Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Song S, Reyes MC. Struma ovarii. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorstruma.html. Accessed August 18th, 2025.
Definition / general
- Monodermal ovarian teratoma primarily (> 50%) or exclusively composed of benign thyroid tissue
- Any mature teratoma with malignant thyroid tissue
Essential features
- Ovarian teratoma either composed predominantly or exclusively of benign thyroid tissue or with any amount of malignant thyroid tissue
- Most common thyroid malignancy to occur in struma ovarii is papillary thyroid carcinoma, followed by follicular carcinoma
ICD coding
Epidemiology
- Most common type of monodermal teratoma
- Accounts for 3% of ovarian teratomas (Pathol 2007;39:139)
- Usually presents in the fifth decade
Sites
- Ovary
Pathophysiology / etiology
- Unknown at this time
Clinical features
- Most often an incidental and asymptomatic finding but may present as a pelvic mass with abdominal pain (Pathology 2007;39:139)
- Uncommonly presents as hyperthyroidism or pseudo-Meigs syndrome (with ascites and pleural effusion) (Pathology 2007;39:139)
- Seen in association with Brenner tumor, serous and mucinous cystadenoma and fibrothecoma (Endocr Pathol 2015;26:342)
Diagnosis
- Diagnosis is made by microscopic examination of resected tissue
Laboratory
- Mildly increased CA125 levels in up to 30% of cases (J Gynecol Oncol 2008;19:135)
Radiology description
- Typically a lobulated and multiloculated solid cystic lesion on imaging (Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2015;37:309, Abdom Imaging 2012;37:904)
- MRI is more specific, showing high and low signal intensity on T1 and T2 weighted images from the colloid (J Med Imaging Radiat Oncol 2009;53:480)
Prognostic factors
- Most cases have a good prognosis, even when malignancy is present
Case reports
- 10 year old girl with tachycardia, normal thyroid and thyrotoxicosis with papillary thyroid carcinoma arising from a struma ovarii (Int J Surg Case Rep 2018;51:218)
