Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology and etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Peripheral smear description | Peripheral smear images | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Khanlari M, OK CY. MCL-aggressive variants. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomamclaggressive.html. Accessed September 17th, 2025.
Definition / general
- 2 types: blastoid and pleomorphic
- Blastoid: cells resemble lymphoblasts with high mitotic rate (> 20 - 30 mitoses /10 high power fields) (Blood 1997;89:1421)
- Pleomorphic: large, pleomorphic cells with variable sizes, prominent nucleoli
- Definition is based on the morphology
Essential features
- Associated with t(11;14)(q13;q32) or IGH/CCND1 and cyclin D1 overexpression
- High proliferation index and unfavorable outcome
Terminology
- Blastoid variant
- Mantle cell lymphoma (MCL), lymphoblastoid variant
- Mantle cell lymphoma (MCL), blastic
- Pleomorphic variant
- Mantle cell lymphoma (MCL), large cell variant
- Mantle cell lymphoma (MCL), anaplastic
- Mantle cell lymphoma (MCL), nucleolated variant
ICD coding
- ICD-O: 9673/3 – mantle cell lymphoma
Epidemiology
- 10 - 20% of all mantle cell lymphomas (J Clin Oncol 2016;34:1386, Leuk Lymphoma 2015;56:2759)
- Frequency may be higher in patients with prolonged follow up
Sites
- Lymph node, spleen, bone marrow
- Extranodal sites:
- Gastrointestinal tract is the most common site
- CNS: More frequently involved by blastoid / pleomorphic variant than classic variant
- Peripheral blood:
- Leukemic involvement at diagnosis
Pathophysiology and etiology
- CCND1 at 11q13 with IGH at 14q32
- New CCND1 will reposition near the nucleoli (nucleolin and RNA polymerase II) (Blood 2014;123:2044)
- Higher level of cyclin D1 RNA, when 3'-untranslated region is deleted (common in blastoid mantle cell lymphoma) (Blood 2007;109:4599)
- Higher level of chromosomal aberration in blastoid / pleomorphic mantle cell lymphoma than in classic mantle cell lymphoma (Hum Pathol 2003;34:1022)
- Frequent tetraploidy in blastoid / pleomorphic mantle cell lymphoma than in classic mantle cell lymphoma (Blood 1997;89:1421)
