Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Goyette ERJ, Muller KE. Encapsulated papillary carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantencapsulatedpapillary.html. Accessed May 13th, 2024.
Definition / general
- Expansile papillary tumor, occurring in postmenopausal women, with low or intermediate grade nuclei surrounded by a fibrous capsule that lacks myoepithelial cells along the papillae and at the periphery or shows focal peripheral myoepithelial staining
Essential features
- Papillary tumor comprised of delicate papillary fronds with fibrovascular cores lined by cuboidal to columnar epithelial cells with low to intermediate grade atypia, often within a cystically dilated duct surrounded by a thick fibrous capsule
- Lacks myoepithelial cells along the papillae and around the periphery of the tumor or only focal peripheral myoepithelial staining
- Staged as ductal carcinoma in situ (DCIS) (i.e., Tis) in the absence of invasive carcinoma, due to indolent behavior and excellent prognosis
- Encapsulated papillary carcinoma (EPC) with high grade cytologic atypia and increased mitotic activity are rare; they are best classified as high grade invasive breast carcinoma with features of EPC and staged as an invasive carcinoma
Terminology
- Intracystic papillary carcinoma (not recommended)
- Encysted papillary carcinoma
ICD coding
- ICD-O:
- ICD-11:
- 2E65.Y & XH9XV2 - other specified carcinoma in situ of breast & noninfiltrating intracystic carcinoma
- 2C6Y & XH0GT6 - other specified malignant neoplasms of breast & encapsulated papillary carcinoma with invasion
Epidemiology
- Postmenopausal women, seventh decade (Am J Surg Pathol 2011;35:1093, Pathol Res Pract 2018;214:579, Breast J 2019;25:539)
- Rare in males (Breast Cancer Res Treat 2020;182:317, Cancer 2008;113:916)
Sites
- Breast, possible central predilection (Pathol Res Pract 2018;214:579)
Pathophysiology
- Classification and pathogenesis are debated:
- Variant of ductal carcinoma in situ (DCIS)
