Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Tozbikian G. Metastases. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantmet.html. Accessed July 29th, 2025.
Definition / general
- Metastasis to the breast from a malignancy arising outside the breast
Essential features
- Rare, < 1% of breast malignancies (Eur J Surg Oncol 2003;29:854, Cancer 2007;110:731, J Clin Pathol 2007;60:1333)
- Can be initially misdiagnosed due to nonspecific / overlapping clinical, radiologic, morphologic and immunophenotypic features with primary breast carcinoma, especially if inadequate clinical history is provided
- Accurate identification of extramammary metastases is critical to avoid unnecessary surgery and inappropriate treatment
Terminology
- Nonmammary metastases to the breast, extramammary metastases to the breast
ICD coding
- ICD-10: C80.0 - disseminated malignant neoplasm, unspecified
Epidemiology
- Metastases to the breast represents 0.2 - 1.3% of breast malignancies (Eur J Surg Oncol 2003;29:854, Cancer 2007;110:731, J Clin Pathol 2007;60:1333)
- More common in women (Cancer 2001;92:2259, Mod Pathol 2013;26:343)
- Median age in fifth decade but can occur in pediatric patients (Mod Pathol 2013;26:343)
Etiology
- A wide range of extramammary malignancies can metastasize to the breast, including lymphoma, melanoma, sarcoma (uterine leiomyosarcoma, rhabdomyosarcoma, liposarcoma) and carcinoma (common primary sites include gynecologic, lung, gastrointestinal, genitourinary, head and neck) (Cancer 2007;110:731, Mod Pathol 2013;26:343)
- Most common primary sites include cutaneous malignant melanoma, lung and ovary (Cancer 2007;110:731, Mod Pathol 2013;26:343)