- 8q24 abnormalities (MYC gene) in blastoid mantle cell lymphoma (Mod Pathol 2002;15:1266)
- High level of p53 expression in a subset of blastoid mantle cell lymphomas (Blood 2017;130:1903)
- Mutated NOTCH1 and NOTCH2: affects signaling pathway (Blood 2012;119:1963, Proc Natl Acad Sci U S A 2013;110:18250)
- De novo or from classic mantle cell lymphoma progression
Clinical features
- Median age: sixth and seventh decades
- Clinical picture resembles classic mantle cell lymphoma
- Male predominance (M:F = 2 - 3:1)
- Ann Arbor clinical stage III/IV in most cases (Leukemia 2001;15:1785)
- Short duration of clinical response after chemotherapy (Leukemia 2001;15:1785)
- Poorer overall survival compared with classic mantle cell lymphoma (Leuk Lymphoma 2016;57:1327)
- More common B symptoms
- Blastoid variant: often presents de novo
- Pleomorphic variant: often history of classic mantle cell lymphoma
- Generalized lymphadenopathy
- Extranodal involvement is common
- Leukemic forms of mantle cell lymphoma (Am J Clin Pathol 2002;117:246)
Diagnosis
- Based on clinical presentation (refer to Clinical features)
- B symptoms
- Tissue biopsy (lymph node / extranodal sites)
- Cytology
- Peripheral blood exam / bone marrow biopsy
Laboratory
- Anemia and thrombocytopenia
- High LDH and β2 microglobulin
- A monoclonal serum component (low level)
- Atypical lymphocytosis
- Reference: Cancer 1998;82:567
Prognostic factors
- Univariate risk factors
- Blastoid morphology
- Leukemic presentation
- High Mantle cell lymphoma International Prognostic Index (MIPI) score (J Clin Oncol 2016;34:1386)
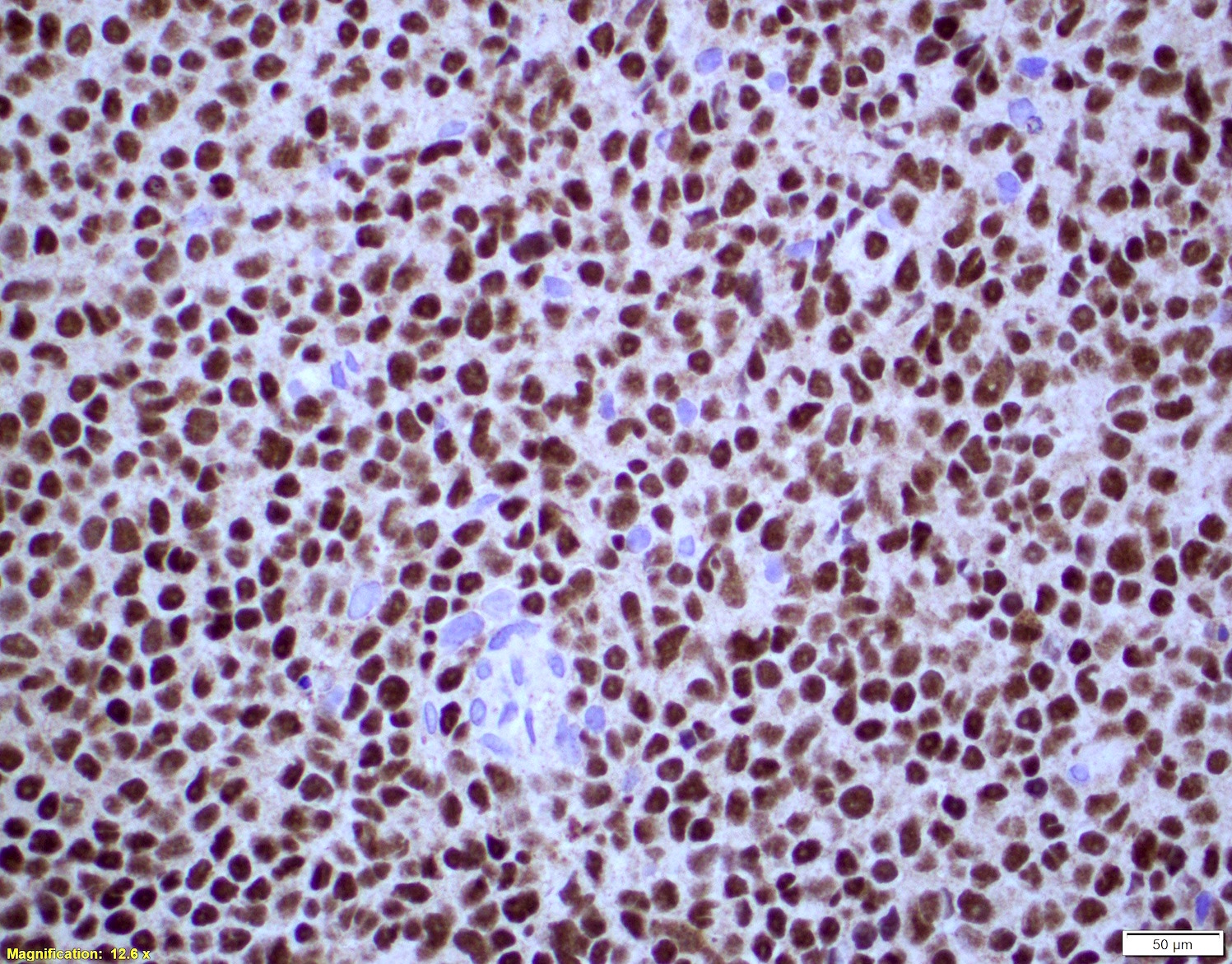
- High cell proliferation (Ki67), 30% cutoff (J Clin Oncol 2016;34:1386)
- Note: Ki67 index overrides the prognostic significance of the cytology subtype (J Clin Oncol 2016;34:1386)
- Other prognostic factors
- CNS involvement
- MYC translocation or overexpression
- Complex karyotype
- Ibrutinib refractory mantle cell lymphoma (Br J Haematol 2018;183:578)
- ATM, TP53 and NSD2 mutations
- TP53 protein expression or mutational analysis (Blood 2017;130:1903, Blood 2015;126:604)
