Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Lahoutiharahdashti AH, Rao RA. Acinic cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsaciniccell.html. Accessed September 17th, 2025.
Definition / general
- Malignant epithelial neoplasm of the salivary glands characterized by serous acinar cell differentiation (cytoplasmic zymogen granules) in at least some of the neoplastic cells
Essential features
- ~6 - 8% of all salivary gland neoplasms and 10 - 17% of primary salivary gland malignancies
- Parotid gland is the most common site
- Solid, microcystic, papillary cystic or follicular growth of acinar cells, with granular to vacuolated cytoplasm and eccentric round nuclei with conspicuous nucleoli
- Neoplastic cells positive for pankeratins, DOG1, SOX10 and PASD
- Favorable prognosis, with low rates of local recurrence, distant metastasis and high grade transformation
ICD coding
Epidemiology
- ~6 - 8% of all salivary gland neoplasms
- ~10 - 17% of primary salivary gland malignancies (Laryngoscope 2014;124:172, Int J Radiat Oncol Biol Phys 2012;84:189)
- Wide age range, from children to older adults (median: 52 years)
- Second most common salivary malignancy in children (after mucoepidermoid carcinoma)
- Third most common salivary malignancy in adults (after mucoepidermoid carcinoma and adenoid cystic carcinoma)
- Slightly more common in females than in males (F:M = 1.6:1) (Eur Arch Otorhinolaryngol 2020;277:2673)
- More common in White populations
- Reference: Oral Oncol 2018;82:53
Sites
