Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Haroon S, Adnan HA. Stromal hyperplasia and hyperthecosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarynontumorhyperthecosis.html. Accessed August 25th, 2025.
Definition / general
- Ovarian stromal hyperplasia is a nonneoplastic functional disorder resulting in nodular or diffuse proliferation of ovarian stroma
- Hyperthecosis is characterized by proliferation of ovarian stroma along with luteinization of stromal cells (J Turk Ger Gynecol Assoc 2013;14:182)
Essential features
- Ovarian stromal hyperplasia and hyperthecosis are nonneoplastic conditions resulting in diffuse or nodular proliferation of ovarian stroma as single cells, clusters or nodules of luteinized cells
- Patients can present with bleeding due to endometrial pathology or symptoms of hyperandrogenism, principally androgenetic alopecia or hirsutism, along with elevated testosterone levels
- Both show an excess of androgen production leading to increased testosterone
- Ovaries with stromal hyperplasia and hyperthecosis secrete more androstenedione than normal ovaries that can be converted to estradiol by peripheral aromatization (BJOG 2003;110:690)
ICD coding
- ICD-11: 5A80.Y - other specified ovarian dysfunction
Epidemiology
- Generally encountered in postmenopausal women with an average age of 55 years (age range: 51 - 64 years) (J Menopausal Med 2020;26:39)
- Rare in women of reproductive age (< 1%) (Case Rep Obstet Gynecol 2023;2023:2783464)
Sites
- Ovarian stroma
Pathophysiology
- Studies have shown that ovaries with stromal hyperplasia and hyperthecosis secrete more androstenedione and estradiol than normal ovaries
- Most patients with stromal hyperplasia and hyperthecosis have normal gonadotrophin levels, unlike patients with polycystic ovary syndrome (Histopathology 1989;14:369)
- Some in vitro incubation studies show that stromal proliferation in premenopausal and postmenopausal women is increased by luteinizing hormone
- Luteinizing hormone also increases androgen production in ovaries with or without stromal hyperplasia (Am J Obstet Gynecol 1980;136:997, J Clin Endocrinol Metab 1992;74:172)
- Most patients with stromal hyperplasia and hyperthecosis show hyperinsulinemia or insulin resistance that likely plays a role in pathogenesis (Am J Obstet Gynecol 1986;154:384)
Etiology
- Etiology is not completely known (J Menopausal Med 2020;26:39)
- Some studies suggest genetic etiology (Medicina (Kaunas) 2023;59:1097)
- There may be an association with hyperandrogenism, insulin resistance and acanthosis nigricans (HAIR AN) syndrome
Clinical features
- Symptoms and signs of hyperandrogenism, such as deepening voice, acne, hirsutism, frontal alopecia, clitoromegaly
- Other features include obesity, hyperinsulinemia, acanthosis nigricans and metabolic syndrome
- There is an increased risk of vaginal bleeding, endometrial hyperplasia and carcinoma, cardiovascular pathology and diabetes mellitus (J Menopausal Med 2020;26:39)
- May be associated with HAIR AN syndrome in a few patients
Diagnosis
- Initial investigation is usually done to rule out adrenal tumors and androgen secreting ovarian tumors
- Clinical assessment for hirsutism, alopecia, deepening of voice, etc.
