Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Kefeli M. Parathyroid carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/parathyroidpthca.html. Accessed September 16th, 2025.
Definition / general
- Malignant neoplasm originating from parathyroid parenchymal cells
Essential features
- 90% of patients present with excess parathyroid hormone (PTH)
- HRPT2 (CDC73) mutation is strongly associated with familial and sporadic parathyroid carcinoma (> 70%)
- One of the following features is necessary for definitive malignancy diagnosis of parathyroid lesion (Endocr Pathol 2022;33:64):
- Angioinvasion (vascular invasion)
- Lymphatic invasion
- Perineural (intraneural) invasion
- Invasion of adjacent structures / organs
- Metastasis
- Estimated 5 year and 10 year overall survival rates are 78 - 85% and 49 - 70%, respectively (Ann Surg Oncol 2015;22:3990)
Terminology
- Parathyroid carcinoma
ICD coding
- ICD-10: C75.0 - malignant neoplasm of parathyroid gland
Epidemiology
- M = F
- Mean age of 56 years (range: 15 - 89 years)
- Usually associated with familial syndromes in younger patients
- < 1% of cases of primary hyperparathyroidism (J Bone Miner Res 2008;23:1869)
Sites
- Normal parathyroid gland location
- Sites of the neck in which parathyroid gland can be seen (e.g., retroesophageal space, mediastinum, thymus and thyroid gland)
Etiology
- 10 - 15% related to hyperparathyroidism jaw tumor (HPT JT) syndrome (N Engl J Med 2003;349:1722)
- Association with familial isolated hyperparathyroidism, multiple endocrine neoplasia types 1 and 2 has been reported (Clin Endocrinol (Oxf) 2016;84:244, Clin Endocrinol (Oxf) 1997;47:747)
- Rare sporadic cases have been reported following radiation exposure and in patients with longstanding secondary hyperparathyroidism (see Molecular / cytogenetics description) (Br J Surg 1988;75:873, Tumori 2005;91:558)
Clinical features
- Palpable neck mass (30 - 75%)
