Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Homsi H, Ronen S. Adenoid cystic carcinoma (primary cutaneous). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticacc.html. Accessed August 27th, 2025.
Definition / general
- Rare, slow growing cutaneous adnexal tumor with 3 major histologic patterns: tubular, cribriform and solid
- Morphologically indistinguishable from adenoid cystic carcinoma at other sites; must rule out cutaneous extension from salivary gland malignancy or metastasis from other locations
- More indolent than salivary gland counterpart (Am J Surg Pathol 2013;37:1603)
Essential features
- Primary cutaneous adenoid cystic carcinoma (PCACC) is a rare adnexal tumor with different histopathologic growth patterns, including cribriform, tubular and solid variants
- Perineural invasion is a common feature and may explain the high recurrence level
- Diagnosis is confirmed only after ruling out metastatic disease through thorough clinical history and imaging studies
- 60% of PCACC cases exhibit MYB overexpression, which is mediated by MYB::NFIB fusion or other MYB chromosomal abnormalities
ICD coding
- ICD-O: 8200/3 - adenoid cystic carcinoma
- ICD-11: 2C33 & XH4302 - adnexal carcinoma of skin & adenoid cystic carcinoma
Epidemiology
- Occurs predominantly in middle aged and elderly individuals; median age is 62 years (JAAD 2021;85:245)
- M:F ratio ranges from 0.79:1 to 1.6:1 (JAAD 2021;85:245, Histopathology 2022;80:407, Am J Surg Pathol 2013;37:1603)
