Table of Contents
Definition / general | Essential features | Terminology | Physiology | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Patil A, Zhang L. Anatomy & histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonhistology.html. Accessed August 22nd, 2025.
Definition / general
- Colon: the terminal portion of the gastrointestinal tract situated in the abdomen and the pelvis
- Includes the cecum, ascending colon, transverse colon, descending colon, sigmoid colon and rectum
Essential features
- Colonic mucosa has 2 predominant functions:
- Absorption of water and electrolytes from the nutrient poor chyme that passes into the colon from the ileum
- Production of mucus to lubricate the fecal material
- Above functions are accomplished by 2 predominant cell types:
- Absorptive columnar cells absorb water and electrolytes, line the surface epithelial layer and are the major cell type of crypts in the right and transverse colon
- Goblet cells secrete mucus and are the major cell type of the crypts in the left side of the colon
- Inflammatory cells are normally present in the lamina propria and include plasma cells, macrophages, eosinophils and lymphocytes
- Lymphoid aggregates and follicles are also normally present
- Architectural discipline of colon with parallel test tube-like arrangement of crypts separated by a consistent amount of lamina propria in between is important to identify
- Expansion of this lamina propria and dropout of crypts can be signs of chronic injury
Terminology
- Lower gastrointestinal tract, large bowel, large intestine
Physiology
- Colon is lined by mucosa on the luminal surface
- Epithelial layer of the mucosa has columnar cells that absorb water and electrolytes from the nutrient poor chyme received from the small intestine as it passes through the proximal colon (Hall: Guyton and Hall Textbook of Medical Physiology, 14th Edition, 2020)
- Chyme is then lubricated with mucus secreted by the goblet cells primarily in the left side of the colon to eventually form feces that is stored in the distal colon and the rectum (Hall: Guyton and Hall Textbook of Medical Physiology, 14th Edition, 2020)
- Propulsion of fecal material in the colon is achieved by the muscular layer of the colon composed of inner circular layer and outer longitudinal layer (Hall: Guyton and Hall Textbook of Medical Physiology, 14th Edition, 2020)
- Colon plays a critical role in immune defense
- Interactions between innate immune system, adaptive immune system and gut microbiota are important in regulating immune homeostasis
Gross description