- Note: More dominant prognostic factor when TP53 detected by IHC and genomic mutations (Int J Oncol 2010;36:699, Blood 2018;131:417)
Case reports
- 45 year old man with blastoid mantle cell lymphoma presenting in leukemic phase (J Clin Diagn Res 2017;11:ED16)
- 65 year old man with blastic transformation of mantle cell lymphoma presenting with acute onset binocular diplopia and proptosis of the left eye (Ocul Oncol Pathol 2019;5:245)
- 66 year old man with cyclin D1 negative blastoid mantle cell lymphoma exhibiting cleaved to bilobated cytomorphology (Blood 2017;129:2711)
- 67 year old woman with triple hit blastoid mantle cell lymphoma presenting like acute leukemia (Blood 2017;129:2593)
- 74 year old man with ascites, liver lesions and growing 5 cm soft tissue abdominal mass (Case #499)
- A case of double hit mantle cell lymphoma (Am J Clin Pathol 2020;153:49)
Treatment
- Aggressive chemotherapy or stem cell transplantation
- Ibrutinib with rituximab (IR) induction
- Followed by R-HCVAD-methotrexate / ara-C
- R-HyperCVAD used at many institutions
- Rituximab, hyperfractionated cyclophosphamide, vincristine, doxorubicin, dexamethasone
- Alternating with methotrexate and cytosine arabinoside (ara-C)
- Venetoclax may be added in some trials
- Stem cell transplant (allogenic versus autologous)
- Autologous SCT: in cases that respond well to initial chemotherapy (Blood 2018;132:2722)
- CNS prophylaxis
- Reference: Am J Hematol 2019;94:710
Gross description
- Lymph node
- Generalized enlargement
- Homogenous tan cut surface
- With or without nodules
- Not distinctive
- GI
- Lymphomatoid polyposis
- Multiple lymphoid polyps, small and large bowel
- Ulcers, tumor masses and diffuse thickening of the mucosa
- Spleen
- Generalized micronodular pattern
- Perivascular infiltration
Frozen section description
- Same criteria applied in microscopic evaluation
- Cytogenetics, flow cytometry, preparation of imprints should be considered
- The nuclear shape, size and chromatin structure are helpful in smears
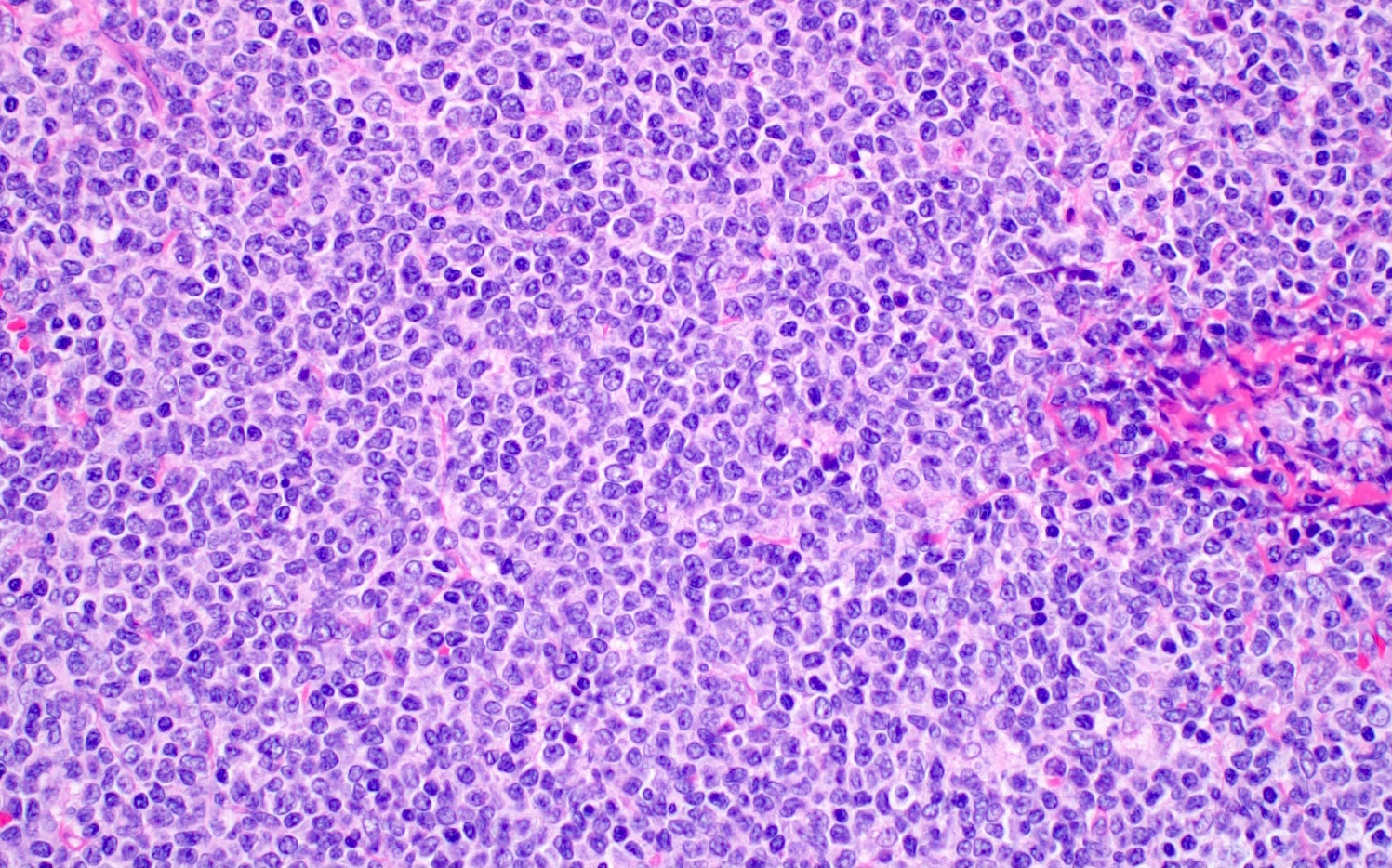
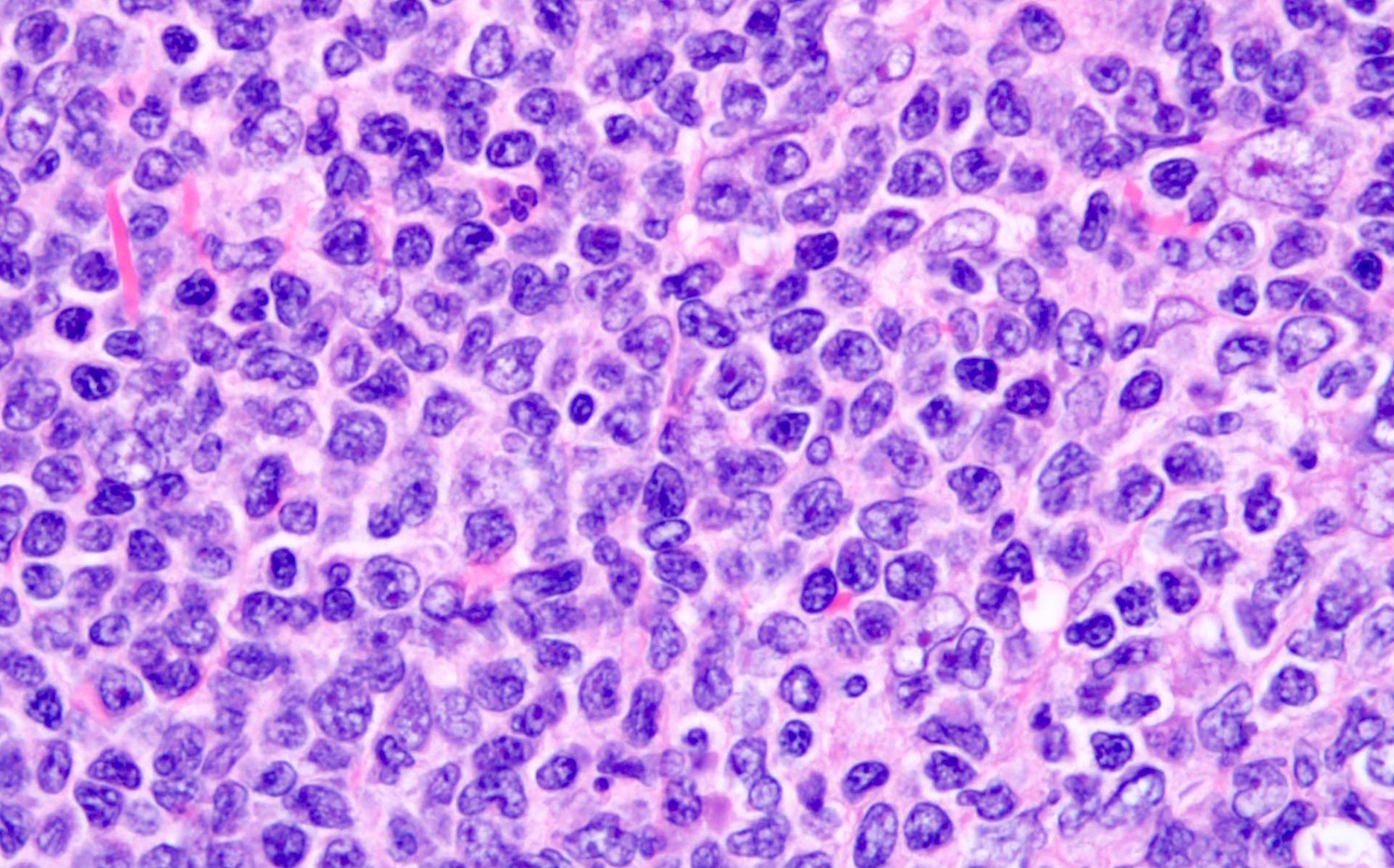
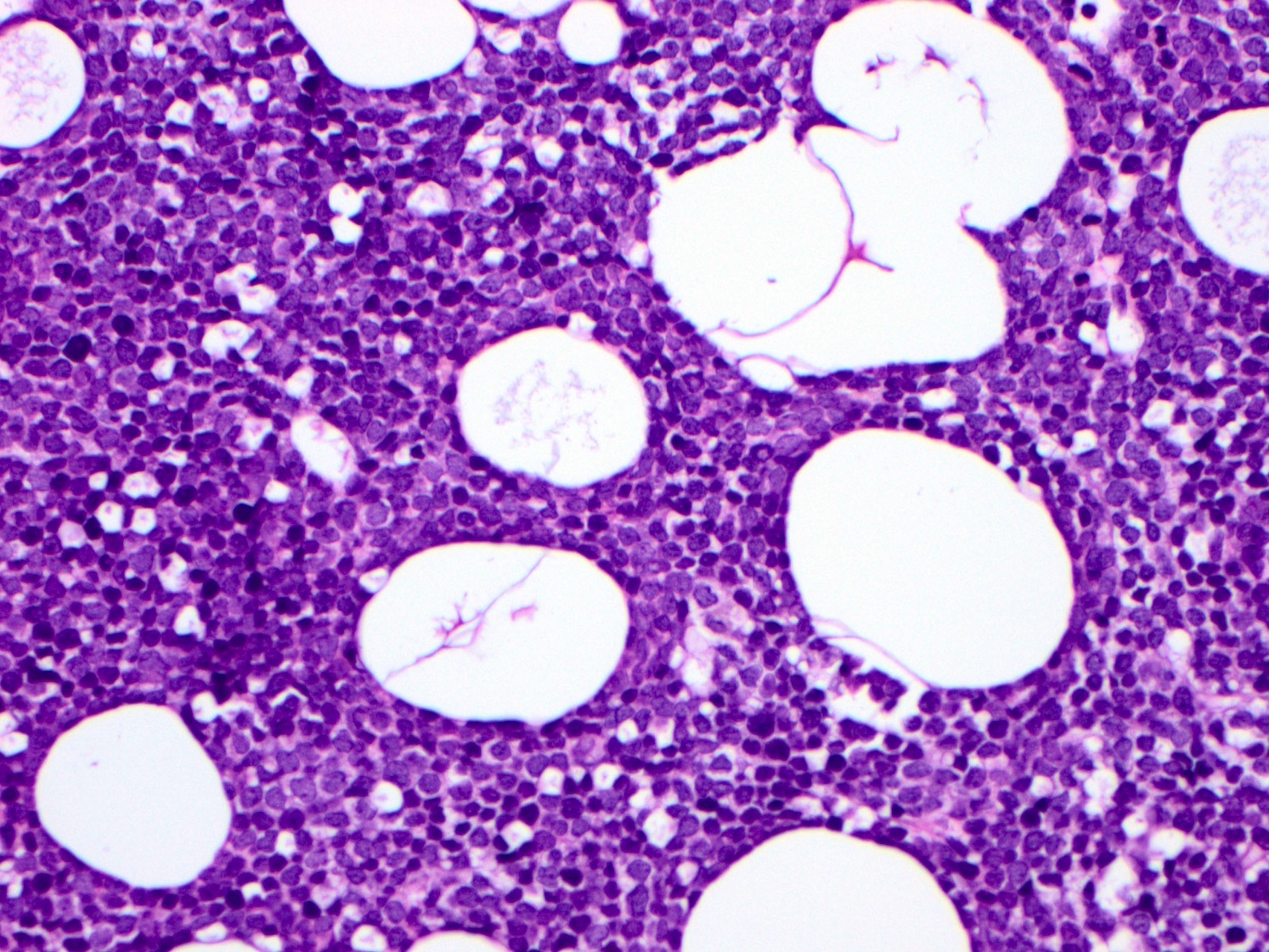
