Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Peripheral smear description | Peripheral smear images | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khanlari M, Chapman J. Follicular-usual. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomafollicularnodalusual.html. Accessed April 28th, 2024.
Definition / general
- Mature B cell neoplasm
- Malignancy of germinal center B cells (centrocytes and centroblasts)
- Biologically and histopathologically heterogeneous
- Indolent lymphoma
Essential features
- Characterized by at least partial follicular (nodular) distribution
- Entirely diffuse pattern in rare cases
- Cytologic composition (centrocyte / centroblast) used for lymphoma grading
- More important than pattern (follicular / diffuse) in diagnosis / prognosis
- Germinal center marker expression
Terminology
- Obsolete names:
- Brill-Symmers disease (Am J Pathol 1942;18:381)
- Nodular lymphoma (Rappaport classification) (Cancer Res 1966;26:1082)
- Centroblastic / centrocytic lymphoma (Kiel classification) (Lennert: History of the European Association for Haematopathology, 1st Edition, 2006)
- Follicular center lymphoma (REAL classification) (Blood 1994;84:1361)
ICD coding
Epidemiology
- ~5% of all hematologic neoplasms
- Second most common non-Hodgkin lymphoma
- ~20 - 25% of all new non-Hodgkin lymphoma diagnoses in Western countries
- Incidence differs among geographical regions and ethnic groups
- 80% of all follicular lymphomas are systemic nodal tumors
- Age standardized incidence: 2 - 4 per 100,000 person years (NIH: Follicular Lymphoma - Cancer Stat Facts [Accessed 5 February 2020])
- M:F = variable (1:1.7 in most references)
- Median age range: 60 - 65 years
- References: Ann Oncol 1998;9:717, Blood 1997;89:3909
Sites
- Cervical and inguinal lymph nodes are more frequently affected
- Extranodal sites that are commonly involved include bone marrow, spleen, liver and peripheral blood
Pathophysiology
- Bone marrow event (Nat Rev Dis Primers 2019;5:83)
- t(14;18) (q32;q21) translocation: repair failure during V(D) J recombination
- t(14;18) (q32;q21) IGH / BCL2: 85% of follicular lymphomas