- Symptoms of overt hyperparathyroidism:
- Bone disease (osteitis fibrosa cystica, osteoporosis, fractures)
- Renal disease (nephrolithiasis, nephrocalcinosis)
- Neurocognitive symptoms (fatigue, weight loss, weakness, anxiety, depression, polyuria, polydipsia)
- Jaw tumor (if associated with HPT JT)
- Neck pain
- References: Turk Patoloji Derg 2015;31:80, Endocr Pathol 2022;33:64
Diagnosis
- One of the following microscopic features is necessary for definitive diagnosis of parathyroid lesion malignancy (Endocr Pathol 2022;33:64):
- Angioinvasion (vascular invasion)
- Lymphatic invasion
- Perineural (intraneural) invasion
- Invasion of adjacent structures / organs
- Metastasis
Laboratory
- PTH levels are usually > 3 times the upper limit of normal (Turk Patoloji Derg 2015;31:80, Nat Rev Endocrinol 2012;8:612)
- Hypercalcemia (often > 14 mg/dL) (Turk Patoloji Derg 2015;31:80, Nat Rev Endocrinol 2012;8:612)
- Third / second generation PTH assay ratio is usually > 1 (Nat Rev Endocrinol 2012;8:612)
- Albumin corrected calcium levels are > 3 mmol/L (85% of patients) (Ann Surg Oncol 2010;17:2156)
- Rare nonfunctioning parathyroid carcinomas have also been reported (Endocr Pract. 2007;13:750)
Radiology description
- Single gland disease
- Infiltration or calcification on neck ultrasound (Eur Radiol 2011;21:1865, Endocr J 2001;48:213)
- Suspicion of metastatic disease on sestamibi or CT scan (Head Neck 2016;38:E2159, Semin Ultrasound CT MR 2012;33:123, J Clin Endocrinol Metab 2014;99:4531)
Radiology images
Prognostic factors
- The following microscopic features have been reported with aggressive growth in some parathyroid tumors (Am J Surg Pathol 1993;17:820):
- Necrosis
- Macronucleoli
- > 5 mitoses per 10 mm2
- Older age at time of diagnosis, larger tumor size and male gender are negative prognostic factors (Ann Surg Oncol 2015;22:3990)
- Estimated 5 year and 10 year overall survival rates are 78 - 85% and 49 - 70% respectively (Ann Surg Oncol 2015;22:3990)
