Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Anderson D, Tretiakova M. Lymphoepithelioma-like. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderlymphoepithel.html. Accessed April 30th, 2024.
Definition / general
- Rare subtype of urothelial carcinoma that occurs throughout the urinary tract
- Resembles nonkeratinizing nasopharyngeal carcinoma, undifferentiated subtype (previously known as lymphoepithelioma) or occasionally oropharyngeal carcinoma but is EBV and HPV negative (Int J Urol 2007;14:1093, Mod Pathol 2006;19:494, Am J Surg Pathol 2011;35:474)
Essential features
- Subtype of invasive urothelial carcinoma that resembles lymphoepithelioma
- Composed of sheets of undifferentiated, pleomorphic carcinoma cells with syncytial appearance, admixed with polymorphic inflammatory infiltrate
Terminology
- Also called lymphoepithelial carcinoma but most authors prefer -like in the name (i.e., lymphoepithelioma-like urothelial carcinoma) since it is EBV negative, in contrast to the nasopharyngeal tumor
ICD coding
- ICD-O: 8082/3 - lymphoepithelioma-like carcinoma
- ICD-10:
- C67 - malignant neoplasm of bladder
- C67.0 - malignant neoplasm of trigone of bladder
- C67.1 - malignant neoplasm of dome of bladder
- C67.2 - malignant neoplasm of lateral wall of bladder
- C67.3 - malignant neoplasm of anterior wall of bladder
- C67.4 - malignant neoplasm of posterior wall of bladder
- C67.5 - malignant neoplasm of bladder neck
- C67.6 - malignant neoplasm of ureteric orifice
- C67.7 - malignant neoplasm of urachus
- C67.8 - malignant neoplasm of overlapping sites of bladder
- C67.9 - malignant neoplasm of bladder, unspecified
- C66.1 - malignant neoplasm of right ureter
- C66.2 - malignant neoplasm of left ureter
- C65.1 - malignant neoplasm of right renal pelvis
- C65.2 - malignant neoplasm of left renal pelvis