- BCL2 expression in precursor follicular lymphoma cells: increase survival in germinal center
- Germinal center events
- Retain germinal center functionality (e.g. BCL6)
- Class switch recombination with retention of IgM / IgD surface expression
- This phenomenon is called allelic paradox
- Postgerminal center events
- Chromosomal alterations
- Molecular changes
- Chromatin modification (KMT2D, EZH2, CREBBP, ARID1A, MEF2B, EP300)
- B cell receptor signaling (CARD11, IgHV, IgLV)
- Cell cycle regulation (RB1, CDK4)
- Transcription factor (FOXO1, MEF2B)
- Immune evasion (EPHA7, TNFRSF14, CREBBP)
Etiology
- Unknown etiology
- Family history is important (especially first degree relatives) (Br J Haematol 2009;146:91)
- Environmental factors: exposure to pesticides and herbicides
- t(14;18) alone is not sufficient to cause lymphoma (Haematologica 2014;99:802)
- Natural history of the disease starts in bone marrow and not germinal center (GC)
Diagrams / tables
| World Health Organization grading of follicular lymphoma | |||
| Grade | Definition | Pattern | Immunohistochemistry and cytogenetics |
| 1 | 0 - 5 centroblasts/high power field | Follicular or diffuse |
IHC: CD10: + (95 - 100%) BCL2: + (85 - 90%) FISH: BCL2 translocation: + (80 - 90%) BCL6 rearrangement: + (3%) Ki67: < 20%* |
| 2 | 6 - 15 centroblasts/high power field | Follicular or diffuse | |
| 3A | > 15 centroblasts/high power field Centrocytes present | Follicular If diffuse component: Reported as diffuse large B cell lymphoma and follicular lymphoma (% of each component is reported); correlate with clinical features and overall grade in cases with small areas of diffuse pattern |
IHC: CD10: + (80 - 95%) BCL2: + (50 - 75%) FISH: BCL2 translocation: + (60 - 70%) BCL6 rearrangement: + (30 - 40%) Ki67: > 20% |
| 3B | > 15 centroblasts/high power field Lack centrocytes | Follicular If diffuse component: Reported as diffuse large B cell lymphoma and follicular lymphoma (% of each component is reported) |
IHC: CD10: + (40 - 85%) BCL2: + (45 - 75%) FISH: BCL2 translocation: + (15 - 30%) BCL6 rearrangement: + (40 - 50%) CD10-IRF4/MUM1+: common Ki67: > 50% |
Notes:
