Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description (Courtesy of Shahid Islam, M.D., Ph.D.) | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Xu B. Papillary thyroid carcinoma overview. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidpapillary.html. Accessed April 27th, 2024.
Definition / general
- Papillary thyroid carcinoma (PTC) is the most common type of thyroid carcinoma, defined by a set of distinctive nuclear features, including:
- Change of nuclear size and shape: nuclear enlargement, elongation and overlapping
- Chromatin characteristics: chromatin clearing, margination and glassy nuclei
- Nuclear membrane irregularity: irregular nuclear contour, nuclear groove and nuclear pseudoinclusion
- There are 15 variants of papillary thyroid carcinoma, including prototypic conventional / classic papillary thyroid carcinoma, as per the 2017 WHO classification (IARC: WHO Classification of Tumours of Endocrine Organs (Medicine), 4th Edition, 2017)
Essential features
- Diagnosis is based on nuclear features
- Subtyping (i.e., variant) is based on a combination of architecture / pattern, cytologic features, size and encapsulation
- BRAFV600E is the most frequent mutation, particularly in tall cell and classic variants
ICD coding
Epidemiology
- Predominant form of thyroid carcinoma, accounting for 80 - 93% in contemporary series (IARC: CI5 Cancer Incidence in Five Continents [Accessed 30 September 2019])
- There is a growing number of papillary thyroid carcinoma in the last 15 - 20 years due to increasing recognition of thyroid nodules on imaging (ultrasound and CT), sometimes referred as thyroid cancer epidemics; most of these tumors are of low risk (N Engl J Med 2015;373:2389, N Engl J Med 2016;375:614)
