Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Bennett J. Sclerosing stromal tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorsclerosingstroma.html. Accessed September 8th, 2025.
Definition / general
- Sclerosing stromal tumor is a benign stromal tumor that has a pseudolobular appearance resulting from alternating cellular and hypocellular areas
Essential features
- Alternating cellular and hypocellular areas impart a pseudolobular appearance
- Pseudolobules contain a haphazard arrangement of epithelioid (lutein) and spindled cells
- Hemangiopericytoma-like vessels are conspicuous in both components
- Positive for sex cord markers but negative for EMA and cytokeratin
ICD coding
Epidemiology
- Most common in the first 3 decades (mean: 29 years; median: 26 years) (Histopathology 2022;80:360)
Sites
- Ovary
Pathophysiology
- FHL2-GLI2 fusions activate the Sonic hedgehog (SHH) pathway (Nat Commun 2020;11:44)
Etiology
- Unknown
Clinical features
- Most patients present with menstrual irregularities or abdominopelvic pain; subset is incidental
- Typically nonfunctioning but androgenic or estrogenic manifestations can occur
- Rarely associated with Meigs syndrome (Eur J Gynaecol Oncol 2004;25:528, J Obstet Gynaecol 2010;30:747, World J Clin Cases 2020;8:6364)
Diagnosis
- Mass is often observed on imaging
- Diagnosis is made by histological examination
Laboratory
- CA-125 often within normal limits but elevated levels have been reported (Eur J Gynaecol Oncol 2004;25:528, World J Clin Cases 2020;8:6364)
Radiology description
- CT:
- Plain: nonhomogeneous density
- Contrast: peripheral ring enhancement; may see enhancement of central patch or internal septa
- Venous phase: enhancement decreases but increases with centripetal progression; no enhancement of cystic component (Oncol Lett 2016;11:3817)
- MRI:
- T1 weighted: slight hyperintense periphery, irregular hypointense center
- T2 weighted: hyperintense cystic components or heterogeneous solid mass with intermediate to high intensity