- C67 - malignant neoplasm of bladder
- ICD-11:
- 2C91.0 & XH8EH1 - urothelial carcinoma of renal pelvis & transitional cell carcinoma, NOS
- 2C92.0 & XH8EH1 - urothelial carcinoma of ureter & transitional cell carcinoma, NOS
- 2C94.2 & XH8EH1 - urothelial carcinoma of bladder & transitional cell carcinoma, NOS
- 2C93.2 & XH8EH1 - urothelial carcinoma of urethra or paraurethral gland & transitional cell carcinoma, NOS
- 2C95.2 & XH8EH1 - urothelial carcinoma involving overlapping sites of urinary organs & transitional cell carcinoma, NOS
- Note: transitional is a term that is no longer recommended; ICD-11 will be updated
Epidemiology
- M:F = 2.8:1; occurs in late adulthood, mean age of 70 years (range: 54 - 84 years) (Am J Surg Pathol 2011;35:474)
- Rare subtype, first reported in 1991 in the bladder
- Estimated incidence is 0.4 to 1.3% of all bladder carcinomas but has also been described in upper ureter and renal pelvis (Can Urol Assoc J 2013;7:E590)
- In renal pelvis, virtually all reported cases from patients 65 and older
Sites
- Urinary tract
- Has been described in the bladder, ureter, renal pelvis and urethra
Etiology
- Derived from urothelium
- May have similar pathogenesis as high grade invasive urothelial carcinoma (Am J Surg Pathol 2011;35:474)
- Not associated with Epstein-Barr virus (EBV) (Urology 2005;66:1109)
- Not associated with HPV
Clinical features
- Painless hematuria (Nat Clin Pract Urol 2007;4:167)
- Commonly presents with advanced stage (pT2 or higher) (Can Urol Assoc J 2013;7:E590)
Diagnosis
- Diagnosis is made in a similar fashion to conventional urothelial carcinoma with cystoscopy and biopsy or TURBT of the lesion
- Essentially an H&E diagnosis with demonstration of characteristic findings of pleomorphic cells with syncytial growth and associated inflammatory infiltrate
Radiology description