- Female predominant with a F:M ratio of ~3:1 (CA Cancer J Clin 2018;68:7)
- Most common histological variants are classic PTC, microcarcinoma and follicular variant papillary thyroid carcinoma
- Occult tumors in 6% at autopsy (1 - 10 mm), 46% multicentric, 14% with nodal metastases (Am J Clin Pathol 1988;90:72)
- Occult tumors in up to 24% with other thyroid disease but with male predominance (Mod Pathol 1996;9:816)
Sites
- Predominantly affects thyroid gland proper
- May also occur in thyroglossal duct (J Med Case Rep 2008;2:42), lingual thyroid, and other ectopic thyroid tissue, e.g., struma ovarii (Endocrine 2016;51:189, Case of the Week #465)
Etiology
- Ionizing radiation before age 20 (for acne, tonsillitis, tinea capitis, enlarged thymus) (Surgery 1991;110:691)
- Post Chernobyl (particularly children) or after exposure to nuclear explosions at Marshall Islands (Endocr Pathol 2006;17:307, J Epidemiol 2003;13:99)
- Hashimoto thyroiditis, possibly (Cancer 1995;76:2312)
- Familial adenomatous polyposis, particularly the cribriform modular variant
- Is familial in 4.5%, similar prognosis as sporadic disease (Surgery 2009;145:100)
Clinical features
- Usually presents as painless thyroid nodule or mass in neck or cervical node; usually cold on scan
- At presentation, 67% in thyroid only, 13% in thyroid and cervical nodes and 20% in nodes only
- Nodal involvement is often not clinically apparent due to small size and similar consistency
Diagnosis
- Diagnosis is typically rendered using preoperative fine needle aspiration cytology based on the presence of typical cytologic features
- Molecular testing of cytologic aspirates may assist in preoperative diagnosis
- Diagnosis in resection specimen is based primarily on nuclear features, including alteration of nuclear size and shape, chromatin pattern and nuclear membrane irregularity