- T1 with contrast: early peripheral enhancement with centripetal progression (AJR Am J Roentgenol 2005;185:207)
Prognostic factors
- Benign tumors; 2 have locally recurred (Int J Gynecol Pathol 2016;35:549, Histopathology 2022;80:360)
Case reports
- 17 year old virilized girl presents with Meigs syndrome (World J Clin Cases 2020;8:6364)
- 22 year old pregnant woman with a 12 cm ovarian mass on imaging (Case Rep Obstet Gynecol 2019;2019:3927971)
- 5 young women (≤ 30 years) with different presentations of an ovarian mass (Indian J Surg Oncol 2018;9:581)
Treatment
- Complete surgical excision (oophorectomy)
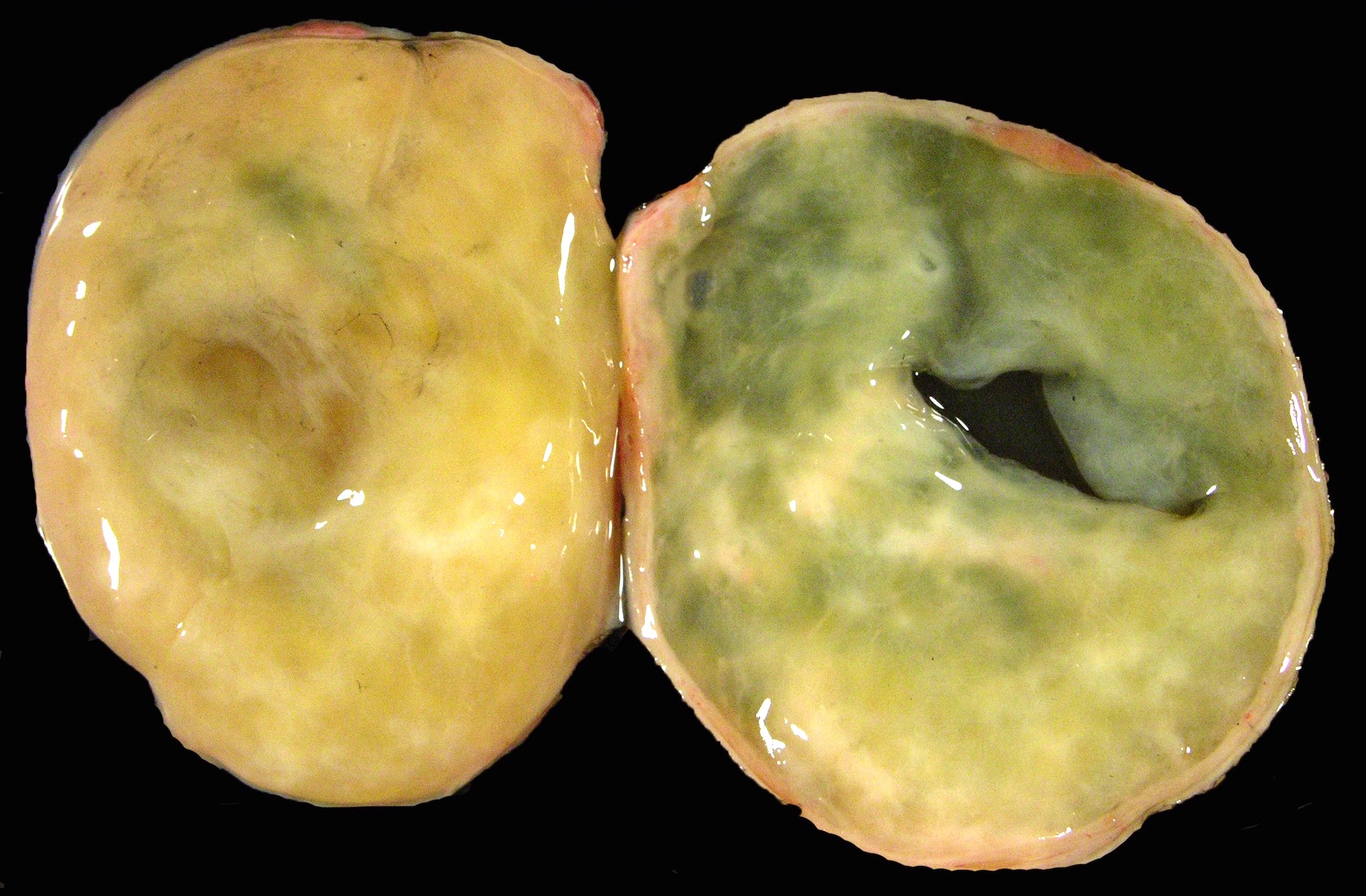
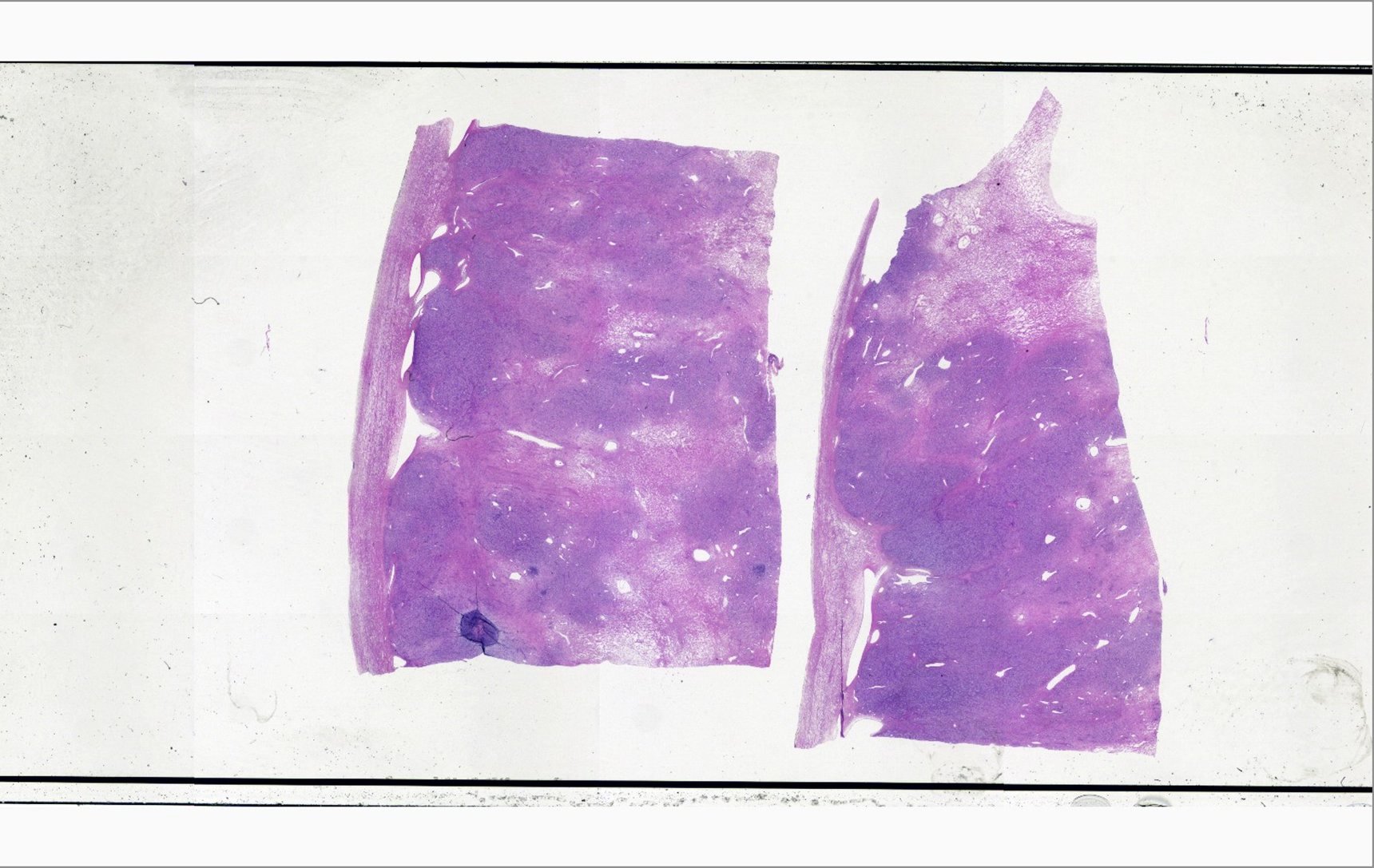
Gross description
- Typically unilateral and well circumscribed, ranging from 1.0 - 23 cm (mean: 8.4 cm) (Histopathology 2022;80:360)
- White-yellow variegated solid mass, often edema and cysts
- Hemorrhage, calcifications and rarely necrosis may be seen
Frozen section description
- Alternating cellular and hypocellular areas that impart a pseudolobular appearance may be seen in Krukenberg tumors; carefully examine for incipient metastases