- 48 year old woman with malignant struma ovarii presenting 14 years after oophorectomy and chemotherapy (Medicine (Baltimore) 2018;97:e13867)
- 52 year old woman with clinical features of advanced ovarian carcinoma found to have a struma ovarii (Oncol Lett 2015;9:1739)
- 61 year old woman with insular carcinoma (90%) and adjacent papillary thyroid carcinoma arising in a struma ovarii (Gynecol Oncol Rep 2016;18:1)
- 62 year old woman with 2 different types of RAS mutations in a papillary thyroid carcinoma from a struma ovarii and papillary thyroid microcarcinoma of the thyroid (J Endocr Soc 2018;2:944)
- 74 year old woman with a mixed ovarian tumor composed of elements of Brenner tumor, mucinous cystadenoma and struma ovarii (Int J Gynecol Pathol 2019;38:576)
Treatment
- Oophorectomy
- Surgery for malignant struma ovarii may include total abdominal hysterectomy and bilateral salpingo-oophorectomy with complete staging (Gynecol Oncol 2004;94:835)
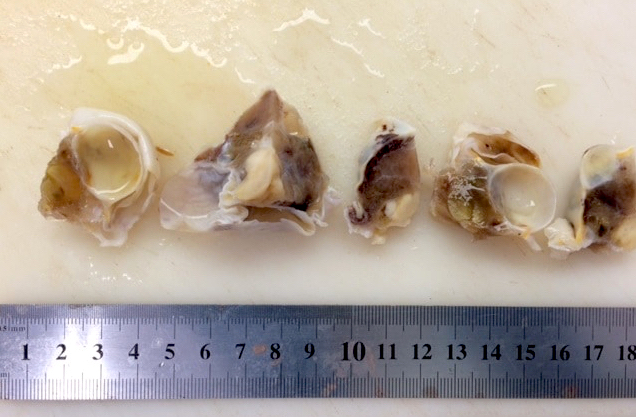