- Most common site: parotid gland (91%)
- Submandibular and sublingual glands (5%)
- Minor salivary glands (4%) (Eur Arch Otorhinolaryngol 2016;273:3511)
- Most common sites in the oral cavity are the buccal mucosa and upper lip (Cancer 1983;52:542)
Etiology
- Familial predisposition (Case Rep Oncol 2015;8:1, Hematol Oncol Stem Cell Ther 2009;2:259)
- Previous radiation exposure
Clinical features
- Typical clinical presentation is a slow growing mass
- Pain, fixation to surrounding tissues and cranial nerve VII dysfunction are uncommon
- Cervical lymph node metastasis uncommon (up to 10%)
- Reference: Cancer 1991;67:172
Diagnosis
- Radiology (ultrasound [US], computed tomography [CT] or magnetic resonance imaging [MRI]) demonstrates presence and extent of mass lesion
- MRI is superior to CT in assessing invasion of adjacent structures
- Fine needle aspiration cytology and core biopsy
- Low sensitivity in parotid
- High false negatives due to morphologic overlap with normal acini (Arch Pathol Lab Med 2005;129:26)
- Diagnosis more challenging if tumor cells lack secretory granules
- Diagnostic accuracy higher in cases with high grade transformation
- Low sensitivity in parotid
- Definitive diagnosis most often established on a surgical excision specimen (e.g., parotidectomy)
- Positron emission tomography (PET) may be done postoperatively in cases of high grade transformation (Eur Arch Otorhinolaryngol 2016;273:3511)
Radiology description
- Ultrasound: well demarcated, lobular, hypoechoic, heterogeneous and poorly vascularized