- In pediatric patients, most common primaries include rhabdomyosarcoma and lymphoma (Pathol Annu 1989;24:296, J Pediatr Surg 1994;29:48)
- Lymphoma involving the breast can be either primary or due to secondary systemic involvement
Clinical features
- Majority of patients have a history of malignancy, often with prior or coincident metastases to other nonmammary sites (Cancer 2007;110:731, J Surg Oncol 2006;94:101, Mod Pathol 2013;26:343)
- In 11 - 30% of cases, breast metastasis is the initial presentation of an occult extramammary malignancy (Cancer 2001;92:2259, J Clin Pathol 2007;60:1333, Mod Pathol 2013;26:343)
- Long interval between primary malignancy and the breast metastasis can be observed in melanoma and ovarian carcinoma (J Clin Pathol 2007;60:1333, Clin Oncol 1976;2:393)
- Frequently presents as a solitary, rapidly growing, palpable mass (Acta Pathol Microbiol Scand A 1981;89:251, AJR Am J Roentgenol 1977;129:673, Mod Pathol 2013;26:343)
- Can present with axillary lymphadenopathy (J Ultrasound Med 2000;19:257, Am J Surg Pathol 2004;28:1646)
- Presentation can mimic inflammatory breast cancer (Eur J Nucl Med Mol Imaging 2016;43:389, Breast Cancer 2008;15:315)
Diagnosis
- Possibility of a nonmammary metastasis should be considered when encountering a breast lesion with unusual clinical, radiologic or histomorphologic features
- Clinical history is critical to establish the correct diagnosis; there is often history of advanced stage, nonbreast malignancy
- Biopsy is performed if clinical evaluation and imaging are inconclusive for primary versus metastasis
