Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Esmaeili A, Jassim SH. Thymic follicular hyperplasia . PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mediastinumthymicfollicularhyperplasia.html. Accessed October 1st, 2025.
Definition / general
- Refers to the increased number of lymphoid follicles within the thymic gland
Essential features
- Usually found incidentally or could present with systemic symptoms (StatPearls: Thymic Hyperplasia [Accessed 28 February 2023])
- Associated with autoimmune diseases such as myasthenia gravis
- Defined as increased number of lymphoid follicles with retained thymic architecture regardless of the gland size
Terminology
- Thymic lymphoid hyperplasia
- Thymic germinal center hyperplasia
ICD coding
- ICD-10: E32.0 - persistent hyperplasia of thymus
Epidemiology
- May be idiopathic or seen in association with other autoimmune disorders, including myasthenia gravis, Graves disease, systemic lupus erythematosus, rheumatoid arthritis, scleroderma and allergic vasculitis
Sites
- Anterior mediastinum
Pathophysiology
- Development of ectopic germinal centers and neoangiogenesis (StatPearls: Thymic Hyperplasia [Accessed 28 February 2023])
Etiology
- Caused by stimulation of B cell compartment and by abnormal growth of secondary follicles
Clinical features
- Usually an incidental finding after imaging for an unrelated chest complaint
- Systemic symptoms: autoimmune disease such as myasthenia gravis and Graves disease (Mediastinum 2018;2:66, StatPearls: Thymic Hyperplasia [Accessed 28 February 2023])
Diagnosis
- Usually discovered incidentally for an unrelated chest complaint or systemic symptom
- Thymic gland usually retains its normal shape but it may be either of normal size or enlarged
- May be associated with autoimmune diseases such as myasthenia gravis and Graves disease
Laboratory
- Acetylcholine receptor antibodies may be positive in patients with myasthenia gravis
- Increased T3 / T4, decreased TSH, increased uptake of radioactive iodine and positive thyroid receptor antibodies in patients with Graves disease
- Possibly workup for other autoimmune disease if clinically suspicious
- References: StatPearls: Graves Disease [Accessed 19 June 2023], JAMA Neurol 2015;72:1170
Radiology description
- Suggested on chest Xray, CT and possibly MRI
- Findings can range from subtle mediastinal findings to large mass or widened mediastinum
- Reference: Cancer Imaging 2005;5:139
Prognostic factors
- Overall, good prognosis