- Further subtyping (i.e., variant) is based on a combination of architecture (e.g., solid, classic, follicular and cribriform morular variant), cytologic features (e.g., oncocytic, tall cell, hobnail and columnar cell variant), size (e.g., microcarcinoma) and encapsulation / infiltration (e.g., encapsulated variant, encapsulated follicular variant and infiltrative follicular variant)
Radiology images
Prognostic factors
- Overall excellent prognosis with a life expectancy similar to general population: 5 year, 10 year and 20 year survival is 96%, 93% and > 90% respectively (IARC: WHO Classification of Tumours of Endocrine Organs (Medicine), 4th Edition, 2017)
- Disease specific survival is close to 100% if under age 20
- Cervical nodal involvement does NOT affect prognosis
- 5 - 20% have local recurrences, 10 - 15% have distant metastases (lung, bones, CNS)
- Adverse prognostic pathologic features recognized by the American Thyroid Association (ATA) Management Guidelines include (Thyroid 2016;26:1)
- Intermediate risk: tall cell / hobnail / columnar cell variant, vascular invasion, pN1 disease with > 5 positive lymph nodes and the largest metastatic focus < 3 cm in greatest dimension, microscopic extrathyroidal extension (perithyroidal fibroadipose tissue)
- High risk: gross extrathyroidal extension (strap muscles and beyond), incomplete tumor resection, distant metastasis, pN1 with a metastatic focus ≥ 3 cm in largest dimension
- Elder age at diagnosis (≥ 55 years) is a poor prognostic factor, which has been included in the prognostic staging group of AJCC Cancer Staging Manual 8th edition (Amin: AJCC Cancer Staging Manual, 8th Edition, 2018)
