiomyosarcomas (Am J Surg Pathol 2011;35:599)
Etiology
- Unclear etiology; PTEN loss of expression has been reported (Appl Immunohistochem Mol Morphol 2013;21:132)
- Rare cases associated with Li-Fraumeni syndrome (Am J Surg Pathol 2011;35:599)
Clinical features
- Nonspecific clinical presentation of a slow growing nodule / mass (Am J Surg Pathol 2011;35:599)
Diagnosis
- Essential histologic criteria (WHO 5th edition)
- Dermal based tumor with infiltrative growth
- Fascicles of relatively uniform, eosinophilic spindled cells with cigar shaped nuclei
- Immunohistochemical expression of SMA, desmin or caldesmon
- Limited involvement of subcutis
Prognostic factors
- Low risk of aggressive behavior
- Local recurrences have been reported
- Surgical margin is an important predictor of recurrence
- Subcutaneous extension (between 1 - 4 mm) does not correlate with recurrence (Appl Immunohistochem Mol Morphol 2013;21:132)
- Metastasis is extremely unlikely; other diagnoses should be pursued if a metastatic lesion is detected (Appl Immunohistochem Mol Morphol 2013;21:132)
Case reports
- 43 year old man with a family history of leiomyomatosis presented with 20 lesions on the right lower leg (J Cutan Pathol 2013;40:564)
- 58 year old man with a painless, pinkish white chest nodule (Ann Dermatol Venereol 2017;144:443)
- 65 year old woman presented with a 5 mm papular lesion on the wrist (Am J Dermatopathol 2016;38:787)
- 68 year old woman presented with a 1 cm asymptomatic nodule on the right thigh (Dermatol Online J 2009;15:6)
Treatment
- Wide local excision is generally the first line treatment (Am J Surg Pathol 2011;35:599)
- Similar outcomes reported for wide local excision versus Mohs procedure (Appl Immunohistochem Mol Morphol 2013;21:132)
Gross description
- Grossly appears as a tan-white or tan colored lesion with infiltrative margins
