Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Perry AM. Marginal zone-nodal. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanodalmzl.html. Accessed September 16th, 2025.
Definition / general
- Primary nodal mature B cell lymphoma derived from postgerminal center B cell
- Morphological and immunophenotypical overlap with extranodal marginal zone lymphoma (EMZL) of mucosa associated lymphoid tissue (MALT) and splenic marginal zone lymphoma (SMZL)
Essential features
- Relatively rare, indolent low grade B cell lymphoma derived from postgerminal center B cell
- Patients present with localized or generalized peripheral lymphadenopathy
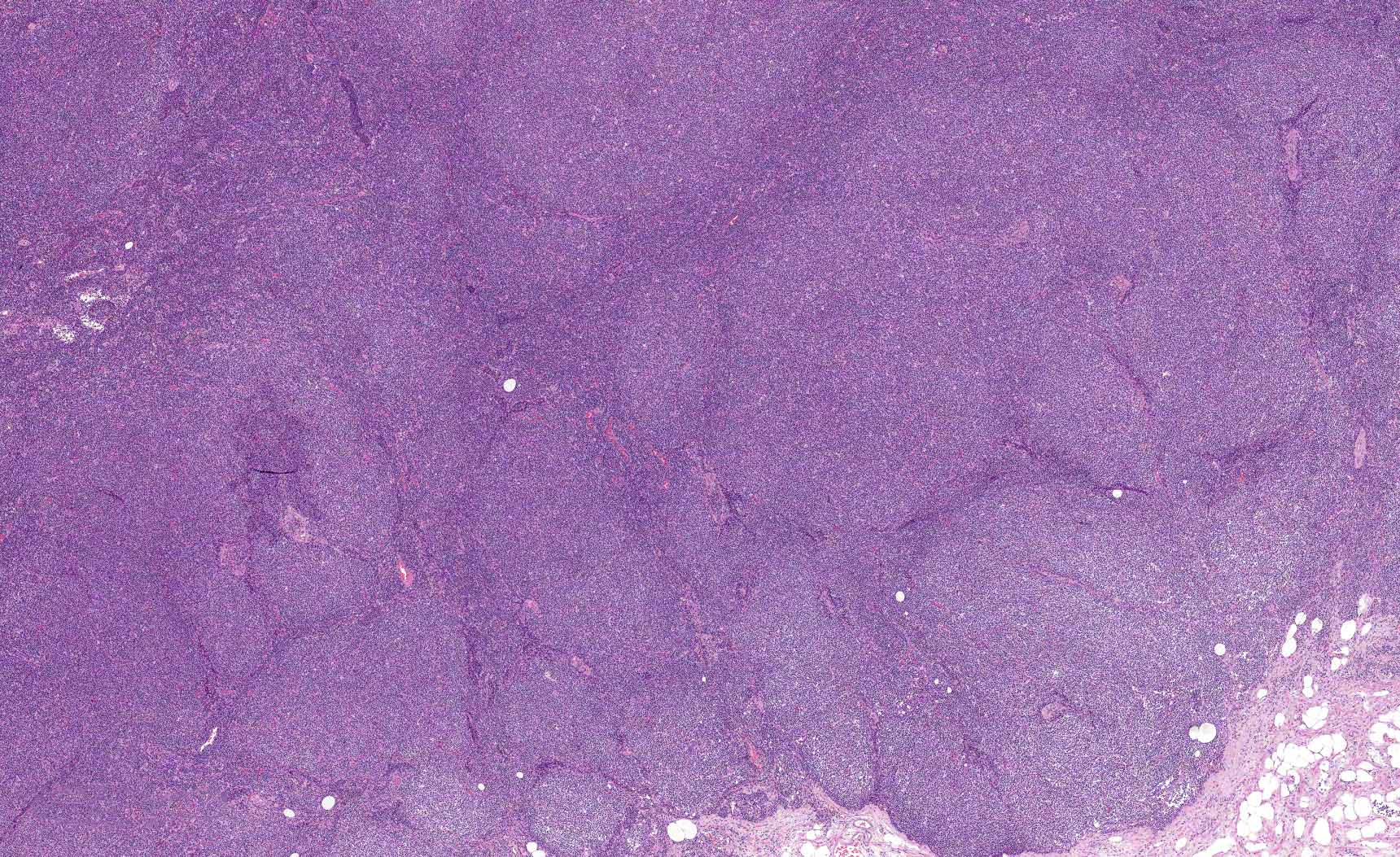
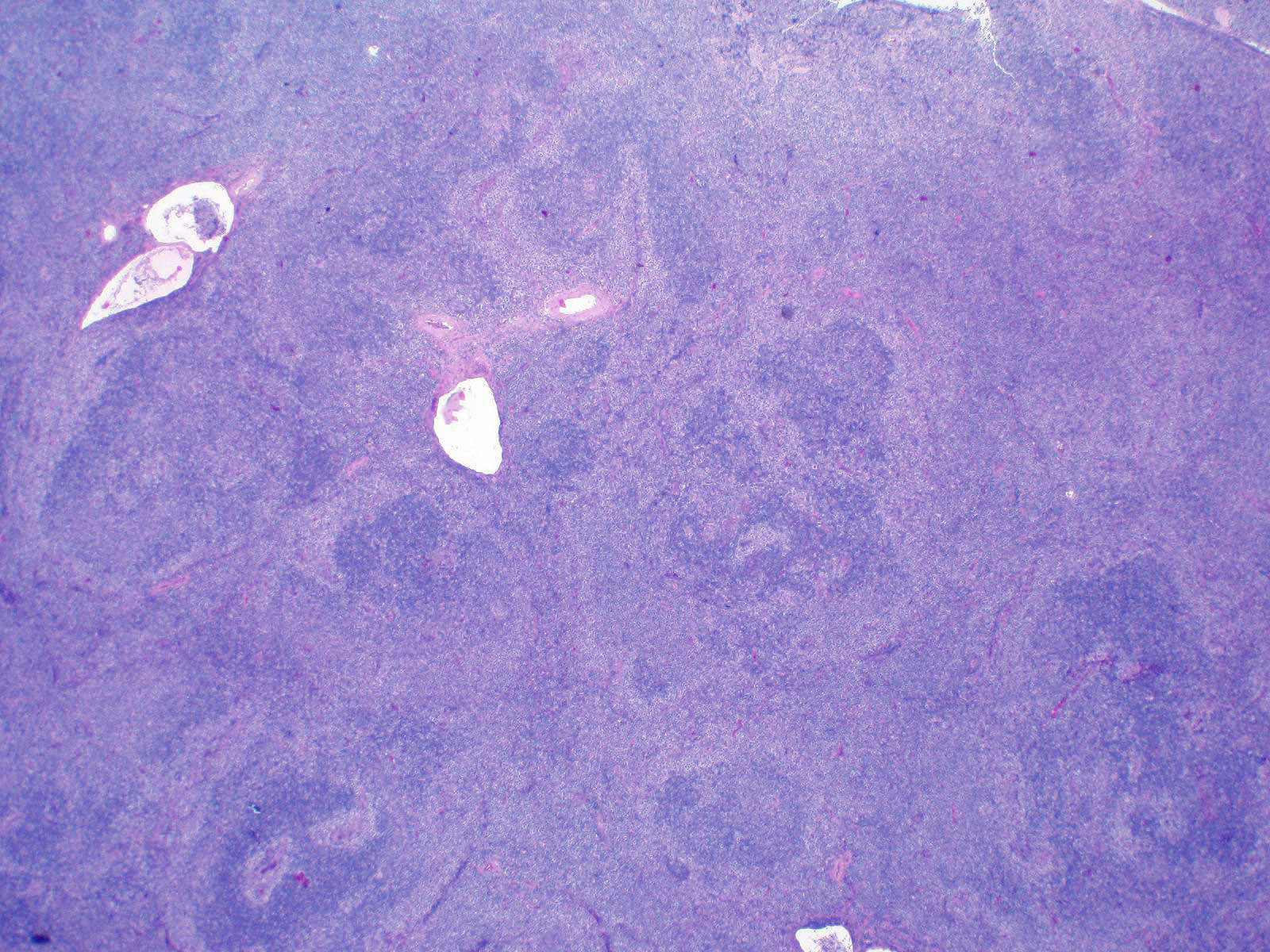
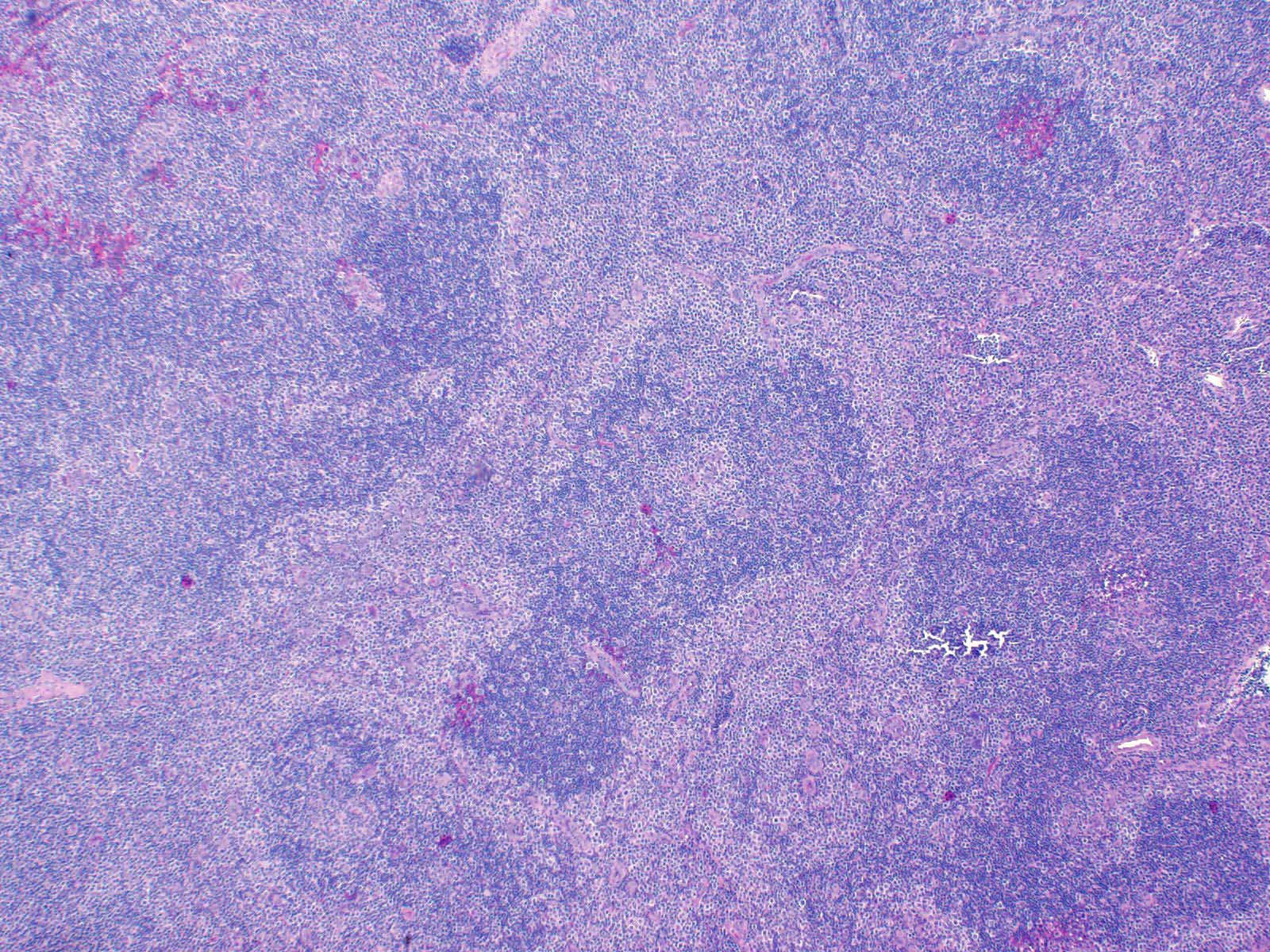
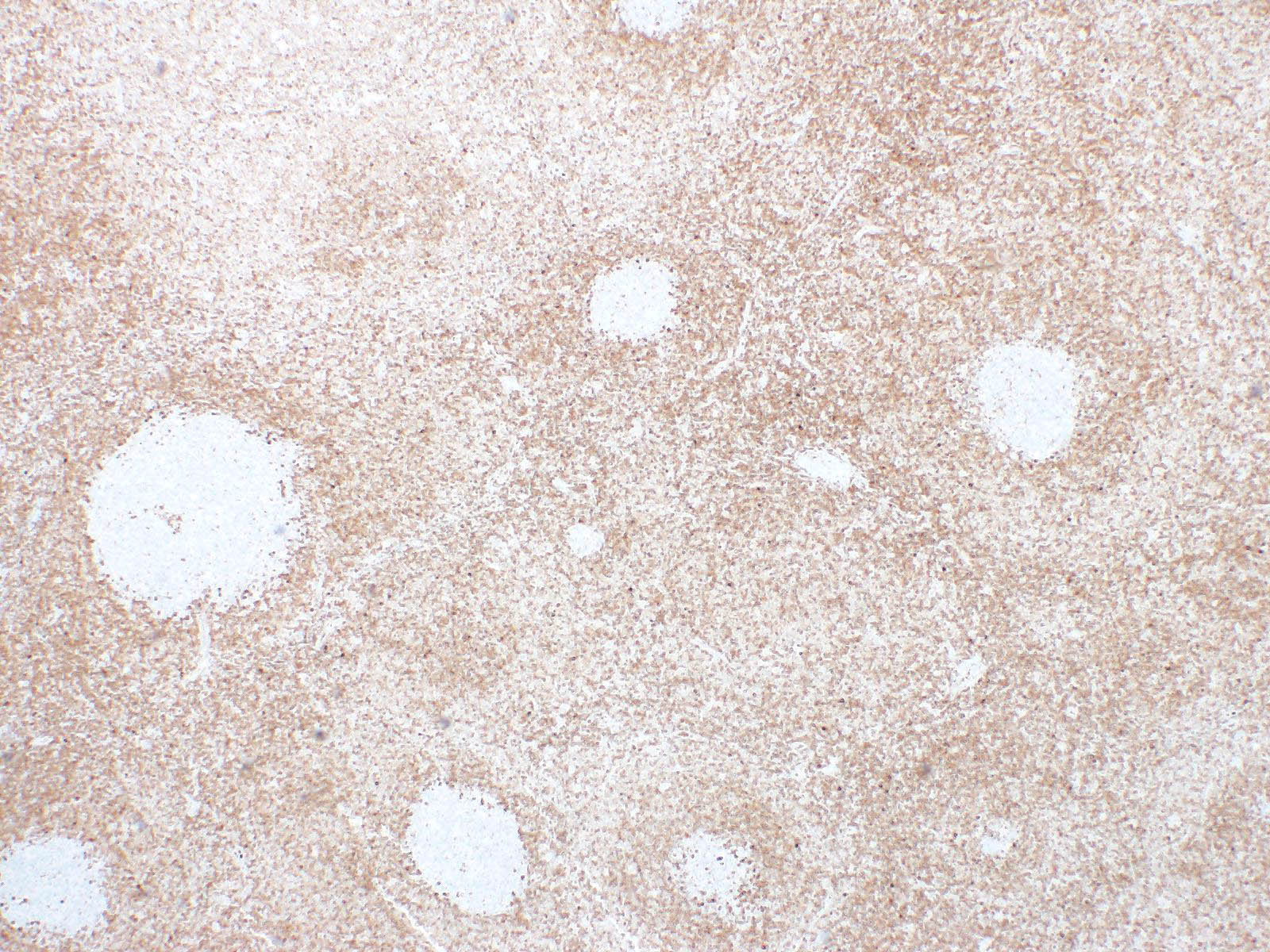
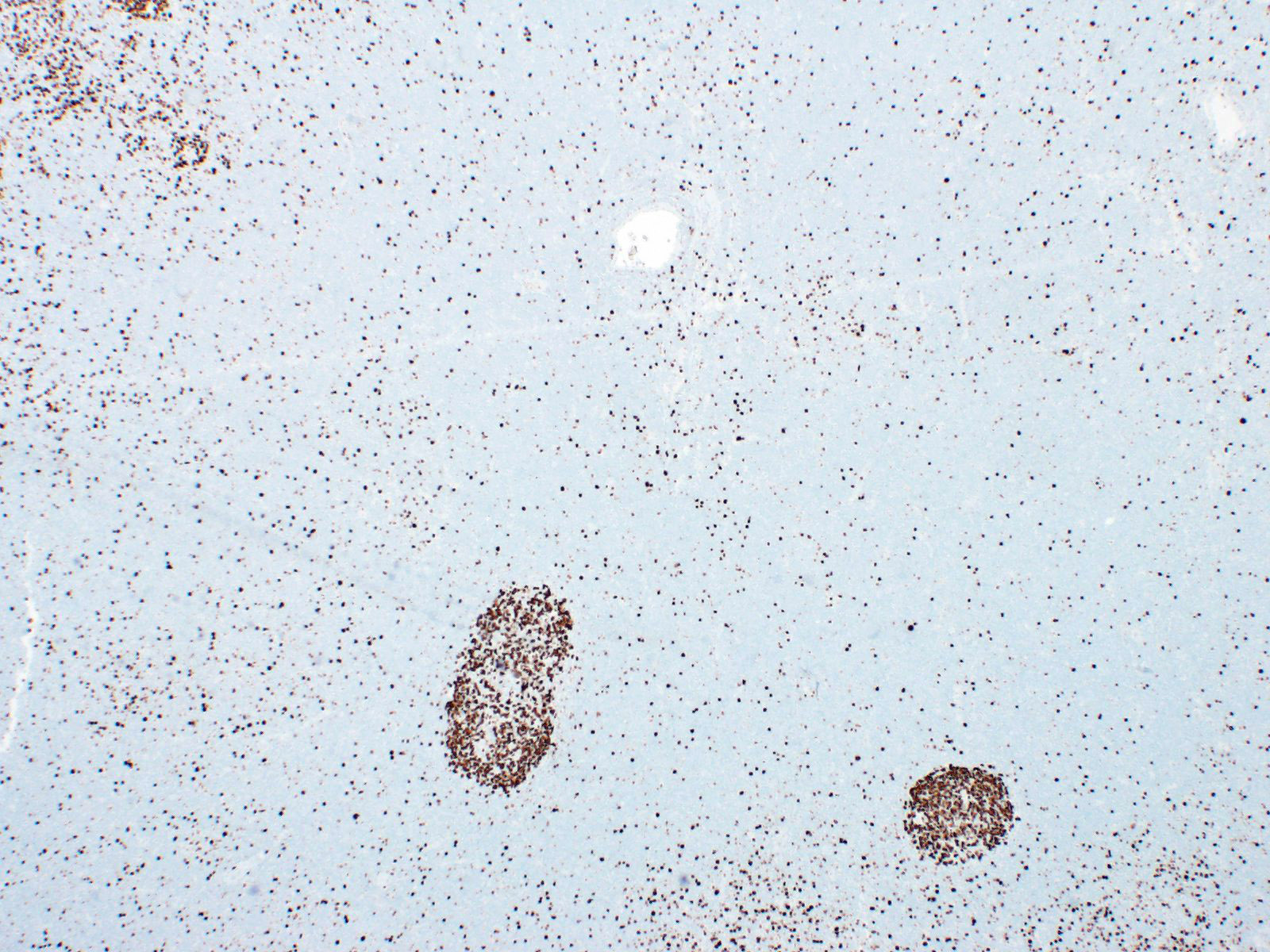
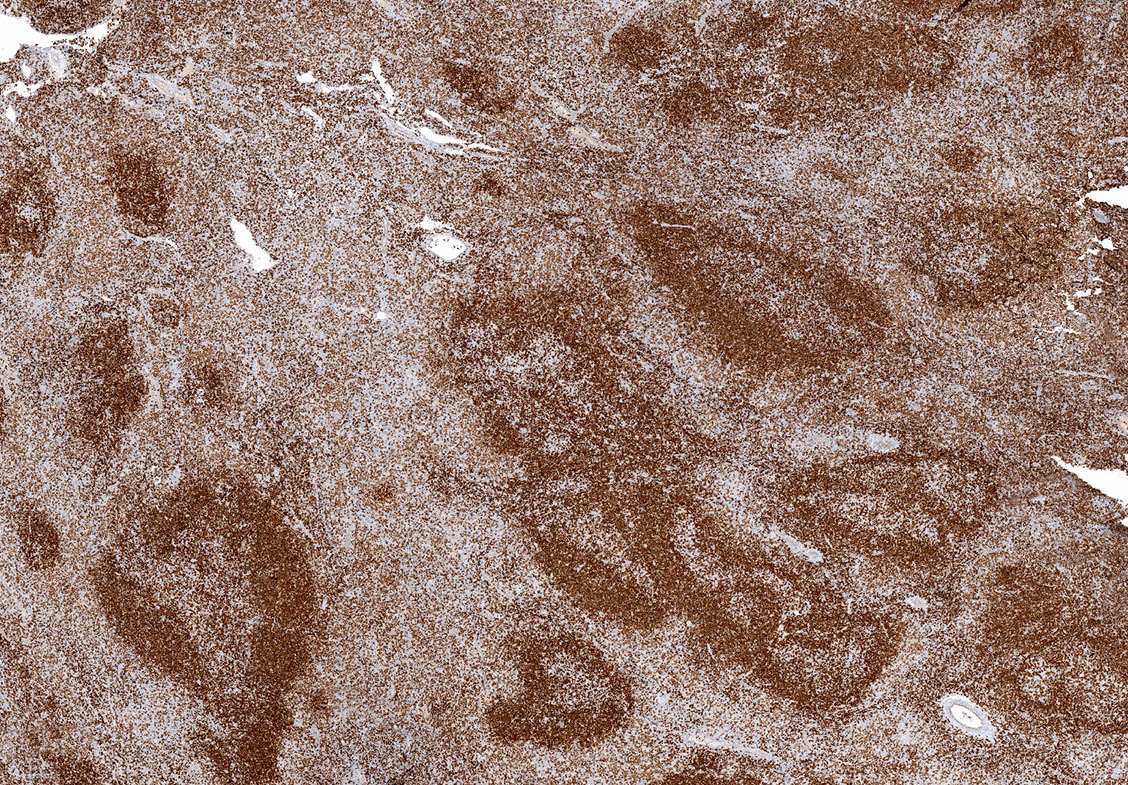
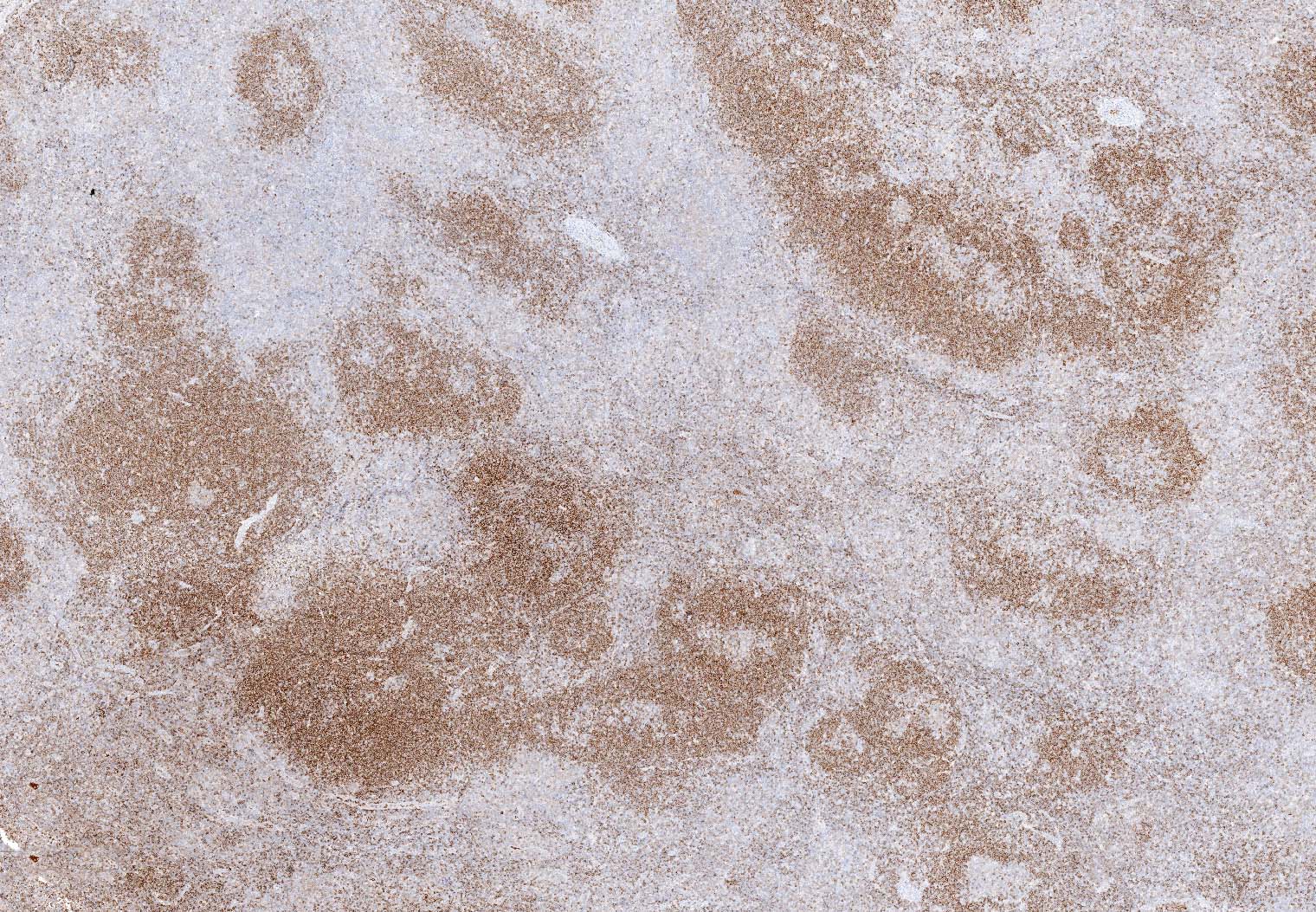
- Perifollicular and interfollicular lymphoid infiltrate that surrounds variably preserved germinal centers; diffuse pattern of infiltration can also be seen