- Serological assessment: elevated testosterone, androgen and estrogen levels, normal or suppressed luteinizing hormone, normal dehydroepiandrosterone (DHEA), DHEA sulfate (DHEAS), 17 hydroxyprogesterone (17 OHP), normal progesterone and prolactin levels
- Imaging: enlarged ovaries without hypervascularization on imaging (J Menopausal Med 2020;26:39)
- Histology: the gold standard diagnostic test used for confirmation (and subsequent treatment) consists of histological investigation performed after bilateral salpingo-oophorectomy (J Menopausal Med 2020;26:39)
Laboratory
- Increased androgen, testosterone and estrogen levels
- Normal or suppressed LH and FSH
- Normal serum androstenedione or dehydroepiandrosterone sulfate (DHEAS) concentrations
- Unfavorable lipid profiles (i.e., increase in low density lipoprotein [LDL] and triglycerides, along with decrease in high density lipoprotein [HDL] associated with the hyperandrogenemia)
Radiology description
- Imaging: enlarged ovaries without hypervascularization on ultrasonography (J Menopausal Med 2020;26:39)
- In severe cases, bilateral expansion of ovarian stroma with more solid ovaries (J Turk Ger Gynecol Assoc 2013;14:182)
- Increased ovarian volume for the age group or nodules / cysts, however, unlike polycystic ovary syndrome, the number of follicles tends to be normal (Case Rep Obstet Gynecol 2023;2023:2783464)
- Magnetic resonance can show homogeneous T2 hypointensity and mild enhancement of the ovaries (Endocrinol Diabetes Metab Case Rep 2021;2021:20)
Prognostic factors