- Colon is approximately 1.5 meters long with a diameter of 6 - 7 cm
- From terminal ileum to anal canal, the colon is divided into cecum, ascending colon, transverse colon, descending colon, sigmoid colon and rectum
- Segments of the colon that are completely intraperitoneal include the cecum, transverse colon and sigmoid colon (Amin: AJCC Cancer Staging Manual, 8th Edition, 2017)
- Ascending colon and descending colon and upper third of the rectum are retroperitoneal, with the anterior and lateral surface covered by peritoneum (Amin: AJCC Cancer Staging Manual, 8th Edition, 2017)
- Middle third of the rectum only has peritoneum on the anterior surface and the lower third is completely nonperitonealized (Amin: AJCC Cancer Staging Manual, 8th Edition, 2017)
- These correct anatomic landmarks are very important in evaluation of margins and staging of colorectal cancers (Amin: AJCC Cancer Staging Manual, 8th Edition, 2017)
- Different from small intestine, the colon has epiploic appendages (pedunculated fat on lateral side) and taeniae coli (discontinuous muscular fibers)
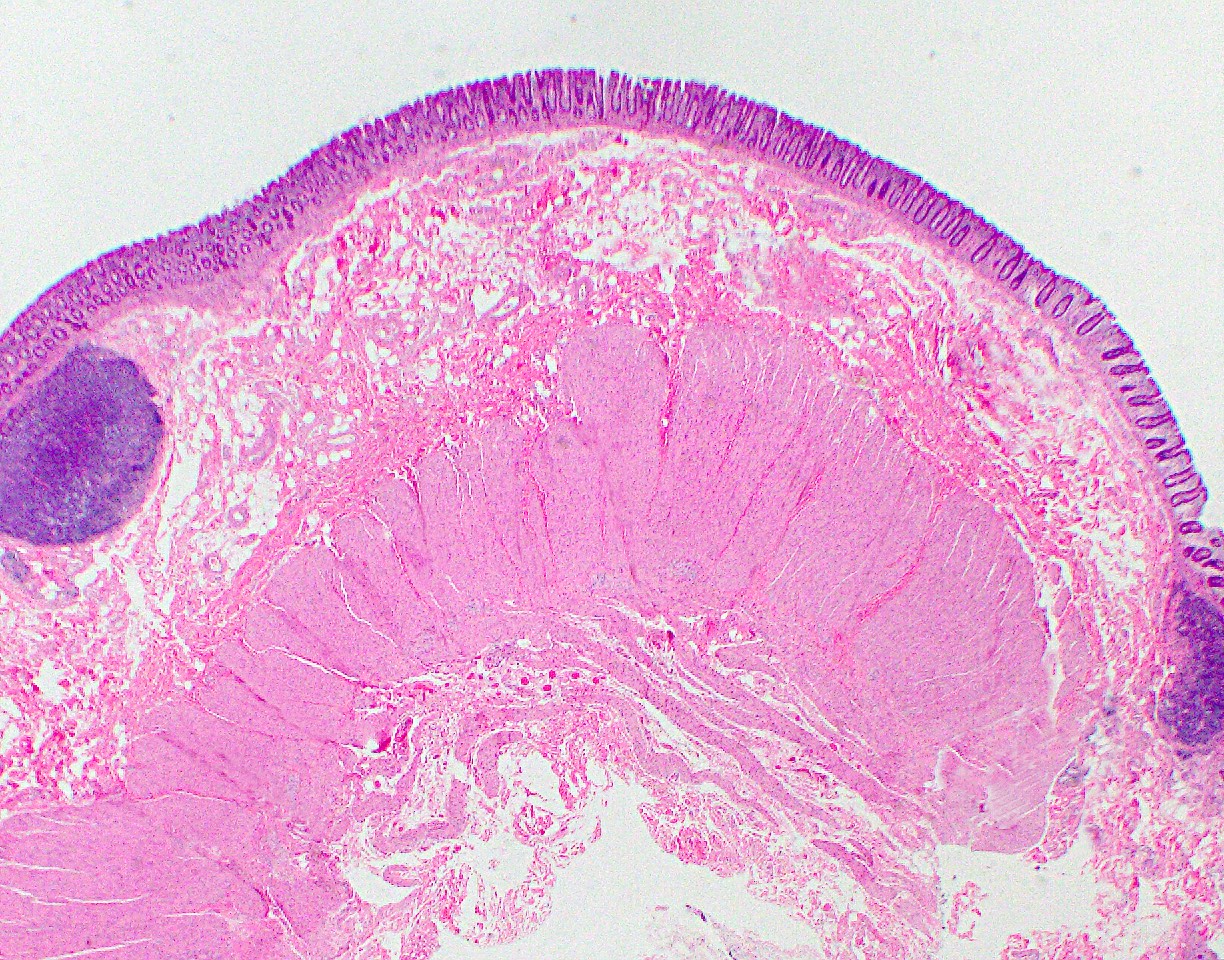
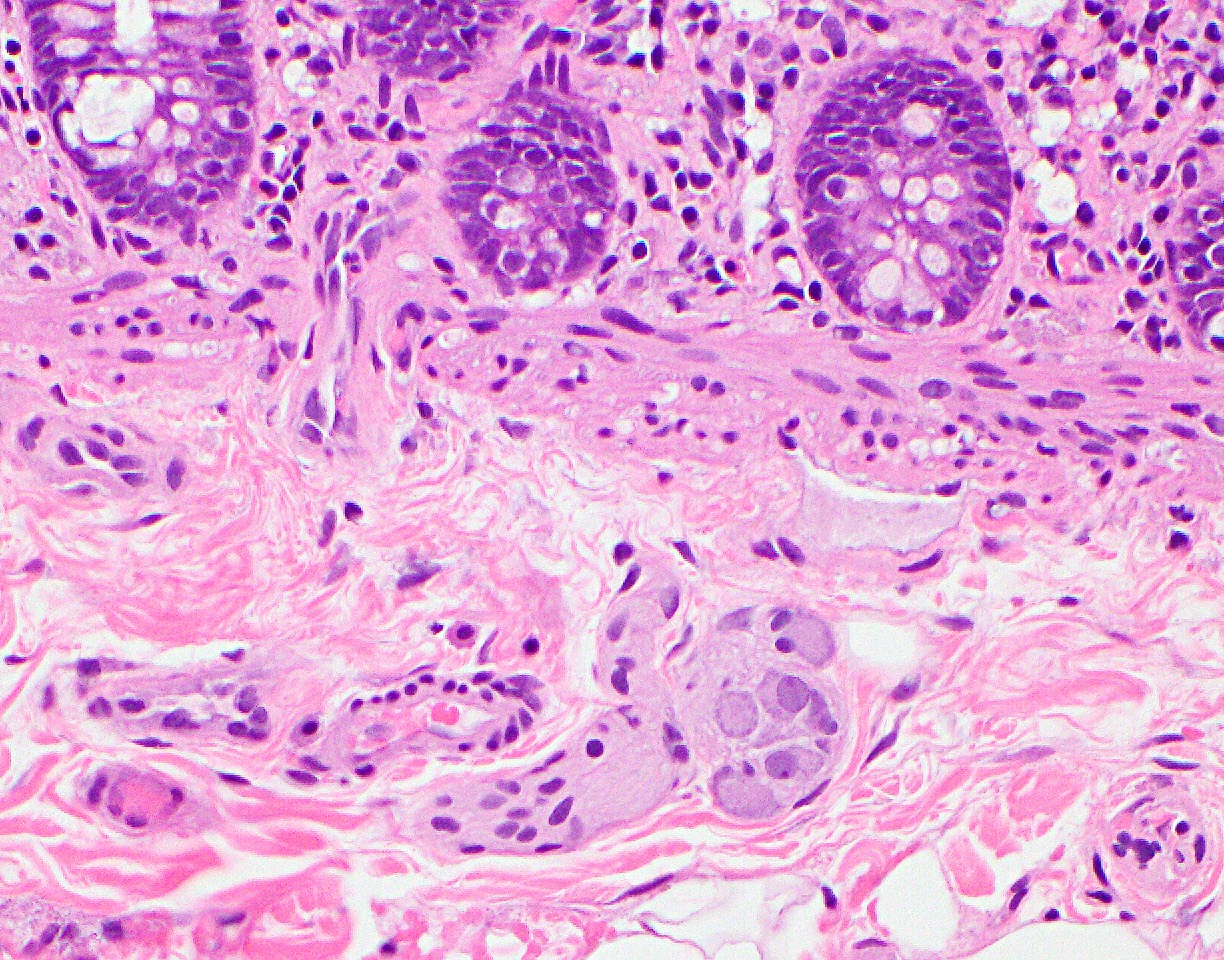
Microscopic (histologic) description
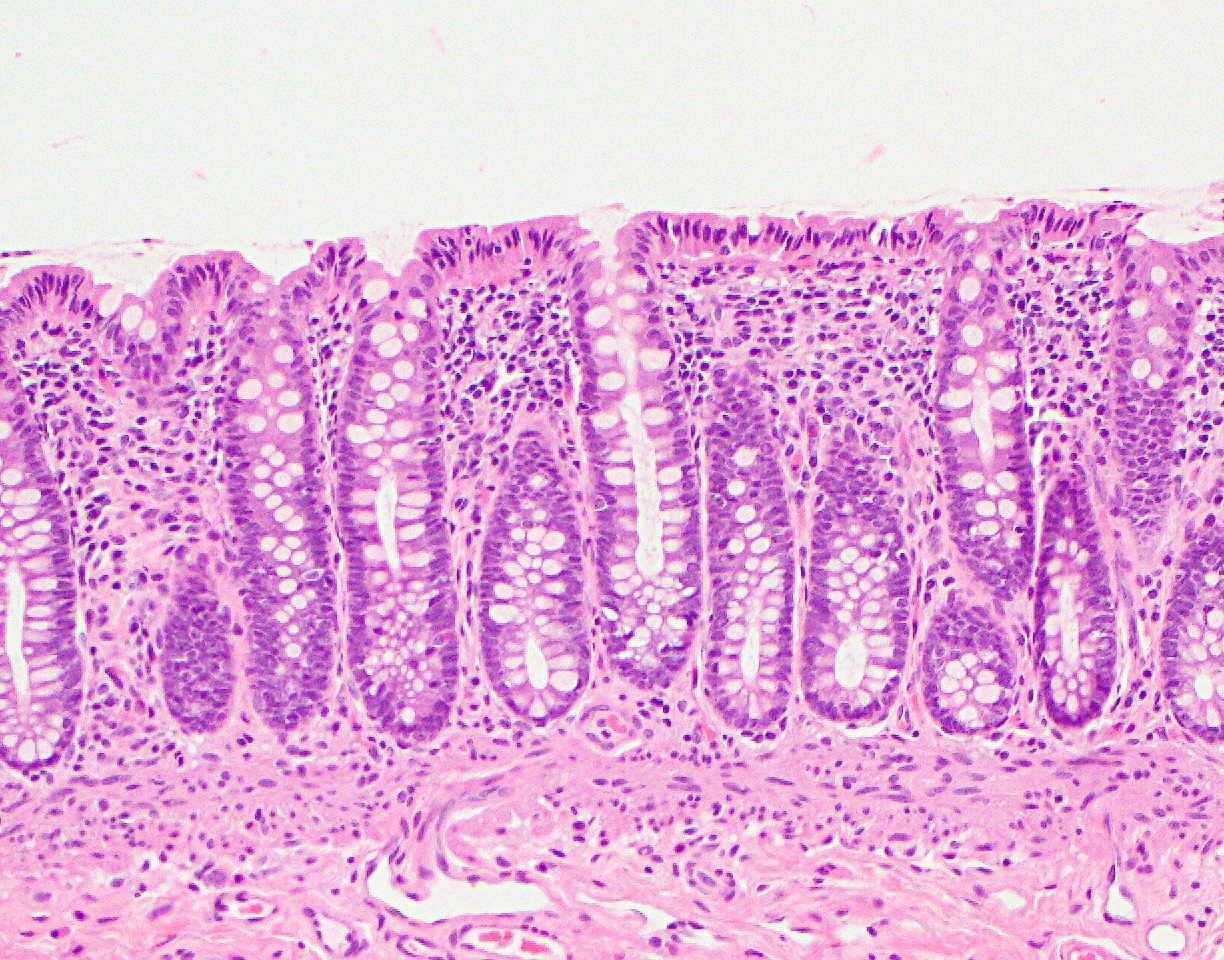
- Mucosa is composed of the epithelium, lamina propria and muscularis mucosa