- Infiltrate composed of monocytoid lymphoid cells, admixed with scattered large transformed B cells, positive for pan-B cell markers with light chain restriction and negative for CD5 and CD10
- Overall favorable prognosis with chemoimmunotherapy as mainstay of treatment
ICD coding
- ICD-0: 9699/3 - marginal zone B cell lymphoma, NOS
Epidemiology
- Rare, most commonly seen in adults; median age 50 - 60 years (Haematologica 2013;98:1003)
- Similar incidence in men and women
- Pediatric variant also encountered (Am J Surg Pathol 2003;27:522)
Sites
- Lymph nodes (Haematologica 2013;98:1003)
- Bone marrow and occasionally peripheral blood can be involved
Etiology
- Association with hepatitis C infection in some studies (Br J Haematol 2007;136:301)
- Increased incidence among women with autoimmune diseases (J Natl Cancer Inst Monogr 2014;2014:52)
Clinical features
- Localized or generalized peripheral lymphadenopathy (Br J Haematol 2007;136:301)
- Bone marrow is involved in < 50% of patients; peripheral blood rarely involved
- B symptoms rare
- Clinical and radiologic evaluation needs to be performed to rule out lymph node involvement by EMZL and SMZL
- Pediatric nodal marginal zone lymphoma (NMZL): predominantly young males, with median age of 16 years (M:F = 20:1); localized head and neck lymphadenopathy (Am J Surg Pathol 2003;27:522)
- Reference: Best Pract Res Clin Haematol 2017;30:92
Diagnosis
- Biopsy of affected lymph node
Laboratory
- Small subset of patients has monoclonal gammopathy (Histopathology 2006;48:162)
Prognostic factors
- Indolent lymphoma with 5 year overall survival of 60 - 70% (Eur J Haematol 2009;83:165)
- Factors associated with worse prognosis include advanced age, high clinical stage and B symptoms
- Pediatric NMZL: excellent prognosis and long term survival (Am J Surg Pathol 2003;27:522)
Case reports
- 15 year old boy with ataxia teleangiectasia and cervical lymphadenopathy (Hum Pathol Case Rep 2019;15:44)
- 34 year old man with left neck lymphadenopathy (Mol Cytogenet 2019;12:3)
- 50 year old man with enlarging neck mass and skin nodules (Case Rep Pathol 2013;2013:784176)
Treatment
- Watch and wait strategy in patients with low tumor burden and no clinical symptoms
- Rituximab combined with chemotherapy is the mainstay of treatment (Ann Oncol 2020;31:17)
- Radiation is a consideration in localized disease
- Pediatric NMZL: conservative therapy (Am J Surg Pathol 2003;27:522)