- Computed tomography
- Findings are nonspecific and there is an overlap with benign tumors
- Solid to cystic mass
- Focal low attenuating portions on CT may be present, corresponding to cystic degeneration or hemorrhage (J Comput Assist Tomogr 2005;29:121)
Radiology images
Prognostic factors
- 5 year survival: 97%
- May recur years or decades after initial diagnosis
- Metastatic rate ~ 16%
- Local recurrence rate is up to 33%; 12% in another large study (Cancer 1978;41:924, Cancer 1983;52:542)
- Adverse prognostic factors include
- Male gender
- Age > 45 (JAMA Otolaryngol Head Neck Surg 2013;139:1195)
- Tumor > 3 cm at presentation (Oral Oncol 2018;82:53)
- Metastatic disease
- Tumor necrosis
- Nuclear pleomorphism
- Mitosis (> 2/10 high power fields [HPF])
- Ki67 index > 5%
- High grade transformation
- Vascular and perineural invasion
- Extracapsular extension (Cancer 2009;115:2128)
- Positive resection margins
- Invasion of the skull base
- Depletion of lymphocytes within the stroma
Case reports
- 31 year old man with a left upper lip nodule (J Clin Exp Dent 2016;8:e638)
- 46 year old man with hypertension, new onset diabetes and hypokalemia (Case Rep Endocrinol 2019;2019:3196283)
- 48 year old woman with a 6 month history of a right parotid swelling that rapidly and progressively increased in size (Case Rep Otolaryngol 2017;2017:7296467)
Treatment
- Complete surgical excision (J Oral Maxillofac Surg 2005;63:917)
- Radiotherapy may be indicated for tumors that metastasize or cannot be completely excised