- Epithelium: colonic epithelium is composed of a single layer of the absorptive columnar cells and the goblet cells
- As the epithelium invaginates into the underlying lamina propria, it forms glandular structures called crypts, arranged in a characteristic parallel test tube-like pattern
- Crypt is a functional unit of colon and is primarily lined by the goblet cells
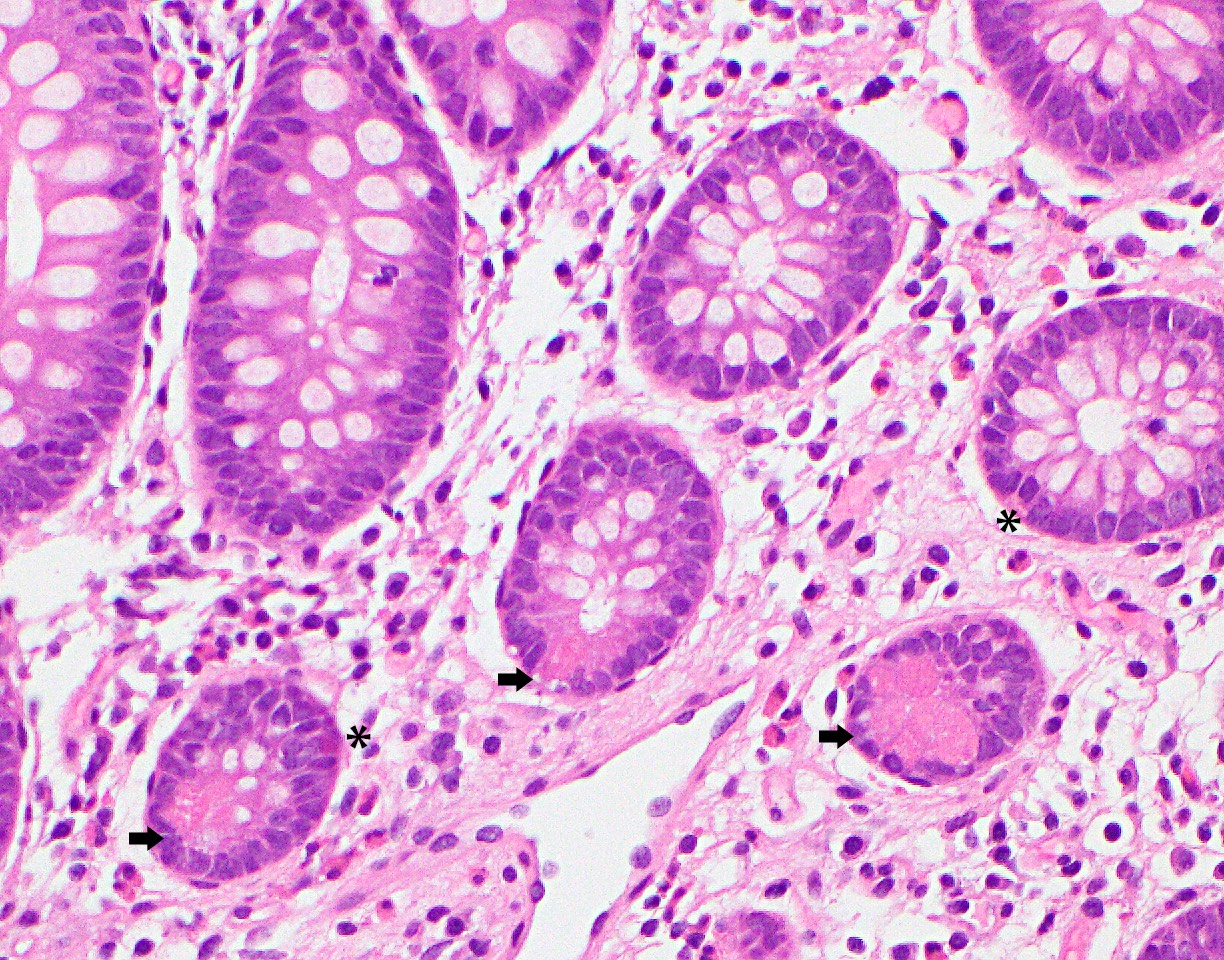
- Crypt also has enteroendocrine cells, Paneth cells and stem cells located at its base
- During the maturation process, the mature epithelial cells migrate toward the surface of the epithelium (luminal migration), while the immature (stem cells) are at the base of the crypts
- On maturation, the Paneth cells migrate to the base of the crypt, instead of the luminal migration
- Enteroendocrine cells also stay in the deeper portion of the crypt and in the middle of the tubule
- Absorptive cells: predominant cells in the right colon
- Columnar cells with eosinophilic cytoplasm, basally located nuclei, small apical mucin vacuoles and apical microvilli
- Primarily line the surface epithelium
- Goblet cells: predominant cells in the left colon
- Large cells with intracytoplasmic mucin and basally located hyperchromatic nuclei