Frozen section images
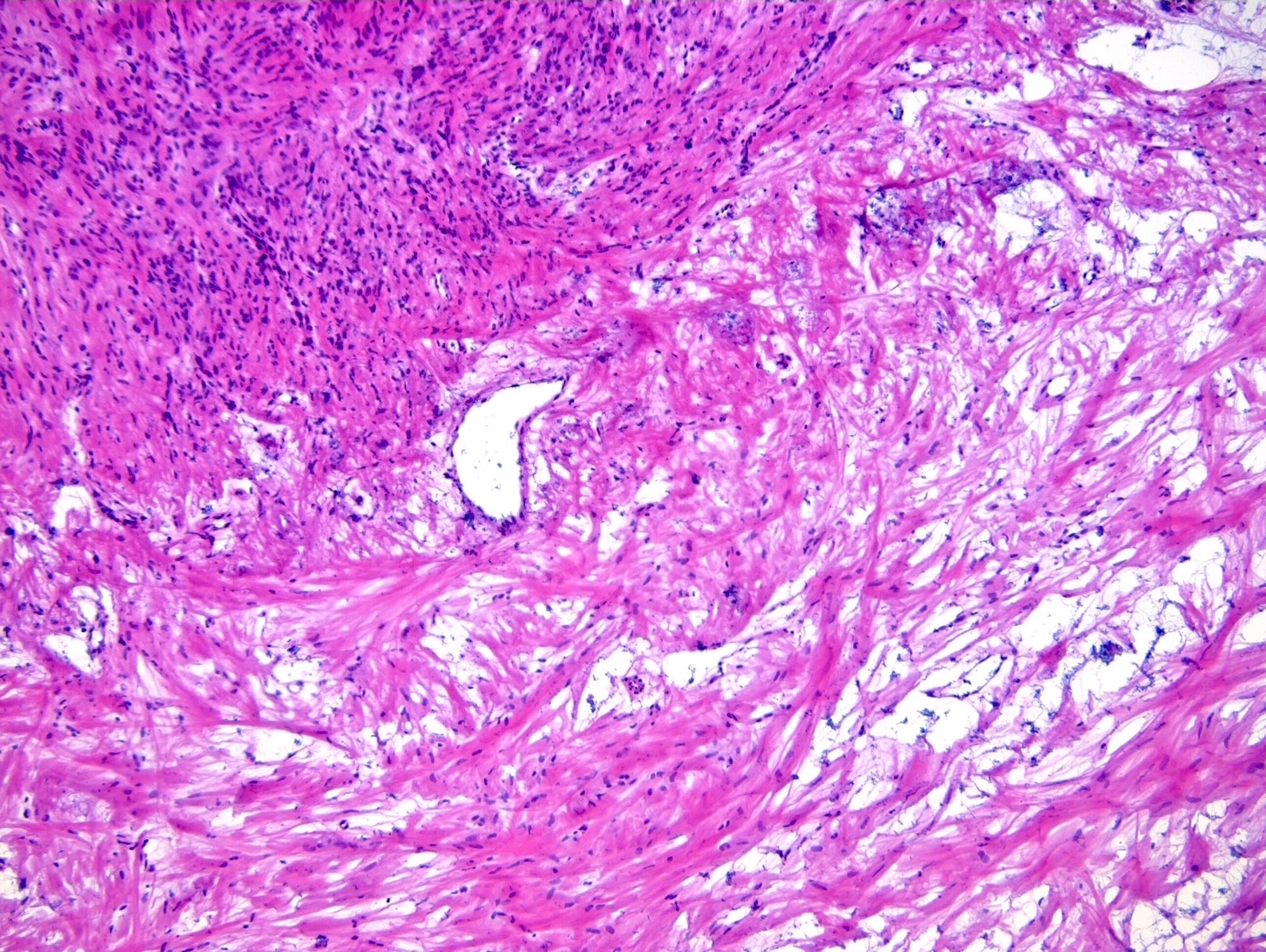
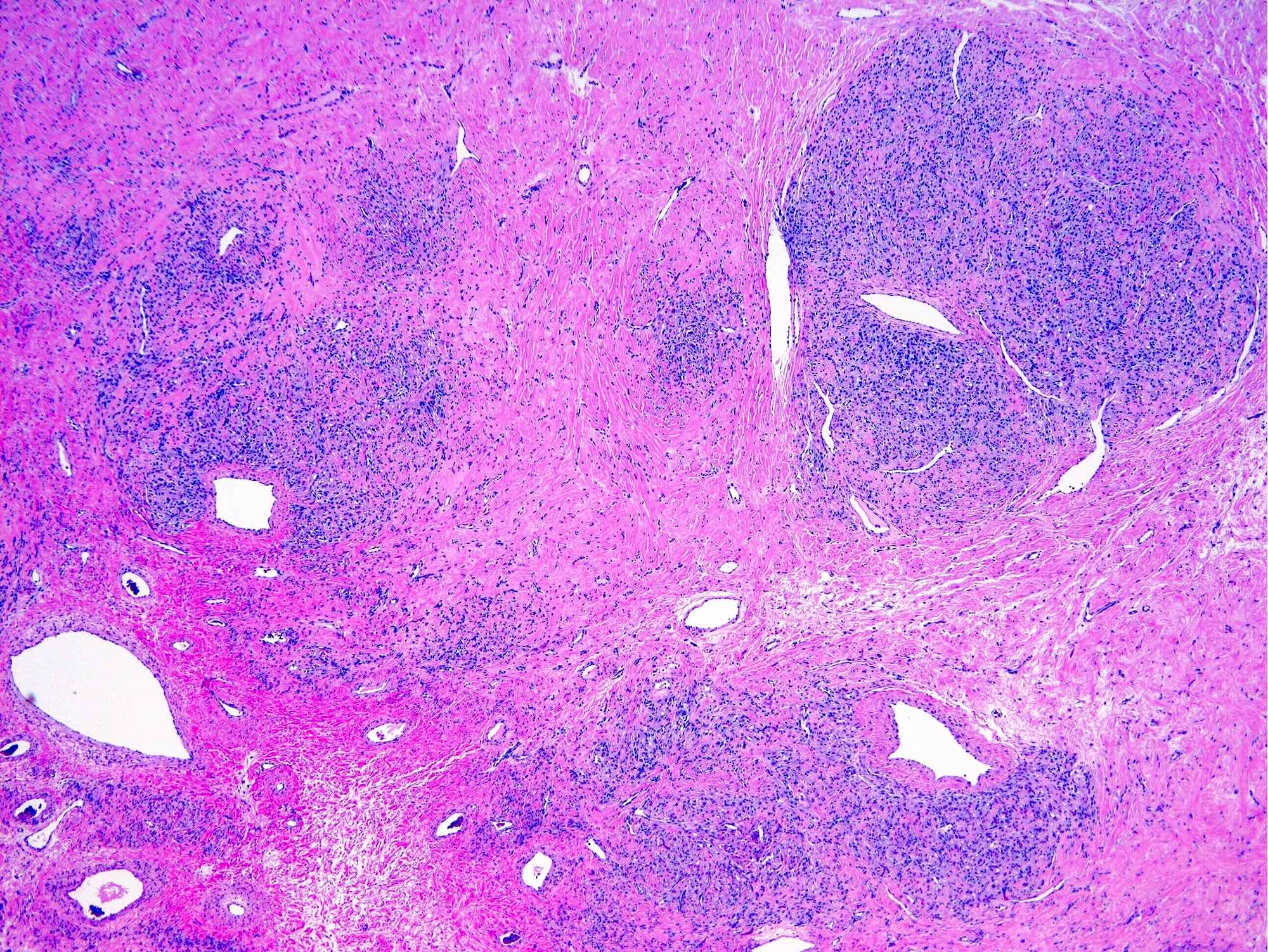
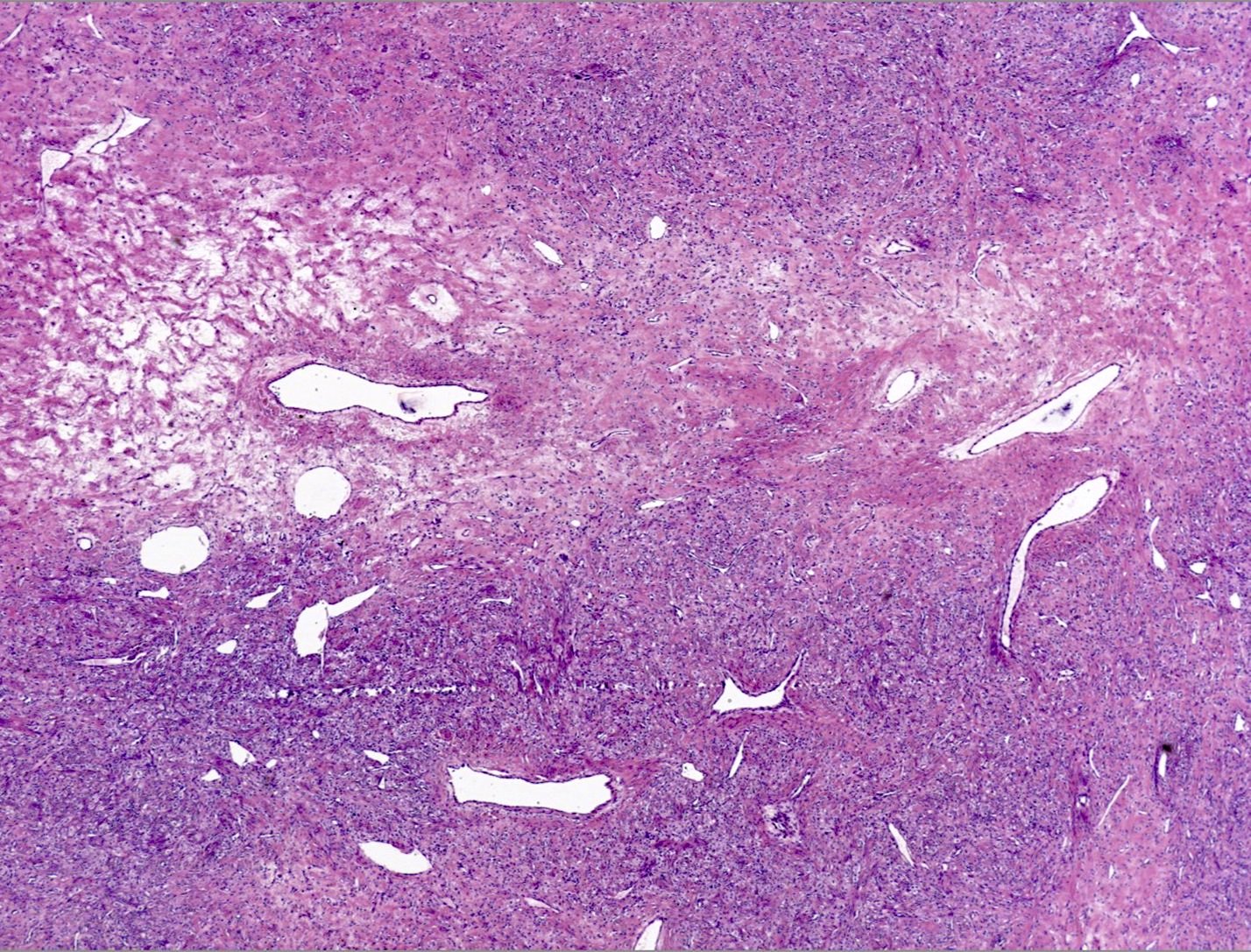
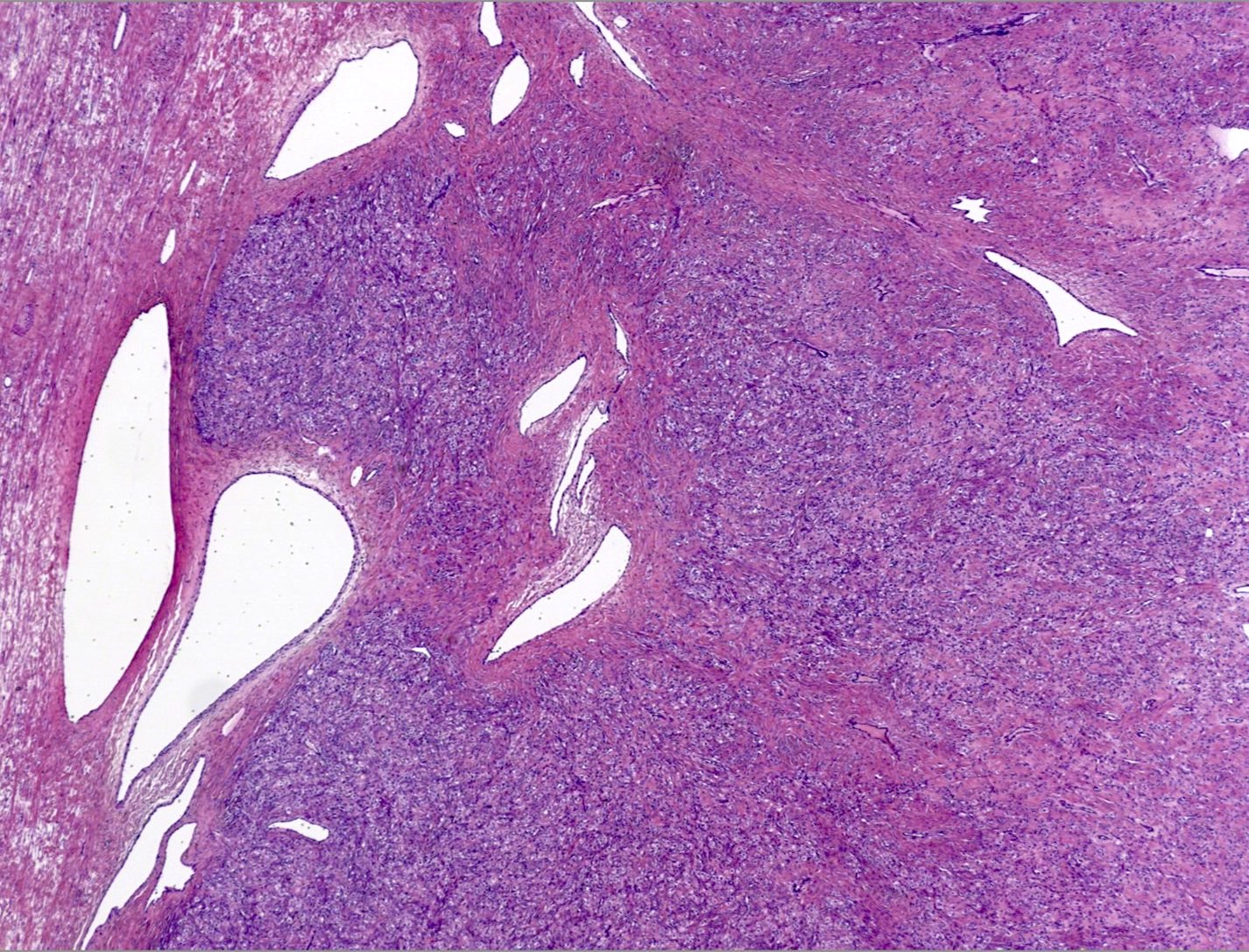
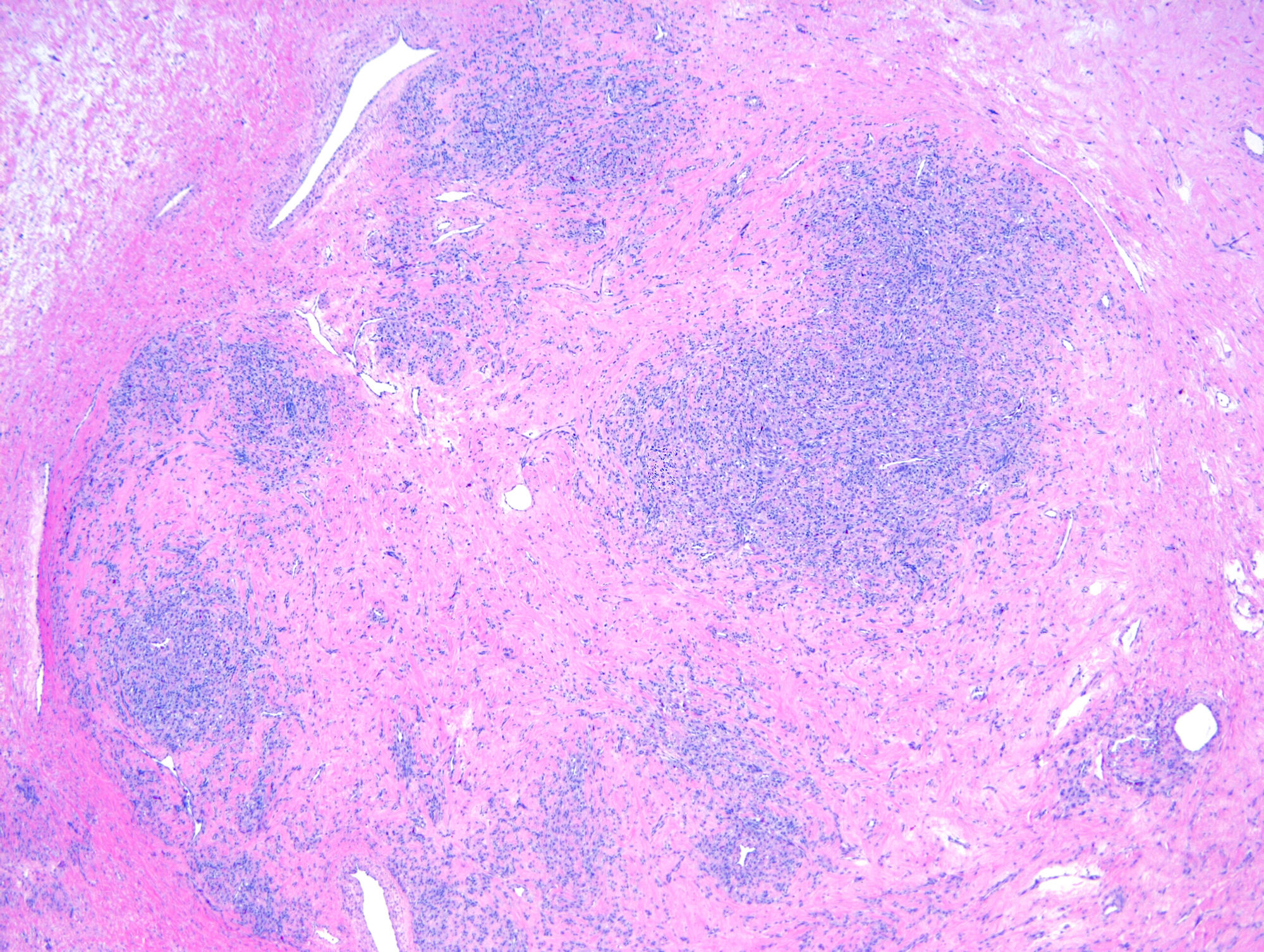
Microscopic (histologic) description
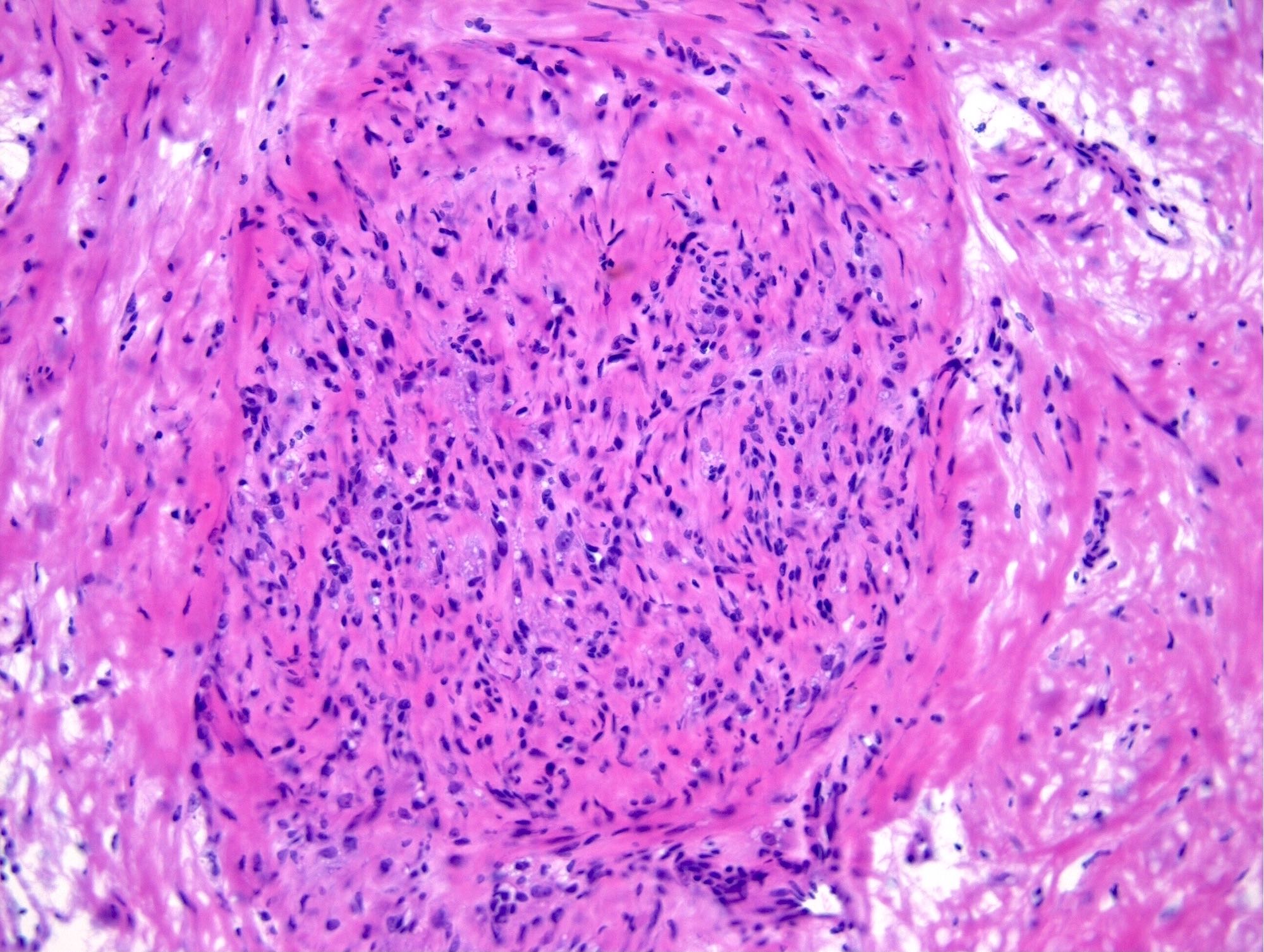
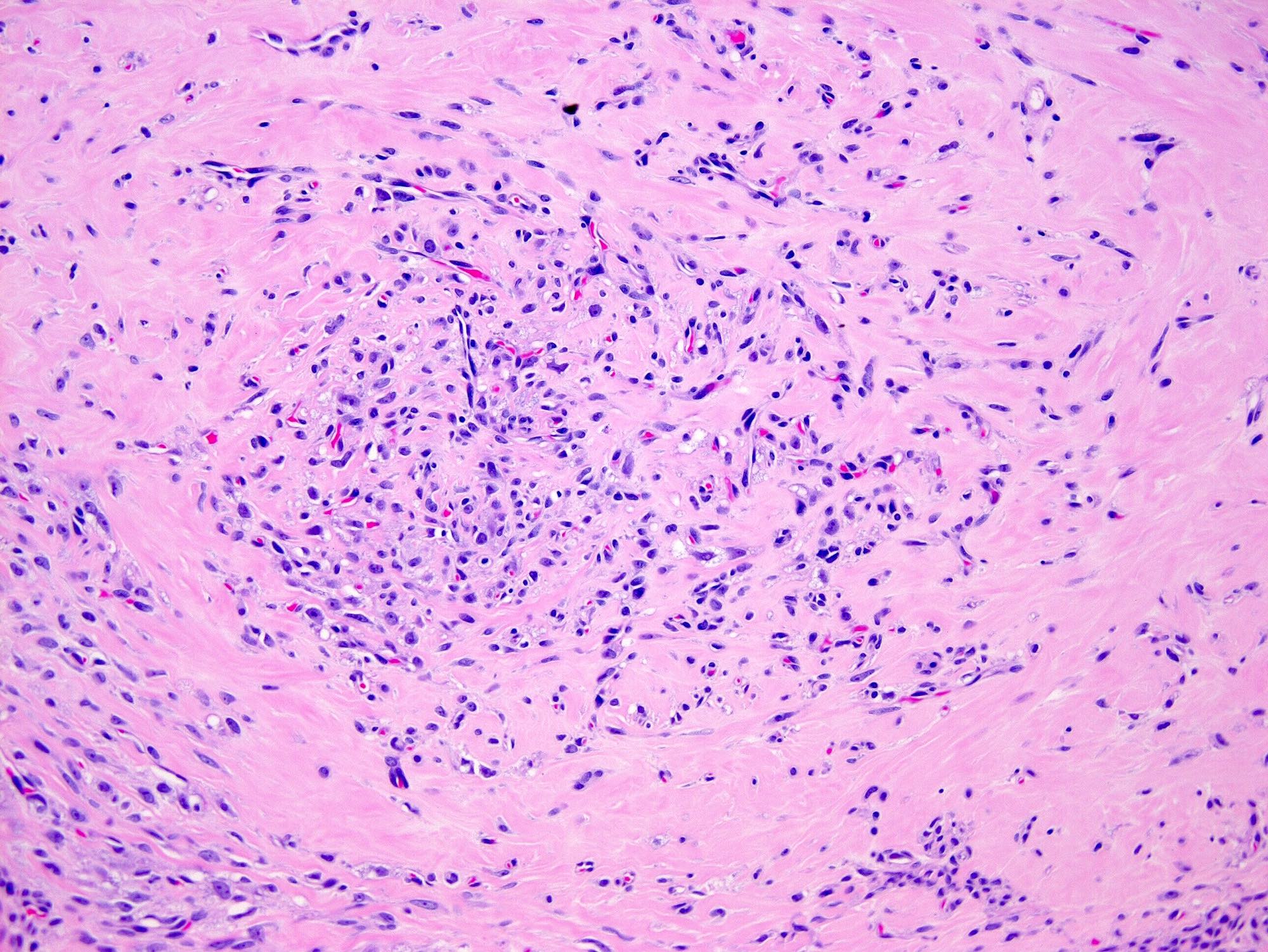
- Alternating cellular and hypocellular areas impart a pseudolobular appearance
- Hypocellular foci may be ill defined in pregnancy due to expansion of the pseudolobules by lutein cells (Int J Gynecol Pathol 2015;34:357)
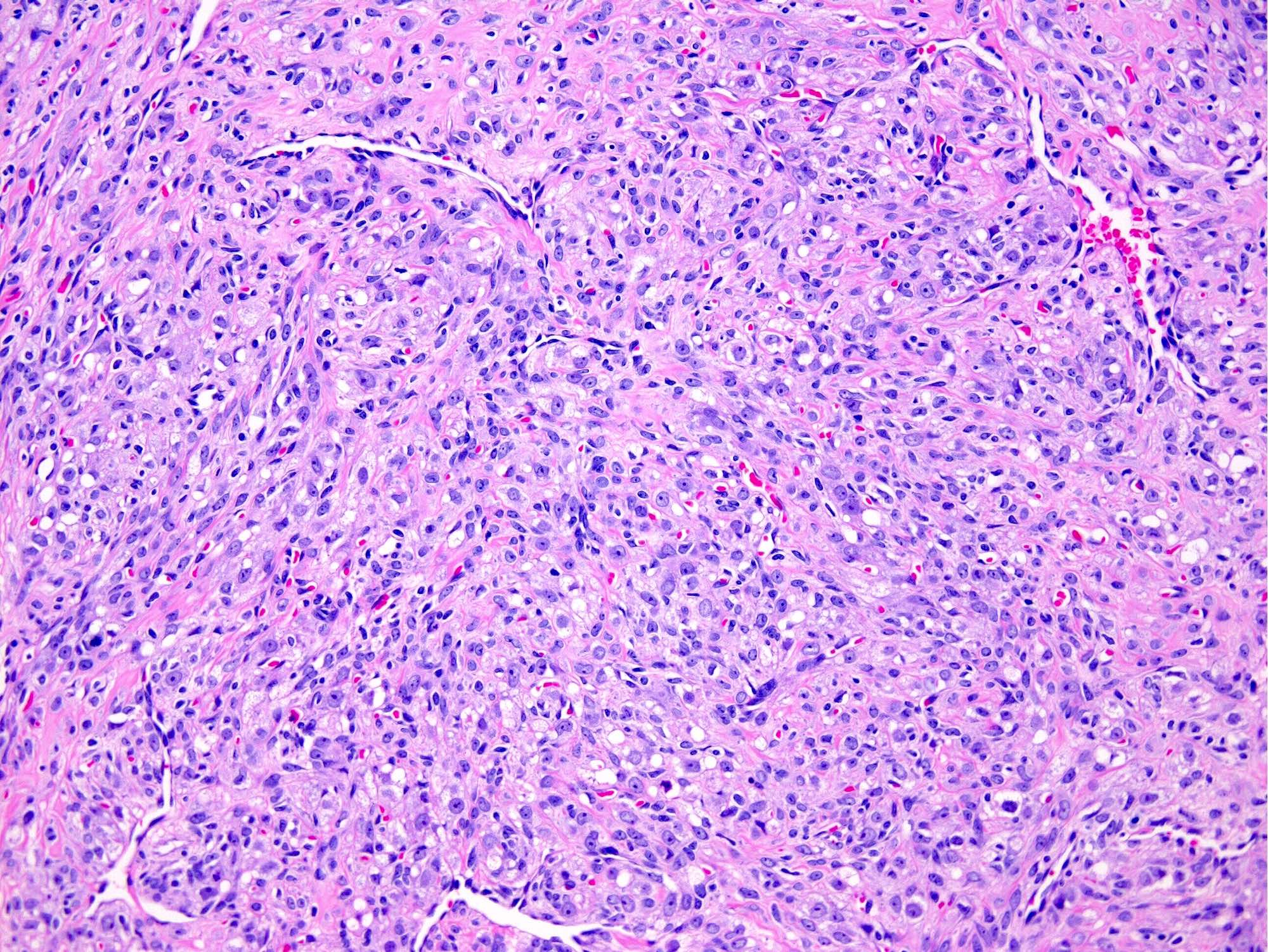
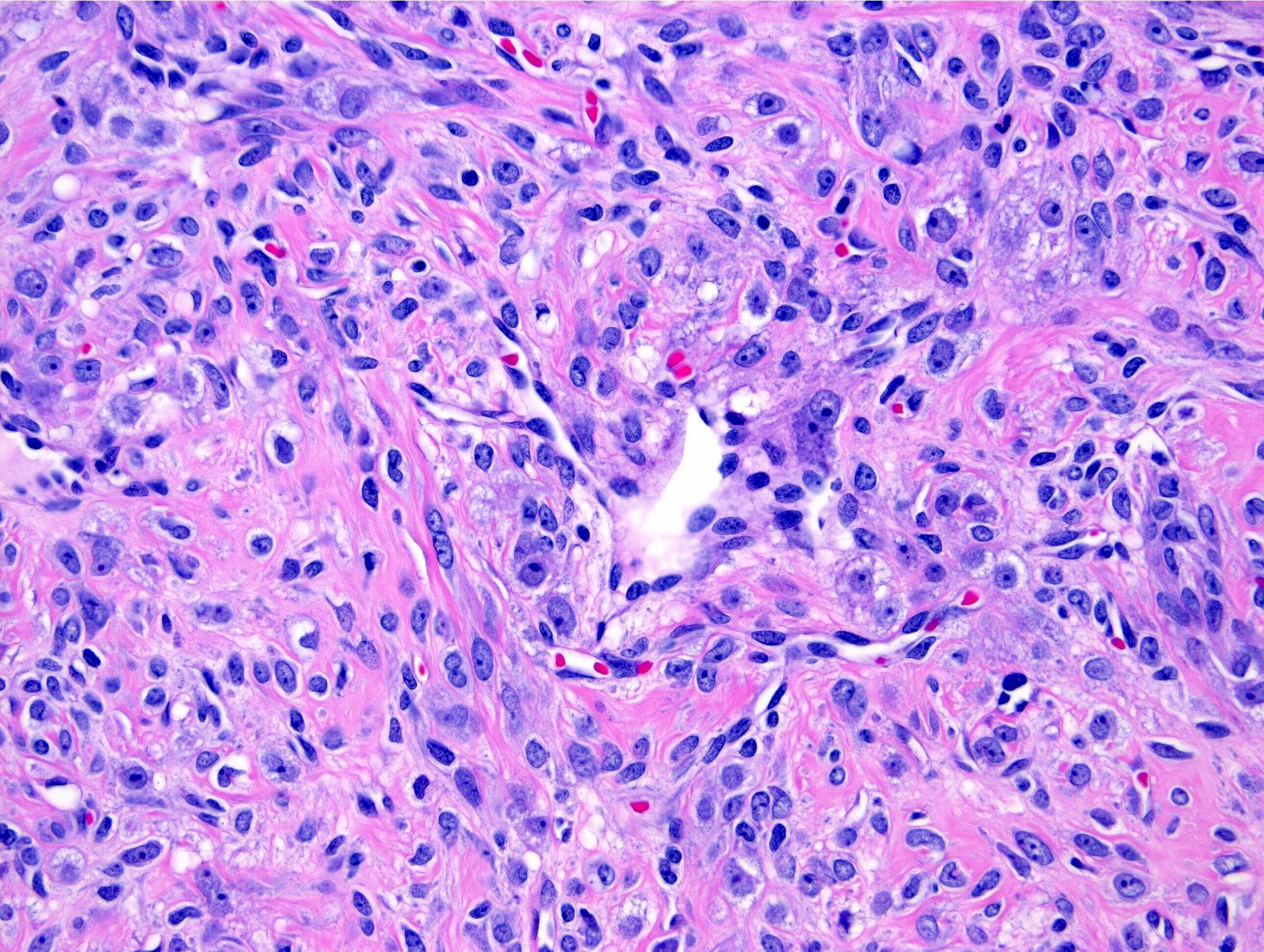
- Thin, dilated and branching hemangiopericytoma-like vasculature is often conspicuous in both components
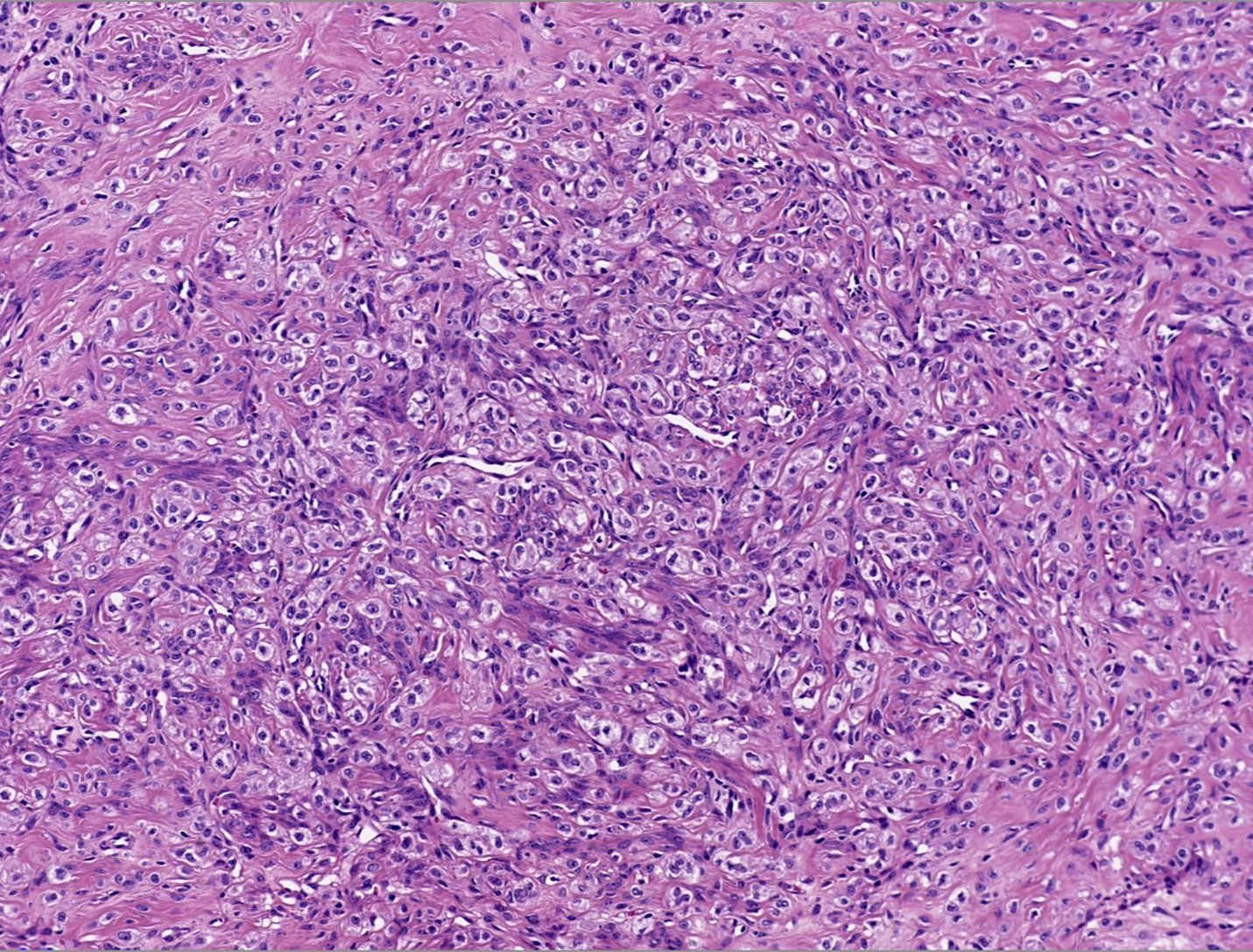
- Pseudolobules comprised of a jumbled admixture of epithelioid (lutein) and spindled cells with minimal atypia
- Epithelioid cells: round nuclei with prominent nucleoli, vesicular chromatin and clear to vacuolated cytoplasm