- Systemic therapy may be indicated for high grade tumors, positive margins, advanced stage disease or metastatic tumors
Gross description
- Tumor dimensions range from < 1 cm to 13 cm (85% of the lesions are < 3 cm) (Cancer 1983;52:542)
- Well circumscribed, soft rubbery, tan-yellow to pink mass with homogeneous cut surface
- Cystic change and hemorrhage may occur
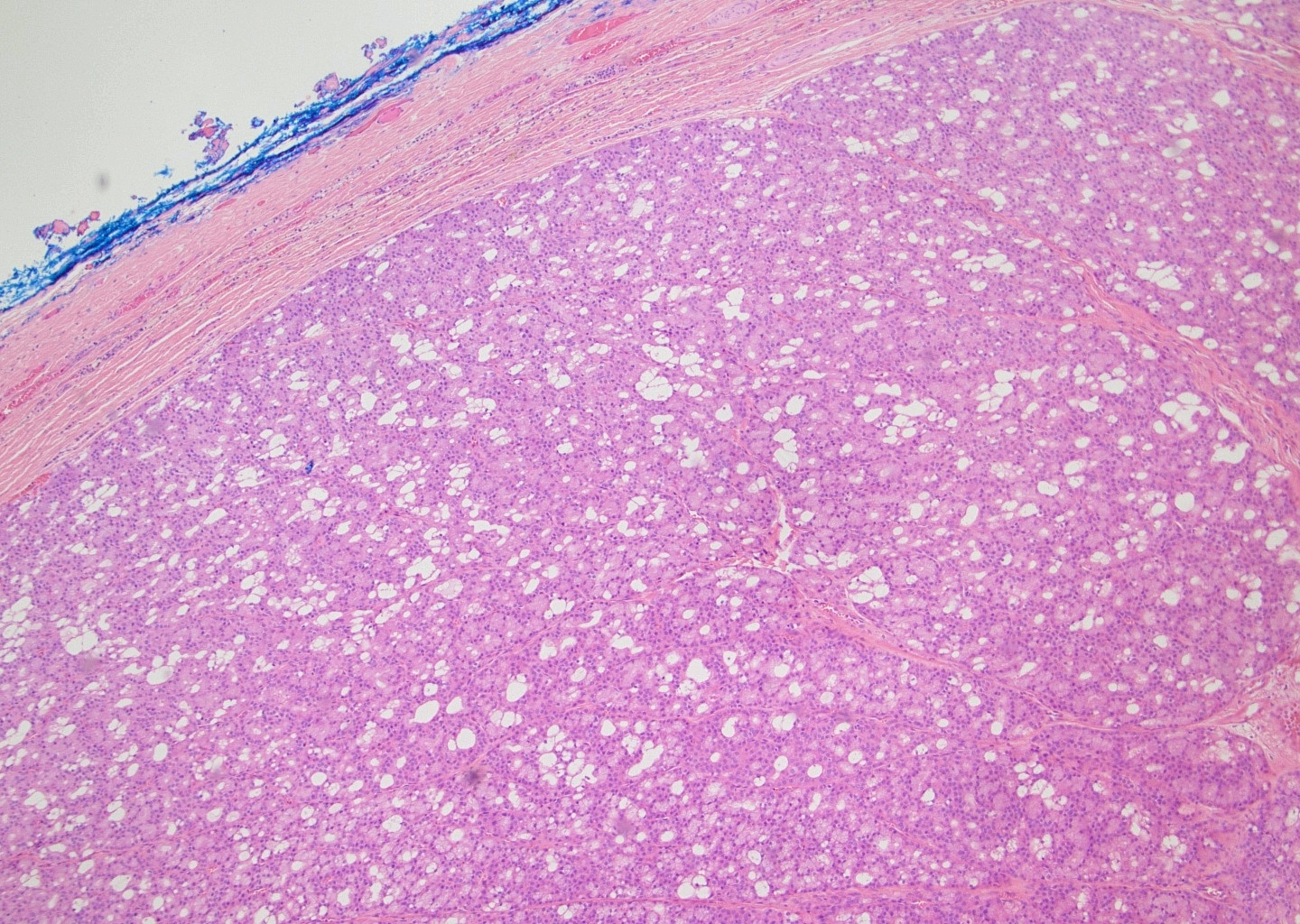
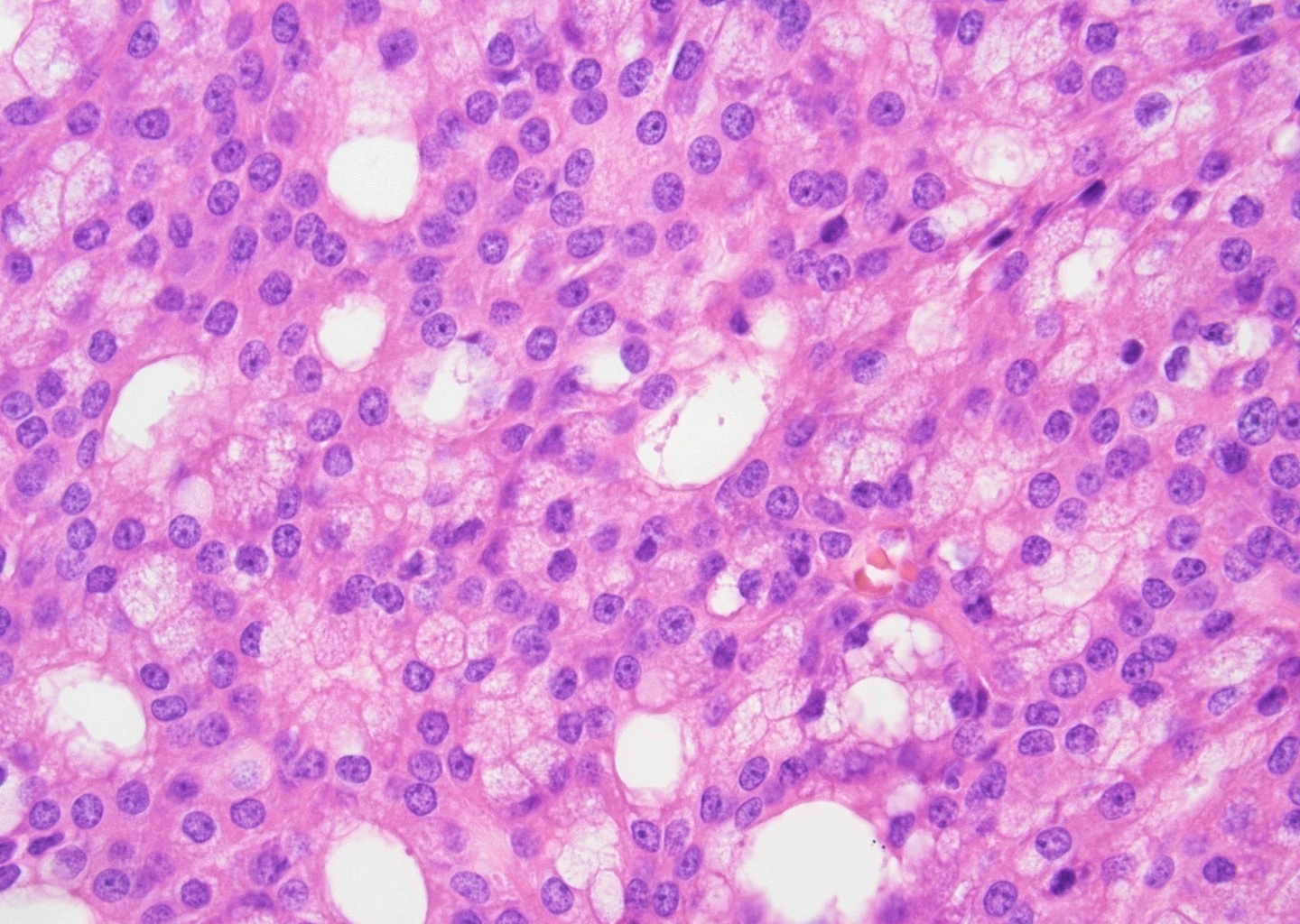
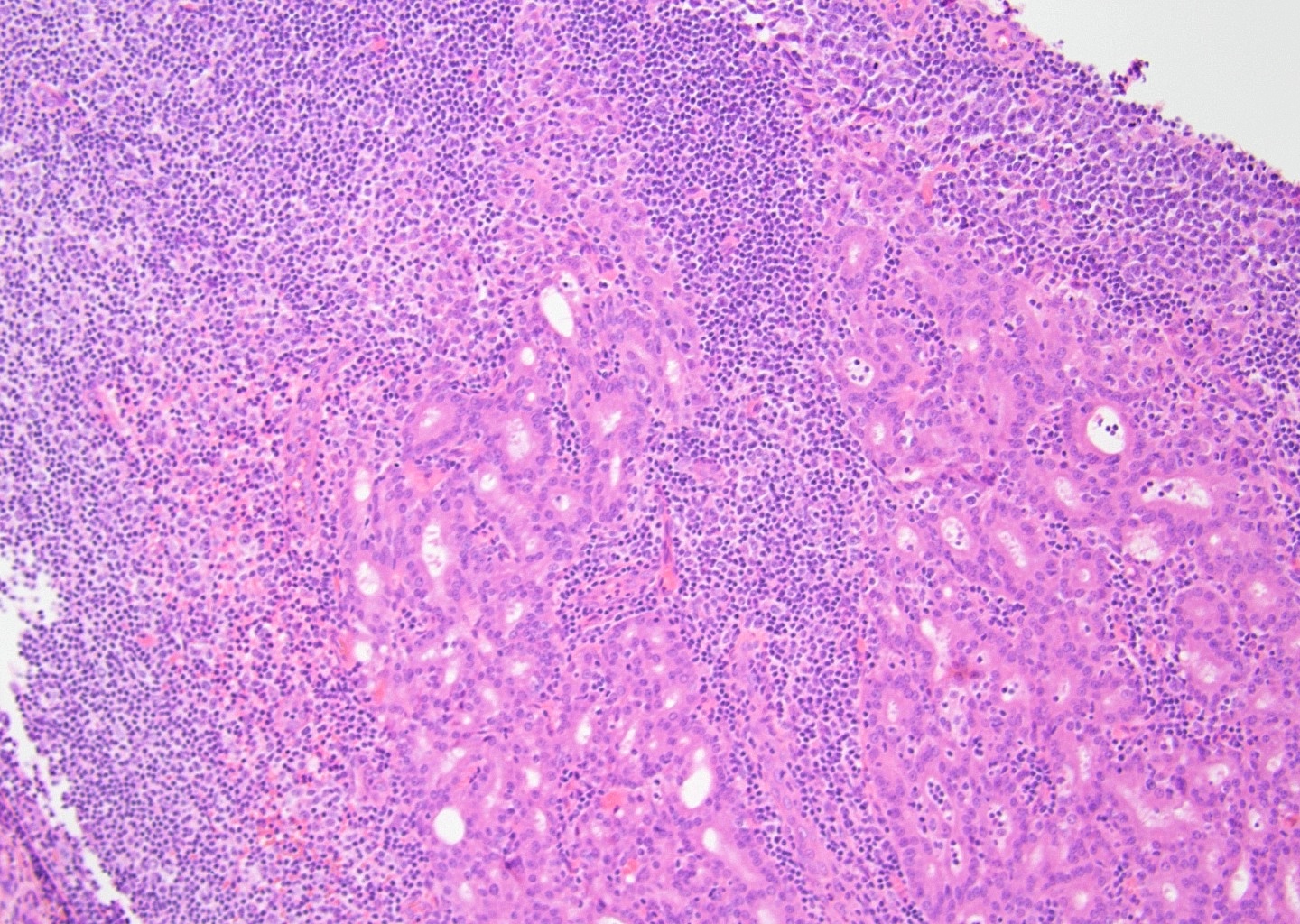
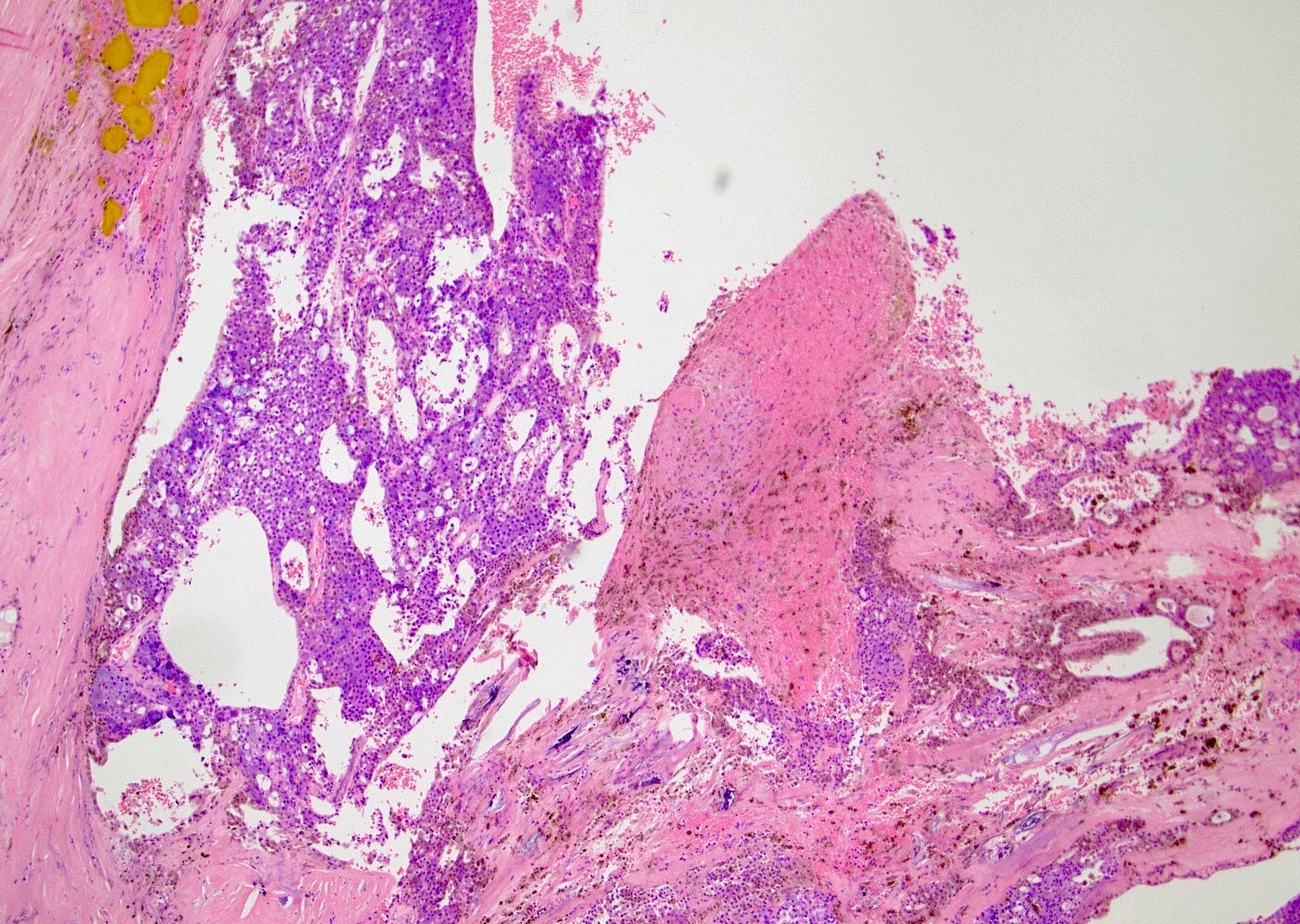
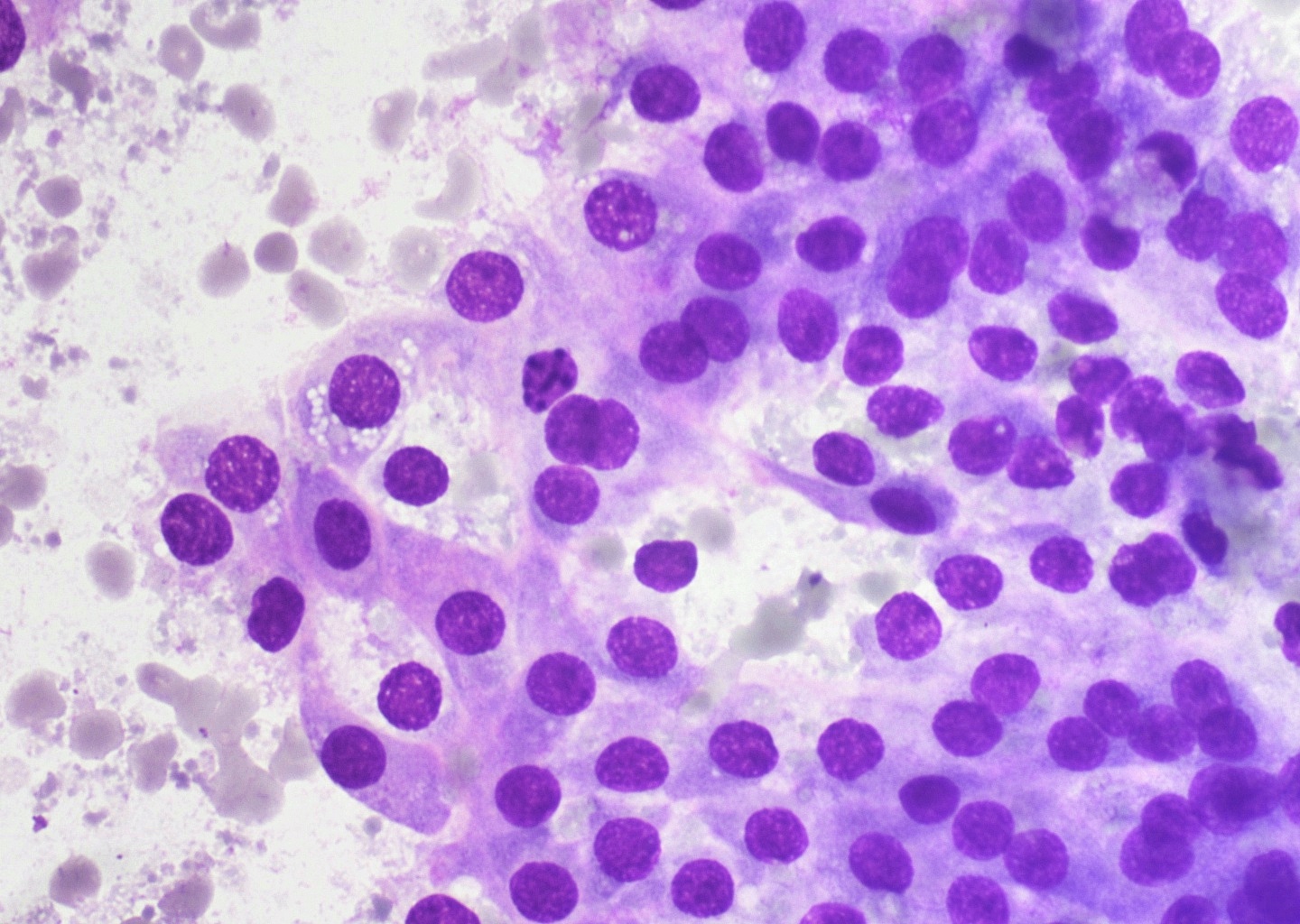
Microscopic (histologic) description
- Multiple cell types are noted
- Cell types include serous acinar, intercalated ductal, vacuolated, nonspecific glandular and clear cells
- Acinar cells are large and polyhedral, with basophilic granular cytoplasm and eccentric nuclei
- Cytoplasmic diastase resistant positive periodic acid-Schiff (PAS) reaction may be focal
- Variety of morphologic patterns, including solid, microcystic, papillary cystic and follicular (Cancer 1983;52:542)
- Prominent lymphoid infiltrate may be present (tumor associated lymphoid proliferation varies from randomly scattered, patchy collections of lymphocytes to diffuse, dense infiltrates with well formed follicles throughout the tumor) (Oral Surg Oral Med Oral Pathol 1994;77:19)
- Mitosis, necrosis and significant pleomorphism usually absent
- Proposed grading system (Am J Surg Pathol 2022;46:933)
- Low to intermediate grade: mitotic count < 5/10 HPF and no necrosis