- Tumors are seen filling gaps within the urinary bladder, commonly with a broader base compared to transitional urothelial carcinomas (Cureus 2022;14:e21281)
- May show enhancing soft tissue mass in the renal pelvis or ureter, involvement of the renal parenchyma or hilar fat when in the upper urinary tract
Prognostic factors
- Some authors report a more favorable prognosis and better response to systemic chemotherapy when pure or predominant (> 50%) (J Urol 1998;159:503, Histopathology 2001;39:106, Urology 2005;66:1109, Mod Pathol 1998;11:1252, Int J Urol 2007;14:1093, BMC Res Notes 2014;7:779, Am J Surg Pathol 2011;35:474, Mod Pathol 2007;20:828, Am J Surg Pathol 1994;18:466, BMC Urol 2017;17:34)
- When there is focal lymphoepithelioma-like carcinoma present, the behavior is similar to conventional urothelial carcinoma of the same grade and stage (Am J Surg Pathol 2011;35:474)
- Other authors contend that lymphoepithelioma-like carcinoma, whether in pure or mixed form, has a similar prognosis to ordinary urothelial carcinoma when treated by cystectomy (Mod Pathol 2007;20:828)
- Survival analysis showed no differences compared with conventional upper urinary tract urothelial carcinoma; pT classification was determined to be the only significant prognostic parameter (Virchows Arch 2017;470:703)
Case reports
- 65 year old woman with lymphoepithelioma-like carcinoma and squamous component in renal pelvis (Korean J Pathol 2014;48:458)
- 67 year old woman with lower pole renal pelvis tumor infiltrating the perirenal hilar fat (J Urol 2002;167:2127)
- 69 year old woman with lymphoepithelioma-like carcinoma of right lateral wall, trigone of the bladder and ureteral orifice (BMC Urol 2017;17:34)
- 71 year old man with primary tumor of ureter (Ann Diagn Pathol 2010;14:209)