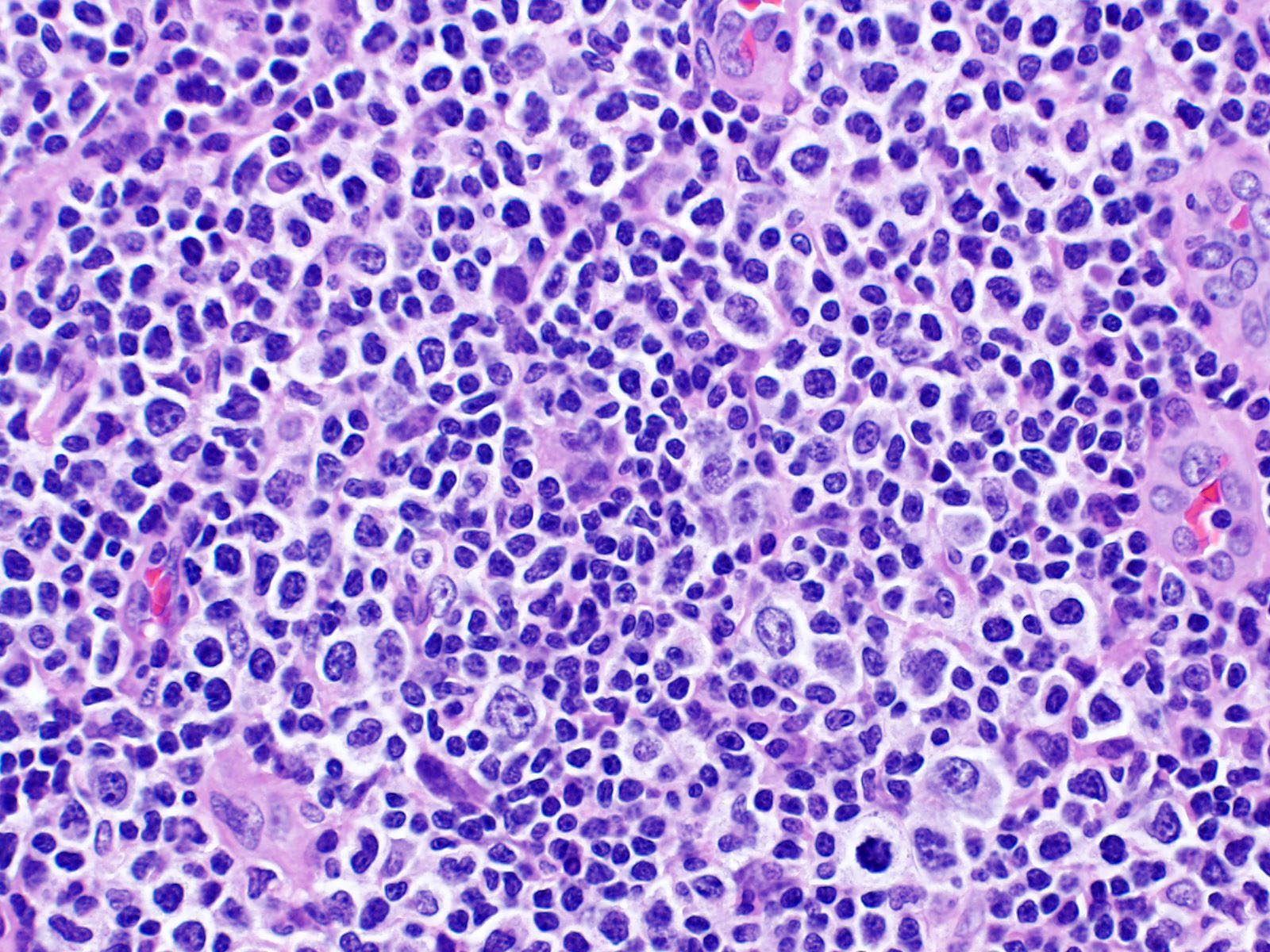
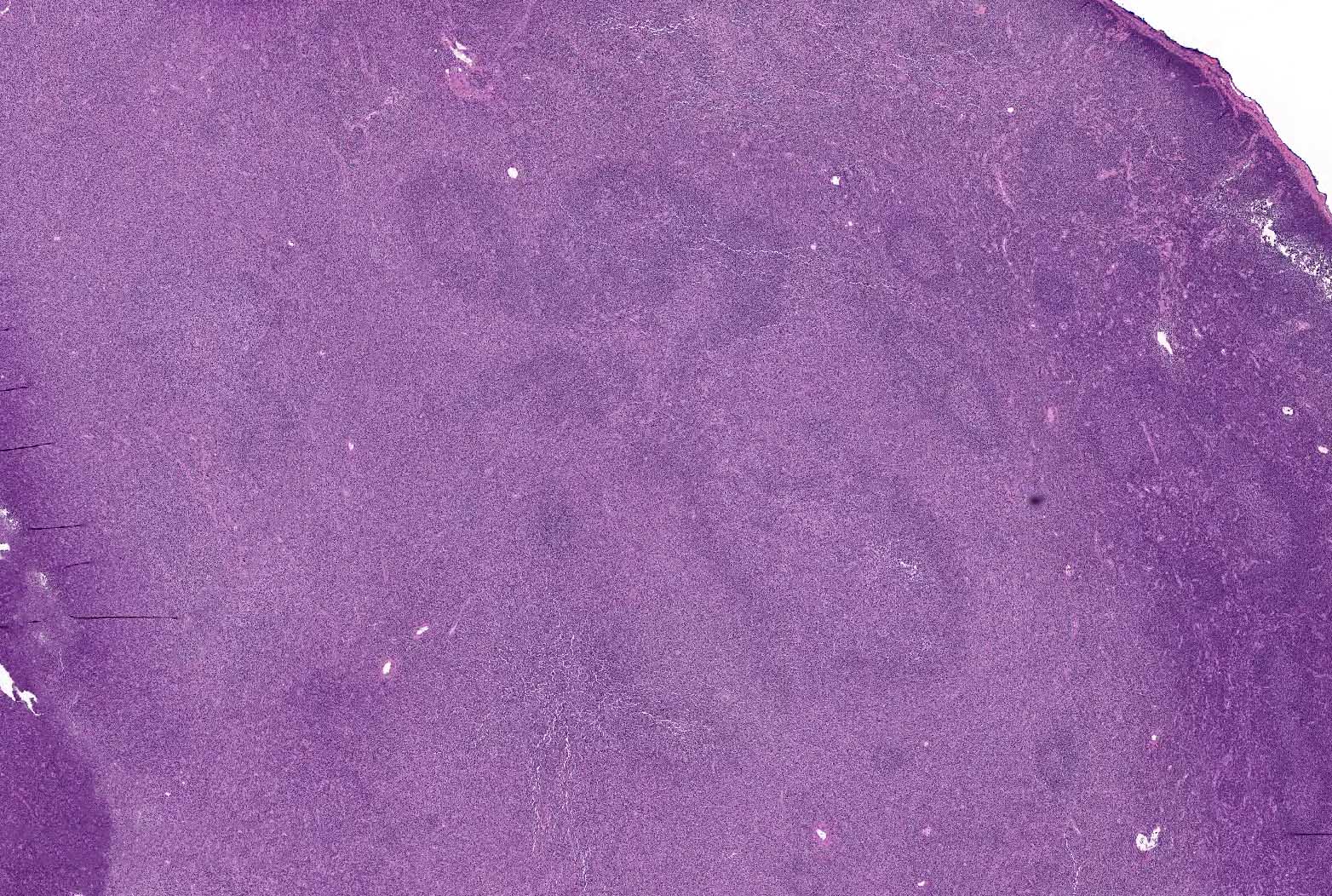
Microscopic (histologic) description
- Typically nodular, perifollicular and interfollicular lymphoid infiltrate that surrounds variably preserved germinal centers (Am J Clin Pathol 2009;132:39)
- Follicular colonization may be seen
- Some cases show diffuse pattern of combined nodular and diffuse patterns
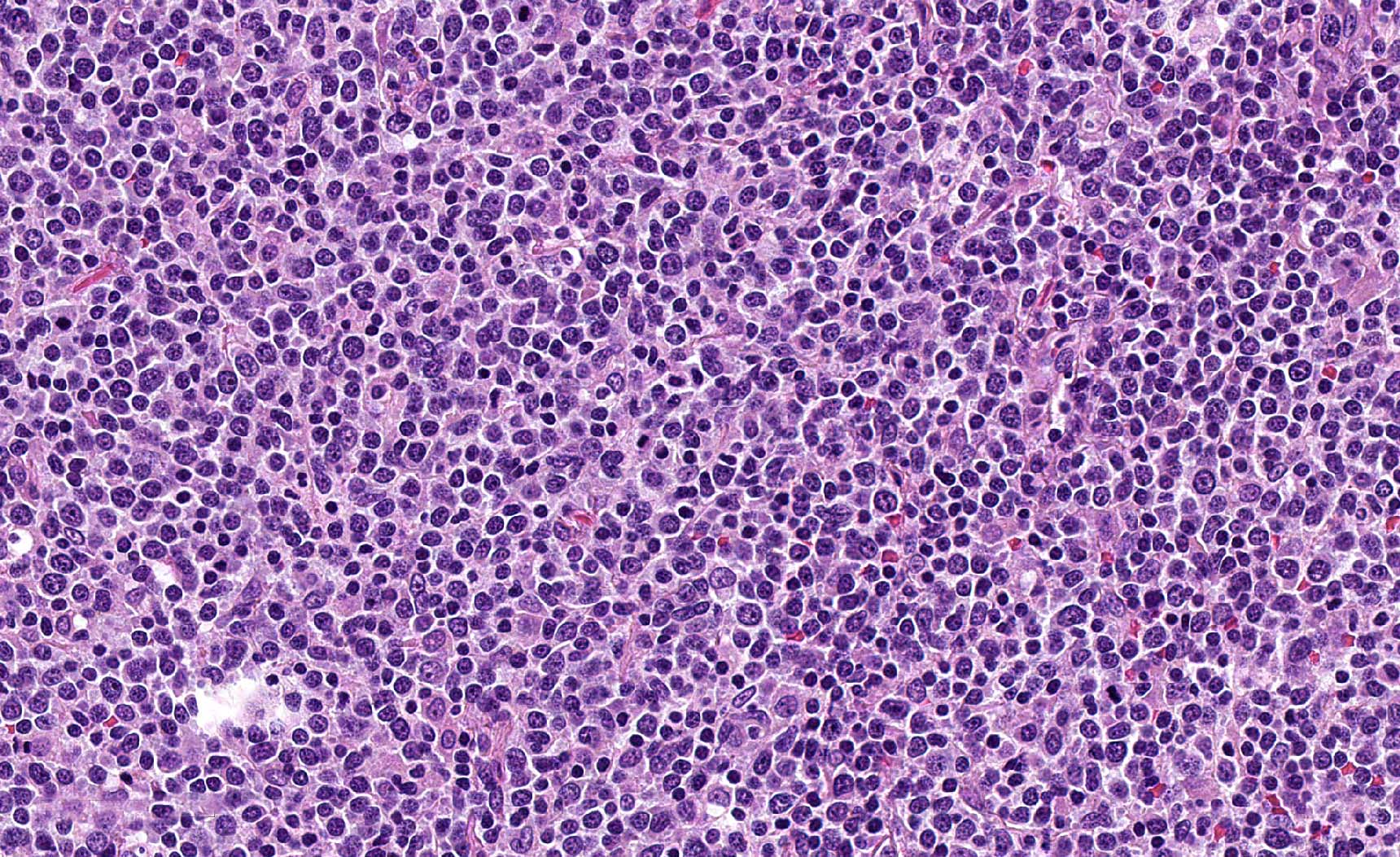
- Neoplastic infiltrate contains marginal zone B cells (monocytoid) with abundant pale cytoplasm, admixed with scattered large transformed B cells; large cells cannot be seen in sheets
- Fraction of cases that show increased large cells appears to be relatively high
- Variable degree of plasma cell differentiation can be seen
- Eosinophilia may be seen
- Some cases have increased number of large B cells (Histopathology 2006;48:162)
- Pediatric NMZL: pattern of follicular hyperplasia with extension of mantle zone cells into germinal centers mimicking progressive transformation of germinal centers (Am J Surg Pathol 2003;27:522)
Microscopic (histologic) images
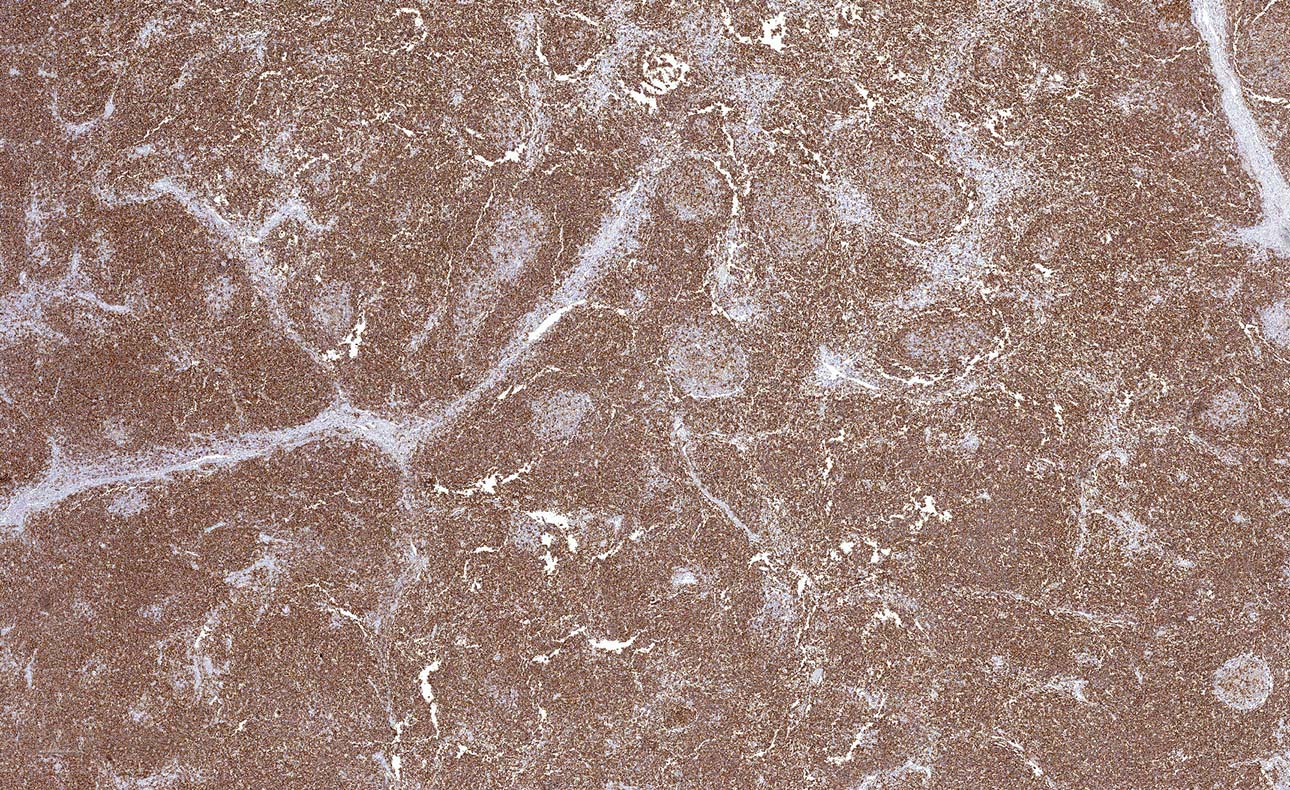
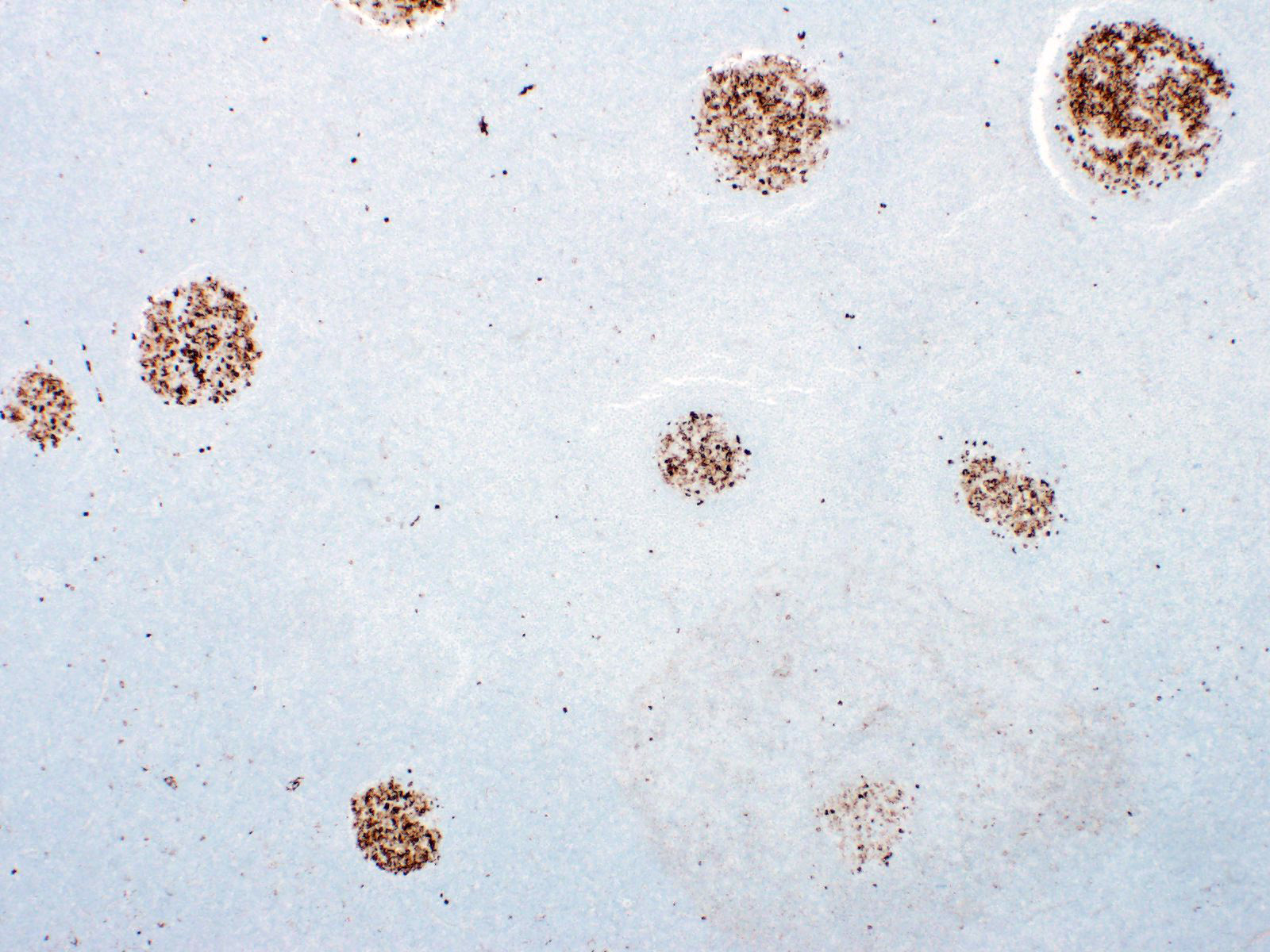