Case reports
- 25 year old man with hyperparathyroidism symptoms and parafibromin deficient parathyroid carcinoma due to a rare germline HRPT2 / CDC73 mutation (Endocr Pathol 2018;29:374)
- 59 year old man with calcitonin and calcitonin gene related peptide expressing parathyroid carcinoma (Endocr Patho 2019;30:168)
- 60 year old woman with intrathyroidal parathyroid carcinoma (Diagn Cytopathol 2018;46:47)
- 61 year old man with multiple endocrine neoplasm type 1 syndrome (Clin Exp Med 2018;18:585)
- 63 year old man with atypical thyroid nodule and symptomatic hypercalcemia (Front Endocrinol (Lausanne) 2018;9:641)
- 67 year old man with nonfunctioning parathyroid carcinoma (Surg Case Rep 2017;3:81)
Treatment
- En bloc resection with ipsilateral hemithyroidectomy and central lymphadenectomy (Nat Rev Endocrinol 2012;8:612, Ann Endocrinol (Paris) 2015;76:169)
- Benefits of adjuvant therapy (chemotherapy and radiotherapy) are unclear (Head Neck 2013;35:35)
Gross description
- Typically large, variably encapsulated, poorly circumscribed mass (Cancer 1973;31:600)
- Mean diameter of 3.4 cm and weight of 19.2 g (J Clin Pathol 2015;68:771)
- Cut section is usually firm, pinkish tan and lobular in appearance (Cancer 1973;31:600)
- Variable, sometimes indistinguishable from parathyroid adenoma (Turk Patoloji Derg 2015;31:80)
Frozen section description
- Distinction between parathyroid adenoma and carcinoma is often difficult to make on frozen section if the tumor does not show grossly evident invasion into adjacent structures
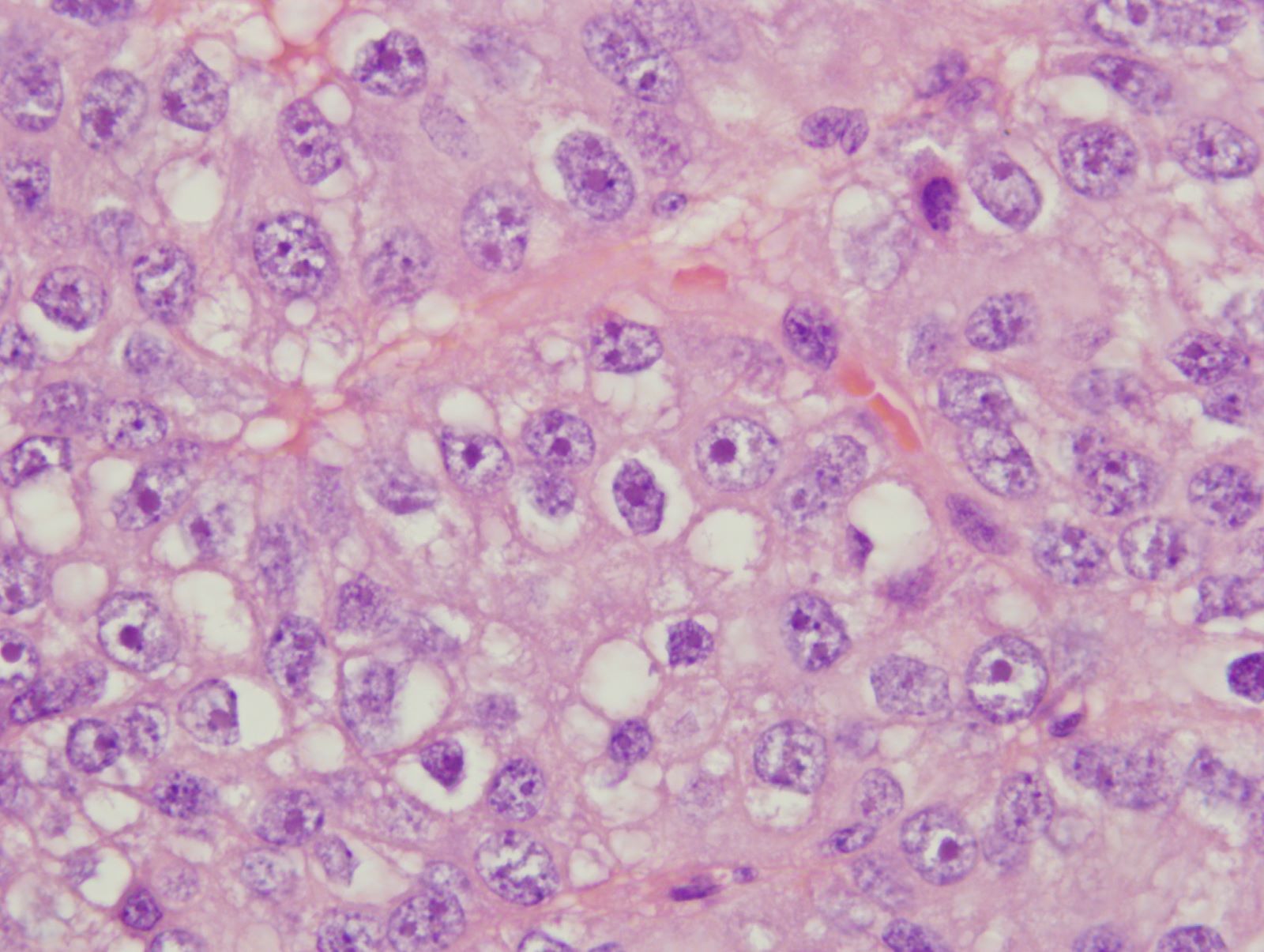
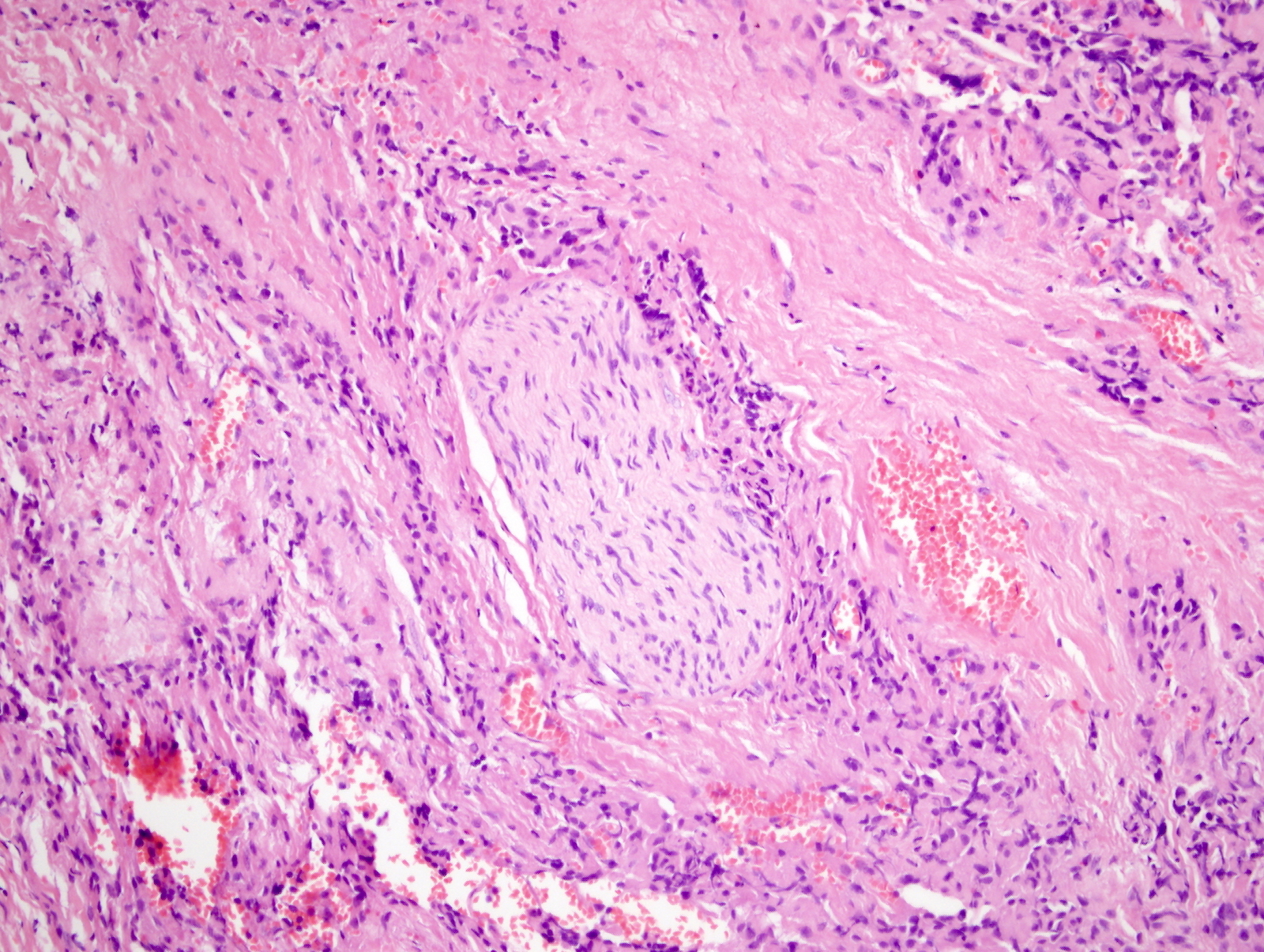
Microscopic (histologic) description
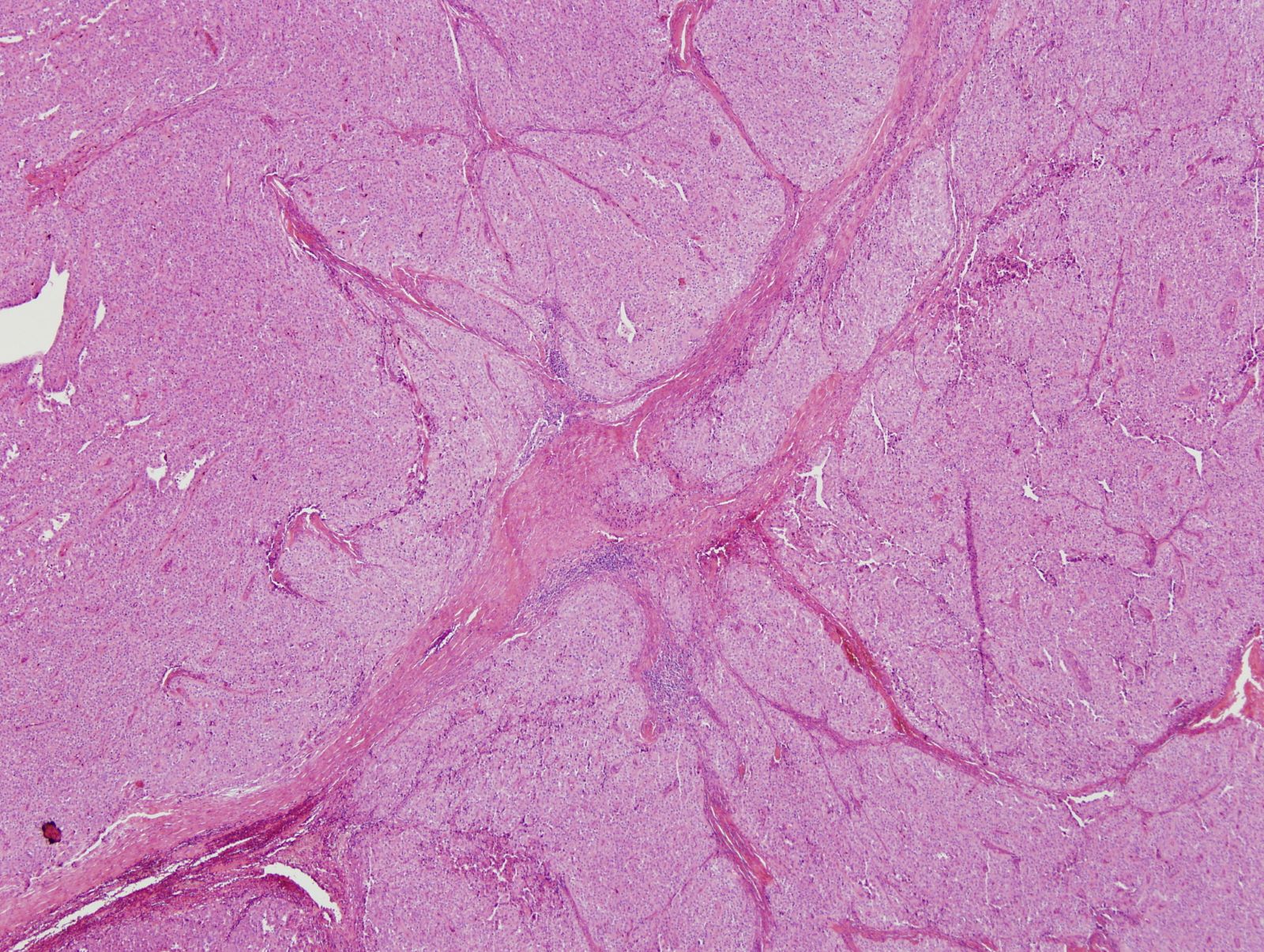
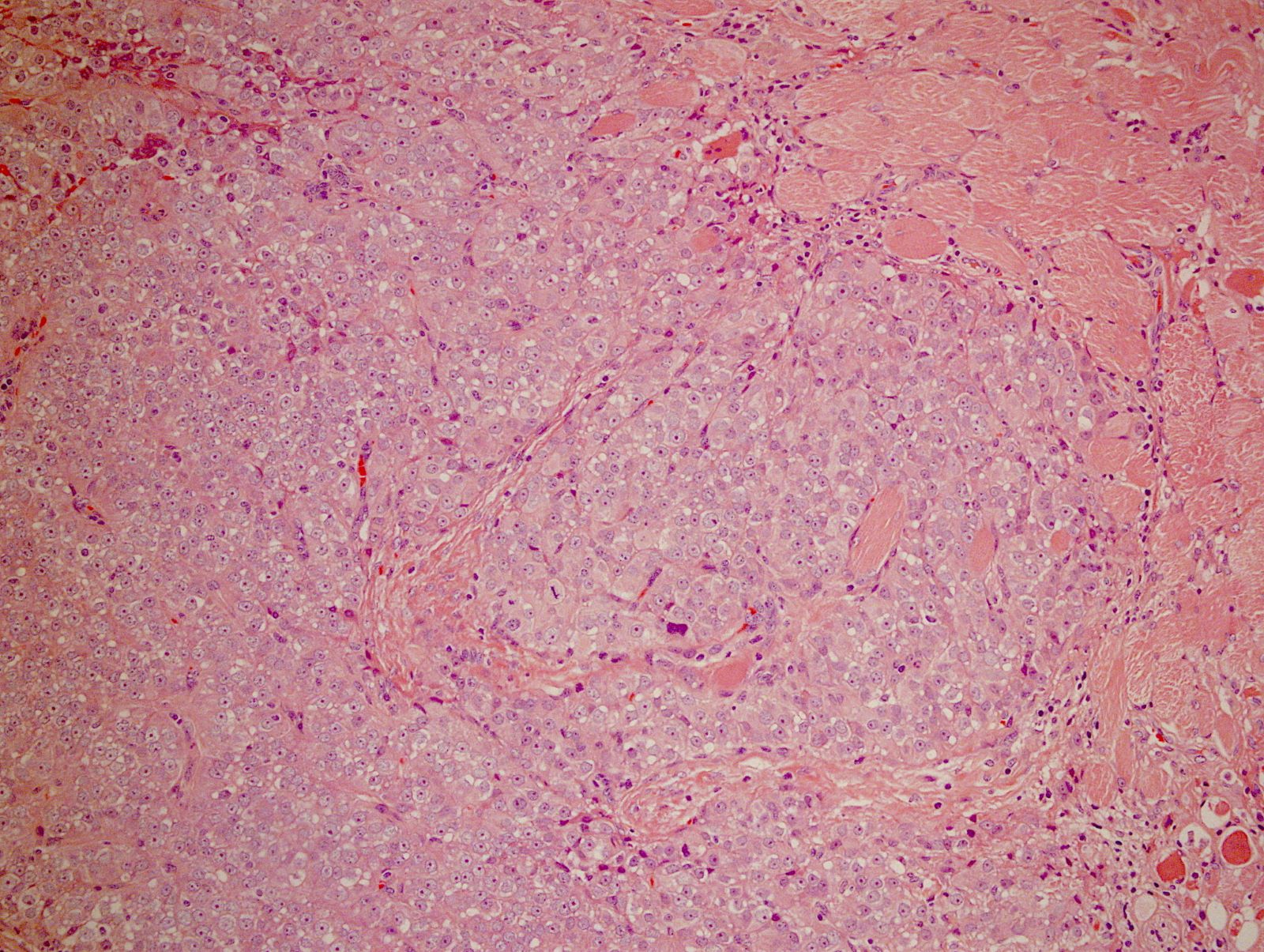
- Nodular and solid growth pattern is common
- Broad fibrous bands can be present
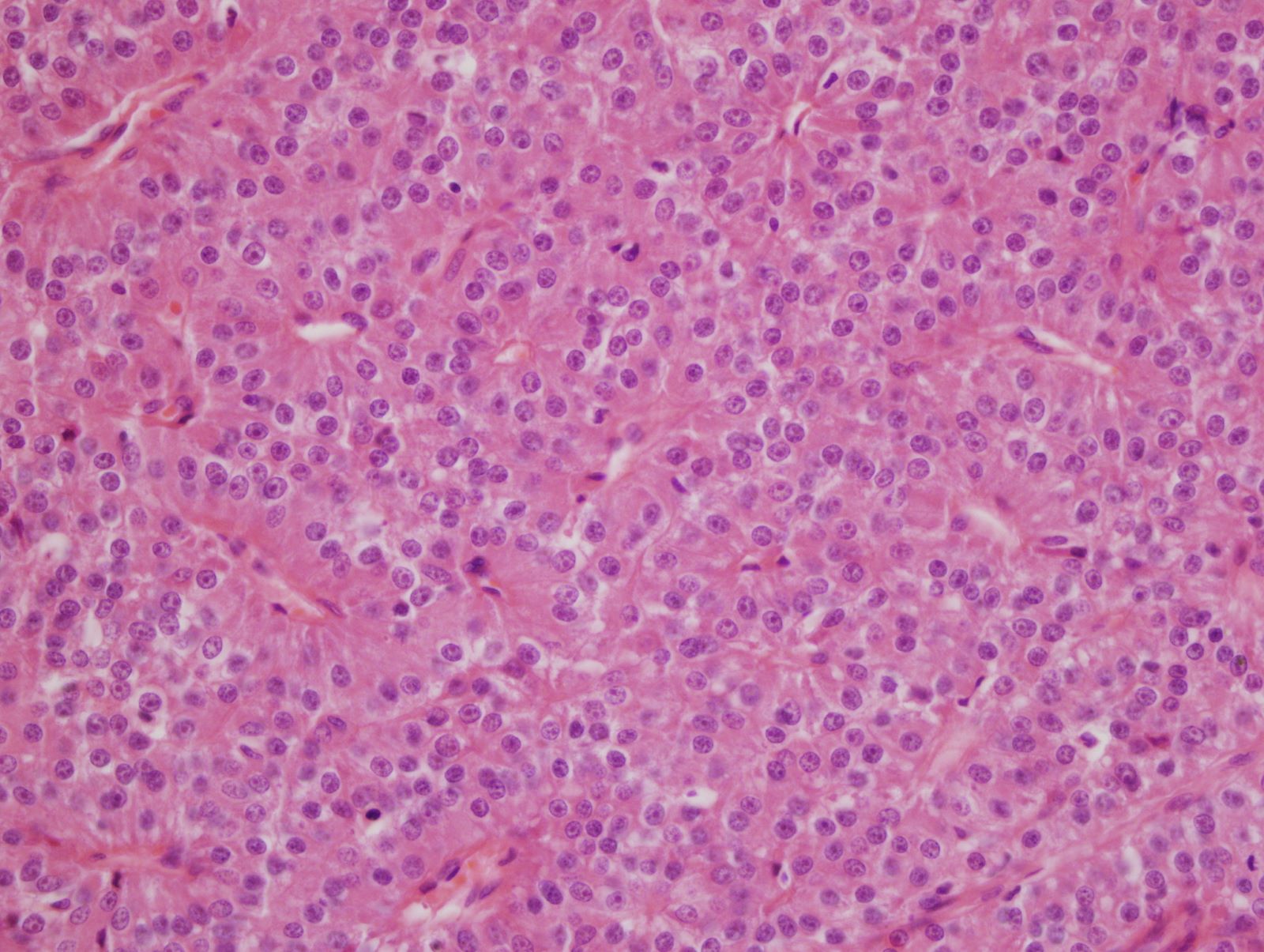