- Identification of a definitive in situ component can be useful to rule out metastasis and confirm a breast primary
- Absence of an in situ component does not conclusively exclude a nonmammary metastasis, as an in situ component is not present in all primary mammary carcinomas
- Immunohistochemical work up is generally required for confirmation of the diagnosis
Radiology description
- Can show variable imaging features depending on the origin and location of the primary tumor (Case Rep Radiol 2019;2019:9454201)
- Generally well defined, discrete, rounded mass, with less spiculation compared with primary breast malignancies (J Ultrasound Med 2000;19:257, Eur J Surg Oncol 2003;29:854)
- Usually presents initially as a unilateral, solitary mass but with progression may present as multiple or bilateral masses (Int J Surg Case Rep 2014;5:34, Am J Surg Pathol 2004;28:1646, Mod Pathol 2013;26:343)
- Calcifications are rare, except in serous carcinoma of the ovary (Am J Surg Pathol 2004;28:1646, Surgery 1991;110:552)
Radiology images
Prognostic factors
- Poor prognosis; most patients present with advanced stage, widely disseminated disease (Cancer 2007;110:731)
- Median survival of 8 - 10 months (Cancer 2007;110:731, J Am Coll Surg 1994;179:49)
- Individual prognosis is dependent on the specific clinical characteristics of the metastatic neoplasm
Case reports
- 40 year old woman with history of ovarian serous cystadenocarcinoma presented with a left breast mass (Cancer Manag Res 2020;12:13015)
- 47 year old woman with pulmonary adenocarcinoma presented with left breast nodule (BMC Cancer 2014;14:736)