- IHC: immunohistochemistry
- FISH: fluorescence in situ hybridization
- High power field of 0.159 mm2 (40× objective)
- Follicular: > 75% (proportion follicular %)
- Diffuse: 0% (proportion follicular %)
- * ~20% of low grade follicular lymphomas have a high proliferation (Ki67) rate (Am J Surg Pathol 2005;29:1490)
- References: Arch Pathol Lab Med 2018;142:1330, Haematologica 2018;103:1182, Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017
Clinical features
- Indolent disease
- Localized diseases 10 - 20%
- Widespread nodal disease is common
- Disseminated (stages III - IV) at diagnosis
- Follows a chronic relapsing course
- A subset progress rapidly and transform to an aggressive lymphoma
- Diffuse large B cell lymphoma
- Double hit lymphoma
- B lymphoblastic leukemia / lymphoma (TdT positive)
- Follicular lymphoma can relapse as classic Hodgkin lymphoma
- Reference: Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017
Diagnosis
- Symptoms: fatigue, fever or night sweats, weight loss or recurrent infections
- Most patients with follicular lymphoma have no obvious symptoms of the disease
- Tissue biopsy (lymph node / extranodal sites)
- Needle biopsy (both core needle biopsy and fine needle aspiration biopsy)
- Peripheral blood exam / bone marrow biopsy (especially in staging)
- Reference: Nat Rev Dis Primers 2019;5:83
Laboratory
- Abnormal laboratory findings are uncommon
- Anemia: 10%
- Rarely leukopenia / thrombocytopenia
- Leukemic phase with lymphocytosis: < 5%
- Increase in lactate dehydrogenase (LDH) and beta 2 microglobulin: ~15%
- Reference: Medeiros: Tumors of the Lymph Nodes and Spleen, 4th Series, 2017
Radiology description
- Widespread lymphadenopathy
Prognostic factors
- Median overall survival of > 15 years
- 5 year progression free survival of ~60%
- Follicular lymphoma frequently transforms into an aggressive subtype
- Resembling germinal center derived diffuse large B cell lymphoma
- In 25 - 35% of follicular lymphomas
- Short remission after treatment: poor prognosis (J Clin Oncol 2015;33:2516)
- The Follicular Lymphoma International Prognostic Index (FLIPI):
- Age (≥ 60 versus < 60 years)