Case reports
- 28 year old woman with Graves disease and anterior mediastinal mass (Gland Surg 2020;9:437)
- 32 year old woman with large mediastinal mass and hyperthyroidism (Ann Thorac Cardiovasc Surg 2009;15:404)
- 37 year old Japanese woman with Sjögren syndrome and multilocular thymic cysts (Diagn Pathol 2015;10:103)
- 44 year old man with asymptomatic anterior mediastinal mass (Surg Today 1997;27:275)
Treatment
- Asymptomatic patients can be followed up
- Management of thymic hyperplasia depends on the underlying disease and signs and symptoms
- Myasthenia gravis: acetylcholinesterase inhibitors, corticosteroids, plasma exchange therapy, thymectomy
- Graves disease: often regresses after treatment of Graves disease
- Patients with serious manifestations such as superior vena cava syndrome or myasthenia gravis should be referred for thymectomy
- Reference: StatPearls: Thymic Hyperplasia [Accessed 19 June 2023]
Gross description
- Thymus gland may or may not be associated with overall gland enlargement
Frozen section description
- Thymus gland with or without discrete mass
- No evidence of invasion
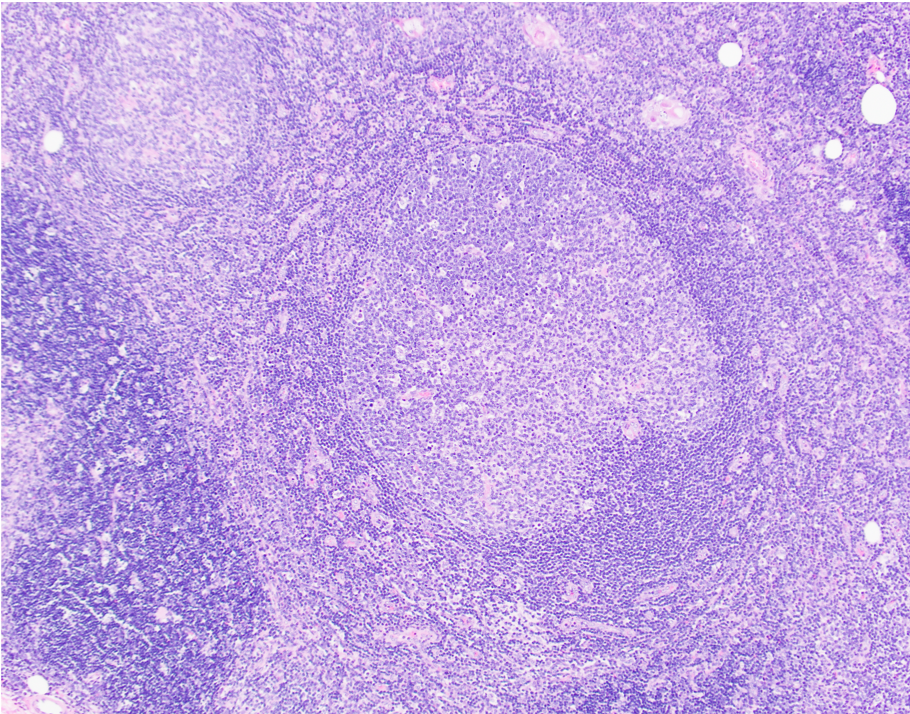
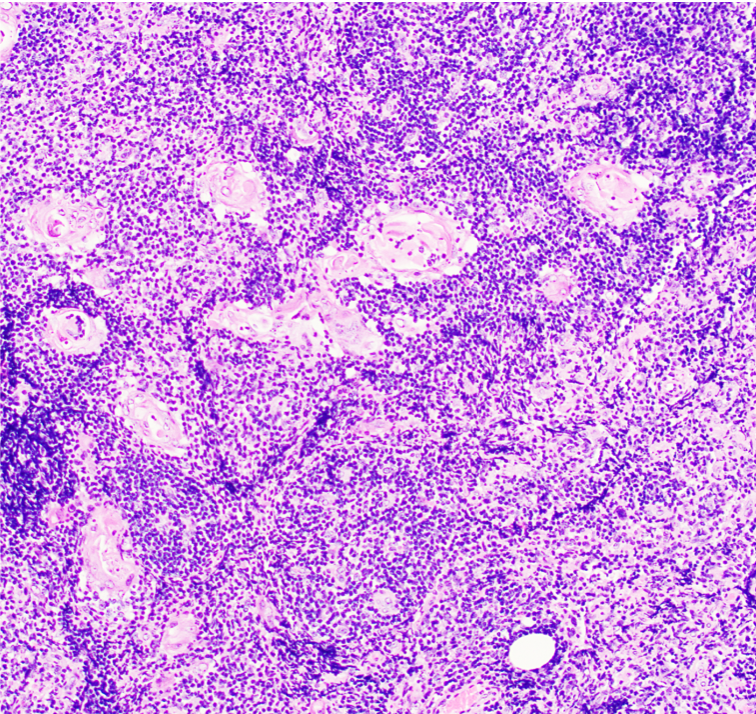
- Retained thymic architecture, increased number of lymphoid follicles with reactive germinal centers
- Presence of Hassall corpuscles
- Absence of a thick fibrous capsule and fibrous septa
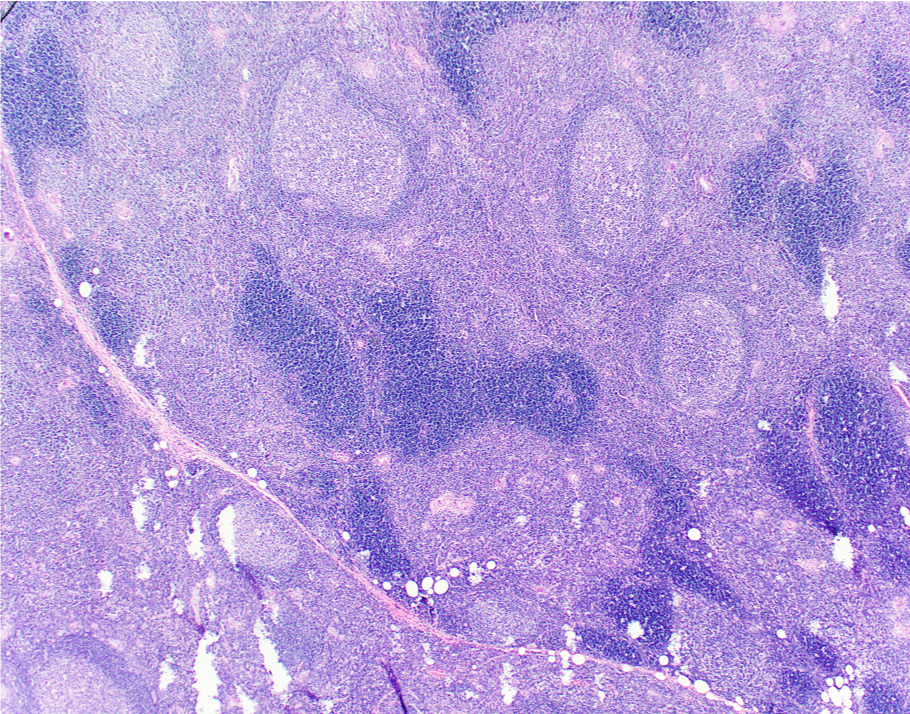
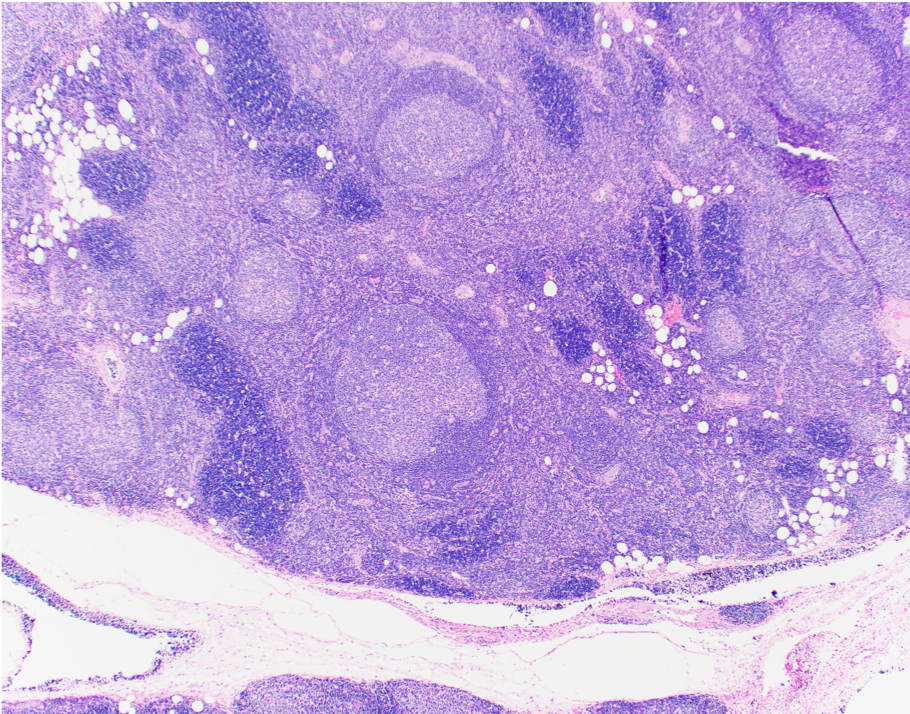
Microscopic (histologic) description
- Preserved thymic architecture
- Increased number of lymphoid follicles with prominent germinal centers of different sizes and tingible body macrophages (StatPearls: Thymic Hyperplasia [Accessed 28 February 2023], Histopathology 2009;54:69)
- Frequent Hassall corpuscles
- Rare germinal centers may be seen in the normal thymus, no clear cutoff is defined
Microscopic (histologic) images
Positive stains
- CD20 highlights B cells and multiple secondary follicles
- CD21 and CD23 highlight follicular dendritic meshwork
- CD10 and BCL6 highlight germinal centers that are appropriately negative for BCL2
- Pankeratin highlights thymic epithelial cells
- Reference: Semin Immunopathol 2021;43:45
Negative stains
Sample pathology report
- Thymus, thymectomy:
- Thymic follicular hyperplasia (see comment)