- Progression from in situ disease to invasive carcinoma
- Low grade indolent invasive tumor with pushing border
- References: Am J Surg Pathol 2011;35:1093, Curr Probl Cancer 2018;42:291, Breast Cancer Res Treat 2020;182:317
Etiology
- Unknown
Clinical features
- Presentation may include palpable mass or nipple discharge (Cancer 2008;113:916, Curr Probl Cancer 2018;42:291, Pathol Res Pract 2018;214:579)
Diagnosis
- Histologic examination of tissue removed by biopsy or surgical excision
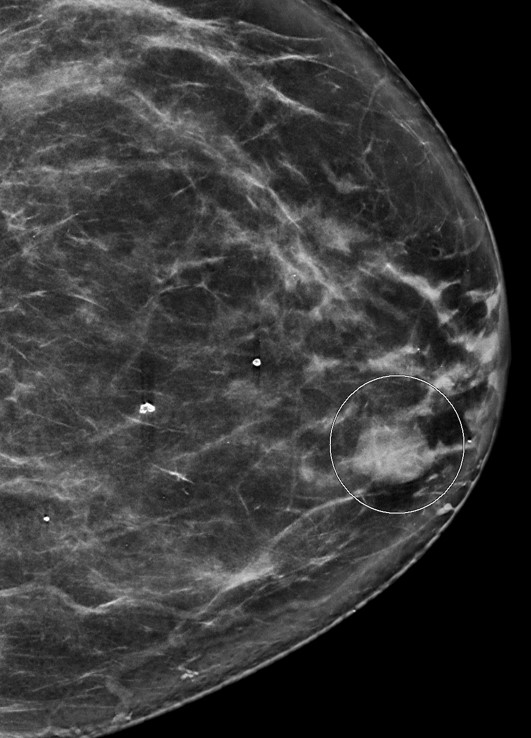
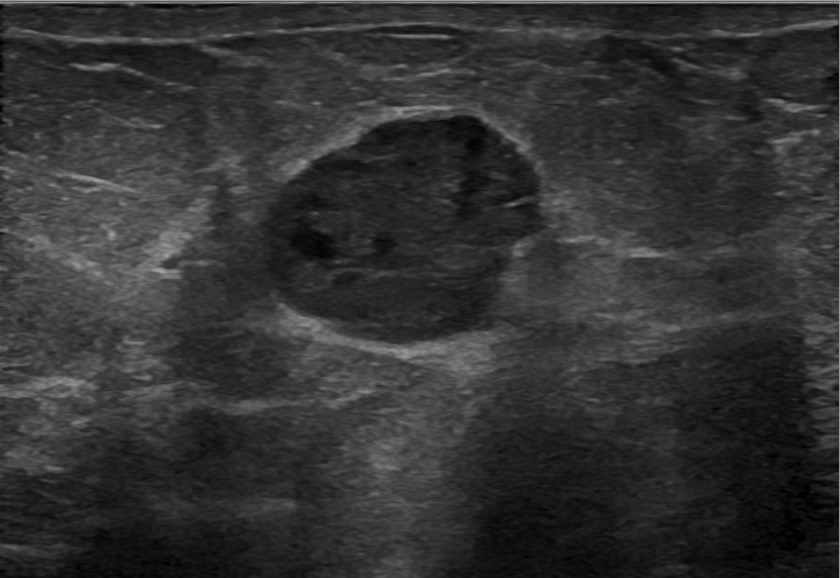
Radiology description
- No distinct imaging findings can distinguish between subtypes of papillary carcinomas (AJR Am J Roentgenol 2012;198:264, Front Surg 2022;8:743881)
- Imaging does not distinguish encapsulated papillary carcinoma (EPC) with and without invasion beyond the capsule (Breast J 2019;25:539, Breast J 2021;27:209)
- Mammography:
- Circumscribed to lobulated, round to oval mass
- May have irregular, angulated or multilobulated borders
- Calcifications uncommon
- Ultrasound:
- Hypoechoic solid mass, sometimes with cystic component
- Color Doppler often highlights prominent vascular supply
- Magnetic resonance imaging (MRI):
- Well defined, round to oval, heterogeneous mass with varying signal intensity depending on cystic fluid content
Radiology images
Contributed by Mariel Molina Nunez, M.D. and Julie Jorns, M.D. (Case #518)
Images hosted on other servers:
Prognostic factors
- Low and intermediate grade EPC without conventional invasive carcinoma (Am J Surg Pathol 2011;35:1093, Curr Probl Cancer 2018;42:291, Am J Clin Pathol 2009;131:228)
- Similar clinical behavior to ductal carcinoma in situ (DCIS), staged as DCIS in the absence of invasive carcinoma
- > 95% 10 year survival in the absence of associated invasive carcinoma
- Local recurrence possible (7%) (Histopathology 2016;68:45)
- Lymph node metastases rare (3%) (Int J Surg Pathol 2007;15:143, Histopathology 2016;68:45)
