Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1Cite this page: Cornejo KM. Adult granulosa cell tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisgranulosa.html. Accessed September 16th, 2025.
Definition / general
- Sex cord stromal tumor resembling granulosa cells of the Graafian follicles of the ovary
Essential features
- Rare, low grade, indolent sex cord stromal tumor; 10% have malignant potential
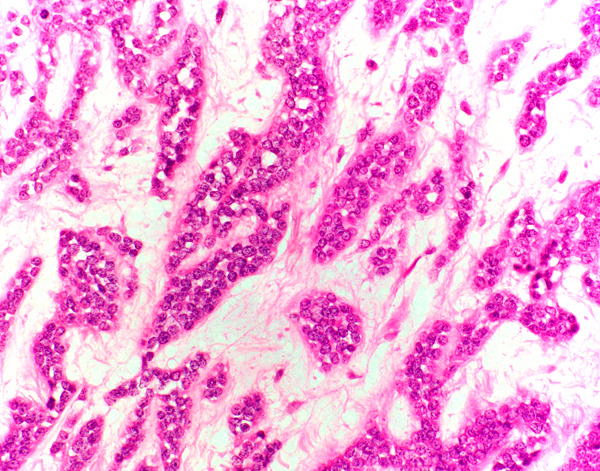
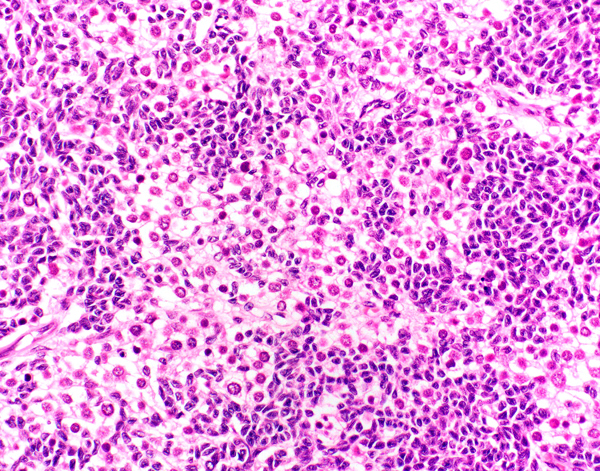
- Most common architectural patterns are diffuse / solid, insular and spindled; pathognomonic Call-Exner bodies, which are a part of the microfollicular pattern, are less common
- Morphologically, the tumor cells characteristically display uniformly round to ovoid nuclei with conspicuous, longitudinal nuclear grooves
- FOXL2 gene mutations occur in a minor subset of cases, which is substantially less frequent than in its ovarian counterpart
ICD coding
Epidemiology
- Rare (< 0.5% of all sex cord stromal tumors)