Positive stains
- CD20, PAX5, CD19, CD79a, BCL2, IRTA1, MNDA (Haematologica 2013;98:1003)
- CD43 (20 - 75%)
- In cases with plasmacytic differentiation, plasmacytoid cells are positive for MUM1; kappa or lambda light chain restriction can be seen
- Pediatric NMZL: CD20, CD43, BCL2 (50% of cases); frequent light chain restriction; IgD shows expanded irregular mantle zones (Am J Surg Pathol 2003;27:522)
Negative stains
Flow cytometry description
- Mature B cell population, negative for CD5 and CD10 with light chain restriction
Molecular / cytogenetics description
- Immunoglobulin gene rearrangement studies show clonal rearrangement in majority of cases (Haematologica 2013;98:1003)
- Recurrent mutations include KMT2D, PTPRD, NOTCH2, KLF2 and BRAF; rare cases show MYD88 mutations (Am J Surg Pathol 2015;39:644, Leukemia 2018;32:2412, Blood 2016;128:1362)
- Recurrent cytogenetic abnormalities include gains of chromosomes 3 and 18 and loss of 6q23-24 (Histopathology 2006;48:162, Blood 2011;117:1595, Hematol Oncol 2000;18:1)
- Pediatric NMZL: clonal immunoglobulin gene rearrangement; recurrent cytogenetic abnormalities include trisomy 18 and trisomy 3 (Mod Pathol 2010;23:866)