- Abundant eosinophilic cytoplasm often seen in pregnancy (Int J Gynecol Pathol 2015;34:357)
- Occasionally have a signet ring-like appearance
- Spindled cells: elongated nuclei with indistinct nucleoli, bland chromatin and scant eosinophilic cytoplasm
- Typically round to ovoid but may show angulation if edema is striking
- Epithelioid cells: round nuclei with prominent nucleoli, vesicular chromatin and clear to vacuolated cytoplasm
- Hypocellular areas can be edematous, collagenous (variably keloid-like) or myxoid
- Mitoses are often inconspicuous but rarely can be up to 12/10 high power fields, no atypical forms (Int J Gynecol Pathol 2016;35:549)
- Infarct type necrosis and calcification infrequent
- References: Cancer 1973;31:664, Histopathology 2022;80:360
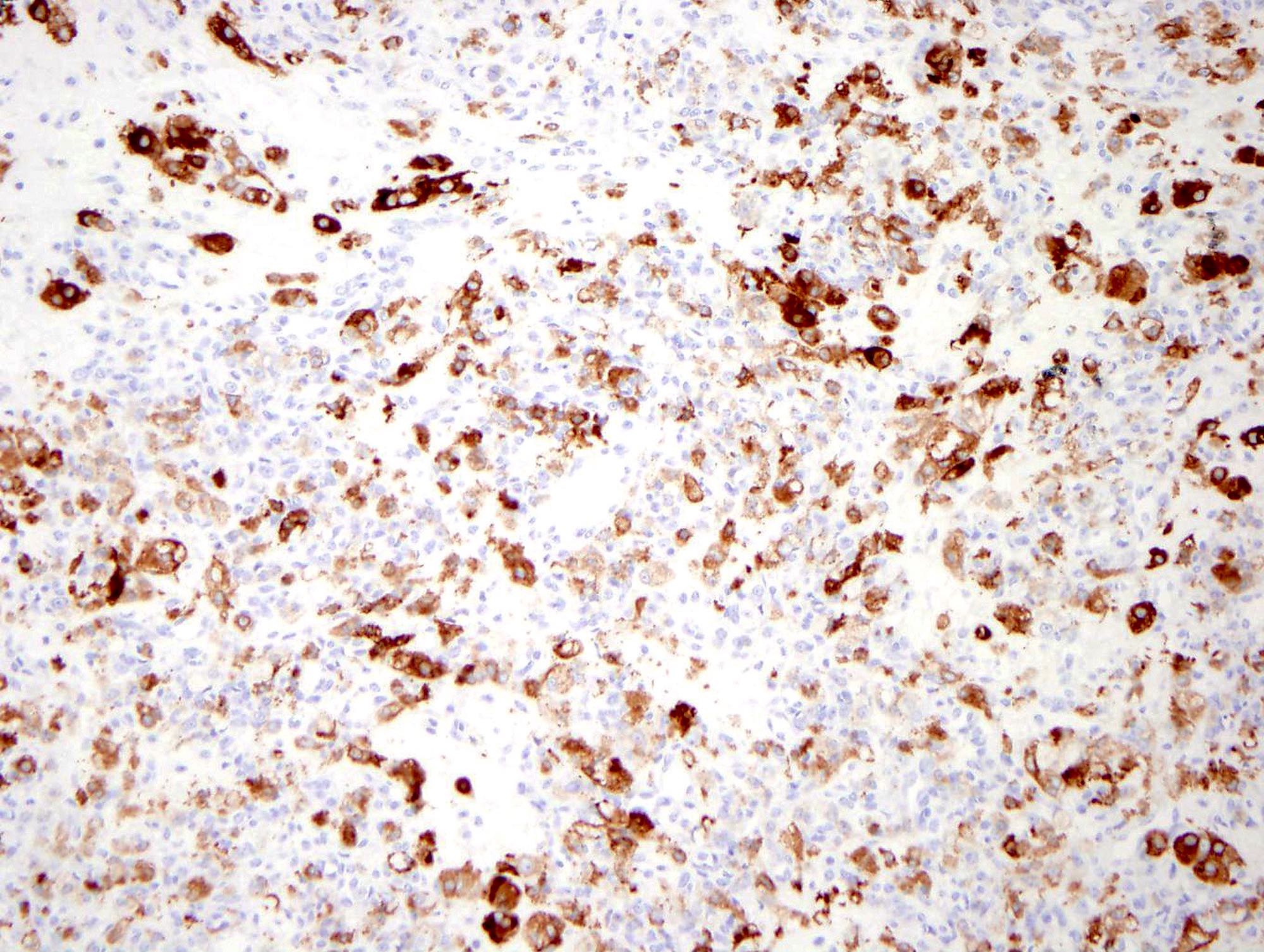
Microscopic (histologic) images
Positive stains
- Inhibin, calretinin, FOXL2
- CD10, smooth muscle actin
- Diffuse TFE3 expression in a subset of tumors (Anticancer Res 2017;37:5441)
Negative stains