- Mean age: 40 years (range: 14 - 87 years) (Am J Surg Pathol 2014;38:1242)
Sites
- Testicular parenchyma
Pathophysiology
- Derived from granulosa cells in which FOXL2, a granulosa cell expressed gene, plays a role in regulating cell fate
- Missense mutation (402C → G, C134W) causes a negative effect by dysregulating gene expression, leading to increased cell proliferation and reducing apoptosis (Oncol Lett 2020;20:293)
Etiology
- Unknown
Clinical features
- Unilateral testicular mass or swelling
- Typically no endocrine related symptoms (i.e. gynecomastia, decreased libido) (Am J Surg Pathol 2014;38:1242)
- Reported in up to 20% of cases (Mod Pathol 2005;18:S81, J Cancer Res Clin Oncol 2020;146:2829)
Diagnosis
- Imaging studies (e.g. ultrasound) may identify a testicular mass
- Definitive diagnosis is made by histopathologic examination only
Laboratory
- No elevated serum makers (Am J Surg Pathol 2014;38:1242)
Radiology description
- Nonspecific findings but typically shows a well demarcated, hypoechoic mass with hyperechoic foci and calcification (Radiol Case Rep 2015;3:188)
Radiology images
Prognostic factors
- Most are benign; 10% have malignant potential (J Cancer Res Clin Oncol 2020;146:2829)
- Pathologic features most commonly associated with more aggressive behavior include (Am J Surg Pathol 2014;38:1242):
- Lymphovascular invasion
- Infiltrative borders / extratesticular involvement
- Size > 4 cm
- Other pathologic features reported to be associated with malignant potential include (J Cancer Res Clin Oncol 2020;146:2829, Hum Pathol 1993;24:1120, Hum Pathol 2008;39:701, Arch Pathol Lab Med 2011;135:143):
- Moderate or marked nuclear atypia
- Presence of necrosis
- > 5 mitotic figures per 10 high power fields
- Association with gynecomastia
Case reports
- 22 year old man with unspecific scrotal discomfort (Case Rep Urol 2019;2019:7156154)
- 43 year old man with left testicular swelling (Int Braz J Urol 2015;41:1226)
- 65 year old man with hepatic metastasis (Indian J Pathol Microbiol 2020;63:470)
Treatment
- Radical orchiectomy