Sites
- Head and neck (particularly the scalp) is the most frequently involved site, followed by the trunk, upper limbs / limb girdle and lower limb / limb gridle (Histopathology 2022;80:407)
Pathophysiology
- Unclear; previously thought to arise from eccrine glands
- Recent hypotheses support apocrine or modified apocrine glands as an origin (Dermatol Online J 2013;19:5)
- ~60% of PCACC cases harbor MYB gene activation (J Cutan Pathol 2017;44:201)
Etiology
- Unknown
Clinical features
- Solitary, slow growing mass; often present for several years prior to diagnosis (Histopathology 2022;80:407)
- Usually skin colored
- Some may be indurated, tender or ulcerate; in the scalp, symptoms may involve localized alopecia (Rare Tumors 2011;3:e3)
- Size range: 1.0 - 5.0 cm, with a median of 2.0 cm (Am J Surg Pathol 2013;37:1603)
Diagnosis
- Essential
- Histology with 2 types of lumina, including true small bilayered ducts (with or without secretion) and pseudocysts containing basophilic mucinous material in multinodular neoplasm
- 2 main cell types: ductal and myoepithelial cells
- Desirable
- Cylindroma-like appearance
- Perineural invasion
- Coexpression of MYB and CD117
- Demonstration of MYB or MYBL1 rearrangements in selected cases
Prognostic factors
- Metastasis is rare (typically to lymph nodes or lungs) and associated with high grade transformation (Histopathology 2022;80:407)