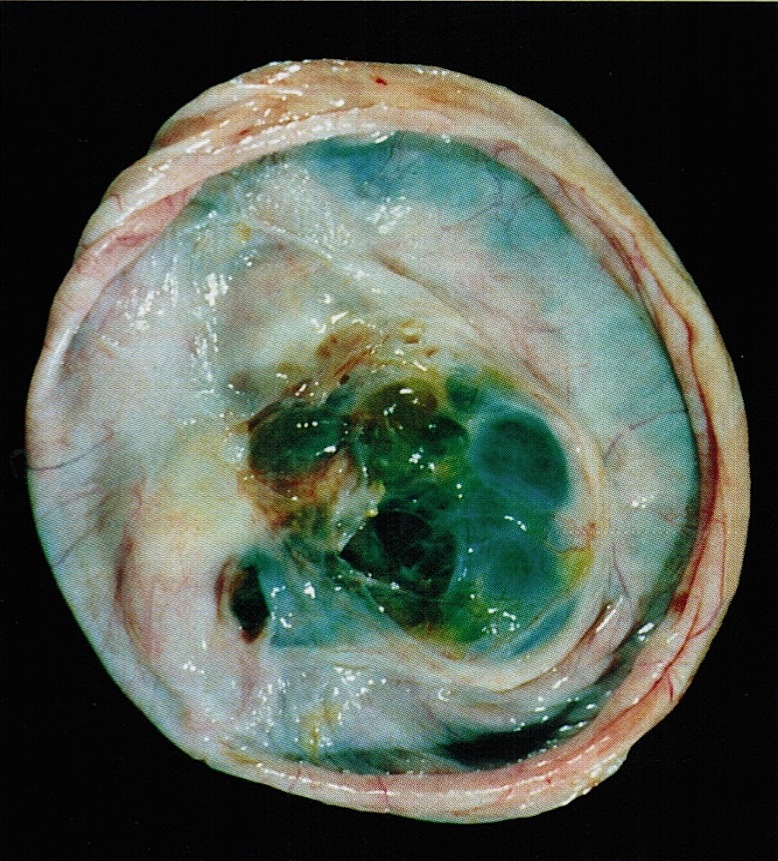
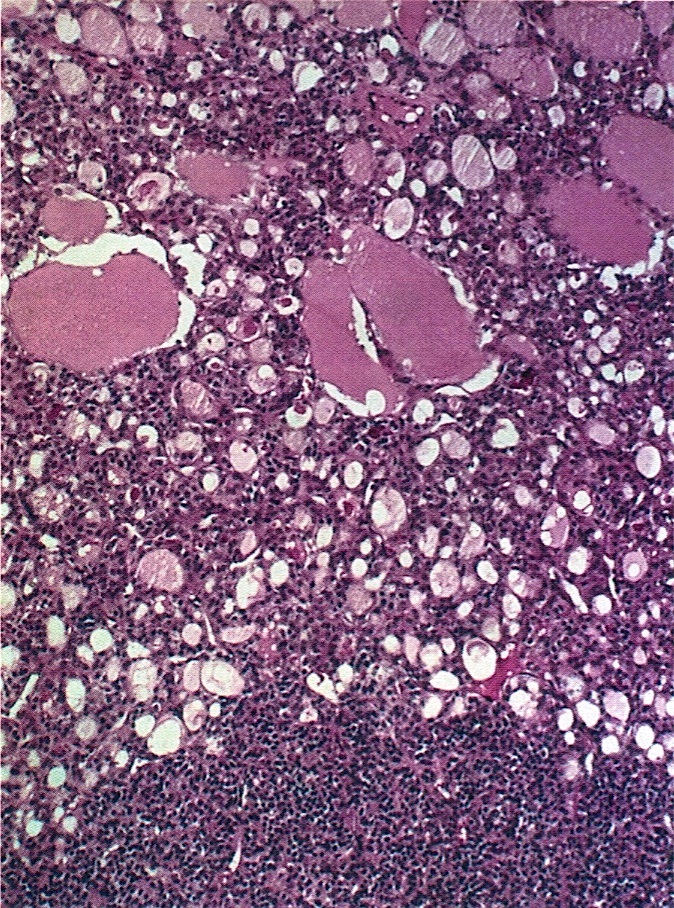
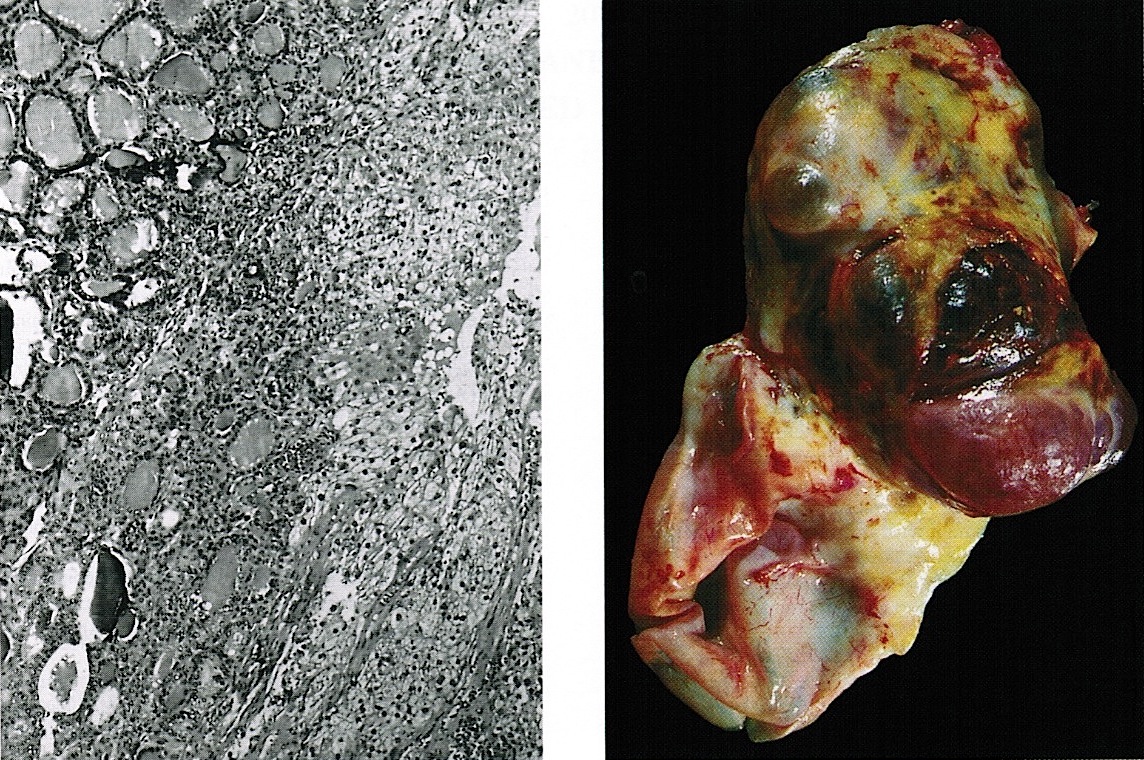
Gross description
- Typically unilateral and solid with a gelatinous, red-brown to green cut surface; may show goiter-like multinodular or cystic change (Am J Surg Pathol 1994;18:785)
Gross images
Frozen section description
- Frozen section sample usually shows a mature teratoma or benign thyroid tissue; rarely, a possible malignant component may be detected
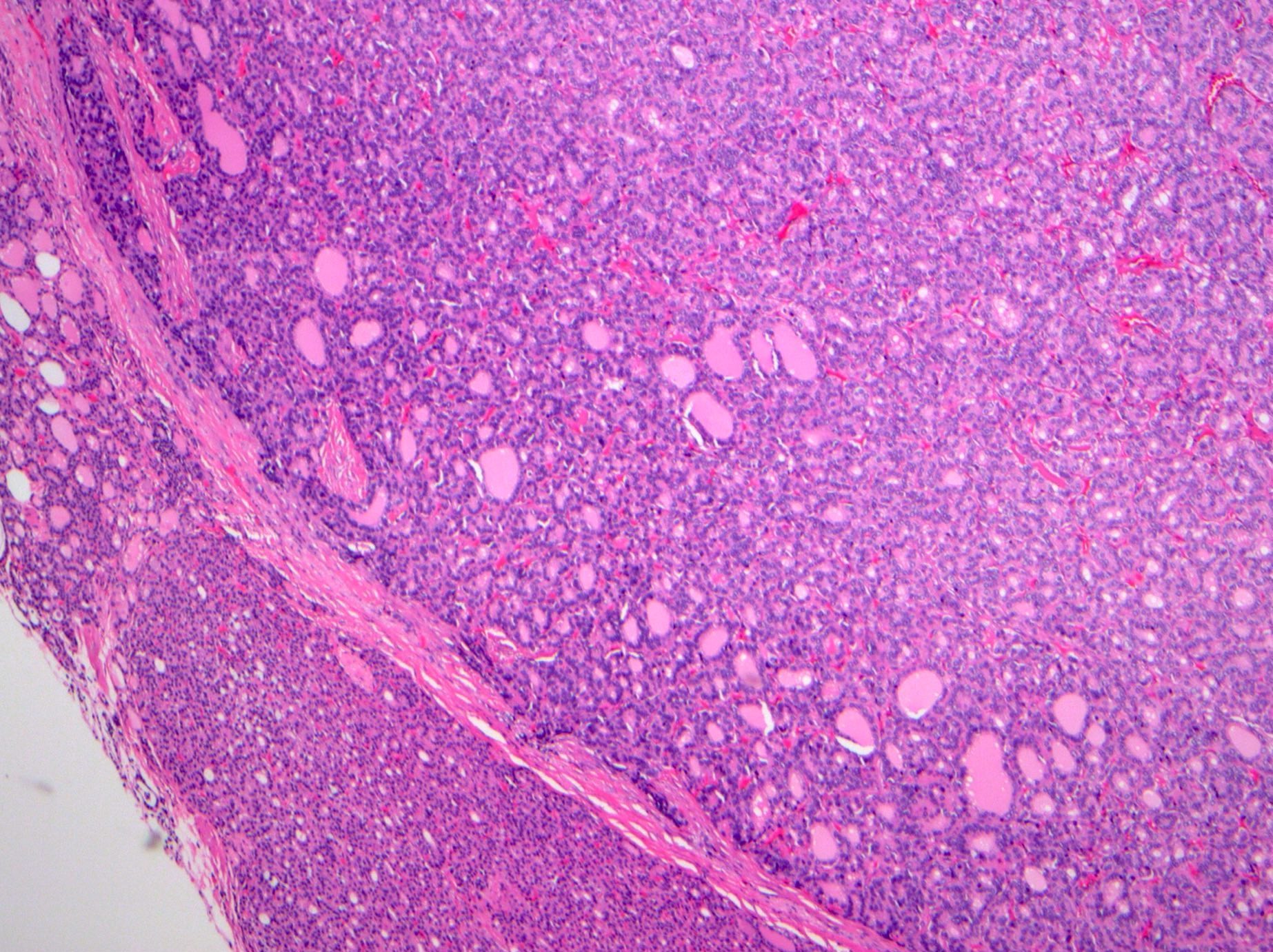
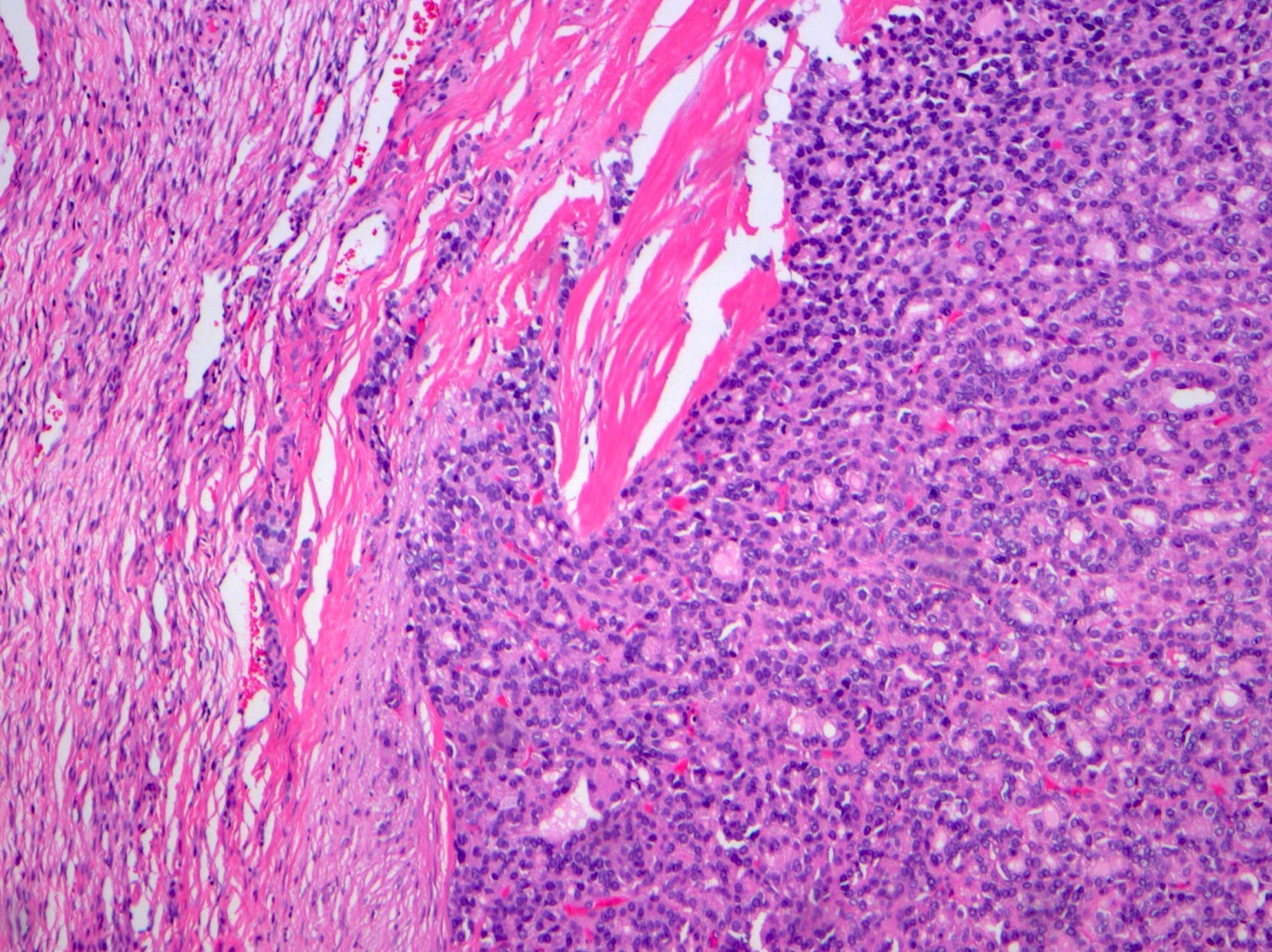
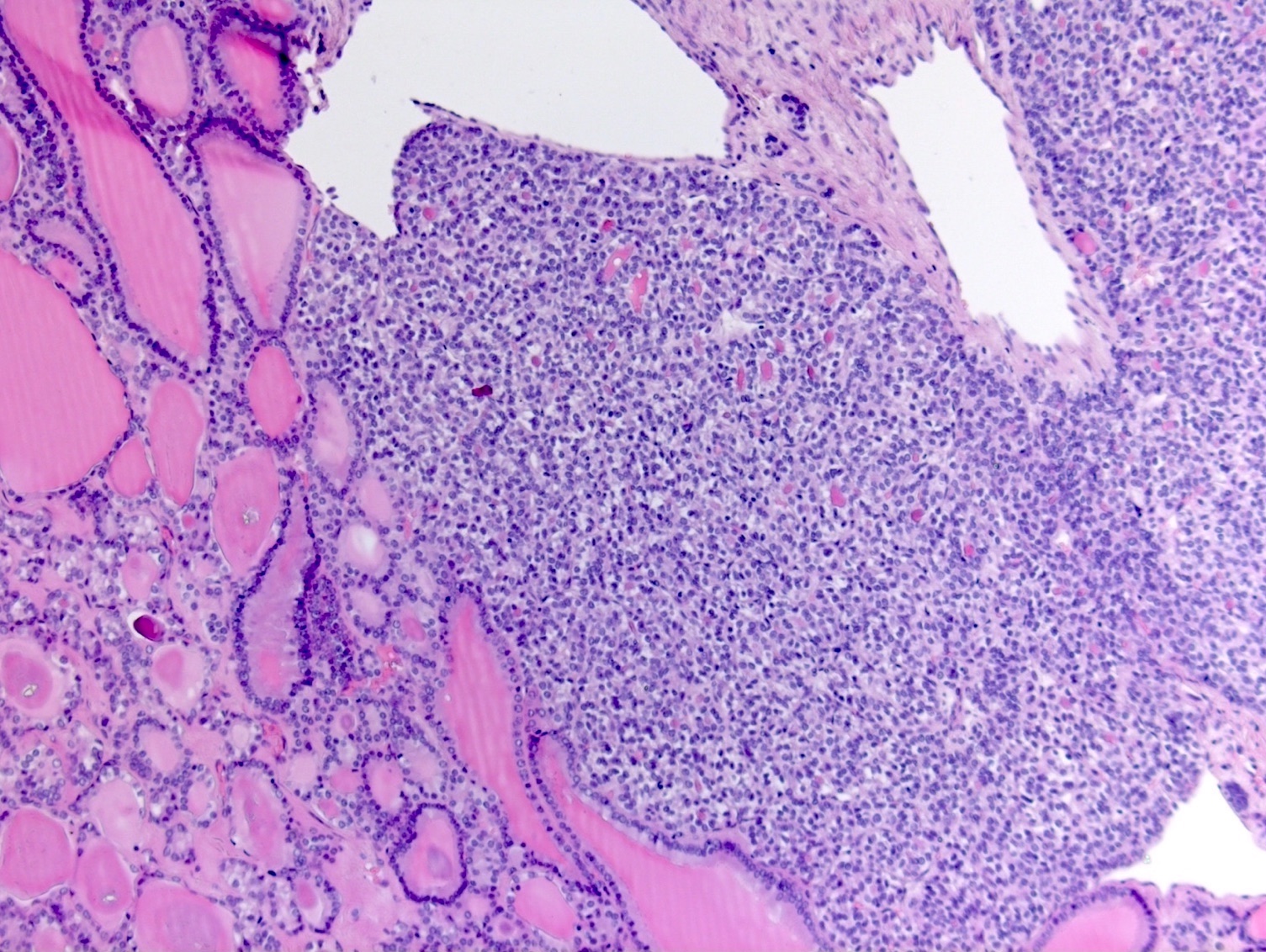
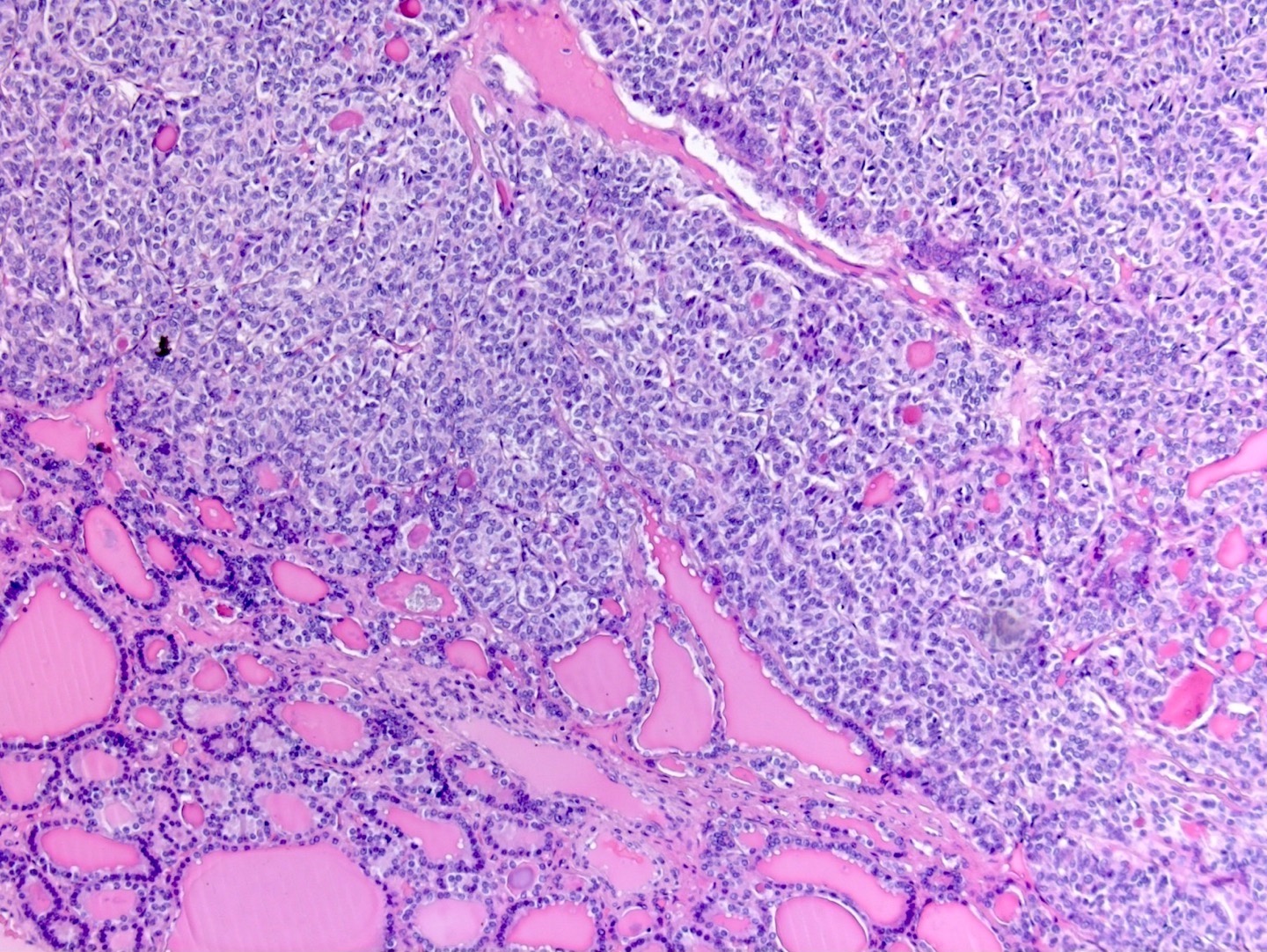
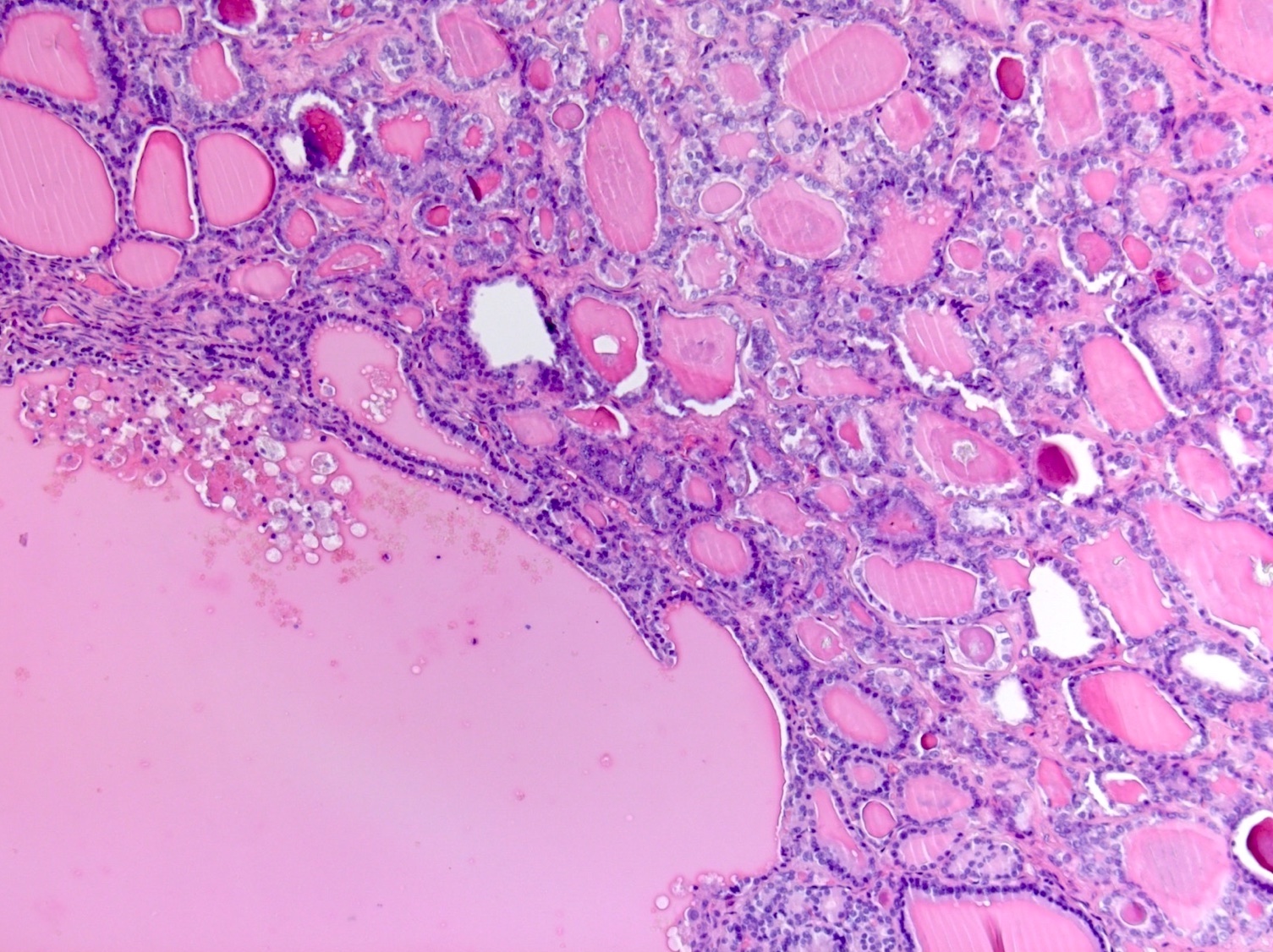
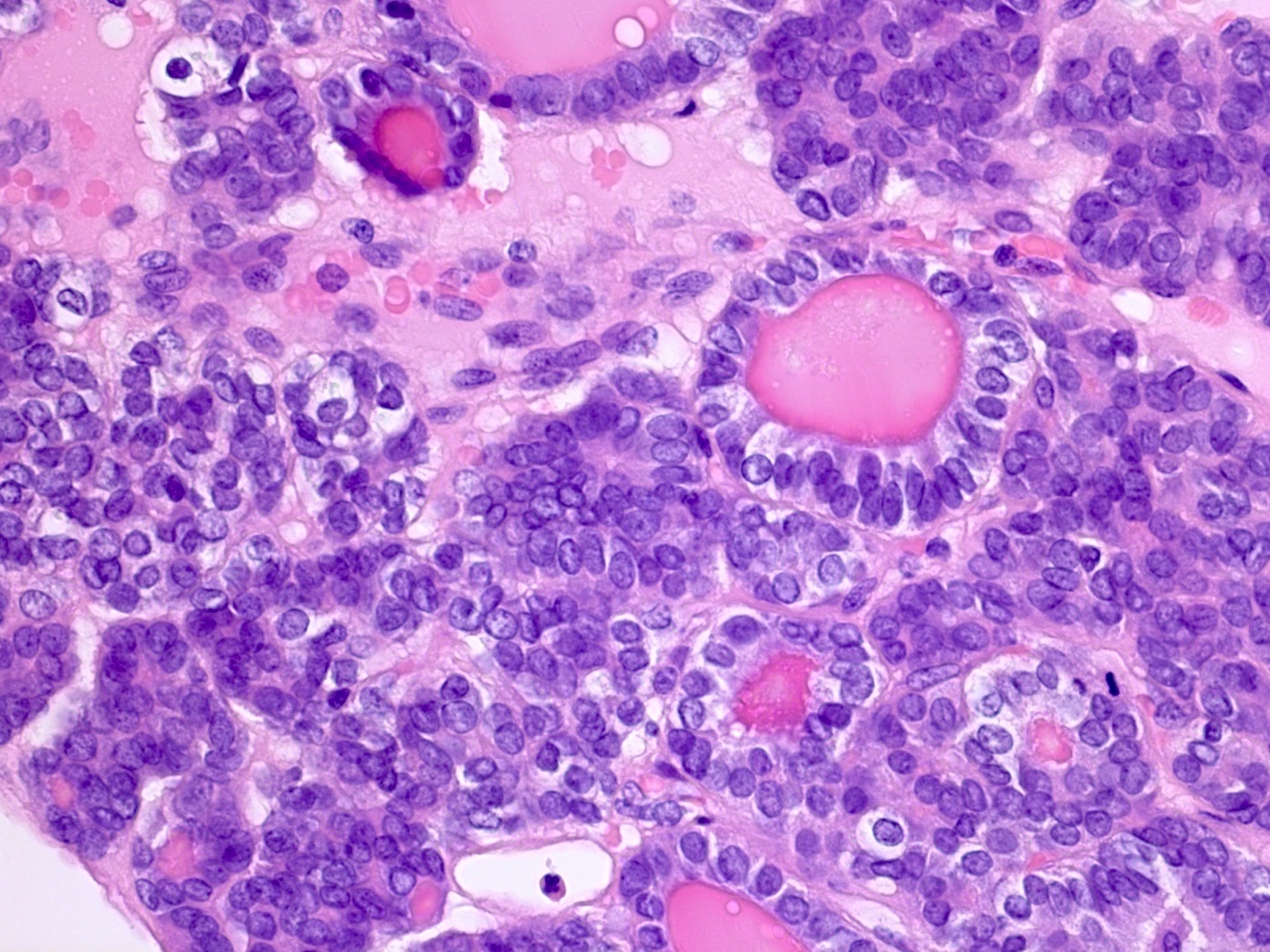
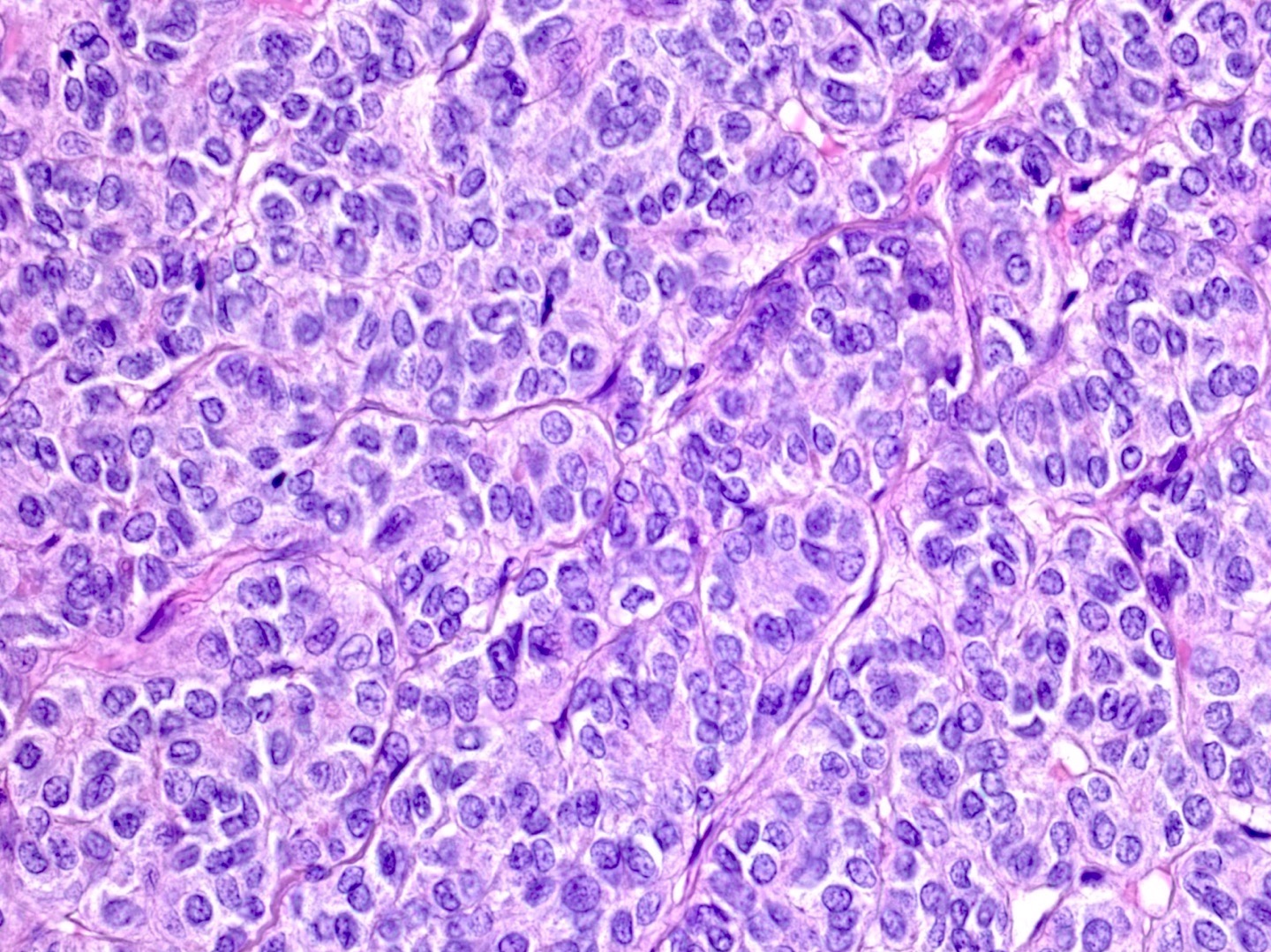
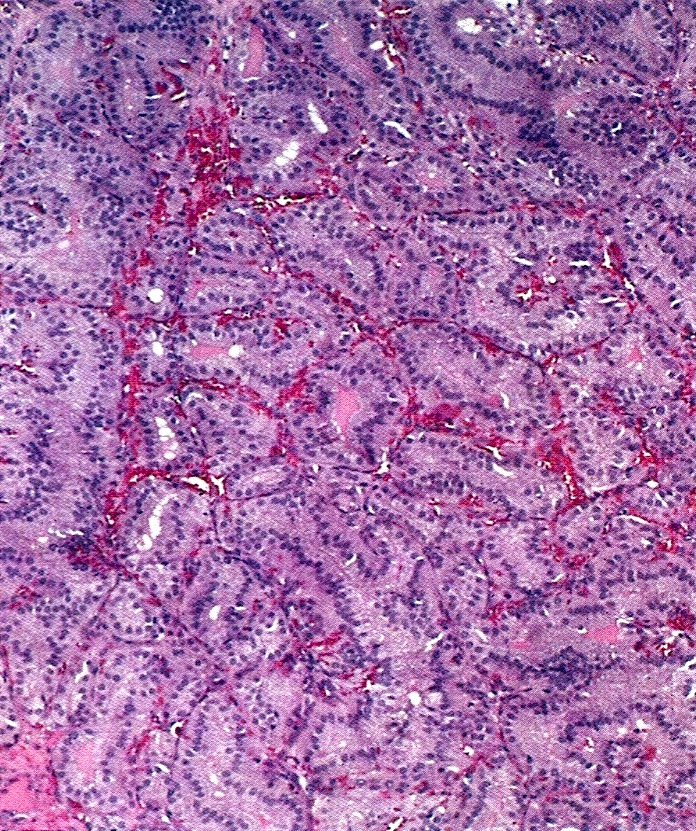
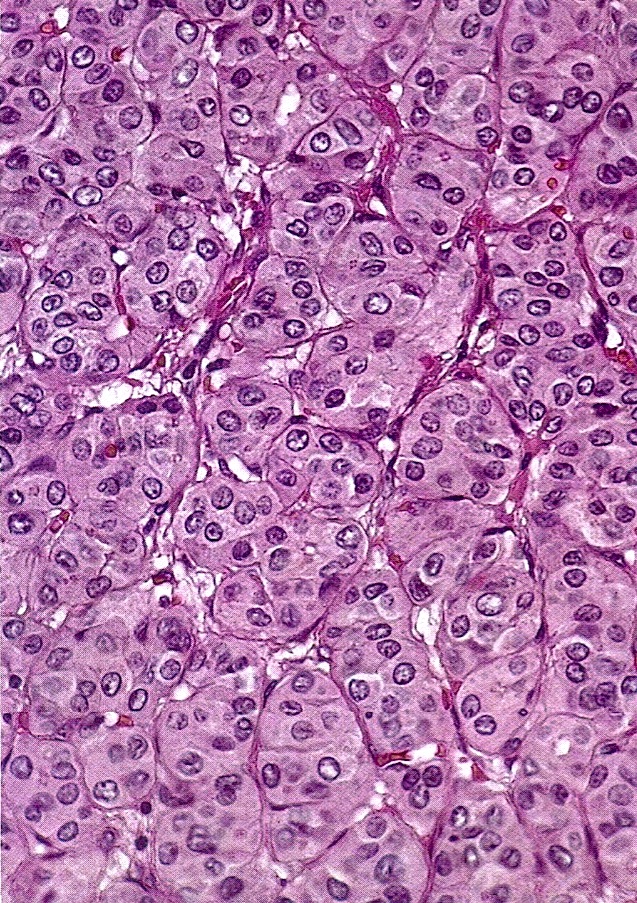
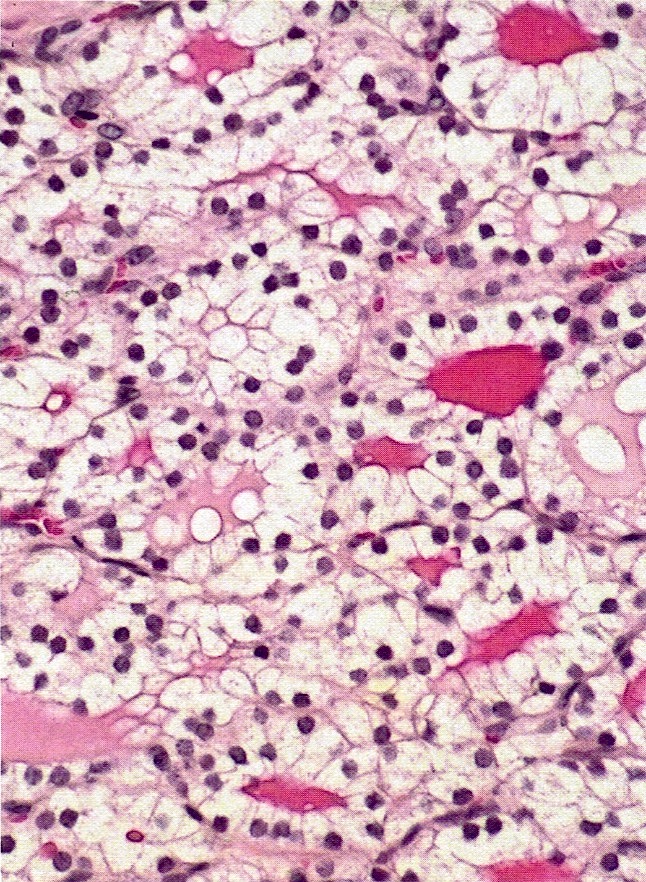
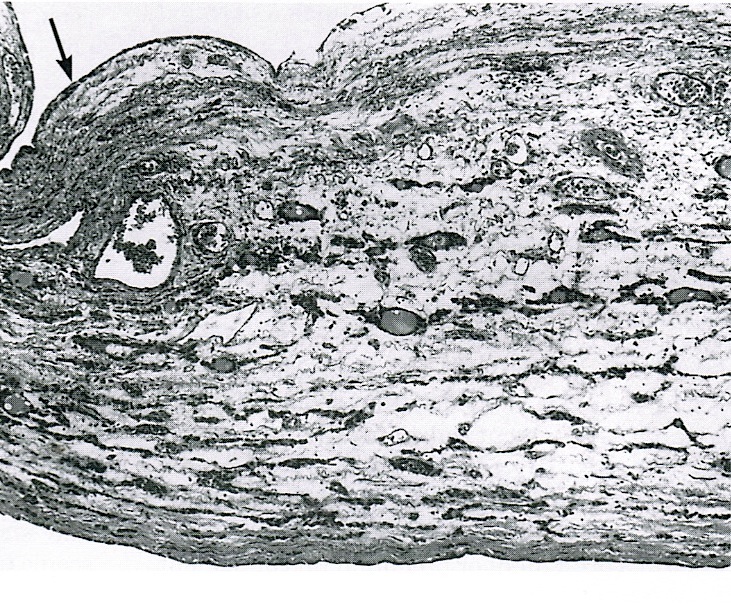
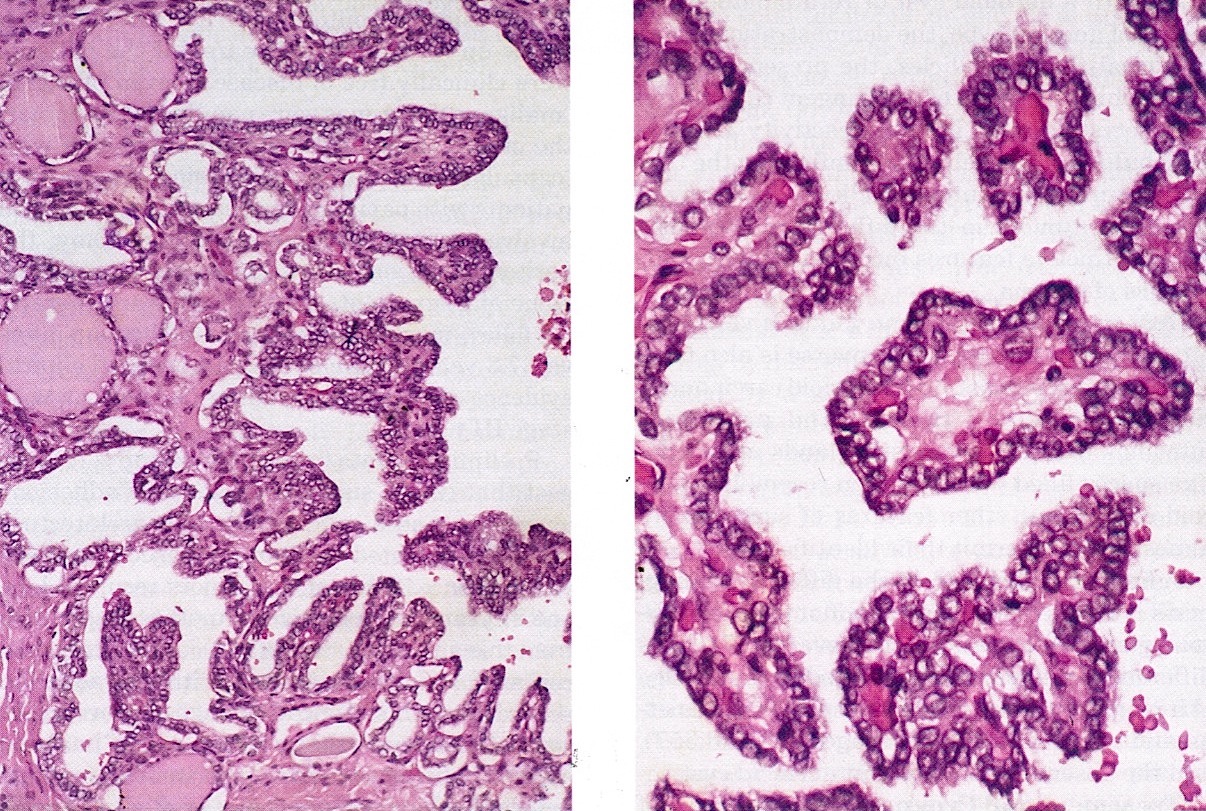
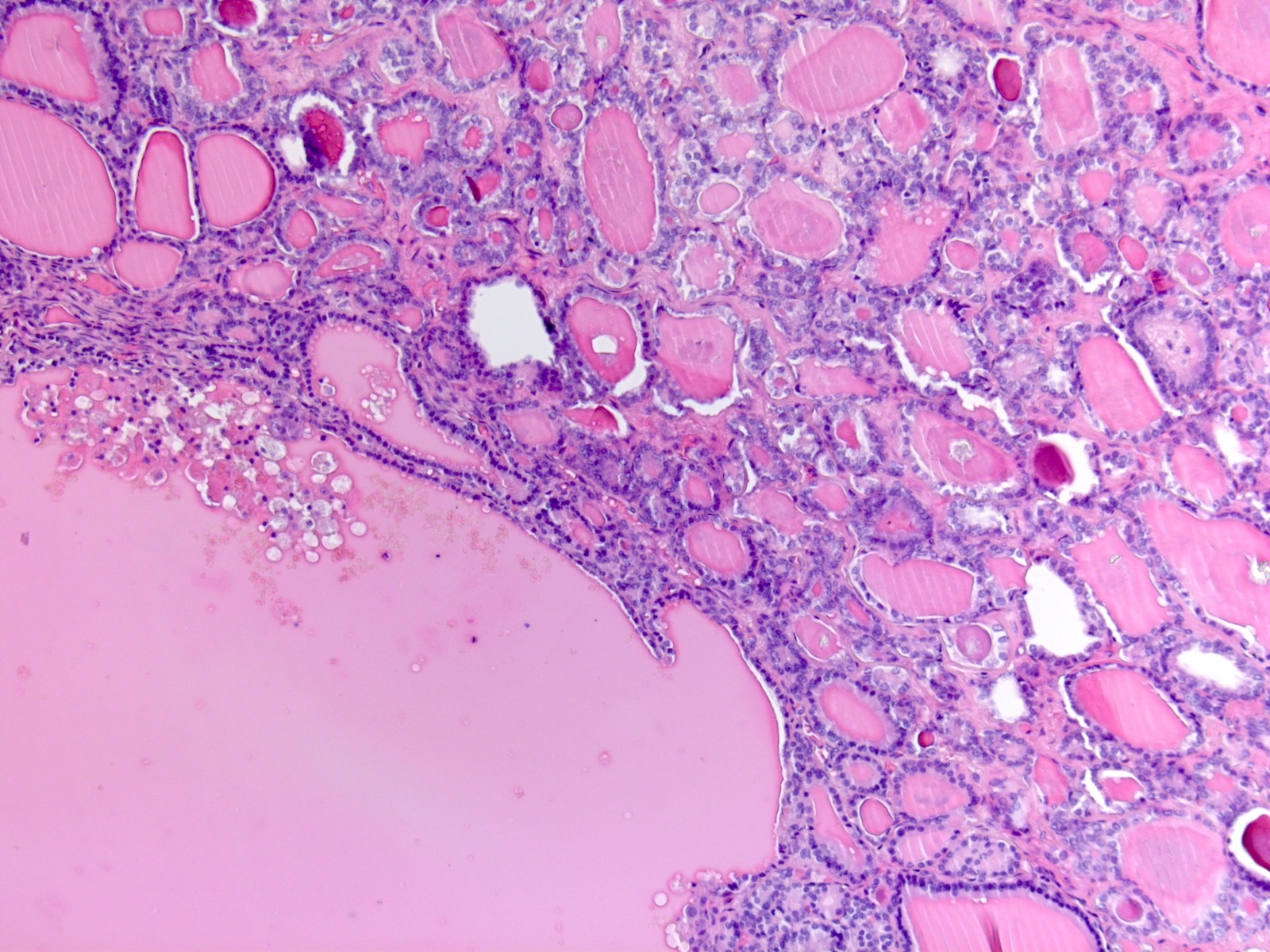