- Progression to poorly differentiated thyroid carcinoma or anaplastic thyroid carcinoma infers a poor prognosis
Case reports
- 10 year old girl with cribriform morular variant (Rom J Morphol Embryol 2016;57:531)
- 40 year old man with a cystic neck mass (Medicine (Baltimore) 2019;98:e16659)
- 46 year old woman with recurrent tumor (Medicine (Baltimore) 2019;98:e15210)
- 46 year old woman with multifocal papillary thyroid carcinoma (Endocrinol Diabetes Metab Case Rep 2019 Mar 18 [Epub ahead of print])
- 56 year old man with follicular variant and multiple metastases (Med Arch 2016;70:314)
- 61 year old woman with tracheal invasion (Medicine (Baltimore) 2019;98:e17033)
- 63 year old woman with synchronous and metastatic papillary and follicular thyroid carcinomas (Endocr Pathol 2018;29:9)
- 69 year old woman with metastatic papillary thyroid carcinoma diagnosed by effusion cytology (Diagn Cytopathol 2018;46:204)
Treatment
- Based on ATA risk stratification (Thyroid 2016;26:1)
- High risk: total thyroidectomy and post operative radioactive iodine therapy
- Intermediate risk: subtotal / total thyroidectomy; postoperative radioactive iodine therapy should be considered and discussed with the patient
- Low risk (includes intrathyroidal encapsulated follicular variant and papillary thyroid carcinoma devoid of the aggressive features seen intermediate or high risk groups): lobectomy alone may be sufficient
- Very low risk (i.e., papillary microcarcinomas without clinically evident metastasis, local invasion or convincing cytologic evidence of aggressive disease): active surveillance may be considered as an alternative for surgical approach
- Other national guidelines (NCCI, European, Japanese) recommendations may differ from ATA
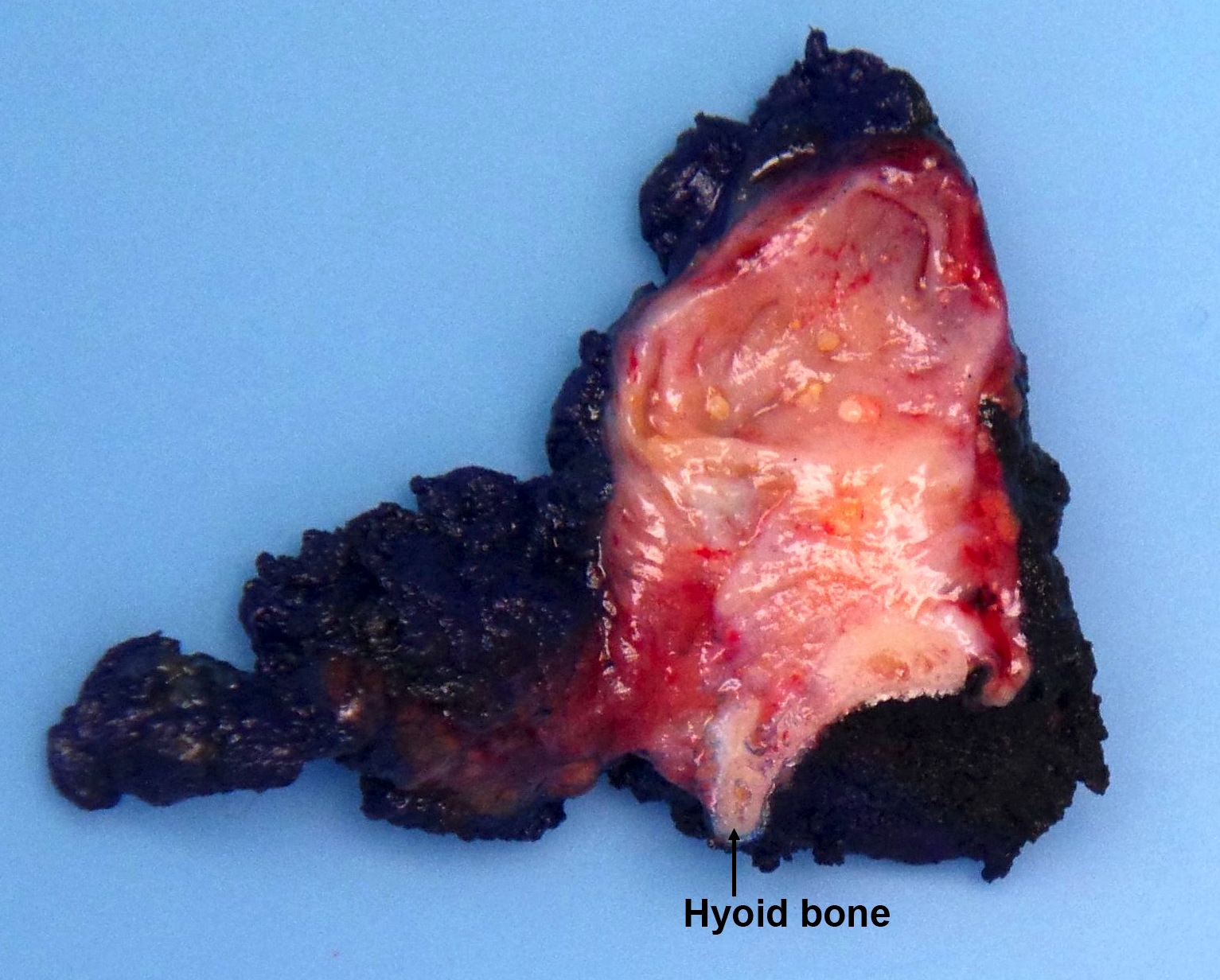
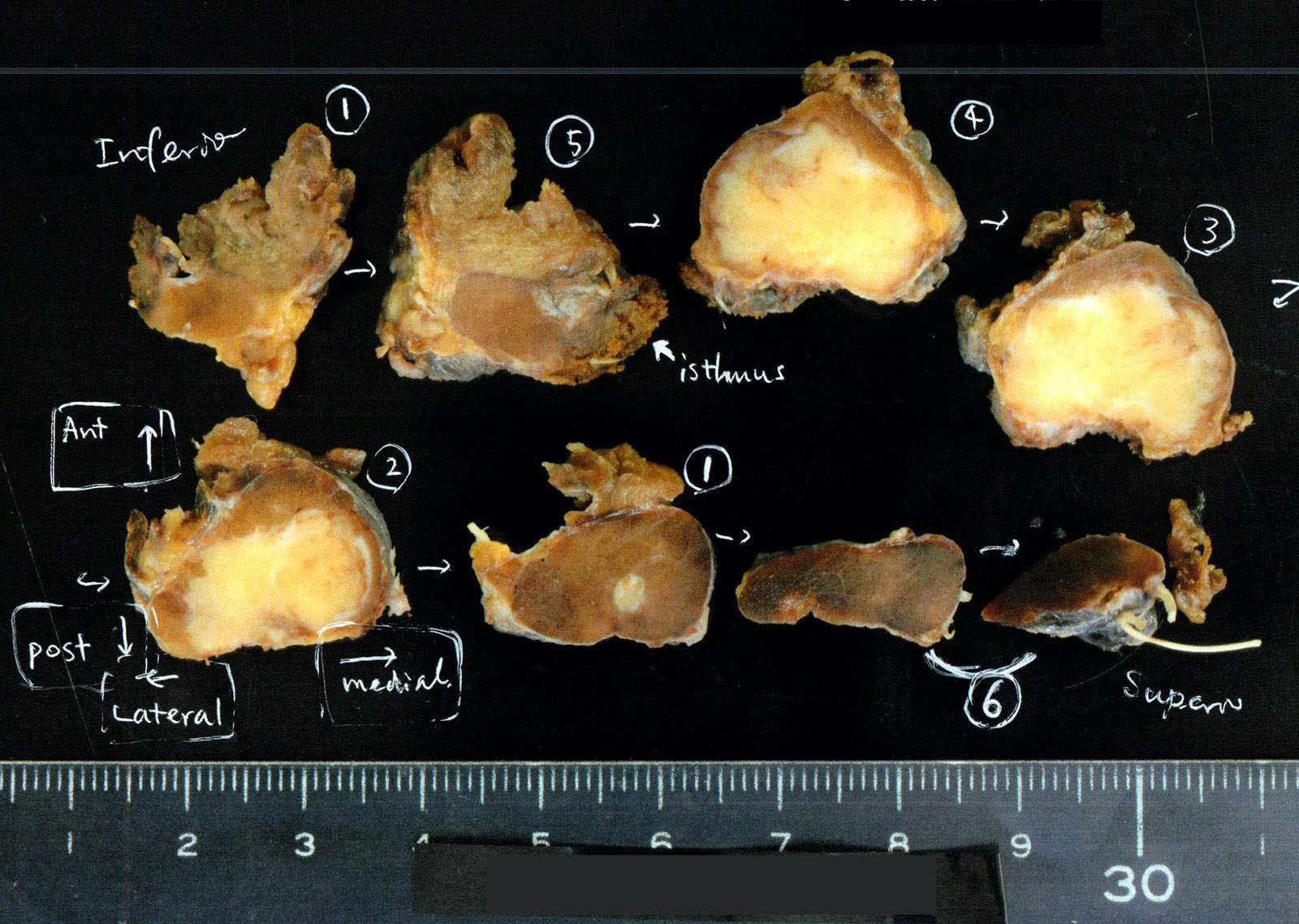