- If invasion beyond the capsule is present, it is staged based on the size of the invasive component, not the size of the EPC
- Patients with invasive carcinomas arising from EPCs may have a better prognosis compared to age and stage matched conventional invasive carcinomas (Breast Cancer Res Treat 2010;122:637)
- Similar clinical behavior to ductal carcinoma in situ (DCIS), staged as DCIS in the absence of invasive carcinoma
- High grade carcinoma with EPC features (Histopathology 2015;66:740, Histol Histopathol 2019;34:137, Am J Surg Pathol 2011;35:1093)
- Low incidence (3% of EPC)
- Similar clinical behavior to invasive carcinoma with greater propensity of lymphovascular invasion and lymph node metastases when compared to low and intermediate grade EPC
- Best classified as high grade invasive breast carcinoma with features of EPC and staged as an invasive carcinoma
Case reports
- 62 year old woman with nipple discharge and encapsulated papillary carcinoma (Radiol Case Rep 2021;16:748)
- 62 year old woman with sudden hemorrhage in encapsulated papillary carcinoma resulting in anemia and emergency surgery (Int J Surg Case Rep 2019;65:201)
- 63 year old man with encapsulated papillary carcinoma (Asian J Surg 2022;45:1511)
- 63 year old man with gynecomastia and encapsulated papillary carcinoma (Eur J Breast Health 2018;14:127)
- 67 year old woman with distant metastasis following encapsulated papillary carcinoma (Case Rep Oncol 2020;13:1196)
- A postmenopausal woman with a 15 mm mass in the lower inner quadrant of the left breast (Case of the Month #518)
Treatment
- May be treated adequately with surgical excision alone, similar to in situ carcinoma (Am J Surg Pathol 2011;35:1093, Mod Pathol 2021;34:1044)
- The need for axillary sentinel lymph node sampling is debated (Breast J 2021;27:209, Clin Breast Cancer 2017;17:127)
- Hormonal therapy may be indicated in certain cases (Am J Surg Pathol 2011;35:1093)
- Chemotherapy not indicated (Am J Surg Pathol 2011;35:1093)
Gross description
- Well circumscribed solid to papillary mass expanding a cystic space lined by a fibrotic capsule (Virchows Arch 2022;480:65)