Microscopic (histologic) description
- Variably sized macro and microfollicles often containing colloid
- Other architectural patterns include solid areas composed of cells with clear to oxyphilic cytoplasm, trabeculae, cords and pseudotubular structures
- Rarely, stroma in between follicles may be fibrotic or edematous; peripheral stromal leutinization may also be seen
- Adenomatous hyperplasia or proliferative changes may be seen, such as areas of densely packed follicles or papillary formations lacking nuclear features of papillary thyroid carcinoma
- Birefringent calcium oxalate crystals may be seen in colloid
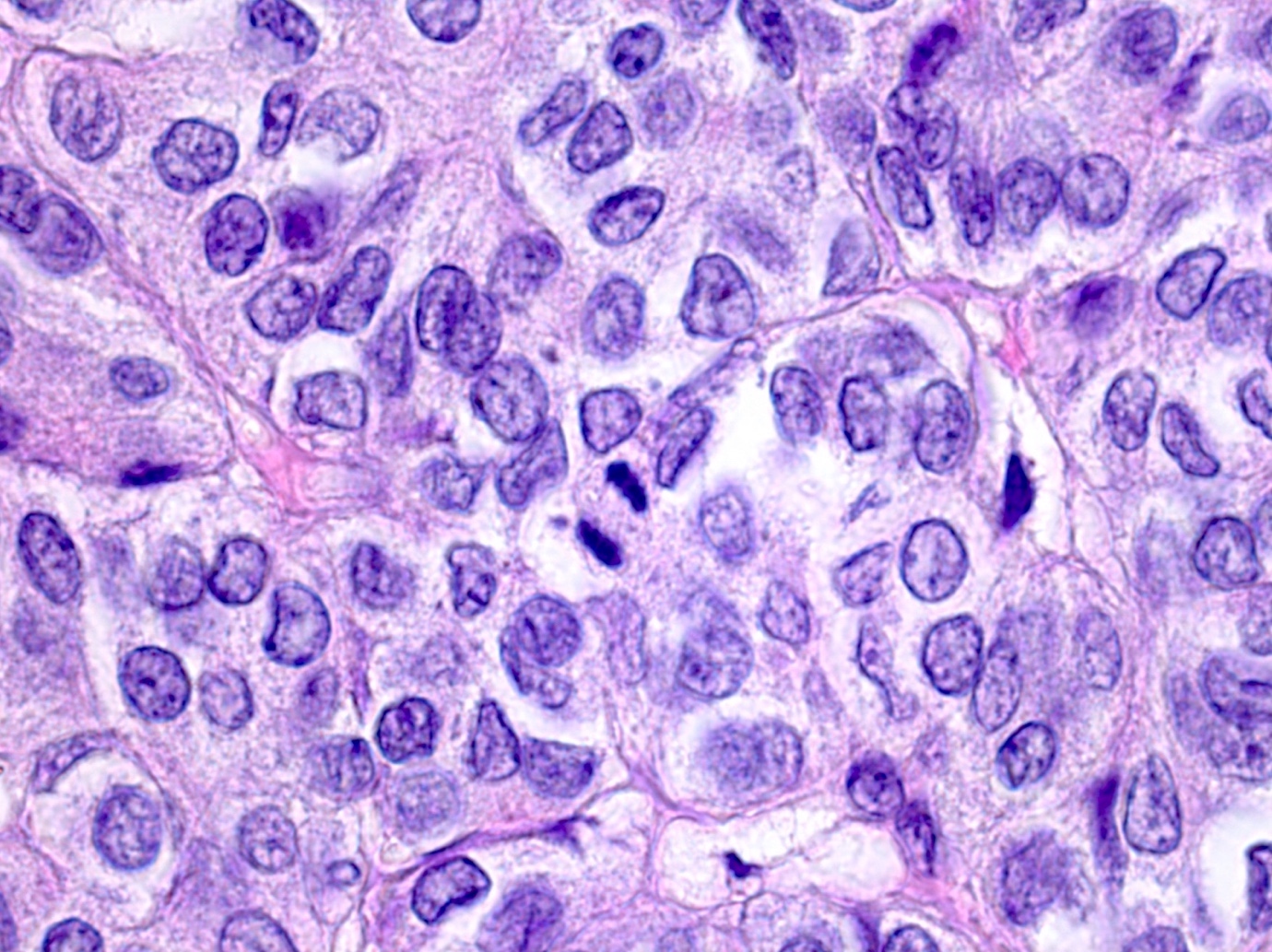
- Most commonly associated malignancy is papillary thyroid carcinoma, cytologically characterized by crowded and overlapping elongated nuclei with irregular contours and chromatin clearing, usually with papillary or follicular architecture