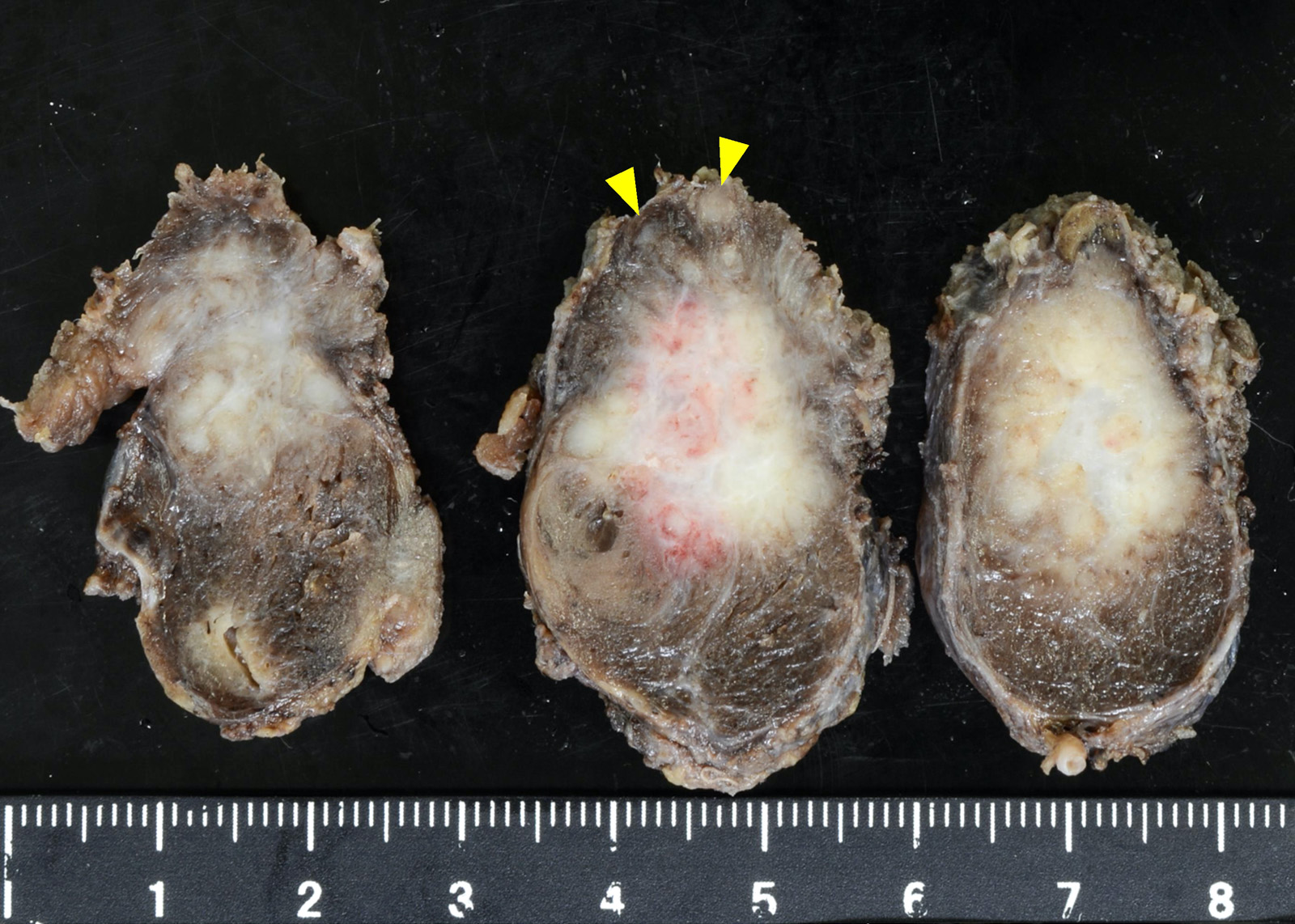
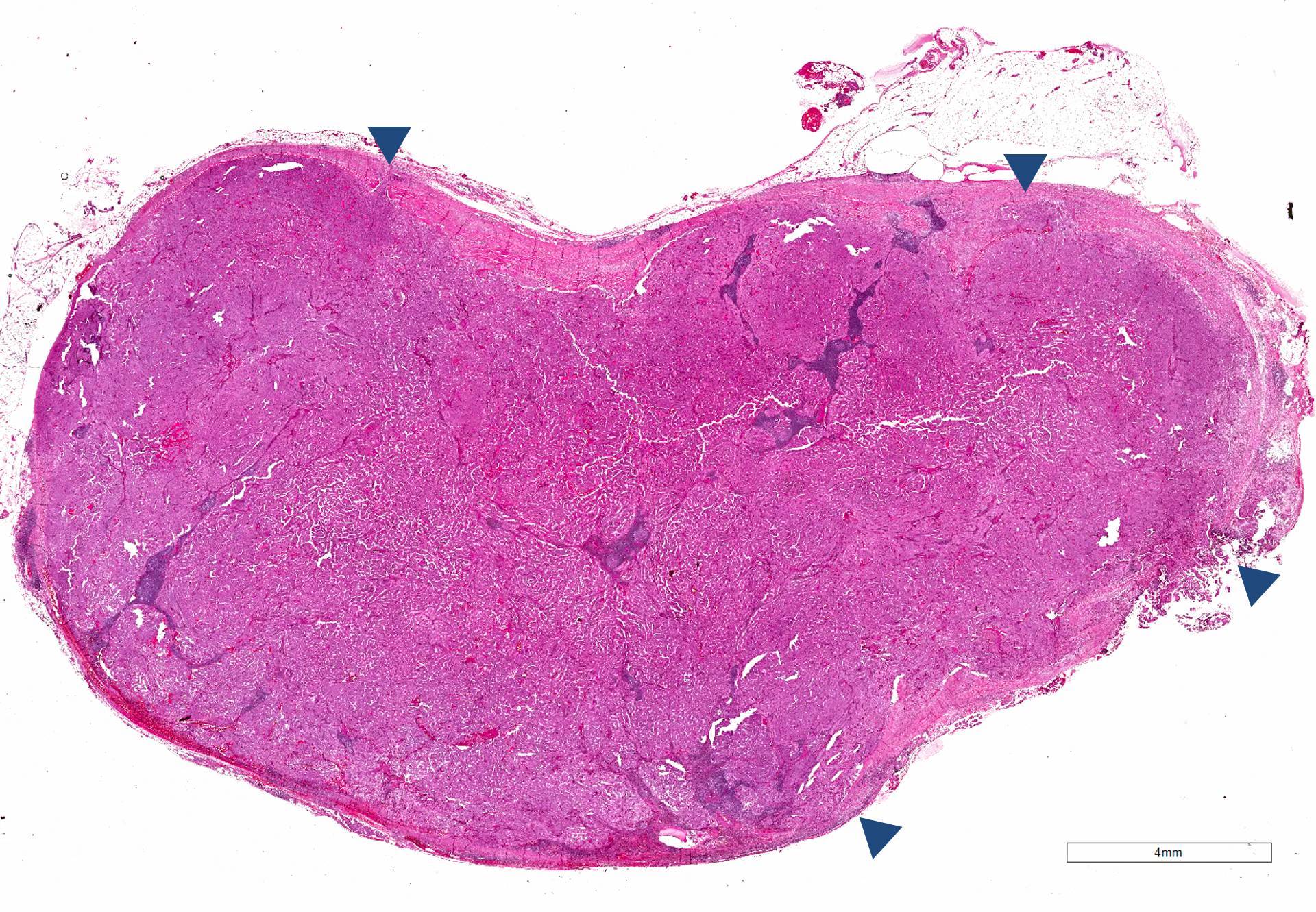
Gross description
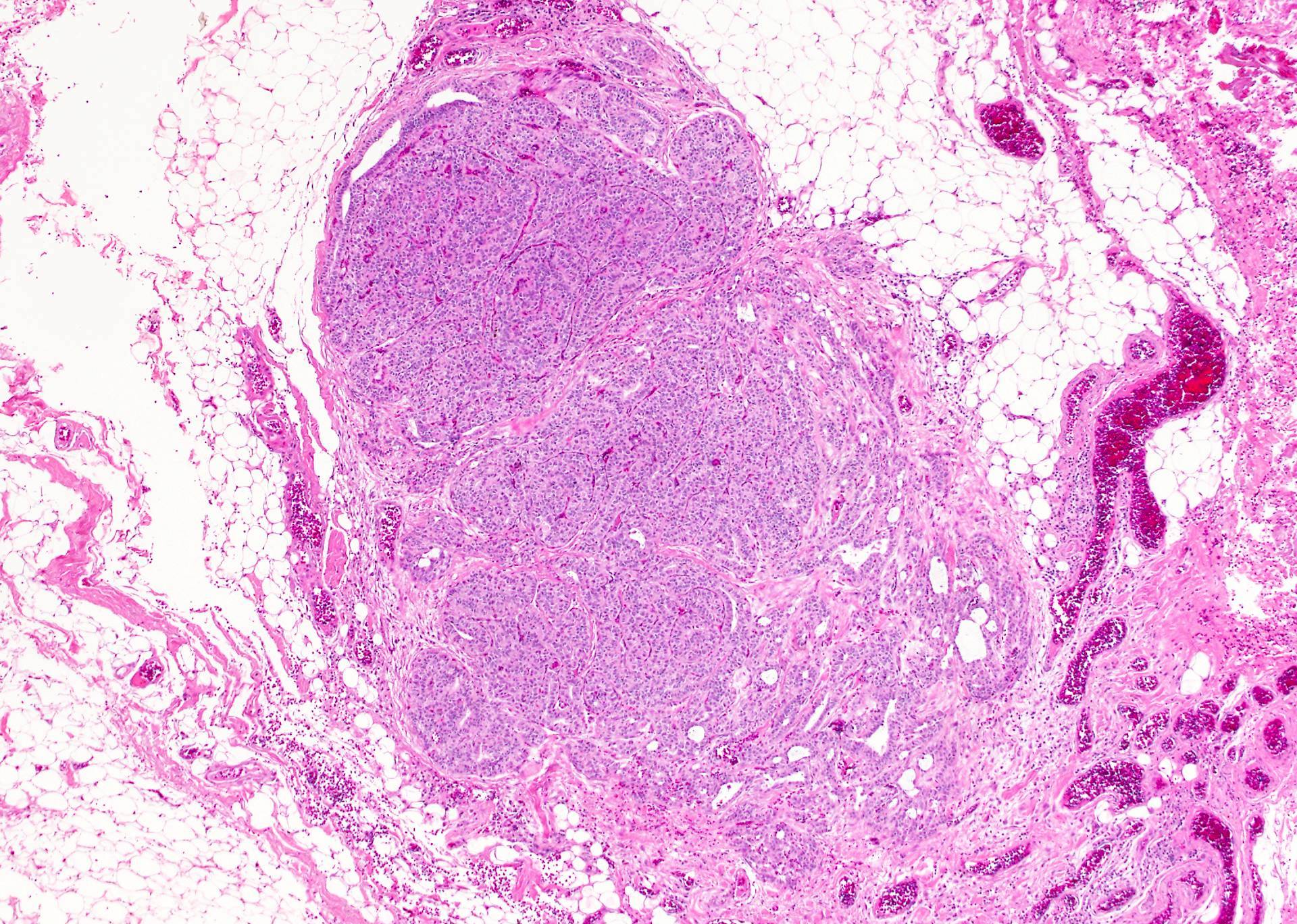
- Solid, white, firm, often multifocal (20%), encapsulated (10%) or infiltrative
- Variable cysts, fibrosis, calcification
- Extrathyroidal extension can be readily apparent, if deep (muscles, trachea) or evident only on microscopy (muscles, perithyroidal fat)
Gross images
Frozen section description
- Frozen section is strongly discouraged as frozen artifacts distort the nuclear features necessary for diagnosis
- Standard care is to perform preoperative fine needle aspiration to establish the diagnosis and to determine the most appropriate surgical procedure
- Frozen in thyroid surgery is frequently used for detecting parathyroid tissue and, sometimes lymph node metastasis
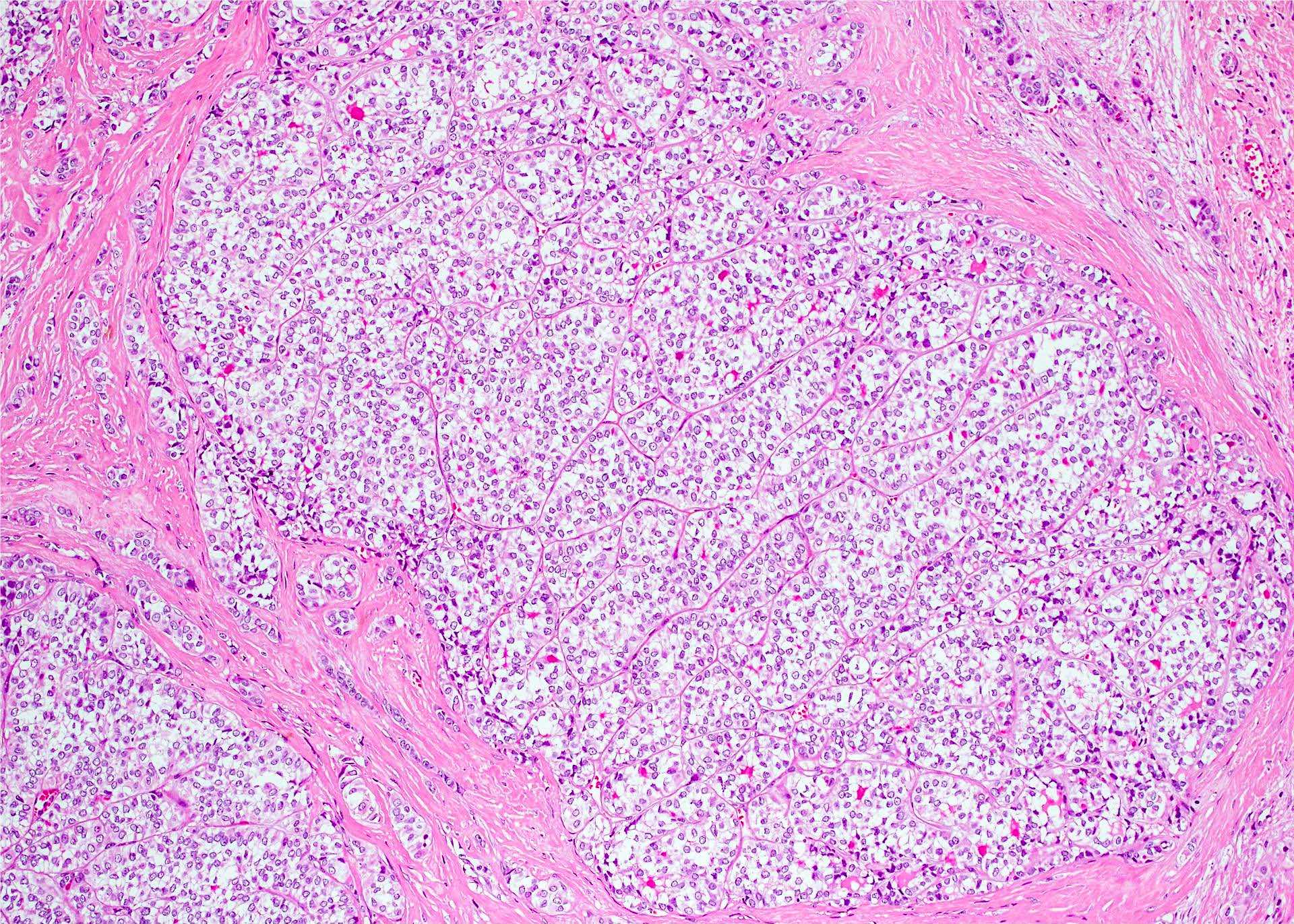
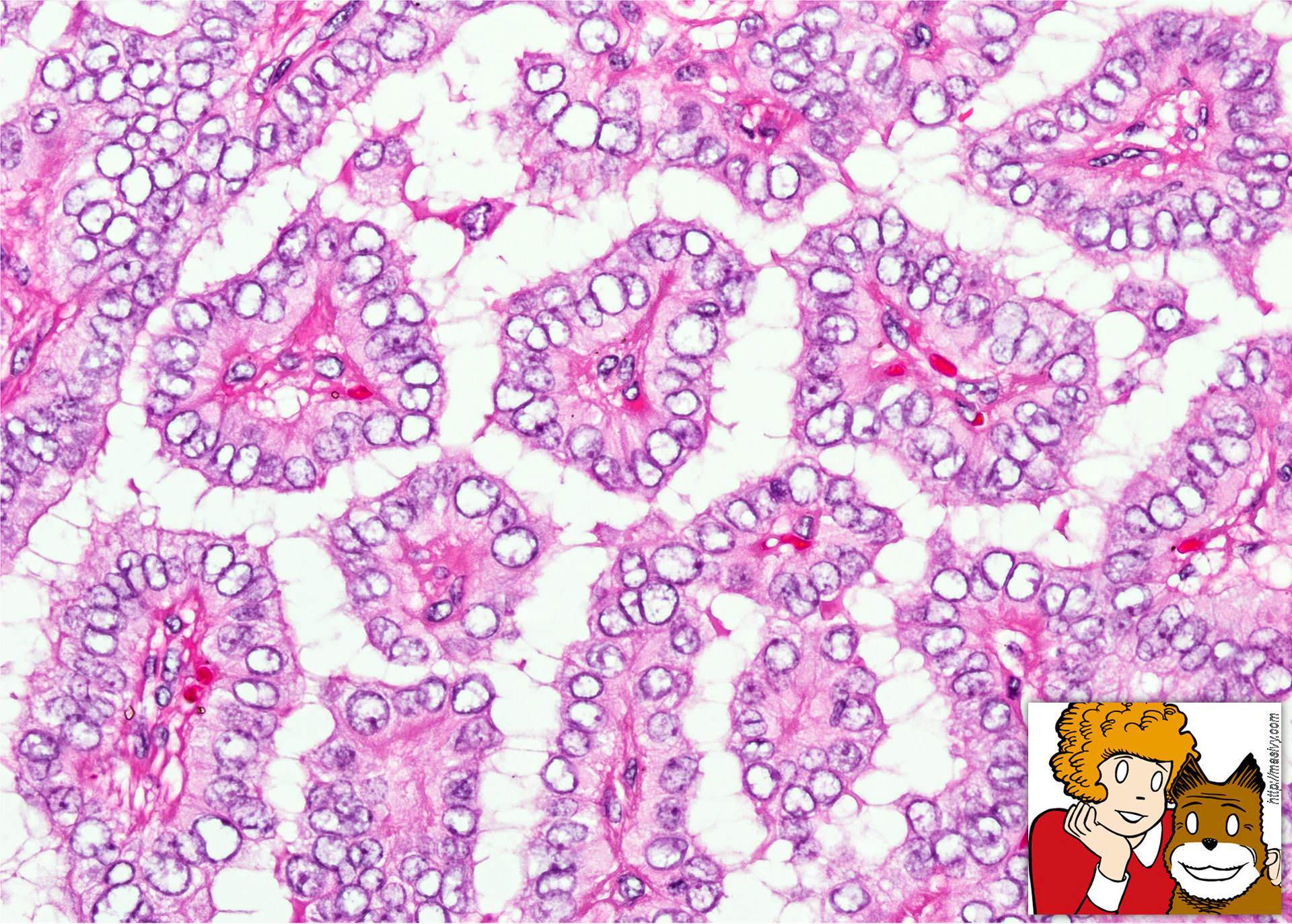
Microscopic (histologic) description
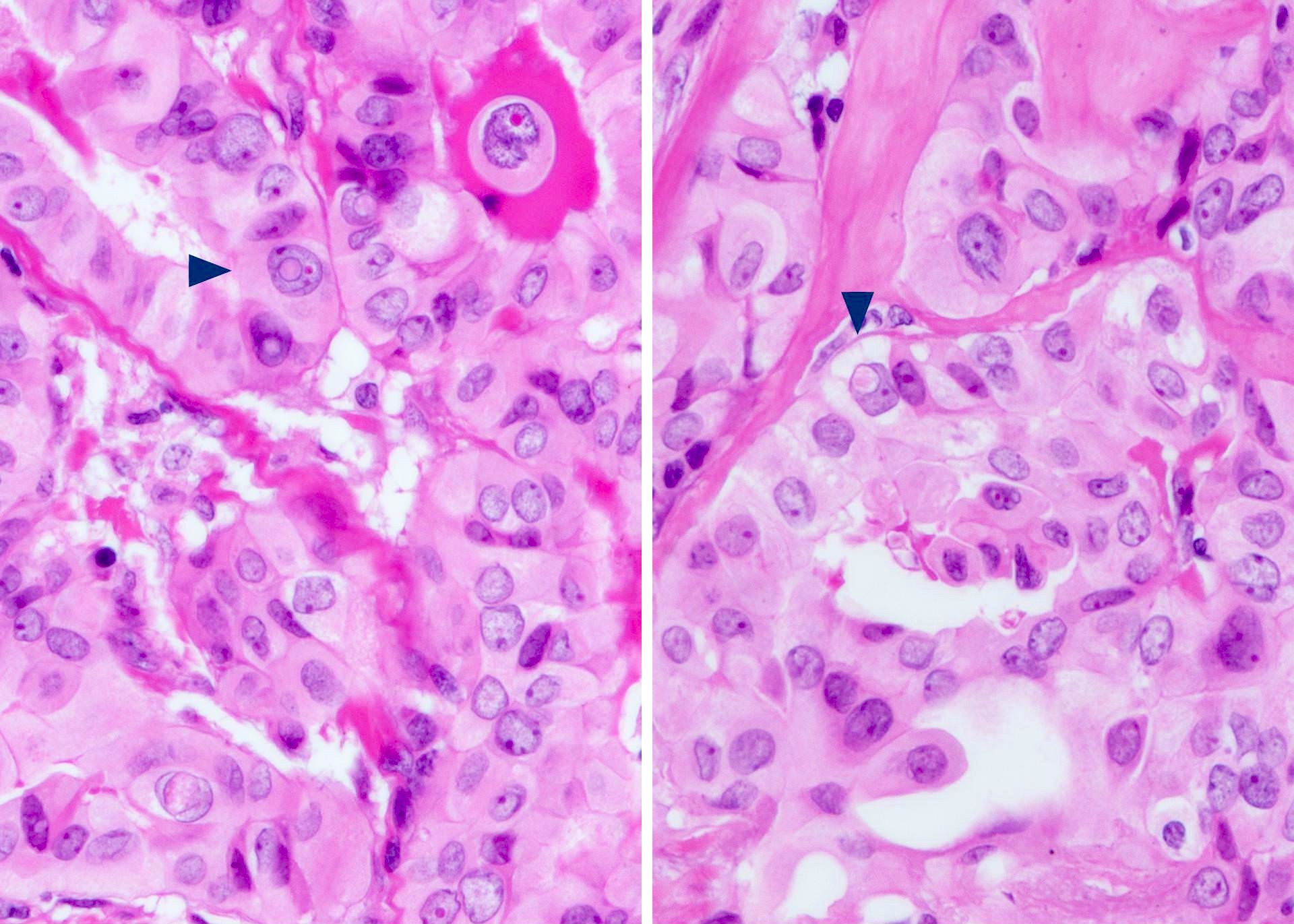
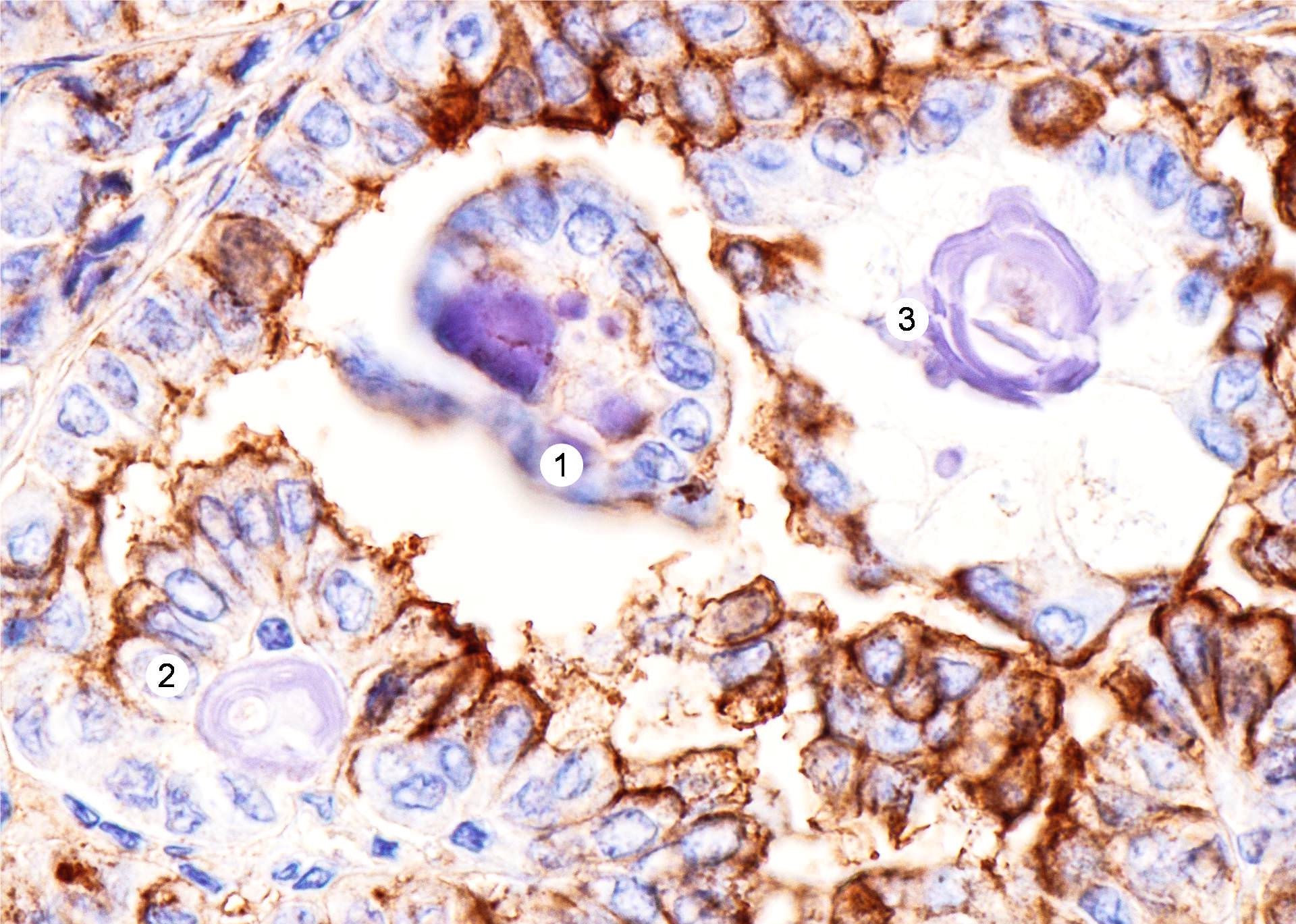
- Nuclear features:
- Change of nuclear size and shape: nuclear enlargement, elongation and overlapping
- Chromatin characteristics: chromatin clearing / optically clear chromatin, chromatin margination, glassy / ground glass nuclei, Orphan Annie nuclei
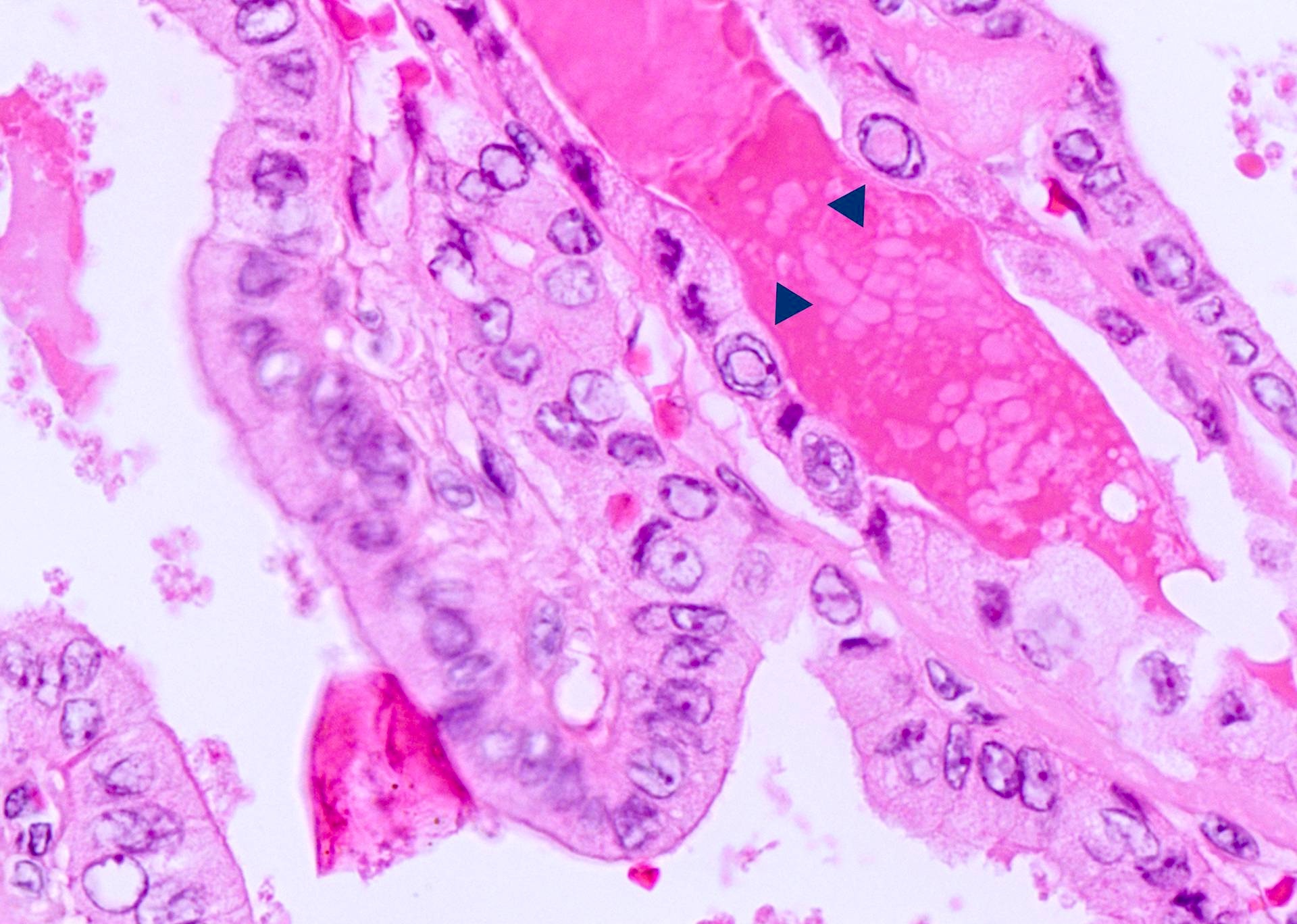
- Nuclear membrane irregularity: irregular nuclear contour, nuclear grooves and nuclear pseudoinclusions (represent cytoplasmic invaginations)
- Variants:
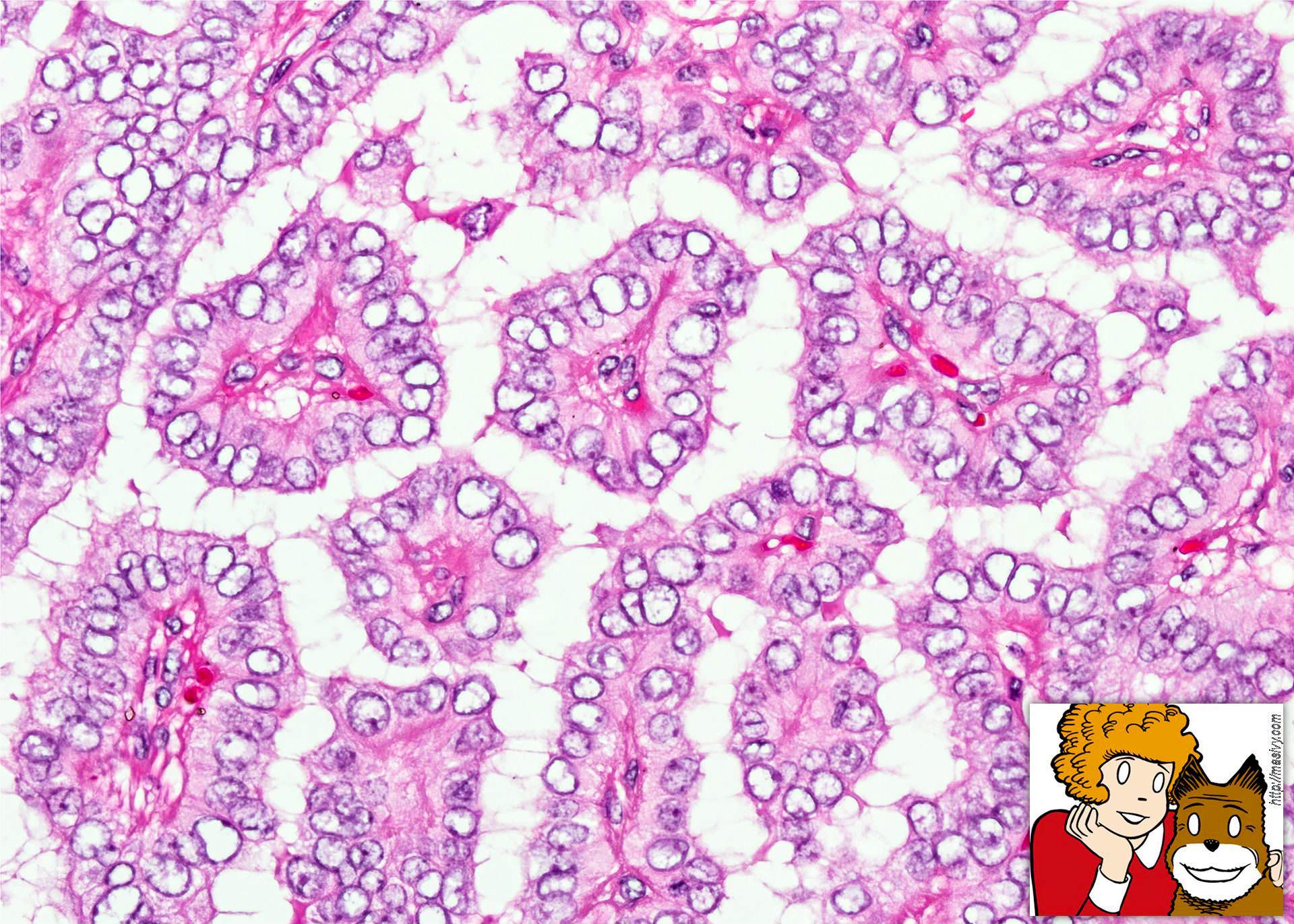
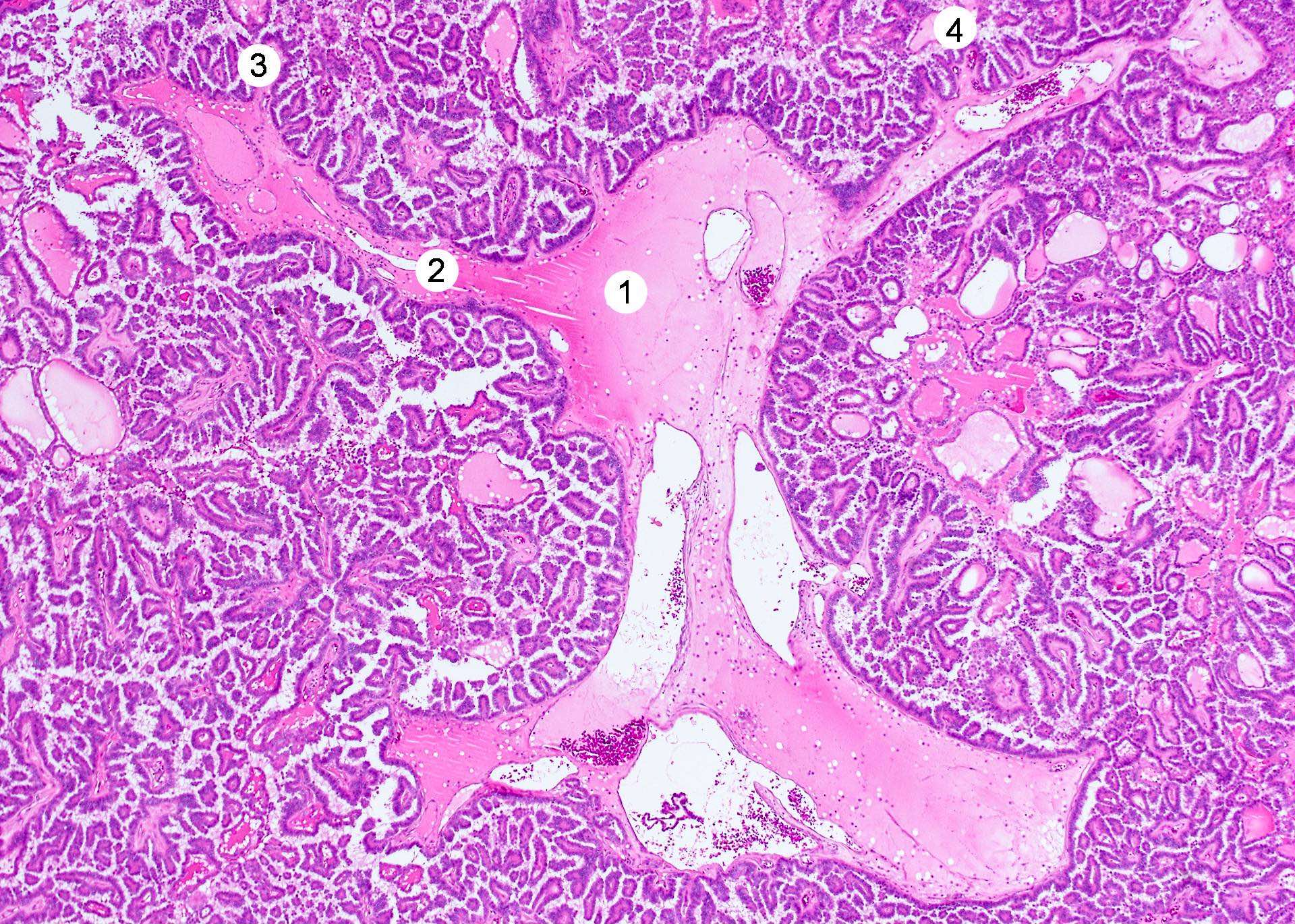
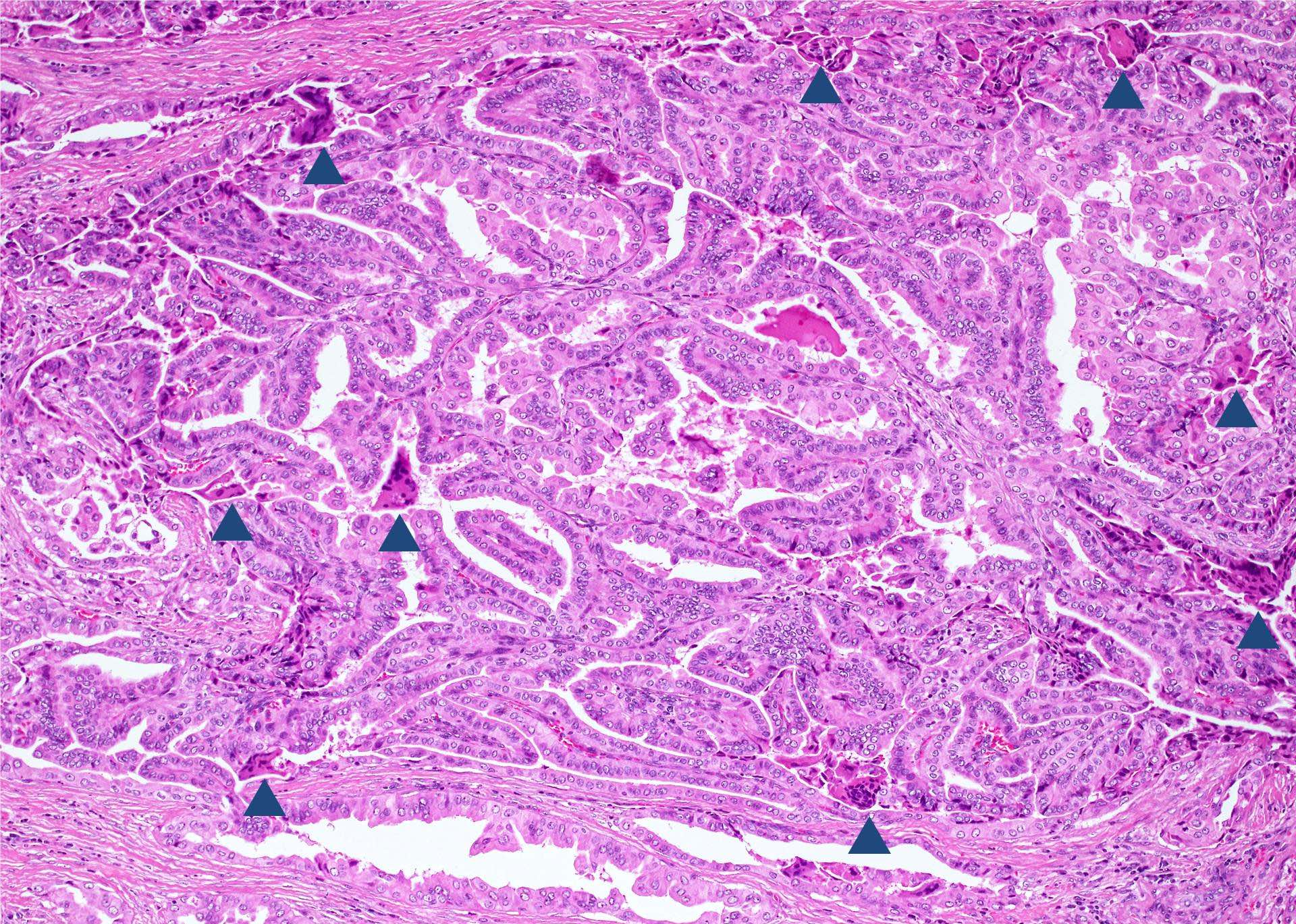
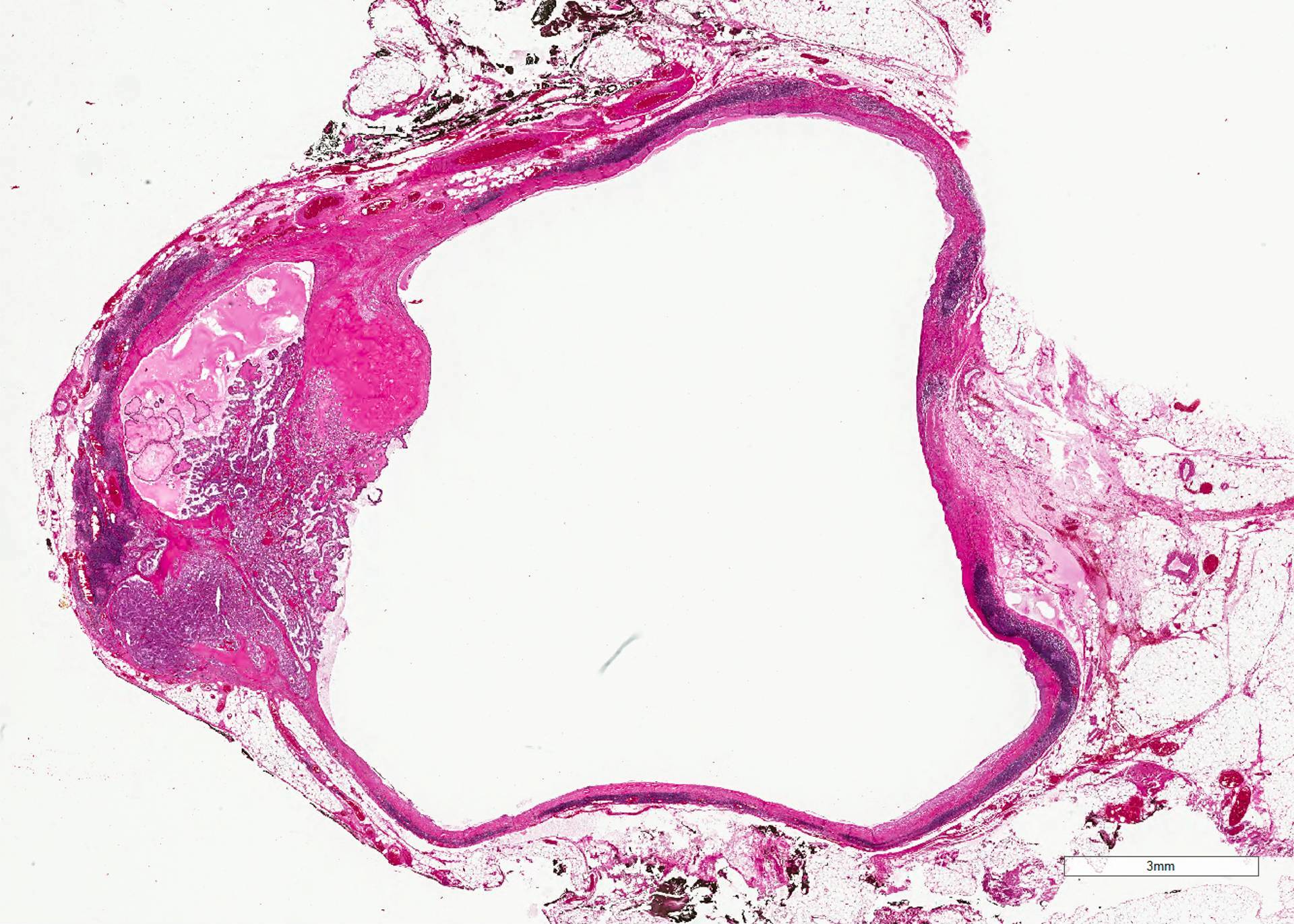
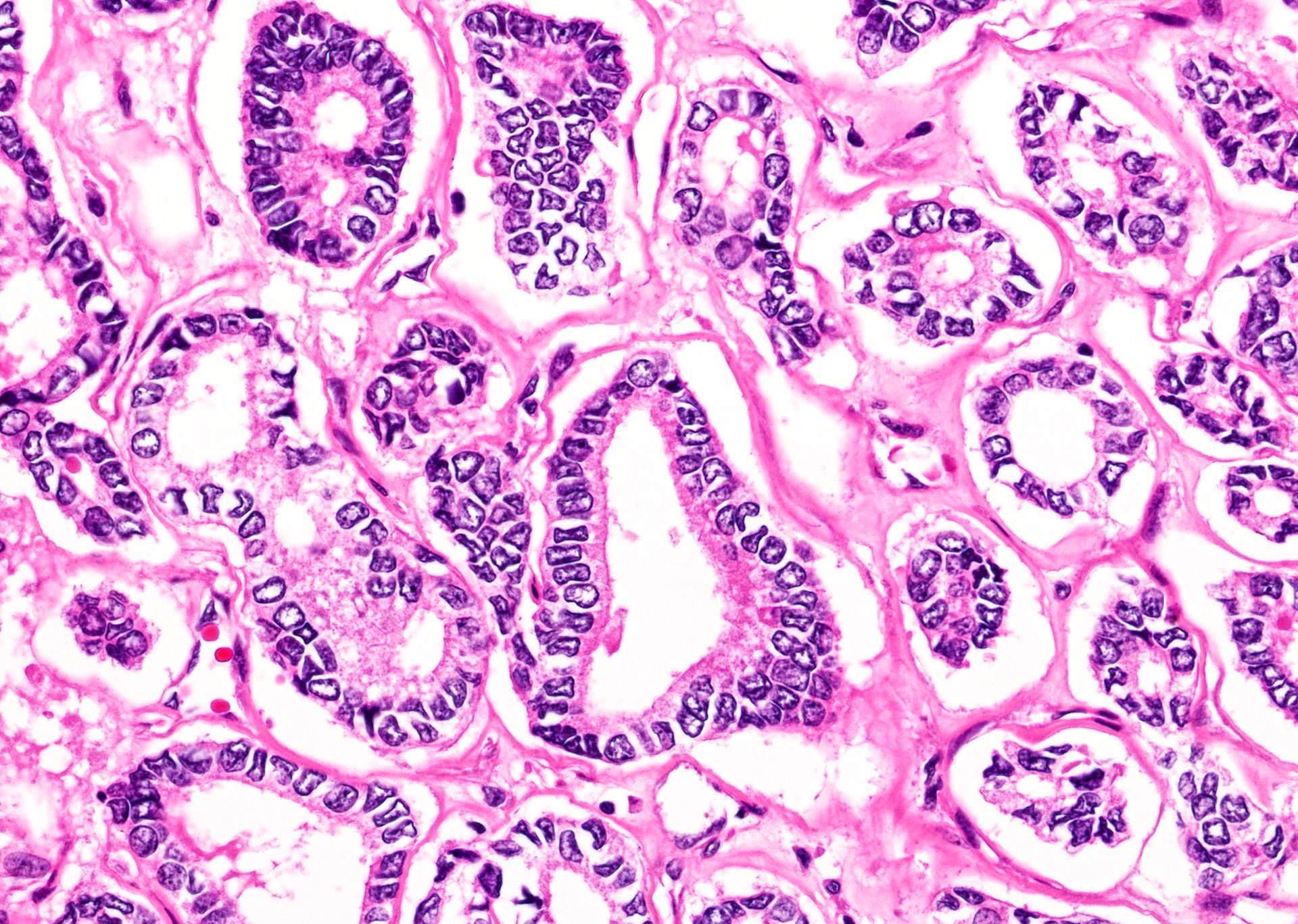
- Classic: complex, branching, randomly oriented papillae with fibrovascular cores