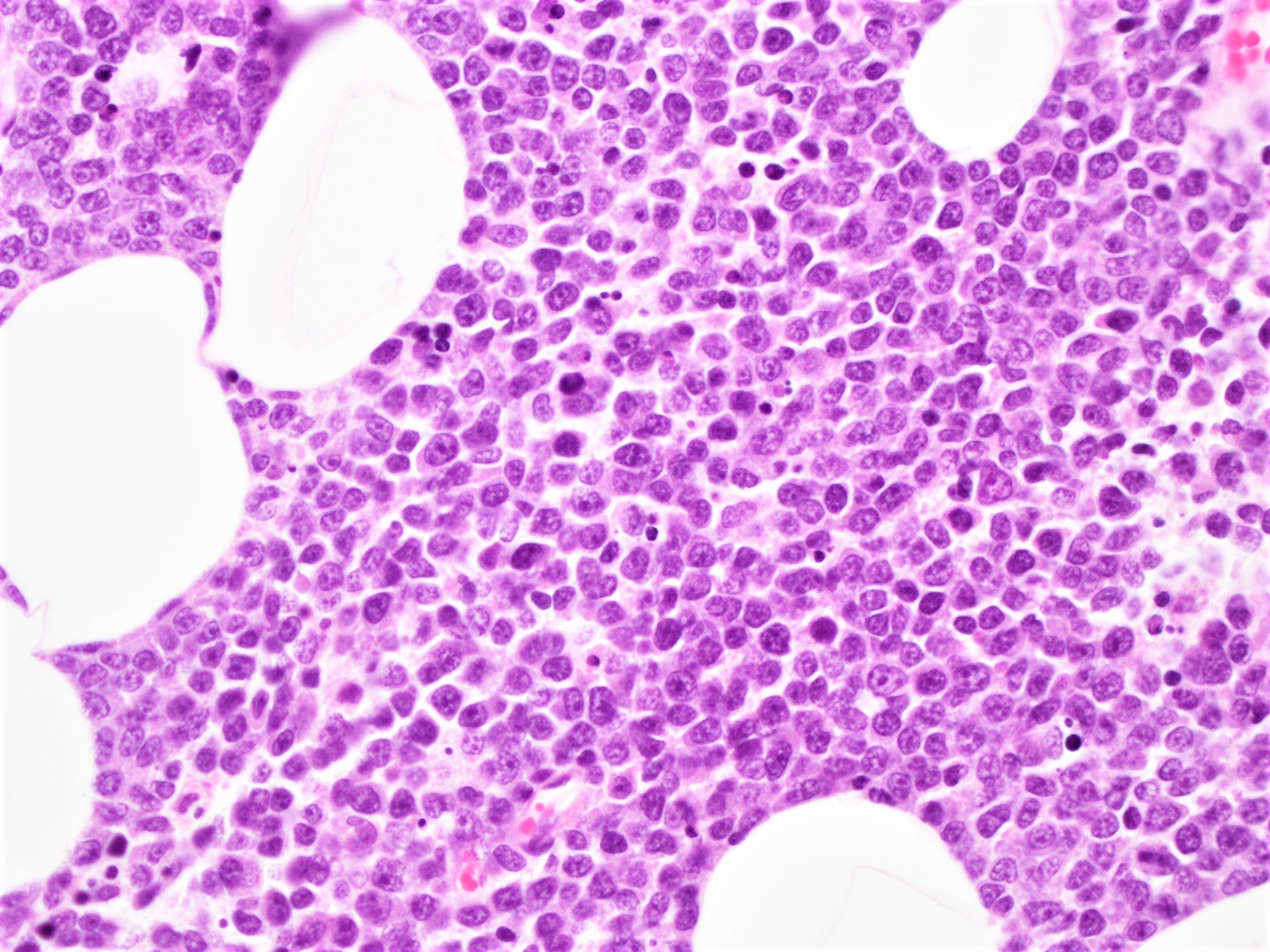
Microscopic (histologic) description
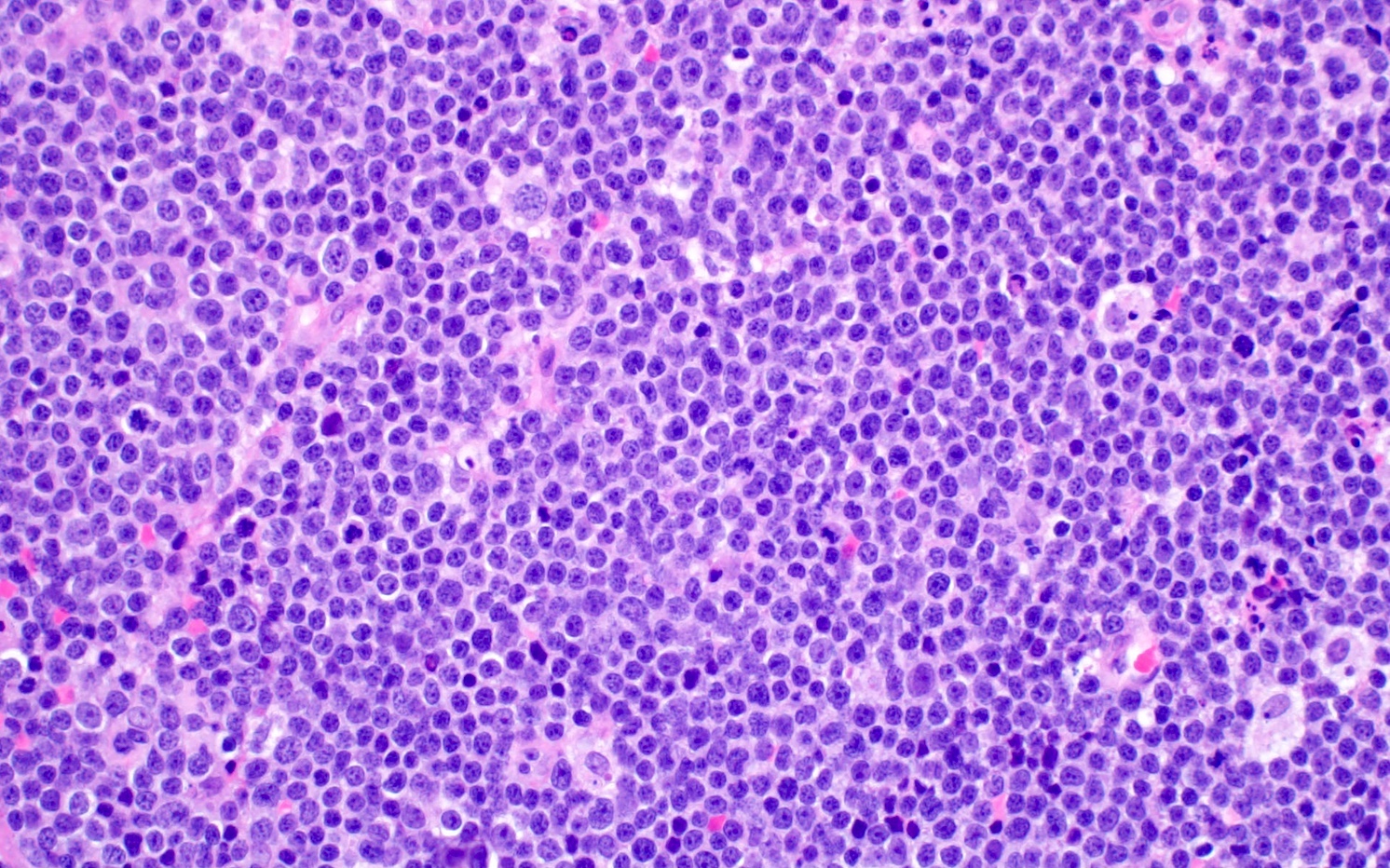
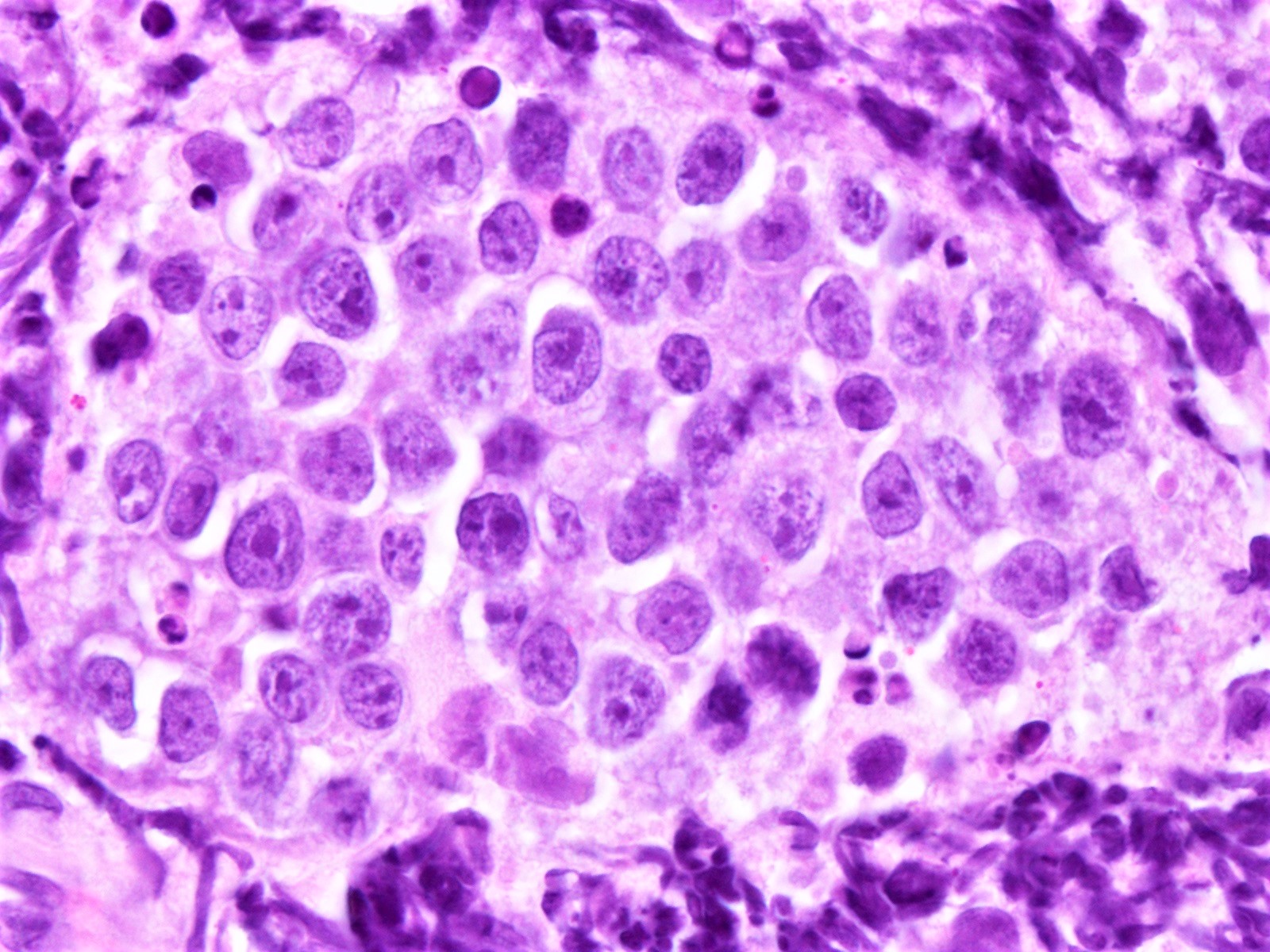
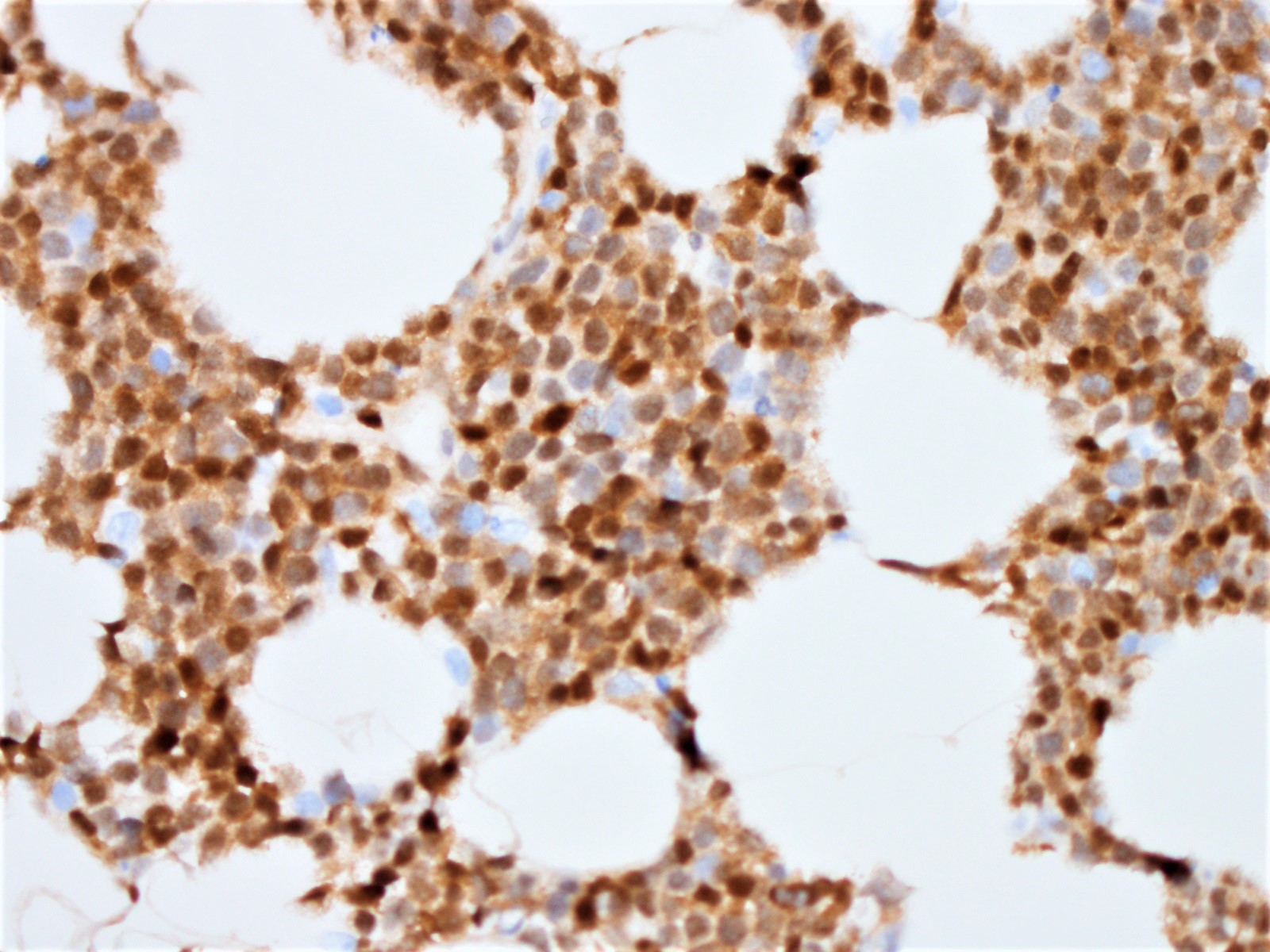
- Blastoid variant
- The growth pattern is usually diffuse
- Less frequently nodular pattern
- Starry sky appearance common in low power
- Intermediate sized cells
- Monotonous population
- Immature chromatin
- Scant cytoplasm
- High mitotic rate > 20 - 30/10 high power fields
- Resembles, in part, lymphoblastic lymphoma
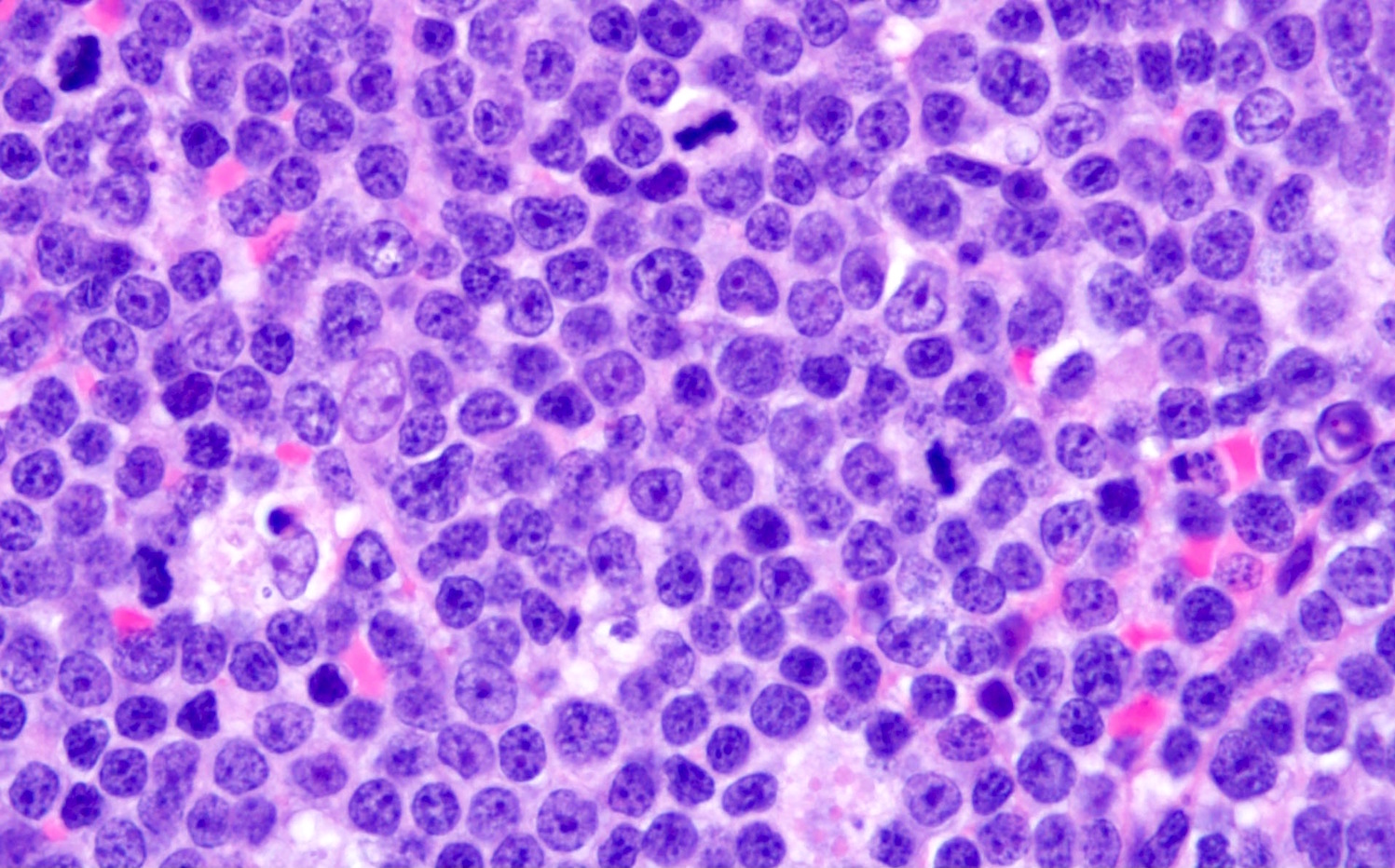
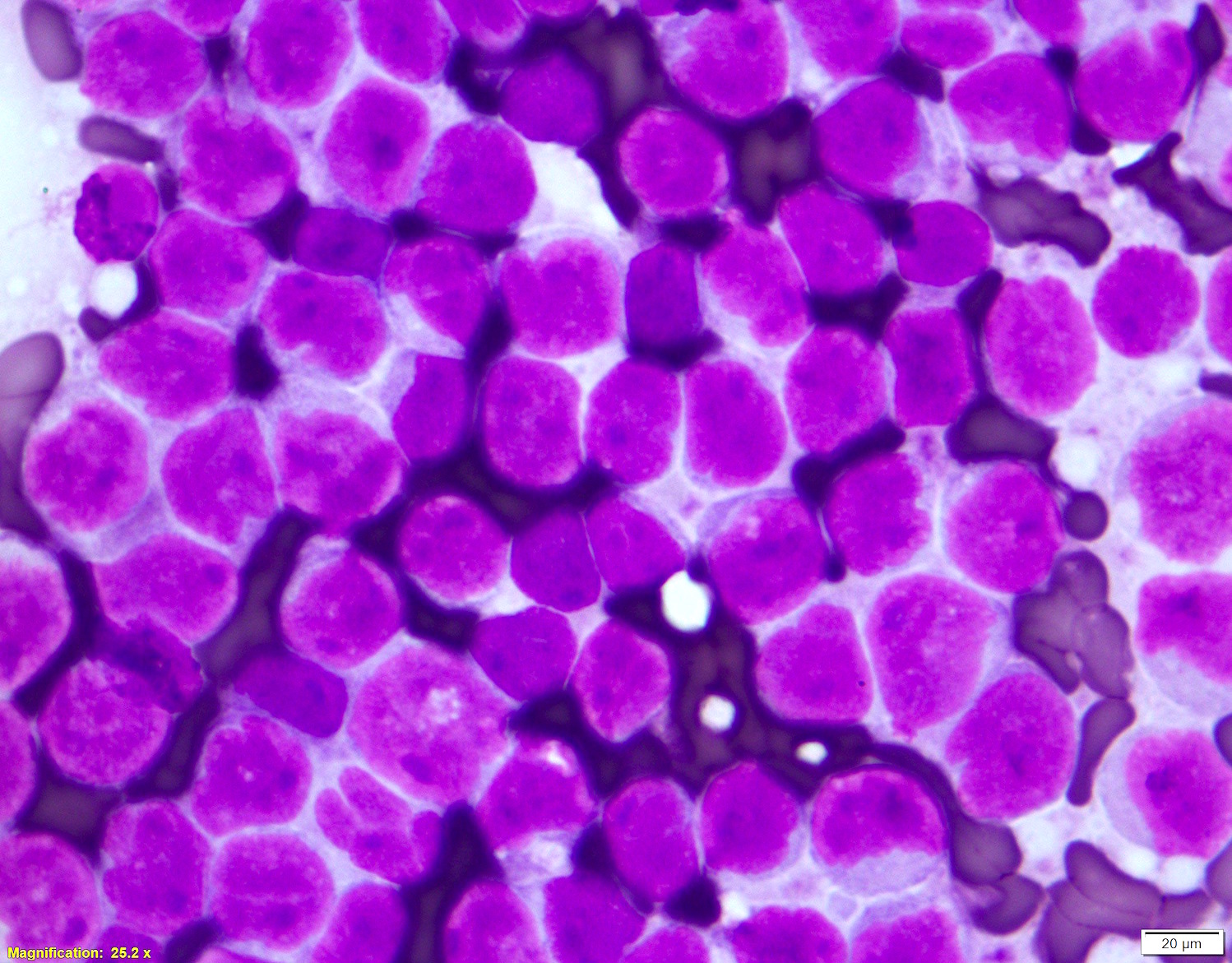
- Pleomorphic variant
- Variable size / heterogenous cell population including large cells
- Prominent nucleoli +/-
- High mitotic rate often seen
- At least 10 mitoses per 10 high power fields and often higher rates
- Resembles, in part, diffuse large B cell lymphoma
- Peripheral blood lymphocytes are intermediate sized with prominent nucleoli
- Resemble prolymphocytes to variable degree
- Multinucleation or cerebriform nuclei often seen
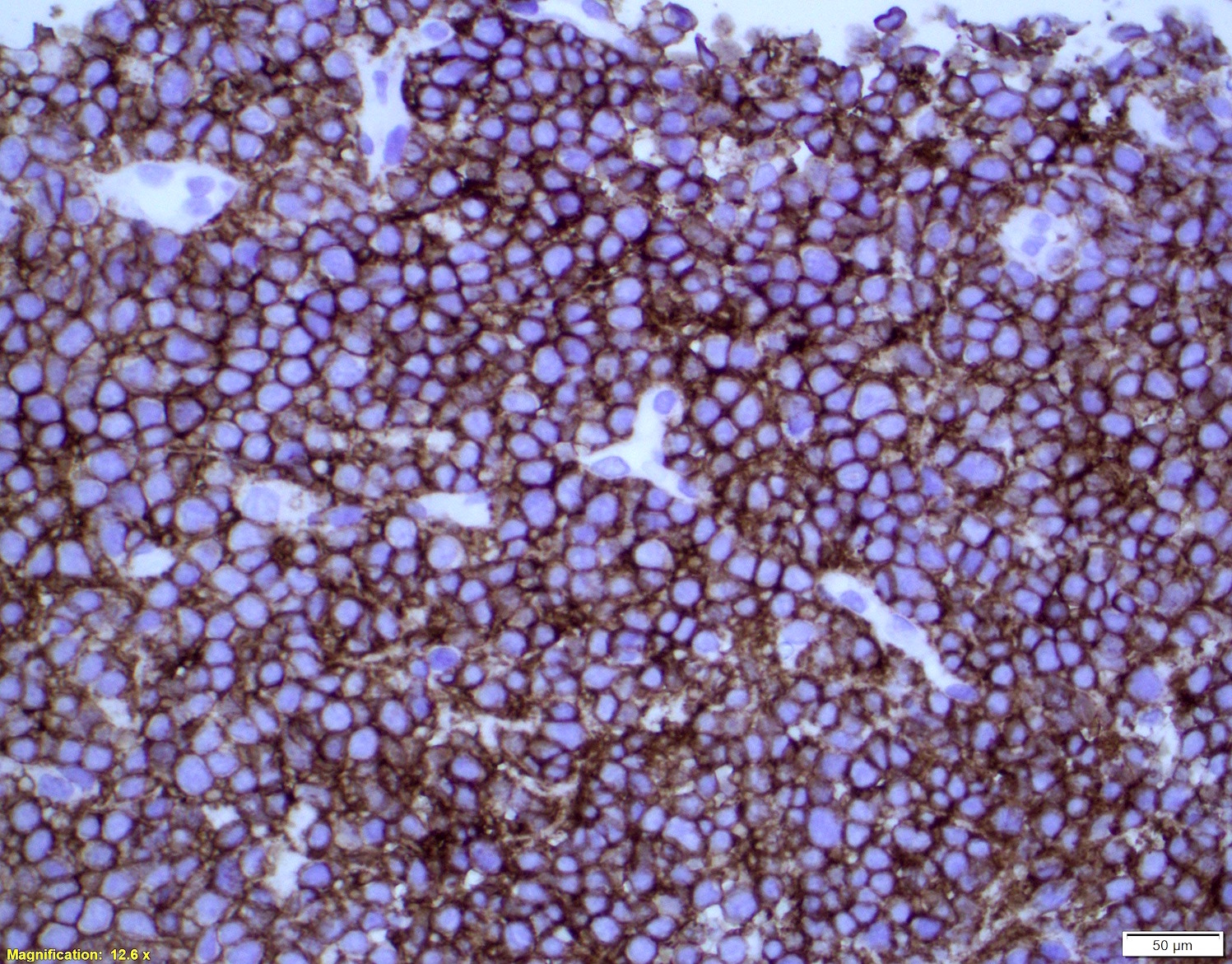
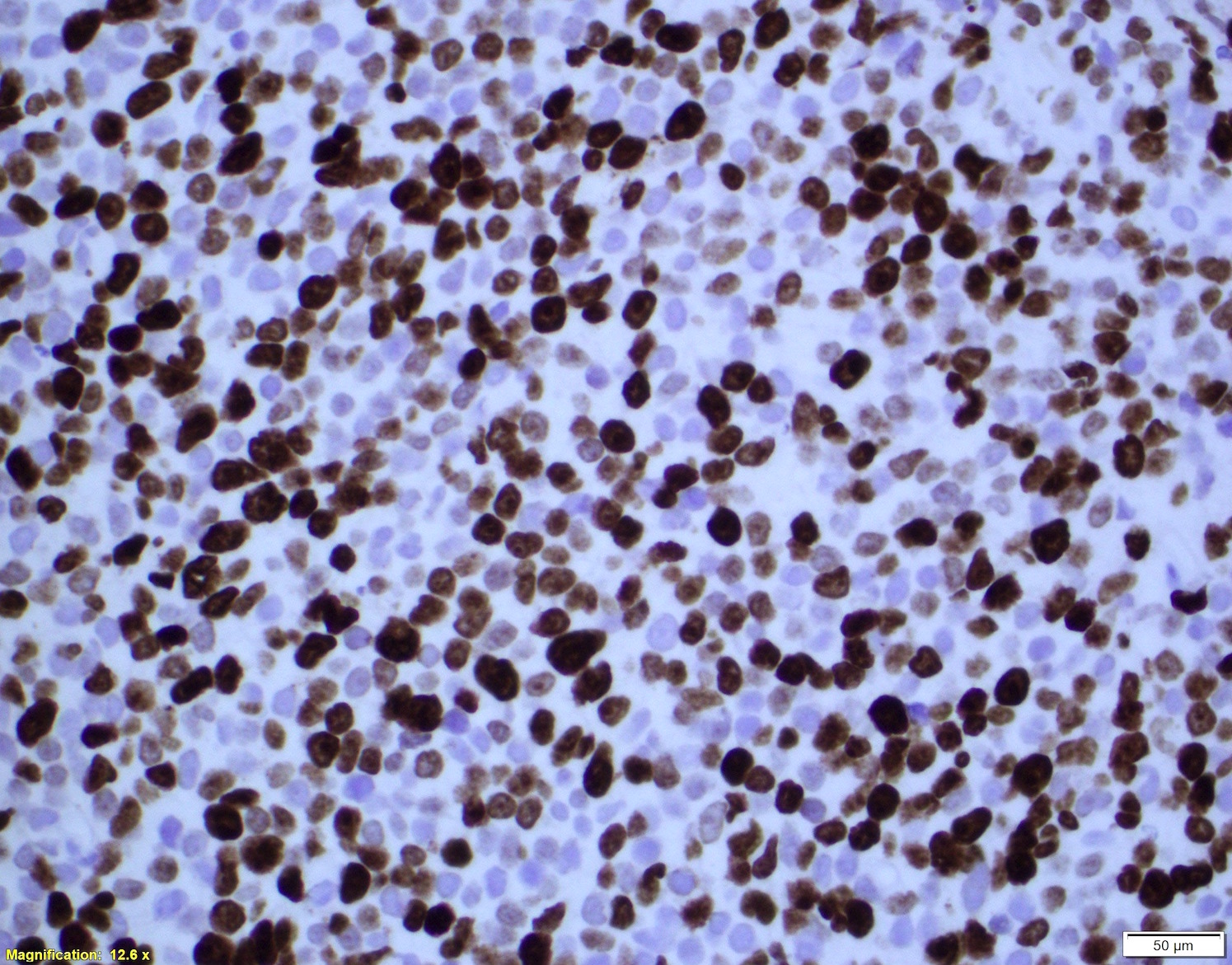
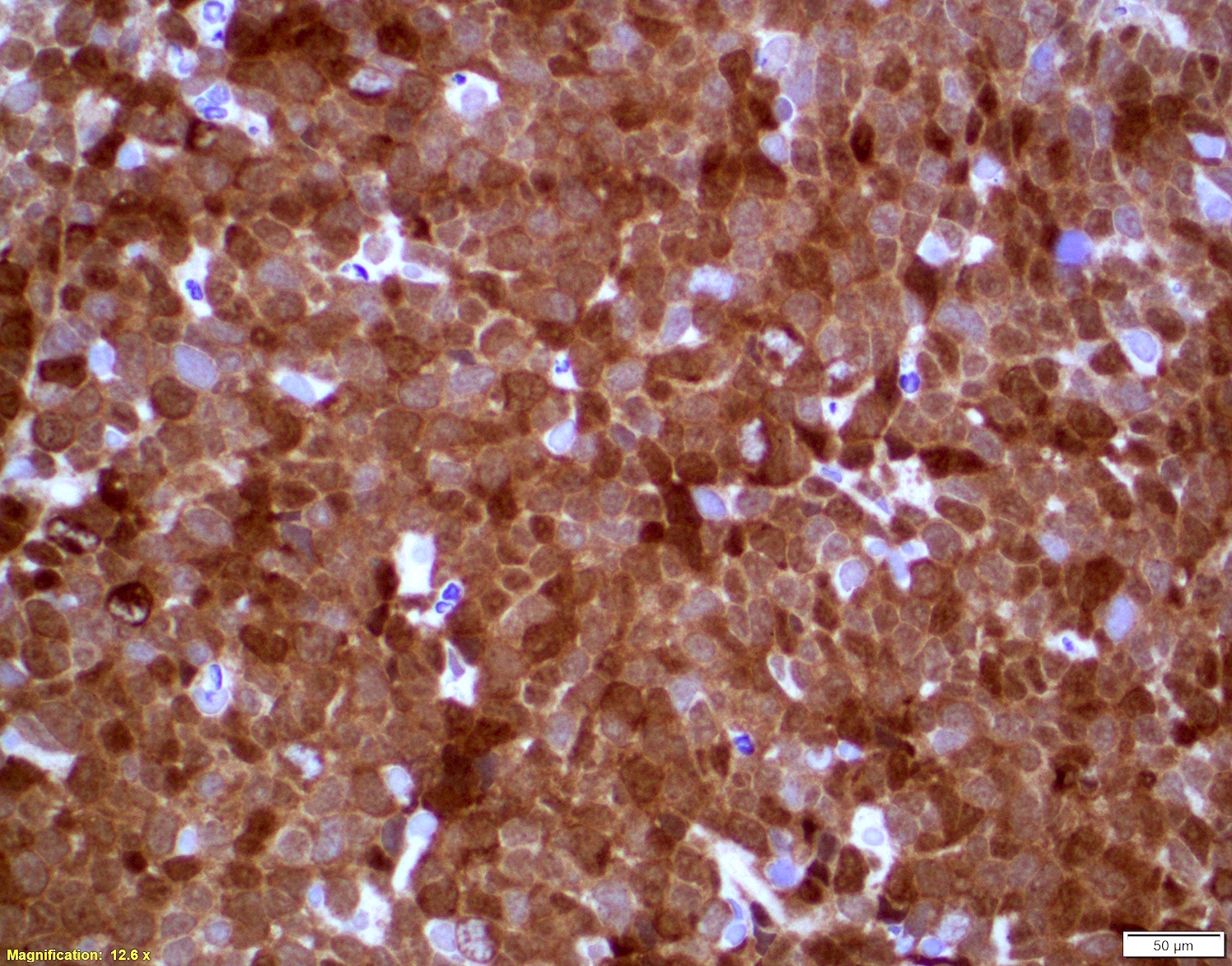
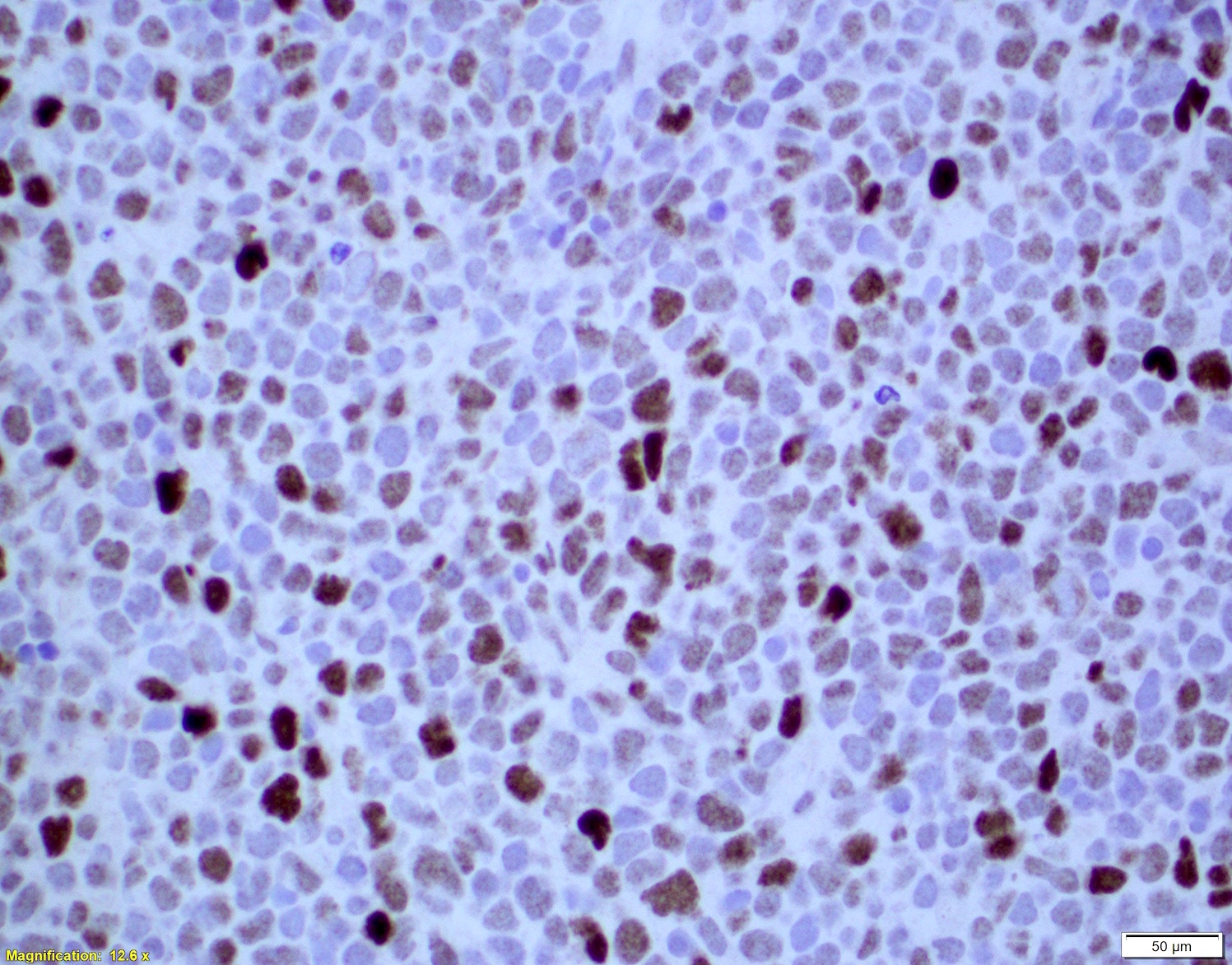
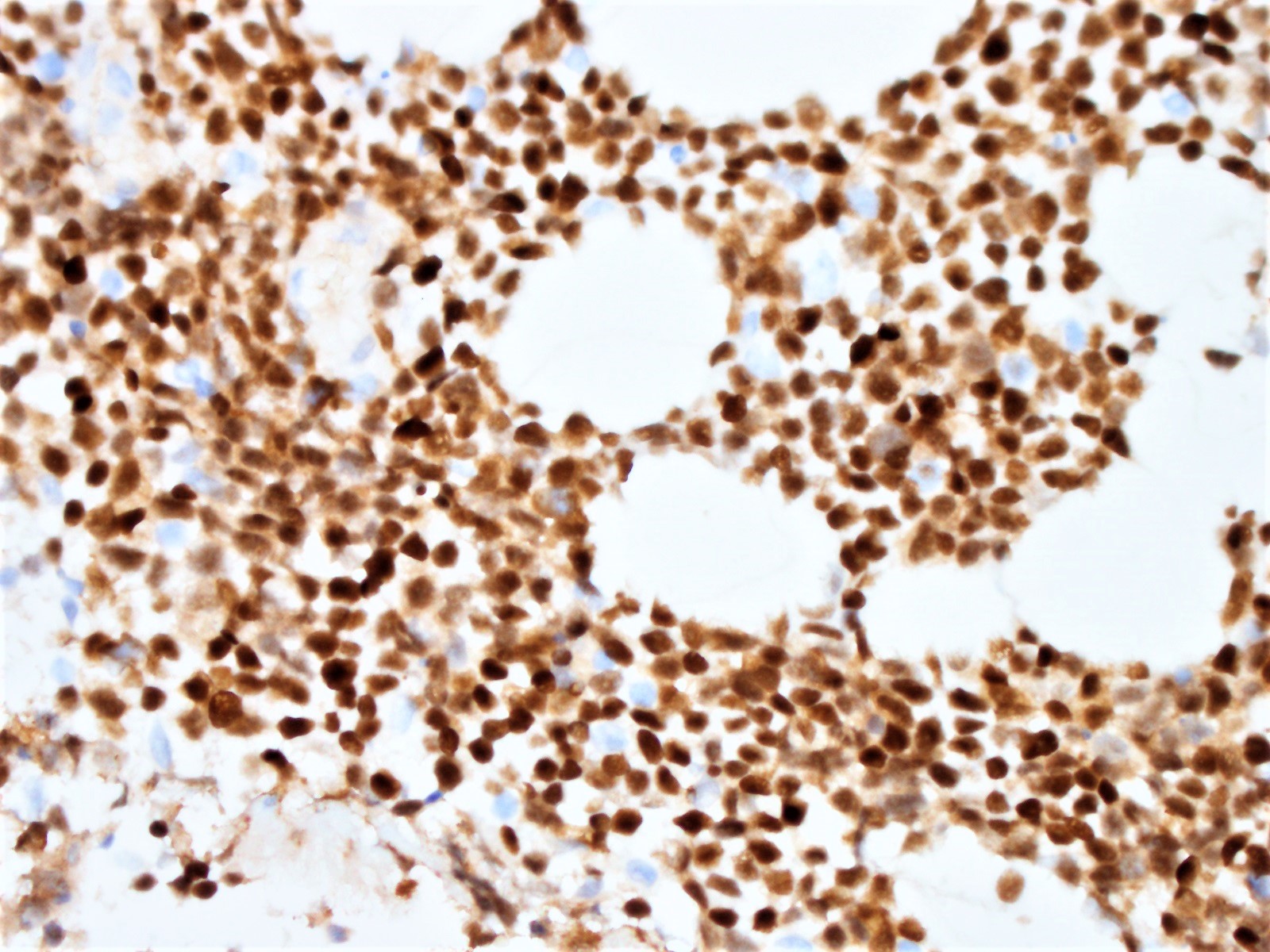
Microscopic (histologic) images
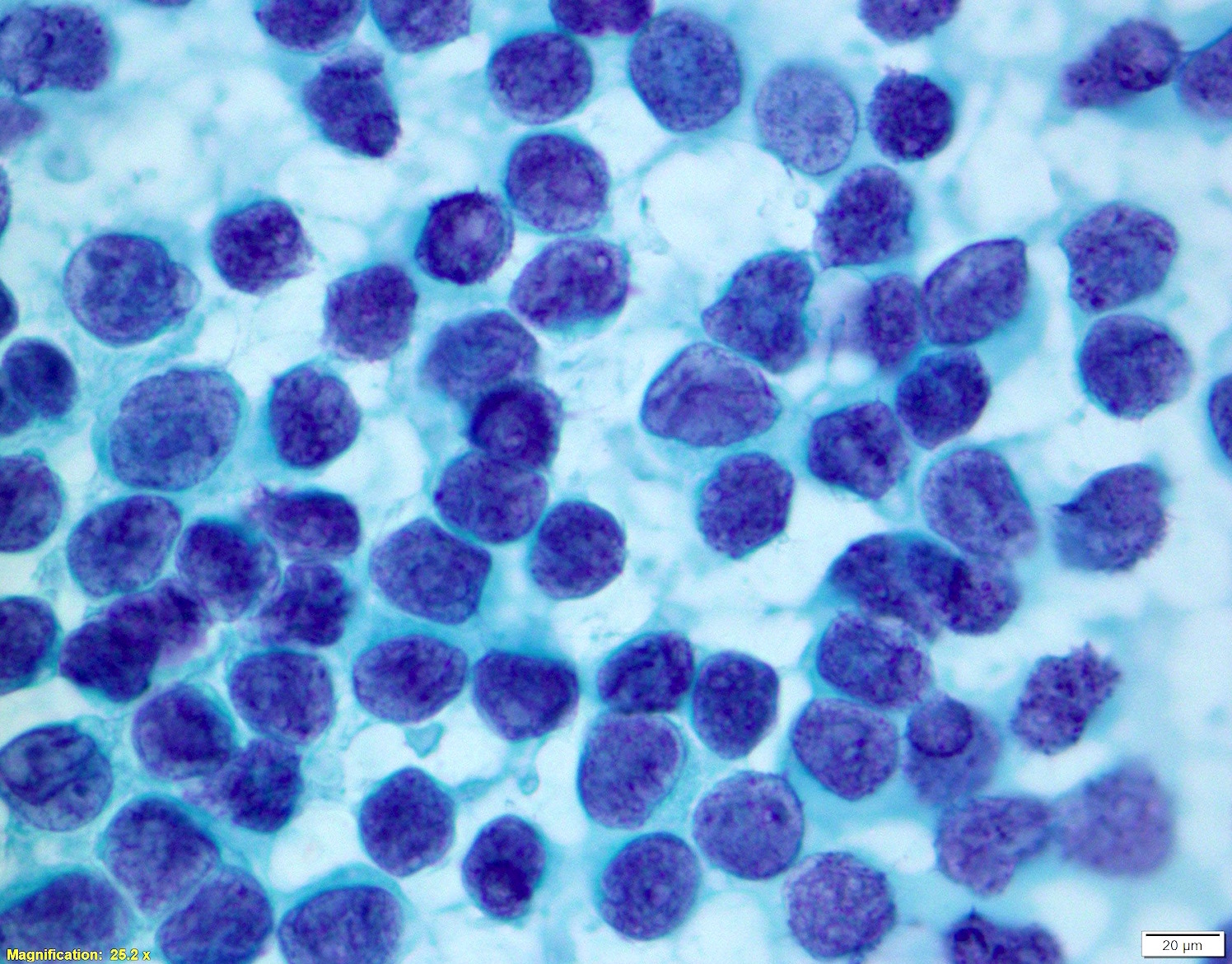
Cytology description
- Blastoid variant
- Monomorphic proliferation of intermediate sized to large lymphoid cells
- Round to oval nuclear contours
- Dispersed chromatin
- Small / inconspicuous nucleoli
- Scant, pale blue cytoplasm
- Pleomorphic variant
- Large, pleomorphic cells
- More nuclear irregularity
- More variation in size of cells
- Vesicular, open chromatin
- Prominent nucleoli often seen (Br J Haematol 1996;93:475)
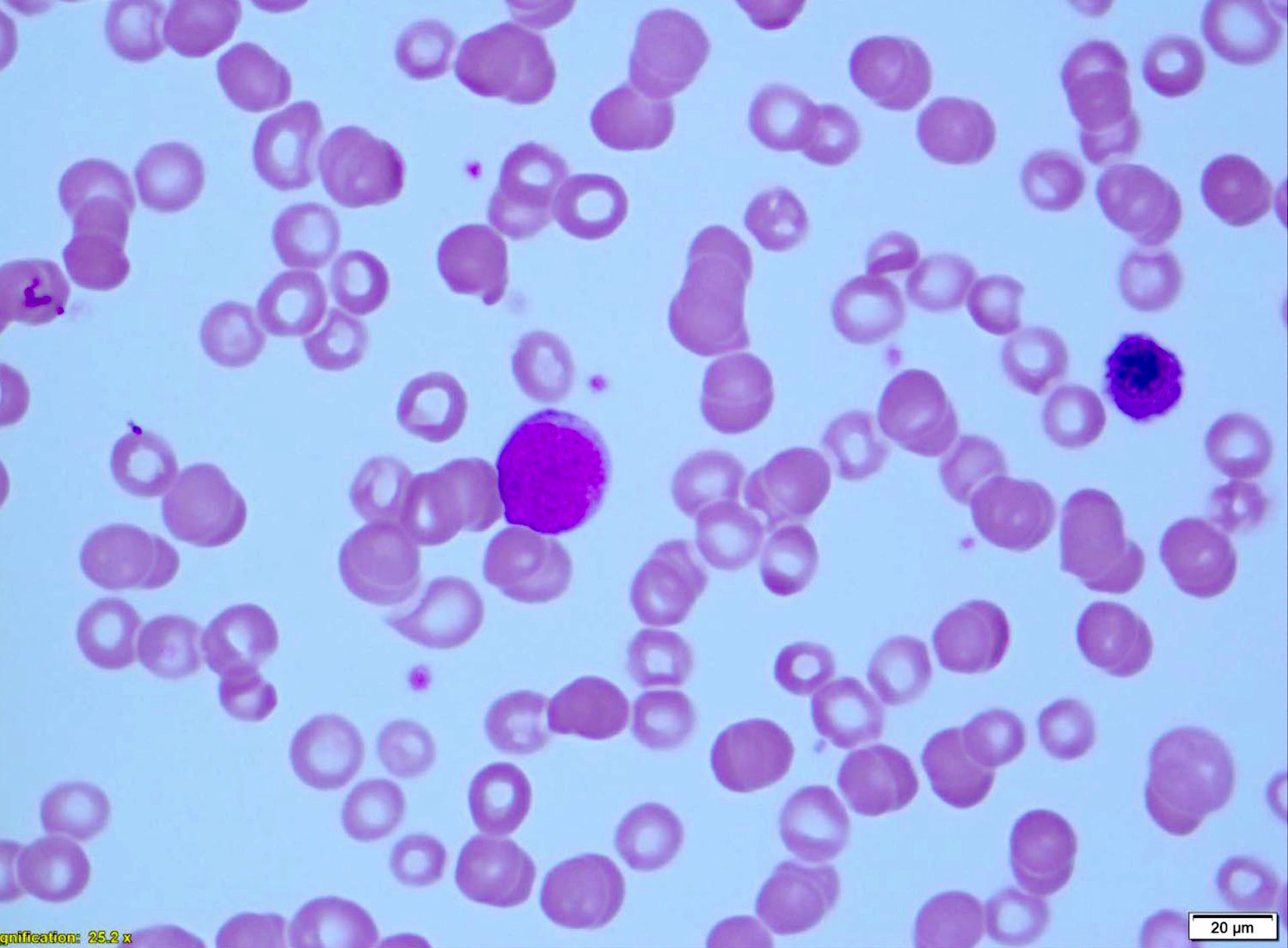
Peripheral smear description
- Prolymphocytoid-like morphology (leukemic form of mantle cell lymphoma)
- Patients present with high leukocyte count (often > 100 x 109/L)
- Extensive bone marrow involvement
- Prominent nucleoli in circulating cells in blood
- Intermediate to large sized cells
- A single, prominent pink nucleolus
- Prominent splenomegaly