- Ann Arbor stage (III - IV versus I - II)
- Hemoglobin level (< 120 versus ≥ 120 g/L)
- Number of nodal areas involved (> 4 versus ≤ 4)
- Serum lactate dehydrogenase (LDH) level (above normal versus normal or below)
- FLIPI2 system (patients treated with rituximab)
- High serum beta 2 microglobulin
- Largest involved lymph node > 6 cm
- Bone marrow involvement
- Hemoglobin < 12 g/dL
- Age > 60 years
- M7 FLIPI (FLIPI combined with 7 genes) better identify the risk
- Pathologic adverse prognostic factors
- High histologic grade and diffuse areas > 25% with predominance of large cells (diffuse large B cell lymphoma)
- High proliferation index
- Low grade follicular lymphoma with high proliferation index behave similar to high grade follicular lymphoma
- Partial involvement by follicular lymphoma has better prognosis
- Cytogenetic adverse prognostic factors
- Complex karyotype
- Both BCL2 and a MYC rearrangement
- Del6q25-27; del17p and mutations of TP53
Case reports
- 55 year old woman presented with a 6 month history of a slow growing mass in her right neck diagnosed as floral variant of follicular lymphoma (Am J Hematol 2011;86:503)
- 64 year old woman diagnosed with follicular lymphoma grade 1 and endometrioid carcinoma transformed to double hit lymphoma during chemotherapy (Int J Hematol 2019;110:375)
- Low grade follicular lymphoma with evolution to a blastic phase (Am J Clin Pathol 1985;83:681)
- Transformation of primary extranodal marginal zone B cell lymphoma of the uterus into a nodal follicular lymphoma grade IIIB (Ann Hematol 2019;98:797)
Treatment
- Stage I or contiguous stage II (nonbulky)
- Localized radiotherapy
- Stage I or stage II (bulky) or noncontiguous stage II
- Anti-CD20 monoclonal antibody with or without chemotherapy or radiotherapy
- Observation, if clinically indicated
- Stage III or stage IV
- Anti-CD20 monoclonal antibody with or without chemotherapy (with or without maintenance anti-CD20)
- Observation, if clinically indicated
- Reference: Nat Rev Dis Primers 2019;5:83
Gross description
- Lymph node: vaguely nodular pattern in cut section with bulging
- Spleen: white pulp expansion