- Necrosis is not routinely described (Am J Surg Pathol 2011;35:599)
Frozen section description
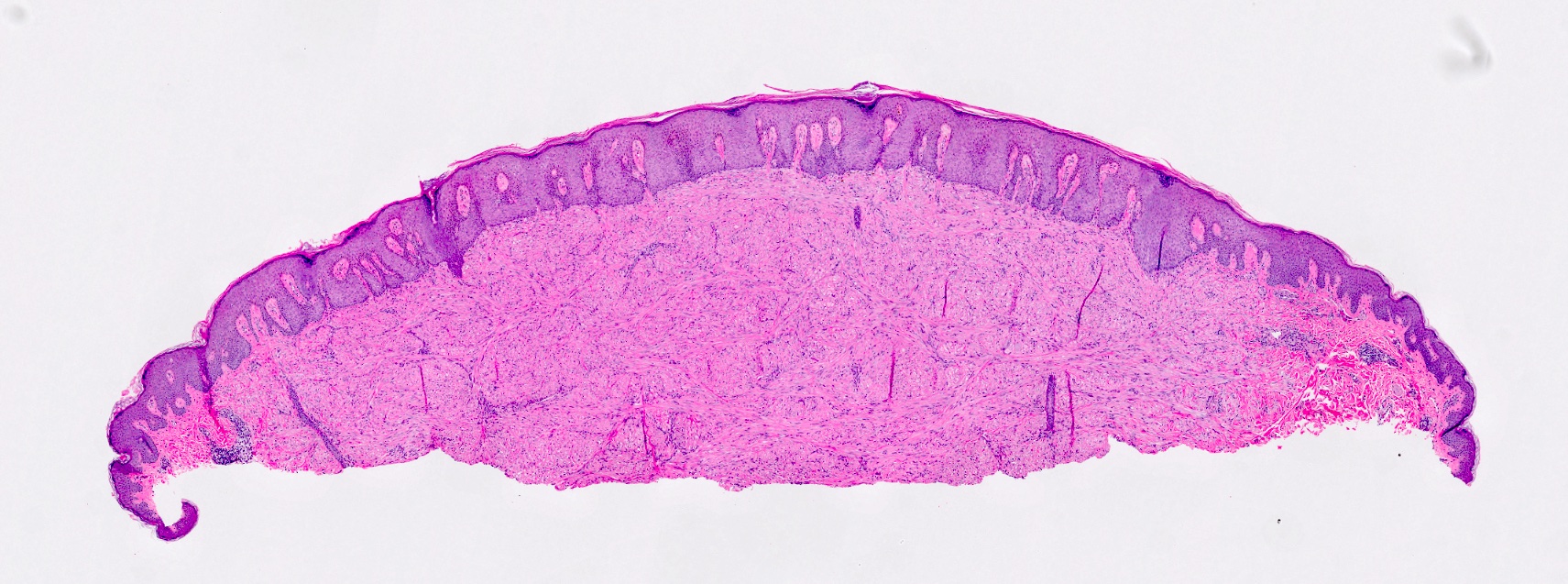
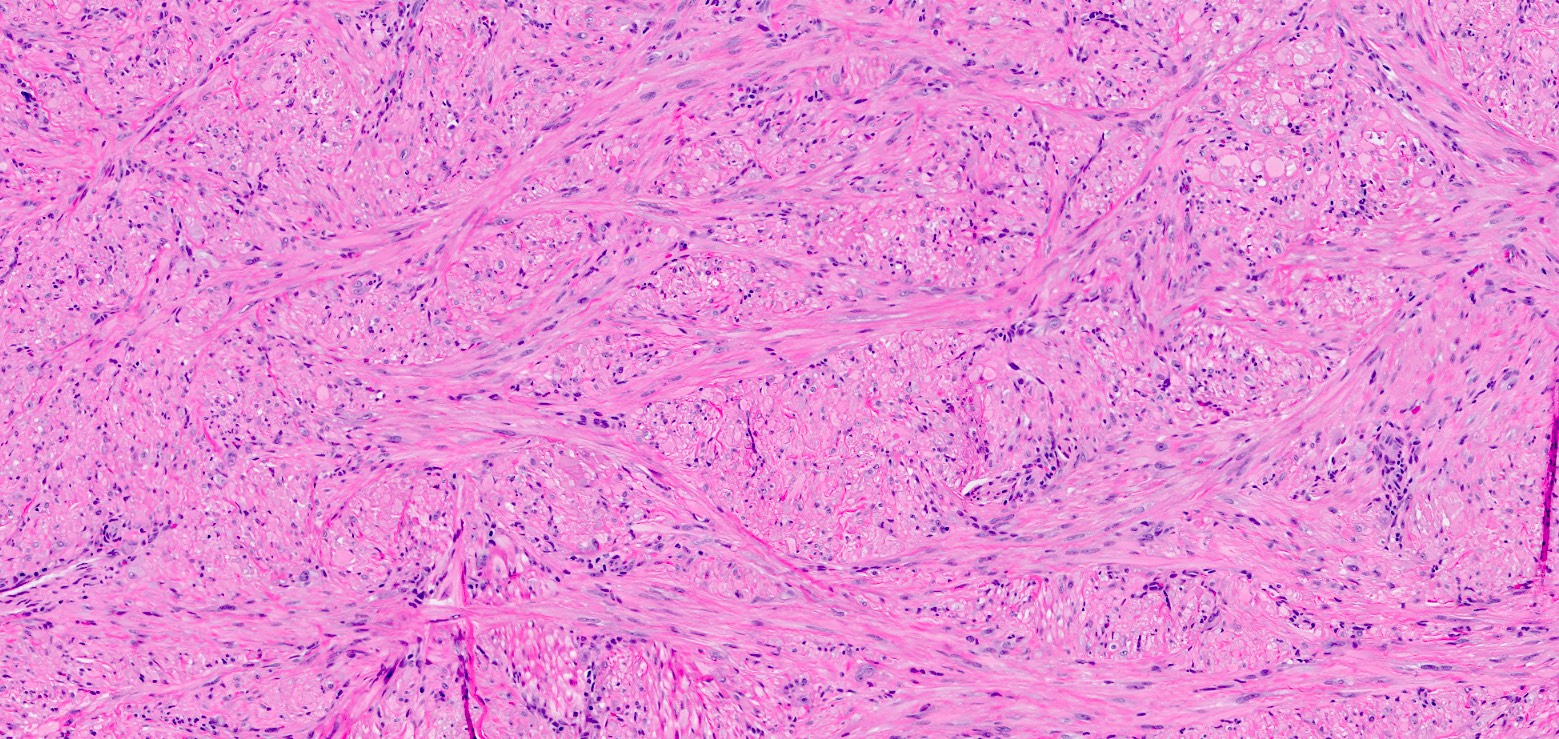
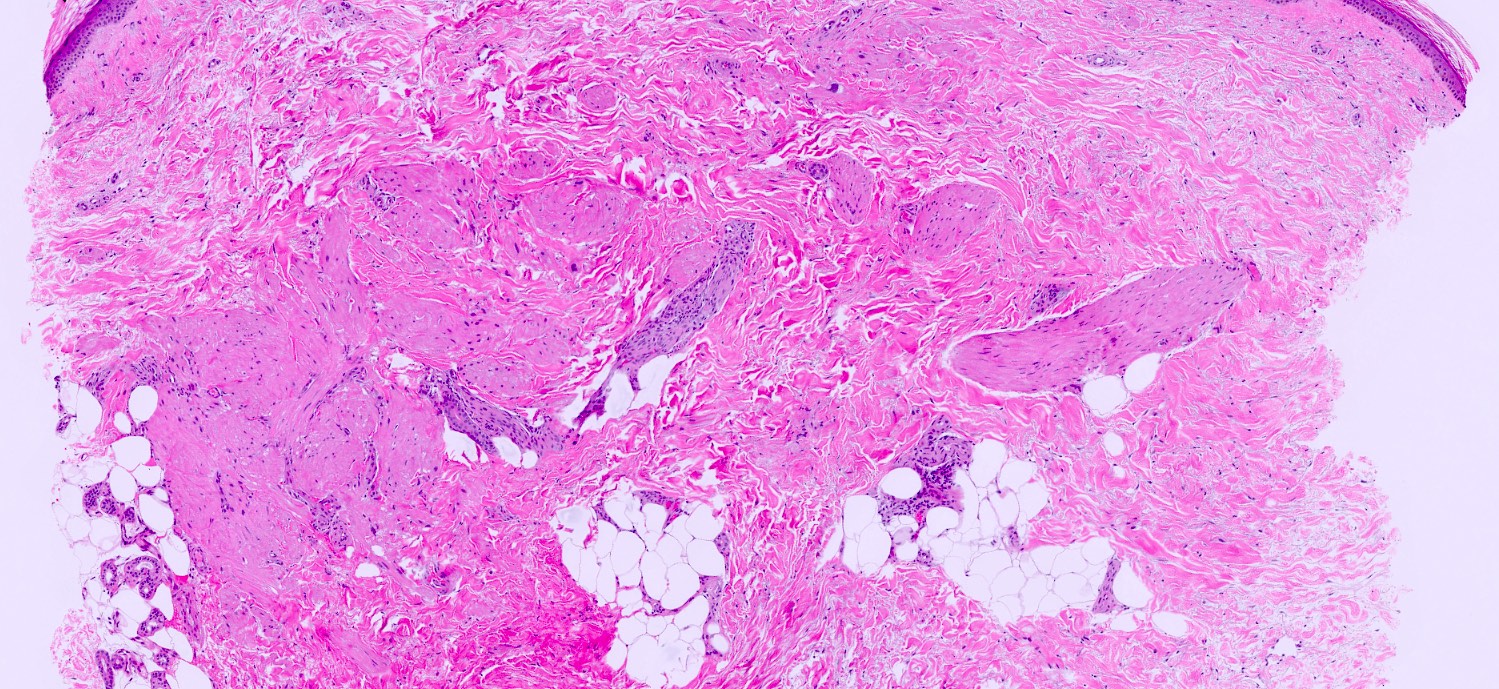
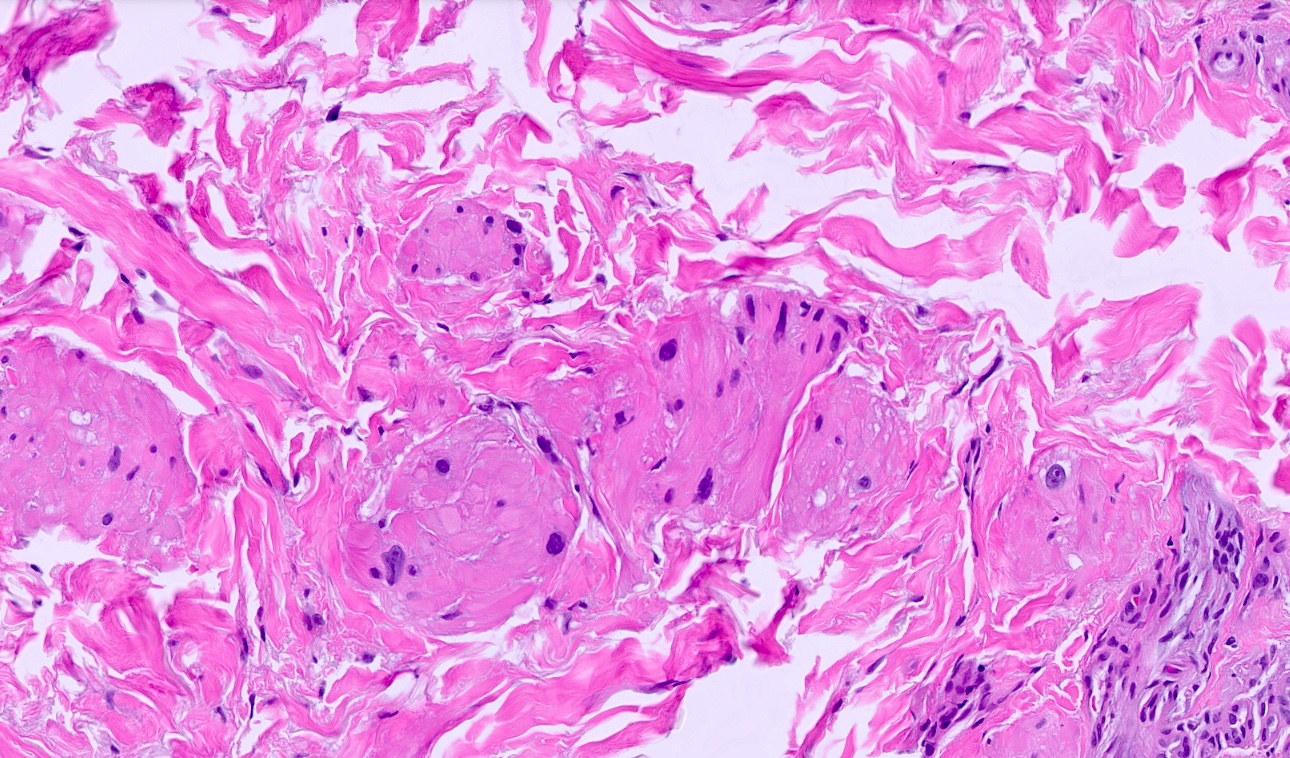
Microscopic (histologic) description
- Fascicles of relatively uniform, eosinophilic spindled cells with cigar shaped nuclei
- Low to moderate pleomorphism, increased mitoses (ranging from 1 - 28 and 13 - 20 per 10 high power fields)
- Necrosis and perineural invasion are uncommon (Appl Immunohistochem Mol Morphol 2013;21:132)
- At most focal involvement of the subcutaneous tissue
Microscopic (histologic) images
Positive stains
- SMA
- Desmin
- Caldesmon
- FXIIIa may be positive / focally positive
- Reference: Appl Immunohistochem Mol Morphol 2013;21:132
Negative stains
- Important for ruling out other cutaneous spindle cell neoplasms
- Reference: Appl Immunohistochem Mol Morphol 2013;21:132
Molecular / cytogenetics description
- PTEN loss of expression has been reported (Appl Immunohistochem Mol Morphol 2013;21:132)
- Rare cases associated with Li-Fraumeni syndrome (TP53) (Am J Surg Pathol 2011;35:599)
Sample pathology report
- Skin, anatomic site, biopsy:
- Surface of smooth muscle neoplasm (see comment)
- Comment: The surface of a smooth muscle neoplasm is seen within the dermis extending to the deep edge of the biopsy. Mild cellular atypia consisting of hyperchromasia, nuclear enlargement and focal pleomorphism is noted. The constellation of histopathologic and immunophenotypic findings are those of an atypical intradermal smooth muscle neoplasm, previously termed cutaneous leiomyosarcoma. Re-excision to ensure complete removal and to exclude deeper involvement of the soft tissue is recommended.