- High grade: mitotic count ≥ 5/10 HPF or necrosis
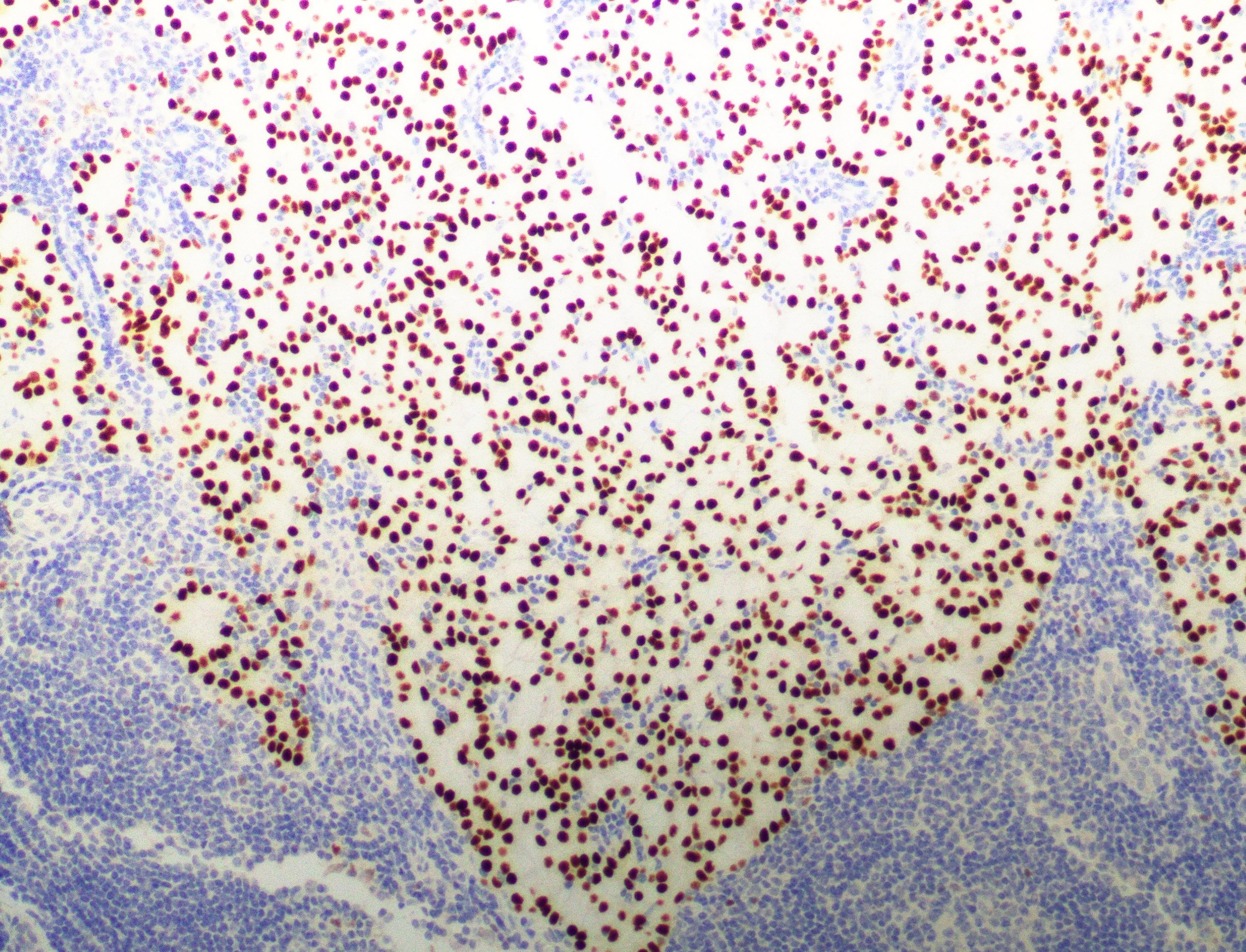
Microscopic (histologic) images
Virtual slides
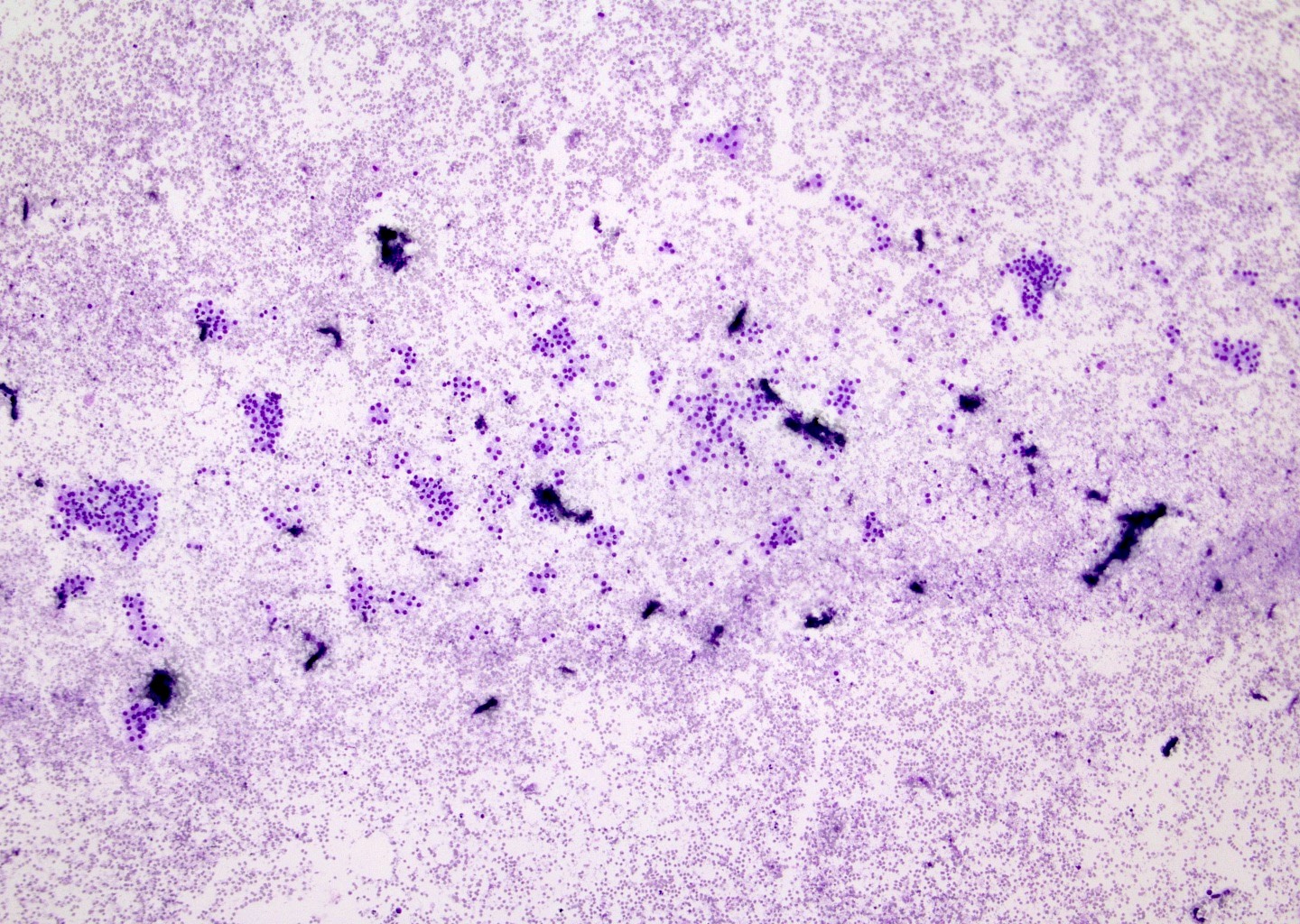
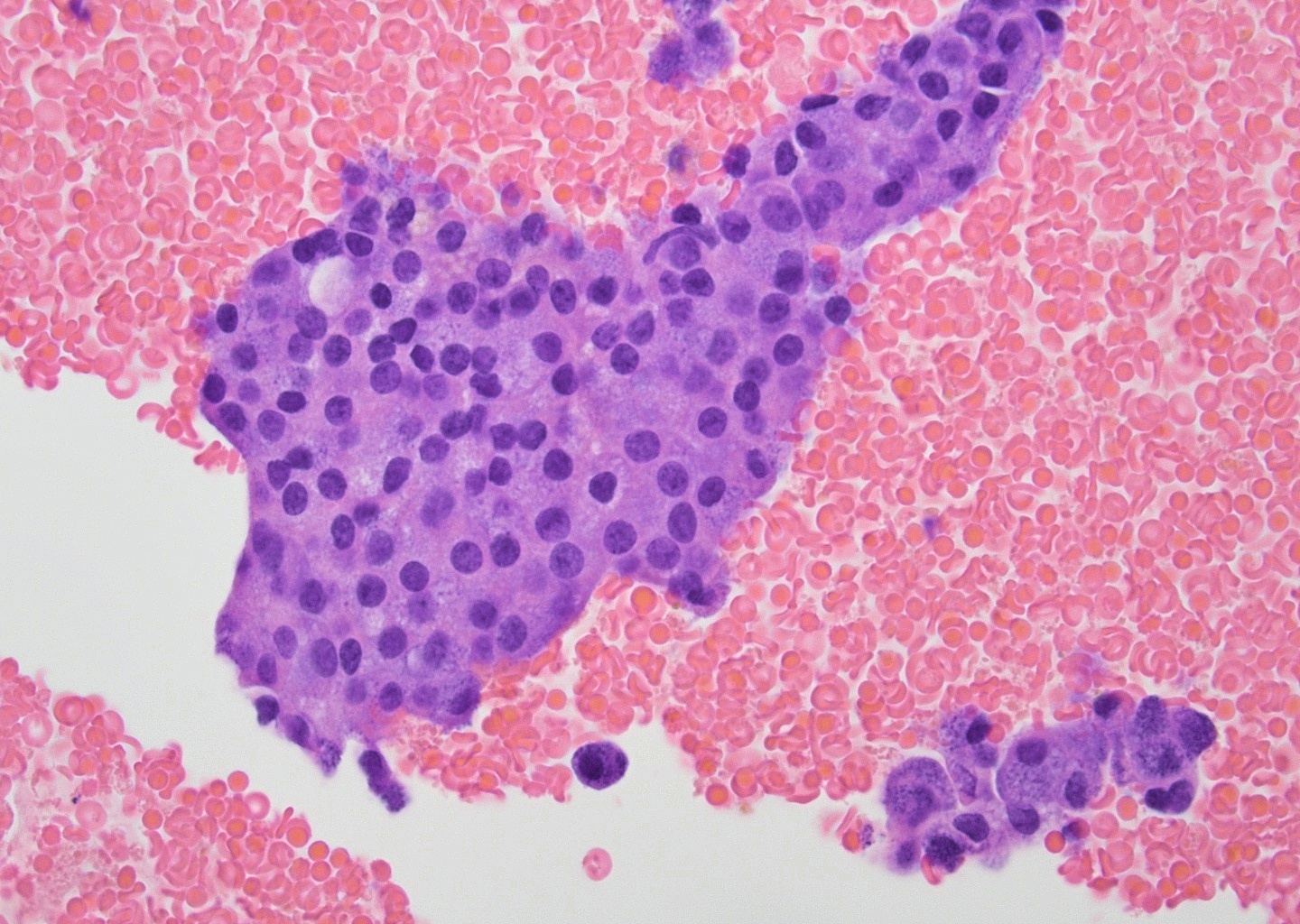
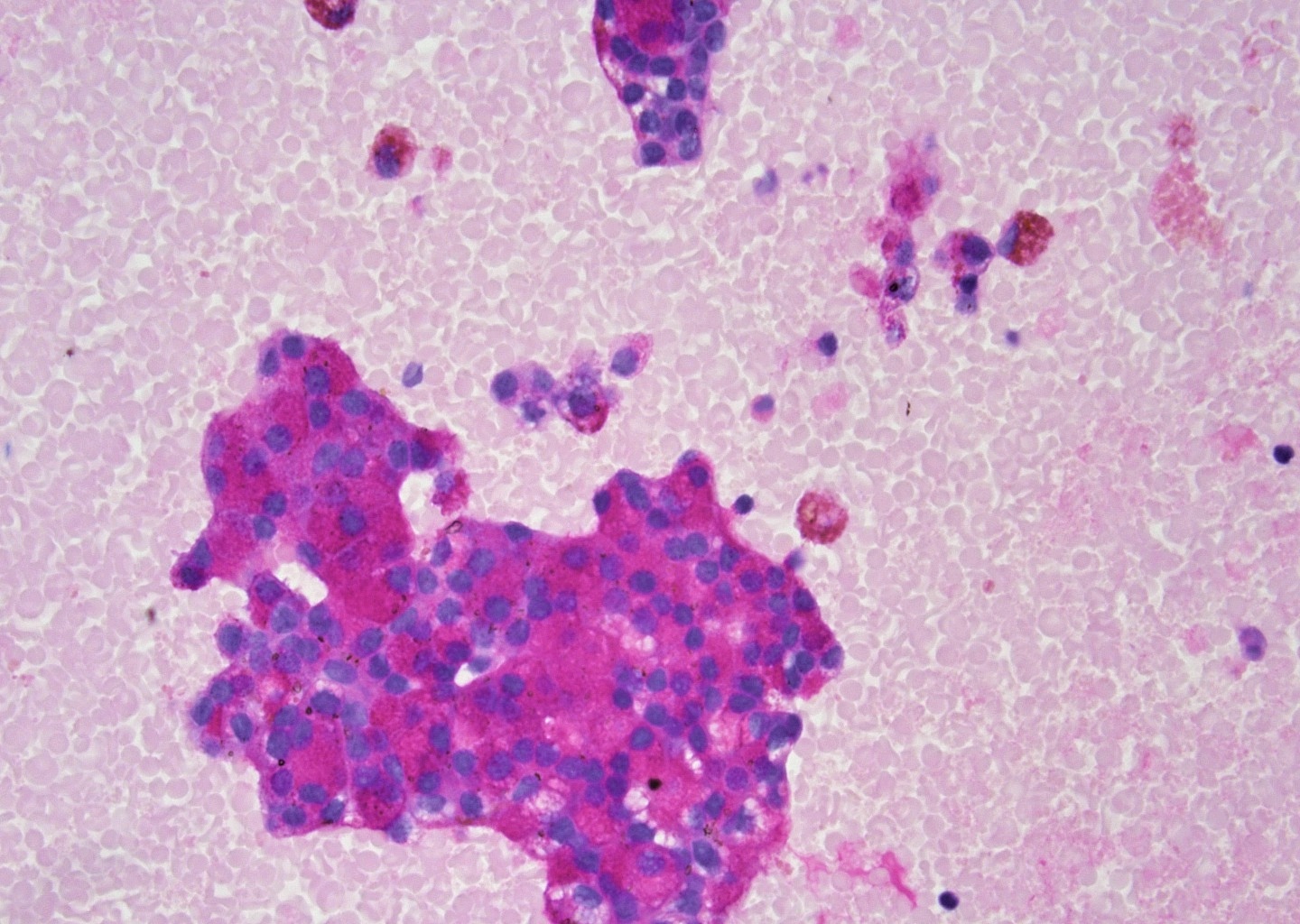
Cytology description
- Cellular aspirates
- Cytologic diagnosis based on identifying acinar-like cells
- Tend to form small groups and loosely cohesive clusters as well as single cells (Diagn Histopath 2018;24:417)
- Cells are large but morphologically resemble normal acinar cells
- Round nuclei with tiny nucleoli
- Abundant finely vacuolated to granular cytoplasm
- Stripped or bare nuclei may be present in the background, can mimic lymphocytes
- Lymphocytic infiltrate may be prominent
- Laminated psammoma body-like calcification may be present
- Pitfall: acinic cells may resemble oncocytes and in the presence of lymphocytic infiltrate, the tumor may be misdiagnosed as Warthin tumor
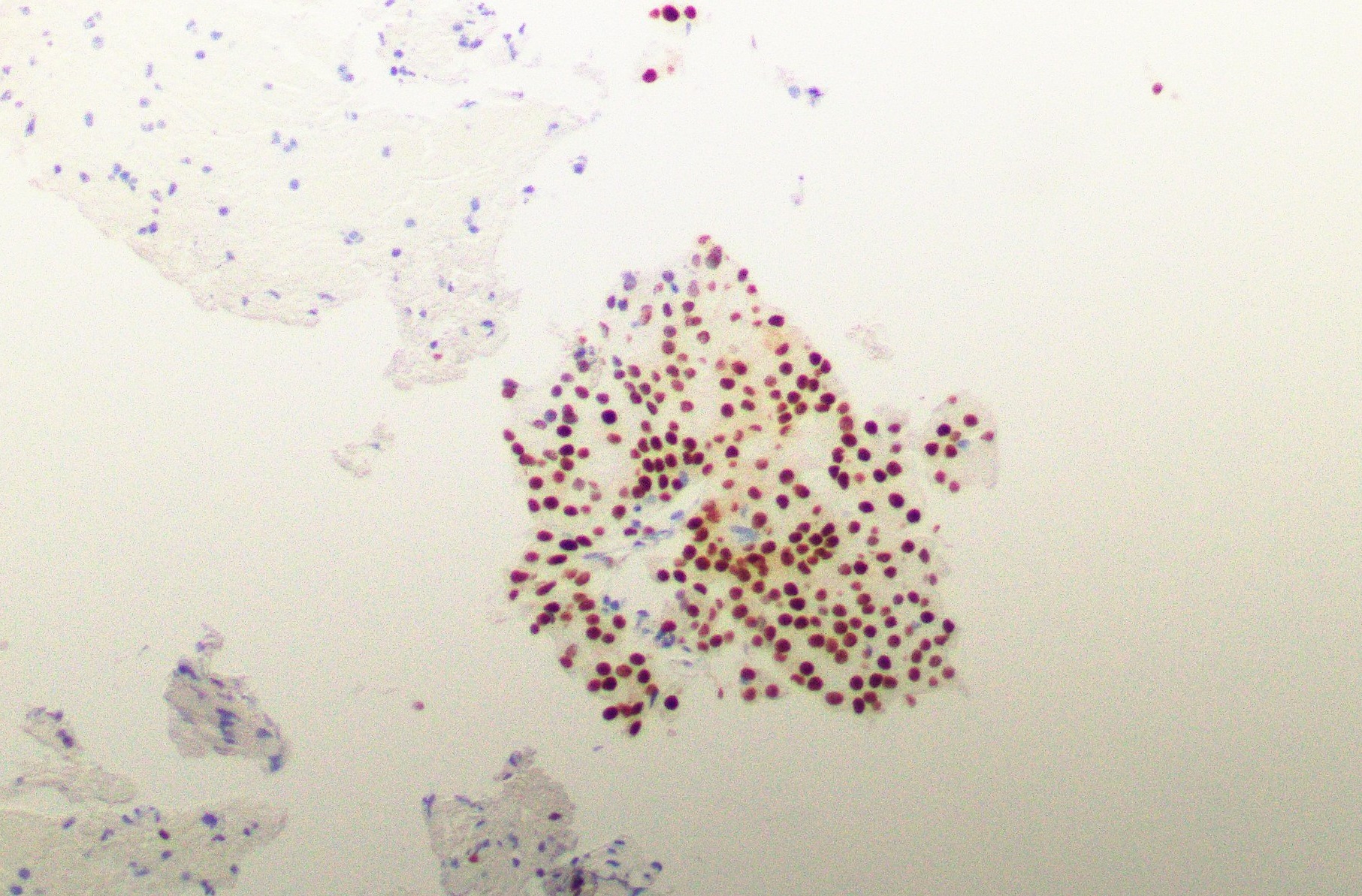
Cytology images
Positive stains
- Pancytokeratins, EMA and CEA
- DOG1: intense positivity (Laryngoscope Investig Otolaryngol 2018;3:268)
- Admixture of apical membranous, cytoplasmic and complete membranous staining
- Nonspecific (expressed in adenoid cystic carcinoma and epithelial myoepithelial carcinoma)
- SOX10
- PASD
- NR4A3 (NOR1) or NR4A2 (NURR1) (novel, highly specific marker) (Cancer Cytopathol 2021;129:104)
Negative stains
- Calponin, p63 and actin (Head Neck Pathol 2013;7:64)
- Mammaglobin (useful in distinction from secretory carcinoma)