- Tumors with both papillary and follicular architecture should be classified as classic variant, given the associated risk of nodal metastasis (Thyroid 2019;29:1792)
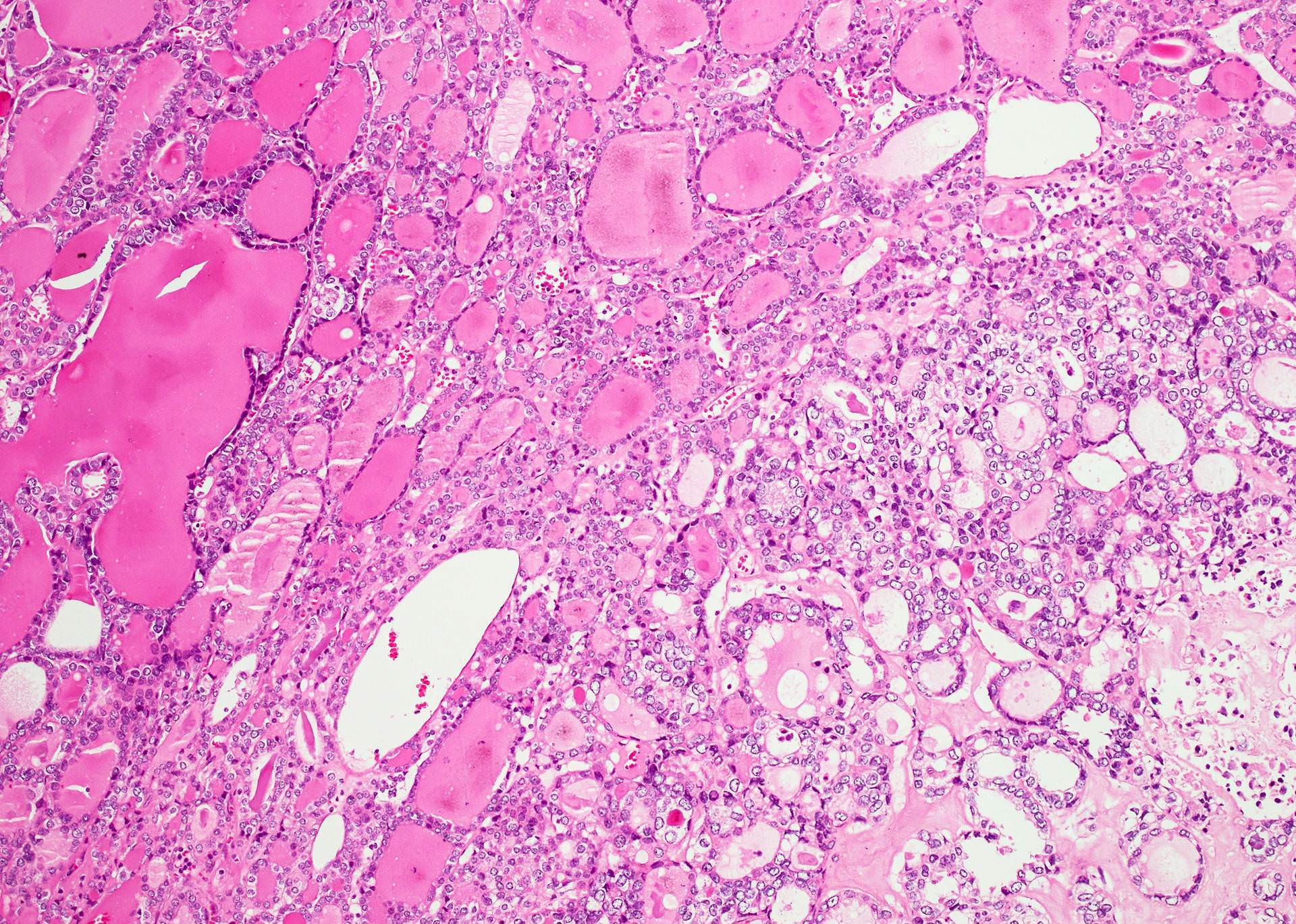
- Follicular: neoplastic cells arranged as macro or microfollicles with central colloid
- Cribriform morular: cribriform architecture and squamous morules; cytologically, tumor cells usually have columnar / cigar shaped nuclei, sometimes with prominent supra / sub nuclear vacuoles
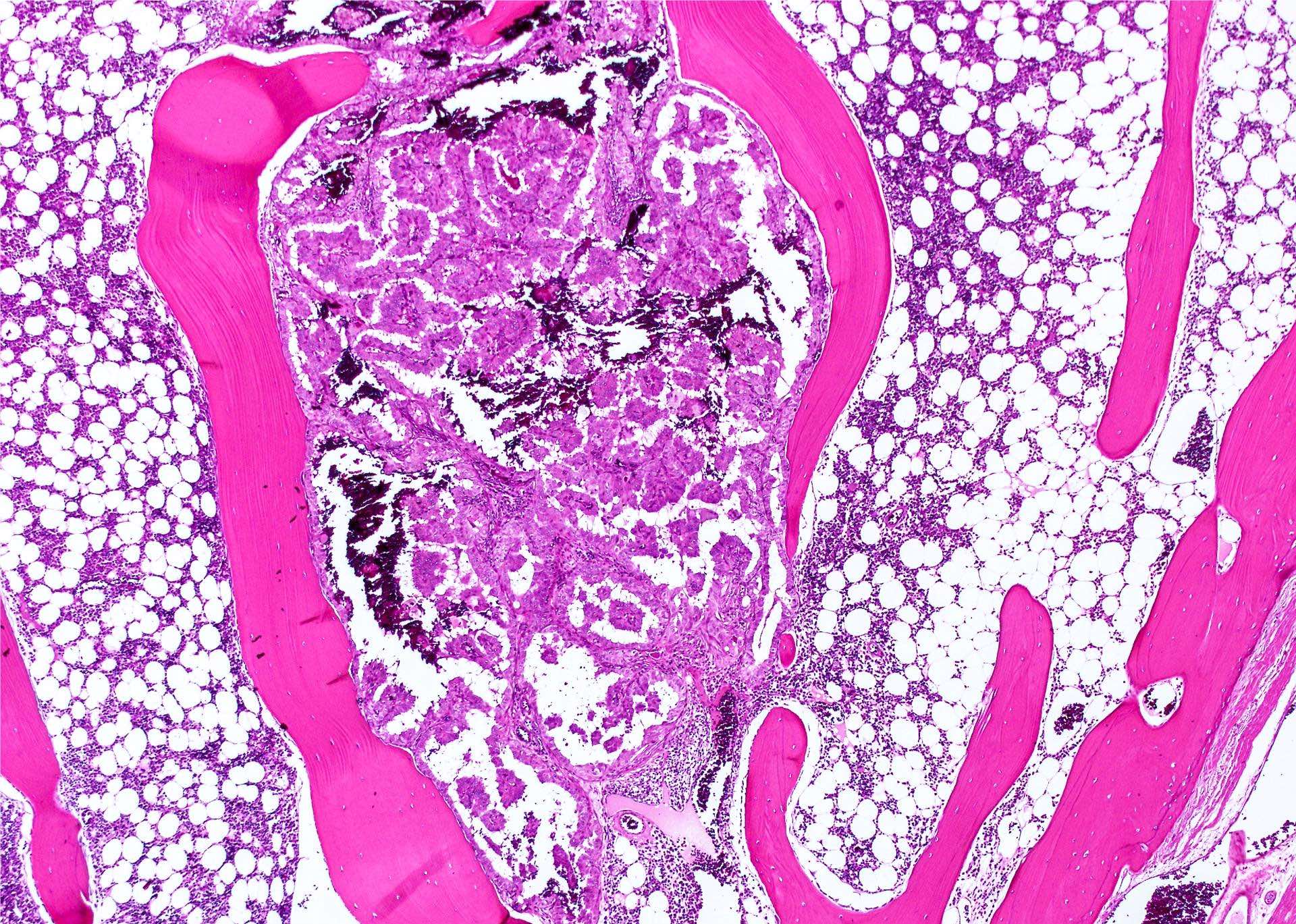
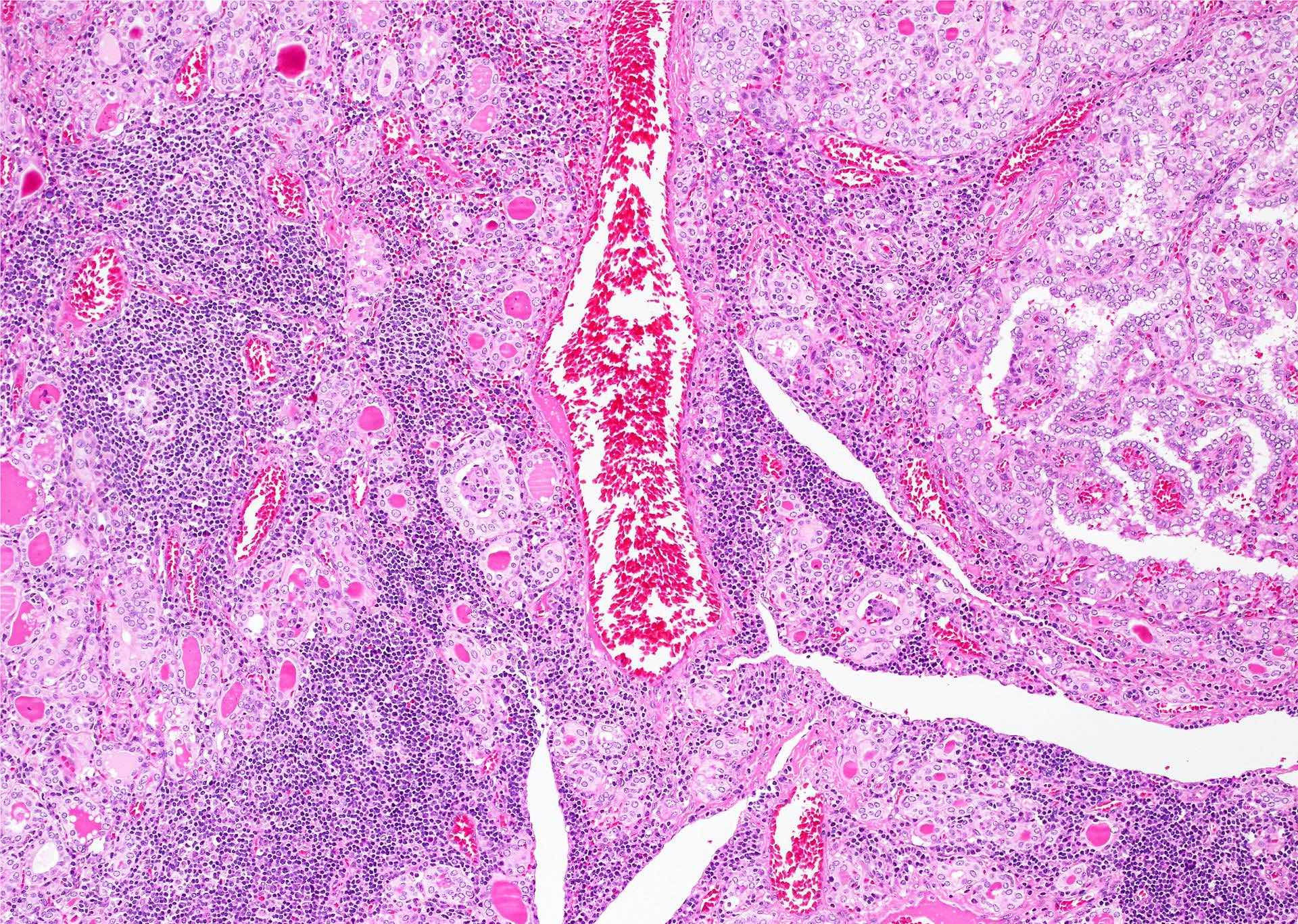
- Diffuse sclerosing: diffuse involvement of at least one thyroid lobe, in association with fibrosis, frequent psammoma bodies, squamous metaplasia and frequent lymphatic invasion; often present in young patients with a background chronic lymphocytic thyroiditis
- Warthin-like: oncocytic tumor cells with a background of reactive lymphoid stroma resemble Warthin tumor at low power; often occur in the setting of chronic lymphocytic thyroiditis
- Solid: tumor with solid / insular growth pattern
- Different patterns (e.g., papillary and follicular) are frequently coexist within 1 tumor
- Classic: complex, branching, randomly oriented papillae with fibrovascular cores
- Cytologic features:
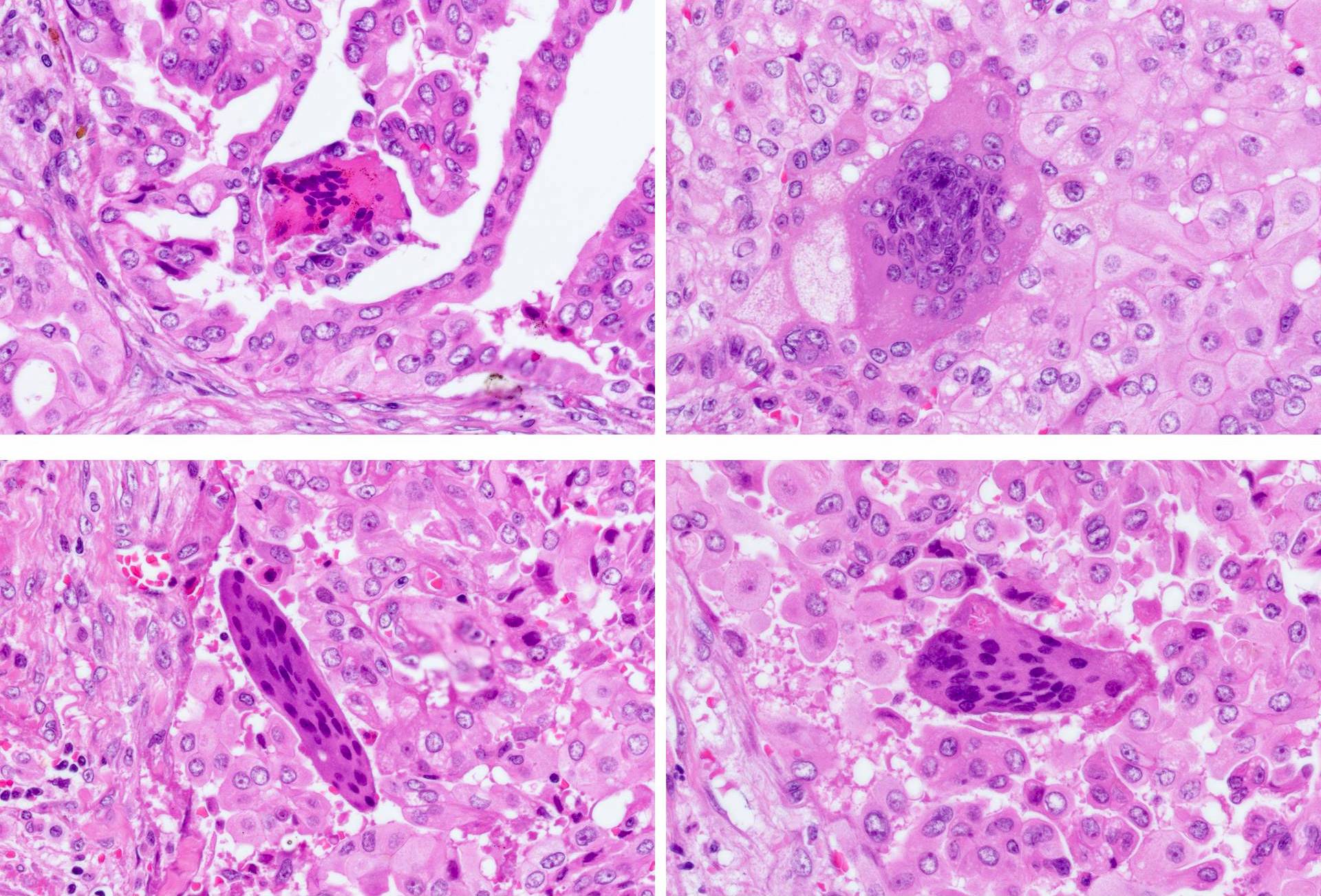
- Tall cell: defined as a cell height at least 2 - 3 times of cell width with distinct cell border; often associated with stretched elongated "tram-track" papillae, eosinophilic cytoplasm (due to the accumulation of mitochondria) and frequent nuclear pseudoinclusions; a tumor can be defined as tall cell variant if at least 30% of the tumor contains tall cells
- Columnar cell: cigar shaped nuclei with nuclear pseudostratification; a tumor can be defined as columnar cell variant if at least 30% of the tumor contains columnar cells