- 72 year old man with predominant lymphoepithelioma-like carcinoma of bladder treated with bacillus Calmette-Guerin and transurethral resection of bladder tumor (Acta Biomed 2021;92:e2021031)
- 74 year old woman with urinary bladder tumor (Arch Pathol Lab Med 2001;125:1383)
- 75 year old woman with ulcerated mass of ureter (Case #267)
- 75 year old women with lymphoepithelioma-like carcinoma in renal pelvis (Can Urol Assoc J 2013;7:E590, Int J Urol 2007;14:851)
- 93 year old woman with lymphoepithelioma-like carcinoma of bladder (Cureus 2022;14:e21281)
Treatment
- No clear treatment guidelines different than conventional urothelial carcinoma
- One study suggests that a combination therapy including radical cystectomy could possibly yield the best outcome of disease free survival (BMC Urol 2017;17:34)
- The impact of neoadjuvant chemotherapy, per the authors, is yet undetermined
- Transurethral resection of bladder tumor alone was associated with both the lowest disease free survival and highest mortality rate
- Conservative treatment should be considered only in cases of pure or predominant lymphoepithelioma-like carcinoma; 5 patients in one study who had pure or predominant lymphoepithelioma-like carcinoma (> 50%) and were treated with transurethral resection followed by chemotherapy were alive without evidence of disease at 2 - 5 years (Am J Surg Pathol 2011;35:474)
- High degree of PDL1 expression could indicate potential for immunotherapy (Mod Pathol 2007;20:828, Am J Surg Pathol 2011;35:474, Virchows Arch 2017;470:703, Transl Androl Urol 2021;10:1521, Am J Pathol 2020;190:134)
Gross description
- In bladder, usually in dome, posterior wall or trigone
Microscopic (histologic) description
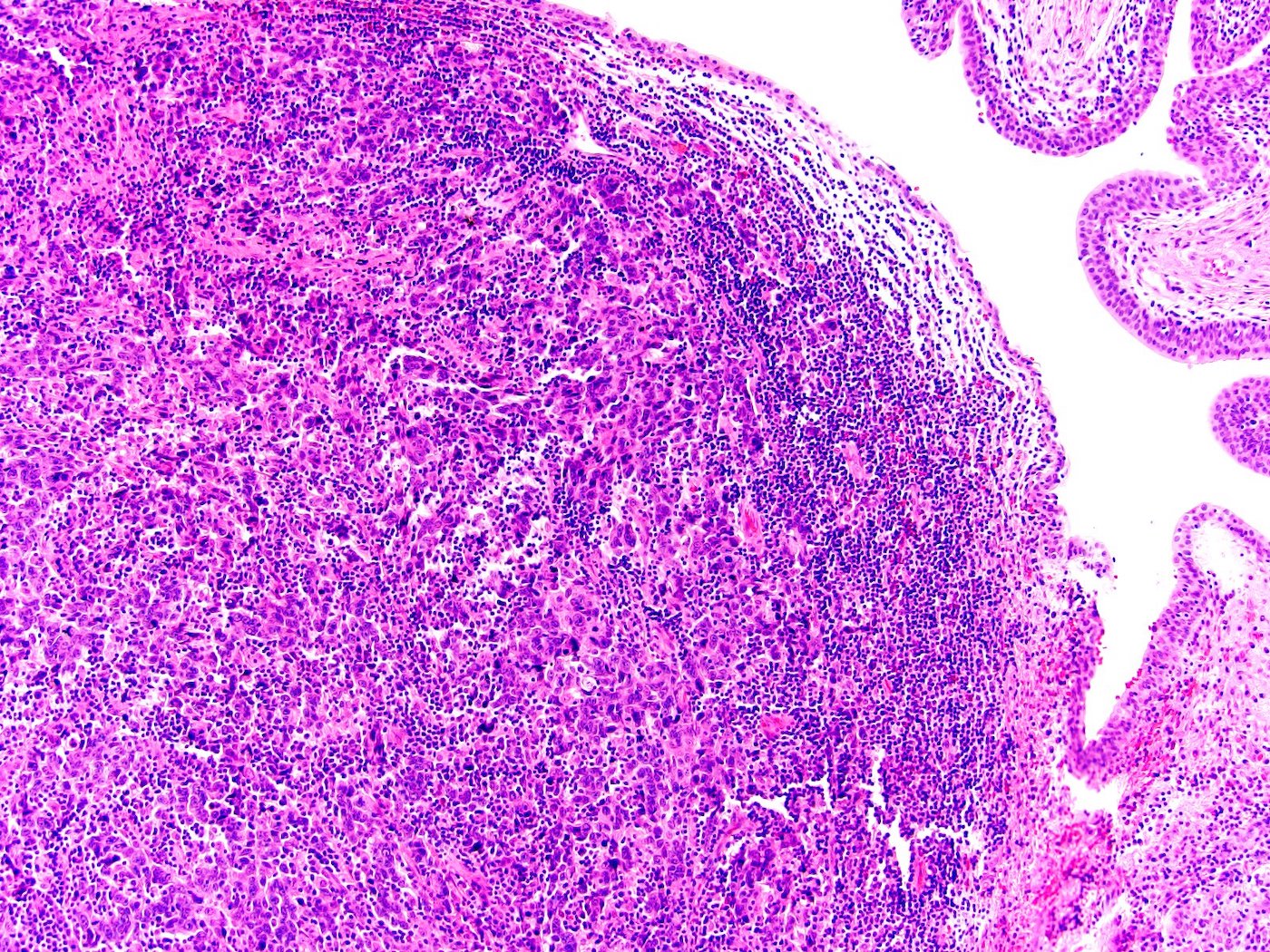
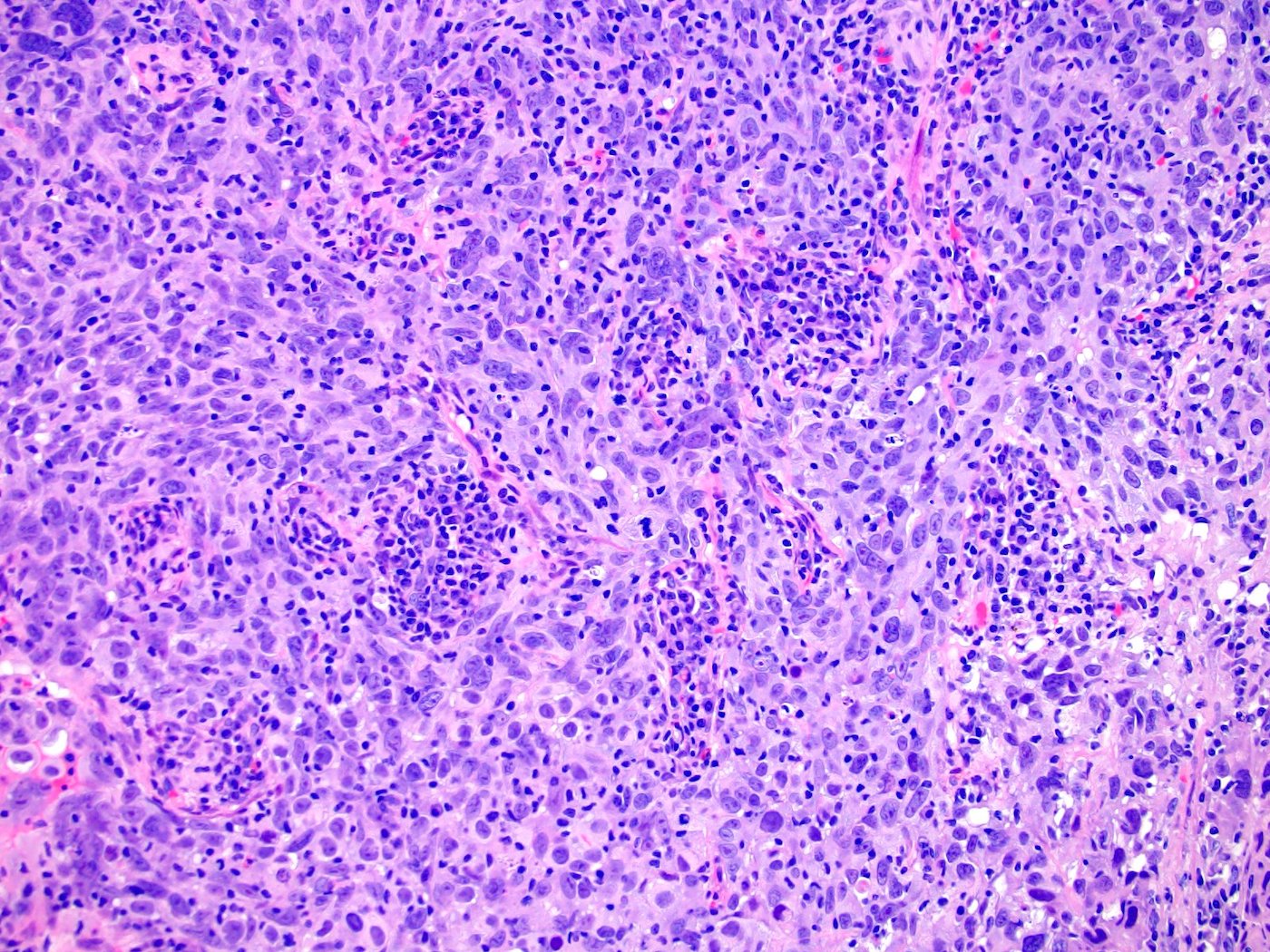
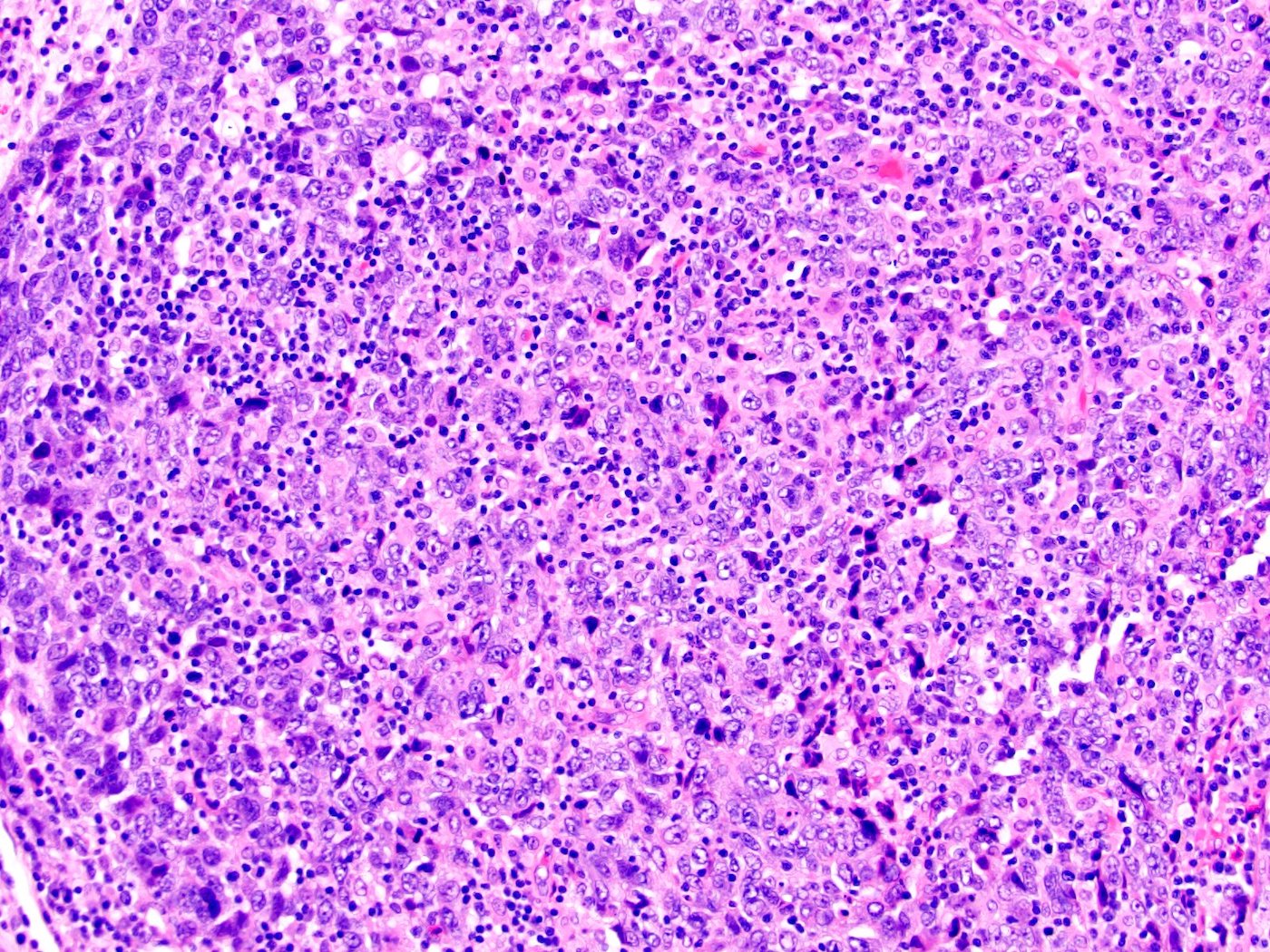
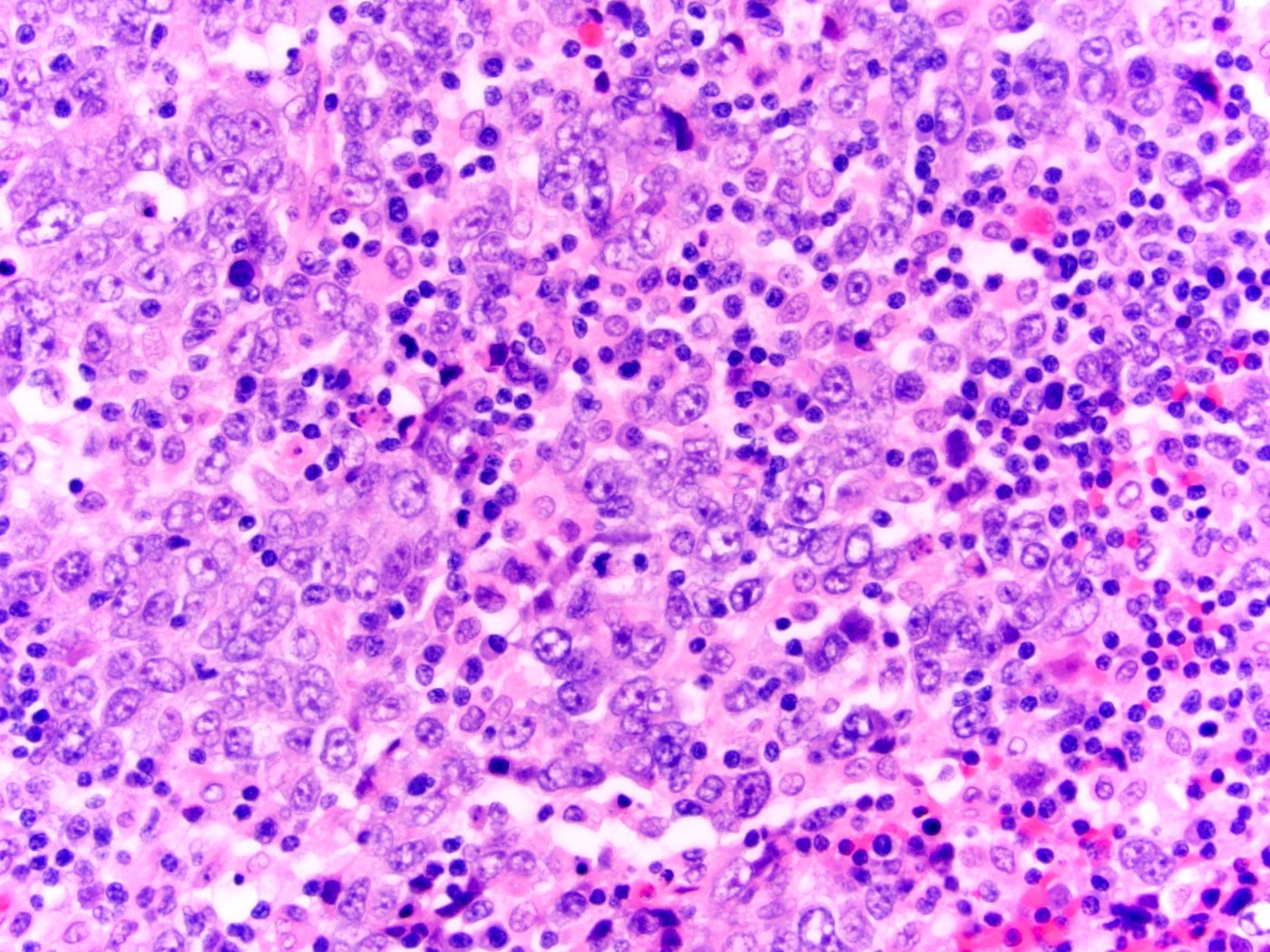