- Reference: Medeiros: Tumors of the Lymph Nodes and Spleen, 4th Series, 2017
Frozen section description
- Same criteria applied in microscopic evaluation
- Cytogenetics, flow cytometry, preparation of imprints should be considered
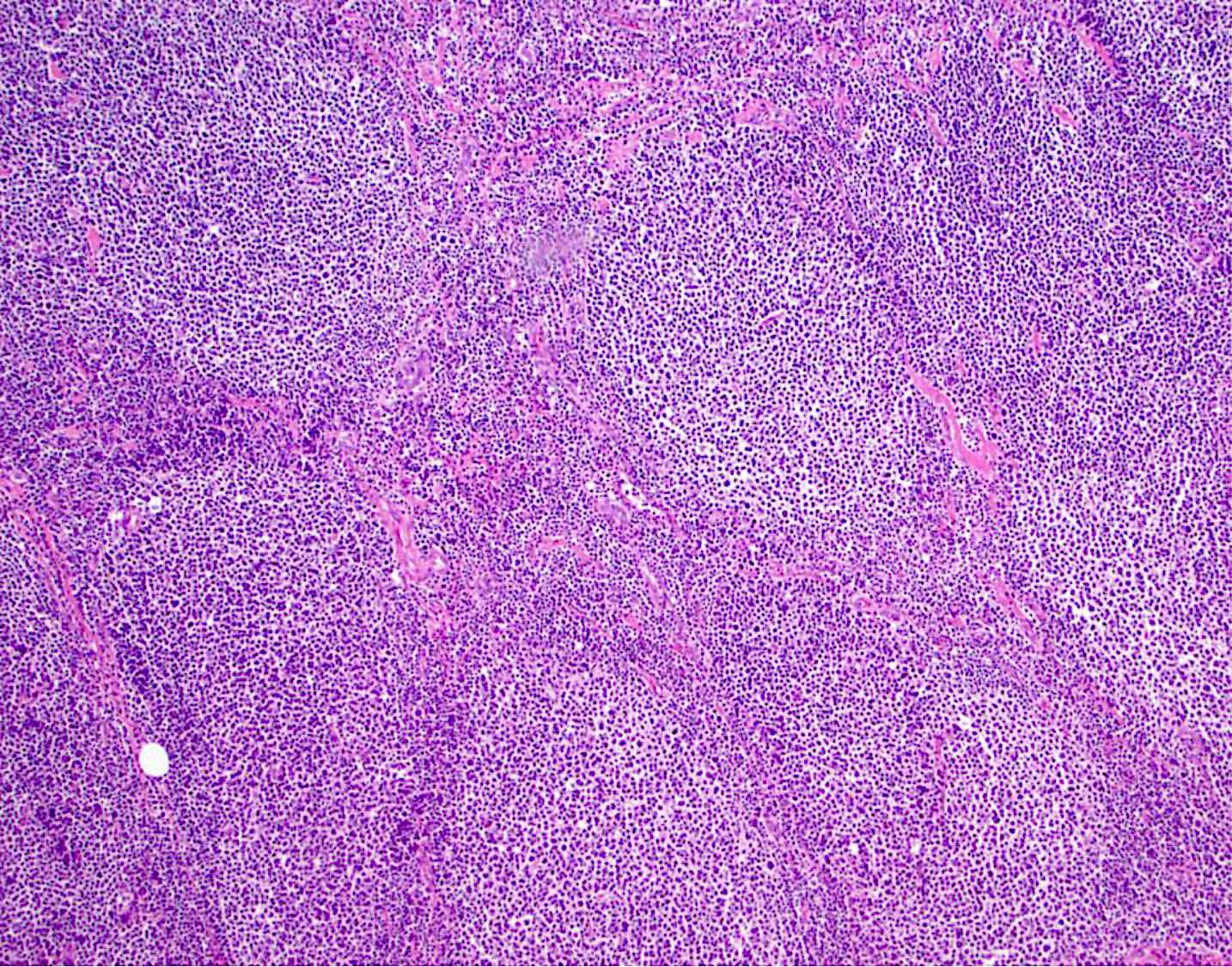
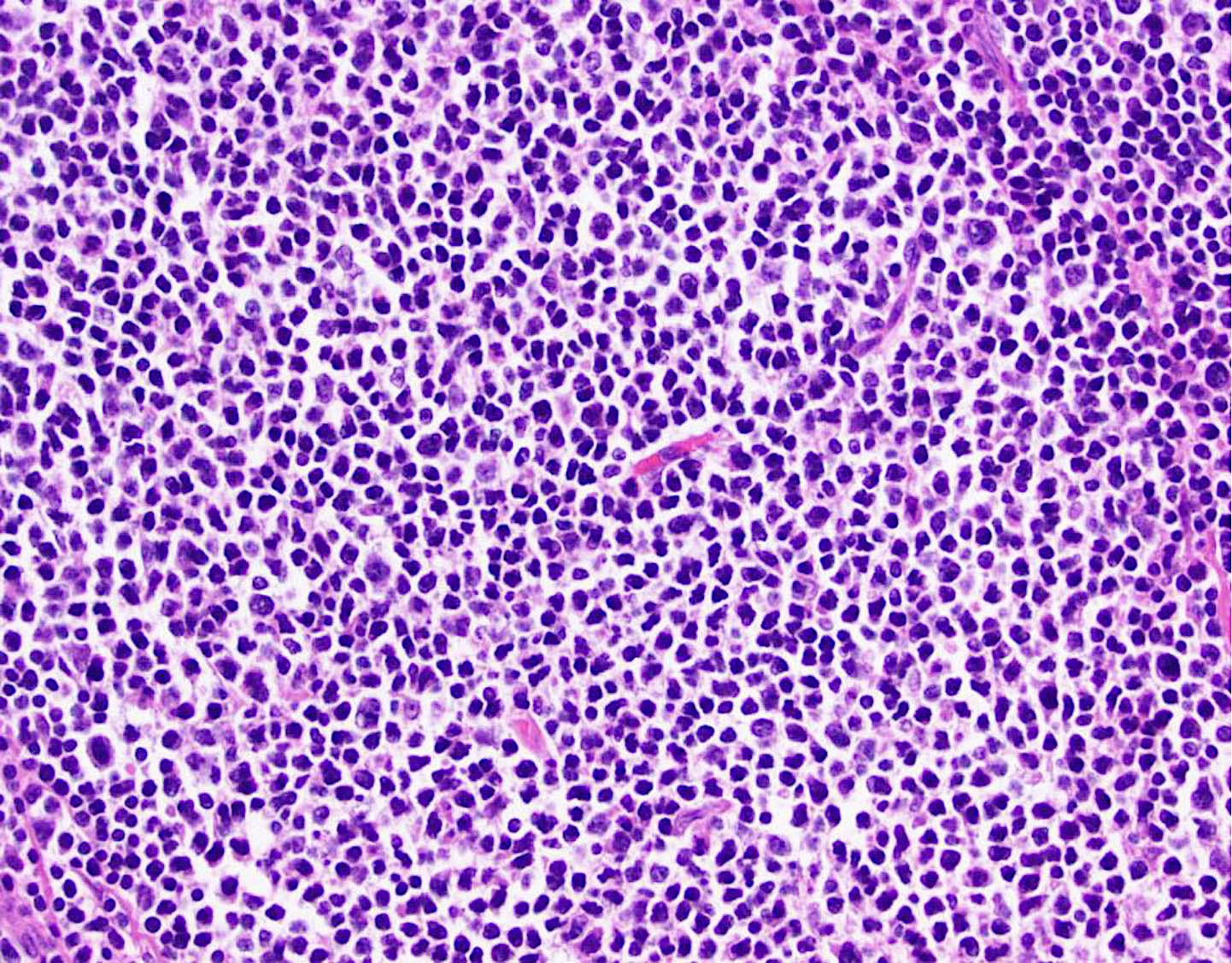
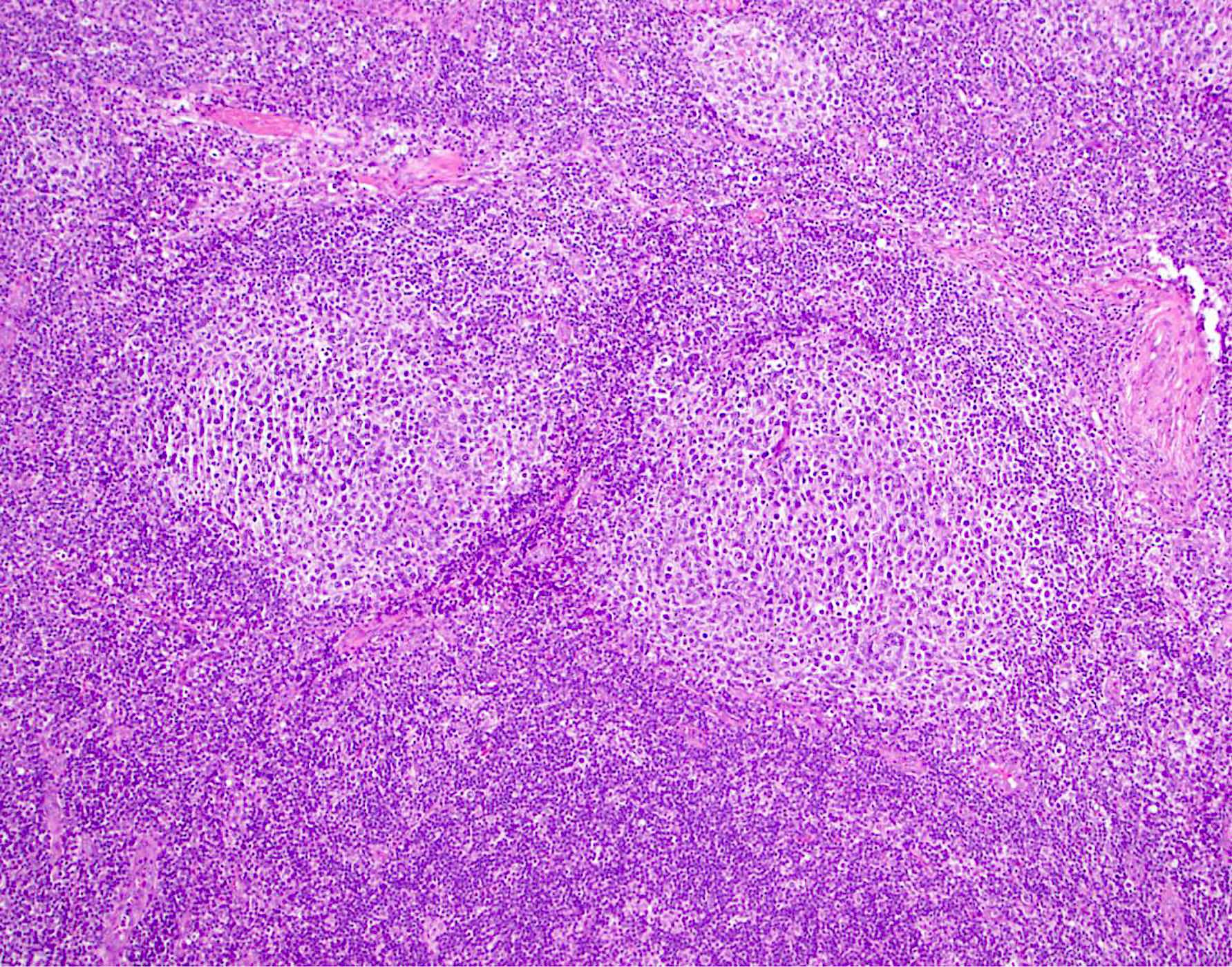
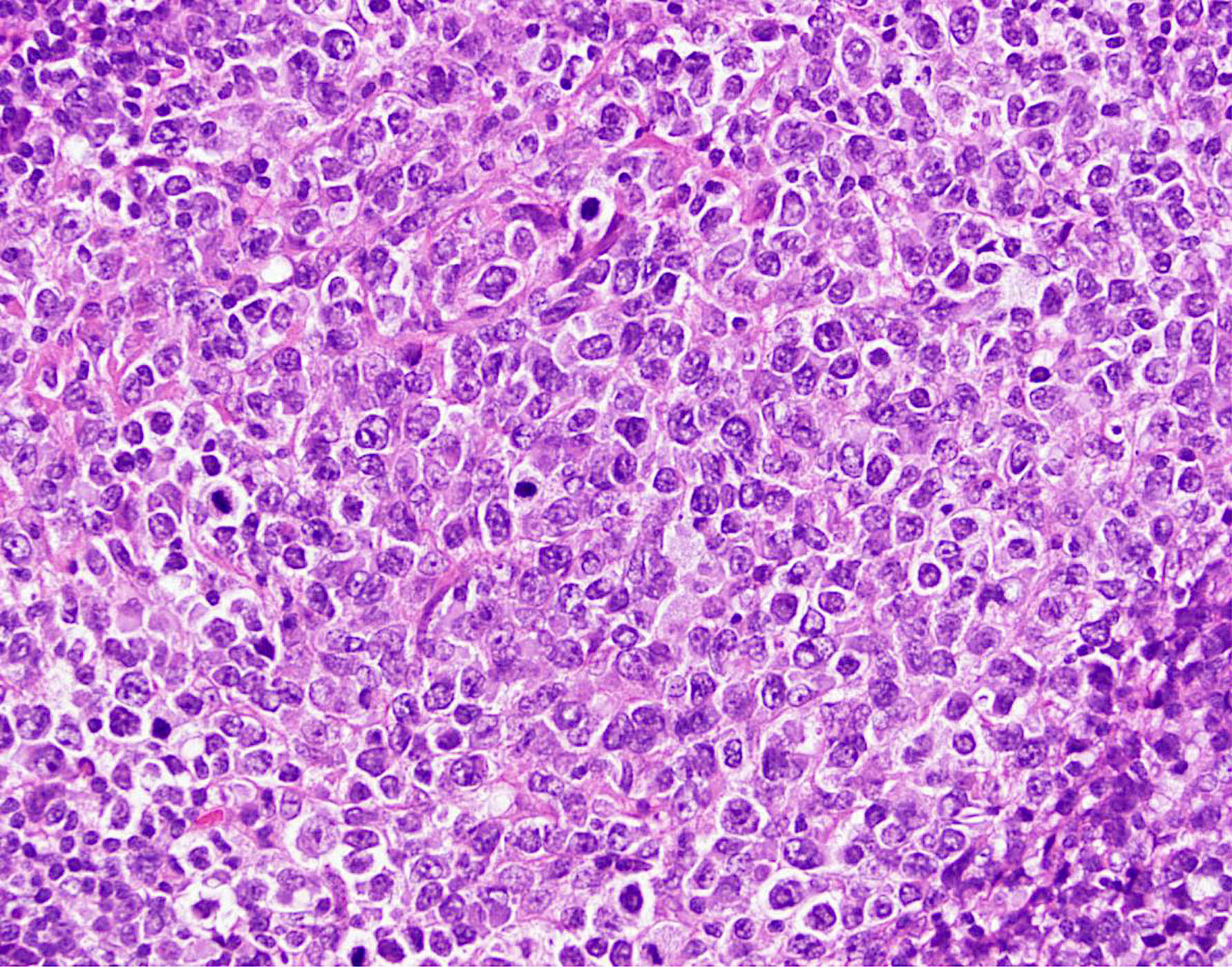
Microscopic (histologic) description
- Lymph node
- Partial or complete effacement of lymph node
- Neoplastic follicles:
- Similarly sized
- Nonpolarized
- Attenuated or absent mantle zones
- Lack tingible body macrophages
- Composed of centrocytes or centroblasts
- Infrequent mitoses (except grade 3)
- With or without sclerosis
- Grading: proportion of centroblasts defines the grade
- Follicular dendritic cell meshworks are absent in diffuse areas
- Partial involvement by follicular lymphoma
- Both neoplastic and reactive follicles are present
- Lymph node architecture is partially preserved
- Floral variant
- Irregular neoplastic follicles
- Darker mantle zone lymphocytes penetrate into neoplastic follicles
- Grade 3 in most cases
- Resembles progressively transformed germinal center
- Signet ring cell variant (differential diagnosis: carcinoma)
- Other uncommon variants (refer to unusual variants of follicular lymphomas)
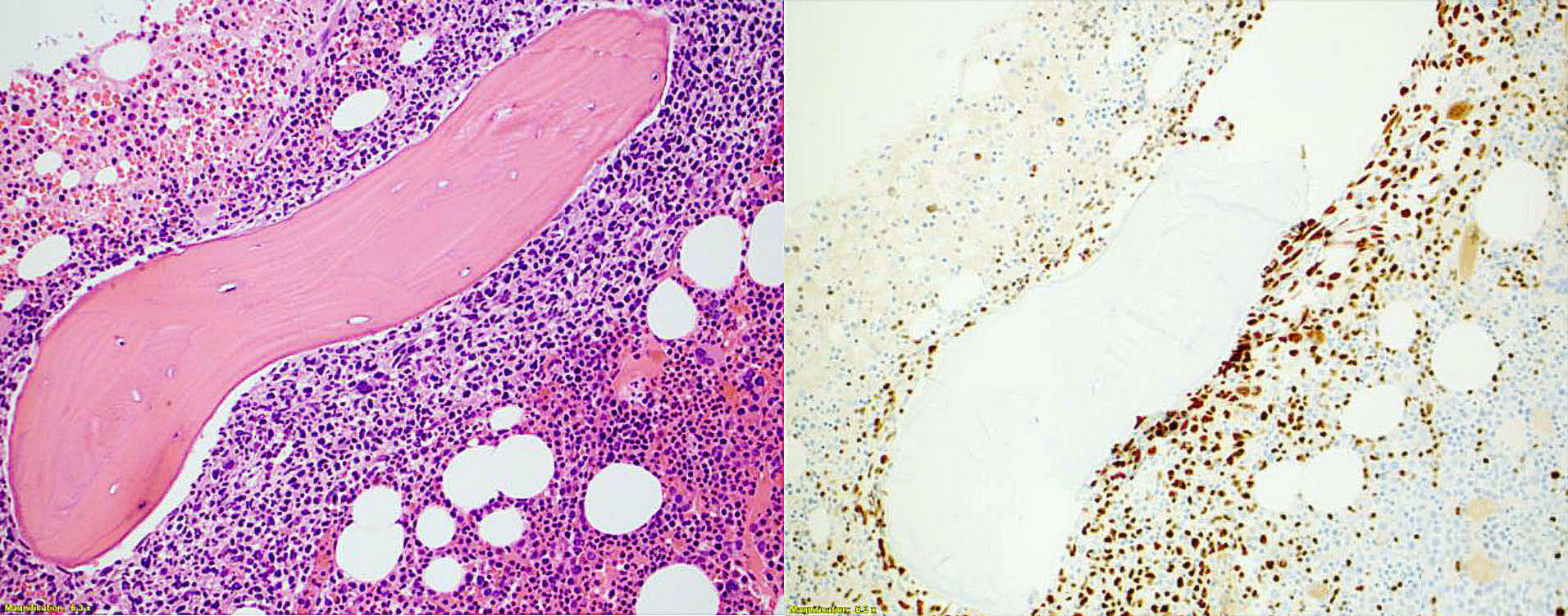
- Bone marrow
- Focal or extensive involvement
- Paratrabecular aggregates of lymphoma cells
- With or without interstitial or diffuse patterns
- Pure follicular pattern in ~5% (Am J Clin Pathol 2002;118:780)
- Liver
- Portal tracts are preferentially involved
- Large nodule in parenchyma in extensive disease
- Spleen
- Preferential involvement of white pulp
- Two patterns
- Expansion of the white pulp
- Relatively preserved architecture
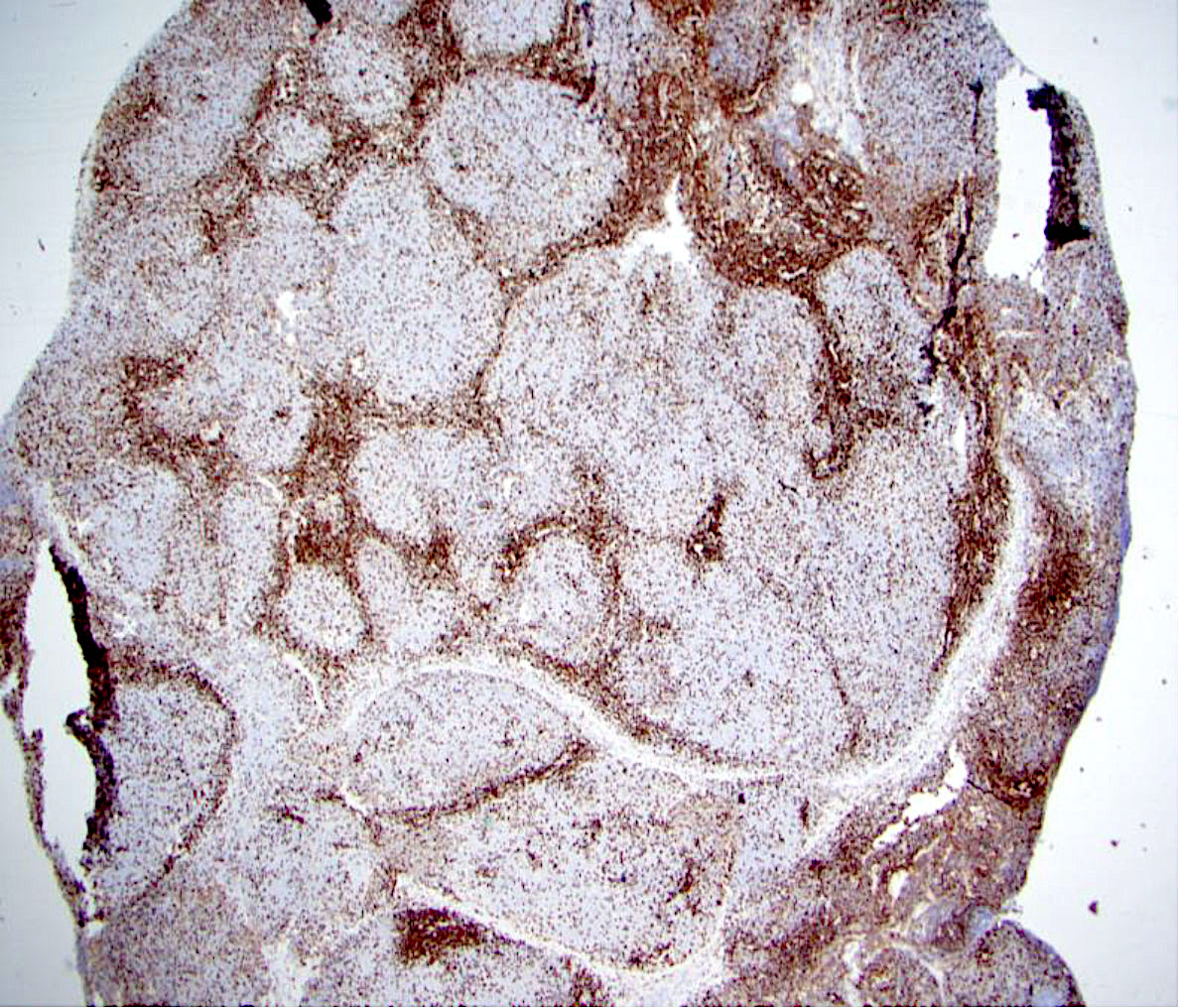
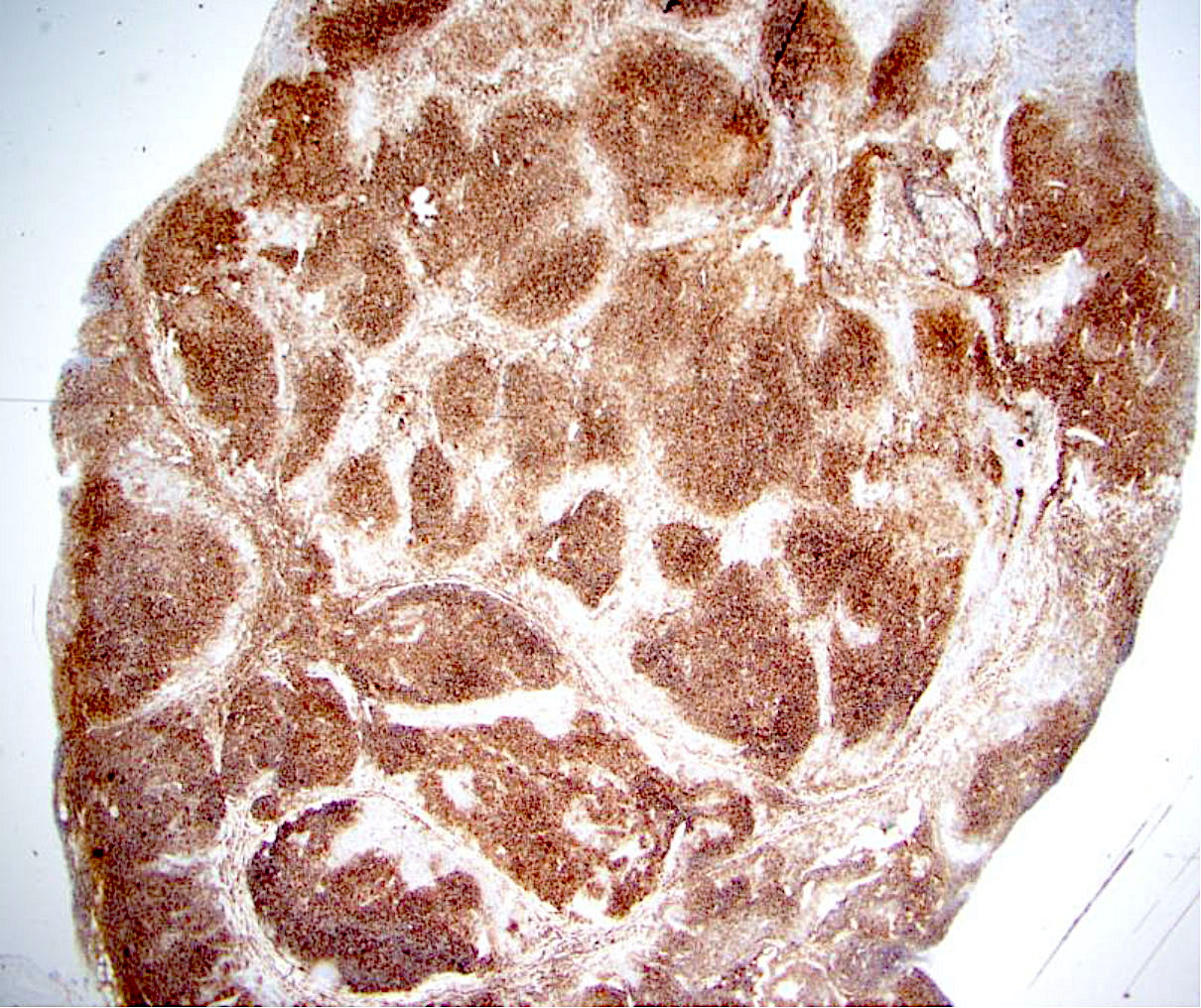
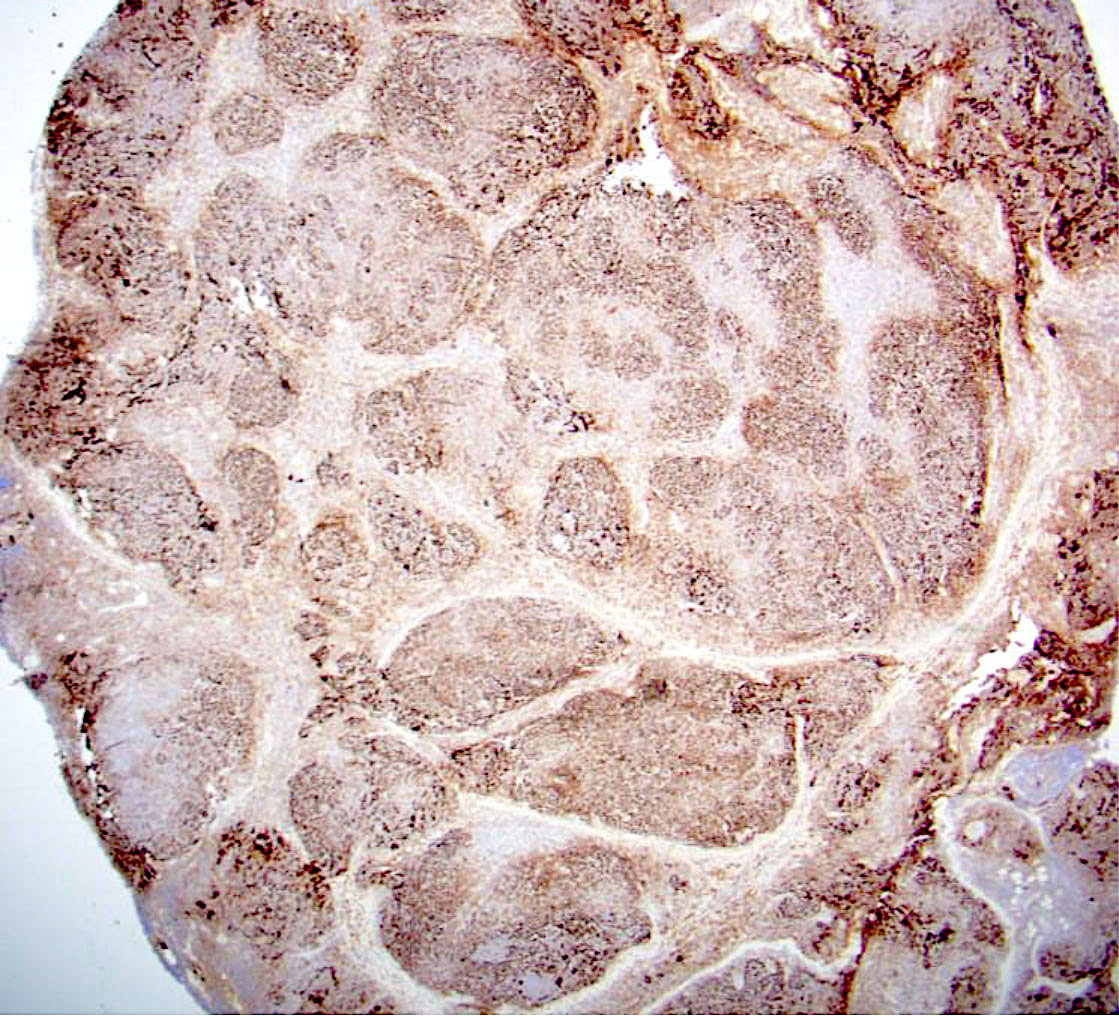
Microscopic (histologic) images
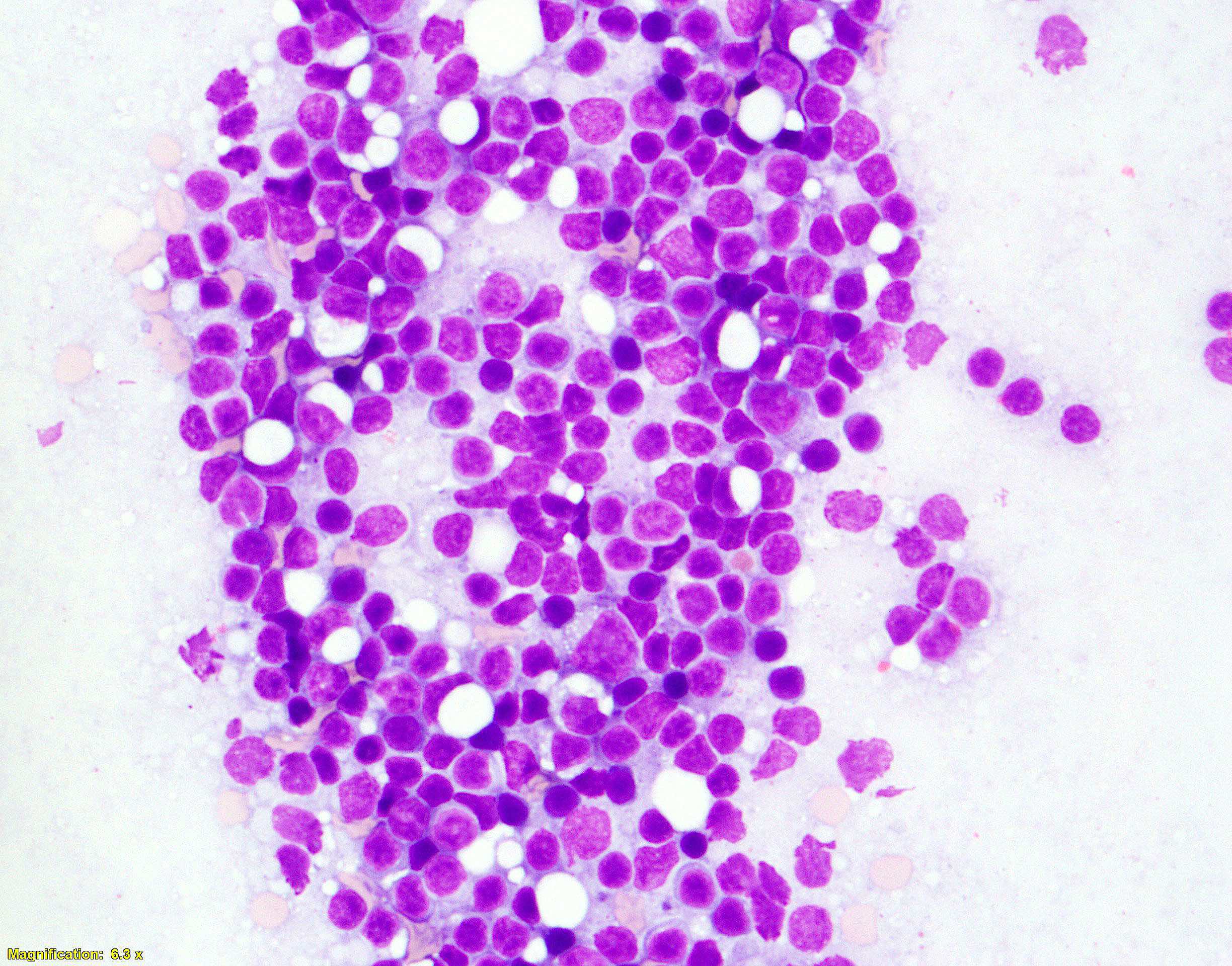
Cytology description
- Variable mixture of centrocytes and centroblasts
- Centrocytes
- Small to large
- Angulated nuclei
- Dense chromatin
- Scant cytoplasm