- Testis sparing surgery / wedge excision for smaller, benign tumors (Am J Surg Pathol 2014;38:1242, J Cancer Res Clin Oncol 2020;146:2829)
- Retroperitoneal lymph node dissection and platinum based chemotherapy (e.g. bleomycin, etoposide, cisplatin) for metastatic disease (J Cancer Res Clin Oncol 2020;146:2829)
- Rare reports of treatment with tyrosine kinase inhibitors, such as pazopanib with partial response (Oncology (Williston Park) 2009;23:792)
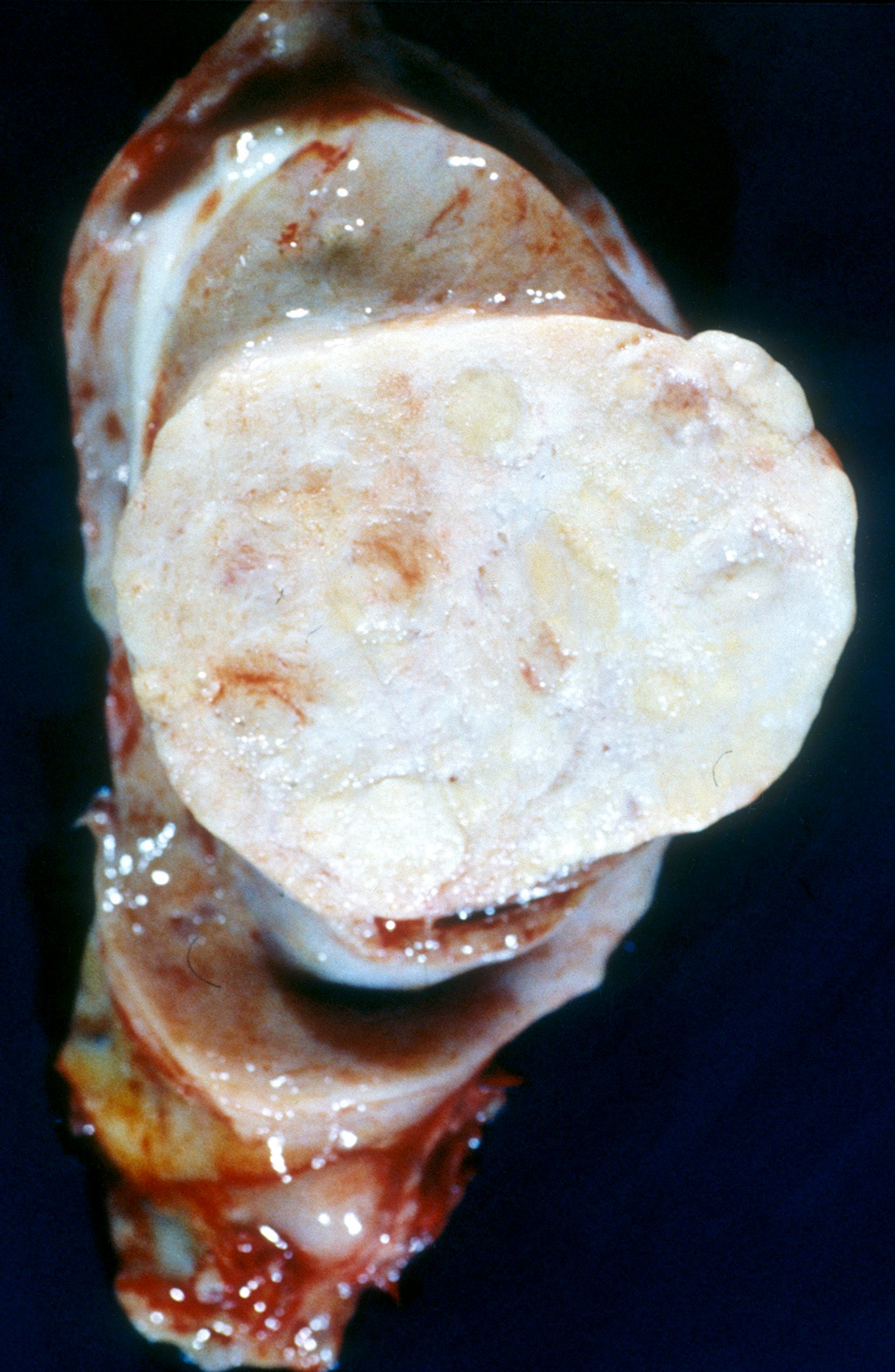
Gross description
- Mean size: 2.8 cm (0.5 - 6.0 cm) (Am J Surg Pathol 2014;38:1242)
- Well circumscribed, predominantly solid; occasionally solid and cystic
- Lobulated, yellow-tan or tan-white cut surface
- Infiltrative borders / extratesticular involvement, hemorrhage and necrosis are rarely seen and often associated with more aggressive behavior
Gross images
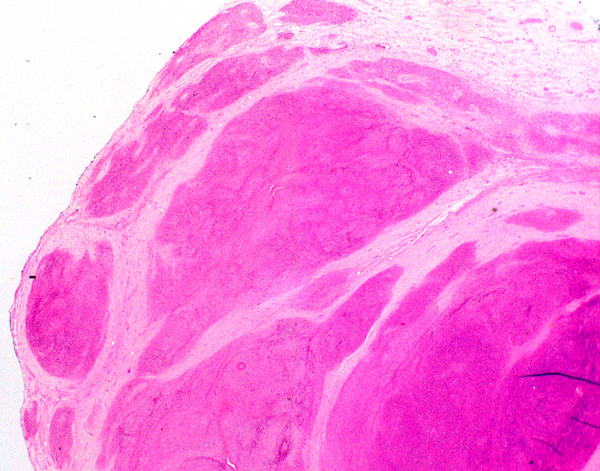
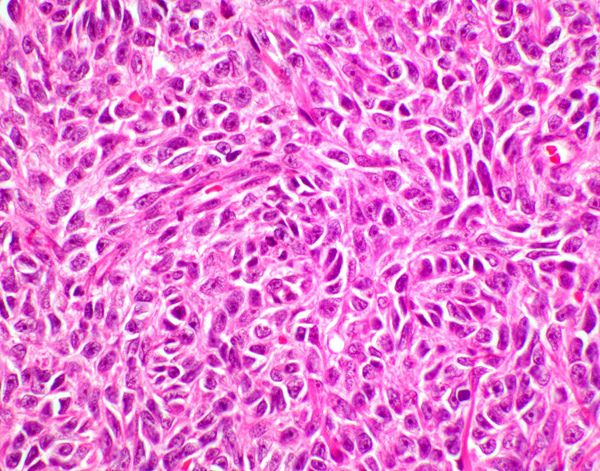
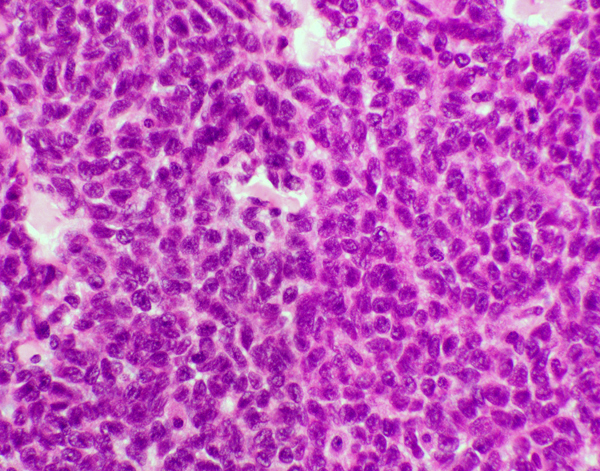
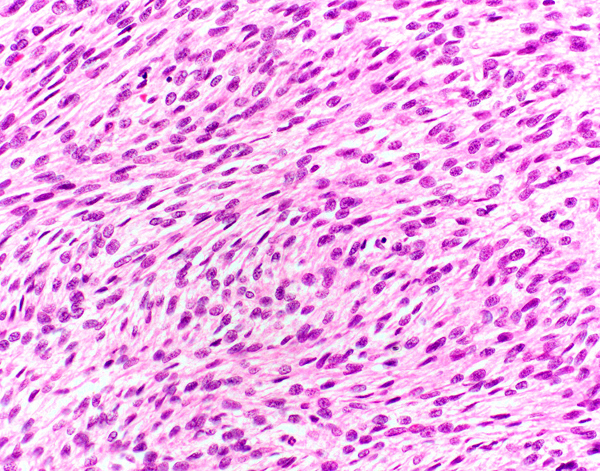
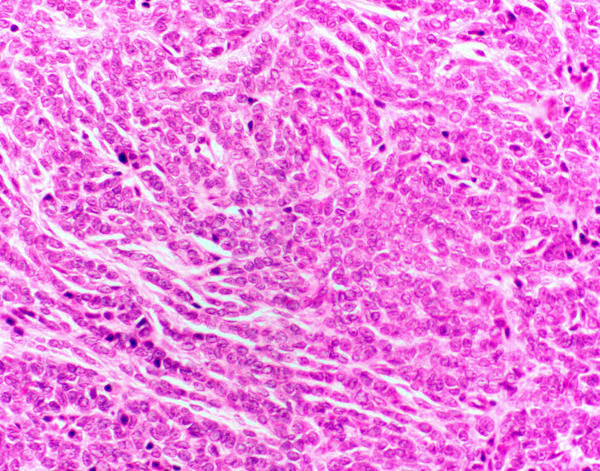