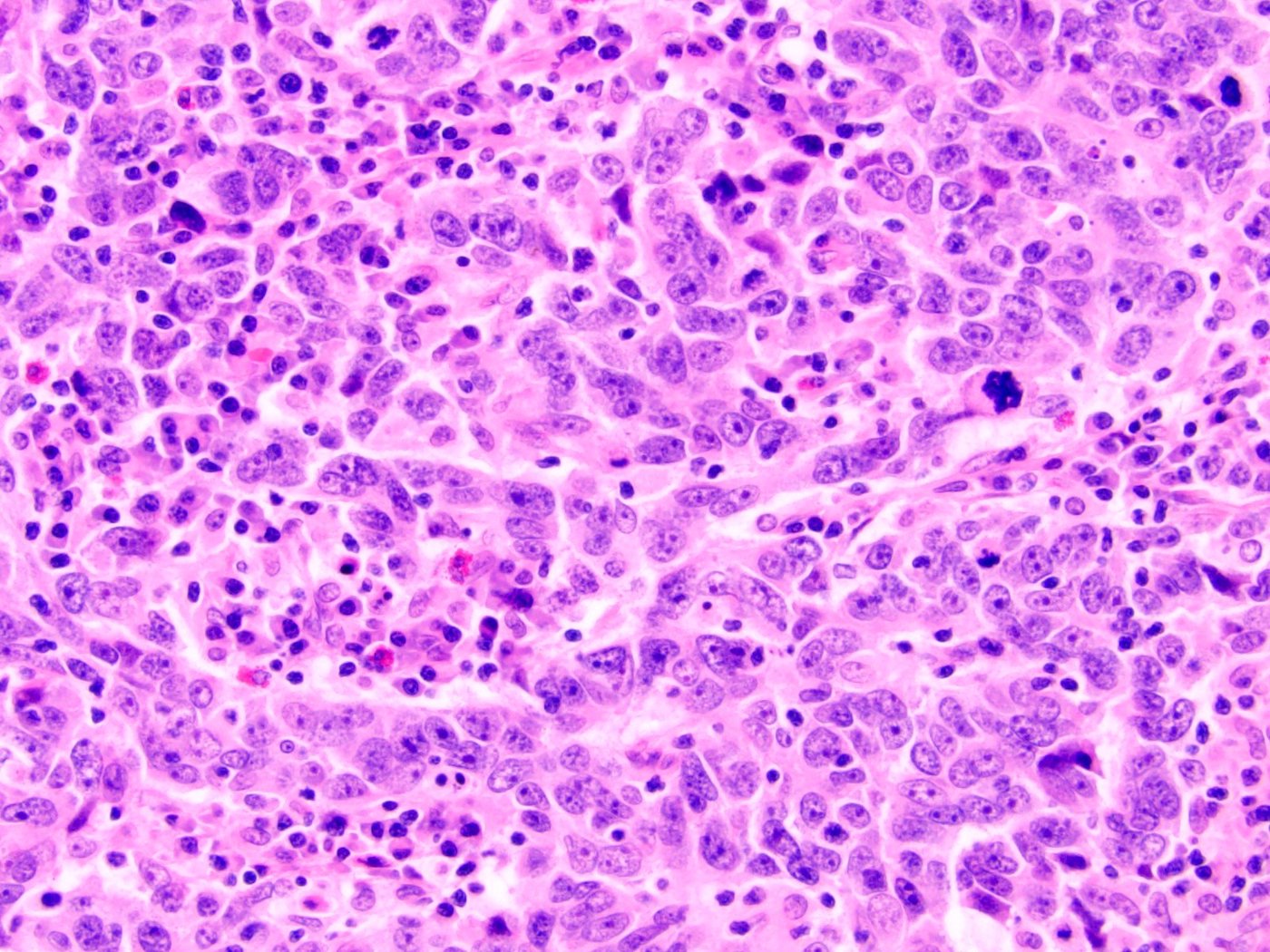
- Large pleomorphic nuclei with prominent nucleoli, ill defined borders and frequent mitosis
- Arranged in syncytial sheets, nests or individual cells with abundant mixed inflammatory cells that often obscure the neoplastic cells (Am J Surg Pathol 1994;18:466)
- Nonneoplastic cells are a mixture of polyclonal B and T lymphocytes, histiocytes, eosinophils, plasma cells and occasional neutrophils or eosinophils that invade the epithelial nests; T cells usually predominate (Histopathology 2019;74:77)
- May be pure or mixed, either predominant or focal; if mixed, consider recording proportion of subtype (Int J Clin Exp Pathol 2009;2:194)
- May be admixed with conventional urothelial carcinoma, urothelial carcinoma with squamous differentiation, glandular differentiation or sarcomatoid components (Am J Surg Pathol 2011;35:474)
- Surface urothelium may demonstrate concurrent carcinoma in situ (CIS), up to 50% of cases in one report or papillary urothelial carcinoma (Am J Surg Pathol 2011;35:474)
Microscopic (histologic) images
Cytology description
- Large atypical, undifferentiated tumor cells, oftentimes in clusters, with high N:C ratio, vesicular chromatin and prominent nucleoli; may be seen singly or in mixture with inflammatory cells
- May be impossible to differentiate from conventional urothelial carcinoma on cytology alone; a diagnosis of this subtype in urine should be rendered with caution and should always be confirmed by the histologic examination of tissue biopsy
- Reference: Diagn Cytopathol 2008;36:600
Positive stains
- Epithelial cells
- Cytokeratin markers: 34betaE12 / HMWCK / high molecular weight keratin, CK7, AE1 / AE3, EMA, CK8 (Am J Surg Pathol 2011;35:474)
- Urothelial markers: GATA3, p63, p40
- Rare cells with CK5/6 (Virchows Arch 2017;470:703, Am J Surg Pathol 2011;35:474)