- Although it is a benign nonneoplastic condition, ovarian stromal hyperplasia / increased ovarian volume is believed to be associated with an increased risk of endometrial cancer; hence, malignancy should be excluded and patient should be treated to reduce the neoplastic risk (Ann Saudi Med 2012;32:588, Cancer Epidemiol Biomarkers Prev 2006;15:1550, Case Rep Obstet Gynecol 2023;2023:2783464)
Case reports
- 55 year old multiparous woman presented with bilateral ovarian hyperthecosis and endometrial intraepithelial neoplasia (EIN) (J Turk Ger Gynecol Assoc 2013;14:182)
- 62 year woman presented with bilateral ovarian stromal hyperplasia (Endocrinol Diabetes Metab Case Rep 2021;2021:20)
- 64 year old woman presented with serous cystadenoma and hyperthecosis (Case Rep Obstet Gynecol 2023;2023:2783464)
- 64 year old woman presented with virilizing symptoms and ovarian stromal hyperplasia (Postgrad Med J 1991;67:304)
Treatment
- Bilateral oophorectomy in postmenopausal women, however, if the patient has multiple comorbidities and is not fit for surgical option, then long term gonadotropin releasing hormone agonist treatment may be an option (J Turk Ger Gynecol Assoc 2013;14:182)
- In young females, long term gonadotropin releasing hormone agonist is an alternative to preserve fertility (Endocrinol Diabetes Metab Case Rep 2021;2021:20)
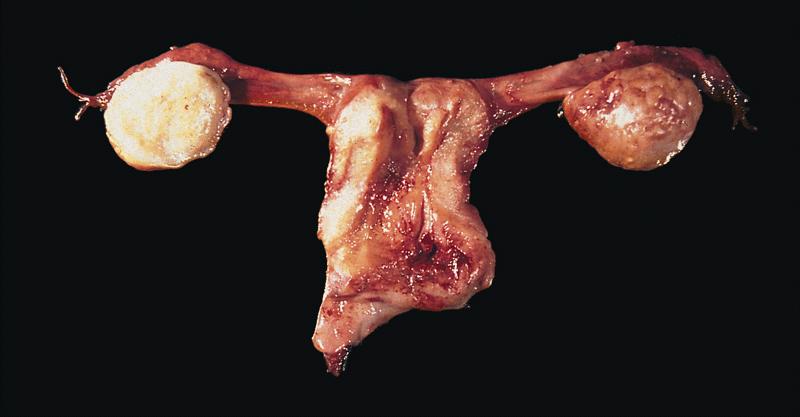
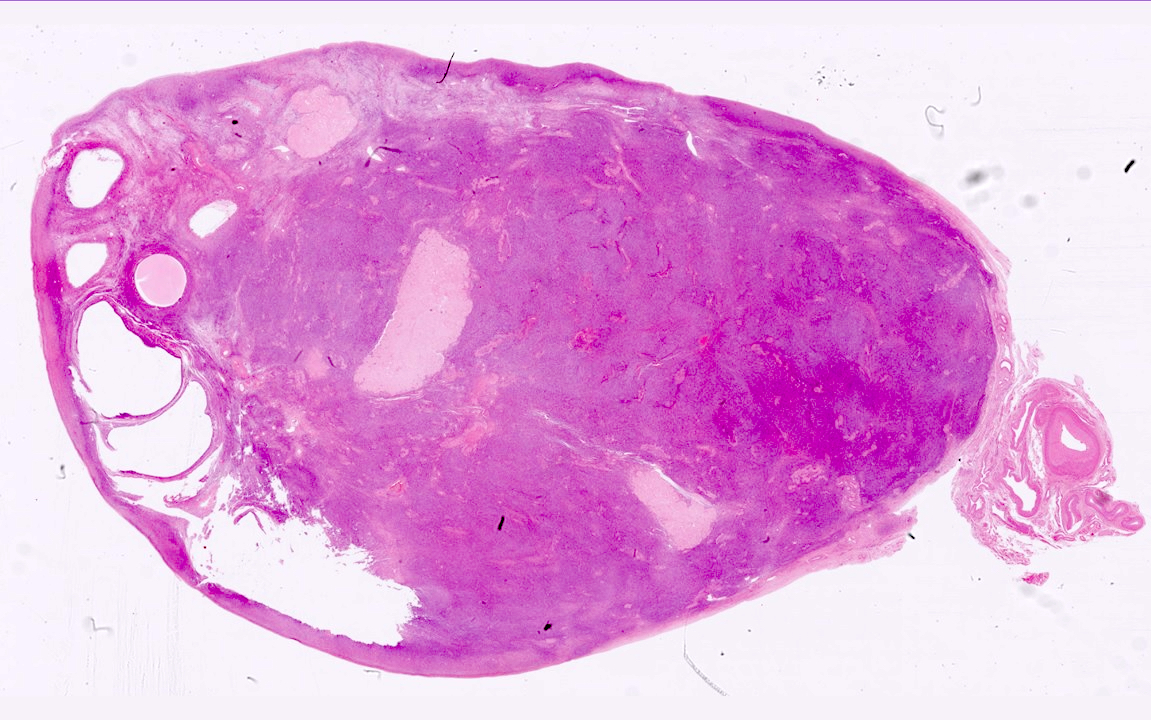
Gross description
- Mostly involves bilateral ovaries with increase in size
- May be nodular or diffuse with solid, firm, homogeneous white to yellow cut surface
Microscopic (histologic) description
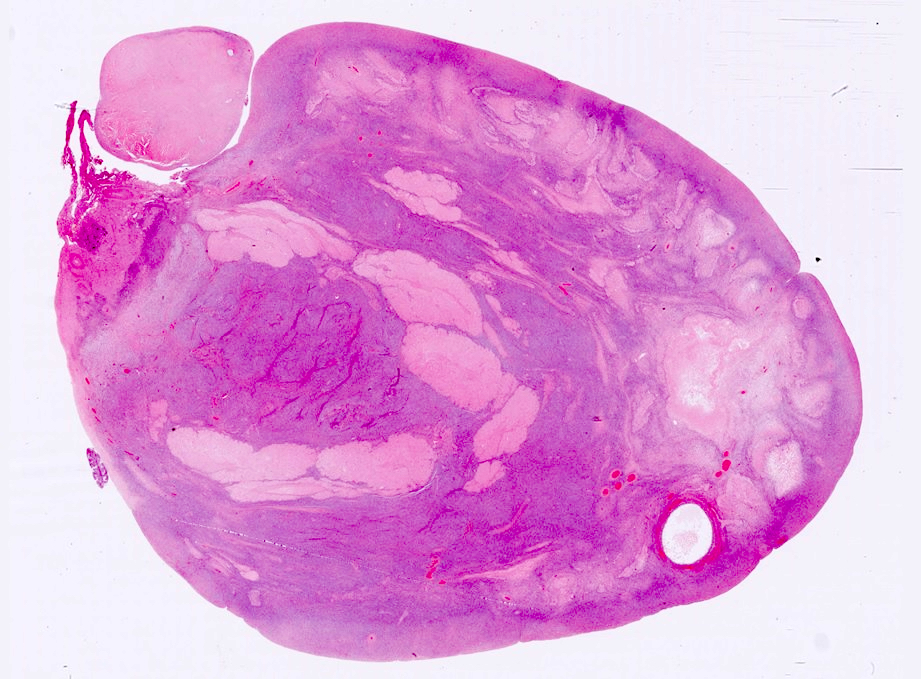