- A subset are pleomorphic mantle cell lymphomas (Am J Clin Pathol 2001;115:571, Leuk Lymphoma 2001;41:683, Am J Clin Pathol 2002;117:246)
- Blastoid morphology (leukemic form of blastoid mantle cell lymphoma)
- High leukocyte count
- Extensive bone marrow involvement
- Blastoid morphology
- Complex karyotypes
- 8q24 anomalies and MYC rearrangements (Mod Pathol 2002;15:1266, Br J Haematol 2001;115:66)
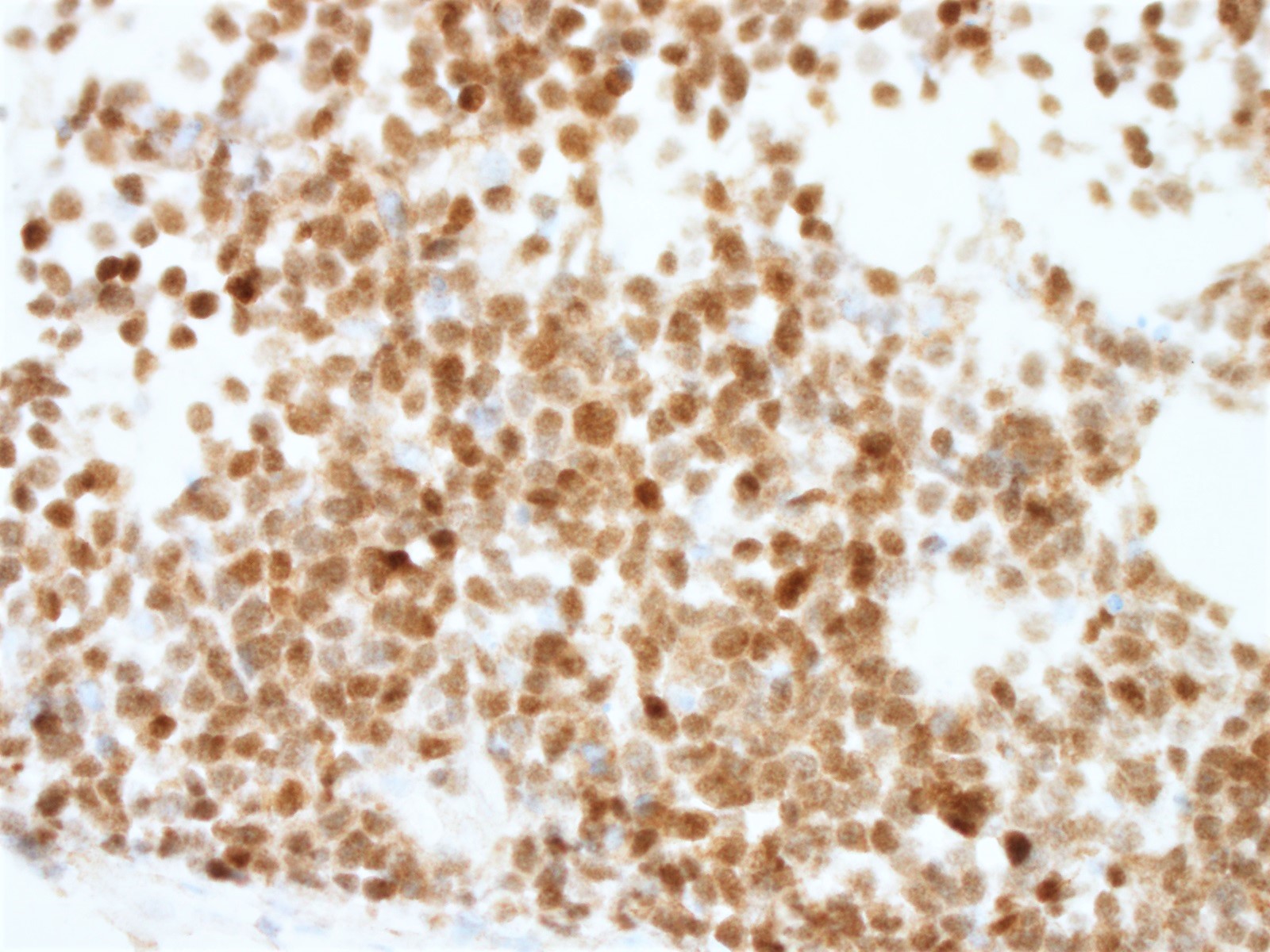
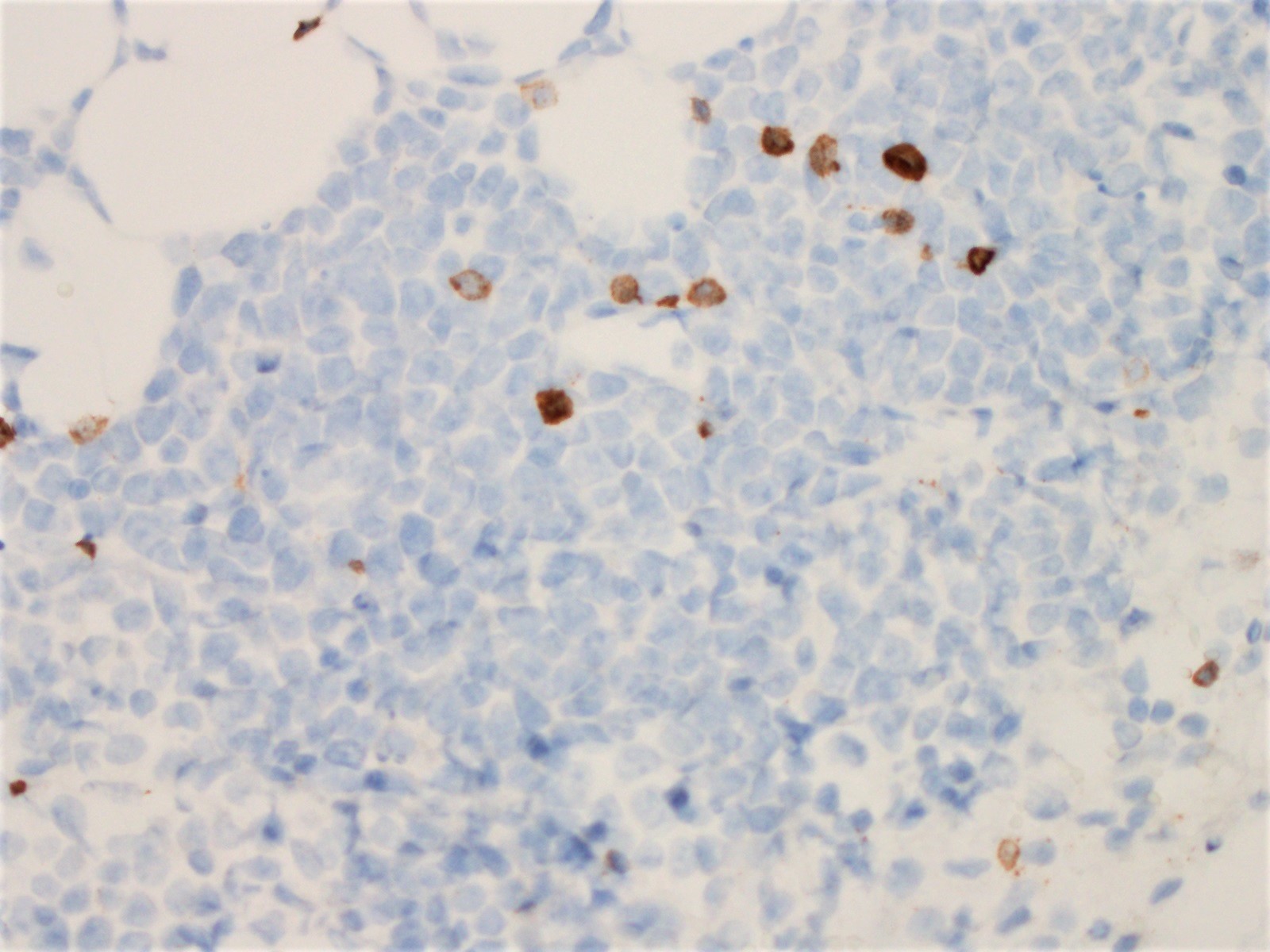
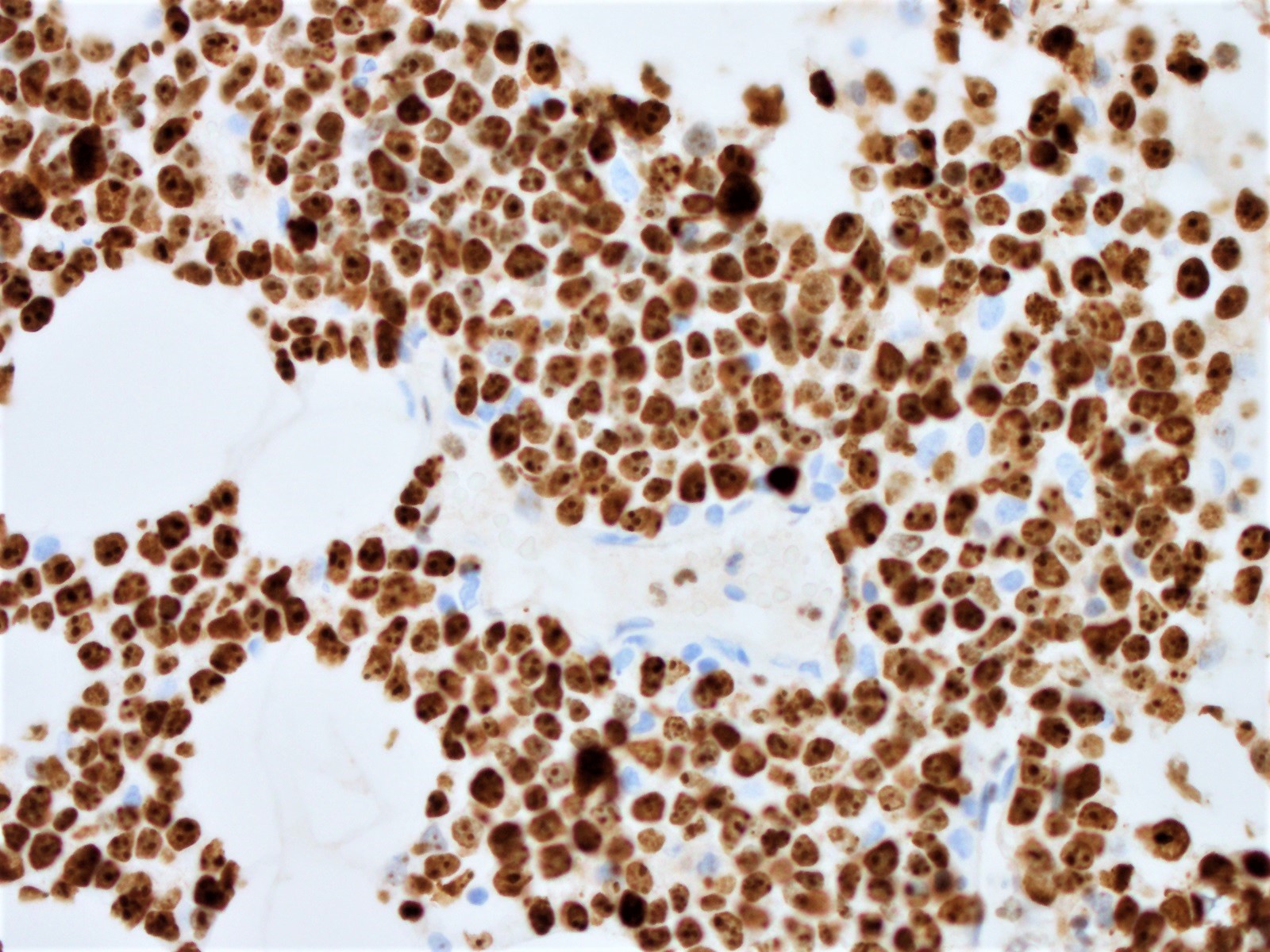
Positive stains
- Immunophenotype similar to classic mantle cell lymphoma
- Cyclin D1
- CD19, CD20, CD43, sIg, IgM with or without IgD
- CD5 (> 95%), SOX11 (> 90%)
- Exceptions:
- SOX11 negative cases
- More indolent
- Leukemic / non-nodal involvement (Am J Surg Pathol 2019;43:710)
- Mutated IGHV
- CD5 negative cases (Am J Surg Pathol 2019;43:1052)
- Cyclin D1 positive
- Cyclin D1 negative cases
- SOX11 positive
- SOX11 negative cases
- MUM1 / IRF4 (50% in small subset)
- BLIMP1 (50%) and XBP1 (30%)
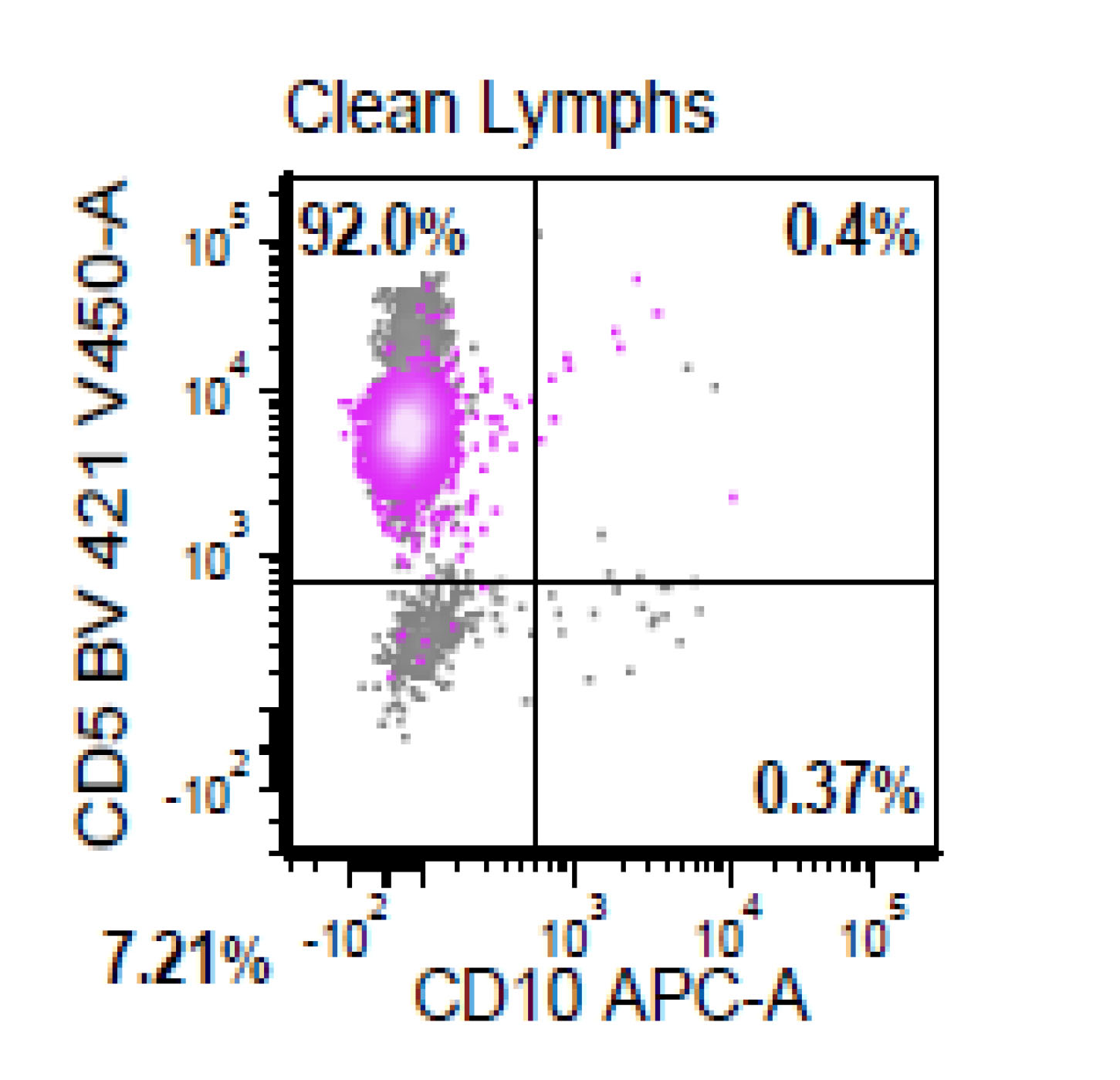
- Small number of mantle cell lymphomas are positive for CD10 (Oncotarget 2017;9:11441)
- Ki67 count (J Hematop 2009;2:103)
- Five independent high power fields count
- Avoidance of residual germinal centers, hot spots and proliferating T cells
- Note: Ki67 index is not sufficient to classify as blastoid or pleomorphic subtype
- Classical mantle cell lymphoma might also show high cell proliferation (Blood 2008;111:2385)
- p53 in subset; intense expression correlates with TP53 gene mutation
- Note: no protein expression; on the other hand, cannot predict the homozygous deletions of the locus (Blood 1996;87:3351)
- MYC in subset
- High expression correlates with MYC translocation (Blood 2017;129:333)
- CD10 or BCL6 expression commonly seen (Oncotarget 2017;9:11441, Am J Surg Pathol 2004;28:1051, Histopathology 2008;53:20)
- CD23: small subset of cases (Mod Pathol 1996;9:925)
Negative stains
- CD200
- May be positive in a subset of SOX11 negative mantle cell lymphomas
- LEF1
- Can be positive in 4 - 9% of mantle cell lymphomas (Ann Diagn Pathol 2017;26:57)