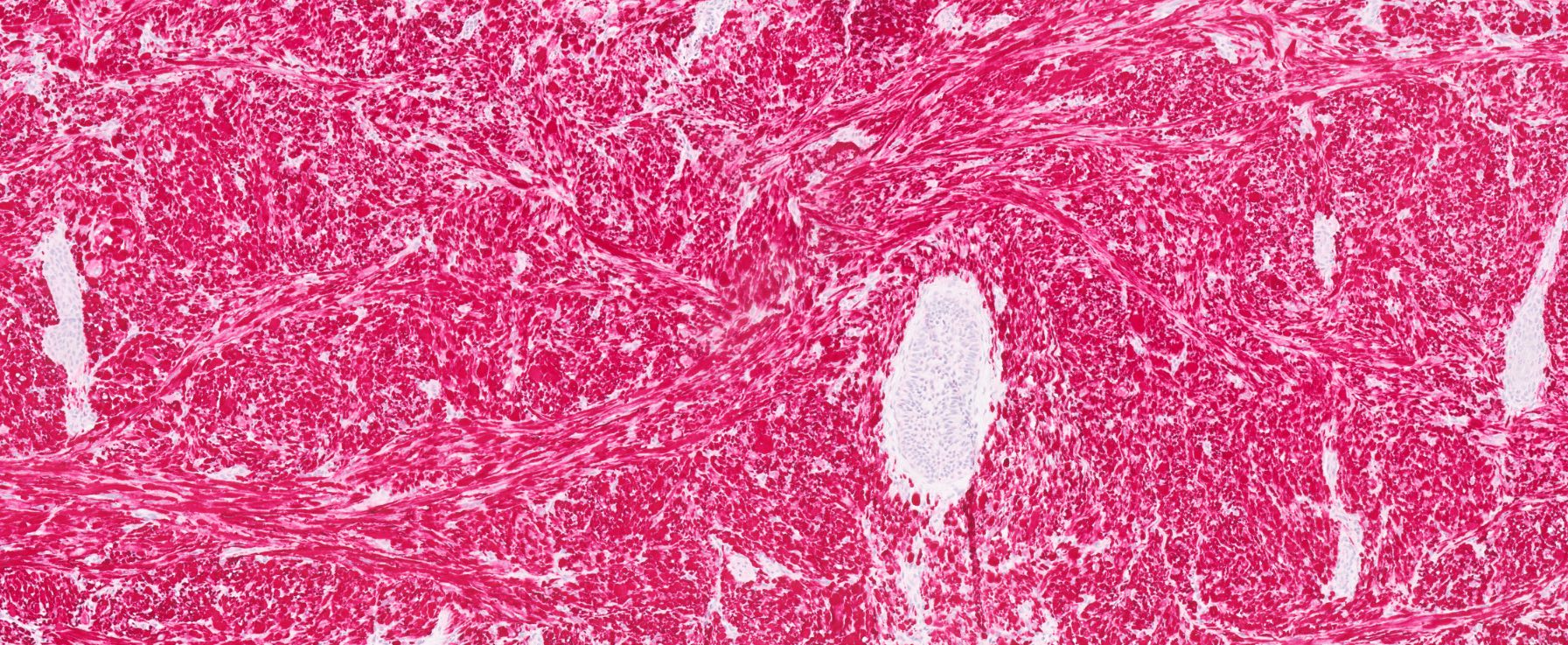
Differential diagnosis
- Deep leiomyosarcoma (An Bras Dermatol 2021;96:278):
- Architecture and soft tissue involvement is key and will require an excisional specimen
- High rates of locoregional recurrence and rates of distant metastases
- Composed of similar fascicles of eosinophilic spindled cells with blunt ended nuclei and variable pleomorphism
- Spindle cell squamous cell carcinoma (Head Neck Pathol 2020;14:109):
- Atypical fibroxanthoma / pleomorphic dermal sarcoma (Head Neck Pathol 2020;14:109):
- Atypical fibroxanthoma is usually confined to the dermis
- Pleomorphic dermal sarcoma is ill defined with diffusely infiltrative growth and invasion of subcutis and skeletal muscle
- Intersecting fascicles of pleomorphic epithelioid and spindle cells
- May have multinucleated tumor giant cells
- Abundant mitoses
- Epidermis is usually ulcerated and there is a background of solar elastosis in the dermis
- Nonspecific CD10 positive staining
- Desmoplastic malignant melanoma (Head Neck Pathol 2023;17:143):
- Scar-like proliferation with fibrosis and scattered spindled cells in the dermis
- May have overlying melanoma in situ
- Atrophic epidermis and solar elastosis in the background
- Lymphocytic infiltrates aggregate at the periphery of the lesion
- Positive for S100, SOX10; usually MelanA / HMB45 negative (in the desmoplastic component)
- Cellular neurofibroma (Acta Neuropathol 2012;123:295):
- Dermatofibroma / cellular dermatofibroma (Head Neck Pathol 2023;17:143):
- Bland spindled cells with collagen trapping
- Follicular induction in overlying epidermis (pigmented, hyperplastic epidermis)
- Positive for FXIIIa
- Leiomyoma:
Additional references
Practice question #1
The image above is seen on a shave biopsy of a 1 cm nodule on the arm of a 50 year old man. A residual histologically identical lesion was seen on the excision specimen with focal involvement of the subcutis. The H&E findings are seen throughout the entirety of the lesion. Immunohistochemical stains for SMA and desmin are strongly positive, while all other markers are negative, including CD10. What is the best diagnosis?
- Atypical fibroxanthoma
- Atypical intradermal smooth muscle neoplasm
- Deep leiomyosarcoma
- Leiomyoma
Practice answer #1