- S100: the focal positivity that is seen highlights the intercalated ducts
- p40
- Reference: Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015
Molecular / cytogenetics description
- Recurrent (t[4;9][q13;q31]) genomic rearrangement (resulting in translocation of active enhancer regions from the secretory Ca binding phosphoprotein [SCPP] gene cluster to the region upstream of nuclear receptor subfamily 4 group A member 3 [NR4A3], leading to NR4A3 IHC overexpression) (Cancer Cytopathol 2021;129:104)
- Loss of function mutations of CDKN2A / CDKN2B gene are associated with high grade histology and distant metastasis (Mod Pathol 2023;36:100150)
Sample pathology report
- Parotid gland, right, inferior, partial parotidectomy:
- Acinic cell carcinoma, 1.7 cm (see synoptic report)
- No lymphovascular invasion identified
- No perineural invasion identified
- Resection margins uninvolved by carcinoma
- 2 lymph nodes, negative for carcinoma (0/2)
- Tumor associated lymphoid proliferation present
Differential diagnosis
- Normal acinar elements:
- Appear as grape-like clusters in cytology or tight lobulated clusters in histology
- Lacks cellularity, looseness of the malignant clusters and numerous bare nuclei
- Secretory carcinoma (formerly mammary analogue secretory carcinoma):
- Lack of zymogen-like secretory granules
- Diffuse and strong positivity for S100 and mammaglobin
- ETV6::NTRK3 translocation
- DOG1 negative
- Lacks NR4A3 translocation and immunostaining (Cancer Cytopathol 2021;129:104)
- Mucoepidermoid carcinoma:
- Presence of extracellular and intracellular mucin, mucicarmine positive
- Has 3 cell types (mucinous, intermediate and epidermoid) in low and intermediate grade
- Harbors CRTC1::MAML2 translocation
- When clear cell component predominates:
- Myoepithelioma:
- Epithelial myoepithelial carcinoma:
- Has a dual staining pattern of malignant epithelial and myoepithelial cells
- Oncocytoma:
- Metastatic clear cell renal cell carcinoma:
- PAX8+
- When follicular pattern predominates:
- Thyroid follicular neoplasms:
- TTF1, thyroglobulin, PAX8 stains positive
- Thyroid follicular neoplasms:
Additional references
Practice question #1
Which of the following statements is true regarding acinic cell carcinoma of salivary glands?
- Acinic cell carcinoma is a high grade malignant neoplasm
- Most commonly occurs in minor salivary glands
- Neoplastic cells express DOG1 and SOX10
- Younger age at presentation and presence of tumor associated lymphocytes are associated with a poor prognosis
Practice answer #1
C. Neoplastic cells express DOG1 and SOX10. DOG1 and SOX10 are expressed in benign acinar cells and intercalated duct cells and other salivary gland neoplasms; however, strong diffuse expression of these markers can help distinguish acinic cell carcinoma from other salivary gland neoplasms. Answer A is incorrect because acinic cell carcinoma is considered low intermediate grade malignancy of salivary glands, although high grade transformation may occur. Answer B is incorrect because the majority of cases arise in the parotid gland. Answer D is incorrect because older age at the onset (> 45) and depletion of lymphocytes within the stroma are linked to worse outcomes.