- Uniform cells or mild to moderate nuclear atypia
- Mostly composed of chief cells; however, oxyphil cells and transitional cells can also be seen
- Nuclear atypia, macronucleoli
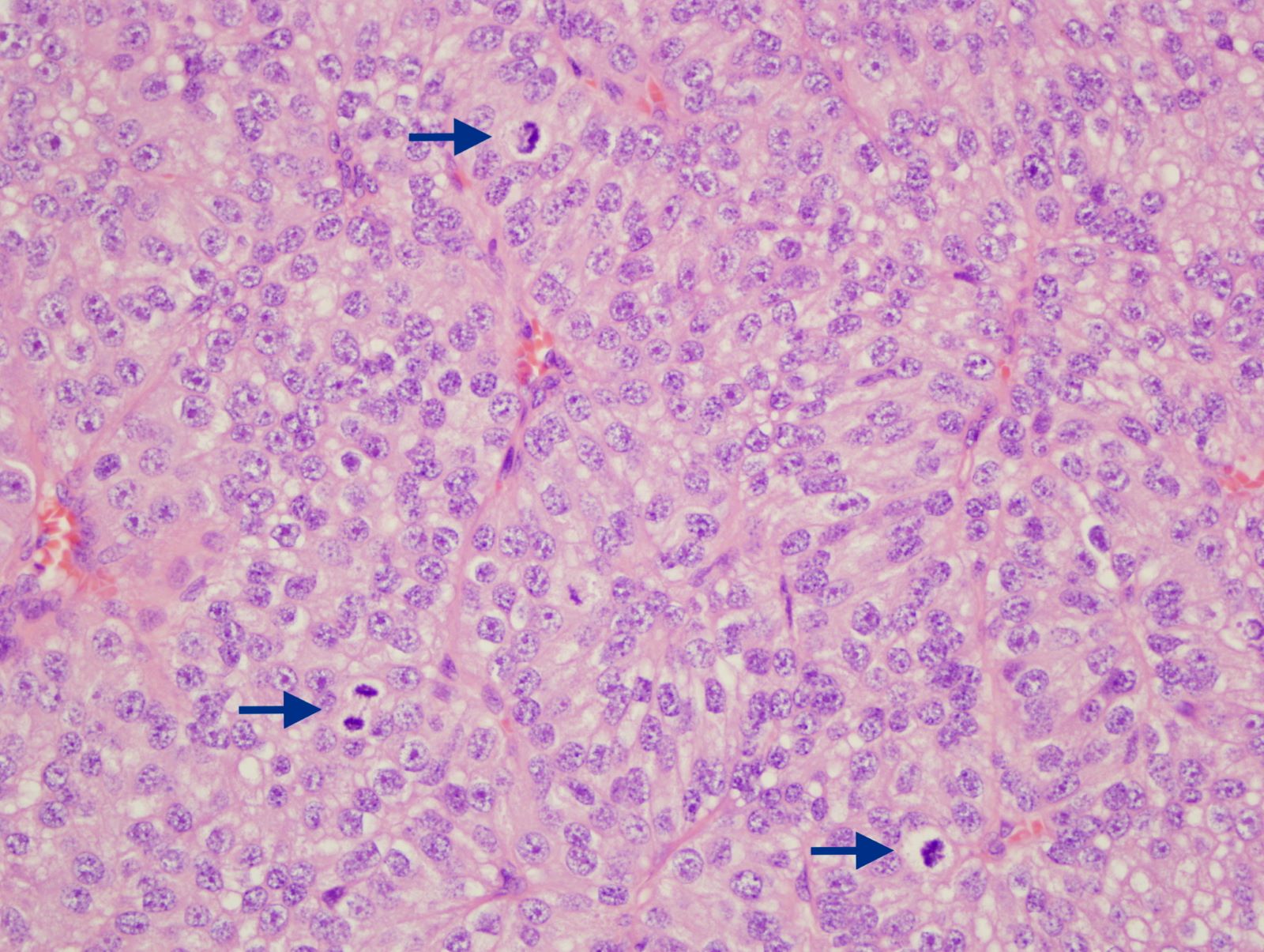
- Increased mitotic activity (> 5/10 mm2) and atypical mitosis may be seen
- Necrosis can be present
- One of the following features is necessary for definitive diagnosis of parathyroid lesion malignancy (Endocr Pathol 2022;33:64):
- Angioinvasion (vascular invasion)
- Lymphatic invasion
- Perineural (intraneural) invasion
- Invasion of adjacent structures / organs
- Metastasis
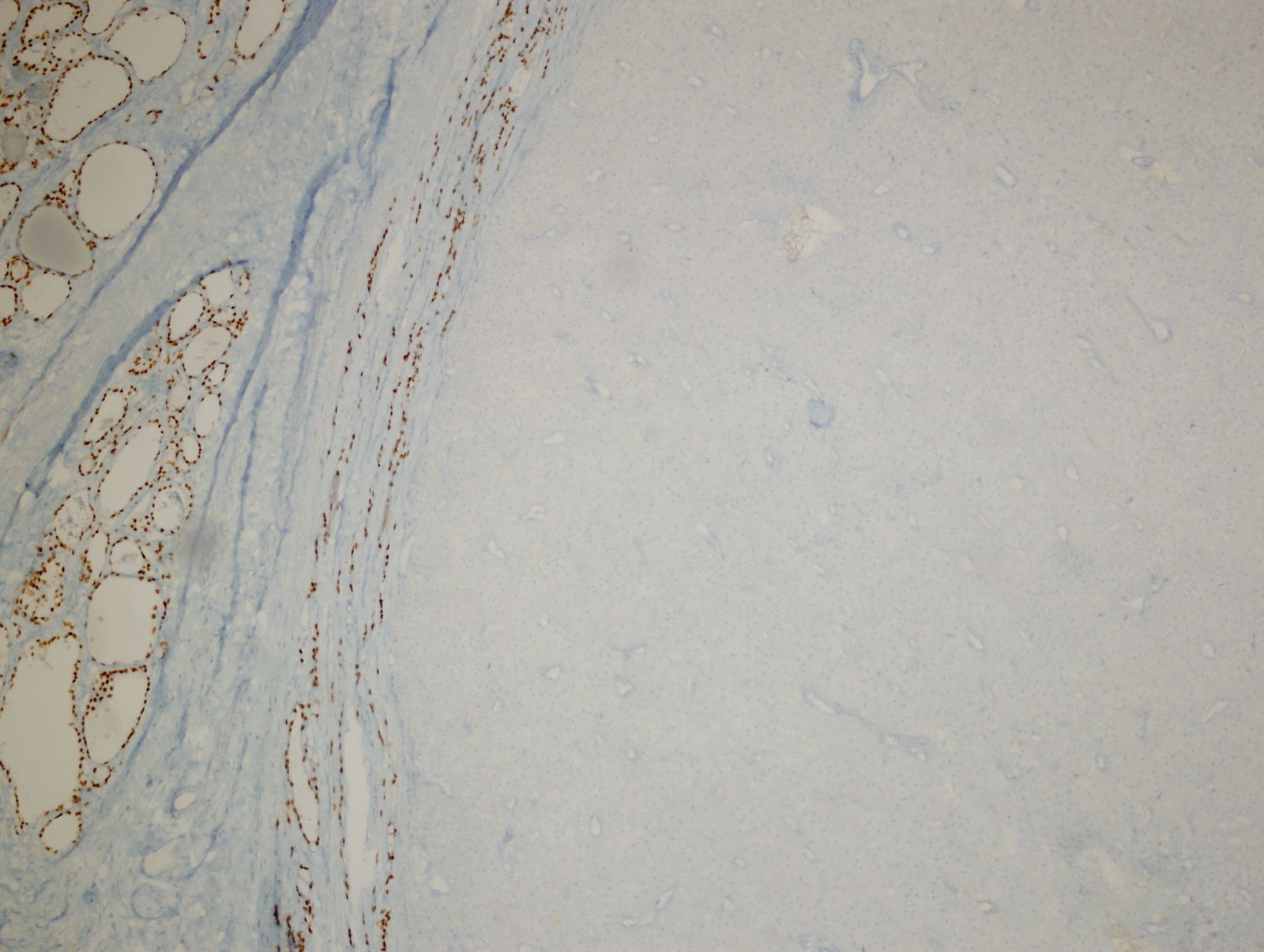
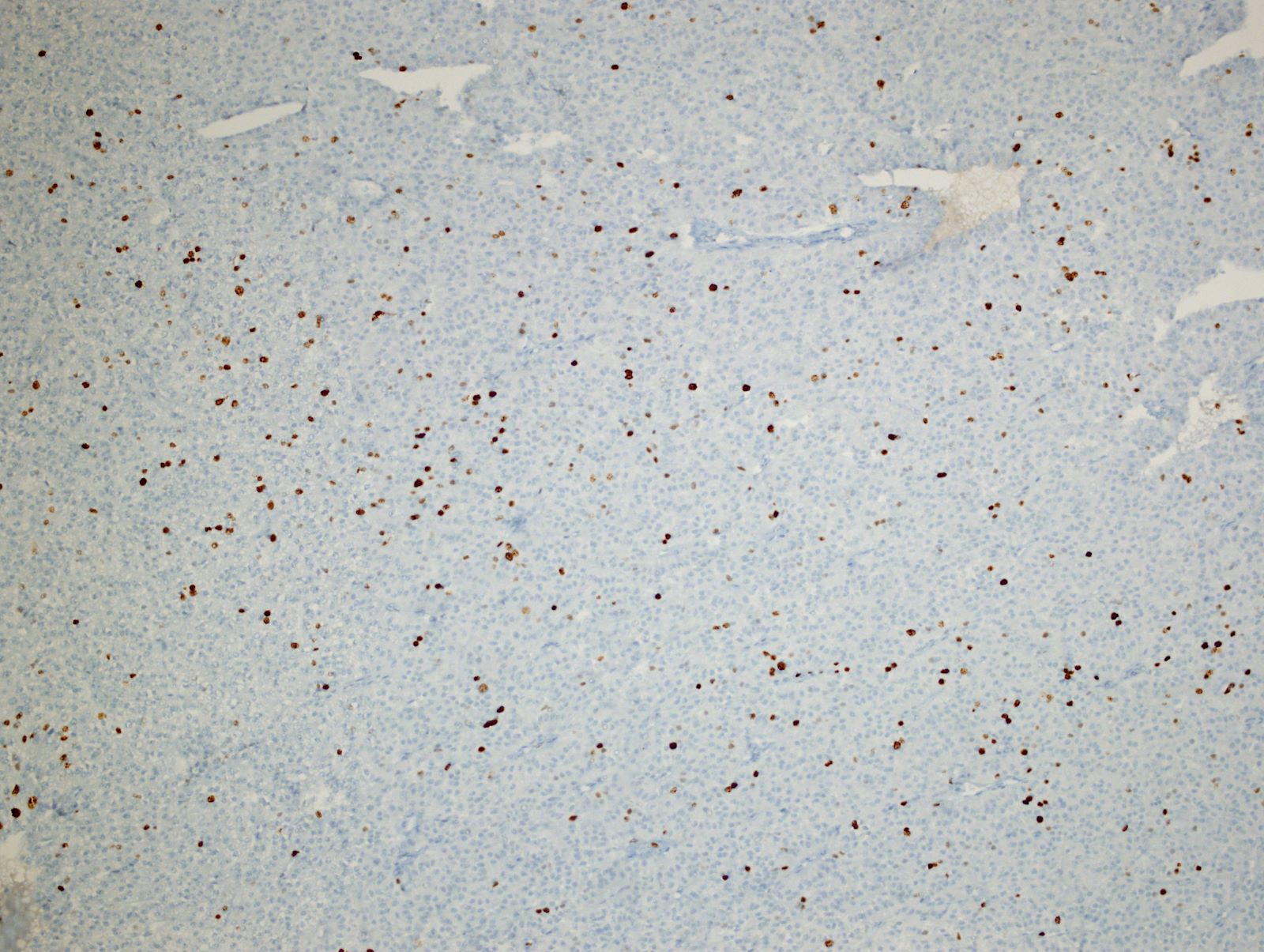
Microscopic (histologic) images
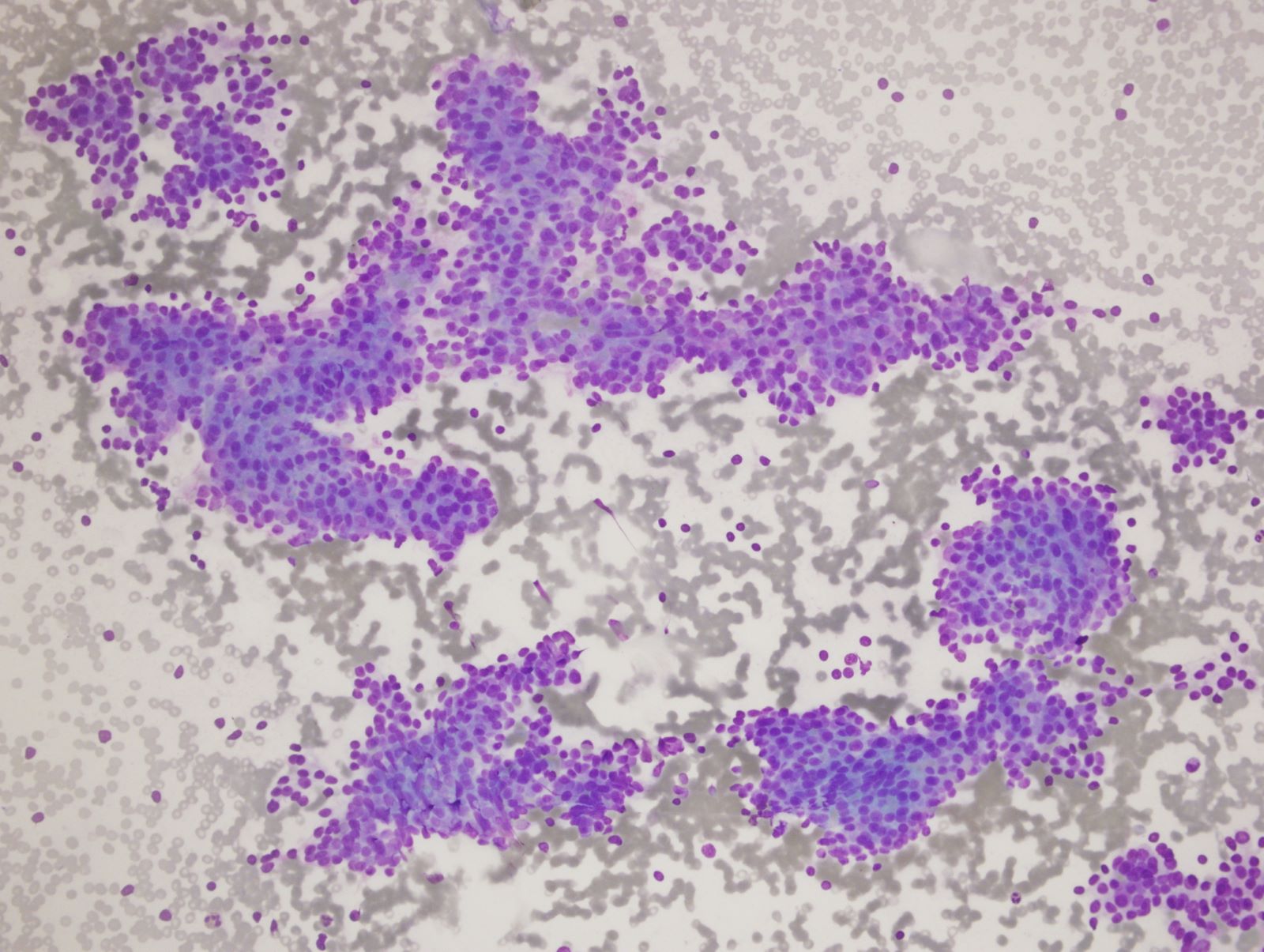
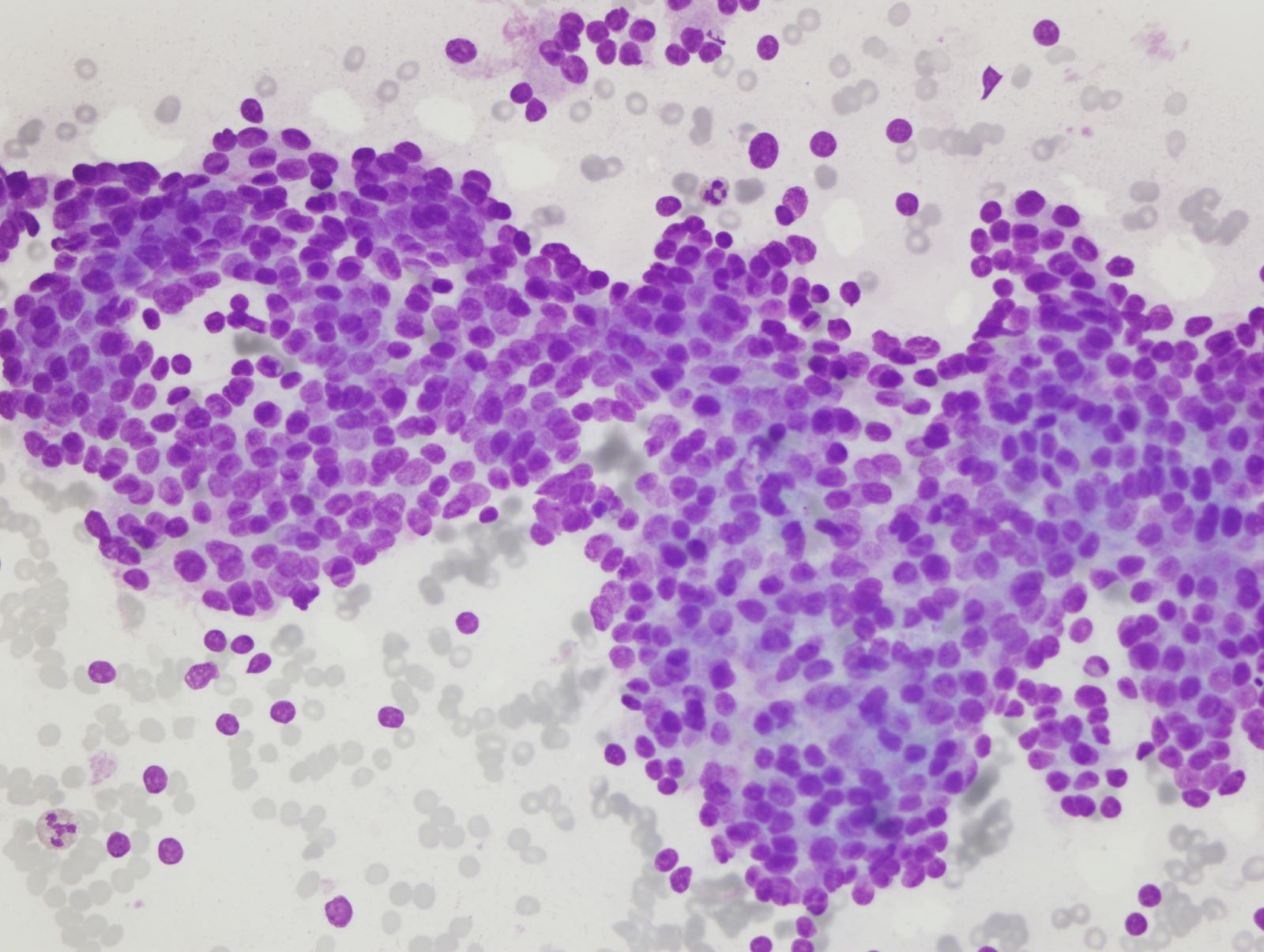
Cytology description
- Cellular, composed of cohesive sheets, ribbon-like cords
- Nuclei are uniform or show mild to moderate atypia
- Coarsely granular chromatin pattern
- Prominent nucleoli
- Cytoplasm is moderately abundant and granular
- Distinction between parathyroid carcinoma and adenoma is extremely difficult to make on cytology; nuclear pleomorphism, prominent macronucleoli, enlarged uniform hyperchromatic nuclei, mitotic figures favor carcinoma (Diagn Cytopathol 2016;44:688)
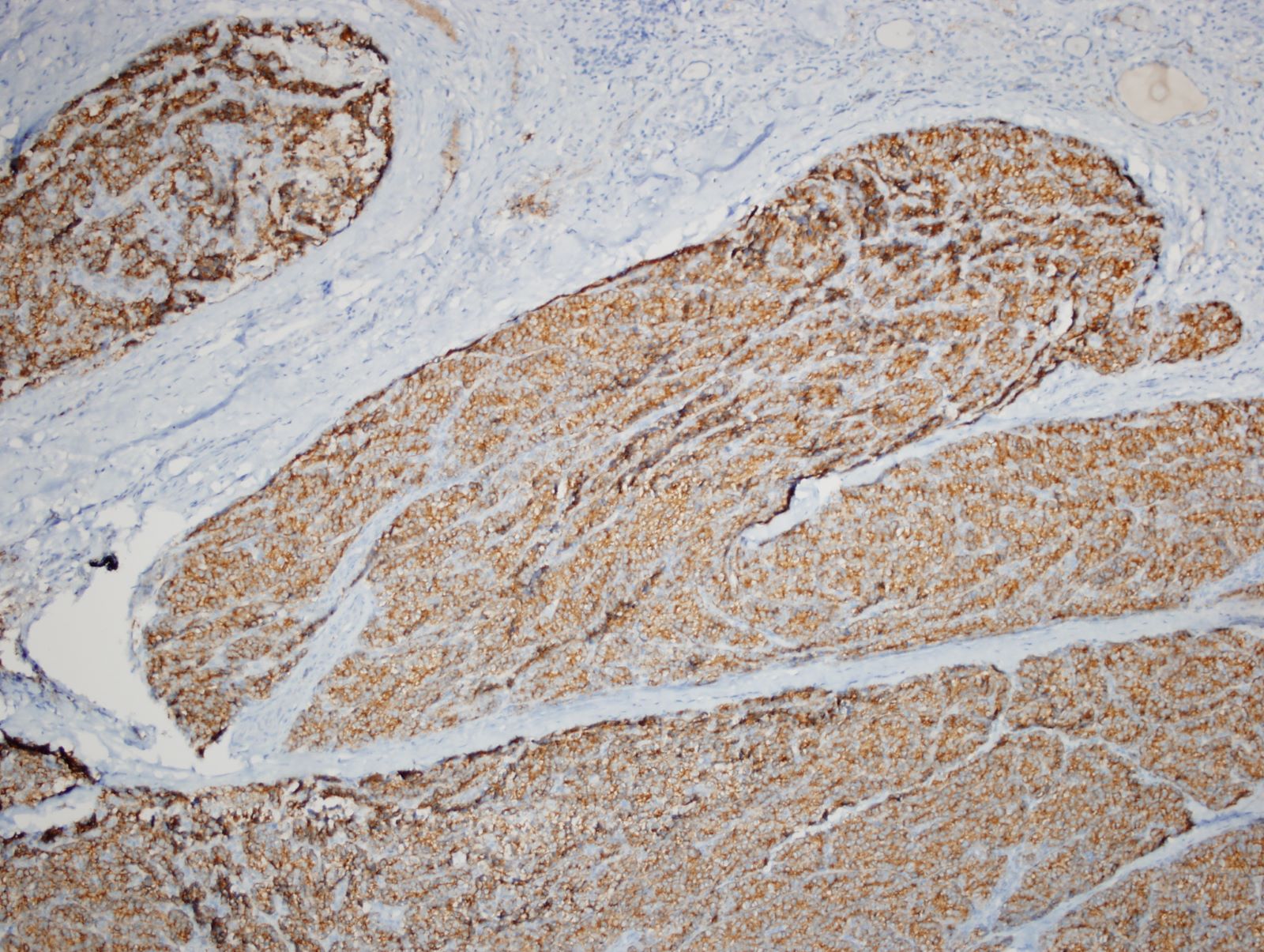
Positive stains
- Parathyroid specific markers: PTH, PTH related peptide, GATA3, GCM2 (Endocr Pathol 2018;29:113)
- Broad neuroendocrine markers: chromogranin A, synaptophysin
- Cytokeratins (Endocr Pathol 2018;29:113)
- CAM 5.2 is the most useful keratin for neuroendocrine tumors
- Keratin 14 may be absent in oxyphil parathyroid carcinoma
- Polyclonal PAX8 may be positive (42 - 83%) but monoclonal PAX8 is negative in parathyroid lesions (Am J Surg Pathol 2011;35:816, Mod Pathol 2011;24:751, Endocr Pathol 2022;33:64)
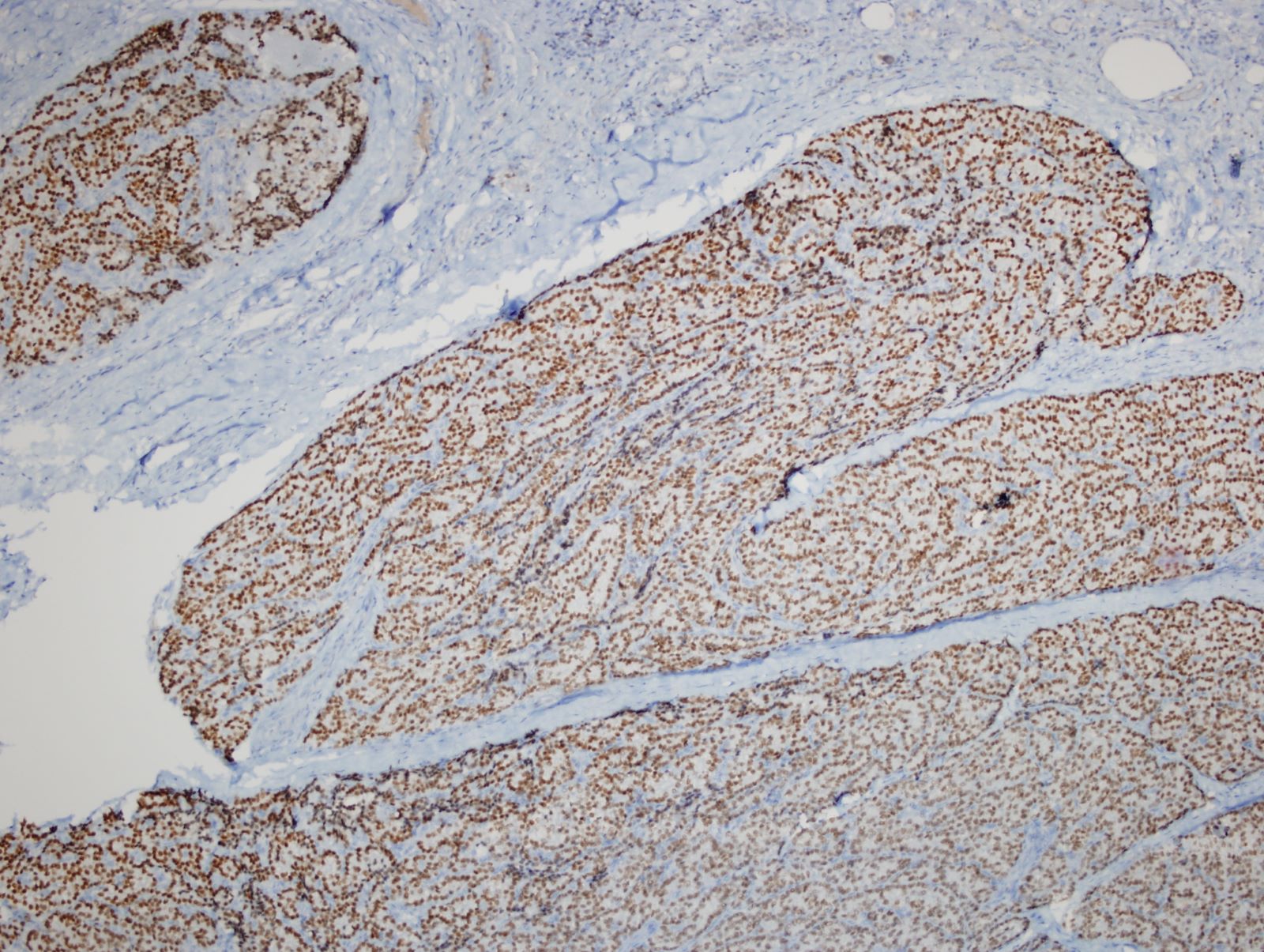
- Ki67 is usually elevated > 5% (Endocr Pathol 2022;33:64)