- Follicular carcinoma is the second most common malignancy; since ovarian lesions typically lack capsule, demonstration of tumor invasion into surrounding ovarian tissue, vascular invasion or metastases is needed as evidence of malignancy
- Uncommonly associated with the more recently described highly differentiated follicular carcinoma of ovarian origin, characterized by extraovarian spread of thyroid elements histologically resembling nonneoplastic thyroid tissue (Int J Gynecol Pathol 2008;27:213)
- Undifferentiated (anaplastic) carcinoma and medullary carcinoma have also been described in association with struma ovarii
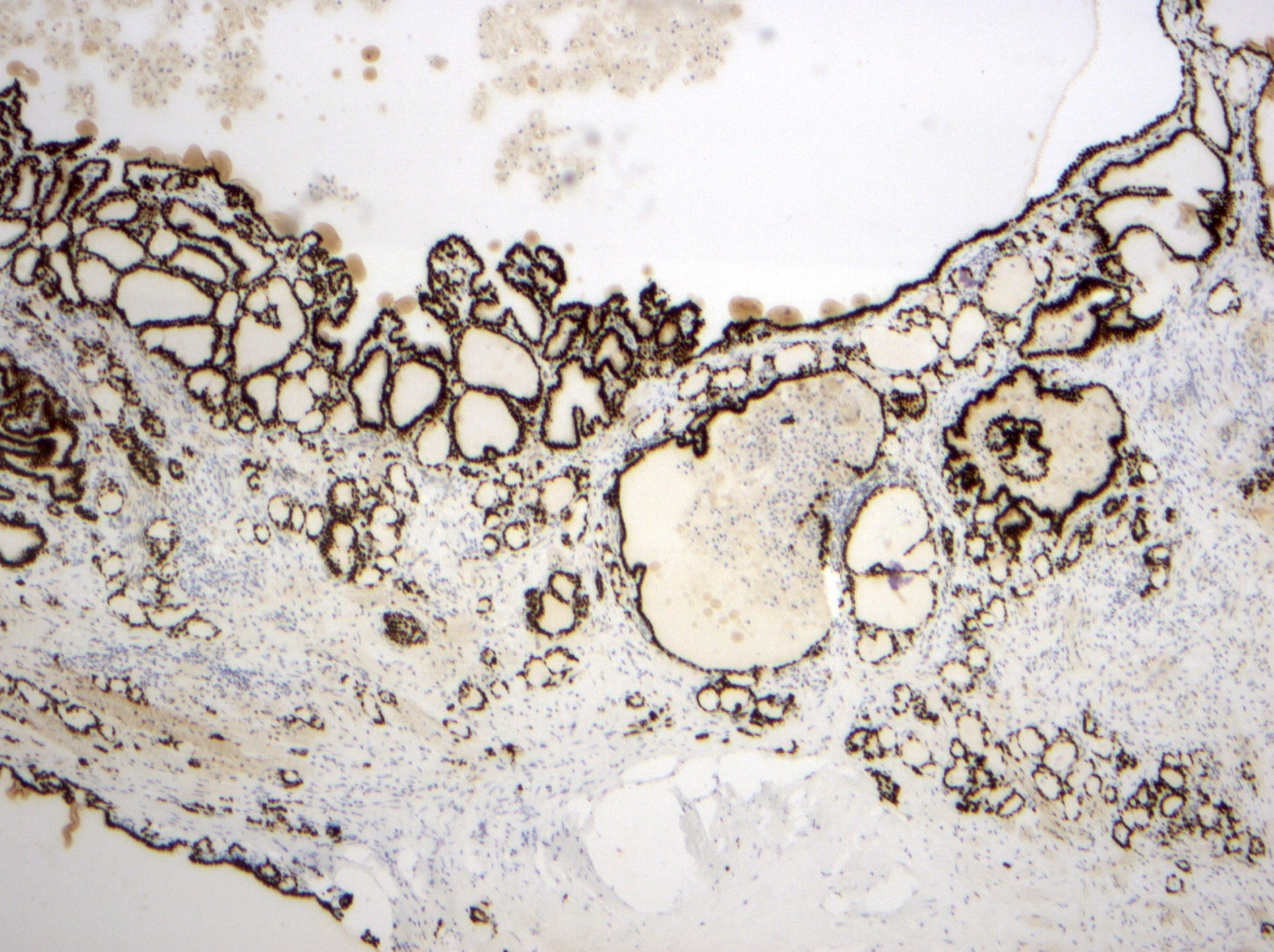
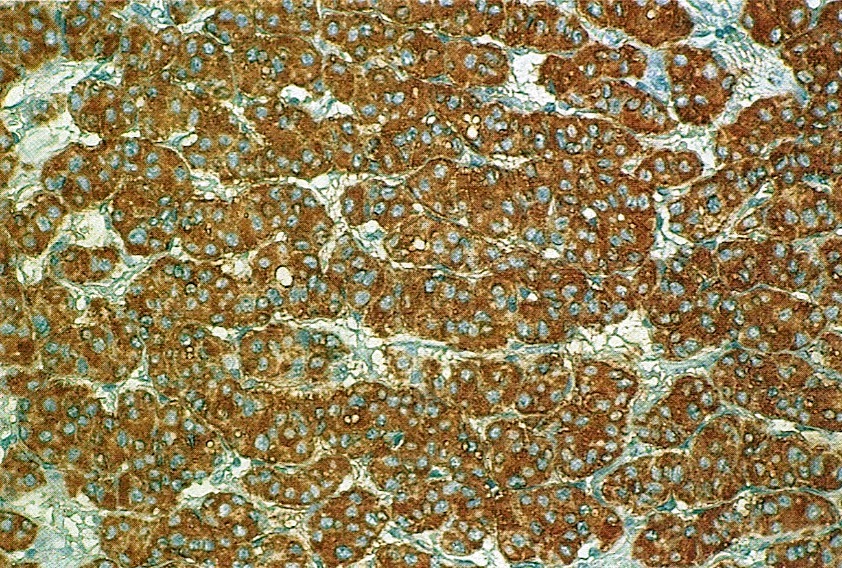
Microscopic (histologic) images
Contributed by Sharon Song, M.S., M.D., Kseniya Korchagina, M.D. and AFIP
Cytology description
- Flattened to cuboidal / columnar cells with small round to oval nuclei, even chromatin and pale to eosinophilic cytoplasm (Crum: Gynecologic and Obstetric Pathology, 3rd Edition, 2017)
- Clear cell change may occasionally be seen
Positive stains
Molecular / cytogenetics description