- 56 year old woman with colonic adenocarcinoma presented with palpable right breast mass (Case Rep Oncol Med 2015;2015:458423)
- 58 year old woman with melanoma presented with a right breast mass (J Med Case Rep 2016;10:363)
- 63 year old woman with renal cell carcinoma presented with breast mass detected by mammography (BMJ Case Rep 2017;2017:bcr2016219124)
- 67 year old woman with a solitary, rapidly enlarging, 2.2 cm right breast mass (Case #504)
- 76 year old woman with ovarian serous carcinoma presented with left breast mass and axillary lymphadenopathy (J Cutan Pathol 2018;45:234)
- 85 year old woman presented with right breast mass (World J Gastrointest Oncol 2020;12:1073)
Treatment
- Primary therapeutic approach is systematic treatment that is specific and appropriate to the primary lesion
- Generally, surgical excision is not indicated for metastatic tumors to the breast, unless performed to palliate symptoms (e.g., bulky, ulcerated lesions)
- It is critically important for the pathologist to recognize the metastatic nature of the lesion, as the treatment and prognosis differ significantly from primary breast cancer and misdiagnosis can result in unnecessary surgery and inappropriate treatment (Mod Pathol 2013;26:343)
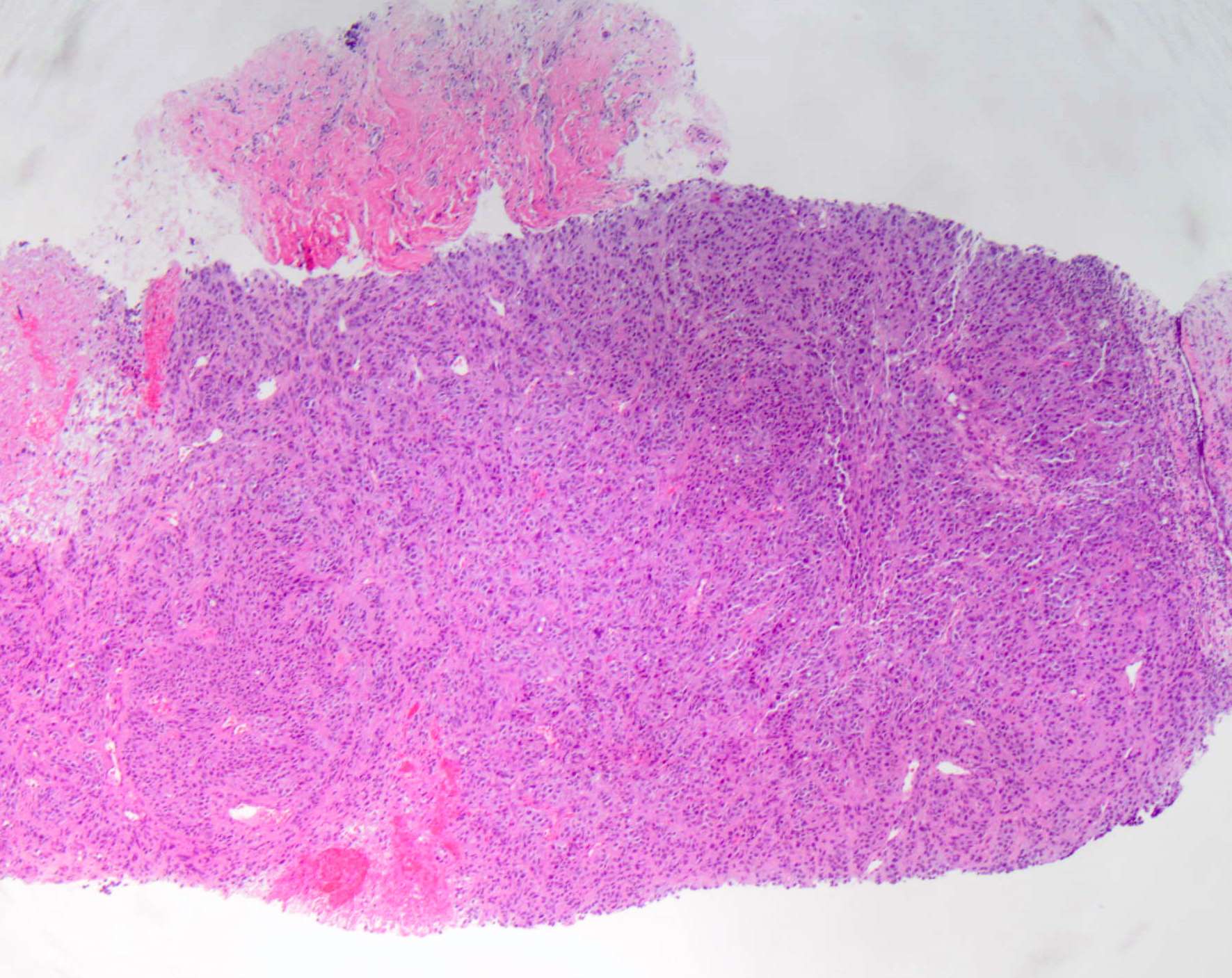
Gross description
- Generally well circumscribed
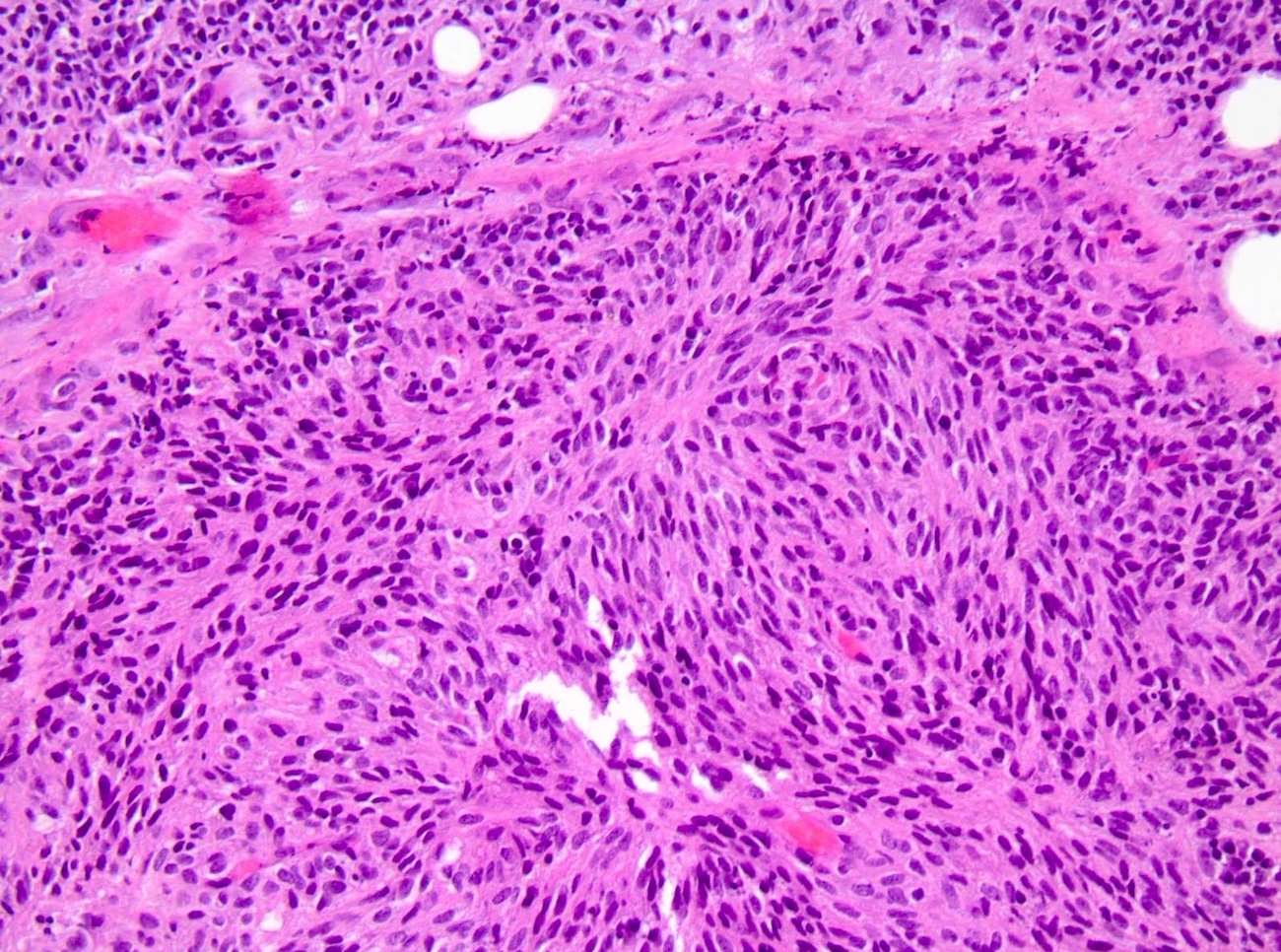
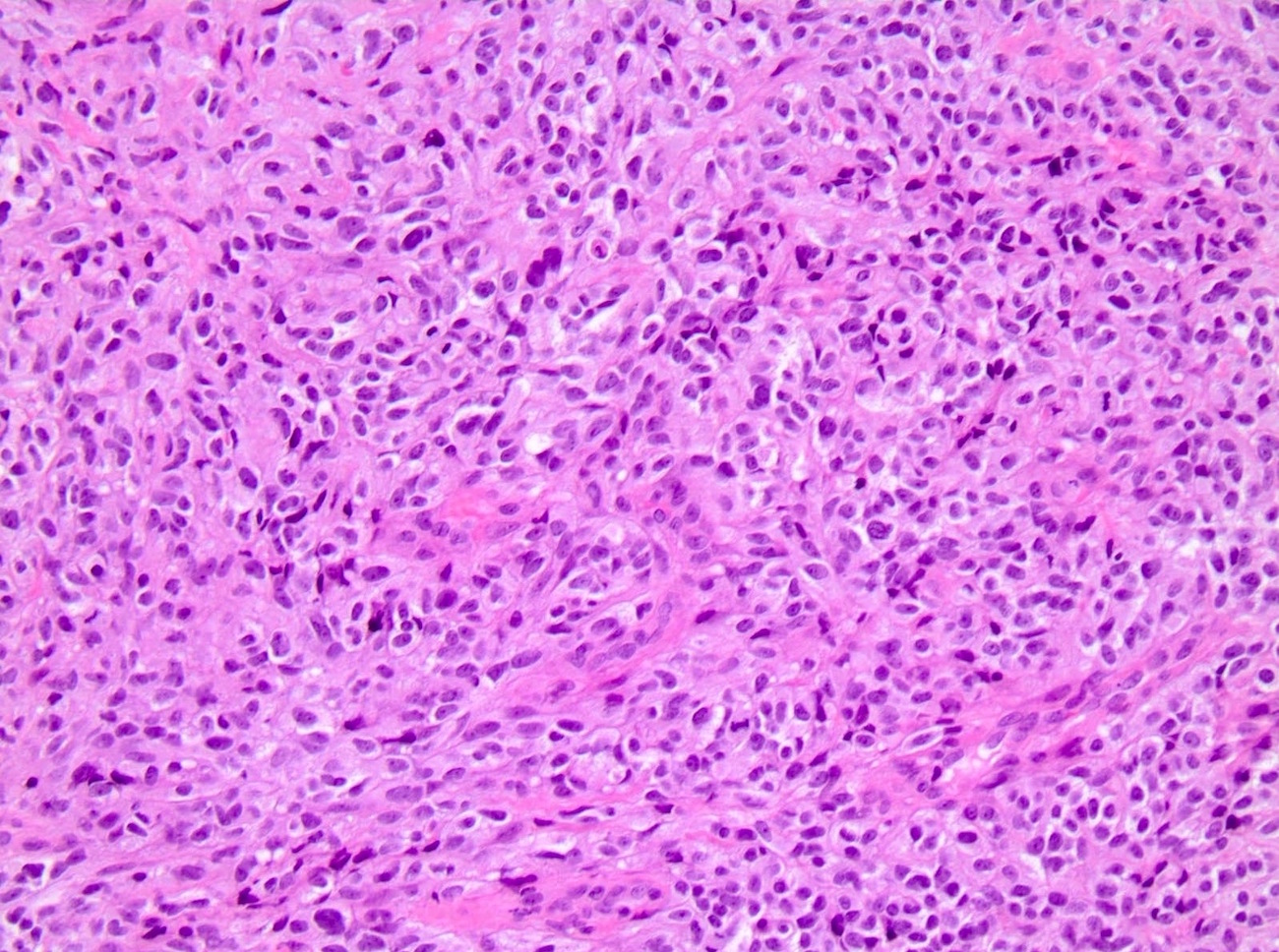
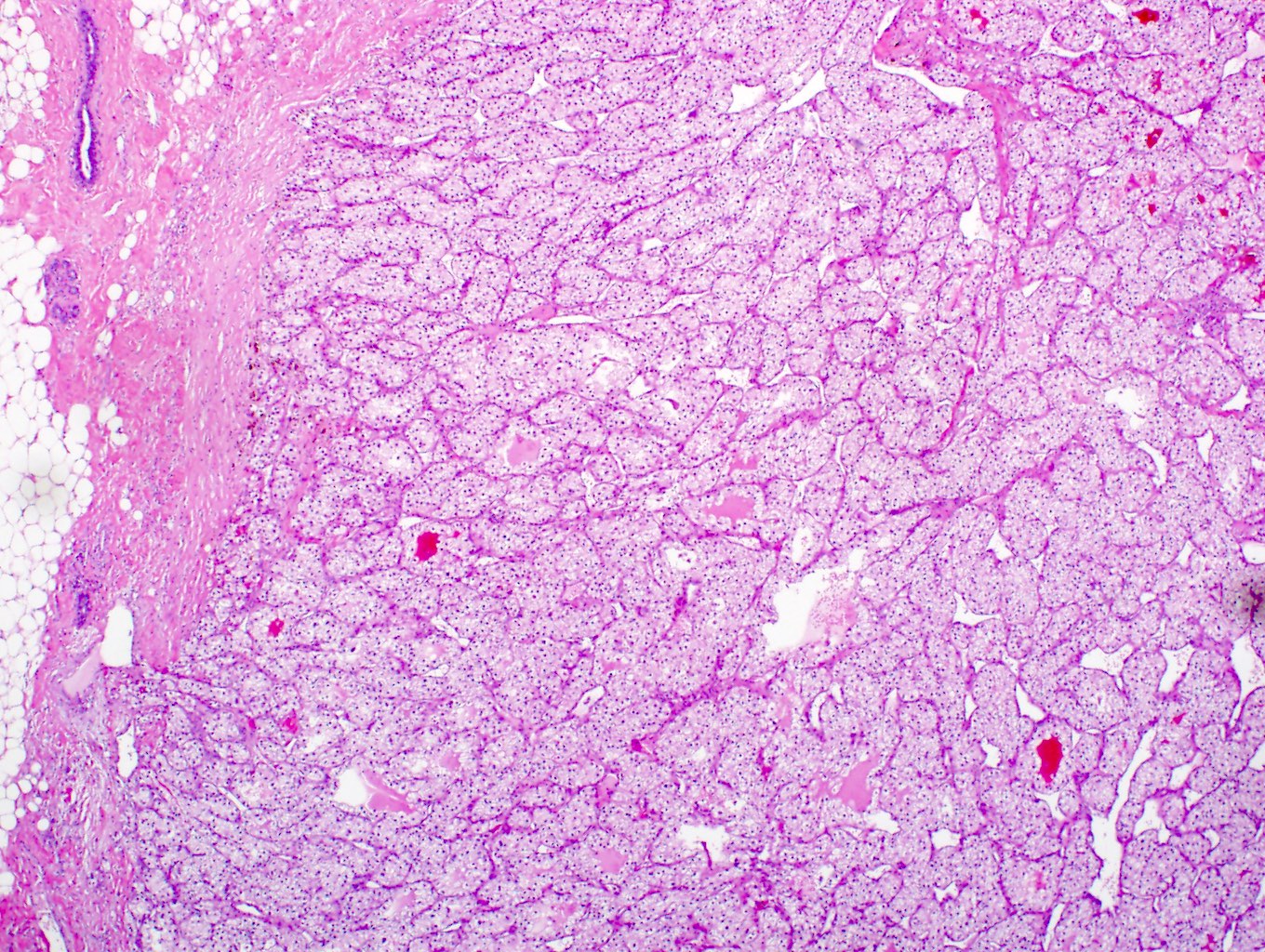
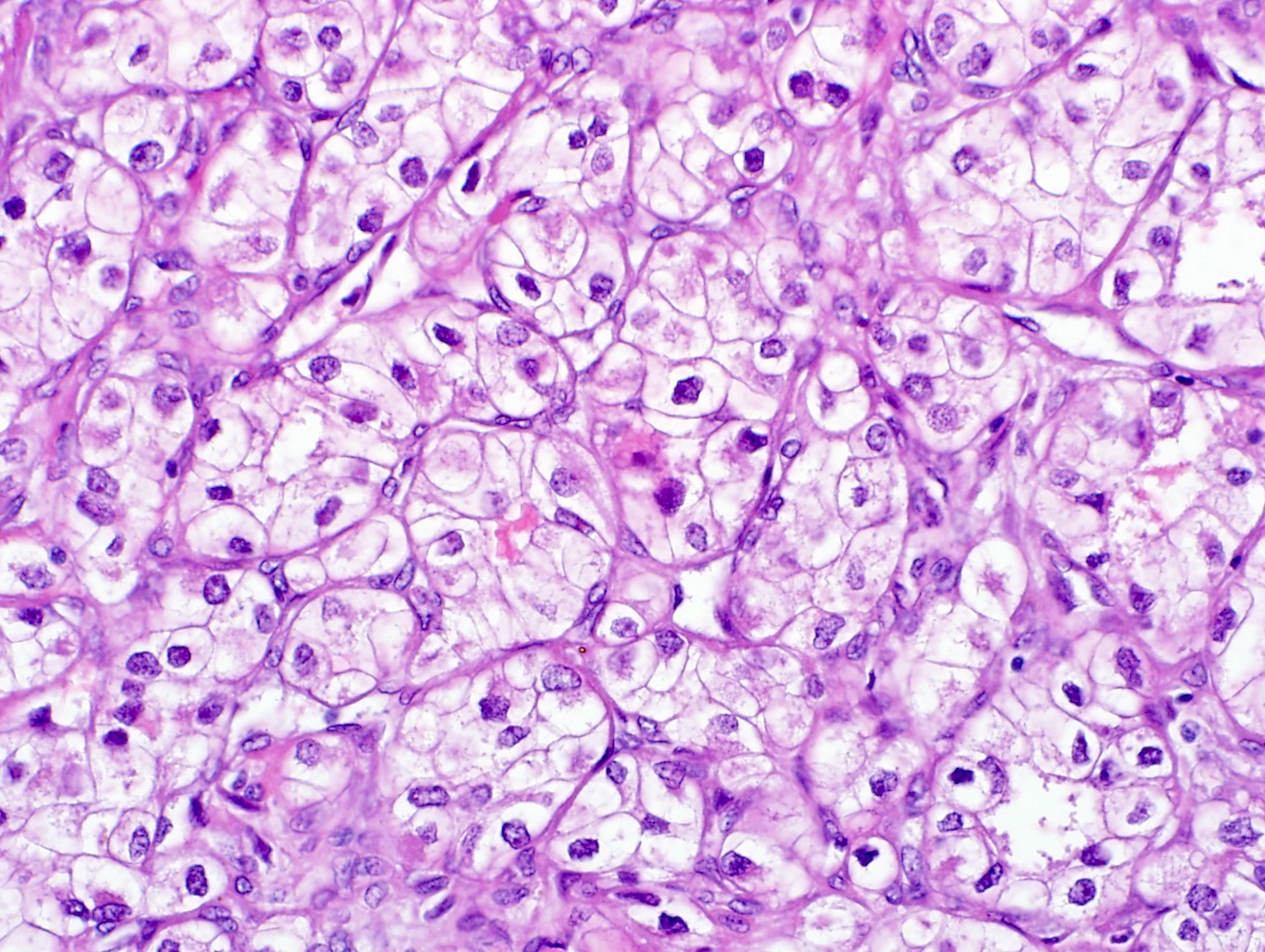
Microscopic (histologic) description
- General
- Often morphologic features are unusual for a primary mammary tumor (J Clin Pathol 2007;60:1333)
- Lack of an in situ component (J Clin Pathol 2007;60:1333)