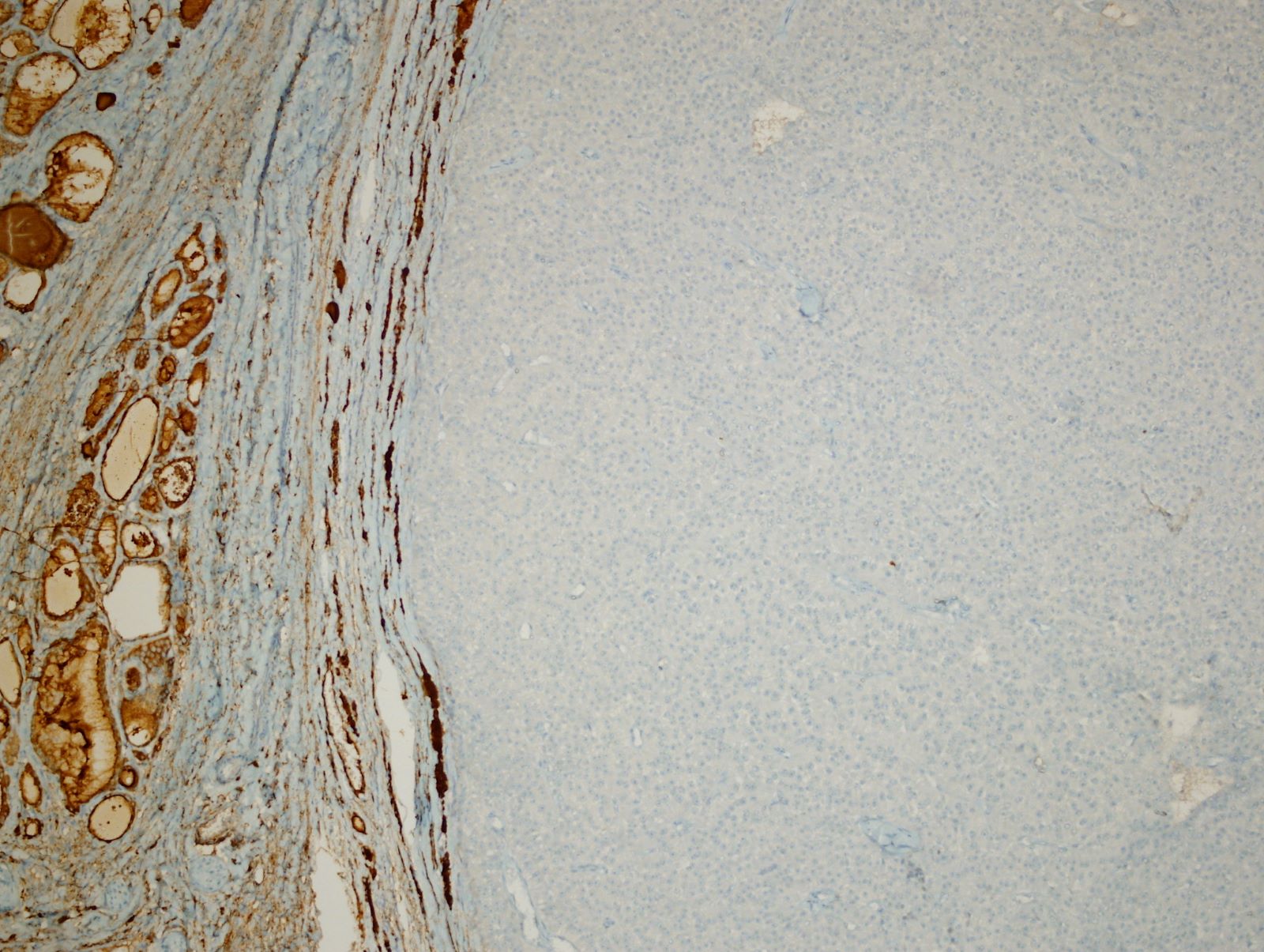
Negative stains
- Thyroid specific markers: TTF1, thyroglobulin (Endocr Pathol 2018;29:113)
- Calcitonin and calcitonin gene related peptide (usually) (Endocr Patho 2019;30:168)
- p27 (CDKN1B): absent or decreased expression (Endocr Pathol 2018;29:113)
- Rb, MDM2, BCL2, APC: often loss observed (Endocr Pathol 2018;29:113, Endocr Pathol 2022;33:64)
- Parafibromin: often loss observed (Endocr Pathol 2018;29:113)
Molecular / cytogenetics description
- HRPT2 (CDC73) mutation (tumor suppressor gene, 1q21-q31, encodes parafibromin) is strongly associated with familial and sporadic parathyroid carcinoma but is uncommon in adenomas, except in the setting of HPT JT (Endocrinol Metab Clin North Am 2017;46:405, N Engl J Med 2003;349:1722, Turk Patoloji Derg 2015;31:80, Mod Pathol 2011;24:S78, Endocr Pathol 2022;33:64)
- 15% with HPT JT (caused by germline HRPT2 inactivating mutation) develop parathyroid carcinoma
- Inactivating mutation of HRPT2 is found in > 70% cases of parathyroid carcinoma
- Complete nuclear loss of parafibromin has shown strong association with HRPT2 mutation; nucleolar loss of parafibromin is an abnormal finding and requires further molecular testing (Endocr Pathol 2022;33:64)
- Cyclin D / CCND1 (11q13, parathyroid adenoma oncogene) encodes cyclin D1 which is overexpressed in some parathyroid carcinomas (J Clin Pathol 2015;68:771)
- MEN1 mutation (tumor suppressor gene, 11q13) has been reported in rare cases (Clin Endocrinol (Oxf) 2007;67:370)
- Additional molecular alterations (nonspecific) also found (CaSR, EZH2, RIZ1, RASSF1, GSK3B, APC, PRUNE2, HIC1, GSK3β, mTOR, MLL2, THRAP3, PIK3CA, WT1) (J Clin Pathol 2015;68:771)
Videos
Parathyroid pathology
Sample pathology report
- Right neck, mass, excision:
- Parathyroid carcinoma, oxyphilic type (see comment)