- Hobnail: tumor cells have high nuclear to cytoplasmic ratio with nuclei protruding away from the stalk into the lumen; often with prominent nucleoli
- Oncocytic: tumor cells with abundant eosinophilic cytoplasm
- Other rare cytologic features that have been reported include spindle cell and clear cell
- Other pathologic features:
- Colloid is usually dense and hypereosinophilic (inspissated colloid)
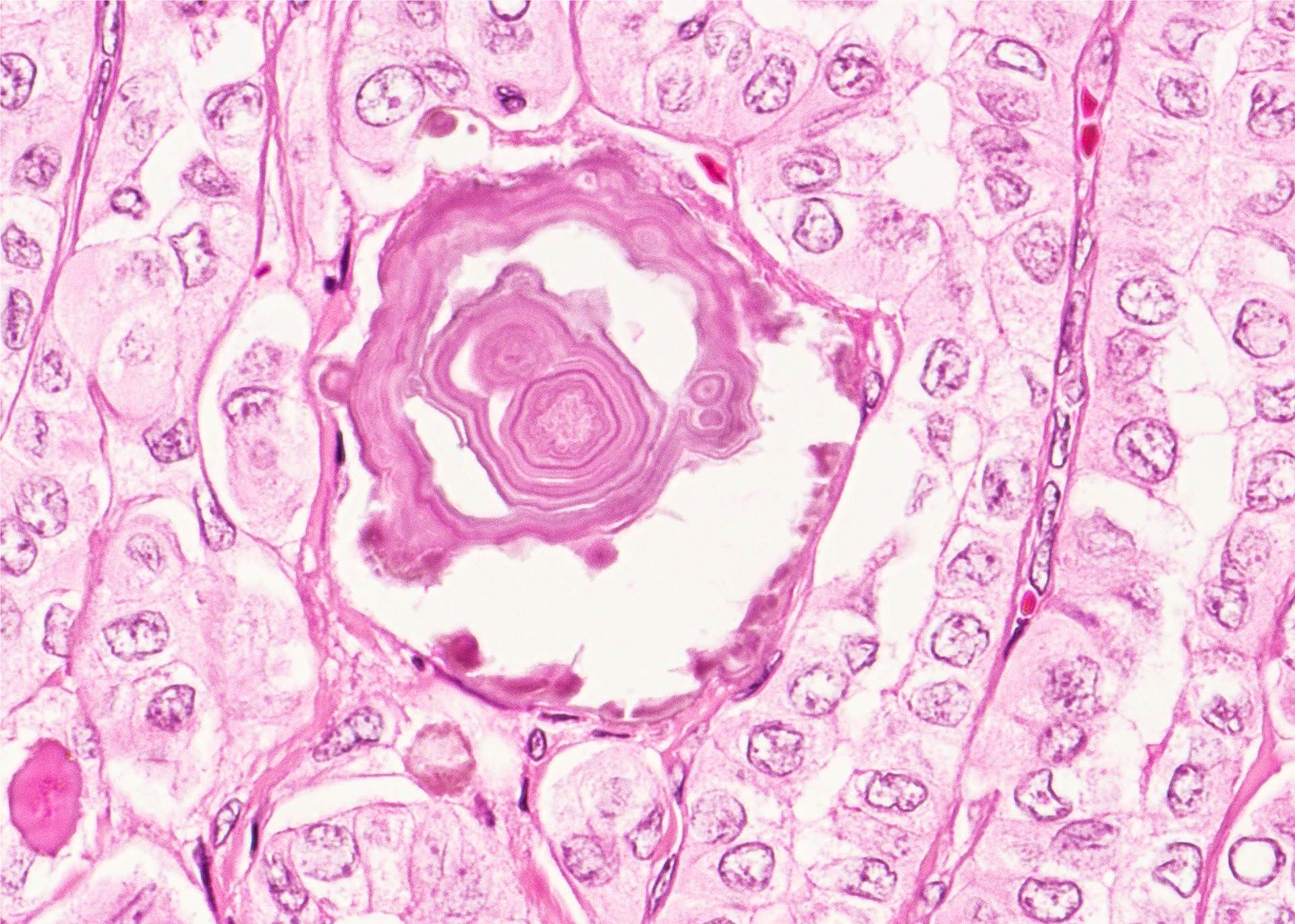
- Psammoma bodies defined as laminated microcalcification are frequently associated with classic, tall cell, hobnail and diffuse sclerosing variants; it is postulated that psammoma bodies are formed in the hyalinized core / stalk of papillae
- Presence of psammoma body alone in lymph node is indicative of metastatic disease and is considered as pN1 by CAP (CAP: Protocol for the Examination of Specimens From Patients With Carcinomas of the Thyroid Gland [Accessed 1 October 2019]) and AJCC 8th edition (Amin: AJCC Cancer Staging Manual, 8th Edition, 2018)
- Most of papillary thyroid carcinoma are infiltrative while some are encapsulated or well demarkated (usually follicular variant)
- Tumor stroma could be fibrotic (predominant in fibromatosis / fasciitis-like variant) or calcified and ossified
- Cystic changes in primary tumor or in metastasis are not infrequent
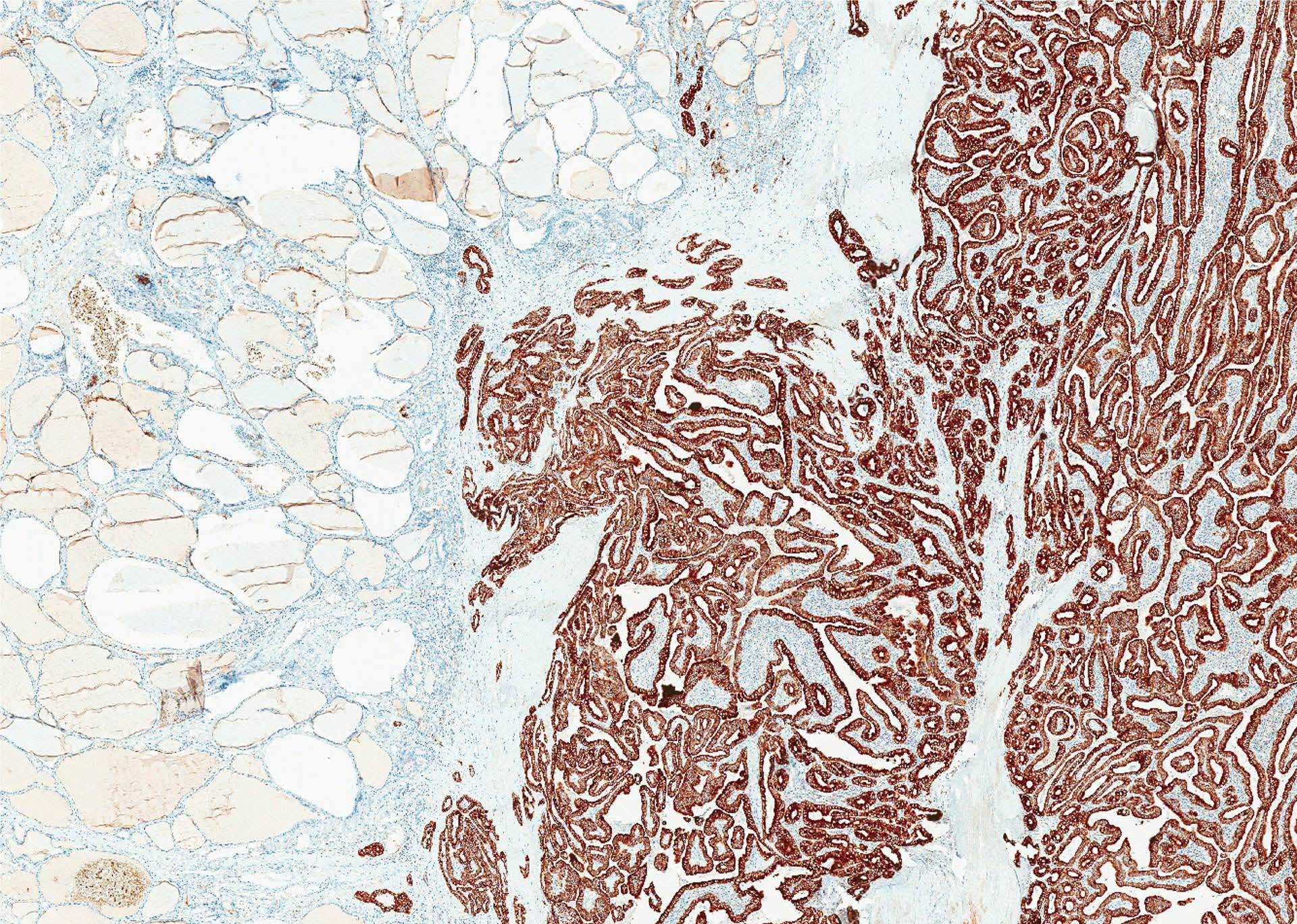
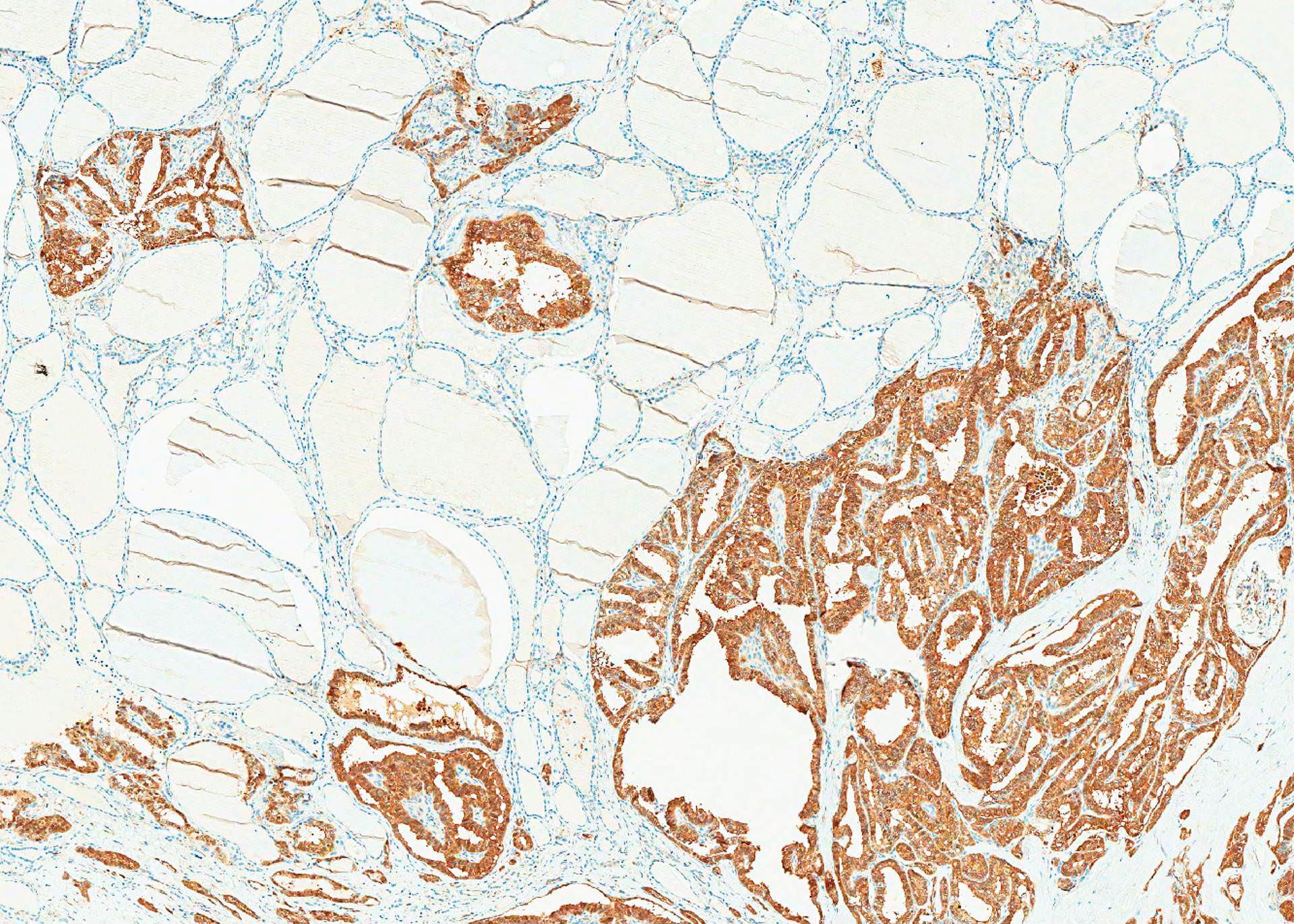
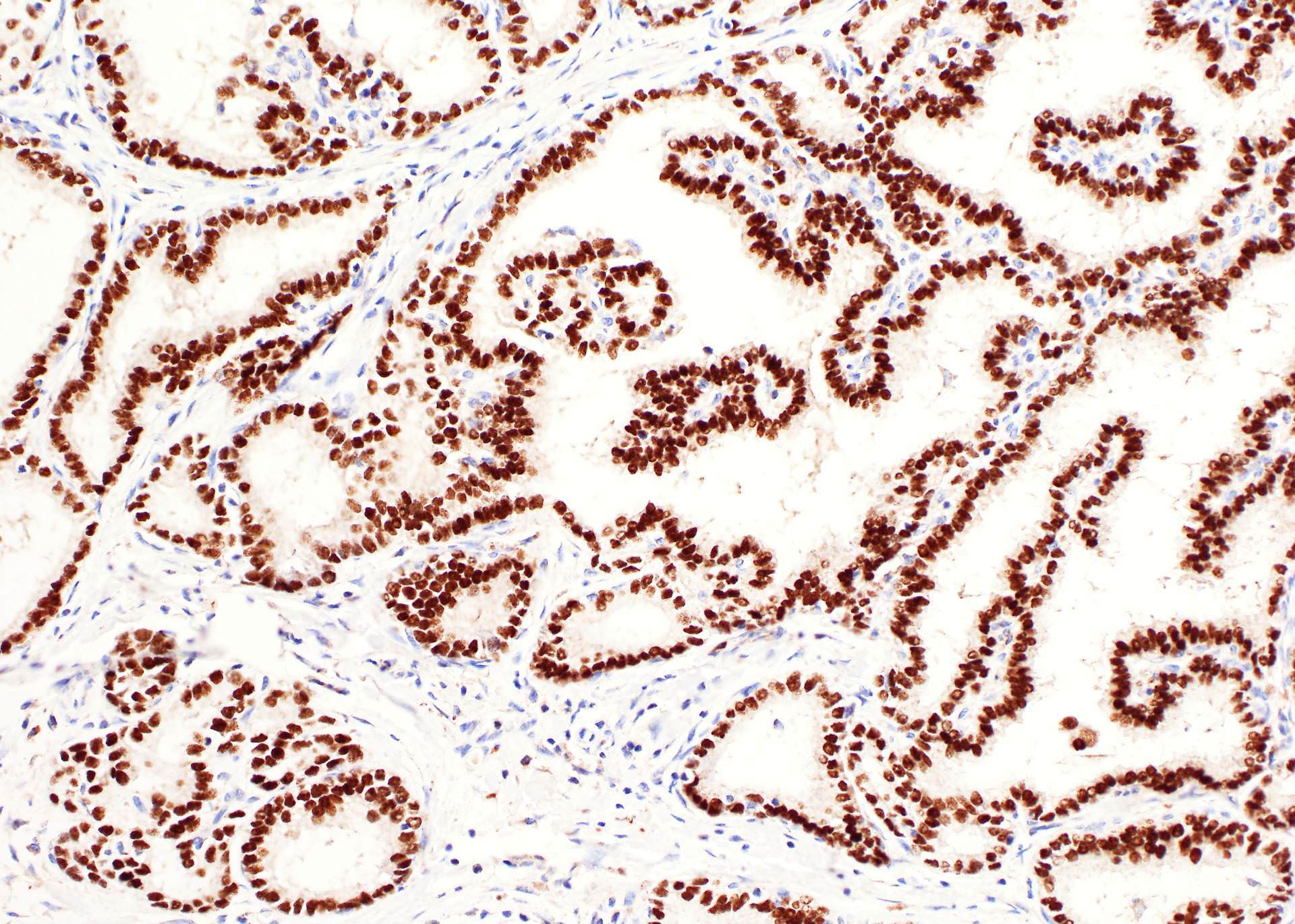
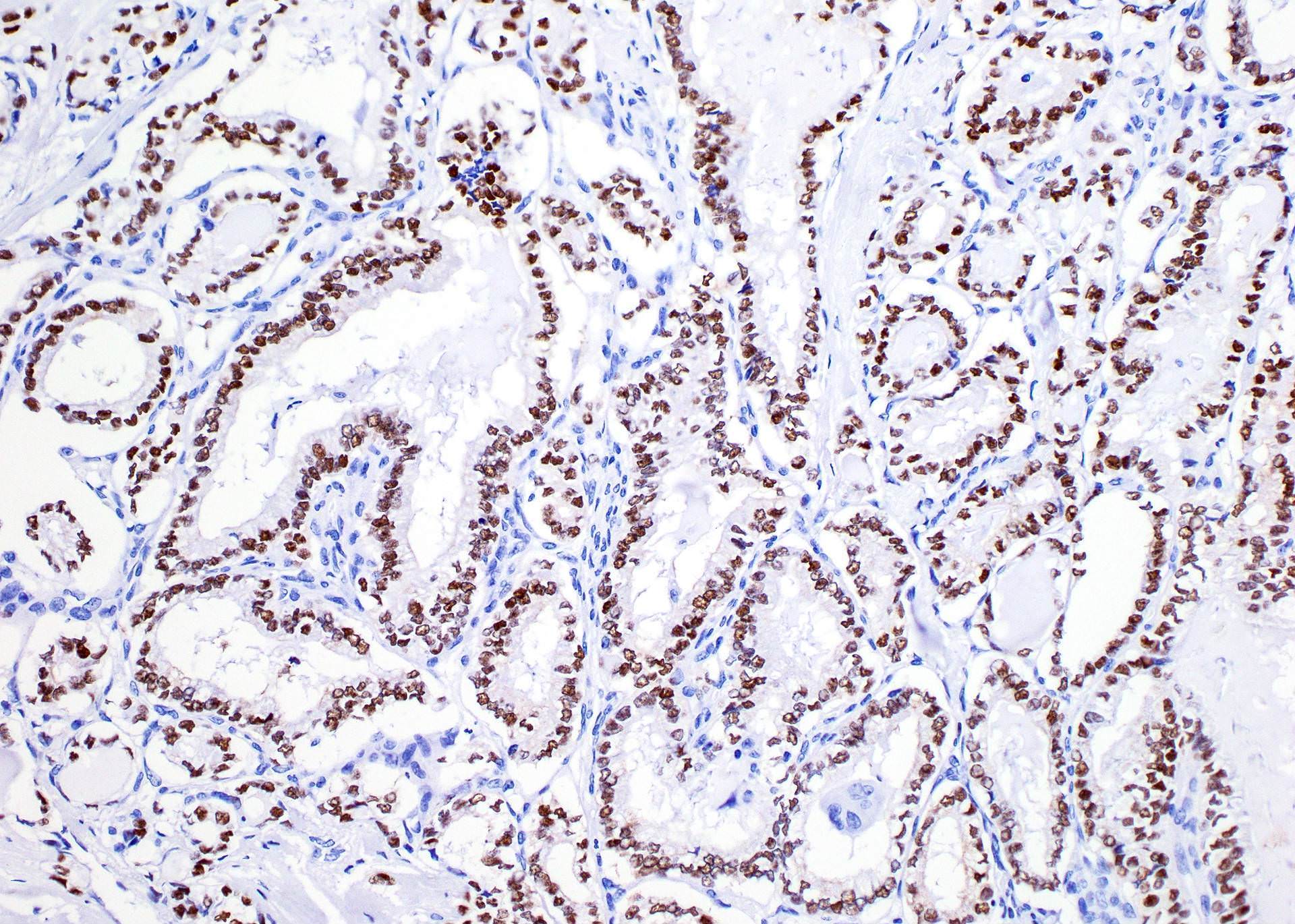
Microscopic (histologic) images
Contributed by Andrey Bychkov, M.D., Ph.D.
Nuclear features
Other histologic features
Stains
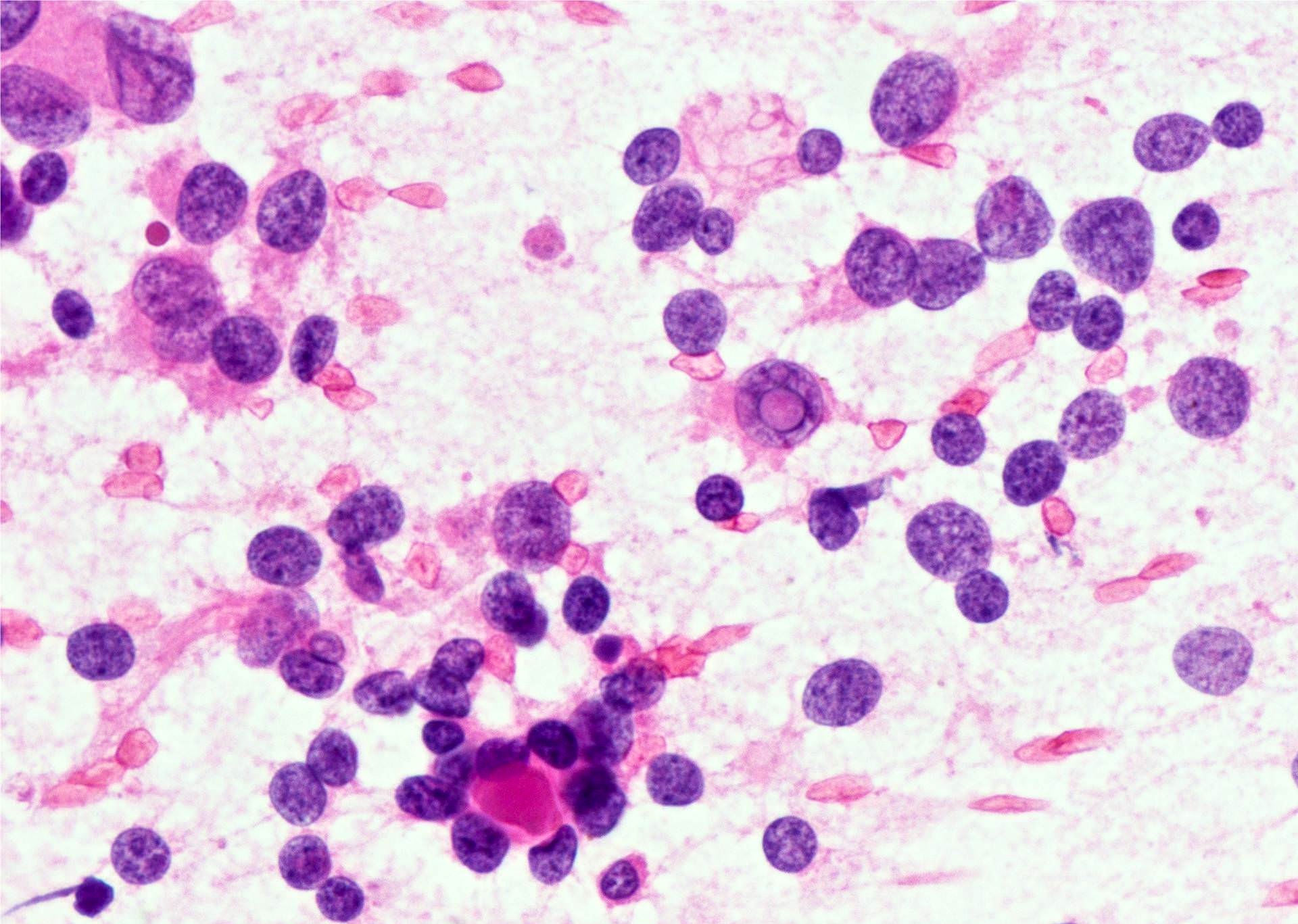
Cytology description (Courtesy of Shahid Islam, M.D., Ph.D.)