- p53 expression (> 10% of cells) in a subset (61%) of tumors and subset of cases showed abnormal suprabasal p53 in adjacent carcinoma in situ (Am J Surg Pathol 2011;35:474)
- Lymphocytes
- Predominately polymorphic T and B cell markers
Negative stains
- CD45 / LCA (stains lymphocytes, not epithelial cells)
- Vimentin, EBV, HPV, TTF1, CD30, AMACR, CDX2, synaptophysin, CD138, CD68 (Virchows Arch 2017;470:703, Am J Surg Pathol 2011;35:474, Mol Oncol 2022;16:3666)
- AMACR (P504S) showed focal positivity in 1 - 5% of carcinoma cells for 18% of cases but predominantly negative (Am J Surg Pathol 2011;35:474)
- CK20 rare to negative (Am J Surg Pathol 2011;35:474)
Molecular / cytogenetics description
- Lymphoepithelioma-like carcinoma of the bladder showed basal-like molecular phenotype by RNA expression profiling with PDL1 IHC positive in 93% of cases; no evidence for loss of MMR
- By UroVysion FISH gains of chromosome 3 were most common (76%), followed by gain of chromosome 17, 9p21 abnormality and gain of chromosome 7
- In cases with other histologic subtypes, squamous, urothelial, sarcomatoid and glandular components showed patterns of gain / loss that were identical to those of the lymphoepithelioma-like carcinoma component (Histopathology 2019;74:77, Am J Pathol 2020;190:134, Am J Surg Pathol 2011;35:474)
- Whole genome sequencing study of lymphoepithelioma-like carcinoma of the renal pelvis showed mutations in susceptibility gene (KDM6A) and driver gene (LEPR) (Mol Oncol 2022;16:3666)
Sample pathology report
- Bladder and prostate, cystoprostatectomy:
- Invasive urothelial carcinoma (3.2 cm), lymphoepithelioma-like subtype (100%); the carcinoma invades muscularis propria (detrusor muscle), margins are negative (see comment and synoptic reports)