- Comment: There is a cellular malignant tumor with thyroid gland and striated muscle invasion. Tumor cells characterized by eosinophilic cytoplasm, nuclear enlargement with distinctive coarse chromatin and prominent nucleoli. There are 12 mitoses per 10 mm2, some of which show atypical features. Lymphatic and vascular invasion are also seen. Immunohistochemically, the tumor cells show strong expression of PTH, GATA3, chromogranin A and synaptophysin while they are negative with thyroglobulin, TTF1, PAX8, CEA and tyrosine hydroxylase. Ki67 index is 16%. Morphological and immunohistochemical features strongly support parathyroid carcinoma, oxyphilic type. Complete nuclear parafibromin loss is detected, which correlates with HRPT2 (CDC73) mutation and also parafibromin deficient parathyroid neoplasm.
Differential diagnosis
- Parathyroid adenoma:
- Benign parathyroid neoplasm composed of chief cells, oncocytes or transitional oncocytes or an admixture of these cell types
- Usually asymptomatic, no palpable mass and grossly smaller than parathyroid carcinoma
- Serum calcium level is elevated but often not as high as carcinoma
- Scattered mitosis may be seen but high mitotic rate is rare and usually lacks atypical mitosis
- Lack of definitive diagnostic features of parathyroid carcinoma (invasion or metastases)
- Atypical parathyroid tumor:
- Rare type of parathyroid tumor which exhibits some of the features of parathyroid carcinoma such as cytological atypia, mitotic activity, fibrous bands, adherence to adjacent structures, trabecular growth pattern, tumor cells within the capsule
- Lack of definitive diagnostic features of parathyroid carcinoma (invasion or metastases)
- Ancillary immunohistochemical markers could be used for differential diagnosis of parathyroid adenoma and carcinoma (Ki67, parafibromin, galectin3, PGP9.5, E-cadherin, 5-hmC, hTERT, p53, Rb, BCL2, p27, MDM2 and APC) (Endocr Pathol 2018;29:113, Endocr Pathol 2022;33:64)
- Well differentiated thyroid carcinoma:
- Well differentiated thyroid malignancy arising from follicular epithelial cells
- Papillary or follicular growth pattern, may have colloid, typical nuclear features for papillary carcinoma, lacks well defined cytoplasmic membrane
- Positive for TTF1, thyroglobulin; negative for PTH, GATA3 (Endocr Pathol 2018;29:91)
- PAX8 expression can overlap between thyroid and parathyroid tumors and should not be considered as a reliable marker for differential diagnosis
- Differentiated high grade thyroid carcinoma:
- Invasive high grade malignancy arising from follicular epithelial cells with necrosis or high mitotic count ≥ 5/10 mm2 (Endocr Pathol 2022;33:27)
- Growth pattern and nuclear features similar to well differentiated tumors; papillary architecture is more common
- Positive for TTF1, thyroglobulin; negative for PTH, GATA3 (Endocr Pathol 2022;33:27)
- Poorly differentiated thyroid carcinoma:
- Follicular cell neoplasm that shows limited evidence of follicular differentiation
- Solid, trabecular or insular growth pattern and lacks well defined cytoplasmic membrane
- Positive for TTF1, thyroglobulin (reduced expression); negative for PTH, GATA3 (Endocr Pathol 2018;29:91)
- Medullary thyroid carcinoma:
- Malignant neuroendocrine tumor derived from C cells of thyroid
- Also lacks colloid and is positive for neuroendocrine markers and keratin
- Positive for calcitonin, CEA, TTF1; negative for PTH and GATA3 (Endocr Pathol 2018;29:91)
- Paraganglioma:
- Nonepithelial tumor originating from neural crest derived paraganglion cells
- Also positive for neuroendocrine markers and GATA3 (some parasympathetic paraganglioma can be negative for chromogranin A) (Arch Pathol Lab Med 2014;138:182)
- Negative for keratin and PTH; positive for tyrosine hydroxylase (can be negative in parasympathetic paraganglioma) (Endocr Pathol 2018;29:91, Endocr Pathol 2018;29:113)
- Metastatic neuroendocrine tumors:
- Clinical history, radiological and laboratory findings are important