- Metastatic tumors with certain morphologies (e.g., spindle cell, mucinous, squamous, clear cell, neuroendocrine) may show significant morphologic overlap with primary breast malignancies
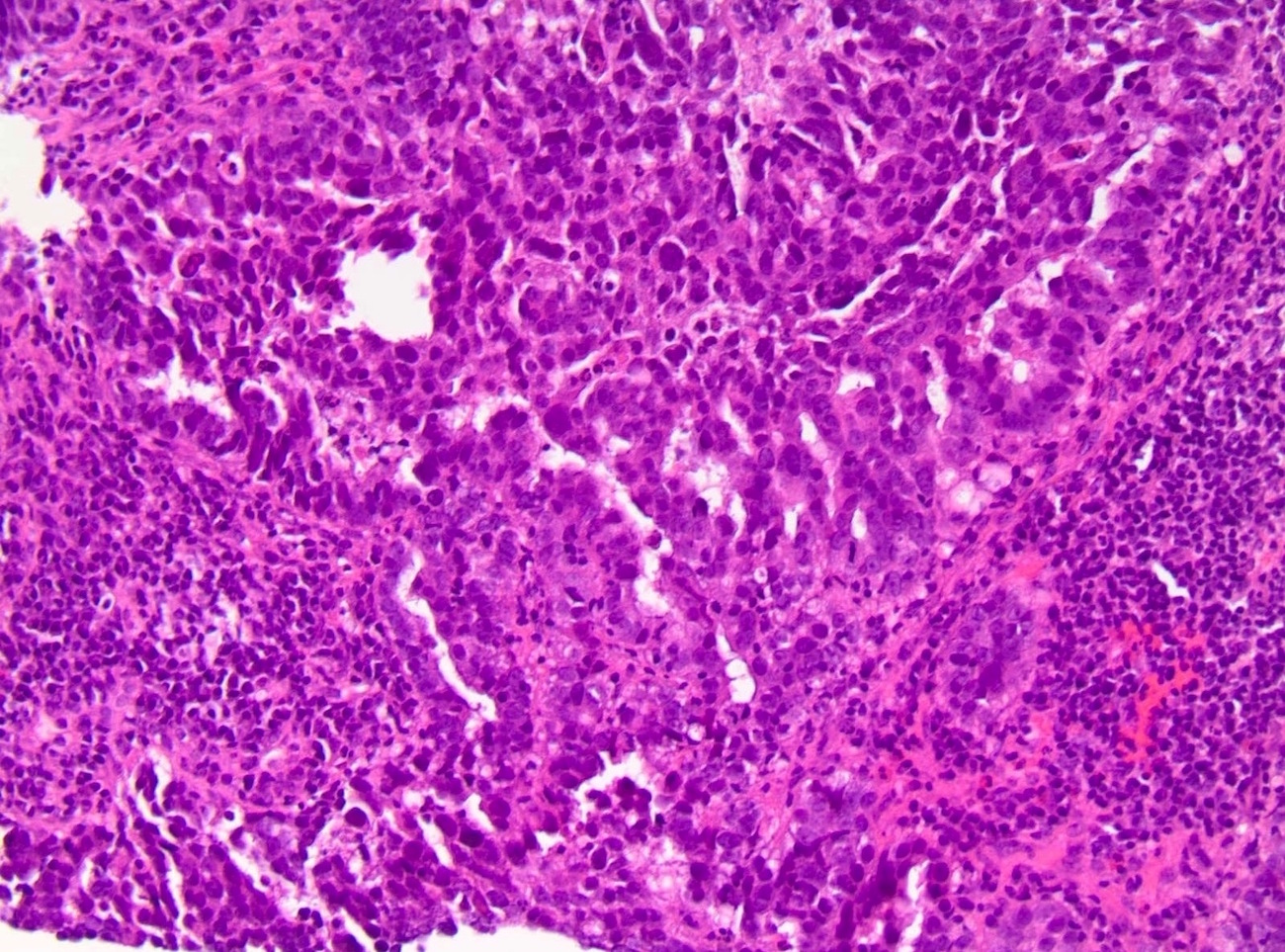
- Malignant melanoma
- Wide range of histologic appearances, may be amelanotic
- Generally high grade cytology
- Pigment, spindle cell morphology, intranuclear inclusions can suggest melanoma (Histopathology 2000;36:387)
- Pulmonary carcinoma
- Wide range of histologic appearances, including cystic papillary and glandular architecture
- Small cell features can suggest pulmonary site of origin
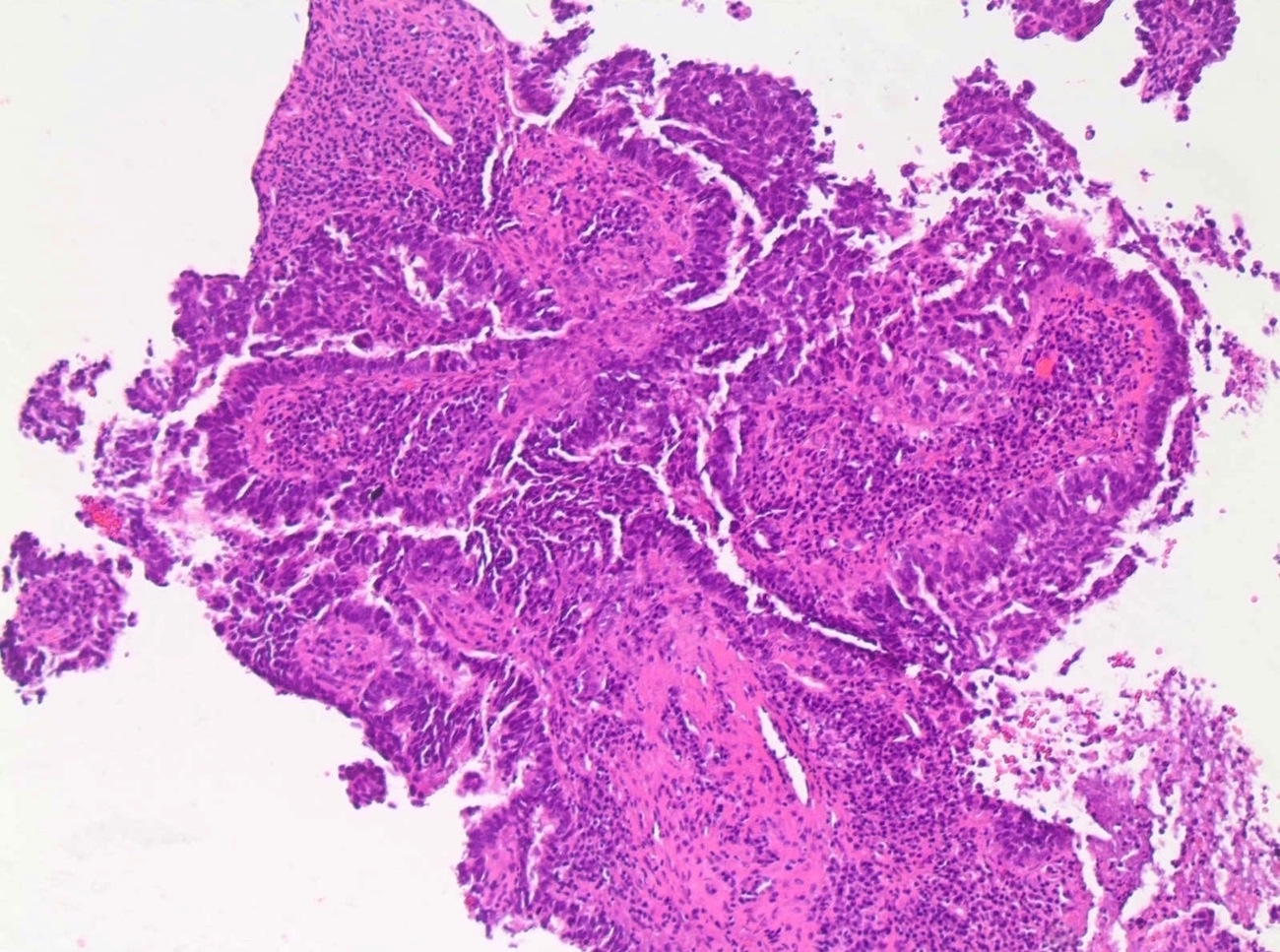
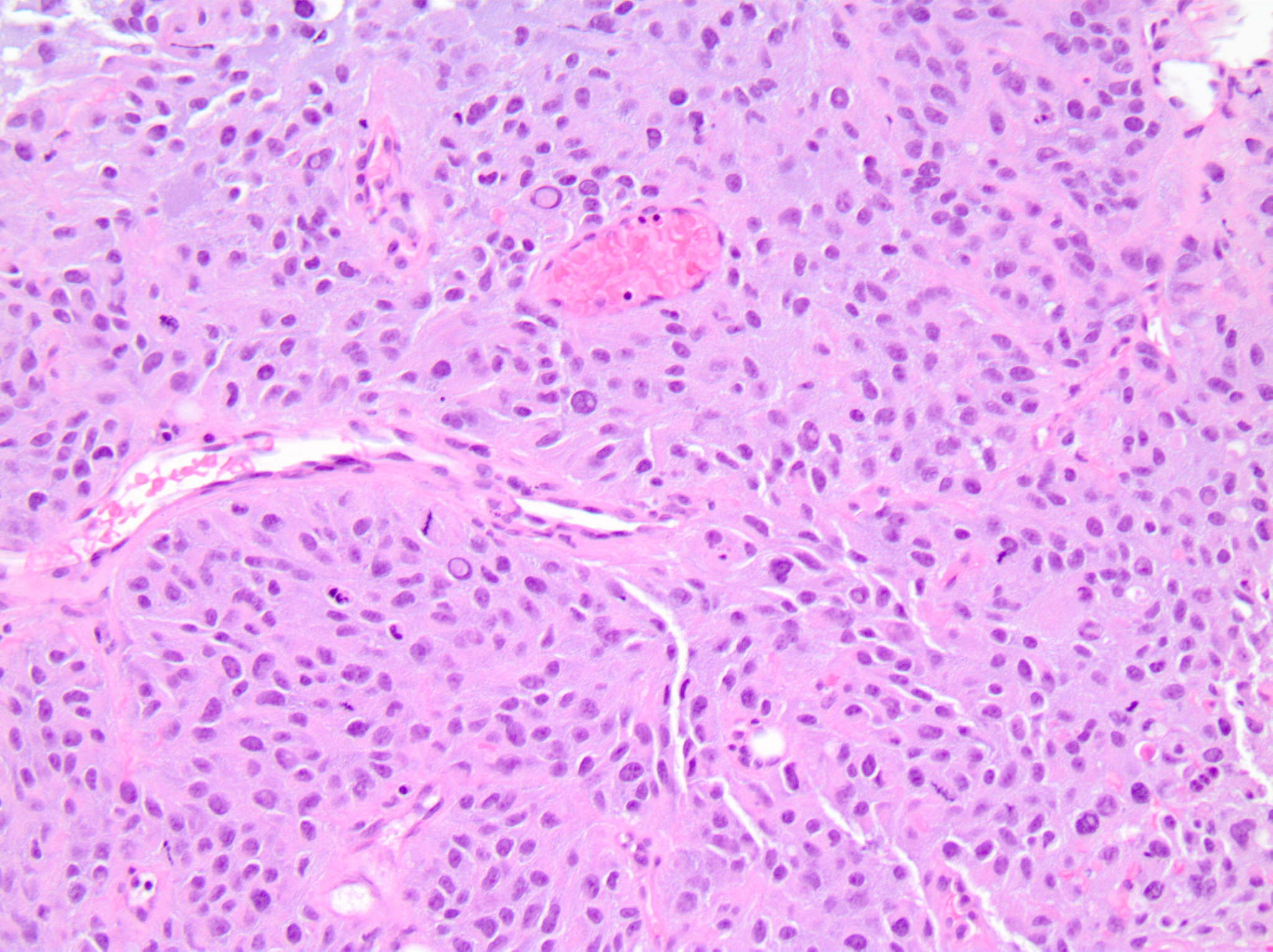
- Ovarian carcinoma
- Usually serous type, less commonly mucinous or clear cell types
- Wide range of histologic appearances, including papillary, glandular and solid architecture
- May show necrosis and high grade cytology
- Papillary morphology, psammomatous calcifications can suggest ovarian serous carcinoma (Am J Surg Pathol 2004;28:1646)
- Often morphologic overlap with breast primary
- Gastrointestinal carcinoma
- If mucinous morphology, can show histologic overlap with mucinous subtype of breast carcinoma
- If signet ring cell morphology, can show histologic overlap with lobular subtype of breast carcinoma
- If neuroendocrine / carcinoid, can show histologic overlap with neuroendocrine carcinoma of the breast
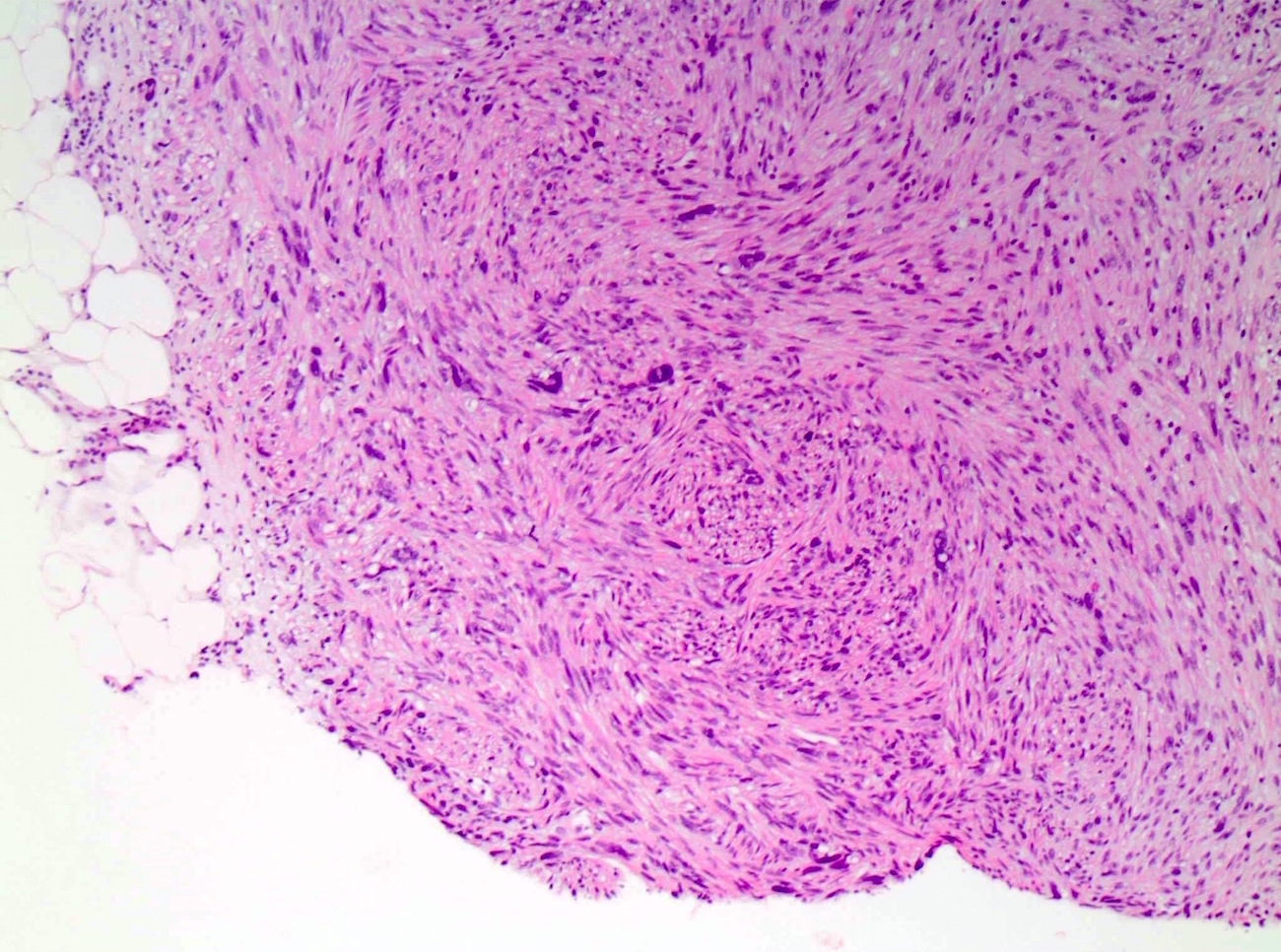
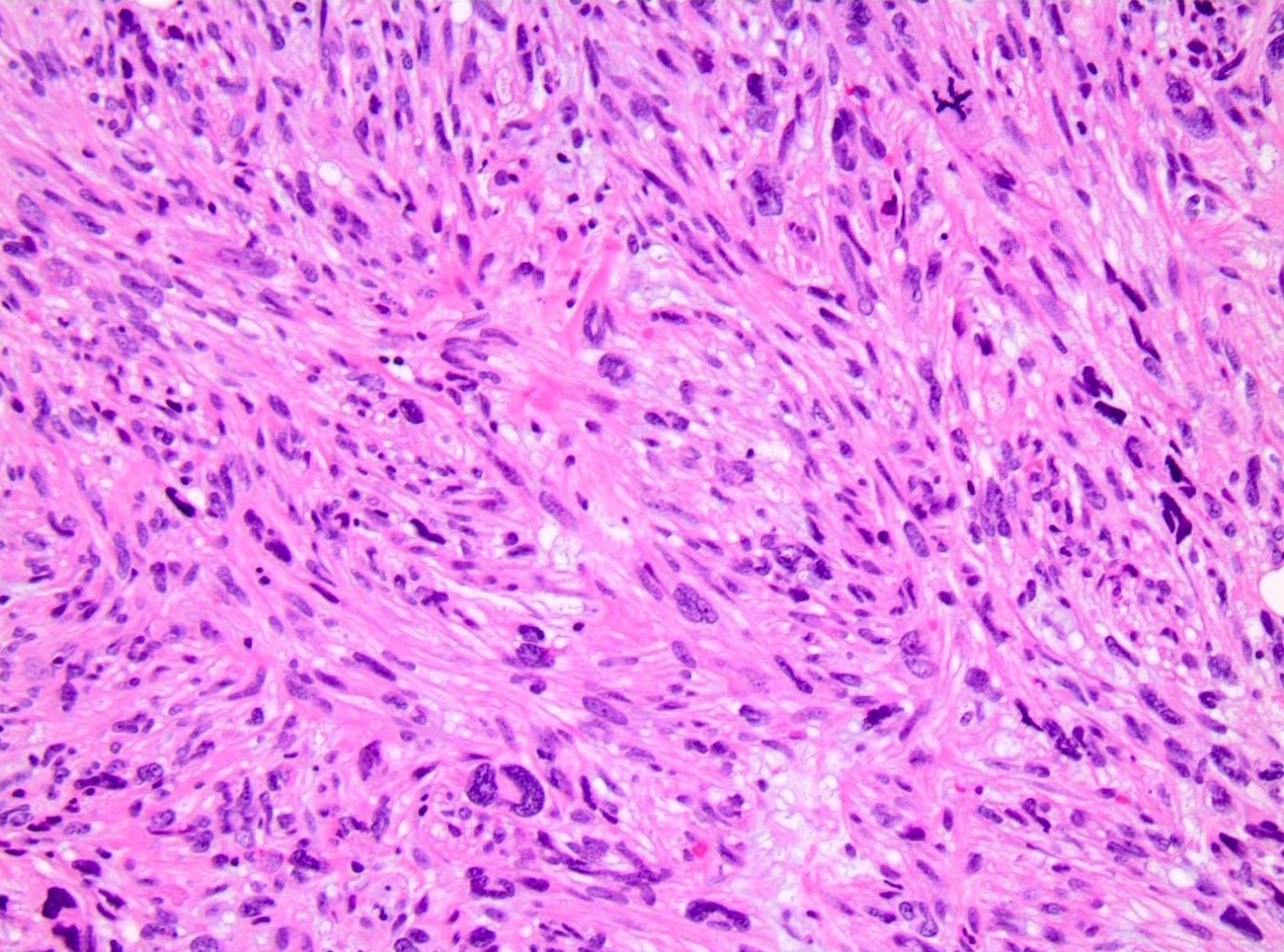
- Renal cell carcinoma
- Clear cell features can suggest renal site of origin