- Recurrence is very common, primarily attributed to perineural invasion (Am J Surg Pathol 2013;37:1603)
- Vulva and perigenital sites may correlate with more aggressive disease / metastases, possibly due to the abundance of nerve tissue in this area; however, larger studies are needed to validate this supposition (Am J Surg Pathol 2013;37:1603)
- Factors that may reflect a more biologically aggressive tumor (Histopathology 2022;80:407)
- Longest diameter of the lesion (≥ 1 cm)
- Involvement of subcutaneous fat tissue and widely infiltrative border
- Grade III / high grade transformation
- In multivariate analysis of 451 cases, more recent year of diagnosis, advanced patient age and advanced stage were associated with poorer outcomes (JAAD 2021;85:245)
Case reports
- 62 year old man with painful and erythematous nodule on his left chest (Exp Oncol 2022;44:174)
- 67 year old woman with firm mobile nodule on her lower back (Cureus 2023;15:e49099)
- 70 year old woman with slow growing, painless, solid to cystic, skin colored lesion on her scalp (Skin Health Dis 2022;2:e118)
- 79 year old man with an asymptomatic, slow growing lesion on the abdomen (Dermatol Online J 2020;26:13030)
- 83 year old man with a 10 year history of nodule on lower leg (J Surg Case Rep 2019;2019:rjz201)
Treatment
- Wide surgical excision to prevent recurrence
- Mohs surgery has been performed for better control of surgical margins (JAMA Dermatol 2013;149:1343)
Clinical images
Gross description