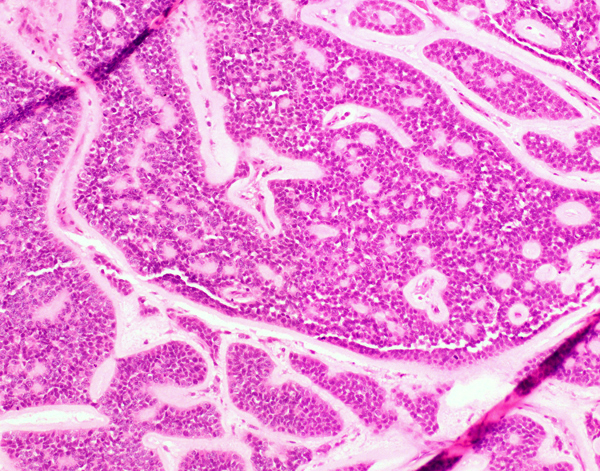
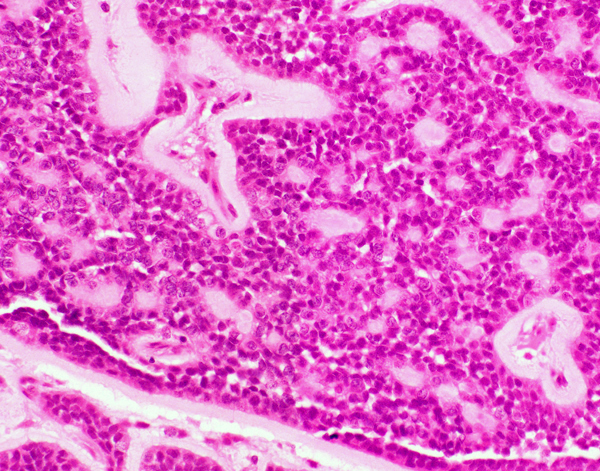
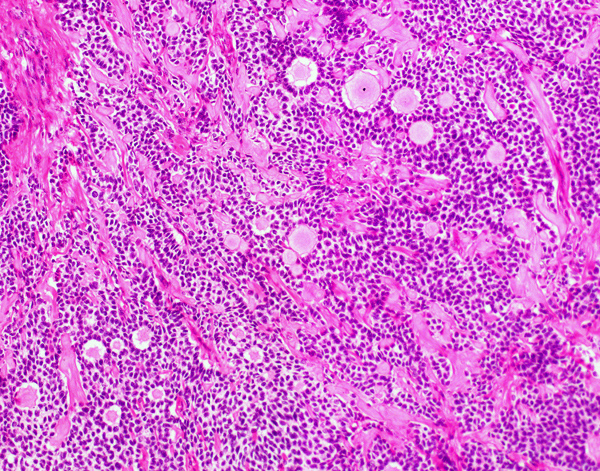
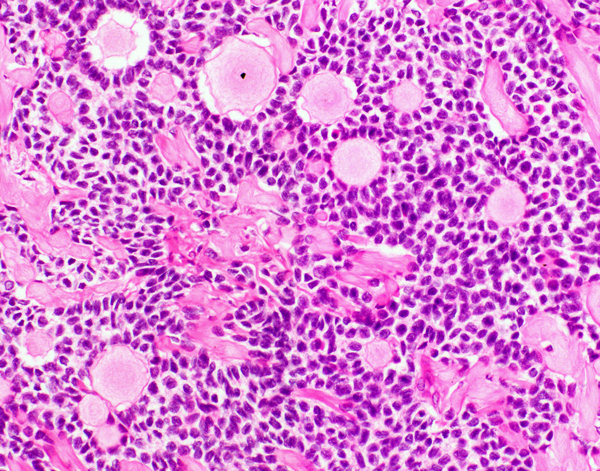
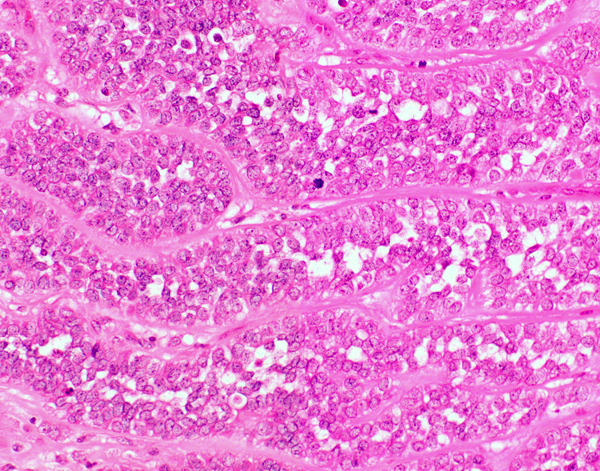
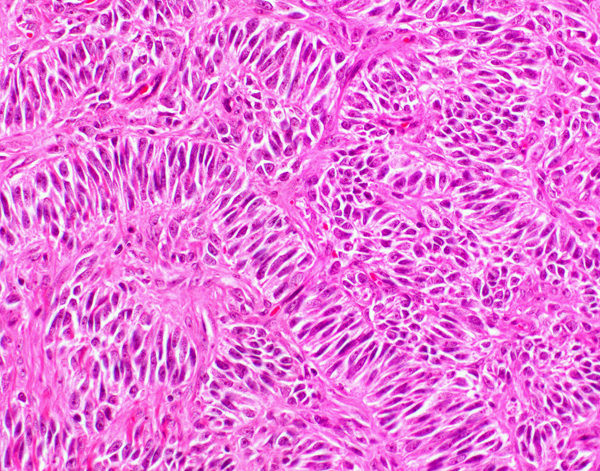
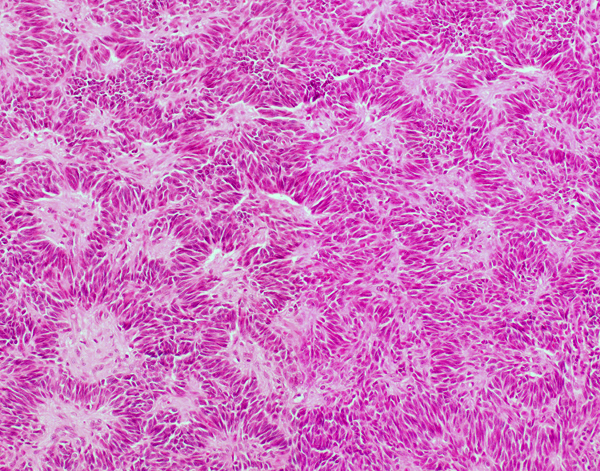
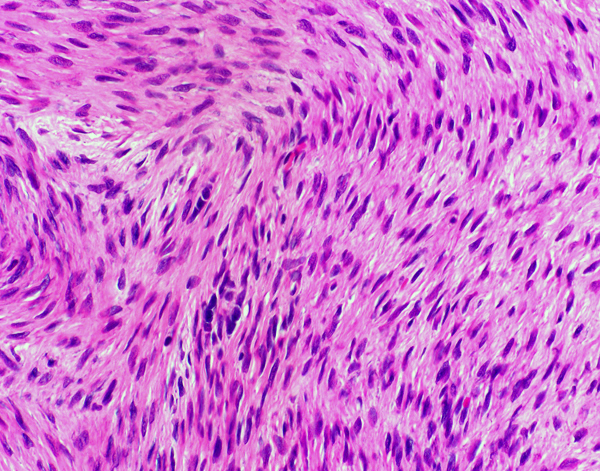
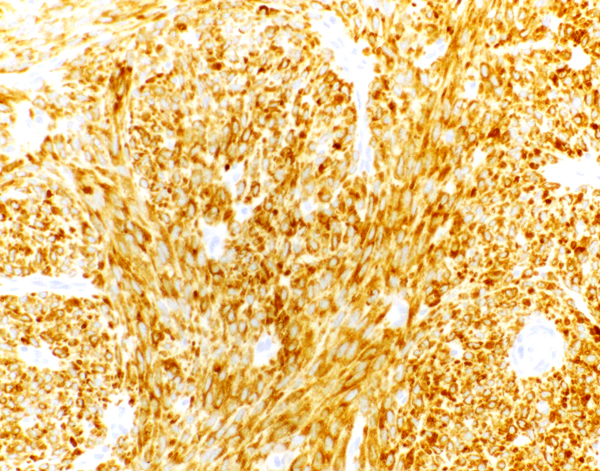
Microscopic (histologic) description
- Low power: typically displays a nodular / lobulated appearance
- High power: tumor cells contain uniformly round to ovoid nuclei with conspicuous longitudinal nuclear grooves, indistinct cell borders, variable amounts of eosinophilic cytoplasm
- Most common patterns: diffuse / solid, insular and spindled (Am J Surg Pathol 2014;38:1242)
- Diffuse / solid: sheets of round cells
- Insular: nests of tumor cells surrounded by stroma
- Spindled: sheets of fusiform cells
- Cords / trabecular: regularly to irregularly arranged thin cords or thick columns of tumor cells
- Water silk / gyriform: interweaving cords and undulating columns of cells
- Microfollicular: numerous small spaces with hyalinized basement membrane material or eosinophilic fluid (Call-Exner bodies)
- Herringbone / fascicular: spindled cells with fibrocollagenous stroma
- Pseudopapillary: tumor cells surrounding fibrovascular cores
- Palisading: tumor cells arranged parallel to each other, resembling a fence
- Luteinized: more abundant clear to eosinophilic cytoplasm with rounded nuclei
- Admixed with varying amounts of fibrocollagenous or edematous stroma
- Mitotic count: mean 4.9/10 high power fields (0 - 18/10 high power fields); suggests the presence of mitoses are not of prognostic significance (Am J Surg Pathol 2014;38:1242)
- May contain hemorrhage or hemosiderin deposition
- Rarely displays necrosis and lymphovascular invasion; features of aggressive behavior
- Tumor often infiltrates between seminiferous tubules and may involve rete testis and tunica albuginea
- Rarely involves paratesticular or extratesticular tissue
Microscopic (histologic) images
Contributed by Kristine M. Cornejo, M.D.