- If spindle cell and sarcomatoid morphology, can show histologic overlap with metaplastic breast carcinoma
- Prostatic adenocarcinoma
- Can show morphologic overlap with breast primary
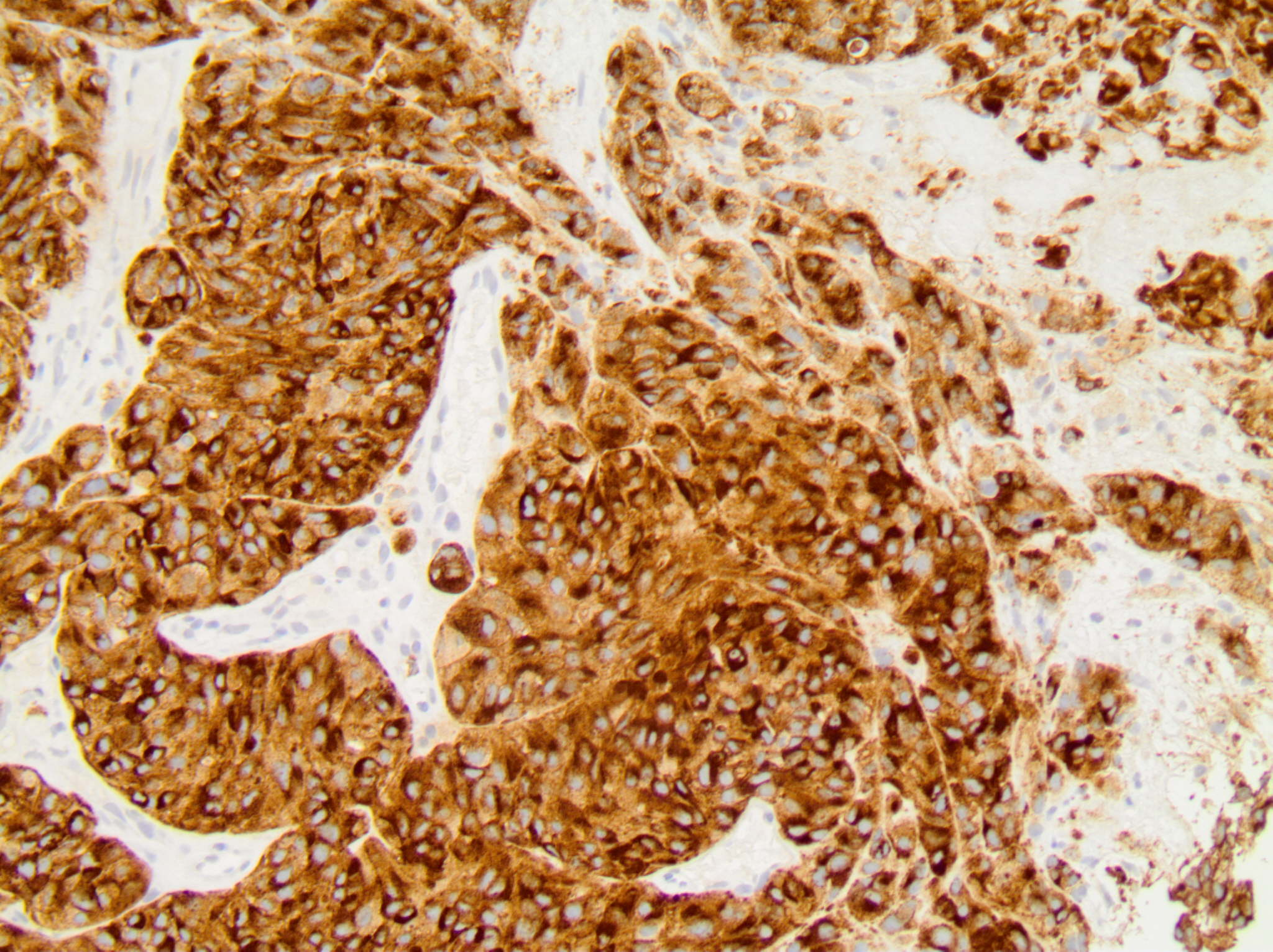
Microscopic (histologic) images
Cytology description
- Malignant melanoma
- Dispersed polygonal and plasmacytoid cells with a moderate amount of granular and vacuolated cytoplasm, can show spindle cell morphology (Diagn Cytopathol 2017;45:446)
- Pulmonary adenocarcinoma
- Groups of medium sized cells showing complex papillary arrangement (Ann Oncol 2008;19:682)
- Ovarian carcinoma
- Medium sized cells arranged in papillary clusters with round nuclei with evident nucleoli and a moderate quantity of grayish cytoplasm, psammomatous microcalcifications (Ann Oncol 2008;19:682)
Cytology images
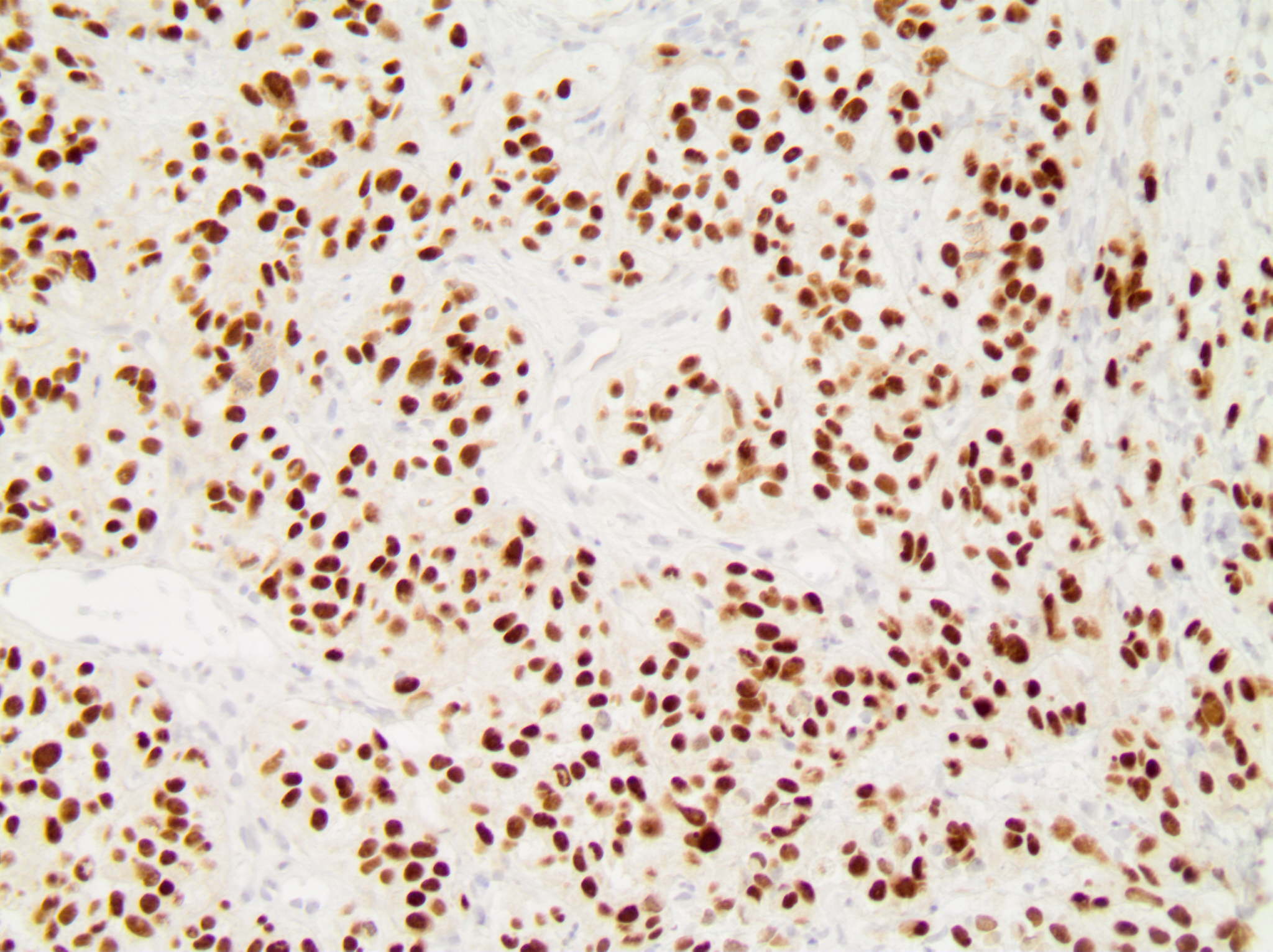
Positive stains
- Malignant melanoma
- S100, HMB45, MelanA (versus negative in breast)
- SOX10 (also positive in triple negative breast cancer) (Hum Pathol 2019;85:221, Hum Pathol 2013;44:959)
- Pulmonary carcinoma
- Ovarian carcinoma
- PAX8, WT1 (serous and clear cell carcinoma) (versus negative in breast) (WT1 can be seen mucinous and micropapillary subtypes of breast cancer) (Am J Surg Pathol 2008;32:1566, Am J Surg Pathol 2011;35:816, Int J Gynecol Pathol 2004;23:110, Mod Pathol 2008;21:1217, Histopathology 2007;51:824)
- CK7, estrogen receptor, progesterone receptor (also positive in breast carcinoma)
- Gastrointestinal carcinoma
- Renal cell carcinoma
- PAX8, PAX2, RCC (versus negative in breast) (Am J Surg Pathol 2011;35:816)
- Prostatic adenocarcinoma
- PSA, PSAP, NKX3.1 (versus negative in breast)