- Typically between 1 - 2 cm (Curr Probl Cancer 2018;42:291)
Gross images
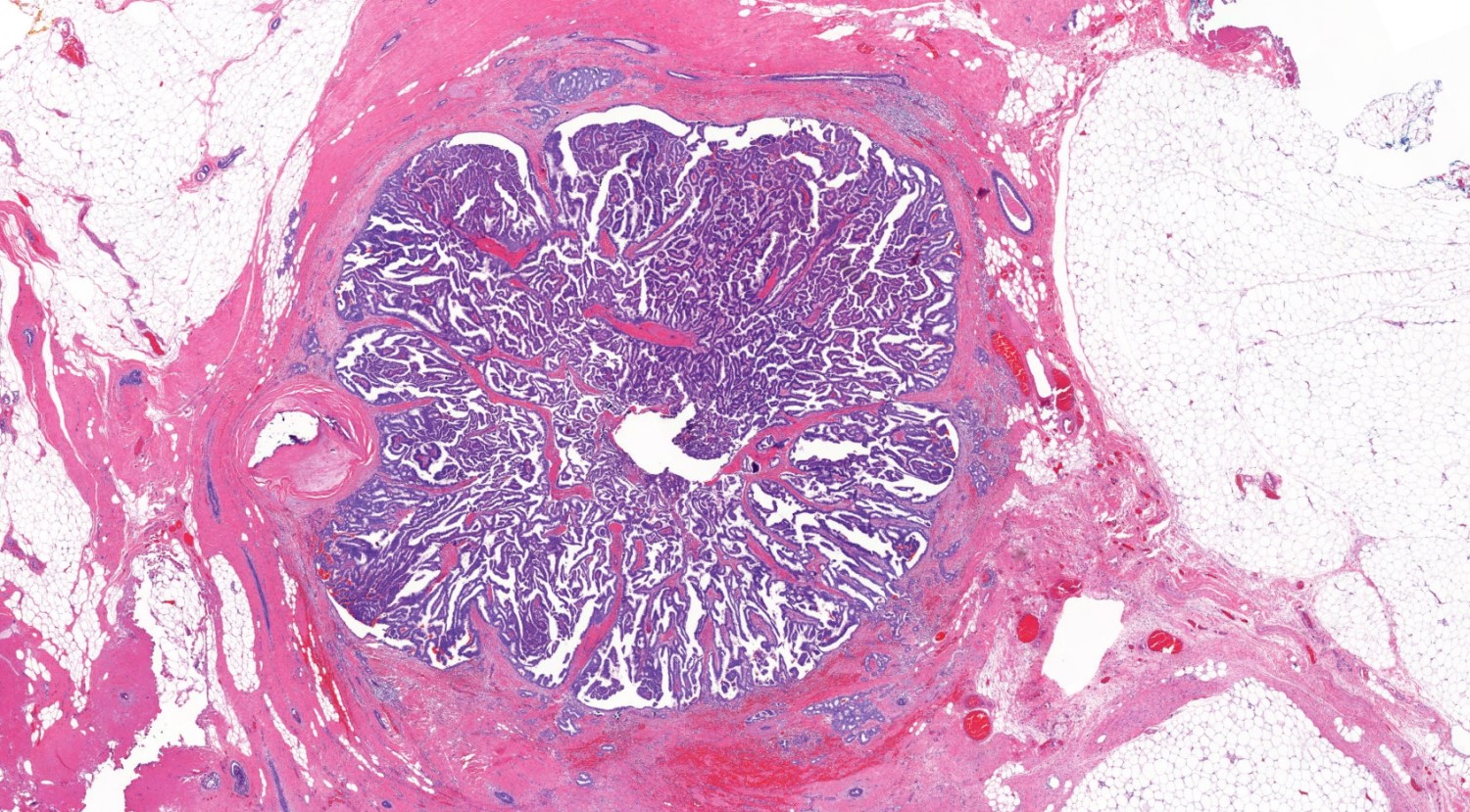
Microscopic (histologic) description
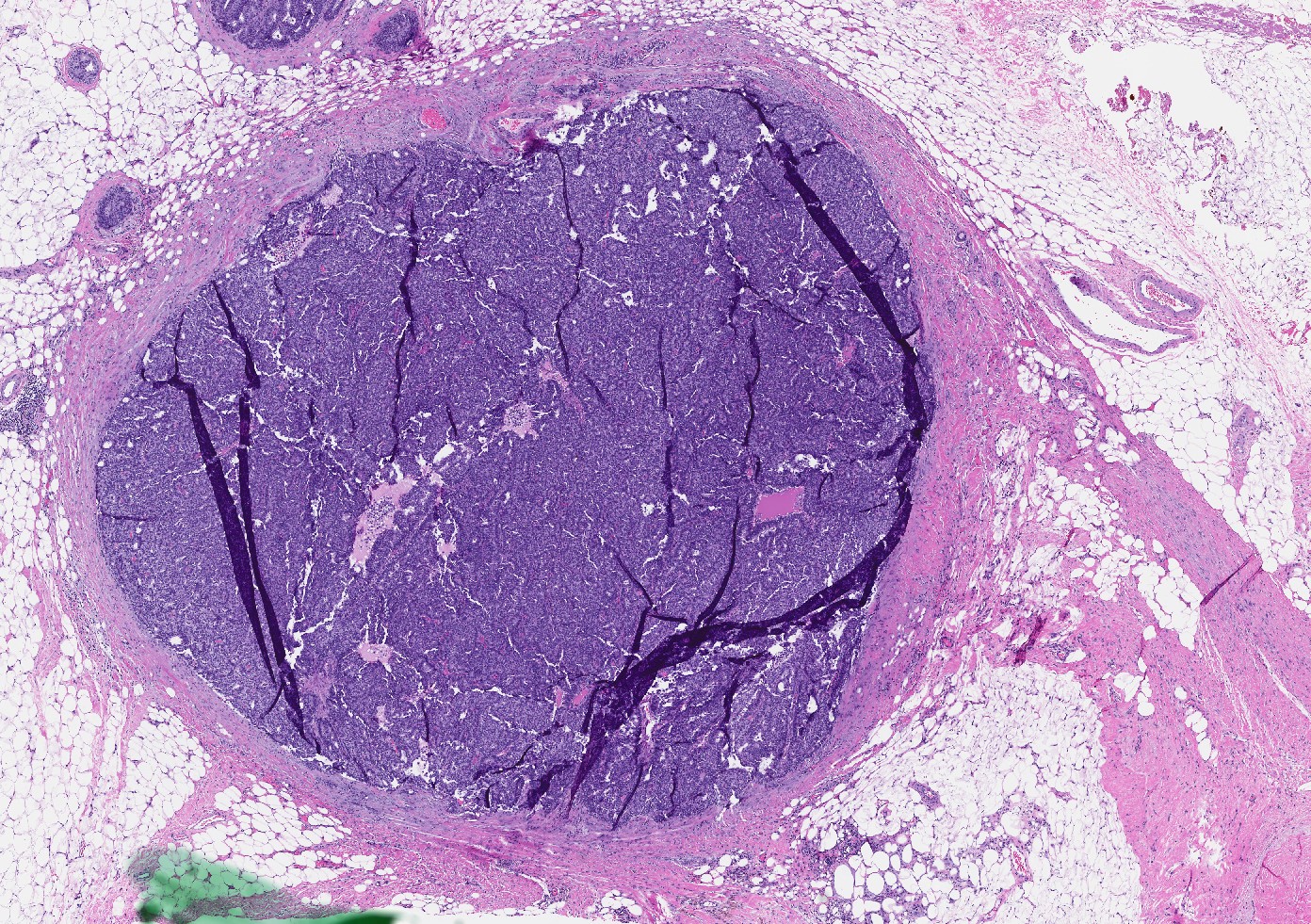
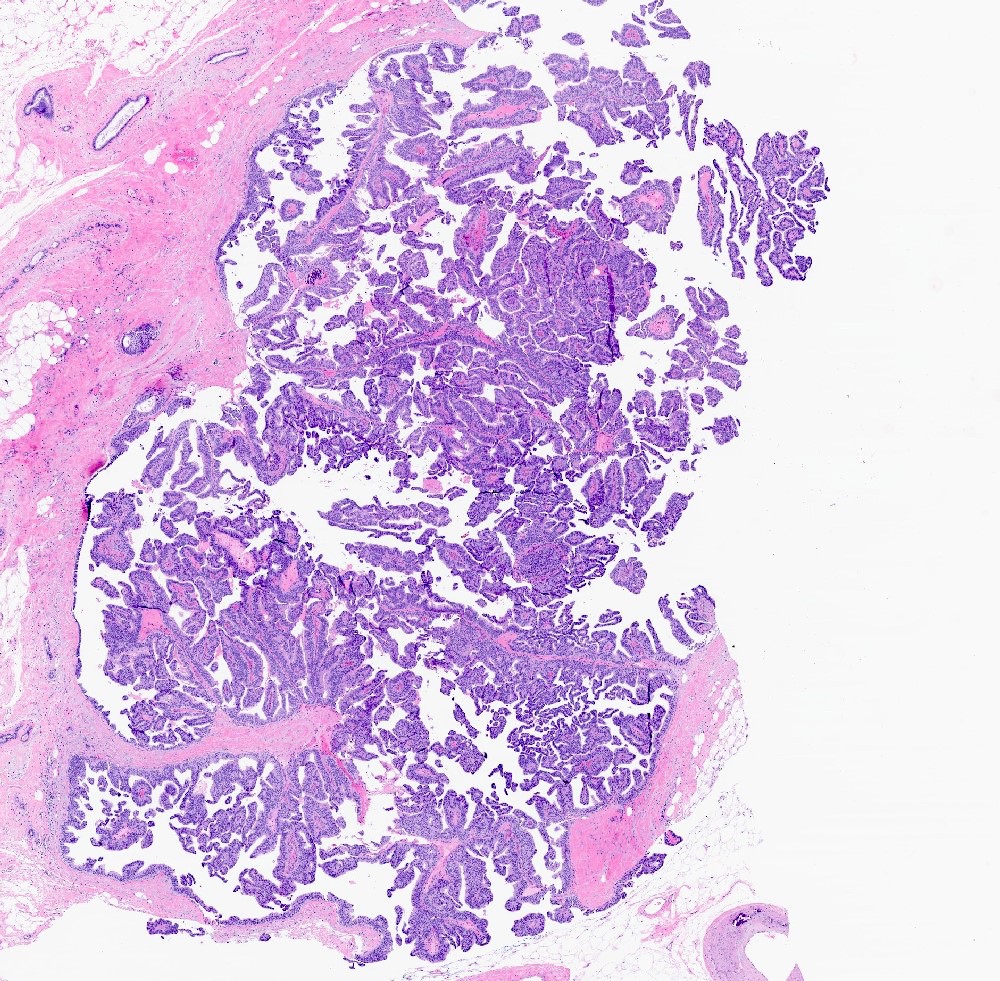
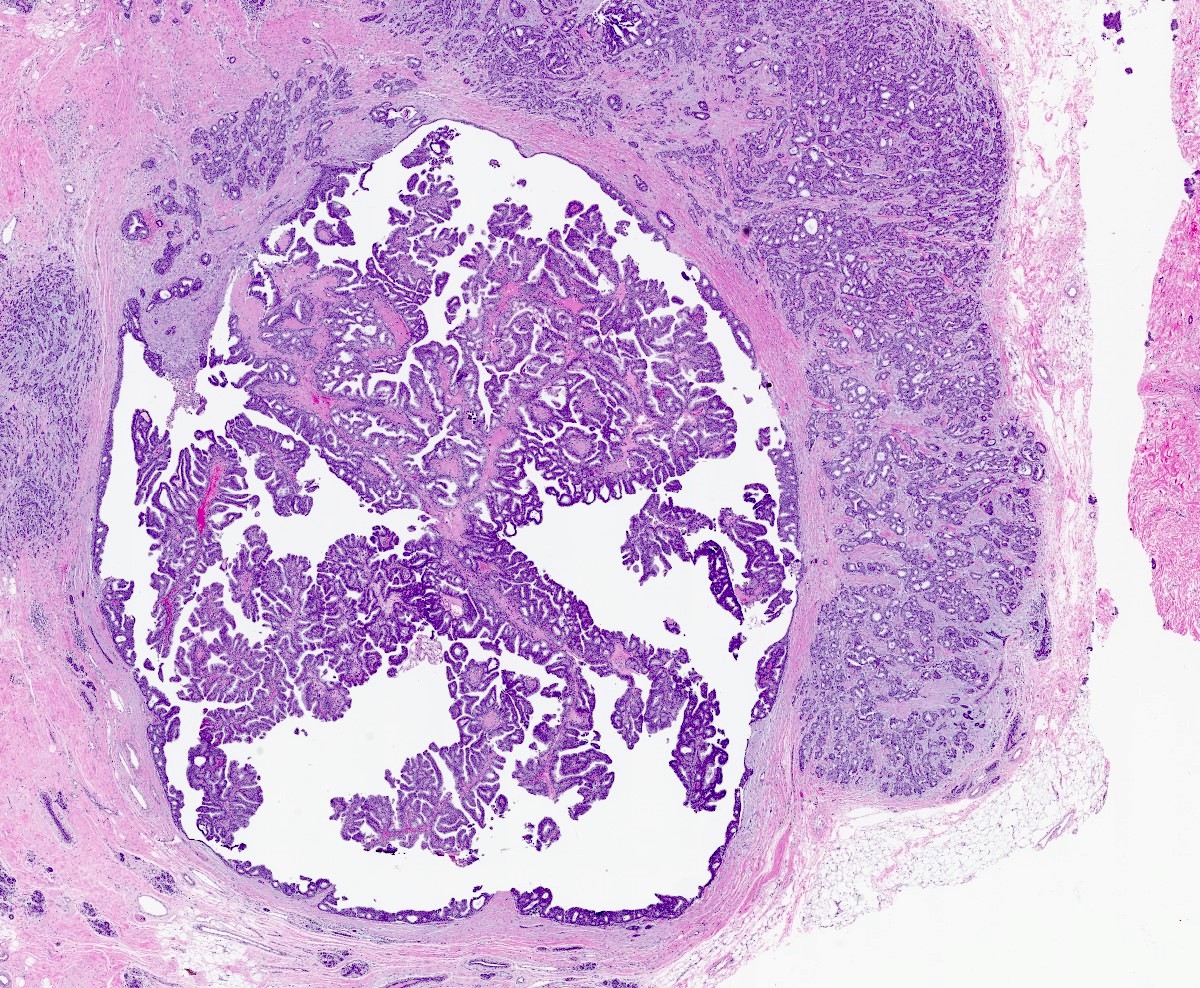
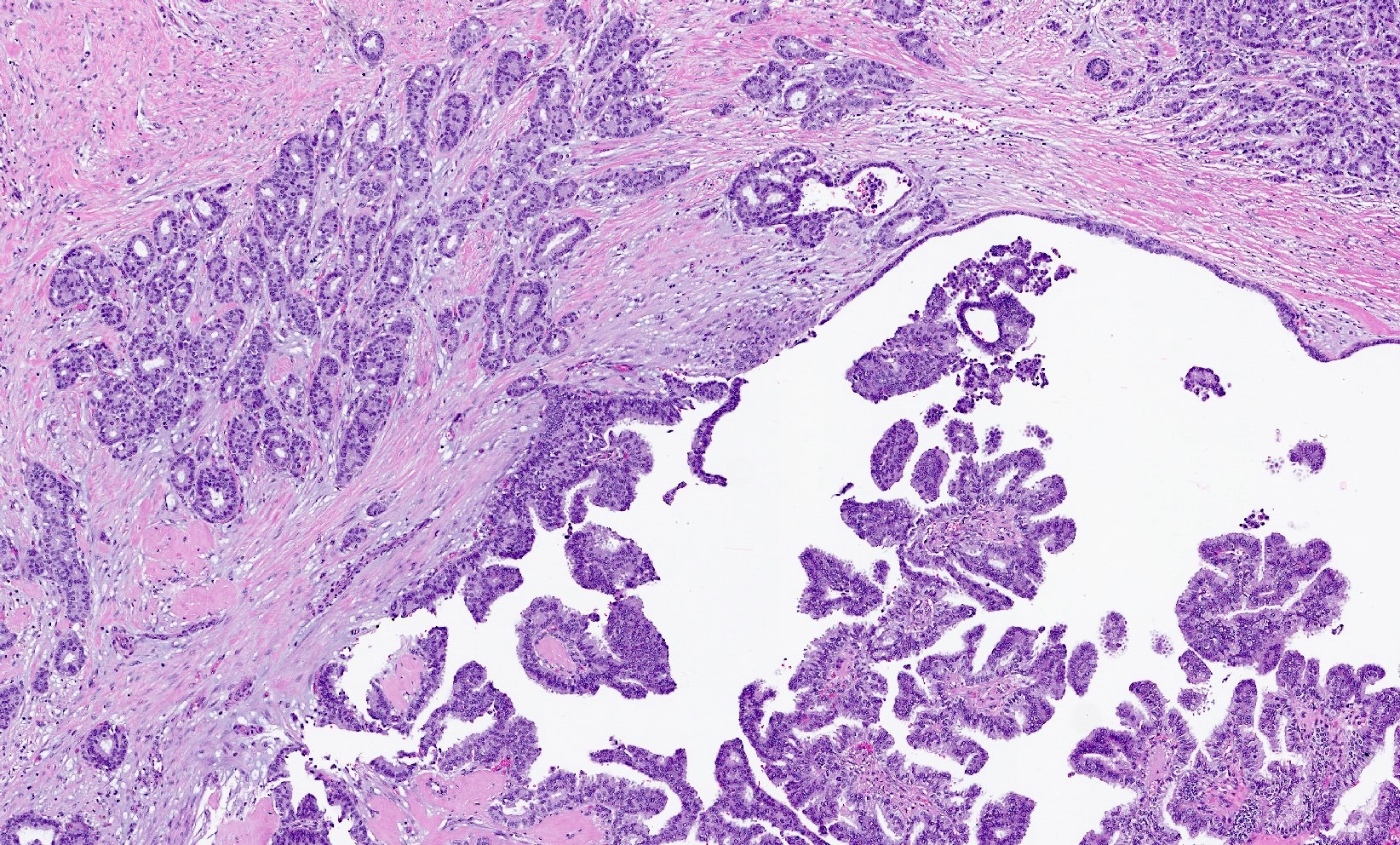
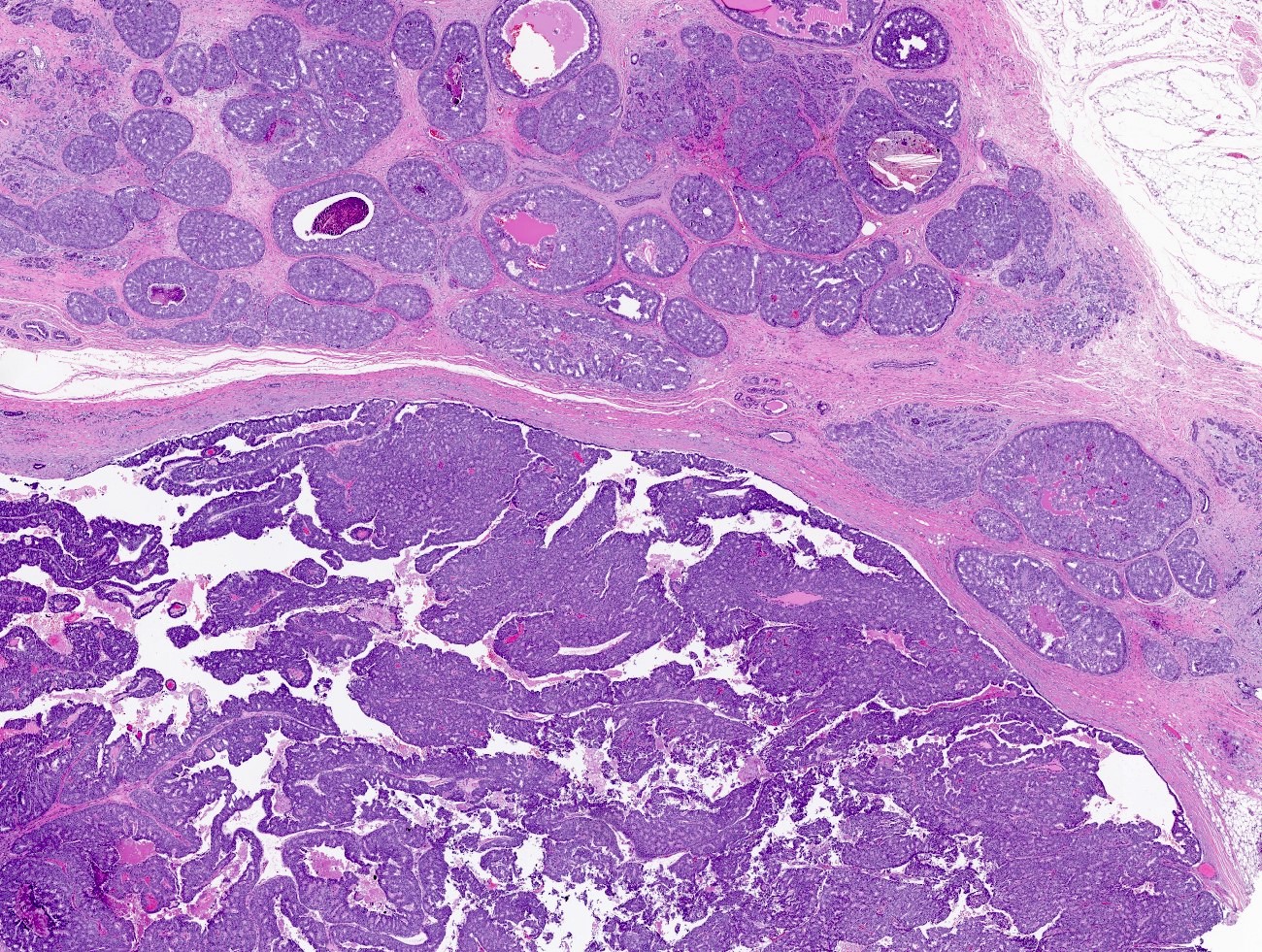
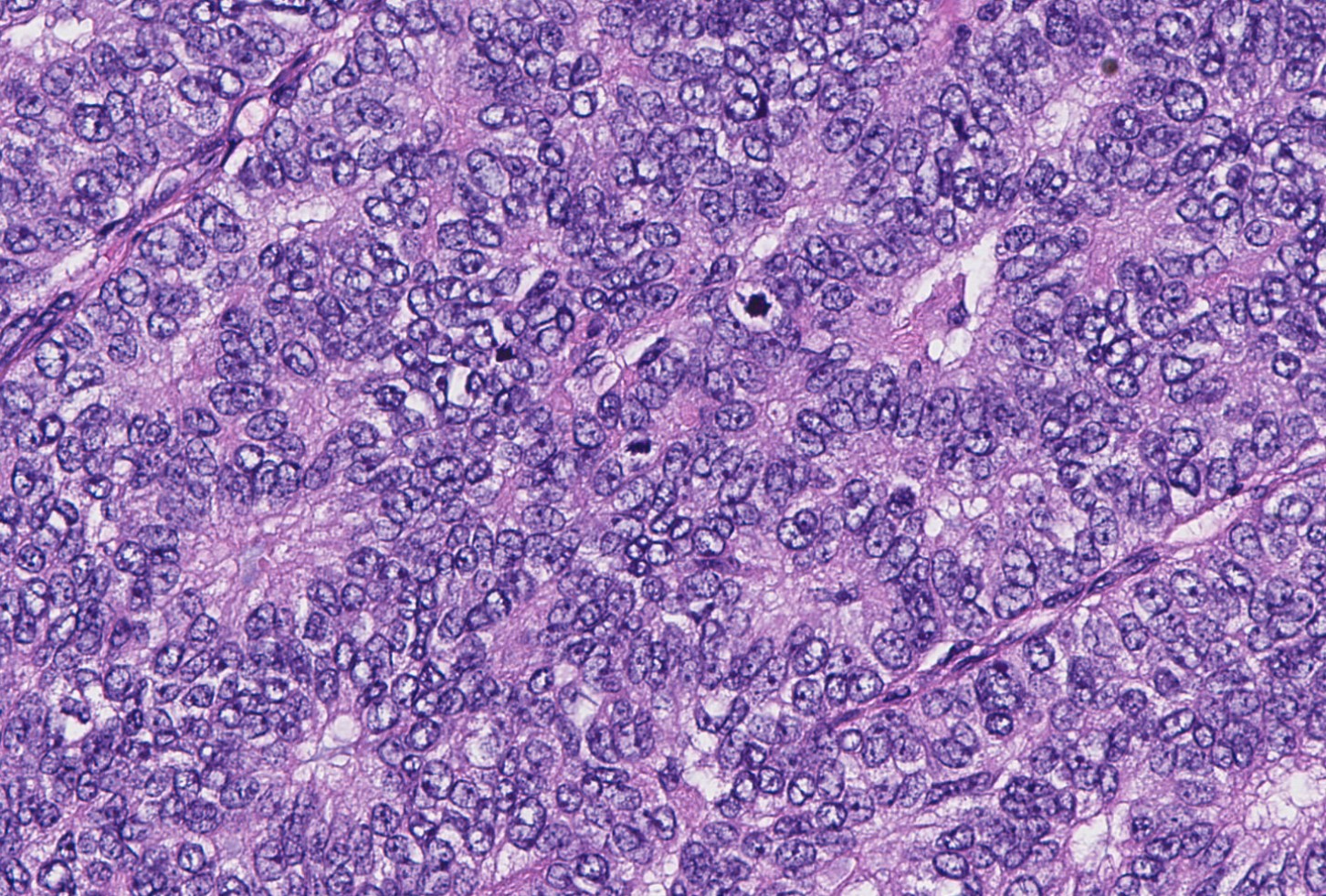
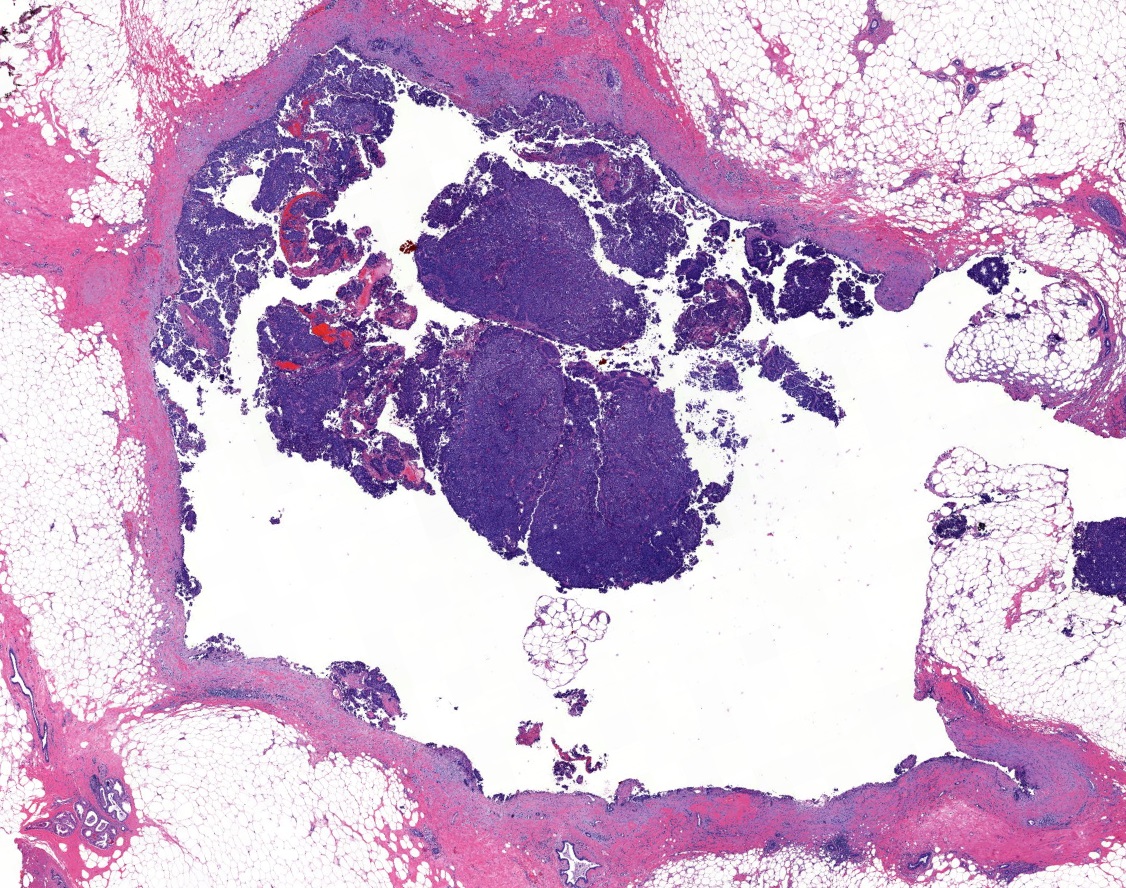
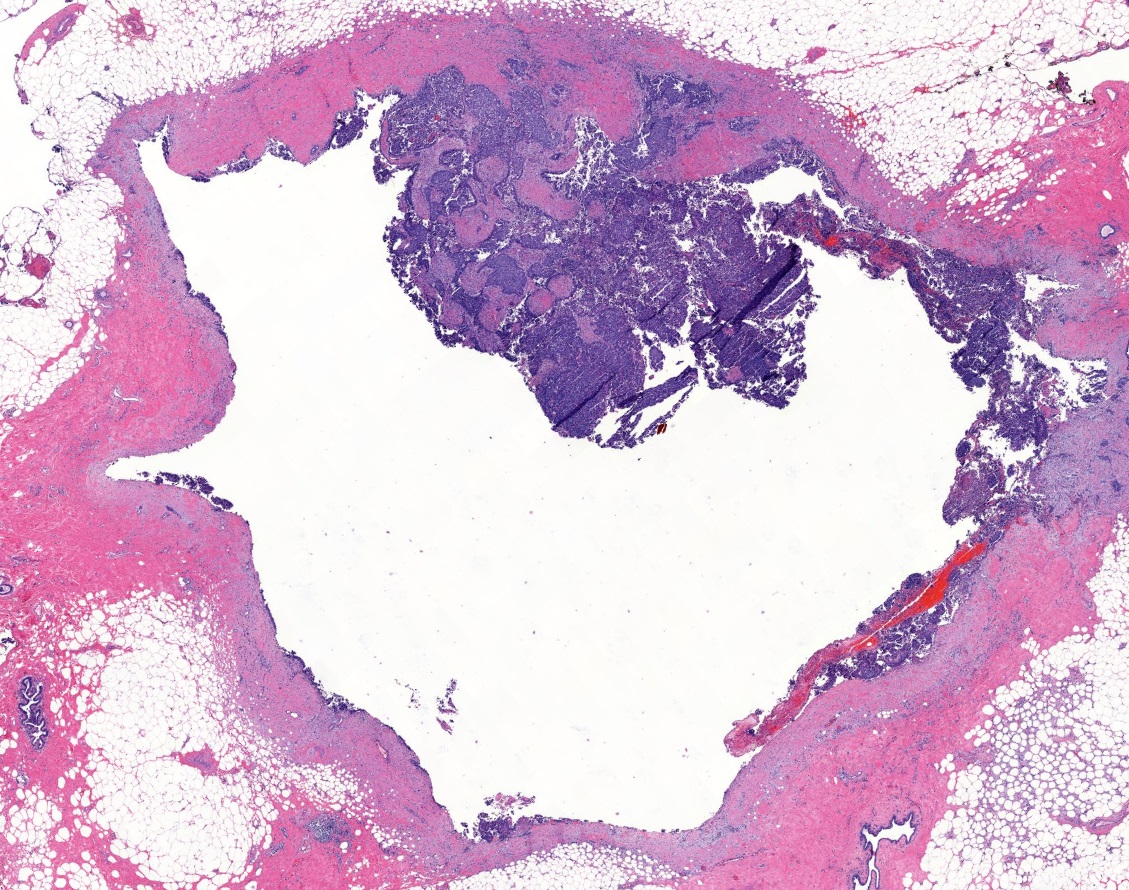
- Papillary tumor with pushing borders, may be within a cystically dilated duct, surrounded by a thick fibrous capsule (Histopathology 2008;52:20, Mod Pathol 2021;34:1044, Virchows Arch 2022;480:5)
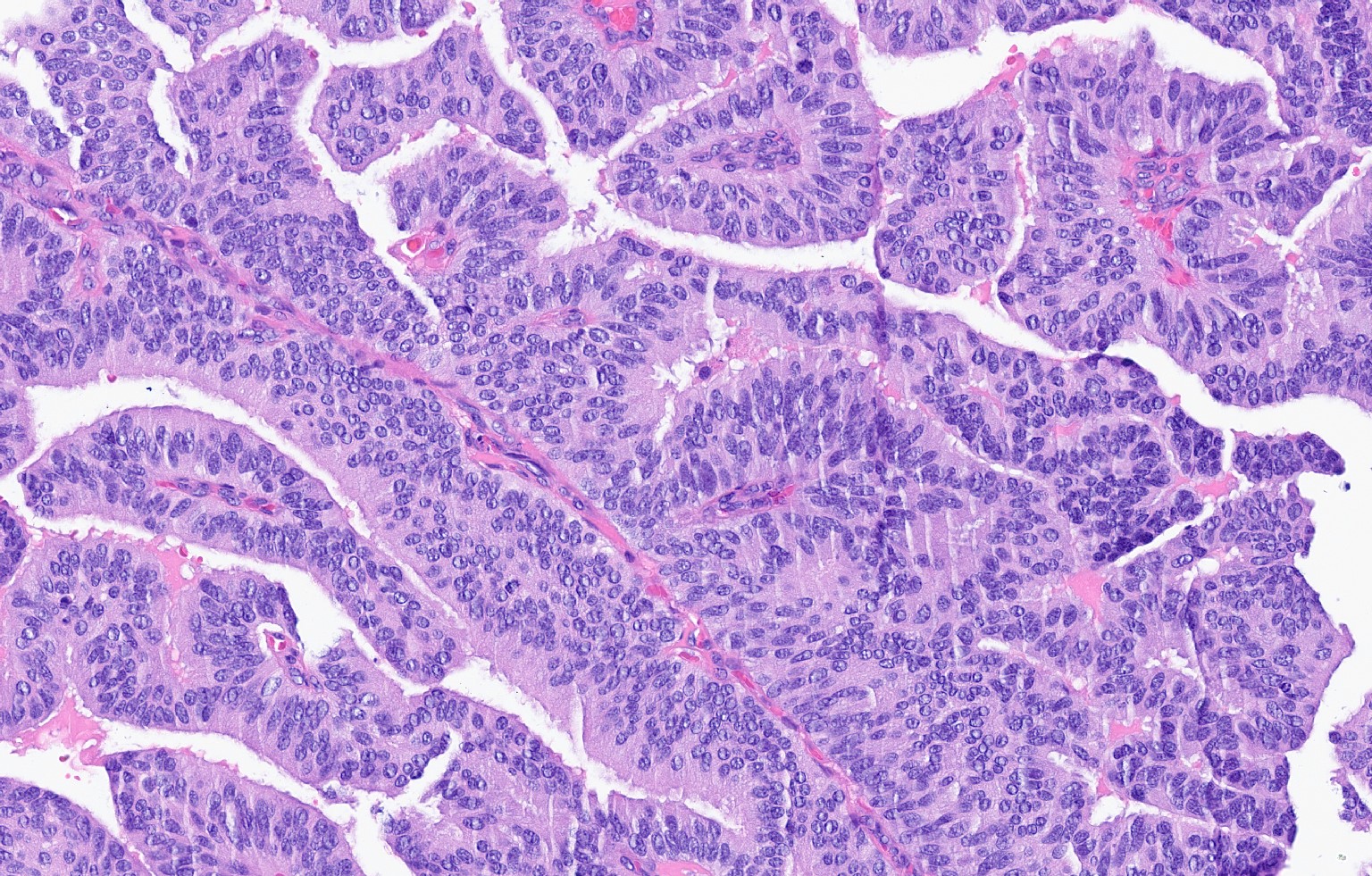
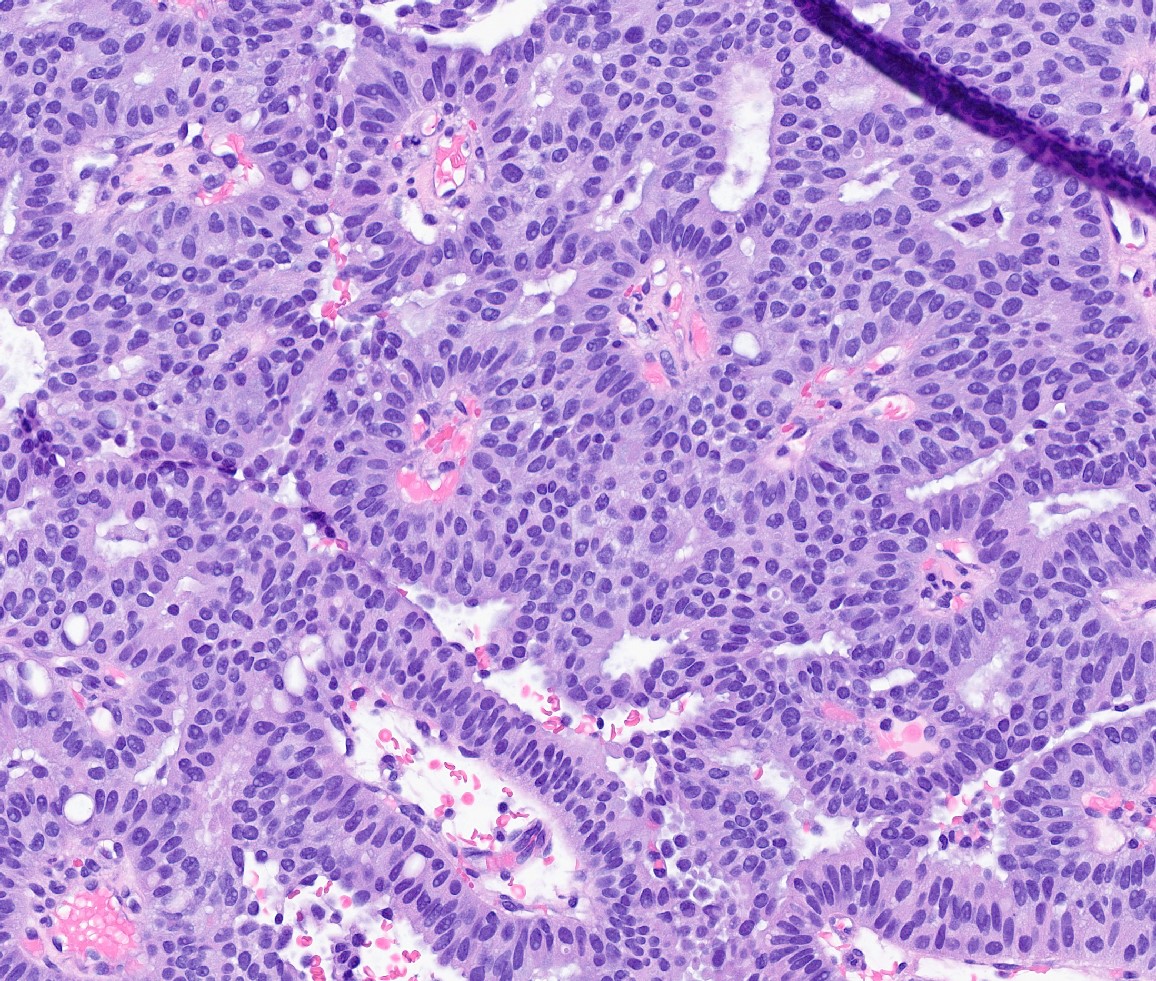
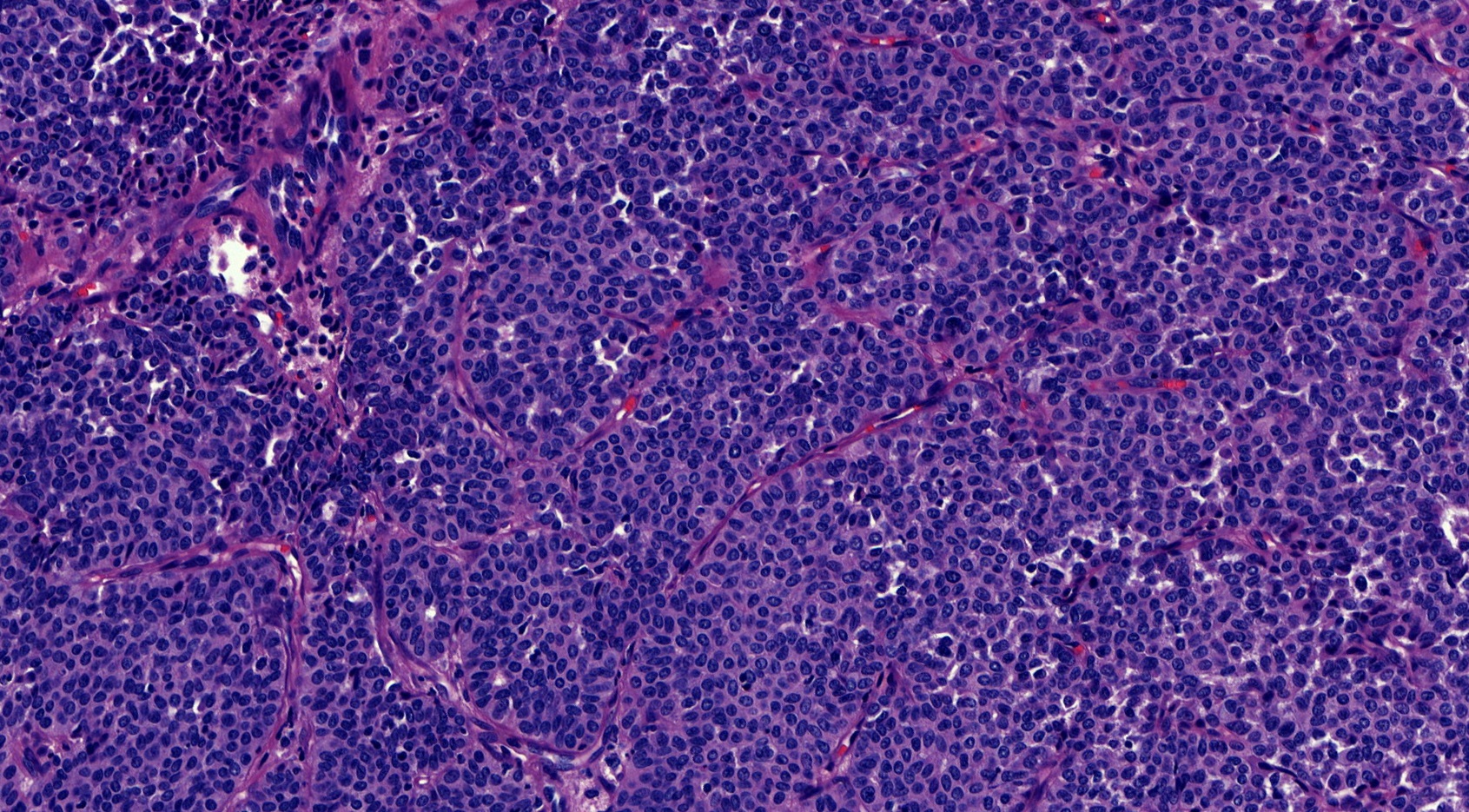
- Delicate papillary fronds with fibrovascular cores lined by cuboidal to columnar epithelial cells with low to intermediate grade atypia
- Cribriform and solid architecture may be present
- Low mitotic activity (average 3 mitoses per 10 high power fields [HPFs]) (Am J Surg Pathol 2011;35:1)
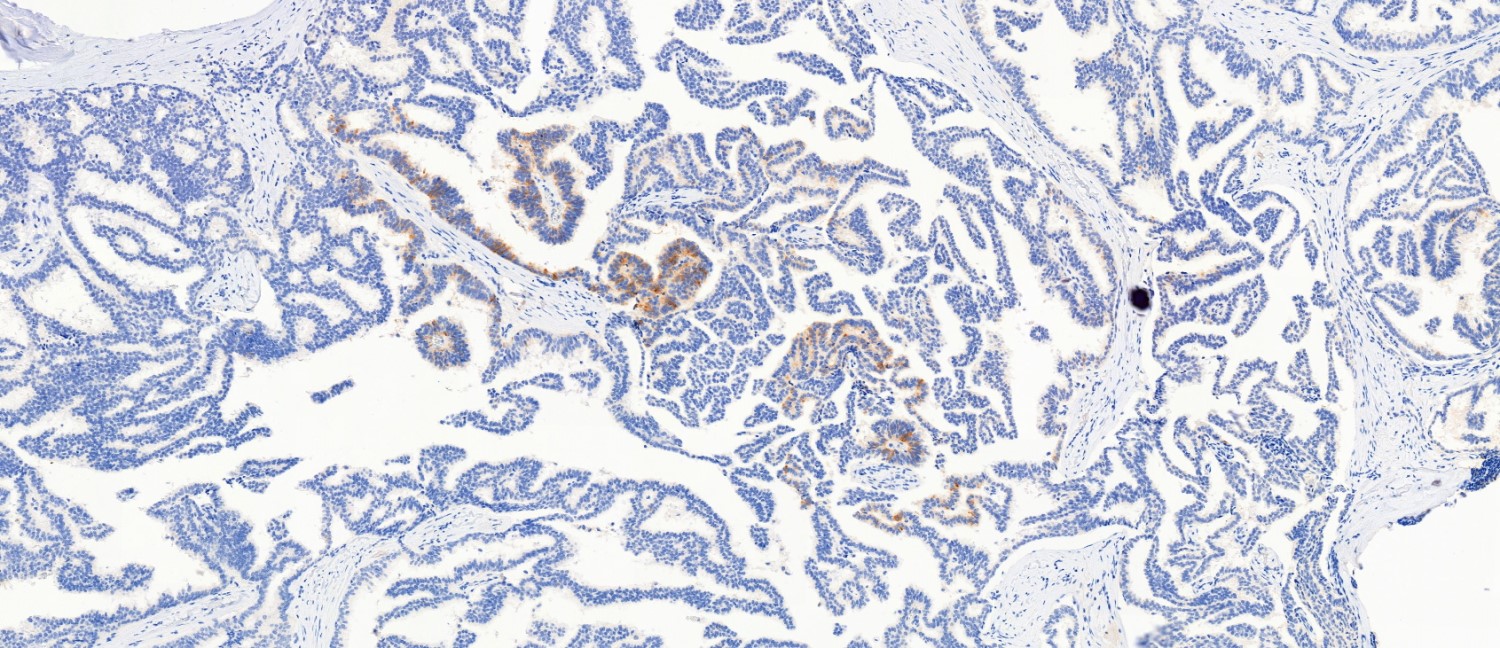
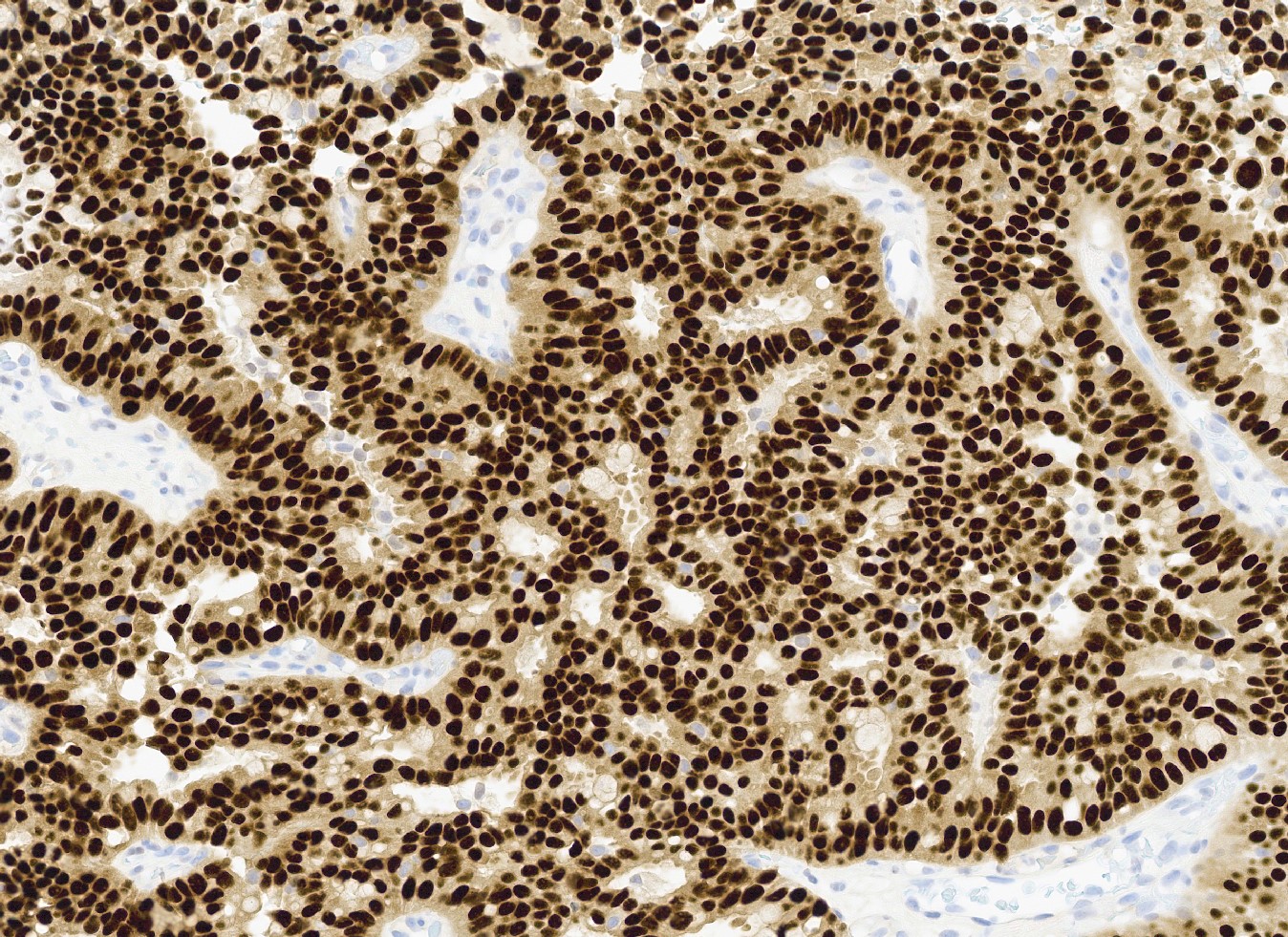
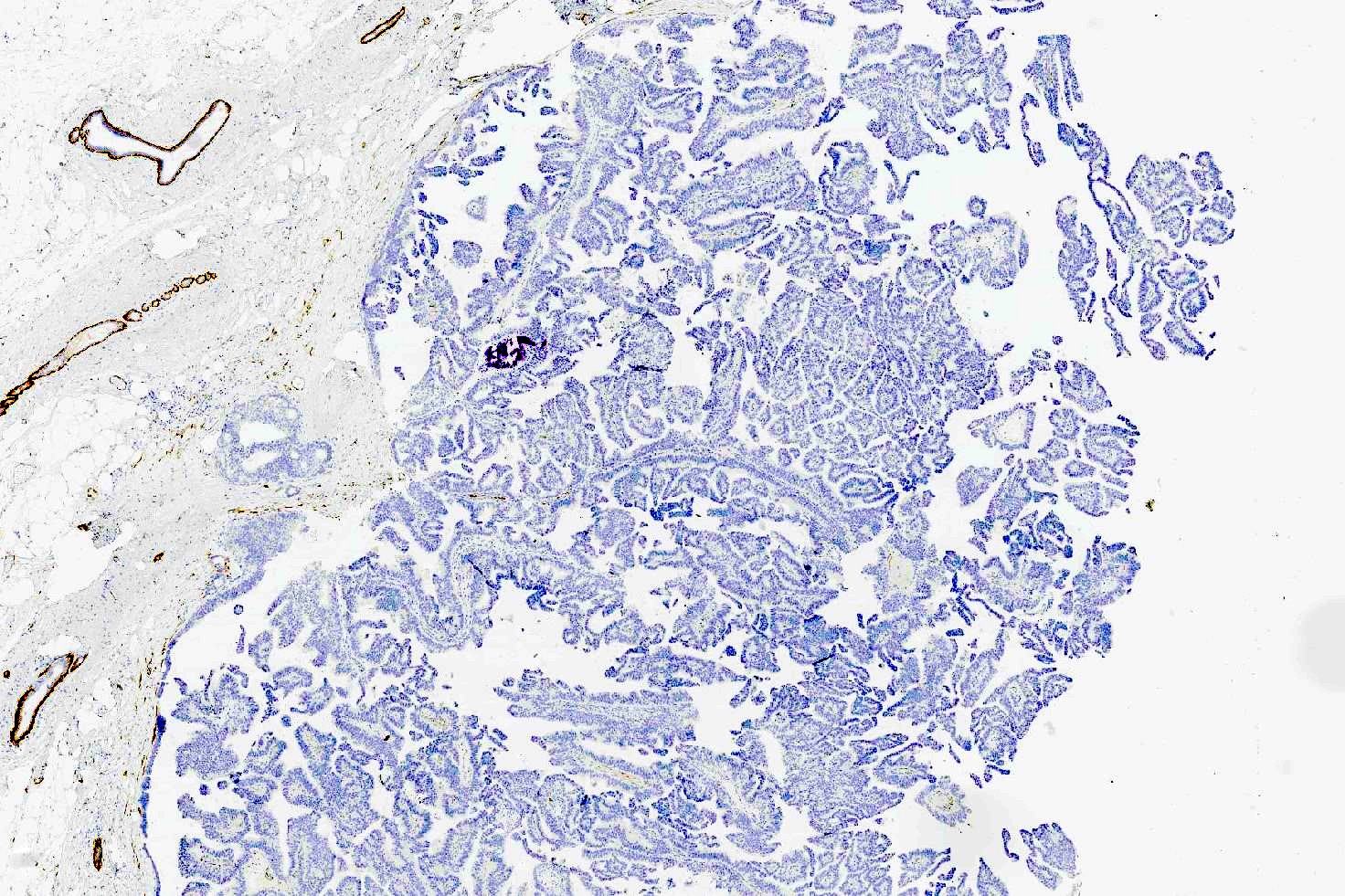
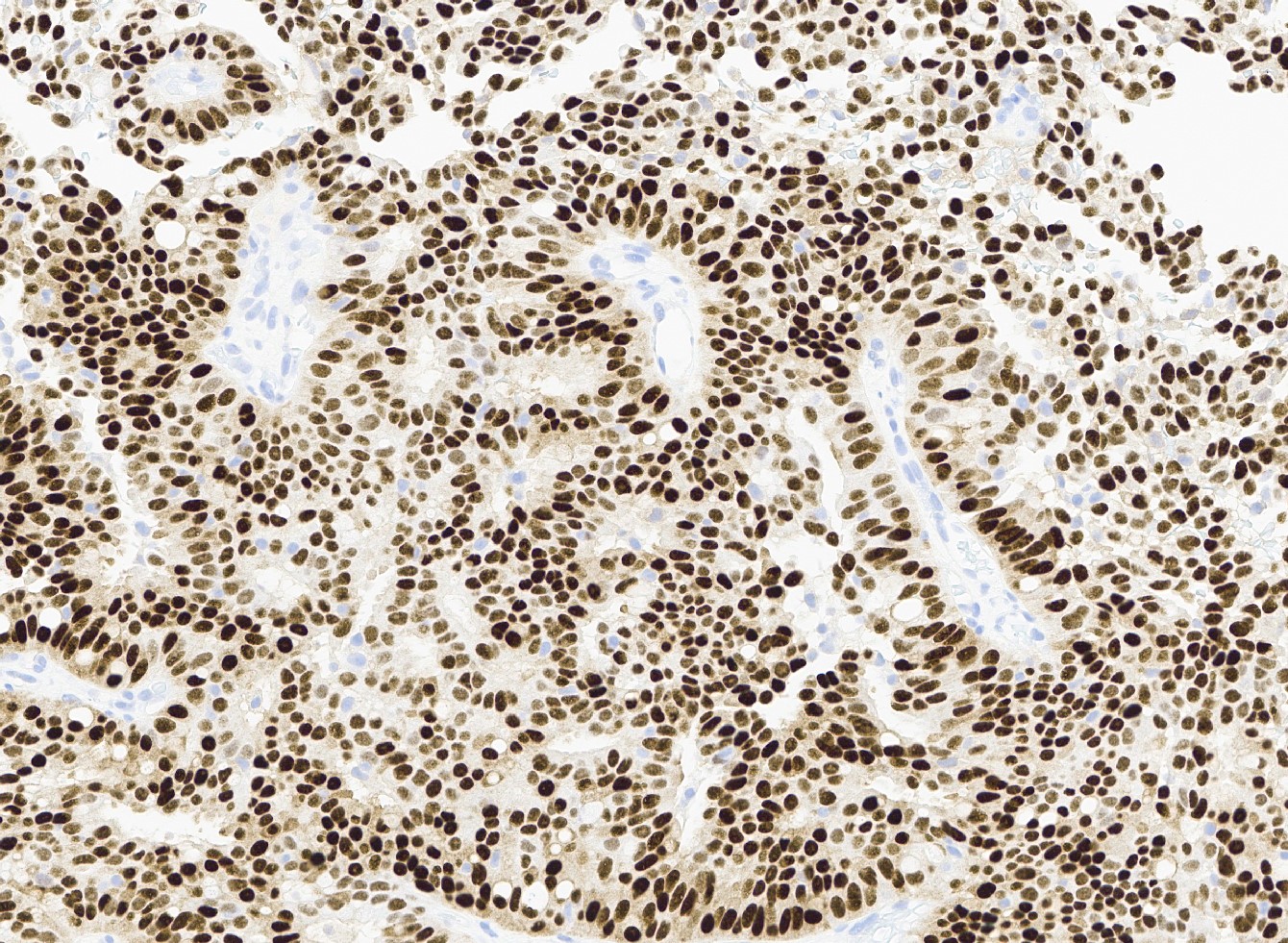
- Most show complete lack of myoepithelial cells along the papillae and around the periphery of the tumor (Am J Surg Pathol 2006;30:1002, Am J Surg Pathol 2011;35:1)
- Basement membrane markers (collagen IV, laminin) may be expressed around the periphery (Pathobiology 2021;88:359, Am J Clin Pathol 2009;131:228)
- Invasive carcinoma is defined as the presence of neoplastic cells infiltrating beyond fibrous capsule (Mod Pathol 2021;34:1044)
- Most commonly invasive carcinoma of no special type (IDC NST), small (pT1), ER+, HER2- and low grade (Am J Surg Pathol 2011;35:1093, Breast J 2021;27:209, Breast J 2019;25:539, Curr Probl Cancer 2018;42:291)
- Staging is based on the size of the conventional invasive component if present