Comment Here
Reference: Acinic cell carcinoma
Comment Here
Reference: Acinic cell carcinoma
Practice question #2
A 51 year old woman presents with a left parotid mass. CT images show a well circumscribed cystic lesion measuring 3 cm. An excisional biopsy is performed (see image above). The neoplastic cells are positive for periodic acid-Schiff with diastase (PASD). Which of the following statements is true regarding this lesion?
- Cytology aspirates of this tumor can show predominance of extracellular mucin
- Mitosis, necrosis and significant pleomorphism are usually present
- MYB immunohistochemical staining in FNA specimens is useful in the diagnosis of this tumor
- Pain and facial nerve dysfunction are uncommon presenting symptoms
Practice answer #2
D. The most common initial presentation in patients with acinic cell carcinoma is a painless mass without facial nerve involvement. Answer C is incorrect because MYB immunohistochemical staining is useful in the diagnosis of adenoid cystic carcinoma. Answer A is incorrect because the presence of extracellular mucin in aspirates is a feature of mucoepidermoid carcinoma. Answer B is incorrect because acinic cell carcinoma is usually a low grade malignant neoplasm without significant mitosis, necrosis or pleomorphic nuceli.
Comment Here
Reference: Acinic cell carcinoma
Comment Here
Reference: Acinic cell carcinoma