- Prostatic adenocarcinoma, Gleason score 3 + 4 = 7 (grade group 2), 5 - 10% Gleason pattern 4; organ confined, margins are negative
- 6 lymph nodes, negative for tumor
- Therapy related changes including foreign body giant cell reaction and scar
- Comment: Lymphoepithelioma-like urothelial carcinoma is a rare subtype of urothelial carcinoma composed of syncytial sheets and clusters of pleomorphic cells with associated inflammatory infiltrate. The tumor has morphologic similarities to lymphoepithelioma of the nasopharynx but differs due to lack of association with EBV infection. Some authors have suggested a better overall survival in patients with pure or predominant (> 50%) lymphoepithelioma-like urothelial carcinoma than conventional urothelial carcinoma. A recent study showed that these tumors are enriched for basal squamous molecular subtype markers and for PDL1 expression, consistent with the known sensitivity for chemotherapy and possibly indicating a potential use for immune checkpoint inhibitors as a therapeutic option.
Differential diagnosis
- Florid chronic cystitis:
- No malignant epithelial component
- Cytokeratin negative
- Differential diagnosis can be challenging on crushed or limited biopsy; epithelial cells in lymphoepithelioma-like urothelial carcinoma can be difficult to identify
- Metastases from other site:
- Lack of urothelial immunohistochemical markers
- Clinical, radiologic correlation
- Lymphoma:
- No syncytial cohesive clusters of malignant epithelial cells
- Cytokeratin and urothelial marker negative
- Lymphocytes are clonal and LCA positive
- Usually lacks overlying carcinoma in situ or usual urothelial component
- Small cell neuroendocrine carcinoma:
- Molding or crush artifact, no prominent nucleoli and usually no prominent lymphocytic component
- Squamous cell carcinoma, poorly differentiated:
- Pure squamous lesion with no in situ or invasive urothelial component