- Androgen receptor (also positive in breast carcinoma)
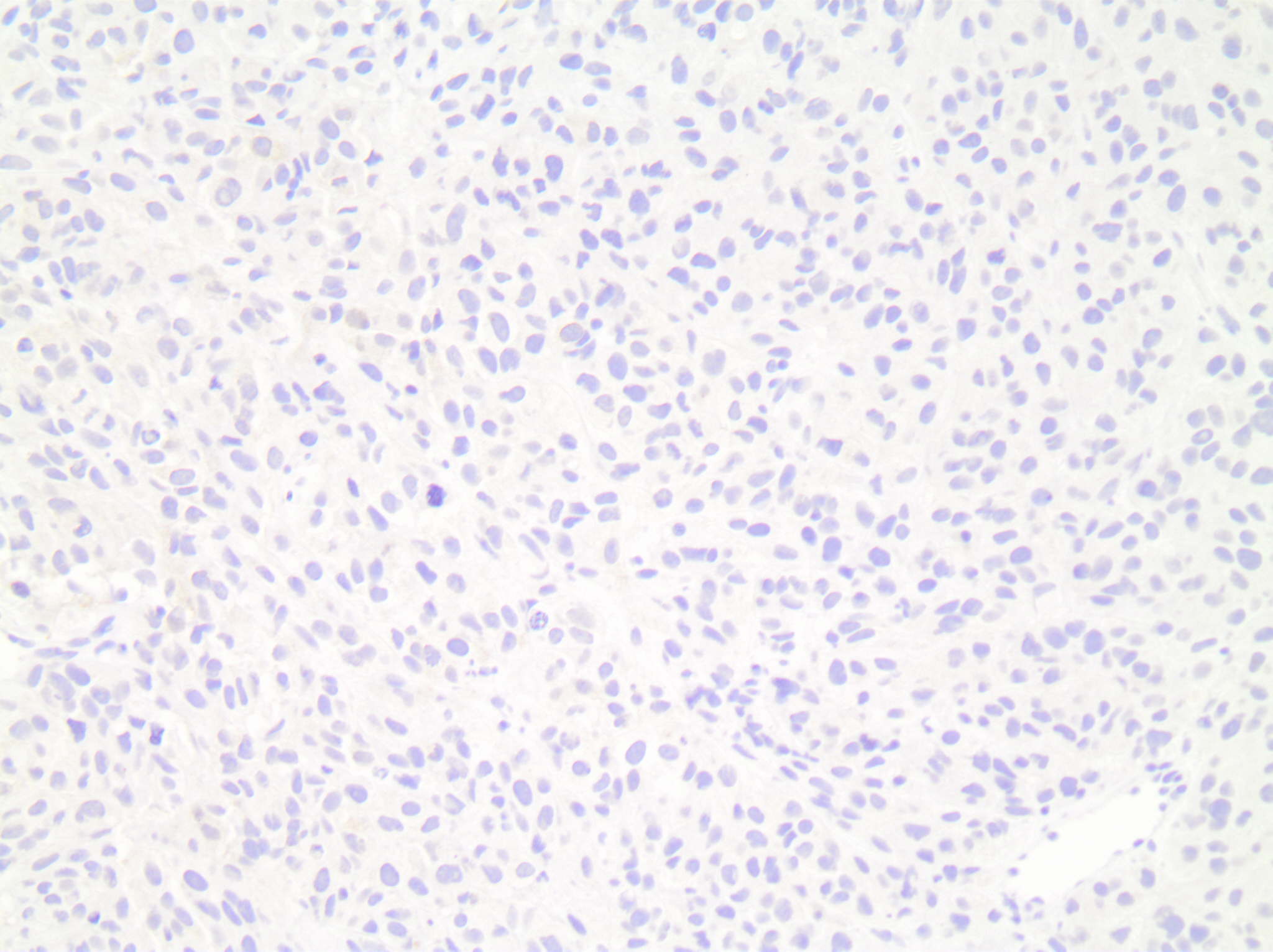
Negative stains
- Estrogen receptor and progesterone receptor (except metastasis from gynecologic primary sites)
- GATA3 (except metastasis from urothelial, salivary gland, pancreatic adenocarcinoma and squamous primary sites) (Am J Surg Pathol 2014;38:13)
- TRPS1 (can be positive in ovarian serous carcinoma, salivary duct carcinoma)
- p63 / p40, calponin / SMMS (myoepithelial markers to confirm lack of in situ component)
- Malignant melanoma
- Cytokeratin (versus positive in breast)
- Prostatic adenocarcinoma
- CK7 (versus positive in breast)
Sample pathology report
- Breast, left, 2:00 zone 2, ultrasound guided core biopsy:
- Metastatic carcinoma, consistent with metastasis of Müllerian origin (see comment)
- Comment: Per the electronic medical record, the patient's history of ovarian cancer is noted. Immunohistochemical stains show that the tumor cells are positive for CK7, estrogen receptor, PAX8 and WT1 and are negative for GATA3, BRST2 and mammaglobin. The findings are consistent with metastasis of Müllerian origin (ovarian serous carcinoma).
Differential diagnosis
- Invasive ductal carcinoma:
- Invasive lobular carcinoma:
- Metaplastic carcinoma:
- Can mimic renal cell carcinoma
- Negative: PAX8
- Mucinous carcinoma of the breast:
- Papillary carcinomas of the breast (solid, encapsulated, invasive):
Practice question #1
A 55 year old woman with history of cutaneous malignant melanoma presents with a solitary, palpable, rapidly enlarging breast mass. Ultrasound guided core biopsy shows a high grade malignant neoplasm. What panel of immunohistochemical stains would be most useful in distinguishing metastatic melanoma versus a primary breast malignancy?