- Centroblasts
- Large cells with oval nuclei
- Vesicular chromatin
- 1 - 3 nucleoli
- Moderate cytoplasm
- > 3 times the size of lymphocytes
- Differentiate from follicular dendritic cells
- Large round nuclei
- Dispersed, nearly clear chromatin
- Single eosinophilic nucleolus
- Indistinct cytoplasm
- Absence / rare tingible body macrophages
- Centrocytes
- Reference: Jaffe: Hematopathology, 2nd Edition, 2016
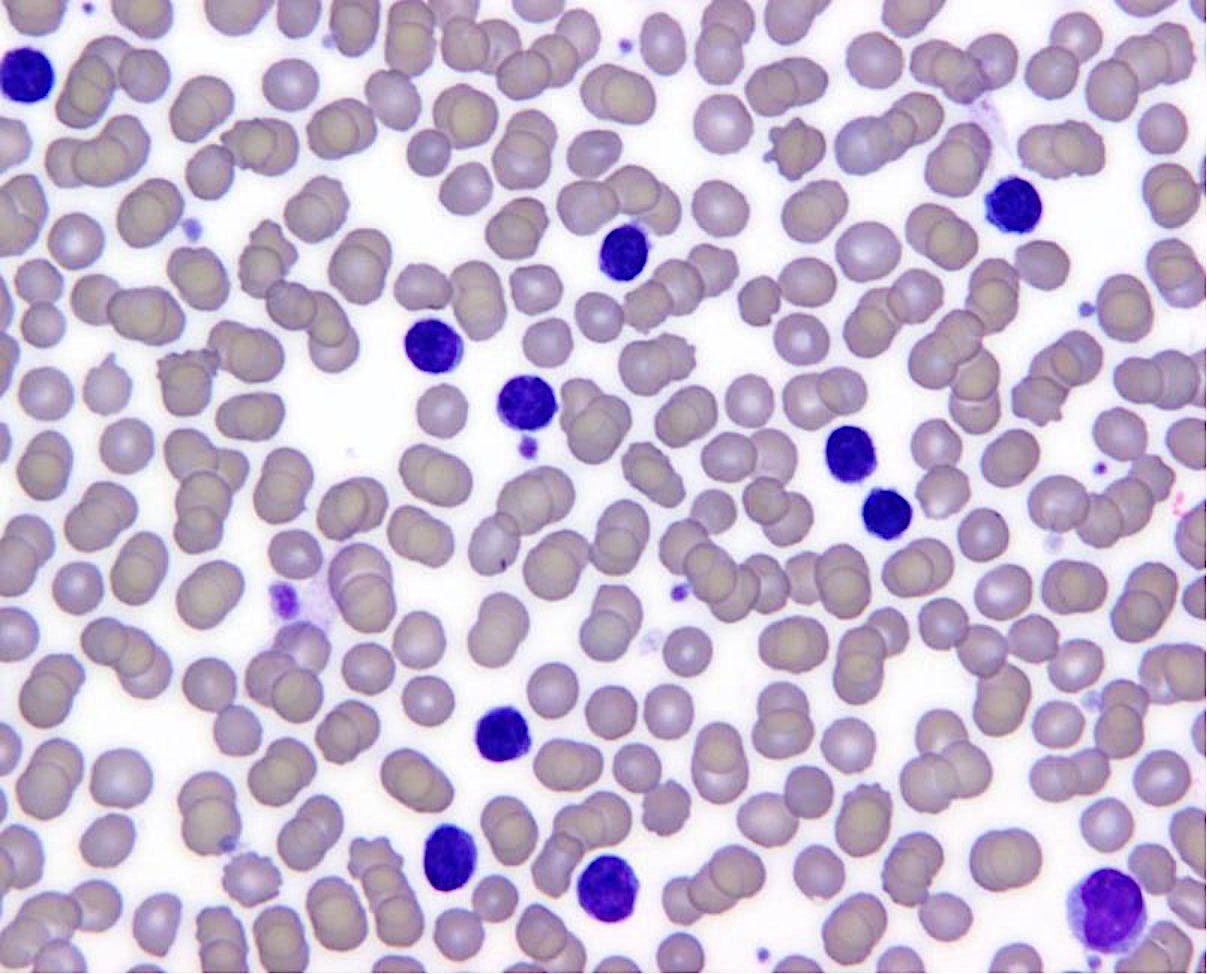
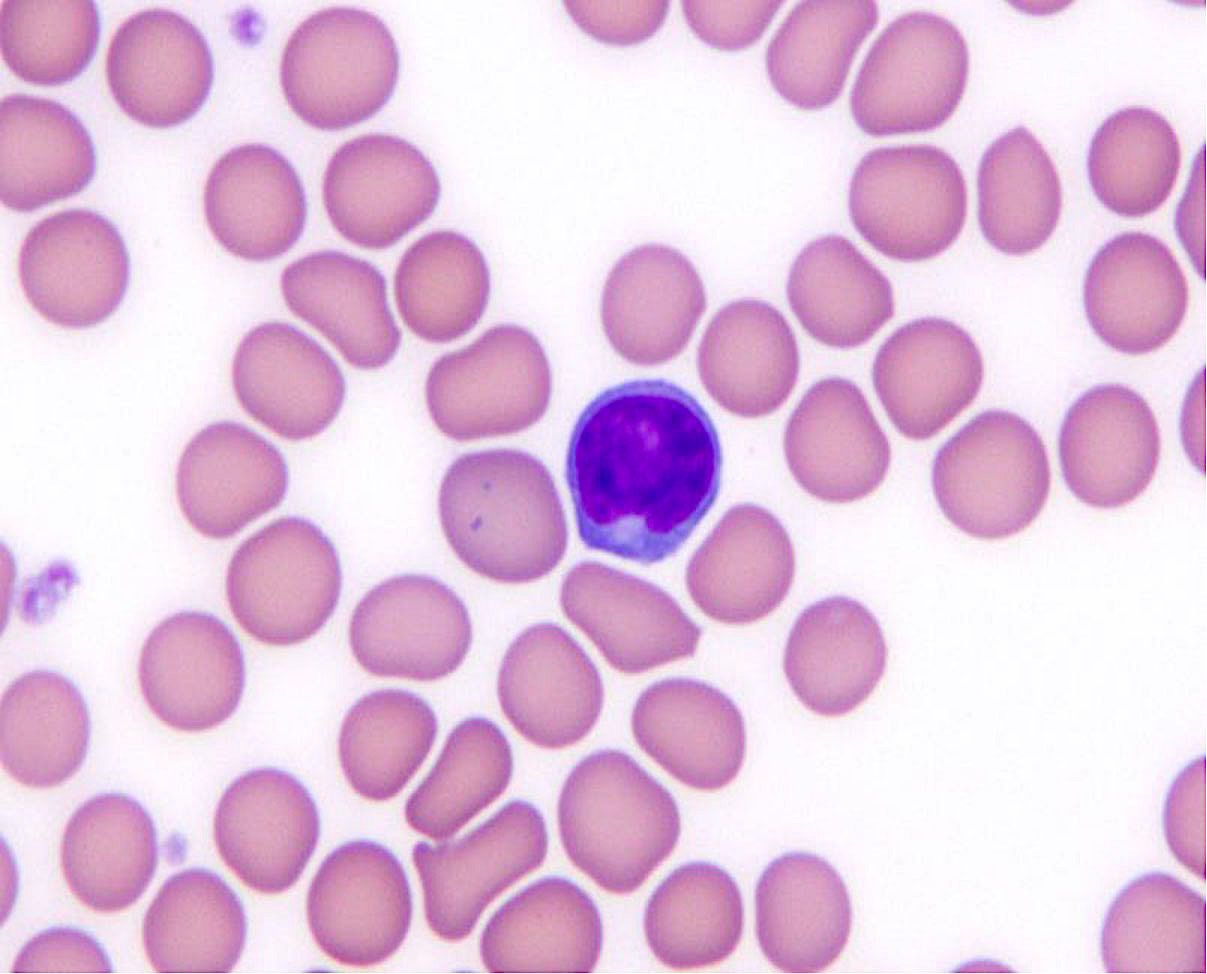
Peripheral smear description
- Low level involvement is common (~90%)
- Absolute lymphocytosis with high count, 5 - 10% of cases (Br J Haematol 2014;164:659)
- Neoplastic cells are small to intermediate in size
- Highly indented nuclei, known as buttock cells
Positive stains
- Monotypic surface Ig
- lgM with or without lgD is the most common surface Ig
- Pan-B cell markers: CD19, CD20, CD22 and CD79a
- Germinal center markers: CD10, BCL6, HGAL, LMO2
- BCL2 (variable)
- Positive in 85 - 90% of follicular lymphoma grades 1 and 2
- It may be negative in grade 3
- False negative: mutations of the BCL2 epitope (anti-BCL2 antibody used)
- Follicular dendritic cell meshworks in follicles
- Proliferation rate of follicular lymphomas assessed by Ki67
- Percentage correlates with grade
- ~20% of low grade follicular lymphomas have high proliferation rate (> 40%)
- These follicular lymphomas appear to behave more aggressively, similar to grade 3A follicular lymphoma
- Report as follicular lymphoma grade 1 to 2 with a high proliferation fraction
- Assess Ki67 in follicles
- If interfollicular area > follicles, estimate Ki67 based on average for entire neoplasm
- Reference: Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017
Negative stains
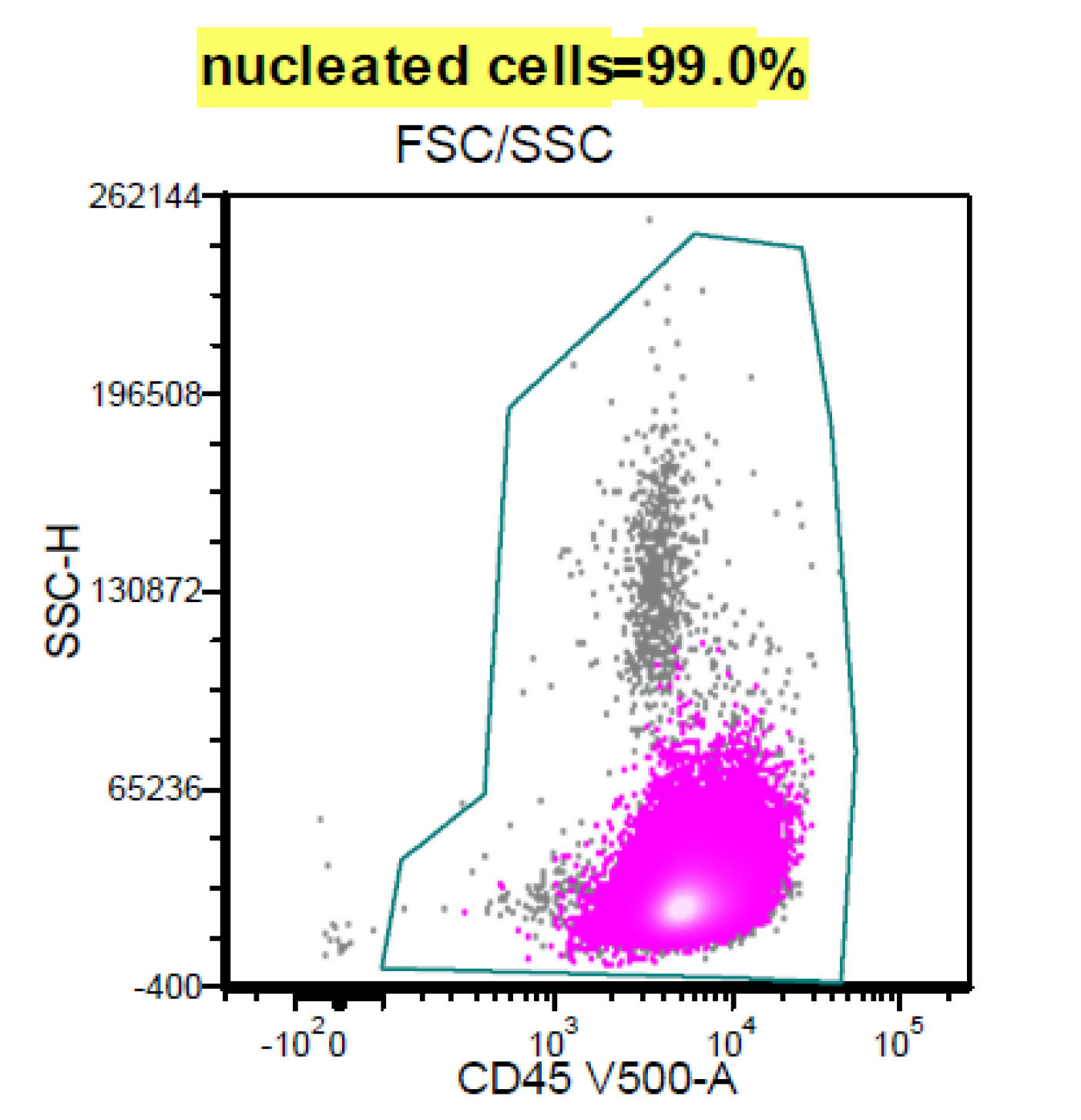
Flow cytometry description
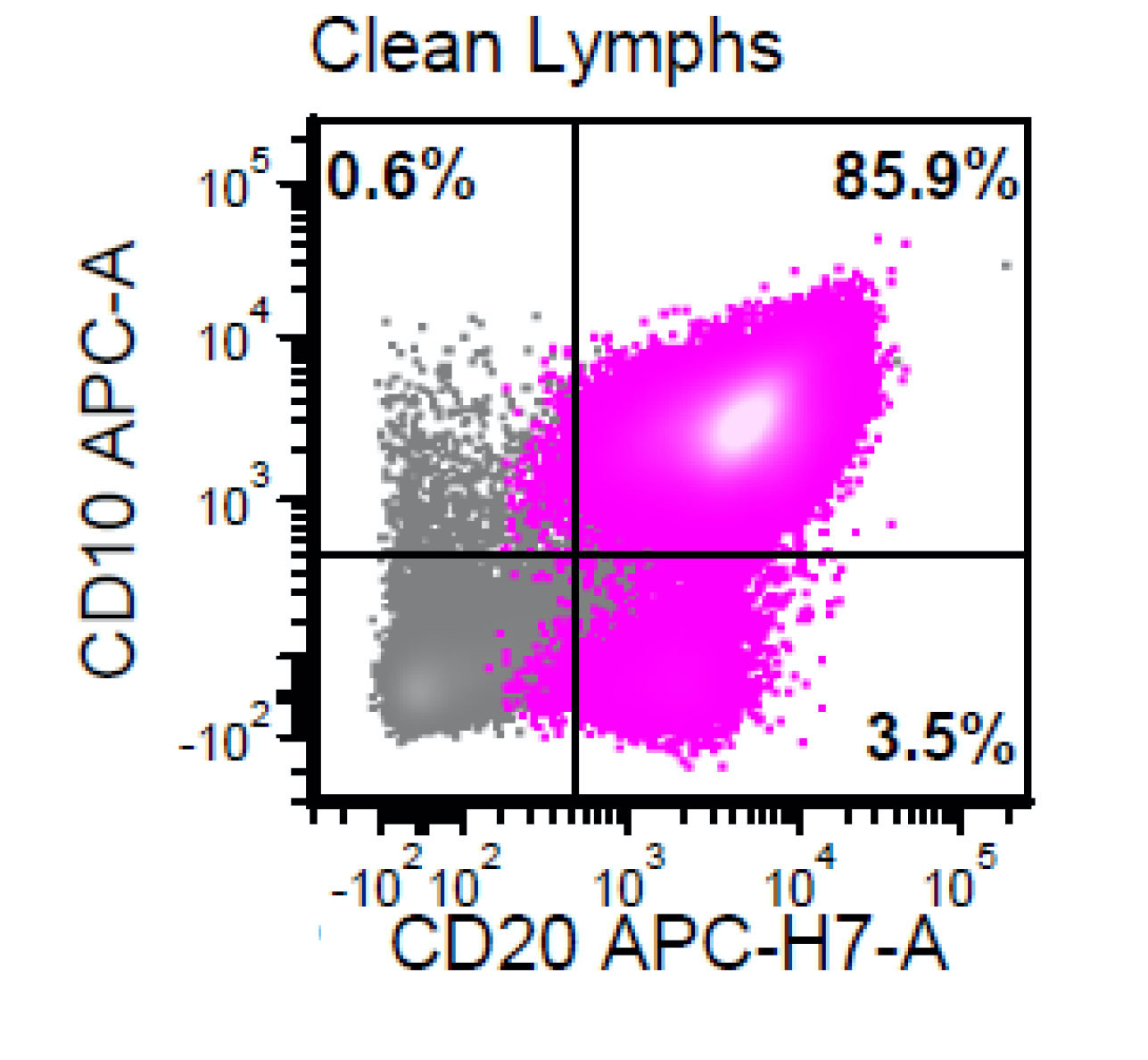
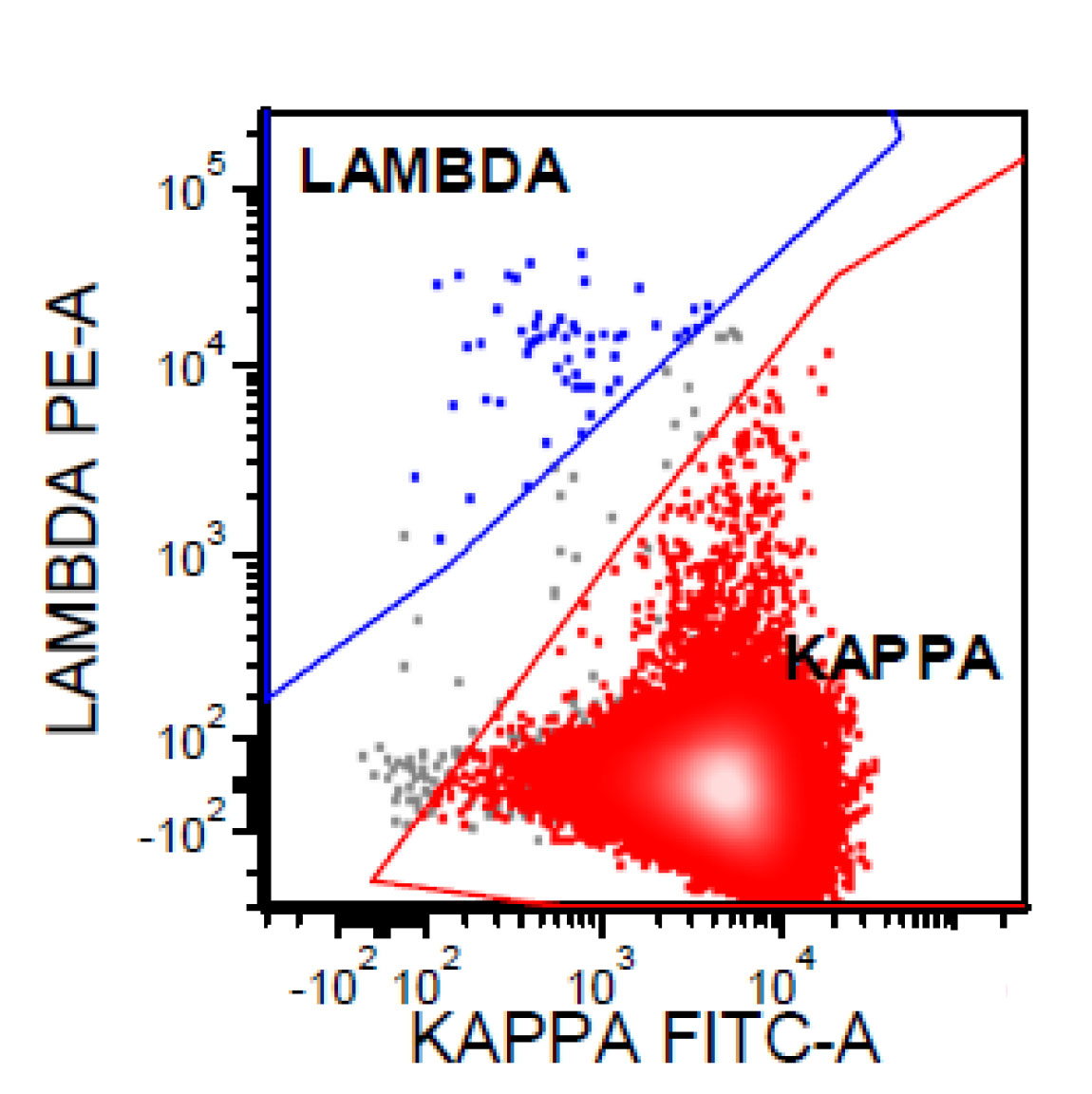
- CD20 bright+, CD19 dim+, CD10+, CD5-, cyclin D1-
Flow cytometry images
Molecular / cytogenetics description
- Monoclonal immunoglobulin (Ig) heavy and light chain gene rearrangements
- FISH can detect t(14;18)(q32;q21) IGH-BCL2 in up to 90% of follicular lymphoma cases