- BRAF mutations and RET / PTC rearrangements may be seen in papillary thyroid carcinomas arising from a struma ovarii (Am J Surg Pathol 2007;31:1337, Endocr Pathol 2007;18:182)
Sample pathology report
- Ovary and fallopian tube, left, salpingo-oophorectomy:
- Struma ovarii, 4.5 cm
- Ovary and fallopian tube, left, salpingo-oophorectomy:
- Papillary thyroid carcinoma, follicular and papillary growth patterns, 1.1 cm, arising in a background of struma ovarii
Differential diagnosis
- Metastatic thyroid carcinoma to the ovary:
- Clinical history of primary thyroid carcinoma
- Strumal carcinoid:
- Corded, trabecular or follicular architecture with salt and pepper nuclear chromatin pattern and occasional eosinophilic granules
- Positive staining for TTF1, PAX8, thyroglobulin (in follicular component) and neuroendocrine markers chromogranin, synaptophysin, CD56 and neuron specific enolase
- Ovarian clear cell carcinoma:
- Tubulocystic, papillary and solid growth patterns with cytologically atypical cells, often hobnailing into cysts
- Positive staining for HNF1β, Napsin A and AMACR
- Negative for TTF1, thyroglobulin
- Sex cord stromal tumor:
- Tubular, trabecular or corded growth without eosinophilic secretions
- Positive staining for inhibin A, calretinin and SF1
- Negative for TTF1, PAX8 (usually negative, Appl Immunohistochem Mol Morphol 2011;19:293), thyroglobulin
- Melanoma:
Practice question #1
What type of crystals may be seen in struma ovarii?
- Calcium carbonate
- Calcium oxalate
- Calcium phosphate
- Triple phosphate
- Tyrosine
Practice answer #1
Practice question #2
Practice answer #2
B. CA125 is a widely accepted biomarker for ovarian cancers that can also be elevated in many other conditions, such as menstruation, endometriosis, pregnancy, pelvic inflammatory disease, fibroids, liver disease and tumors of the endometrium, breasts and lungs. It can be increased in up to 30% of struma ovarii.
Comment Here
Reference: Struma ovarii
Comment Here
Reference: Struma ovarii