- Cytokeratin and estrogen receptor
- Cytokeratin, HMB45 and MelanA
- Estrogen receptor and S100
- SOX10 and estrogen receptor
- SOX10 and S100
Practice answer #1
B. Cytokeratin, HMB45 and MelanA. A panel of cytokeratins and melanoma markers (e.g., S100, HMB45, MelanA) would be most useful. 20% of breast cancers will be negative for estrogen receptor. A negative result for estrogen receptor would not rule out a breast primary. SOX10 can be expressed in both melanoma as well as triple negative breast cancer.
Comment Here
Reference: Metastases
Comment Here
Reference: Metastases
Practice question #2
A 45 year old BRCA+ woman with a history of ER+ primary ductal carcinoma of the breast 5 years ago now presents with ascites and omental caking. Peritoneal biopsy shows a high grade malignant neoplasm with glandular and papillary features. Given the history, an initial panel of breast biomarkers is performed. The tumor is strongly positive for ER and PR and negative for HER2. What panel of additional immunohistochemical stains would be most useful in the diagnosis?
- CK20 and CDX2
- GATA3 and androgen receptor
- MelanA and HMB45
- PAX8 and WT1
- TTF1 and Napsin A
Practice answer #2
D. PAX8 and WT1. Given the clinical presentation, hormone receptor positivity and history of BRCA mutation, a metastasis from a gynecological primary (e.g., ovarian carcinoma) is the main concern. The most appropriate immunohistochemical stain panel would include PAX8 and WT1.
Comment Here
Reference: Metastases
Comment Here
Reference: Metastases