- Mucin composition of goblet cells is different from the mucin in the absorptive cells (Histopathology 2000;37:561)
- Other cell types of the epithelium:
- Enteroendocrine cells:
- Located at the base of the crypts and have eosinophilic secretory granules in the cytoplasm with apically located nuclei
- Apical location of the nuclei helps to differentiate these cells from the Paneth cells
- Paneth cells:
- Paneth cells have a triangular shape with densely eosinophilic cytoplasmic granules
- Nuclei are basally located, unlike enteroendocrine cells described above, a distinction important in the left colon, since the presence of Paneth cells in this part of colon is abnormal and could be a sign of chronic injury
- M cells: typically not identified on routine histology
- Usually associated with lymphoid follicles and seen best with electron microscopy
- Enteroendocrine cells:
- Lamina propria:
- Loose connective tissue rich in capillaries and lymphatics
- Supports the crypts and consists of supportive mesenchymal cells and inflammatory cells
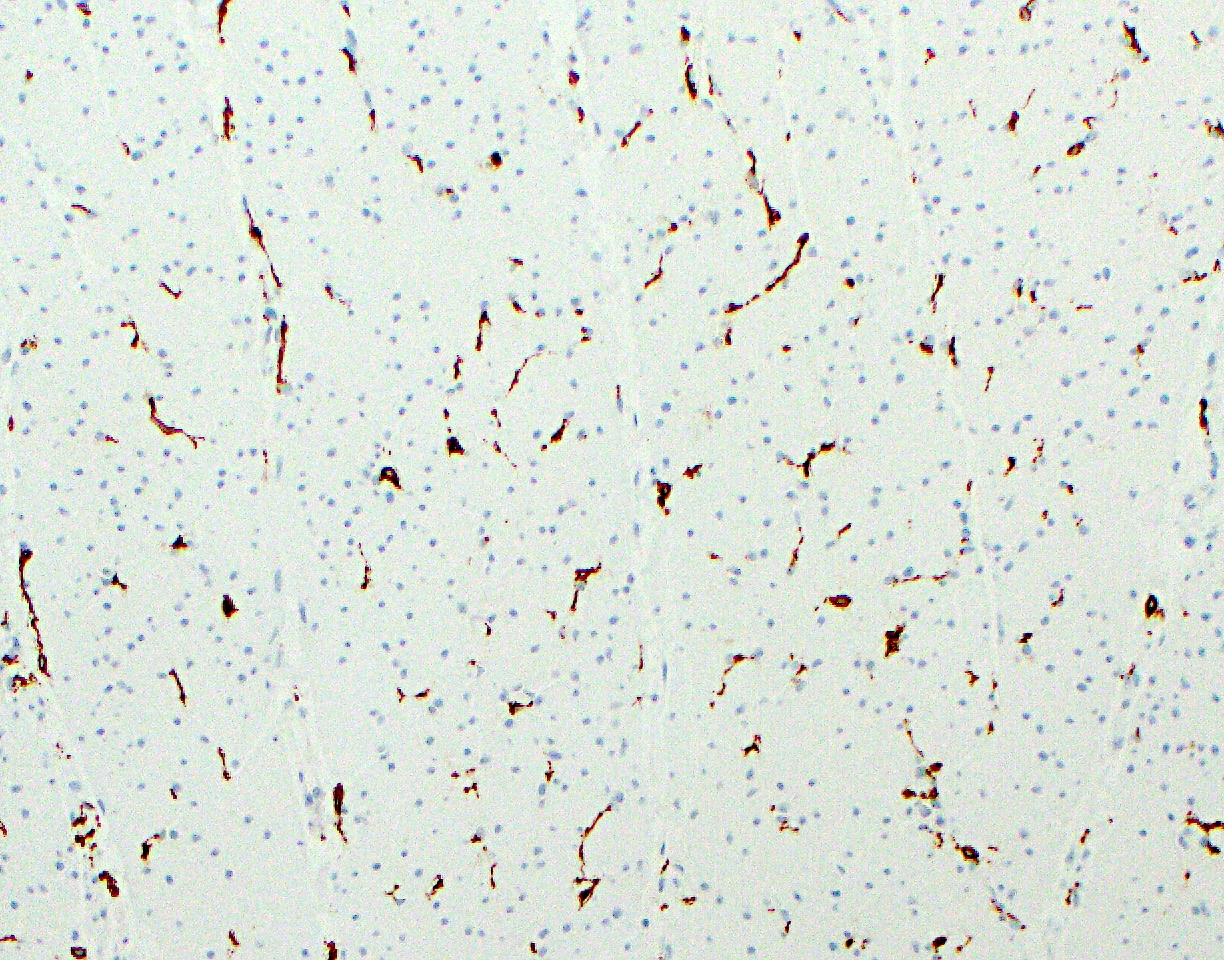
- Mesenchymal cells are divided into 2 types: pericrypt myofibroblasts and subepithelial myofibroblasts
- Inflammatory cells vary in type and number
- Presence of eosinophils, macrophages, lymphocytes and mast cells is normal