Positive stains
- Inhibin A: best marker of sex cord stromal tumors (Am J Surg Pathol 2014;38:e50)
- Vimentin, calretinin, CD99
- SMA (70%), S100 (60%) (Am J Surg Pathol 2014;38:1242)
- FOXL2 positive in sex cord stromal tumors, such as adult granulosa cell tumor, juvenile granulosa cell tumor, Sertoli cell tumor and thecoma fibroma; positivity does not correlate to mutation status (Appl Immunohistochem Mol Morphol 2011;19:347, Am J Surg Pathol 2011;35:484)
Negative stains
- EMA, HMB45, desmin (Am J Surg Pathol 2014;38:1242)
- OCT 3/4, SALL4 (markers of germ cell tumors) (Am J Surg Pathol 2014;38:e50)
- Beta catenin (no nuclear staining) (Am J Surg Pathol 2015;39:1390)
- Variable for cytokeratin / low weight cytokeratin (45% positive, paranuclear and dot-like pattern), melanA (25% positive) (Am J Surg Pathol 2014;38:1242)
Molecular / cytogenetics description
- FOXL2 C134W (c.402C > G) gene mutation in a minor subset of cases (up to 40%; 2 of 5 tumors) (Arch Pathol Lab Med 2012;136:825)
- Less frequently identified in comparison to its ovarian counterpart (Appl Immunohistochem Mol Morphol 2011;19:347)
Sample pathology report
- Left testis, radical orchiectomy:
- Adult granulosa cell tumor (3.0 cm), confined to the testis (see comment)
- Comment: The tumor is small, well circumscribed and lacks features associated with a more aggressive behavior, such as significant cytologic atypia, conspicuous mitoses, presence of lymphovascular invasion or necrosis.
Differential diagnosis
- Juvenile granulosa cell tumor:
- Typically occurs in the first 6 months of life; rare after 1 year of age
- Associated with ambiguous external genitalia and karyotypes
- Most common patterns are solid and follicular, in which the follicles are irregular in size and shape lined by granulosa cells with an outer thecal layer; contains mucinous material that is not found in adult granulosa cell tumor and the follicles tend to be more uniform
- Usually lacks Call-Exner bodies and nuclear grooves
- Leydig cell tumor:
- Presents at a similar age (mean: 46.5 years)
- Similarly presents with sheets or lobular aggregates of cells with abundant eosinophilic cytoplasm arranged with variable amounts of fibrous stroma
- Cells may be vacuolated and contain Reinke crystals, which are not seen in adult granulosa cell tumors
- Sertoli cell tumor:
- Presents at a similar age (mean: 45 years)
- Displays a variety of patterns, such as trabecular, corded and diffuse, in addition to varying amounts of well formed tubules; the latter is typically not seen in adult granulosa cell tumors and lacks the typical microfollicular pattern or Call-Exner bodies
- Composed of tumor cells with abundant pale to lightly eosinophilic cytoplasm, which may display nuclear grooves
- Positive for nuclear beta catenin (Am J Surg Pathol 2015;39:1390)
- Fibrothecoma:
- Presents at a similar age (mean: 44 years)
- Composed of ovoid or spindled cells in varying amounts of collagenous stroma
- Lacks varied architectural patterns and nuclear grooves
- Inhibin A positive (patchy to diffuse pattern) (Am J Surg Pathol 2013;37:1208)
- Sex cord stromal tumor, unclassified:
- Tumors that have features of indeterminate differentiation; lack findings characteristic of adult granulosa cell tumors or other sex cord stromal tumors
- Sex cord stromal tumor, mixed:
- Tumors that contain characteristics of 2 or more tumor subtypes
Additional references
Practice question #1
A 47 year old man presented with a right testicular swelling. Histologic examination revealed the tumor shown above. This tumor typically shows which of the following immunoprofiles?
- OCT4+ / SALL4+ / inhibin A- / FOX2L-
- OCT4- / SALL4+ / inhibin A+ / FOX2L-
- OCT4- / SALL4- / inhibin A+ / FOX2L+
- OCT4- / SALL4- / inhibin A- / FOX2L-
Practice answer #1
C. OCT4- / SALL4- / inhibin A+ / FOX2L+. Histology shows Call-Exner bodies, which are pathognomonic for adult granulosa cell tumor. Adult granulosa cell tumor expresses general sex cord stromal tumor immunohistochemical markers, such as inhibin A. FOX2L has also been found to be a marker of sex cord stromal tumors and does not necessarily correlate with a FOX2L gene mutation, which has been identified in a small subset of testicular adult granulosa cell tumors. OCT4 and SALL4 are markers of germ cell tumors.
Comment Here
Reference: Adult granulosa cell
Comment Here
Reference: Adult granulosa cell