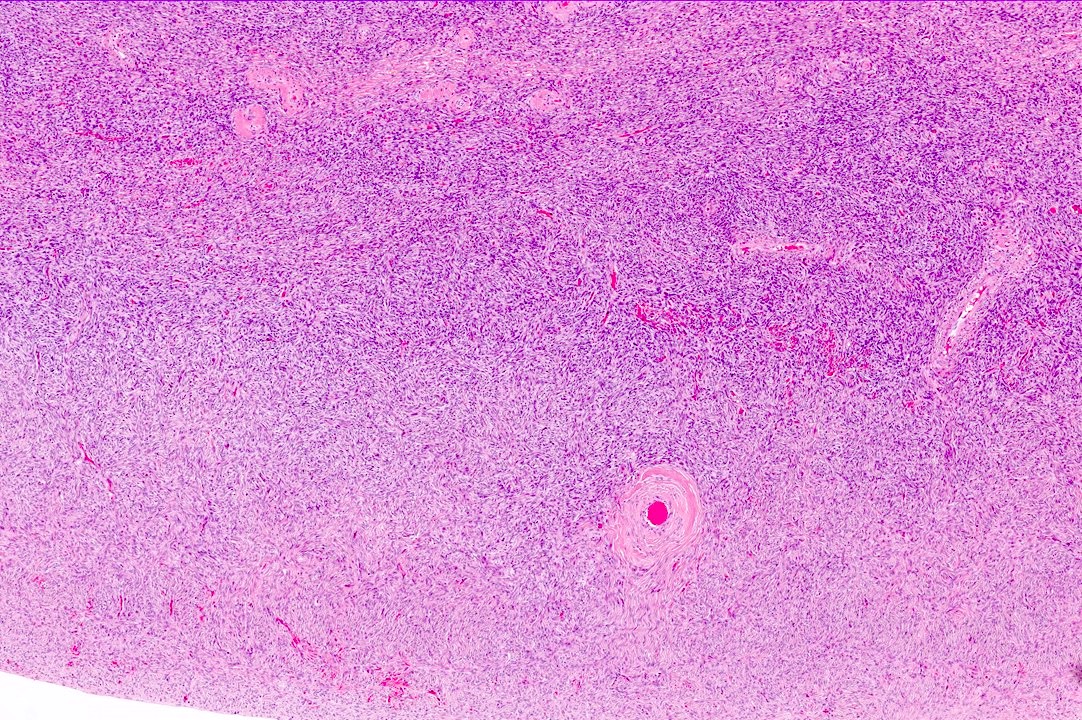
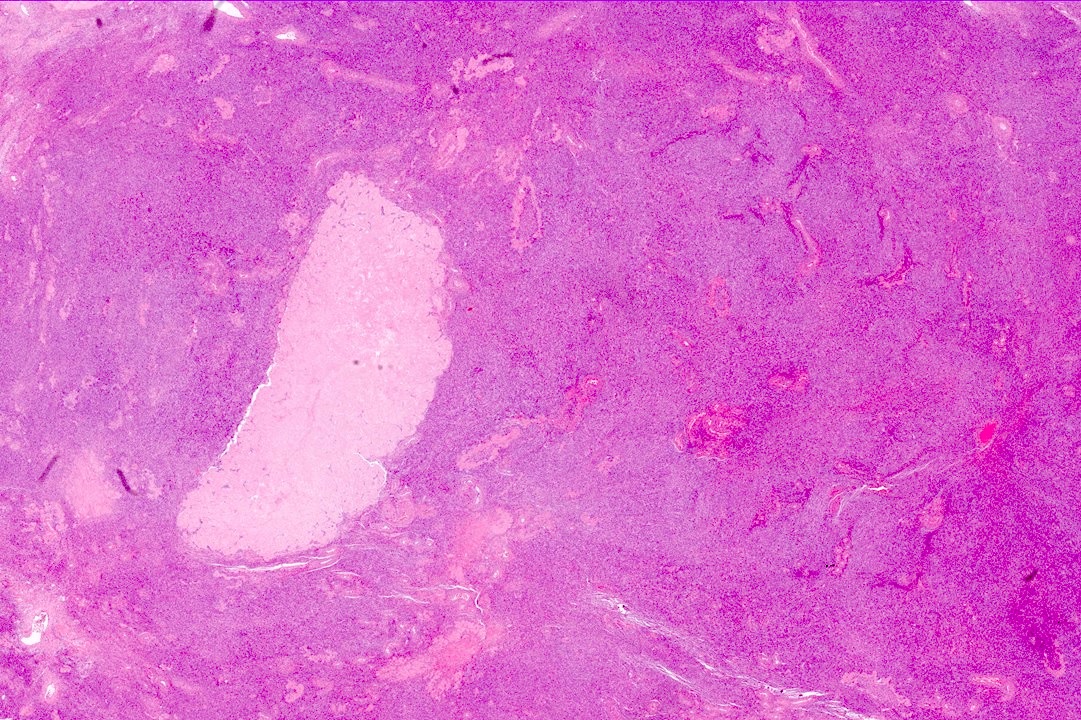
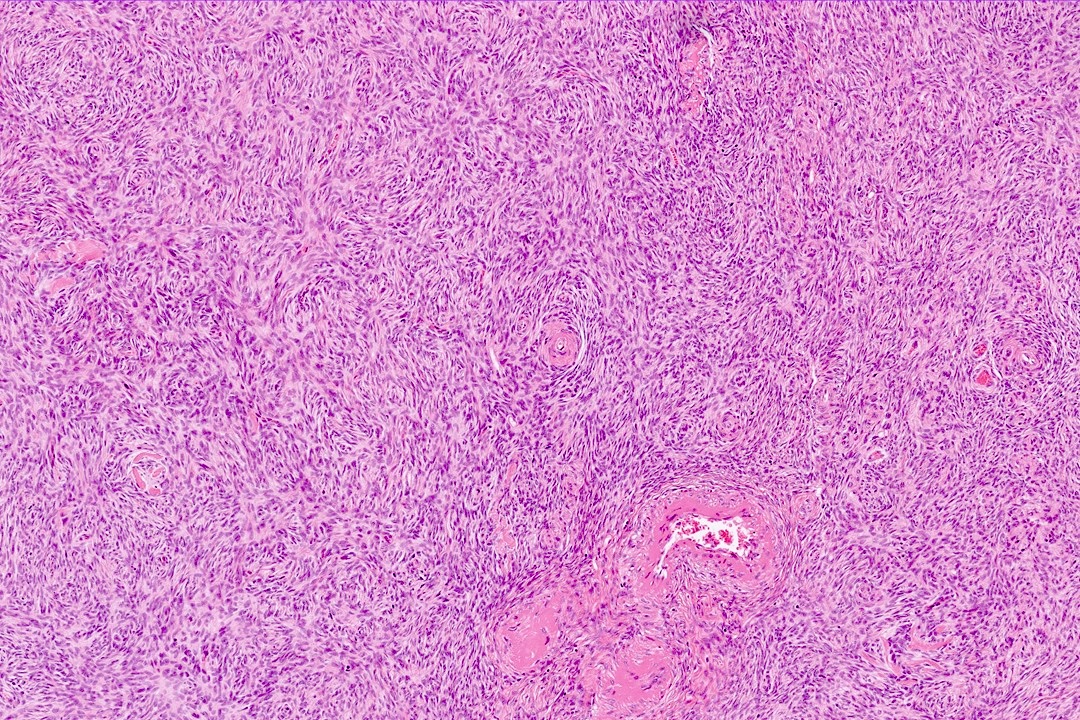
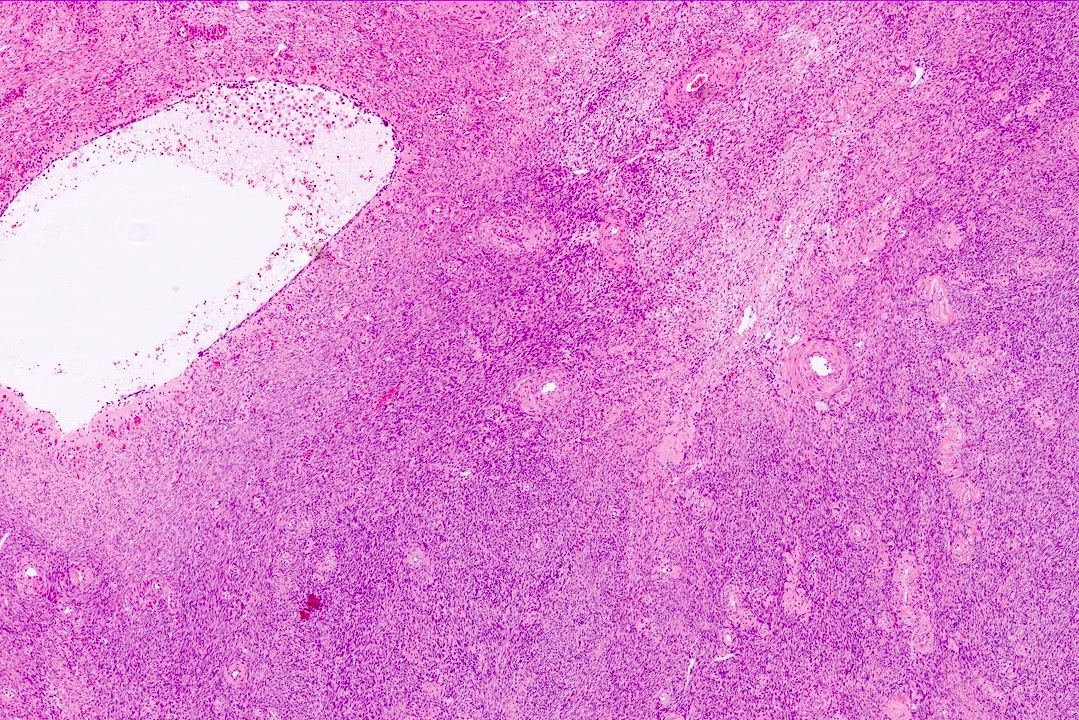
- Diffuse or nodular proliferation of ovarian stroma in cortex, medulla or both
- Stromal proliferation of spindle cells with scant intervening collagen
- May be diffuse or present as a nodule with coalescent nodules (Endocrinol Diabetes Metab Case Rep 2021;2021:20)
- Entrapped follicular derivatives may be present
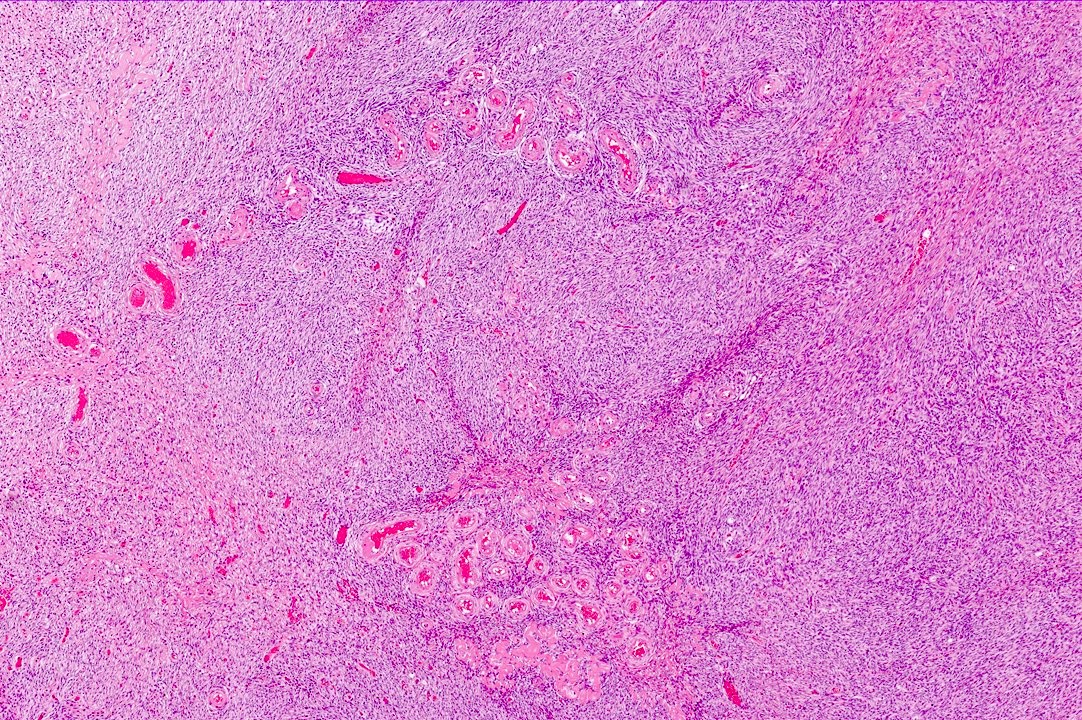
- In hyperthecosis, single cells, nests or nodules of polygonal luteinized theca cells with eosinophilic or clear cytoplasm < 1 cm are present
Microscopic (histologic) images
Positive stains
- WT1, ER, PR, CD56 in stromal cells (Am J Surg Pathol 2008;32:884)
- Inhibin and calretinin strongly positive in luteinized cells, negative or weakly positive in stromal cells
- FOXL2
Negative stains
- AE1 / AE3, EMA, cytokeratin MNF 116 and CD10
Sample pathology report
- Right ovary, oophorectomy:
- Ovarian stromal hyperplasia / hyperthecosis (see comment)
- Comment: This ovarian tissue shows expansion of ovarian stroma due to diffuse proliferation of stromal cells. In between these stromal cells, few clusters of eosinophilic luteinized cells are also present. No evidence of epithelial elements, increased mitosis, pleomorphism or necrosis is identified.
- Clinicopathological correlation: Correlation with serological markers and endometrial thickness is recommended as this condition is frequently associated with hyperandrogenism and endometrial hyperplasia.