- Cellular aspirate with monolayer sheets of cells, often with three dimensional papillary architecture (thick or thin fragments with fibrovascular cores), multilayered syncytial fragments or branched sheets
- May see psammoma bodies
- Cells have enlarged overlapping nuclei with irregular contours, intranuclear inclusions, nuclear grooves and pale finely chromatin
- No feature by itself is diagnostic, must see a constellation of findings
- Addition of BRAF analysis may be useful (Endocr J 2007;54:399)
- False negatives usually due to nodule heterogeneity (Cancer 2008;114:27)
Cytology images
Positive stains
- Markers of thyroid follicular cells, including cytokeratin AE1 / AE3, CK7, TTF1, thyroglobulin and PAX8
- A proportion is positive for mutation specific protein by immunohistochemistry, e.g., BRAFV600E (VE1 antibody) and NRAS Q61R (Thyroid 2019;29:1792)
- Utility of CK19, galectin3 and HBME1 to differentiate from benign mimics remains controversial (Am J Clin Pathol 2002;118:186, Am J Clin Pathol 2001;116:696, Am J Clin Pathol 2006;126:700)
- Variant specific immunohistochemistry
- CDX2 for columnar cell variant (positive in 50% of cases, Histopathology 2018;72:40)
- Beta catenin for cribriform morular variant showing abnormal nuclear accumulation
- Ki67 index is low (1 - 5%), > 10% is associated with aggressive histotype and higher recurrence risk (Sci Rep 2017;7:41752)
Negative stains
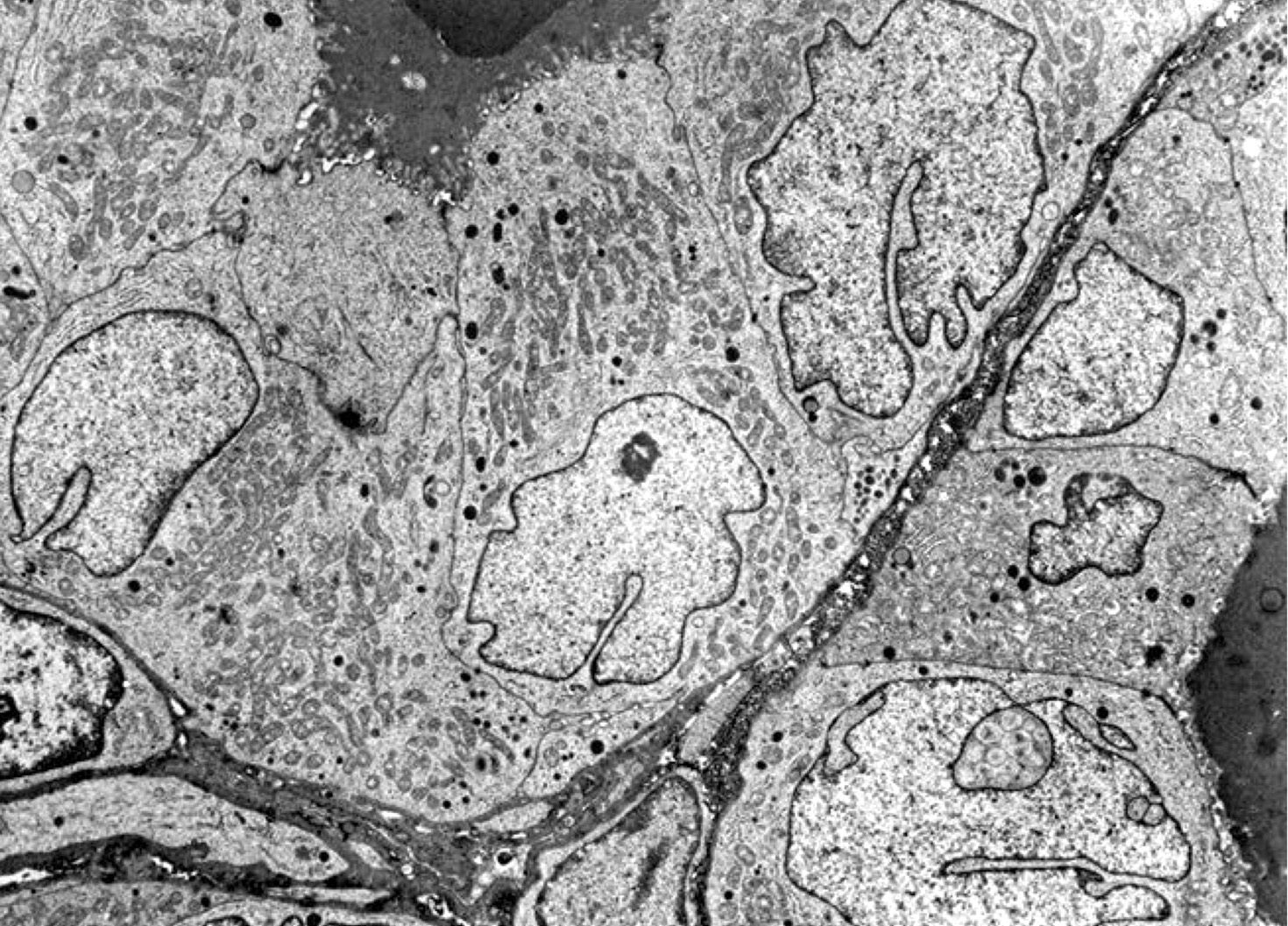
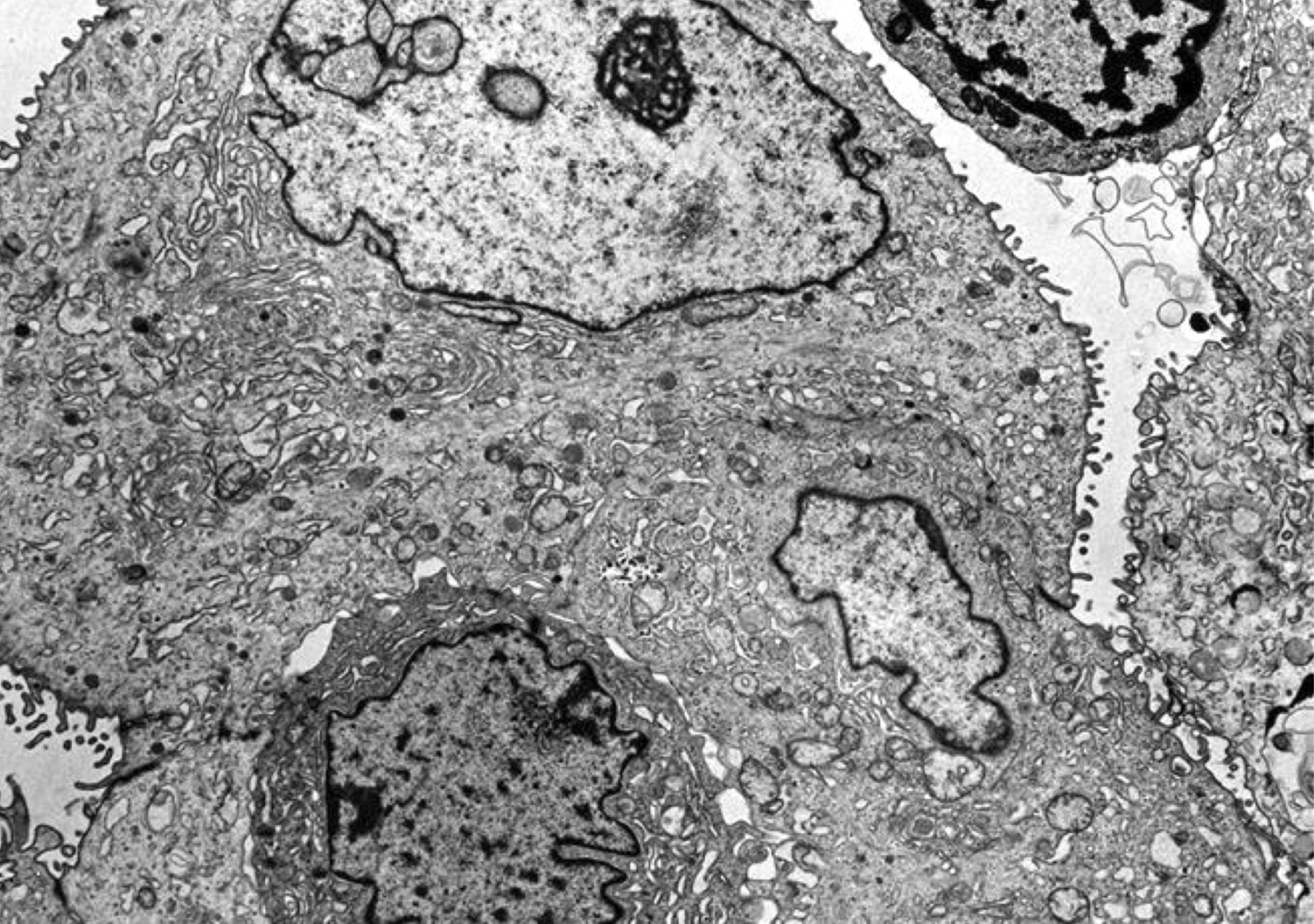
Electron microscopy description
- Highly indented nuclear membrane with pseudoinclusions and multilobation
- Clusters of large interchromatin granules, nucleoli have microfibrillar cortex with segregation of their components
- Also dense RNA containing microspherules in nucleoli (Arch Pathol Lab Med 1978;102:635)
Molecular / cytogenetics description
- In 2014, The Cancer Genome Atlas (TCGA) published comprehensive genomic alterations (Cell 2014;159:676); key findings are:
- BRAF is the most frequently mutated gene, occurring in 60% of cases
- Most frequent mutation is BRAFV600E, which is associated with classic variant and tall cell variant, as well as a low thyroid differentiation score (i.e., less differentiated)
- BRAF is highly prevalent (80 - 90%) in PTC from coastal Asian countries with high iodine intake (Japan, Korea) (Malays J Pathol 2017;39:95)
- RAS (HRAS, NRAS and KRAS) occurs in 13%, in particular follicular variant; RAS mutation is associated with a high thyroid differentiation score
- Fusions involving BRAF, RET, PPARG, NTRK1, NTRK3, ALK, LTK, MET, FGFR2 or THADA are detected in 15%; among them, RET fusion is the most common, seen in 6%
- TERT promoter mutation is present in 10% and is often associated with aggressive histology, e.g., tall cell variant and poor prognosis (Endocr Relat Cancer 2013;20:603)
- BRAF is the most frequently mutated gene, occurring in 60% of cases
Videos
Papillary thyroid carcinoma: cystic
Thyroid carcinoma
Thyroid: compare and contrast
Histopathology thyroid: papillary carcinoma
Histopathology thyroid: Hashimoto thyroiditis, papillary carcinoma
Integrated genomic characterization of papillary thyroid carcinoma
An alphabet soup of thyroid neoplasms
Sample pathology report
- Thyroid, total thyroidectomy:
- Papillary thyroid carcinoma, tall cell variant, 1.2 cm (see synoptic report)
Differential diagnosis
- Lymphocytic thyroiditis with reactive nuclear changes:
- Nuclei are round without nuclear pseudoinclusions
- In the context of marked lymphocytic thyroiditis, mild chromatin clearing and nuclear enlargement are not sufficient for a diagnosis of papillary thyroid carcinoma
- Papillary foci of Graves disease or other papillary hyperplasia:
- Graves disease may have abundant papillary infoldings and the cytoplasm may be tall/columnar; however, the nuclei are small and round without nuclear features of papillary thyroid carcinoma
- Medullary thyroid carcinoma:
- Both may show solid or papillary architecture
- Contains nuclei typical of neuroendocrine neoplasm with salt and pepper chromatin and is positive for synaptophysin and chromogranin and negative for PAX8 and thyroglobulin
- Hyalinizing trabecular tumor:
- Also can have frequent nuclear grooves and nuclear pseudoinclusions
- Shows unique architectural patterns with trabecular architecture and tumor cells arranged perpendicularly to the trabeculae
- Has characteristic GLIS rearrangement (Thyroid 2019;29:161)
- Hyperplastic ultimobranchial body rests / solid cell nests:
- In lateral lobes
- Round to oval structures, may have chromatin clearing or grooves, central cysts, mucin and squamous metaplasia
- Solid cell nests are usually positive for high molecular weight cytokeratin and p63 but negative for TTF1 / thyroglobulin and papillary thyroid carcinoma associated mutations
Board review style question #1
Board review style answer #1
Board review style question #2
- Which of the following variants of papillary thyroid carcinoma is considered as an aggressive variant?
- Follicular variant
- Oncocytic variant
- Papillary microcarcinoma
- Tall cell variant
- Warthin-like variant
Board review style answer #2
D. Tall cell variant. Tall cell variant is one of the aggressive variants that is considered as intermediate risk by the American Thyroid Association Management Guidelines.
Comment Here
Reference: Papillary thyroid carcinoma
Comment Here
Reference: Papillary thyroid carcinoma