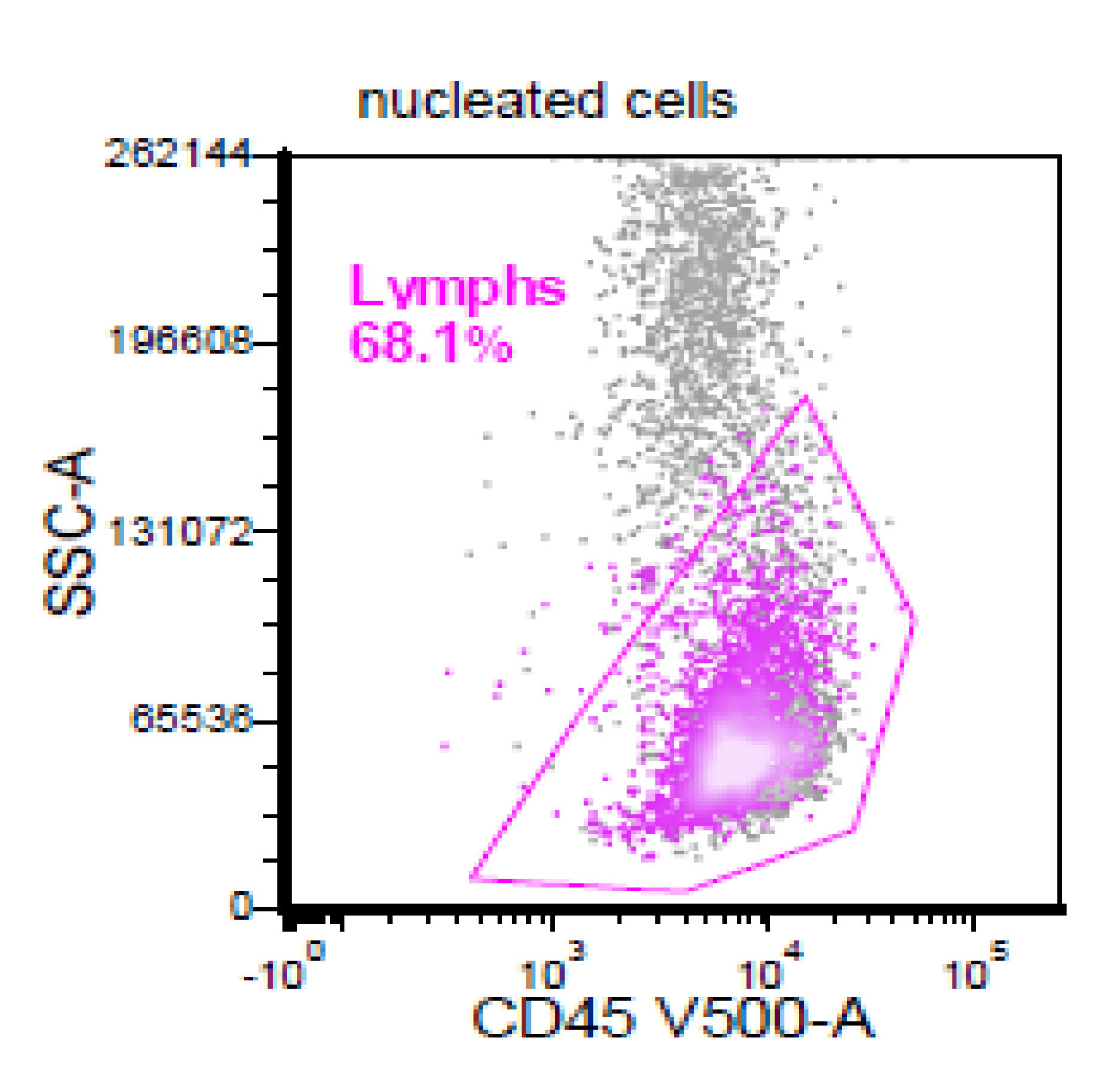
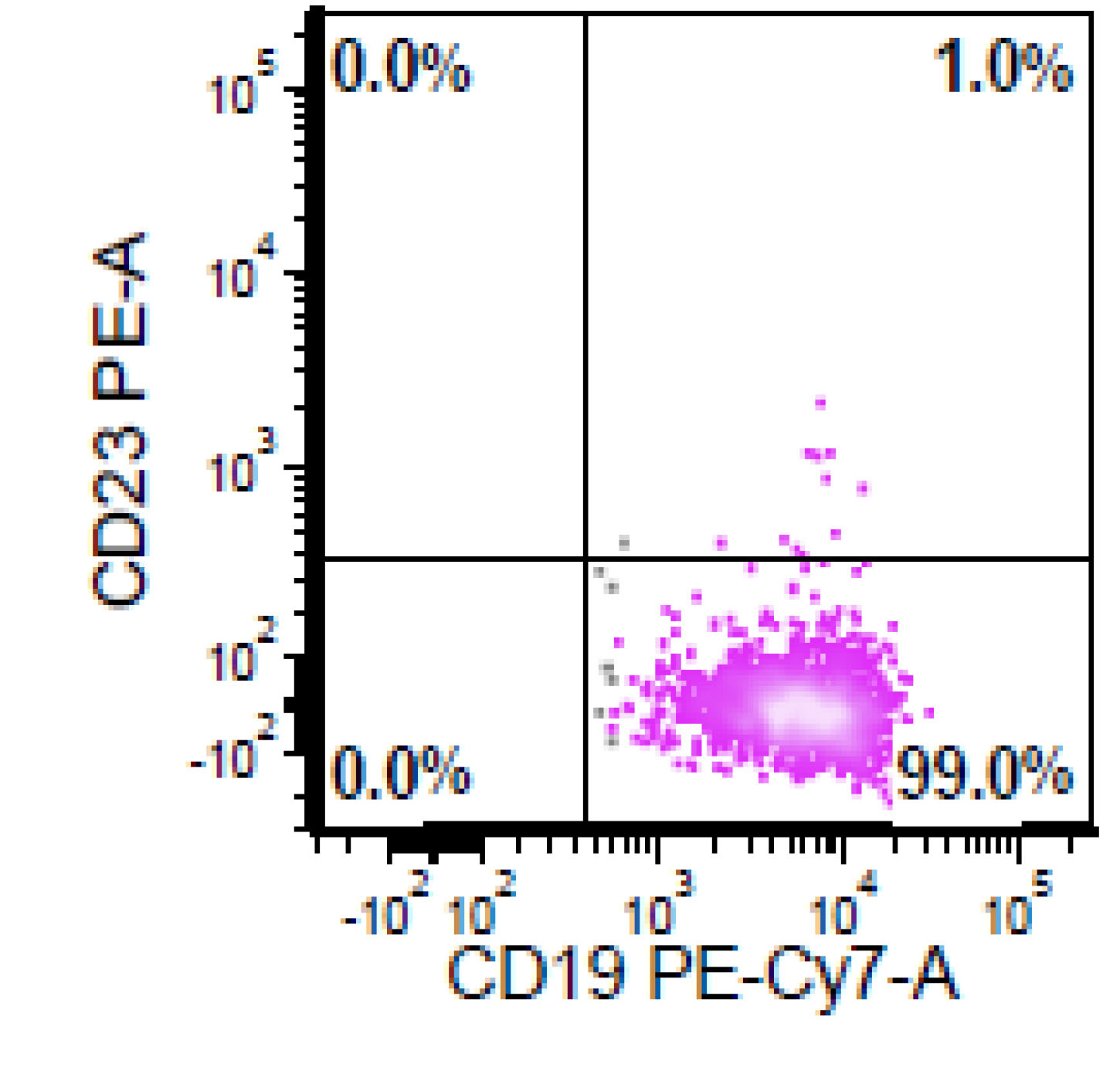
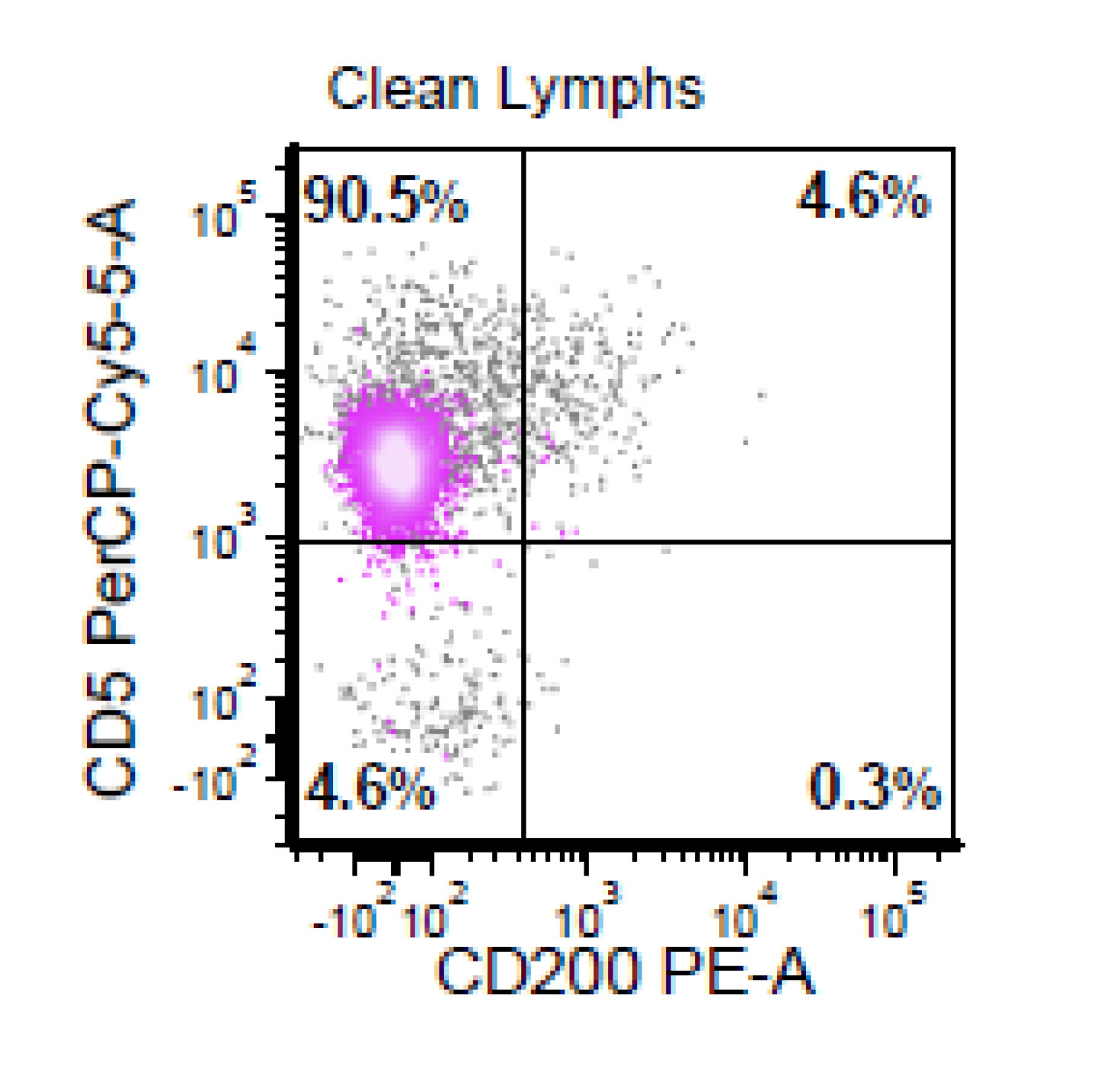
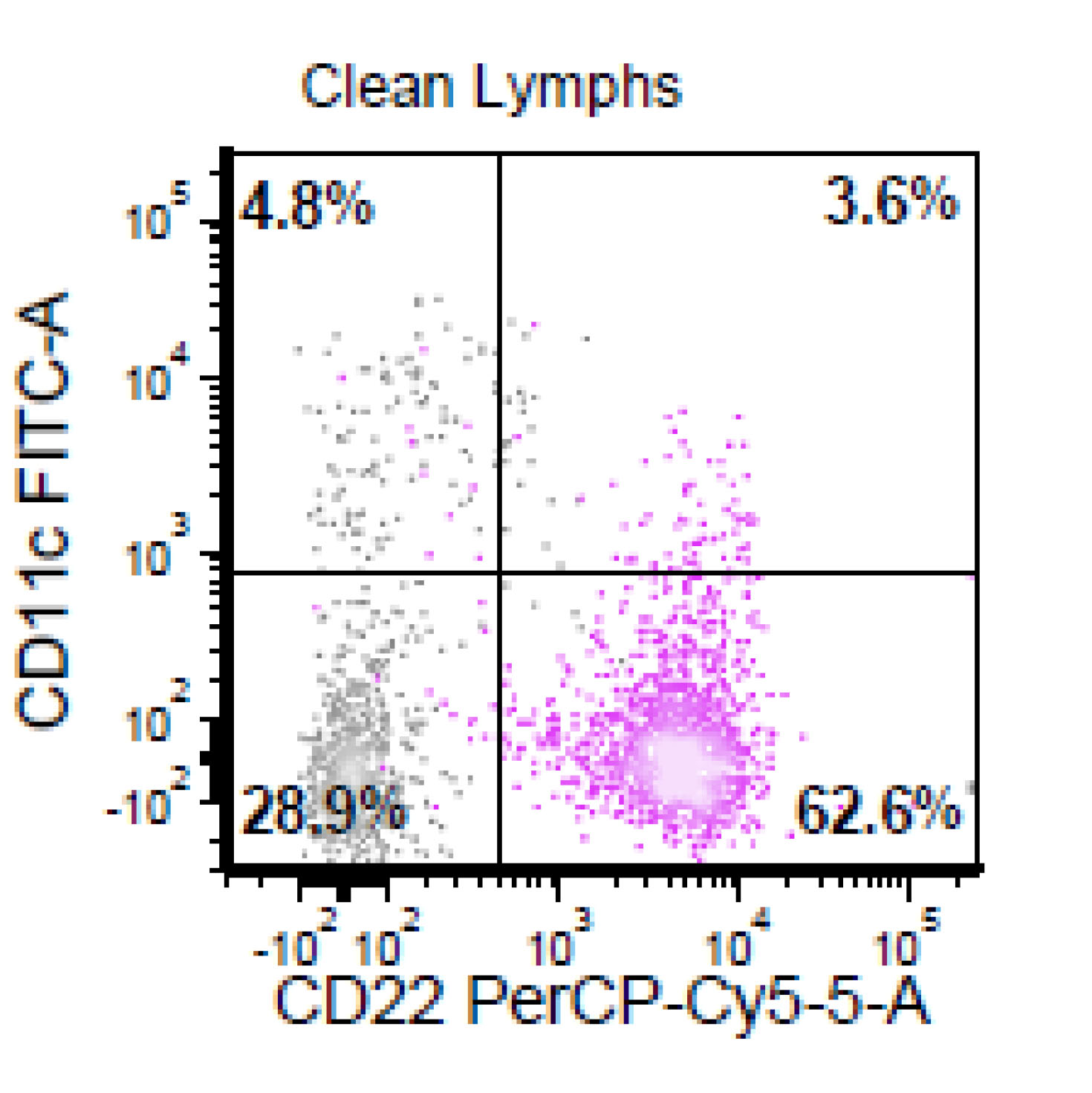
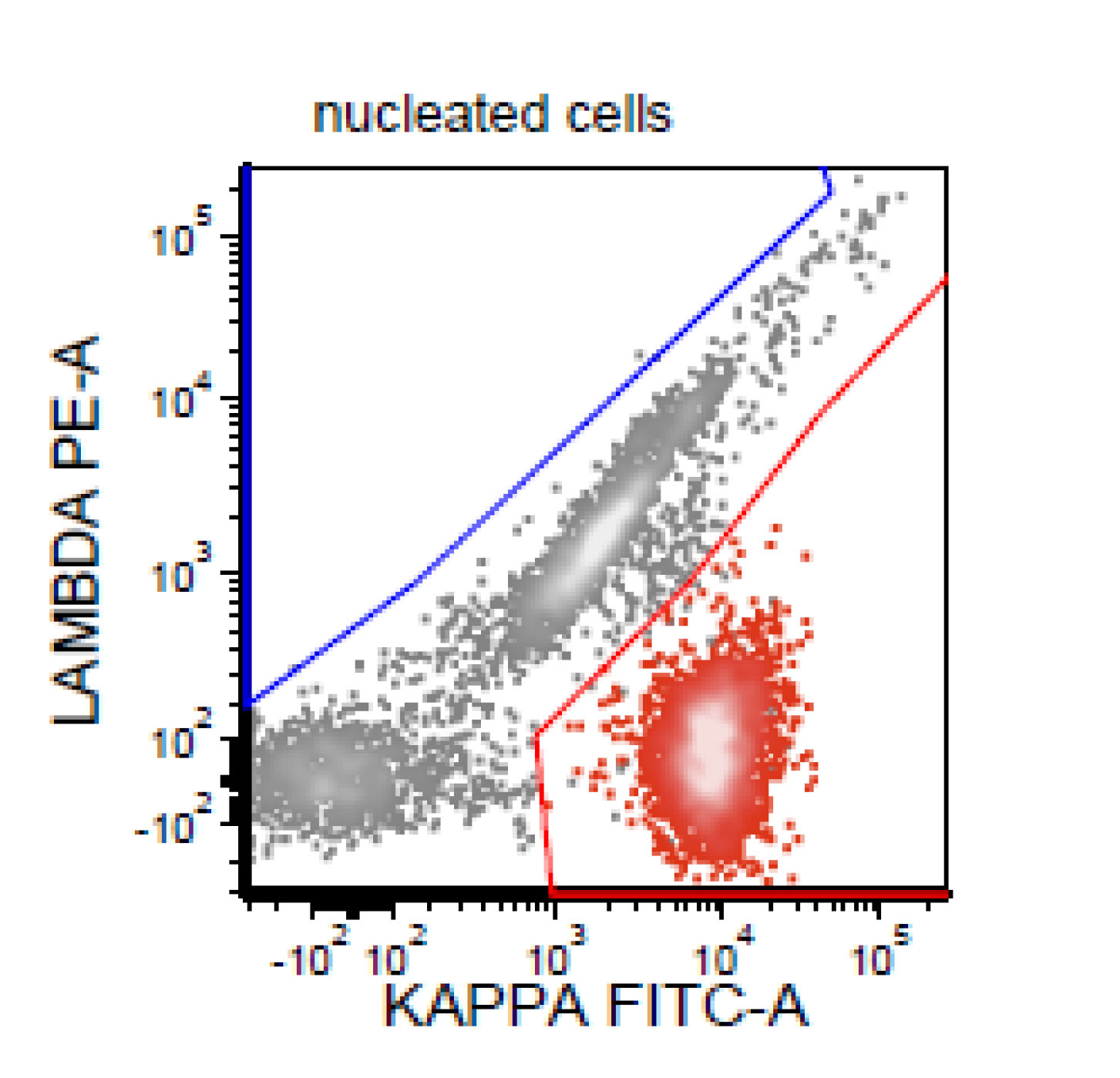
Flow cytometry description
- CD5+, CD19+, CD20+, CD22+, CD79b+, FMC7+
- Monotypic Ig (high level expression of surface light chains)
- CD11c variable, CD43 variable, CD200 variable
- CD3-, CD10-, CD23-
- Rare cases have atypical immunophenotype:
- CD5- or CD10+, CD200+ or CD23+ (dim ~10%)
Flow cytometry images
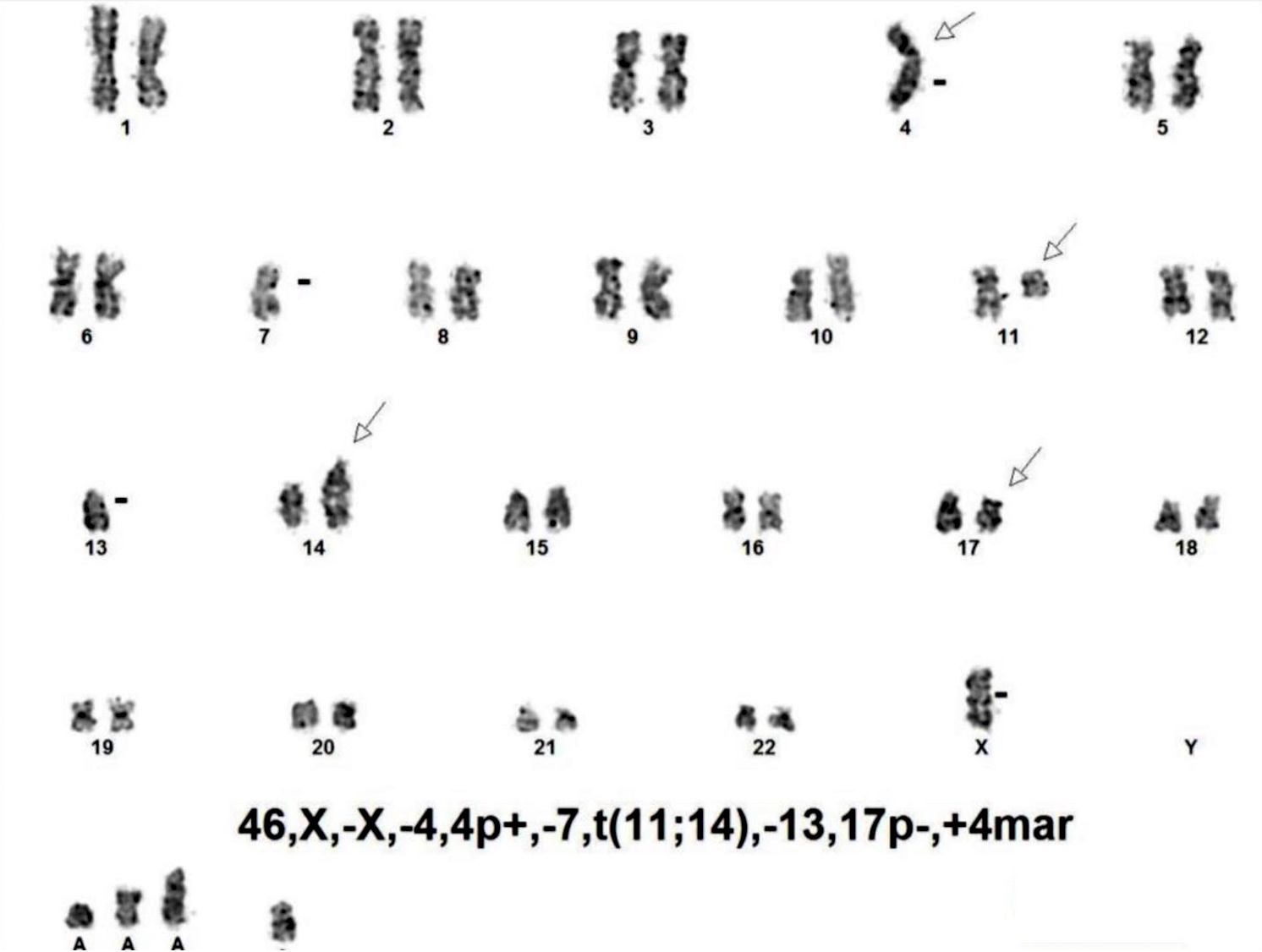
Molecular / cytogenetics description
- Karyotypes are often complex (≥ 3 abnormalities)
- Tetraploid clones are more frequently found in pleomorphic (80%) and blastoid (36%) variants
- Some abnormalities may be specifically involved in pathogenesis
- Chromosome 17p deletions (TP53)
- Chromosome 9p deletions (CDKN2A)
- Chromosome 8q24 translocations or amplification (MYC)
- Chromosome 3q27translocations (BCL6)
- Expression abnormalities can be simplified into 2 general types by array CGH
- Cell cycle dysregulation / impaired DNA repair (ATM, cyclin D1, TP53 mutations)
- Impaired apoptosis (BIRC3)
- IG genes are clonally rearranged
- IGV genes are unmutated or minimally mutated in most cases
- t(11;14)(q13;q32)
- FISH is convenient; it can be performed on fixed tissue sections
- Conventional cytogenetics if fresh material available
- Most PCR assays detect 1 major breakpoint region in mantle cell lymphoma
- Aggressive variants of mantle cell lymphoma
- TP53 or p16 mutations are common
- t(8;14)(q24;q32)(IGH/MYC) in a small subset of cases
- Mutations in many genes
- ATM (~ 40%), TP53 (~ 25%), CDKN2A (TP16) (10 - 20%)
- Other mutations correlated with blastoid or pleomorphic variant
- KMT2D/MLL2 (~ 10%), WHSC1 (~ 10%), BIRC3 (~ 5%)
- NOTCH1 (~ 5%), NOTCH2 (~ 5%), MEF2B (~ 3%), MYD88 (~ 1%)
- CARD11 (10%)
Molecular / cytogenetics images
Sample pathology report
- Left retroperitoneal lymph node, needle biopsies:
- Mantle cell lymphoma, diffuse pattern, blastoid variant (see comment)