Sample pathology report
- Lymph node, left neck, excisional biopsy:
- Morphologically consistent with nodal marginal zone lymphoma (see comment)
- Comment: Correlate with clinical, laboratory and radiologic findings.
Differential diagnosis
- Extranodal marginal zone lymphoma (EMZL):
- Occasionally involves lymph nodes and shows overlapping morphologic and immunophenotypic features with NMZL
- Typically, well preserved reactive follicles with mantle zone are seen with expanded marginal zone by monocytoid cells
- Clinical and radiologic correlation is needed to rule it out
- Splenic marginal zone lymphoma (SMZL) (Blood 2016;127:2072):
- Clinically, patients present with splenomegaly and bone marrow involvement
- Clinical and radiologic correlation is needed
- Occasionally, SMZL can involve lymph nodes and show overlapping features with NMZL
- Lymphoplasmacytic lymphoma (LPL) (Hematol Oncol Clin North Am 2019;33:639):
- Lymph node architecture usually partially preserved with open sinuses
- Infiltrate is composed of small lymphocytes, plasmacytoid cells and plasma cells with frequent Dutcher bodies
- Bone marrow is involved in LPL and patients have monoclonal protein (IgM); therefore, correlation with laboratory findings and bone marrow biopsy is recommended
- MYD88 mutation is consistently seen in LPL, while it has been reported in rare cases of NMZL
- Marginal zone hyperplasia:
- Expanded marginal zone seen in some reactive conditions
- Difficult to distinguish from NMZL bases on morphology alone
- Identification of clonal B cell population favors the diagnosis of NMZL
- Follicular lymphoma (FL) with marginal zone differentiation:
- Neoplastic nodules show cells with monocytoid appearance having abundant pale cytoplasm
- In the centers of neoplastic nodules, lymphoma cells frequently show more typical FL appearance
- Lymphoma cells are CD10 and BCL6 positive and coexpressing BCL2, although monocytoid component could show weak / absent CD10
- Additional useful immunostains - HGAL, LMO2 and MEF2B are positive in FL, while MNDA and IRTA1 are positive in NMZL
- Small lymphocytic lymphoma (SLL):
Additional references
Practice question #1