- Plasma cells are also normally present and predominantly secrete IgA
- Presence of neutrophils in large number is abnormal
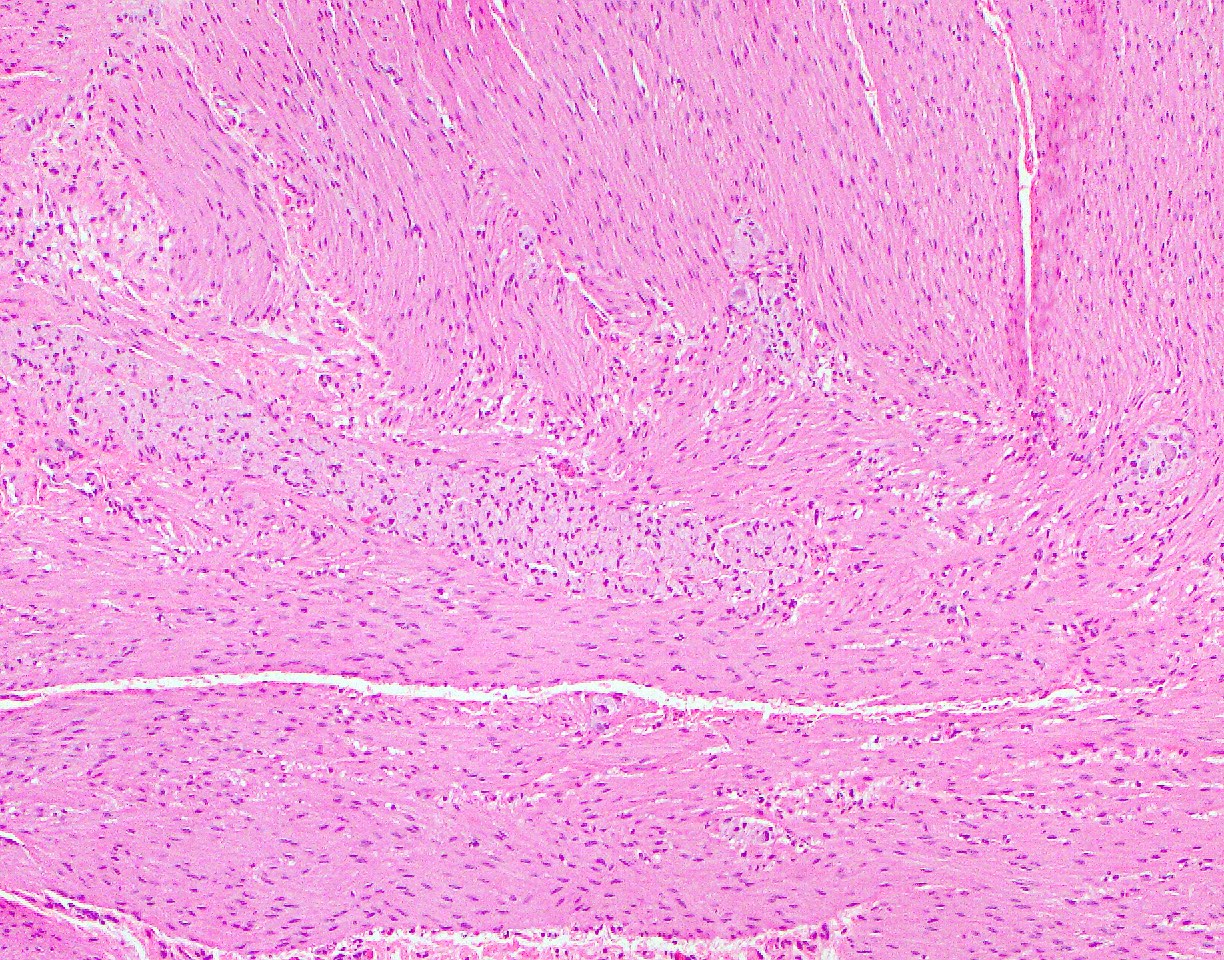
- Muscularis mucosa:
- Muscularis mucosa consists of thin strands of smooth muscle fibers separating the mucosa and submucosa
- Presence of muscularis mucosae in biopsies is critical to evaluate for architectural distortion
- Epithelium: colonic epithelium is composed of a single layer of the absorptive columnar cells and the goblet cells
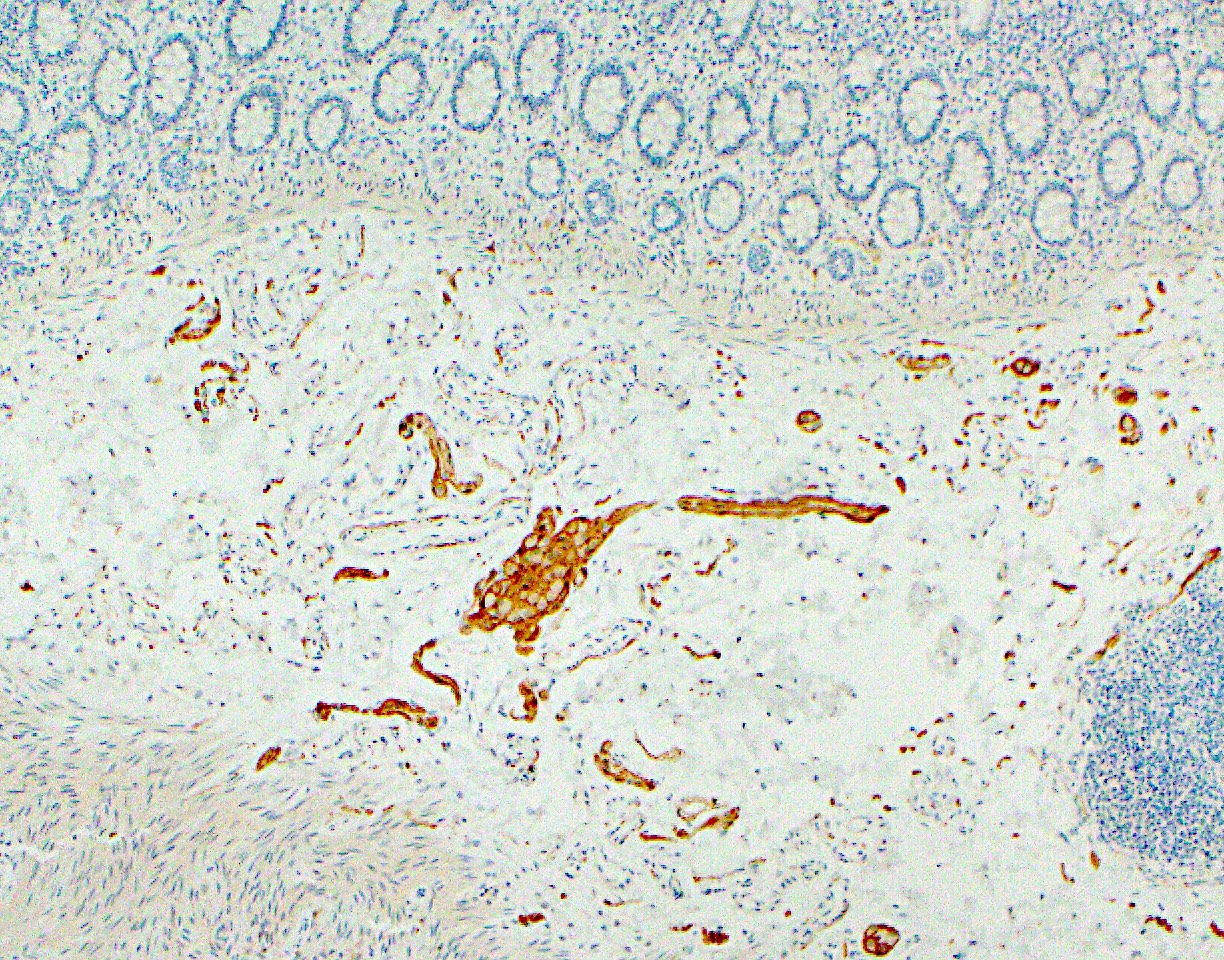
- Submucosa:
- Consists of loose connective tissue, thin smooth muscle bundles, nerve plexuses (Meissner plexus and Henle deep submucosal plexus) with ganglion cells, stromal cells, adipose tissue and vasculature
- Well circumscribed areas of adipose tissue forming a discrete mass within the submucosa may represent lipomas and may present as a mass on endoscopy
- Mucosal lymphoid aggregates or follicles may extend into submucosa, which may contain the crypts, so called lymphoglandular complex mimicking invasive carcinoma in the submucosa
- Muscularis propria:
- Consists of inner circular layer and outer longitudinal layer and Auerbach nerve plexus in between the 2 muscle layers
- Interstitial cells of Cajal are present within the muscularis propria and play a role in peristalsis