Electron microscopy description
- 3 cell types (Int J Gynecol Pathol 1988;7:280):
- Epithelioid cells: membrane bound cytoplasmic lipid, well developed Golgi
- Spindled cells: fibroblast-like, prominent rough endoplasmic reticulum
- Undifferentiated primitive mesenchymal cells (in hypocellular areas): few organelles, rare cilia and basal lamina
- Smooth muscle differentiation supported by aggregates of cytoplasmic filaments with interspersed dense bodies, pinocytotic vesicles and basal lamina (Ultrastruct Pathol 1992;16:363)
Molecular / cytogenetics description
- GLI2 rearrangements in 81% (Nat Commun 2020;11:44)
- FHL2 is the most common gene partner
Sample pathology report
- Right ovary, oophorectomy:
- Sclerosing stromal tumor (5.0 cm)
Differential diagnosis
- Thecoma (Am J Surg Pathol 2014;38:1023):
- Typically postmenopausal (mean: 50 - 60 years)
- Hormonal manifestations common
- Indistinct cell borders
- Pale gray cytoplasm
- Steroid cell tumor:
- Older (mean: 43 years)
- Hormonal manifestations common
- Staghorn vessels absent
- No spindled cells
- Fibroma:
- Older (mean: 48 years)
- Often have a uniform white cut surface
- Hyalinized plaques
- Metastatic signet ring cell carcinoma (Krukenberg tumor) (Am J Surg Pathol 2006;30:277):
- Clinical history
- Bilateral in > 50%, often with extraovarian disease at presentation
- Staghorn vessels absent
- Admixed with glands, nests or cords of malignant cells (may be very focal)
- Cytokeratin, EMA and mucicarmine positive
- Pregnancy luteoma:
- Often bilateral and multifocal
- Brown and hemorrhagic cut surface
- No admixture of cells
- Solitary fibrous tumor (Histopathology 2018;72:749, Am J Surg Pathol 2022;46:363):
- Microcystic stromal tumor (Histopathology 2022;80:898):
- Triad of microcysts, solid areas and fibrous stroma
- No admixture of cells
- Subset with bizarre nuclei
- Beta catenin (nuclear and cytoplasmic) and cyclin D1 positive
- Inhibin and calretinin negative
- CTNNB1 or APC mutations
Practice question #1
A 30 year old woman presented with pelvic pain; ultrasound detected a 10 cm mass in the left ovary. She underwent an oophorectomy. You receive the intact specimen with a 10 cm well circumscribed yellow-white edematous lesion with multiple cysts that replaces the entire ovary. Histologic examination shows cellular areas that alternate with hypocellular edematous foci. Staghorn vessels are prominent. What is the likely diagnosis?
- Pregnancy luteoma
- Sclerosing stromal tumor
- Solitary fibrous tumor
- Steroid cell tumor
- Thecoma
Practice answer #1
Practice question #2
Which of the following is true regarding the ovarian lesion pictured above?
- It is characterized by a recurring mutation
- It is only seen in pregnancy
- It is typically white, firm and uniform on cut surface
- Marked cytologic atypia, tumor cell necrosis and atypical mitoses are common
- The cellular foci are composed of lutein and spindled cells
Practice answer #2
E. The cellular foci are composed of lutein and spindled cells
Comment Here
Reference: Sclerosing stromal tumor
Comment Here
Reference: Sclerosing stromal tumor