Differential diagnosis
- Normal ovary:
- Normal appearance of cortex and medulla
- Cortex is the hypercellular outer zone having majority of follicles in premenopausal women; medulla is the hypocellular central area containing blood vessels and diffuse or nodular population of spindle cells
- Young women have thick cortex and contain follicles in various stages of development, while this is atrophied in old age and mainly contain corpus albicans
- Diagnosis of stromal hyperplasia and hyperthecosis is a subjective estimation of cortex and medullary cellularity with respect to age
- Fibroma:
- Mostly unilateral mass
- Usually well circumscribed and composed of variable cellular spindle to oval cells with scant cytoplasm, arranged as intersecting fascicles with intervening collagen; sometimes hyaline plaques are also present
- Cellular fibroma is densely cellular with little intervening collagen that may be mitotically active
- Steroid cell tumor, NOS:
- This tumor is comprised of expansile diffuse proliferation of large polygonal cells with eosinophilic, pale or vacuolated cytoplasm
- Steroid cells nodules > 1 cm arising in a background of stromal hyperthecosis are now best diagnosed as steroid cell tumor, NOS, as the previous diagnostic category of stromal luteoma is no longer recognized as a distinct entity
- Luteinized thecoma associated with sclerosing peritonitis:
- Extremely rare lesion, patient presents with abdominal swelling, ascites and bowel obstruction
- Almost always bilateral, ovaries have tan to red sectioned surface
- Microscopically, ovaries are hypercellular and show microcystic appearance due to edema
- Cells are predominantly spindled with minority component of small luteinized cells
- SF1 and FOXL2 are positive in spindle cells while calretinin and inhibin are positive in luteinized cells
- Sex cord stromal tumor, NOS:
- Both sex cord and stromal components are present
- Stromal component highlighted by reticulin staining
- Pregnancy luteoma:
- Associated with pregnancy
- Comprised of oval to round uniform cells with abundant eosinophilic cytoplasm
- Massive ovarian edema and fibromatosis:
- Prominent edema of stroma sparing cortex
- Clusters of luteinized cells may be present
- Krukenberg tumor:
- Isolated atypical cells with signet ring cell morphology in ovarian stroma
- AE1 / AE3 positive
- Low grade endometrial stromal sarcoma:
- Oval to spindle cells with minimal atypia and associated arterioles
- CD10 positive
Additional references
Practice question #1
A specimen for bilateral oophorectomy is received with enlarged ovaries. One ovary measures 44 x 30 x 25 mm while the second measures 35 x 30 x 25 mm. Sectioning shows homogeneous solid areas with a single 3 mm cyst. Microscopy shows a diffuse population of spindle cells with no pleomorphism, mitosis or necrosis. What is the likely diagnosis?
- Adult granulosa cell tumor
- Fibroma
- Metastatic tumor
- Sex cord stromal tumor, NOS
- Stromal hyperplasia
Practice answer #1
E. Stromal hyperplasia. There is a homogeneous population of spindle cells with no atypia. Answer A is incorrect because adult granulosa cell tumor will show atypia with variable patterns and nuclear grooving. Answer B is incorrect because no hyalinized areas with intersecting fascicles are present. Answer C is incorrect because no epithelial elements are present in this tumor. Answer D is incorrect because no sex cord-like areas or biphasic cell populations are identified.
Comment Here
Reference: Stromal hyperplasia and hyperthecosis
Comment Here
Reference: Stromal hyperplasia and hyperthecosis
Practice question #2
A 57 year old woman presents with postmenopausal bleeding. Endometrial biopsy shows FIGO grade 1 endometrioid type endometrial cancer and hysterectomy reveals stage IA endometrioid type endometrial carcinoma with enlarged bilateral ovaries. Microscopic findings are shown in the image above. What is the diagnosis?
- Fibroma
- Leydig cell tumor
- Metastatic endometrioid type endometrial cancer
- Sex cord stromal tumor
- Stromal hyperplasia and hyperthecosis
Practice answer #2
E. Stromal hyperplasia and hyperthecosis. Clusters of luteinized cells are present in stromal hyperplasia. Answer A is incorrect because no hyalinized areas with intersecting fascicles are present. Answer B is incorrect because no Leydig cell population is identified and the cells do not contain Reinke crystals. Answer C is incorrect because no epithelial elements are identified. Answer D is incorrect because no tumor-like mass or epithelial elements are identified.
Comment Here
Reference: Stromal hyperplasia and hyperthecosis
Comment Here
Reference: Stromal hyperplasia and hyperthecosis