- Comment: Routinely stained histologic sections reveal needle shaped fragments of tissue with partial crush artifact infiltrated by a diffuse monotonous infiltrate with focal starry sky pattern composed of large cells with irregular nuclei, blastoid chromatin, small nucleoli and scant cytoplasm. There is single cell apoptosis and mitotic figures are increased (45/10 high power fields).
We performed immunohistochemical studies using paraffin embedded tissue, which show that the neoplastic cells are positive for cyclin D1, SOX11 (diffuse nuclear) and p53 (> 90%); while negative for TDT. Ki67 demonstrates a proliferation index of 100%. PAX5/CD5 immunohistochemical cocktail shows that the neoplastic cells are positive for PAX5 without co-expression of CD5.
Fluorescence in situ hybridization (FISH) studies for t(11;14) translocation and MYC rearrangements are in progress and will be reported separately.
Flow cytometry immunophenotyping detected a lambda restricted B cell population positive for CD10, CD19, CD20, CD22, CD38, CD79b; while negative for CD5, CD11c, CD30, CD43, CD44, CD200 and kappa light chain.
- Addendum:
- Positive for IGH/CCND1 gene rearrangement
- Negative for MYC gene rearrangement
Differential diagnosis
- Lymphoblastic lymphoma
- Burkitt lymphoma
- Diffuse large B cell lymphoma (DLBCL)
- In differential diagnosis of pleomorphic variant
- Diffuse large B cell lymphoma: usually CD5-, cyclin D1-
- Cyclin D1+ diffuse large B cell lymphoma rarely occurs (~2% of all diffuse large B cell lymphoma) (Cancer 2014;120:1818)
- These diffuse large B cell lymphomas do not have the t(11;14)(q13;q32) and are SOX11 negative (Histopathology 2012;61:685)
- B cell prolymphocytic leukemia (B-PLL)
- The immunophenotype can overlap with other lymphoid leukemias
- CD5 can be expressed in 20 - 30% in B cell prolymphocytic leukemia
- cyclin D1+ or t(11;14)(q13;q32) (IGH/CCND1) supports mantle cell lymphoma
- MYD88 mutations occur rarely (1 - 2% of cases) in mantle cell lymphoma
- A subgroup of B cell prolymphocytic leukemia cases with genetic findings similar to mantle cell lymphoma
- 50% with TP53 mutation
- Recurrent MYC abnormalities
- In high risk category model (Blood 2019;134:1777)
- Blastic plasma cell myeloma