B. Atypical intradermal smooth muscle neoplasm. The biopsy shows a spindle cell proliferation with atypia. The subsequent excision had the same morphology with evidence of smooth muscle differentiation by IHC stains. Focal involvement of the subcutis does not rule out atypical intradermal smooth muscle neoplasm. Answer A is incorrect because atypical fibroxanthoma typically has a greater degree of pleomorphism with abundant mitoses. There is little solar elastosis in the background and CD10 (nonspecific) was negative. Answer D is incorrect because leiomyoma should not have this degree of cytologic atypia throughout the entirety of the lesion. Answer C is incorrect because the lesion is nearly entirely confined to the dermis.
Comment Here
Reference: Atypical intradermal smooth muscle neoplasm
Comment Here
Reference: Atypical intradermal smooth muscle neoplasm
Practice question #2
A 65 year old man presents with shortness of breath and multiple lung nodules on imaging. Core needle biopsies consist of pleomorphic spindle cell neoplasm composed of intersecting fascicles of eosinophilic cells with abundant mitoses and tumoral necrosis. Immunohistochemical stains are only positive for SMA and desmin. He has a history of excision of a reported atypical intradermal smooth muscle neoplasm with positive deep margins involving the subcutis. What is the most likely diagnosis?
- Atypical intradermal smooth muscle neoplasm
- Benign metastasizing leiomyoma
- Metastatic leiomyosarcoma
- Metastatic pleomorphic dermal sarcoma
Practice answer #2
C. Metastatic leiomyosarcoma. The key point is recognizing that atypical smooth muscle neoplasms are extremely unlikely to metastasize. A revision of the pre-existing diagnosis should be considered. Answer A is incorrect because atypical intradermal smooth muscle neoplasms have an extremely low (essentially nonexistent) risk of metastasis. Answer B is incorrect because leiomyoma should not have significant pleomorphism with associated mitoses or necrosis. Answer D is incorrect because although this is an important differential to rule out given the history of the previous excision, pleomorphic dermal sarcoma usually has nonspecific staining with CD10 or CD68.
Comment Here
Reference: Atypical intradermal smooth muscle neoplasm
Comment Here
Reference: Atypical intradermal smooth muscle neoplasm