A 60 year old woman presents with cervical and axillary lymphadenopathy and history of night sweats for the past 3 months. Cervical lymph node is excised and infiltrate is shown in the image above. Flow cytometry showed clonal B cell population and was positive for CD20 and CD19 with kappa light chain restriction. The population was negative for CD5, CD10 and CD23. Which of the following genetic abnormalities can occasionally be found in this lymphoma?
- DUSP22 rearrangement
- IGH-BCL2 rearrangement
- IGH-CCND1 rearrangement
- MYD88 mutation
- t(2;5)(p23;q35); ALK-NPM1
Practice answer #1
Practice question #2
A 13 year old boy presents with cervical lymphadenopathy. Cervical lymph node is excised and infiltrate is shown in the images above. Molecular studies were performed on the excisional biopsy and showed clonal immunoglobulin gene rearrangement. Which of the following is true about this lymphoma?
- Approximately 50% of cases transform to diffuse large B cell lymphoma
- It is more common in women
- Long term prognosis is poor
- Most cases show TNFRSF14 mutation
- Patients typically present with head and neck lymphadenopathy
Practice answer #2
E. Patients typically present with head and neck lymphadenopathy
Comment Here
Reference: Nodal marginal zone lymphoma
Comment Here
Reference: Nodal marginal zone lymphoma