- Urothelial carcinoma with prominent lymphoid stroma:
- Lacks syncytial growth pattern and typical cytology
- Xanthogranulomatous pyelonephritis and other inflammatory lesions:
- Foamy histiocytes
- Cytokeratin negative
Additional references
Board review style question #1
A 65 year old man presents with hematuria and is discovered to have a 3 cm urinary bladder mass located in the dome. Histological examination on transurethral resection of bladder tumor shows a brisk, predominately lymphocytic, inflammatory infiltrate with sheets / nests of large epithelial cells displaying syncytial growth (see photomicrograph above). The epithelial cells are positive for high molecular cytokeratins and GATA3. No other components are identified. Which of the following statements is true about this carcinoma subtype in its pure form?
- Always expresses both CK7 and CK20
- Associated with EBV infection and often positive for EBV ISH
- Low to no PDL1 expression
- Poorer prognosis and less responsive to chemotherapy than conventional urothelial carcinoma
- Shows a basal type molecular phenotype
Board review style answer #1
E. Shows a basal type molecular phenotype. Lymphoepithelioma-like carcinoma of the bladder shows a basal type molecular profile. Some authors contend this subtype has a more favorable prognosis and is more responsive to chemotherapy when pure or predominant than compared to conventional urothelial carcinoma. Recent studies show a high degree of PDL1 expression, which could indicate a potential target for immunotherapy. The carcinoma cells express high molecular weight keratins, CK7, 34BE12, p63, GATA3 and are mostly negative for CK20. This carcinoma is not associated with EBV infection.
Comment Here
Reference: Lymphoepithelioma-like carcinoma
Comment Here
Reference: Lymphoepithelioma-like carcinoma