- Subserosa and serosa: subserosa is composed of fibroadipose tissue and is covered by the serosa lined by cuboidal mesothelial cells
- Rectum: a continuation of the sigmoid colon with thicker mucosa and longer crypts primarily lined by the goblet cells; the mucosa gradually transitions from columnar to squamous from the rectum into the anal canal
- References: Westerhoff: Histology for Pathologists, 5th Edition, 2019, Kierszenbaum: Histology and Cell Biology - An Introduction to Pathologists, 5th Edition, 2019
Microscopic (histologic) images
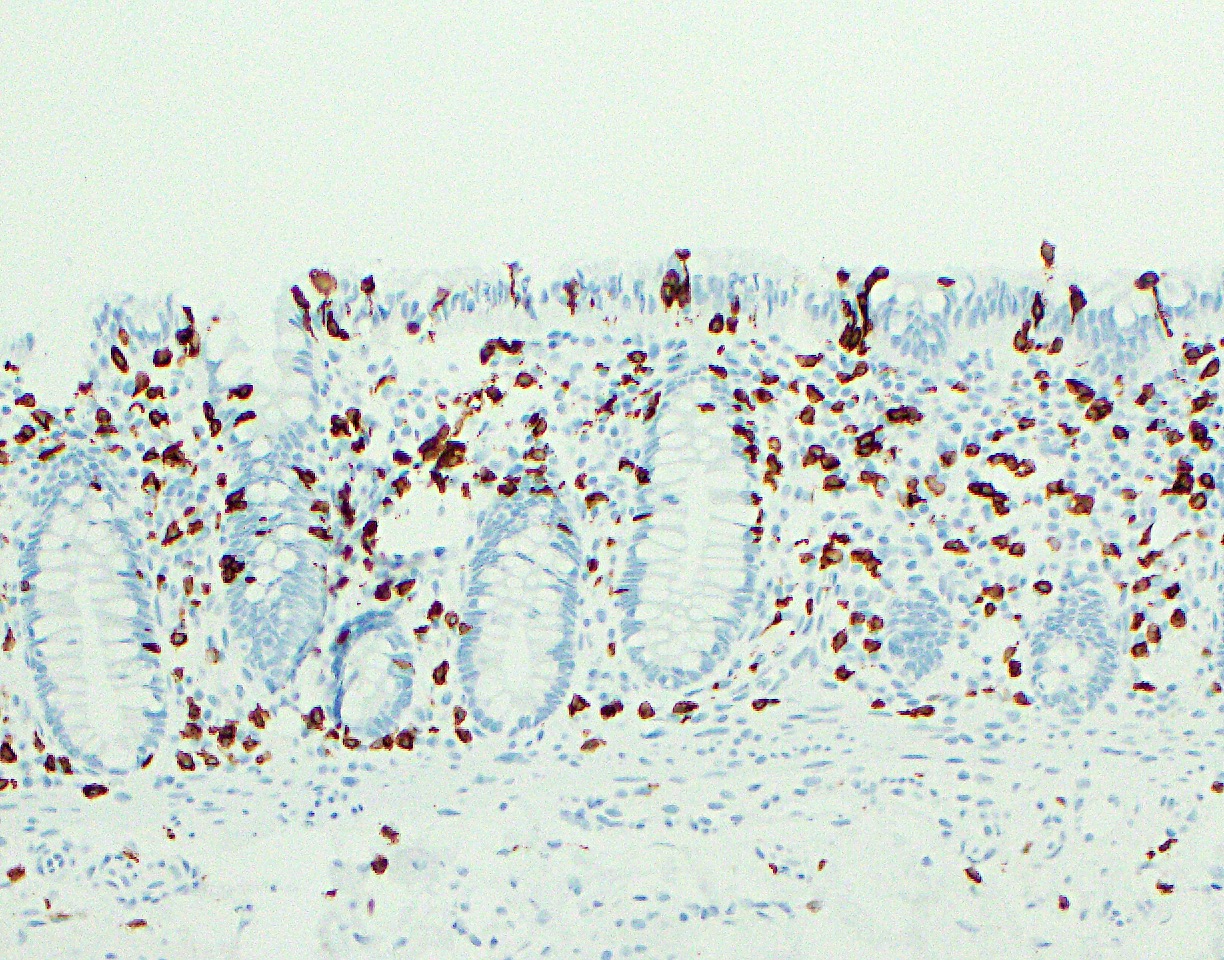
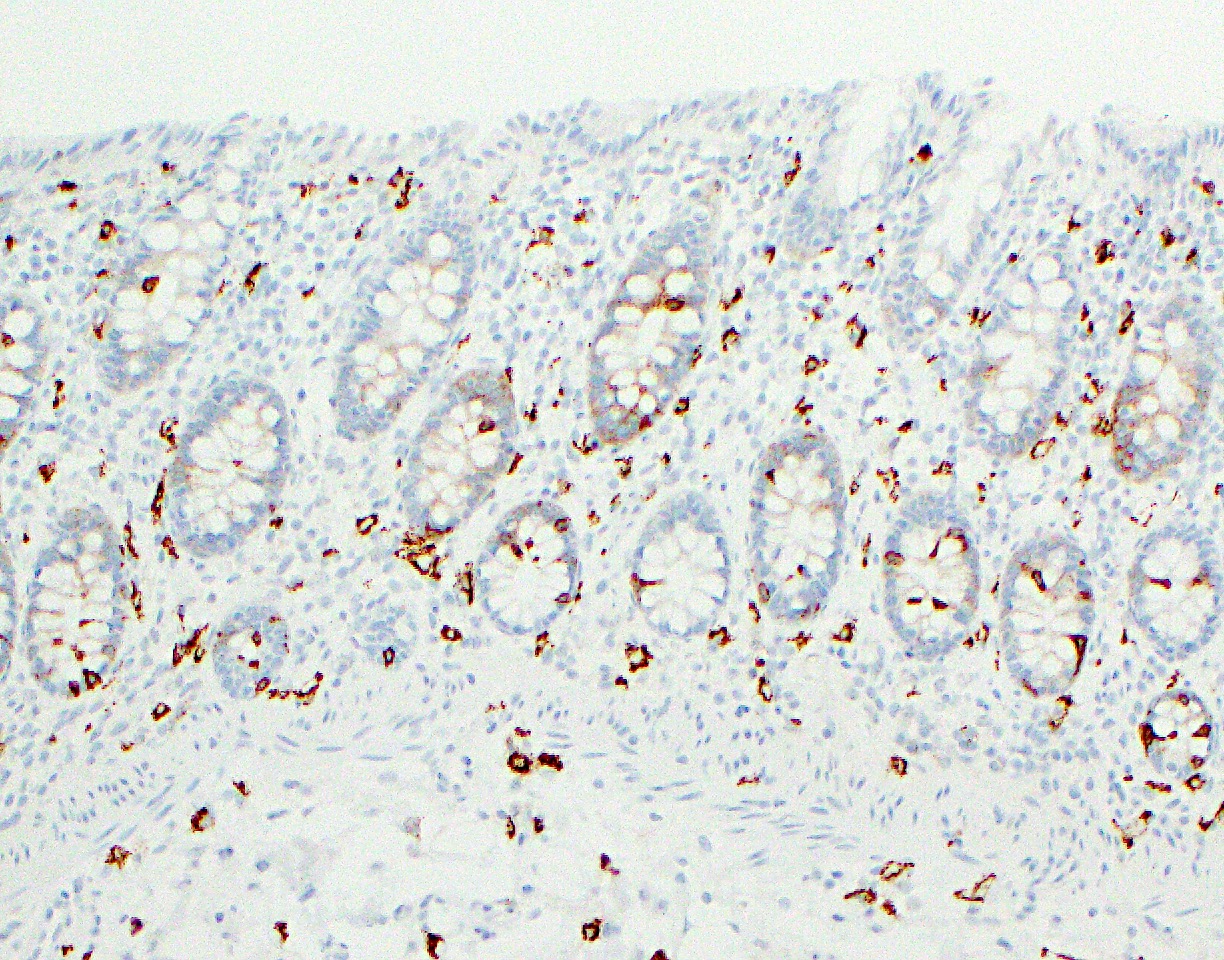
Positive stains
- Enterocytes (absorptive cells): pankeratin AE1 / AE3, CK20, CDX2, SATB2 and villin
- Goblet cells: MUC2, depending on their surface or crypt location in the mucosa; periodic acid Schiff (PAS), PAS diastase (PASD), mucicarmine and Alcian blue also stain the mucin in goblet cells (Histopathology 2000;37:561)
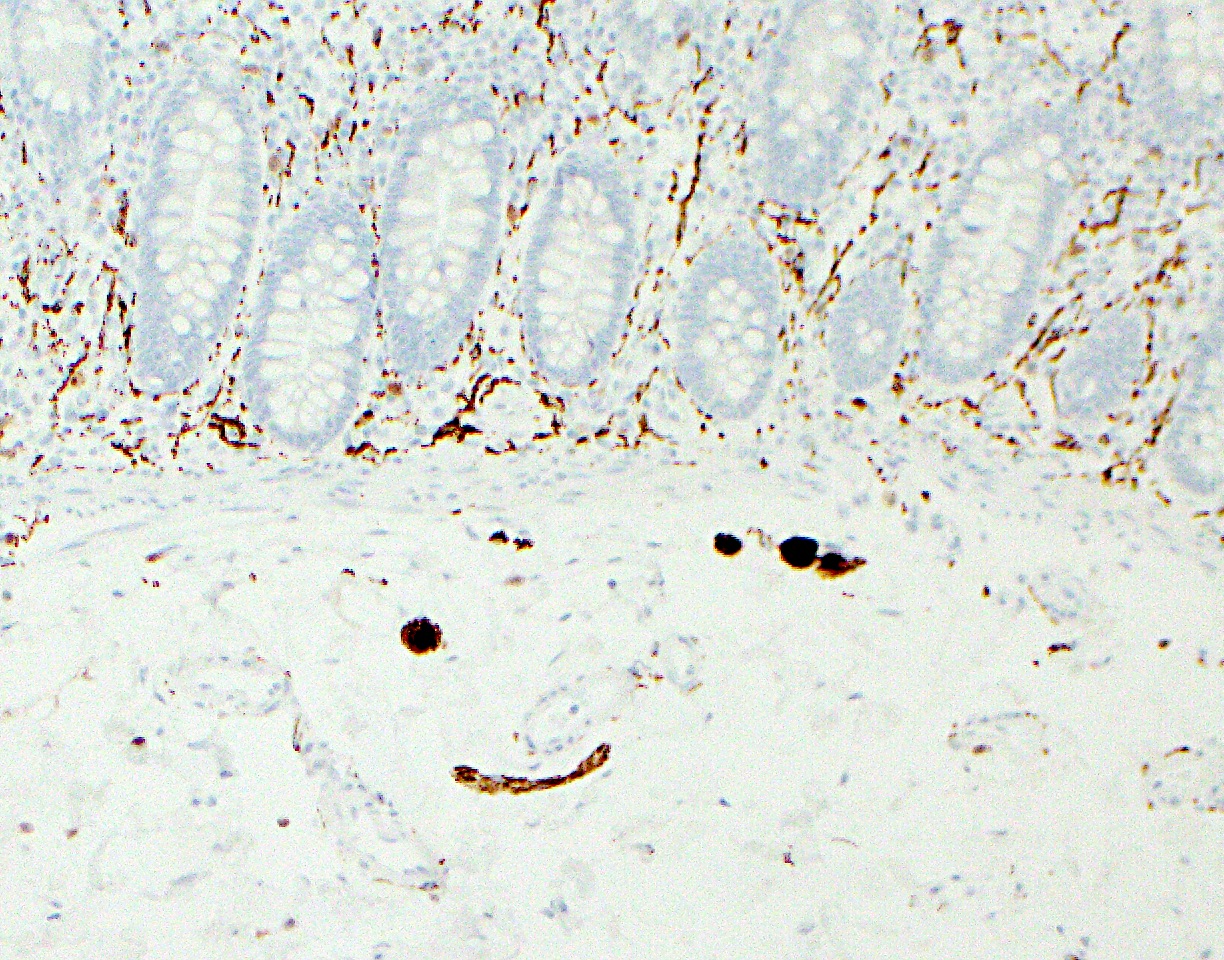
- Enteroendocrine cells: synaptophysin, chromogranin, neuron specific enolase (NSE) and pankeratin AE1 / AE3
- Paneth cells: AE1 / AE3
- Interstitial cells of Cajal: KIT
- Muscularis mucosae and propria: desmin, vimentin, SMA
- Ganglion cells: calretinin