- Epithelial displacement / entrapment of neoplastic cells within capsule can occur and must be distinguished from true invasion beyond the fibrous capsule
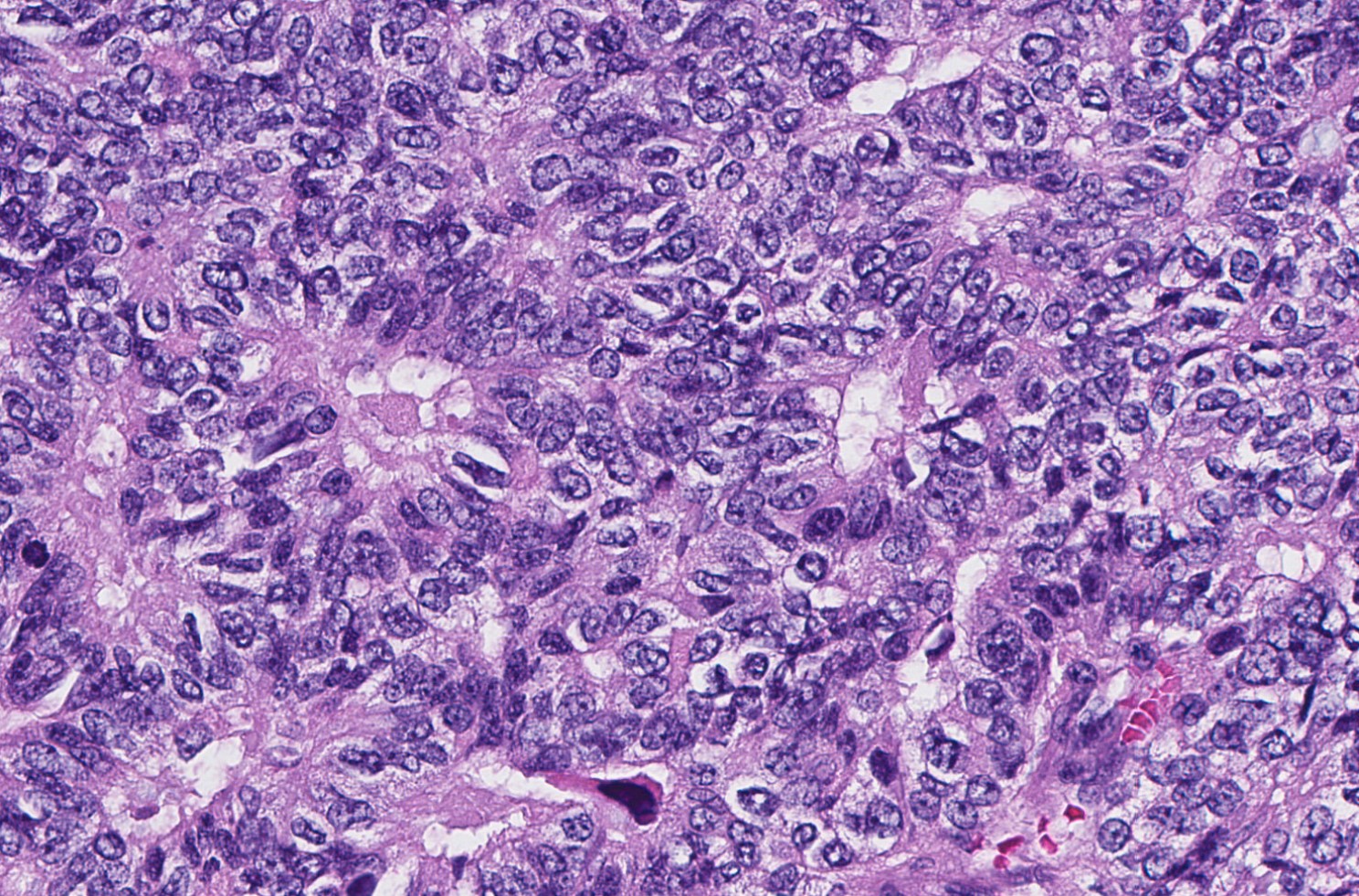
- High grade invasive carcinoma with EPC features (Histopathology 2015;66:740, Histol Histopathol 2019;34:137)
- High grade cytologic atypia with nuclear pleomorphism, frequent mitotic figures (mean mitotic activity 22 per 10 HPFs) and occasional necrosis
- More likely to be ER- or triple negative
Microscopic (histologic) images
Contributed by Kristen E. Muller, D.O. , Mariel Molina Nunez, M.D. and Julie Jorns, M.D. (Case #518)
Cytology description
- No formal cytologic criteria exist to distinguish EPC from other benign papillary lesions (J Clin Pathol 2008;61:945)
- Sensitivity and specificity for specific diagnoses is low
- If papillary lesion is suspected on FNA, surgical biopsy is necessary for further classification
- General findings in fine needle aspirates of EPC (Breast J 2006;12:237, J Clin Pathol 2008;61:945)
- High cellularity, presence of cell balls, presence of slender papillae, mild cytologic atypia
Positive stains
- ER and PR (strong, diffuse) (Curr Probl Cancer 2018;42:291, Mod Pathol 2021;34:1044)
Negative stains
- Myoepithelial markers (i.e., p63, calponin, actin, smooth muscle myosin heavy chain, CD10) negative within papillae and around the tumor or focally present at the periphery of the lesion (Am J Surg Pathol 2006;30:1002, Am J Surg Pathol 2011;35:1, Curr Probl Cancer 2018;42:291)
- HER2
- Chromogranin, synaptophysin (J Pathol 2012;226:427)
Molecular / cytogenetics description
- Similar to ER+, low grade invasive breast carcinomas (J Pathol 2012;226:427, Mol Oncol 2014;8:1588)
- Luminal A
- Frequent PIK3CA mutations
- 16q losses, 16p gains and 1q gains
- Similar copy number alterations to solid papillary carcinoma and invasive papillary carcinoma (Mol Oncol 2014;8:1588)
Videos
Papillary lesions of the breast
Sample pathology report
- Breast, right, partial mastectomy:
- Encapsulated papillary carcinoma (see comment)
- Comment: Histologic sections show a circumscribed papillary tumor surrounded by a thick fibrous capsule. Cytologically, the tumor cells are columnar and cuboidal with low grade nuclear atypia. The lesion lacks myoepithelium throughout the fibrovascular cores and around the periphery. Conventional invasive carcinoma is not seen infiltrating into or beyond the fibrous capsule. In the absence of an invasive carcinomatous component, encapsulated papillary carcinomas are staged as in situ (Tis); however, some believe that they may actually be a very good prognosis subtype of invasive carcinoma due to the lack of myoepithelium.
- Breast, right, core needle biopsy (when entire lesion is not removed or cannot be visualized):
- Low grade papillary carcinoma (see comment)
- Comment: The biopsy contains fragments of an atypical lesion with papillary architecture and low grade monomorphic nuclear atypia. p63 and calponin immunostains are negative for myoepithelium throughout the lesion and around the periphery; however, the periphery of the lesion is not completely visualized in the biopsy. The findings raise the possibility of a low grade encapsulated papillary carcinoma. Papillary ductal carcinoma in situ is also in the differential. A conventional invasive carcinoma is not present in this biopsy. Definitive classification is deferred to the surgical specimen.
Differential diagnosis
- Papilloma with atypical ductal hyperplasia (ADH) or ductal carcinoma in situ (DCIS):
- Residual underlying papilloma may be present with areas of usual ductal hyperplasia (UDH), apocrine metaplasia and columnar cell change which lack atypia
- Myoepithelial cells present in residual fibrovascular cores in nonatypical areas and at the periphery
- Papillary ductal carcinoma in situ (DCIS):
- Involvement of multiple ducts in DCIS pattern
- May coexist with other patterns of DCIS
- Myoepithelium present at the periphery
- Intraductal papilloma:
- Lacks cytological atypia