- ~ 30 - 40% of plasma cell myeloma can express cyclin D1
- Cytoplasmic Ig+, CD138+, CD5-, CD20-
- A subset of plasma cell myelomas express CD20 or t(11;14) (Blood 2003;102:1070, Ann Diagn Pathol 2006;10:263)
- Leukemic non-nodal mantle cell lymphoma (so called indolent / smoldering mantle cell lymphoma)
- Peripheral blood, bone marrow and sometimes splenic involvement
- Without significant adenopathy
- Circulating cells resemble chronic lymphocytic leukemia (CLL)
- SOX11 negative
- Immunophenotype may overlap with chronic lymphocytic leukemia
- Fewer genomic abnormalities in comparison to nodal mantle cell lymphoma
- Better prognosis
Additional references
- Jaffe: Hematopathology, 2nd Edition, 2016
- Hsi: Hematopathology - Foundations in Diagnostic Pathology, 3rd Edition, 2017
- Swerdlow: WHO Classification of Tumors of Hematopoietic and Lymphoid Tissues, 4th Edition, 2017
- Aster: Hematopathology - High Yield Pathology, 1st Edition, 2013
- Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017
- Kumar: Robbins and Cotran Pathologic Basis of Disease, 9th edition, 2015
- Wang: Diagnosis of Blood and Bone Marrow Disorders, 1st Edition, 2018
Practice question #1
- In the blastoid variant of mantle cell lymphoma, which of the following is the correct option?
- Morphology is composed of cells with variable size and prominent nucleoli
- Most cases are CD5 negative and CD23 positive
- Most cases are Cyclin D1 and SOX11 positive
- Ki67 index is typically below 20%
Practice answer #1
C. Most cases are Cyclin D1 and SOX11 positive
Comment Here
Reference: Mantle cell lymphoma, aggressive variant
Comment Here
Reference: Mantle cell lymphoma, aggressive variant
Practice question #2
- This is the concurrent fine needle aspiration flow cytometry of the lymph node in a 70 year old man with lymphadenopathy. Cytology smears show intermediate to large lymphoid cells in a necrotic background. What is the most probable preliminary diagnosis before further work ups on the excised lymph node?
- Nodal marginal zone lymphoma
- Follicular lymphoma, grade 3A
- Mantle cell lymphoma
- Chronic lymphocytic lymphoma
Practice answer #2