- Enteric glial cells: S100, GFAP, synaptophysin, PDGFRA (R), neuron specific enolase (NSE)
- Inflammatory cells:
- Lamina propria T lymphocytes: CD3+ / CD4+
- Intraepithelial T lymphocytes: surface - CD3+ / CD8+ and TCRαβ+; near lymphoid follicles - CD3+ / CD45RO+ (Chem Immunol 1998;71:1)
- Lamina propria plasma cells: CD138, MUM1 and CD79a
- Macrophages: CD68, CD163, HAM56, MAC387, lysozyme and alpha-1 antitrypsin
- Mast cells: KIT, tryptase
Practice question #1
Practice answer #1
D. Paneth cells. They have a triangular shape with densely eosinophilic cytoplasmic granules and basally located nuclei, as opposed to enteroendocrine cells (see image above). Their presence in the left side of the colon can be a sign of inflammatory bowel disease.
Comment Here
Reference: Colon - Anatomy & histology
Comment Here
Reference: Colon - Anatomy & histology
Practice question #2
Which of the following parts of the colon is entirely intraperitoneal?
- Ascending colon
- Cecum
- Descending colon
- Rectum
Practice answer #2
B. Cecum. It is entirely intraperitoneal. The ascending and descending colon are retroperitoneal. Upper third of the rectum is covered by the peritoneum on the anterior surface.
Comment Here
Reference: Colon - Anatomy & histology
Comment Here
Reference: Colon - Anatomy & histology