- FISH is more sensitive than PCR based approaches
- Variation in breakpoint regions
- Juxtaposition of the Ig light chain promotors to BCL2: t(2;18) and t(18;22)
- 3q27 BCL6 rearrangement or amplification mostly in follicular lymphoma 3B
- Loss of 1p36 which contains TNFRSF14 is common
- MYC rearrangement / activation of MYC is rare in follicular lymphoma (< 5%)
- Associated with transformation to diffuse large B cell lymphoma
- Categorized as double hit lymphoma if transformed and also has BCL2 or BCL6 translocation
- Other genetic alterations associated with transformation to diffuse large B cell lymphoma
- Inactivation of TP53 and CDKN2A
- Frequent genetic alterations
- BCL2 > KMT2D / MLL2 > EPHA7 > EZH2 > BCL6 > CREBBP > TNFRSF14
- Less common genetic alterations
- ARID1A, CARD11, TNFAIP3, MYC, FOXO1, TP53
- Comparative genomic hybridization:
- Gains: 1, 2p15, 6p, 7p, 7q, 8q, 12q, 18p, 18q, X
- Losses: 1p36, 3q, 6q, 9p, 10q, 11q, 13q, 17p
- References: Medeiros: Diagnostic Pathology - Lymph Nodes and Extranodal Lymphomas, 2nd Edition, 2017, Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th Edition, 2017
Sample pathology report
- Inguinal lymph node, core needle biopsy:
- Follicular lymphoma, low grade, grade 1 - 2 / 3, follicular pattern (see comment)
- Comment: This patient presented recently with inguinal lymphadenopathy. Histologic sections consist of a core needle biopsy of lymph node demonstrating complete nodal architectural effacement by malignant lymphoma. Lymphoma cells are arranged in an entirely follicular distribution. Neoplastic follicles are composed predominantly of small cleaved cells (centrocytes) with fewer large noncleaved cells (centroblasts), the latter of which comprise < 15 cells per high power field (grade 1 - 2 / 3).
- Immunoperoxidase studies confirm that the tumor cells are positive for CD20, CD10, BCL6, LMO2 and BCL2 (dim) and negative for CD3 and CD5. The proliferation rate of lymphoma cells, measured by Ki67 (MIB1), is ~10%. These morphologic and immunophenotypic findings support the above interpretation.
Differential diagnosis
- Reactive follicular hyperplasia:
- Follicles mostly in cortex
- Widely spaced follicles
- Variation in size and shape of follicles
- Polarization of germinal centers into light and dark zones (higher proliferation)
- Frequent mitoses
- Tingible body macrophages in germinal centers
- Sharply demarcated mantle zones
- No evidence of monoclonality by IG rearrangement
- Negative for t(14;18)(q32;q21)
- Progressive transformation of germinal centers:
- Nodules are 3 - 5x larger than background reactive follicles
- It may be hard to separate from floral variant of follicular lymphoma on morphology
- Germinal center B cells are BCL2-
- No evidence of monoclonality
- Negative for t(14;18)(q32;q21)
- Castleman disease, hyaline vascular variant:
- Follicles are widely spaced
- Concentric mantle zones
- Depleted germinal centers
- Prominent follicular dendritic cells
- BCL6- in most of the lymphoid cells of atretic follicles
- Refer to unusual variants of follicular lymphomas (follicular lymphoma with Castleman-like features)
- Nodular lymphocyte predominant Hodgkin lymphoma:
- Lymphocyte rich classic Hodgkin lymphoma:
- Mantle cell lymphoma:
- Nodal marginal zone lymphoma:
Additional references
Board review style question #1
All of the following genes are frequently associated with large cell transformation in follicular lymphoma, except
- BCL6
- CDKN2A
- MYC
- TP53
Board review style answer #1
Board review style question #2
Which of the following is true of follicular lymphoma?
- Abnormal expression of BCL2 protein by germinal center B cells is required for diagnosis of follicular lymphoma
- Follicular lymphoma is generally systemic in nature and stage IV at initial diagnosis
- Grading in follicular lymphoma is based on proliferative rate, as measured by Ki67 immunostaining
- High grade follicular lymphomas more frequently show upregulation of BCL2 protein expression compared to low grade follicular lymphomas
Board review style answer #2
B. Follicular lymphoma is generally systemic in nature and stage IV at initial diagnosis
Comment Here
Reference: Follicular lymphoma, nodal, usual variant
Comment Here
Reference: Follicular lymphoma, nodal, usual variant