- Areas of benign proliferative changes (UDH, apocrine metaplasia, columnar cell changes)
- Myoepithelium present throughout papillae and at the periphery
- Solid papillary carcinoma:
- Single or multiple nodules with solid architecture and rudimentary, delicate fibrovascular cores
- Lacks encircling dense fibrous capsule
- Cells may be spindled, produce mucin and have neuroendocrine features
- Similar to encapsulated papillary carcinoma, lacks myoepithelium within tumor nests and around the periphery
- Invasive papillary carcinoma:
- Cystically dilated small glands with papillae with frankly infiltrative pattern without surrounding fibrous capsule
- Negative for myoepithelium
- Invasive lobular carcinoma with papillary growth pattern (Breast J 2020;26:1231, Breast Cancer 2021;28:1383, Pathobiology 2016;83:221):
- Rare growth pattern of invasive lobular carcinoma that mimics encapsulated or solid papillary carcinoma
- Classic invasive lobular carcinoma, atypical lobular neoplasia (ALH), LCIS present beyond the capsule
- Discohesive tumor cells
- Negative for E-cadherin
Additional references
Board review style question #1
What is the expected pattern of myoepithelial cell distribution in encapsulated papillary carcinoma of the breast?
- Absent both centrally within the lesion and along the periphery
- Absent centrally within the lesion but diffusely present along the periphery
- Present both centrally within the lesion and along the periphery
- Present only focally within the center of the lesion but diffusely present along the periphery
Board review style answer #1
A. Absent both centrally within the lesion and along the periphery. Encapsulated papillary carcinomas characteristically lack myoepithelial cells both within and along the edge of the lesion. The remaining answer choices apply to other papillary lesions of the breast; a benign intraductal papilloma has myoepithelial cells lining the entirety of the proliferation both centrally and peripherally, whereas a papilloma involved by DCIS and papillary DCIS will show focal to complete absence of myoepithelium centrally (corresponding to the regions of atypia) with retention peripherally.