- Comment: Thymic tissue, consisting of thymic epithelial cells and associated small mature lymphocytes, in addition to occasional lymphoid follicles with prominent germinal centers. Hassall corpuscles are also noted. These histopathologic findings represent thymic follicular hyperplasia, a condition present in association with myasthenia gravis. Defining morphologic features of thymoma are not present.
Differential diagnosis
- True thymic hyperplasia:
- Expansion of the normal component of the thymic gland, normal cortex, medulla, Hassall corpuscles in an organoid configuration
- Thymoma:
- Thymic follicular hyperplasia is discerned from thymoma by the preservation of thymic architecture in thymic lymphoid hyperplasia
- Lymphoproliferative disorders involving the thymus (e.g., T lymphoblastic lymphoma / leukemia, B and T cell lymphomas, classic Hodgkin lymphoma):
- Effaced architecture in lymphoma versus an expansion of the normal component of the thymic gland in true thymic hyperplasia
- Germ cell tumor (e.g., seminoma) with florid follicular lymphoid hyperplasia:
- Usually morphology is different; however, seminoma can have lymphoid hyperplasia and remnant thymic tissue
- Normal thymus with rare germinal centers
- Thymic carcinoma:
- Distorted architecture with desmoplasia and often increased cytologic atypia
Practice question #1
Practice answer #1
E. Normal distribution of cortex and medulla. Answers A - D are incorrect because effacement of normal thymic architecture, large lobules separated by fibrous bands, lack of reactive secondary follicles and diffuse meshwork of epithelial cells are features of thymoma.
Comment Here
Reference: Thymic follicular hyperplasia
Comment Here
Reference: Thymic follicular hyperplasia
Practice question #2
Which of the following is the most common thymic entity found in patients with myasthenia gravis?
- Lymphoma
- Thymic follicular hyperplasia
- Thymoma
- True thymic hyperplasia
Practice answer #2
B. Thymic follicular hyperplasia. Thymic follicular hyperplasia may be seen in association with autoimmune disorders, including myasthenia gravis, Graves disease, systemic lupus erythematosus, rheumatoid arthritis, scleroderma and allergic vasculitis. Answer A is incorrect because lymphoma can be found with autoimmune disorders but not often in myasthenia gravis. Answer B is incorrect because thymoma may be found in ~50% of patients with myasthenia gravis, however, it is not most common. Answer D is incorrect because true thymic hyperplasia is only found incidentally with myasthenia gravis.
Comment Here
Reference: Thymic follicular hyperplasia
Comment Here
Reference: Thymic follicular hyperplasia