- Usually positive for neuroendocrine markers and keratin (Cancer Cytopathol 2016;124:871)
- TTF1 (lung but also positive in medullary carcinoma), CDX2 (gastrointestinal), p16 (cervical), ISL1 and PDX1 (pancreatic) useful for detection of primary tumor site (Cancer Cytopathol 2016;124:871)
Additional references
Practice question #1
Practice answer #1
D. Perineural invasion of tumor cells is diagnostic of malignancy for parathyroid neoplasm. Although the other options are also atypical features and commonly seen in parathyroid carcinoma, based on the 2022 WHO classification one of the following features is required for definitive malignancy diagnosis of the parathyroid lesion: angioinvasion (vascular invasion), lymphatic invasion, perineural (intraneural) invasion, invasion of adjacent structures / organs, metastasis (Endocr Pathol 2022;33:64).
Comment Here
Reference: Parathyroid carcinoma
Comment Here
Reference: Parathyroid carcinoma
Practice question #2
- Which of the following markers is recommended for atypical parathyroid tumors and parathyroid carcinoma in routine practice and may also be associated with the risk of tumor recurrence?
- Isocitrate dehydrogenase 1 (IDH1)
- Menin
- Parafibromin
- SMARCB1 / INI1
- Succinate dehydrogenase B (SDHB)
Practice answer #2
C. Parafibromin. Parafibromin is the protein encoded by the tumor suppressor gene HRPT2 (CDC73). Complete loss of nuclear parafibromin immunoreactivity indicates biallelic CDC73 inactivation and requires routine germline CDC73 mutation testing. Based on the 2022 WHO classification, complete nuclear loss of expression of parafibromin is considered parafibromin deficiency. Parafibromin deficient parathyroid neoplasms may show metachronous disease in the other glands and increased recurrence (Endocr Pathol 2022;33:64)
Comment Here
Reference: Parathyroid carcinoma
Comment Here
Reference: Parathyroid carcinoma