Comment Here
Reference: Encapsulated papillary carcinoma
Comment Here
Reference: Encapsulated papillary carcinoma
Board review style question #2
A 72 year old woman undergoes partial mastectomy for a 1.8 cm papillary lesion in the retroareolar tissue of her left breast. A diagnosis of encapsulated papillary carcinoma is made upon finding absent myoepithelium within the papillae and around the periphery. How should this lesion be staged, according to the AJCC TNM classification system?
- T0
- Tis
- T1
- T2
Board review style answer #2
B. Tis. Encapsulated papillary carcinoma is staged as an in situ lesion given its similar clinical behavior to ductal carcinoma in situ. If conventional invasive carcinoma is found, infiltrating beyond the fibrous capsule, the lesion should be staged according to the size of the invasive component only; the size of the EPC should not be included for staging.
Comment Here
Reference: Encapsulated papillary carcinoma
Comment Here
Reference: Encapsulated papillary carcinoma
Board review style question #3
In which group is encapsulated papillary carcinoma of the breast most commonly seen?
- Childhood (≤ 18 years)
- Lactating / pregnant
- Men
- Postmenopausal women
Board review style answer #3
D. Postmenopausal women. Encapsulated papillary carcinoma (EPC) of the breast is an uncommon breast cancer that is classified as in situ, is typically low to intermediate grade and most frequently occurs in elderly, postmenopausal women rather than in younger women. EPCs constitute a slightly higher proportion of breast cancers in male patients as compared to female patients. However, male breast cancer is uncommon and is most frequently invasive ductal carcinoma (comprising about 85% of male breast cancers).
Comment Here
Reference: Encapsulated papillary carcinoma
Comment Here
Reference: Encapsulated papillary carcinoma