- Smooth surface with a firm consistency and a tan-gray color
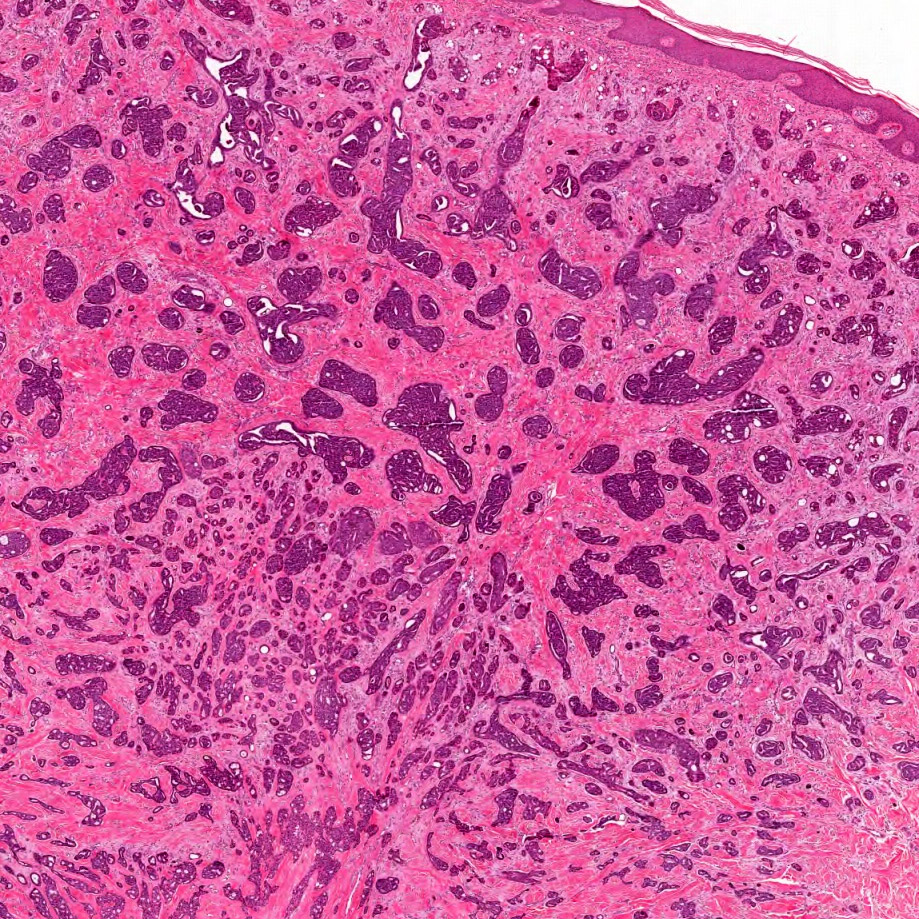
Frozen section description
- Frozen sections are only utilized to confirm diagnosis or verify that the surgical margins were negative
- Shows the characteristic histologic findings of PCACC: basaloid cells within dermis, arranged in cords and islands forming tubular structures and cribriform patterns
Frozen section images
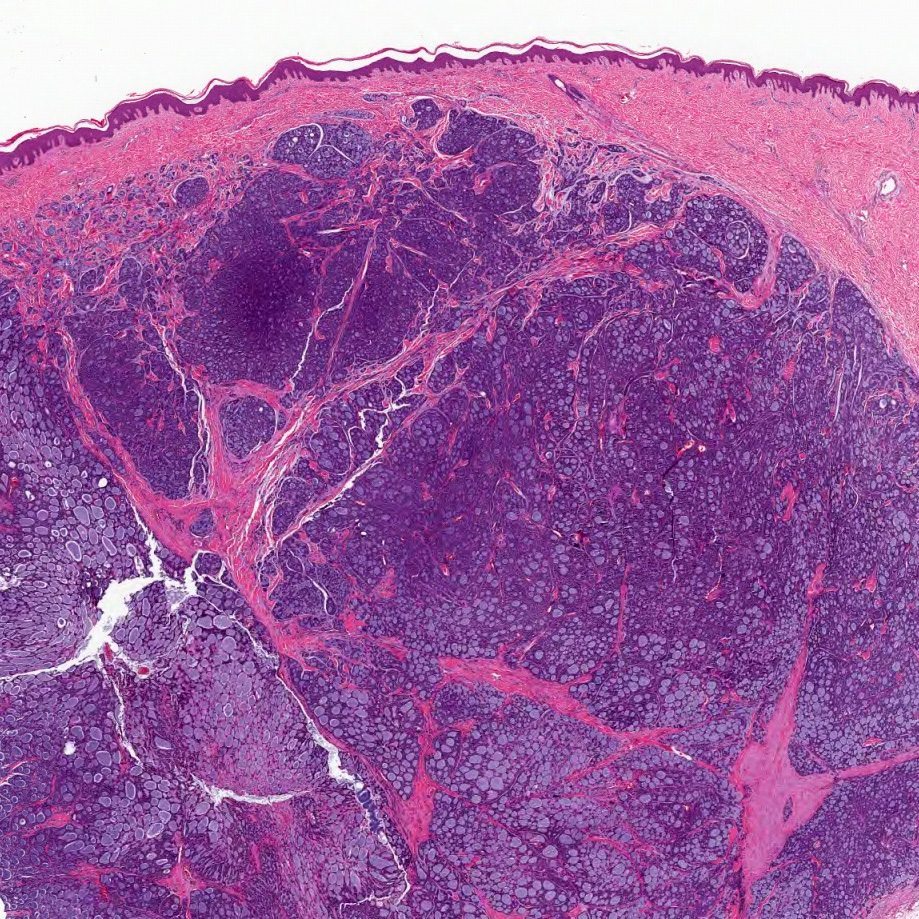
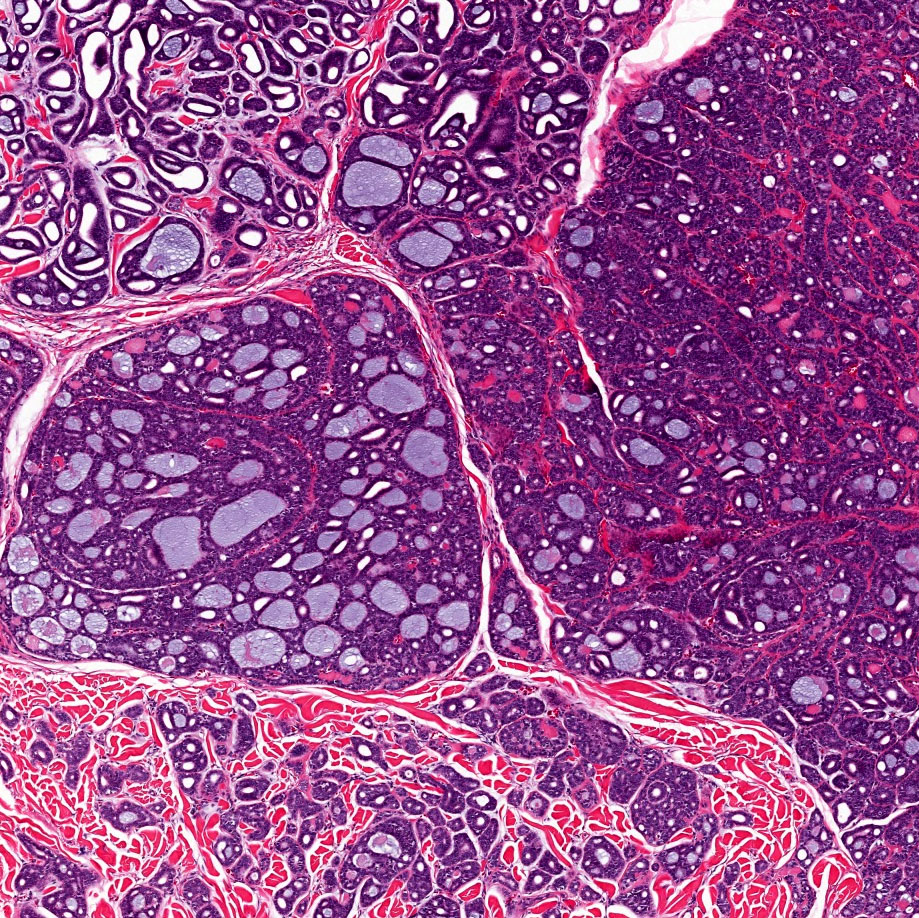
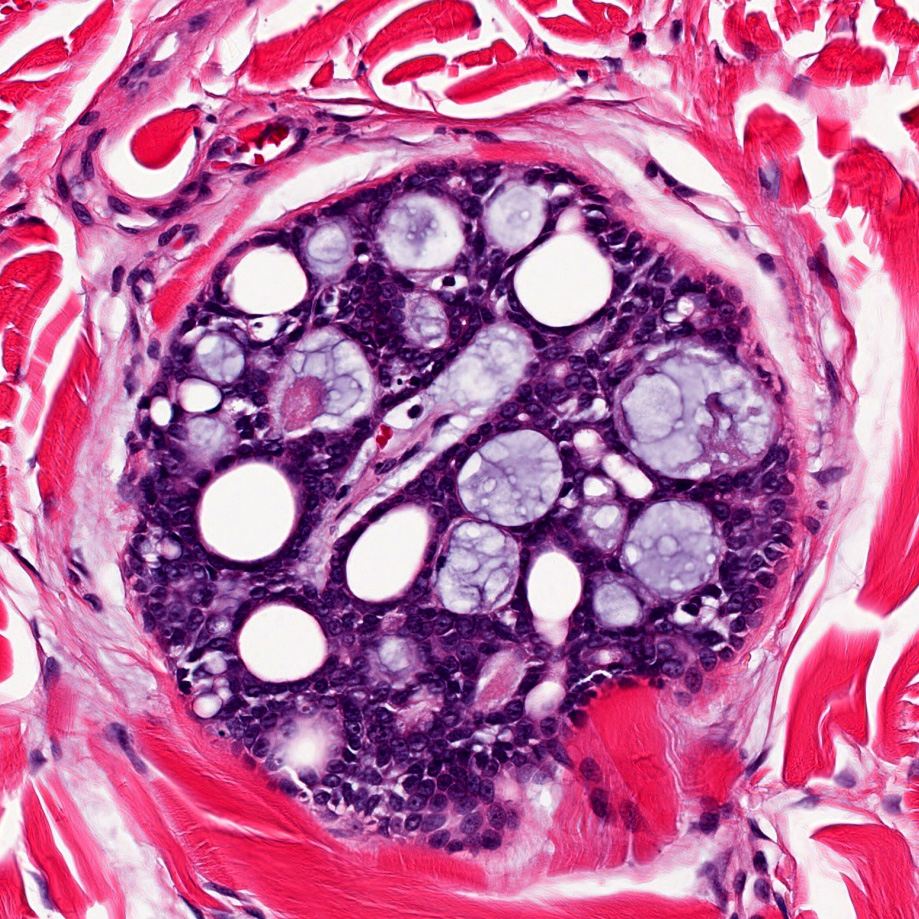
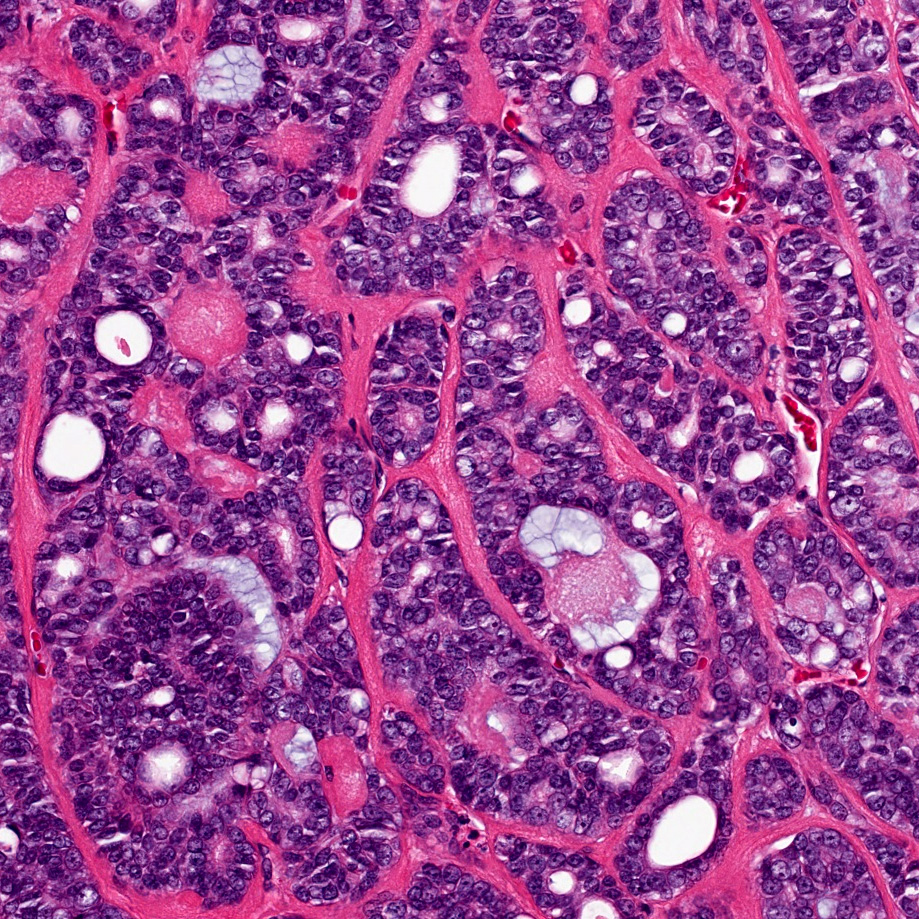
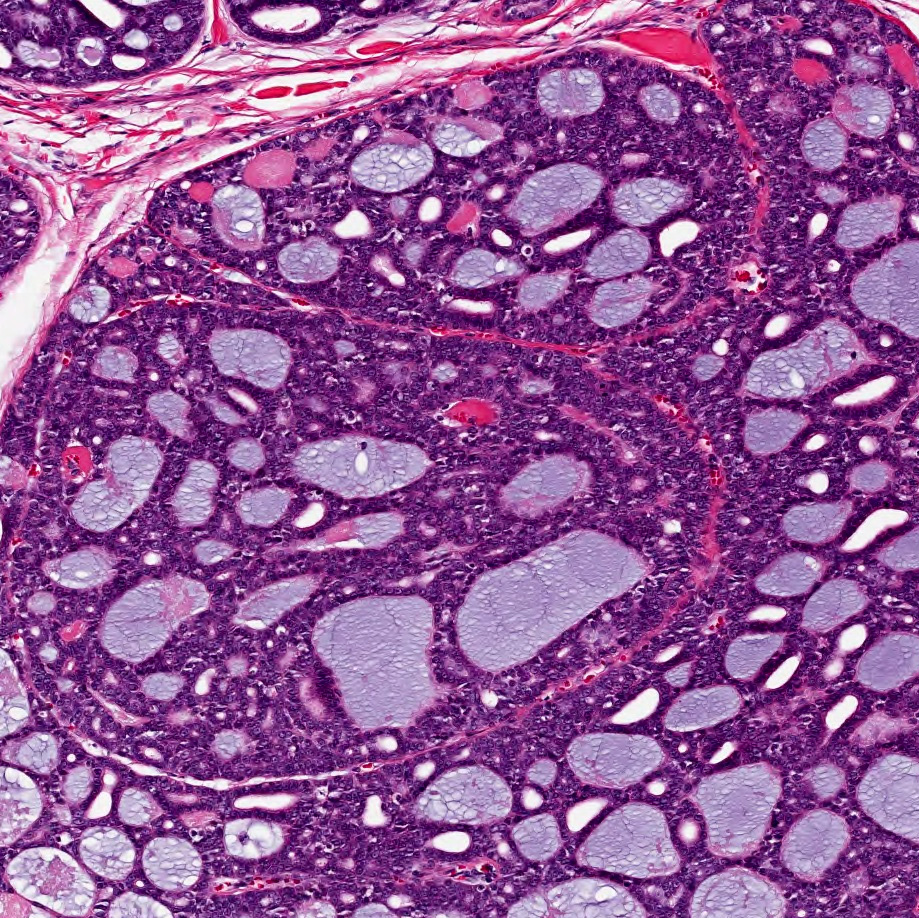
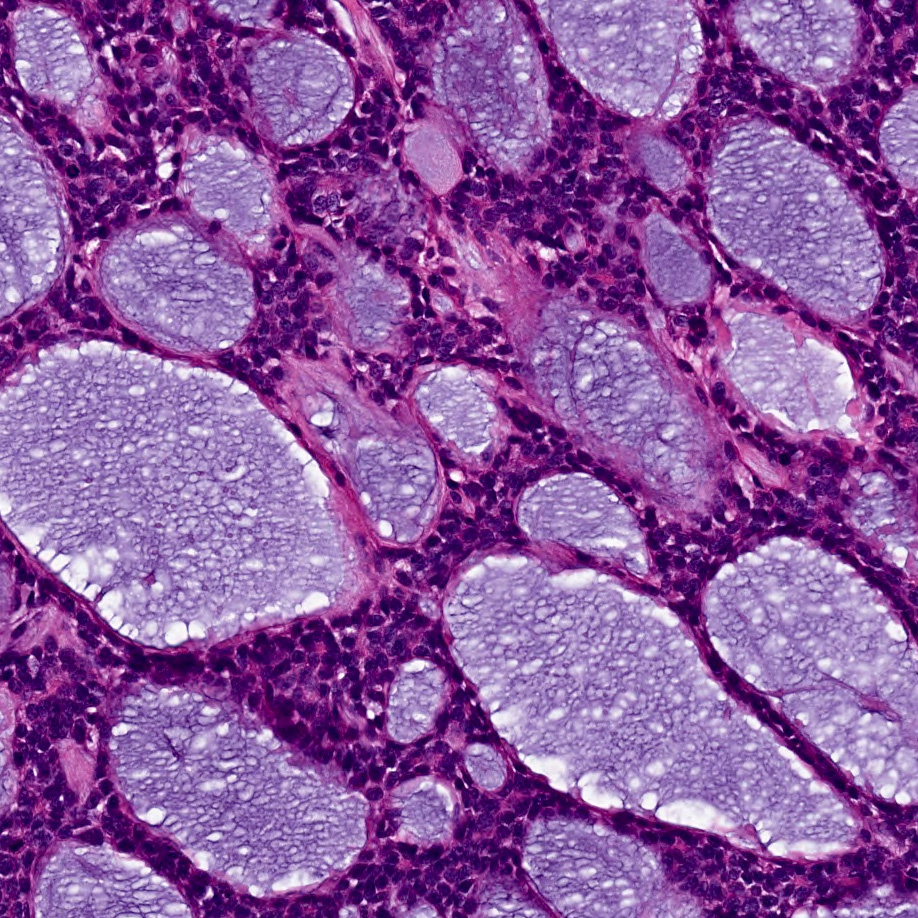
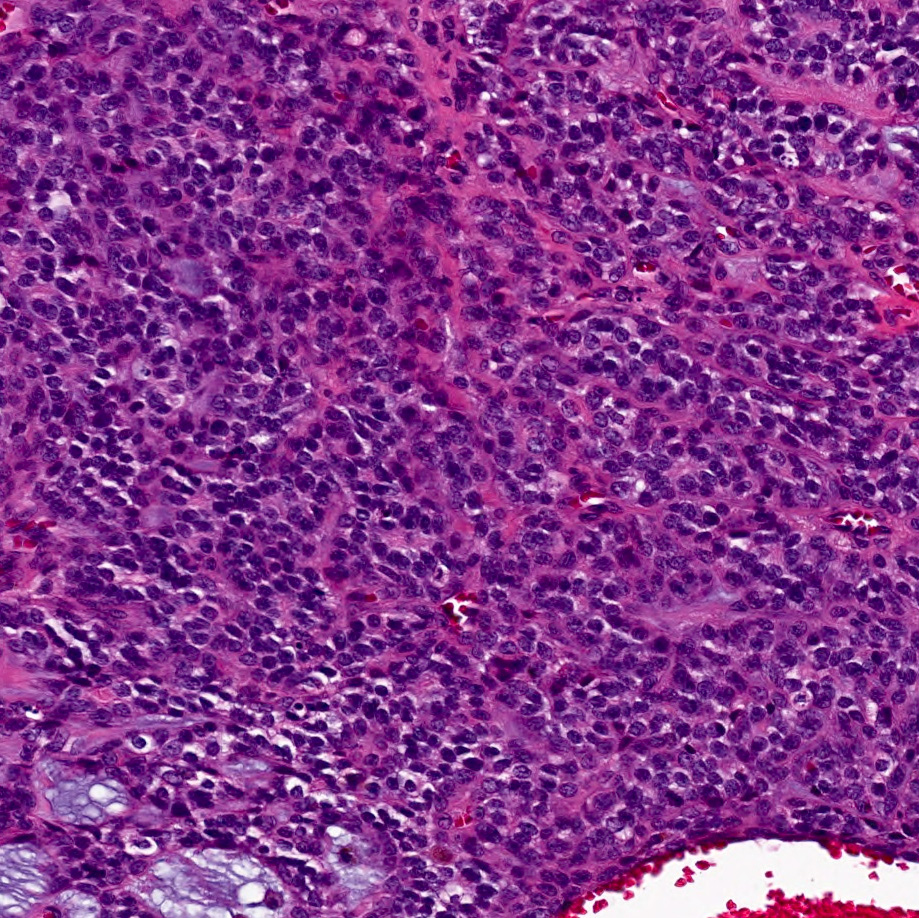
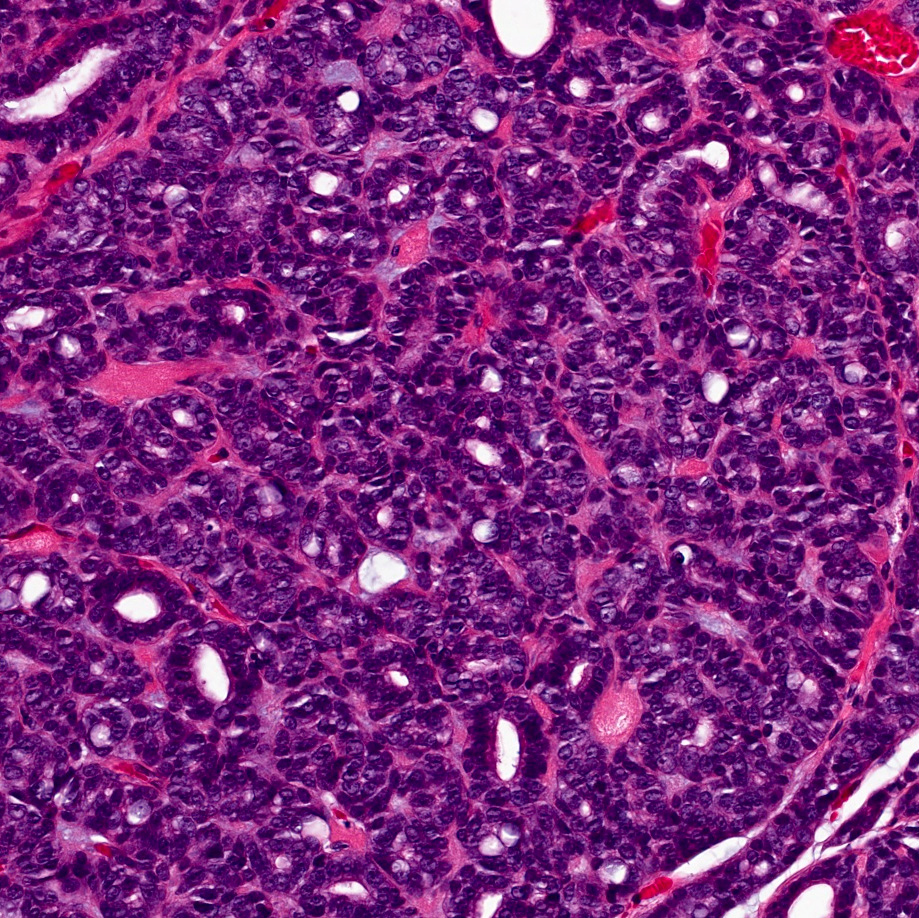
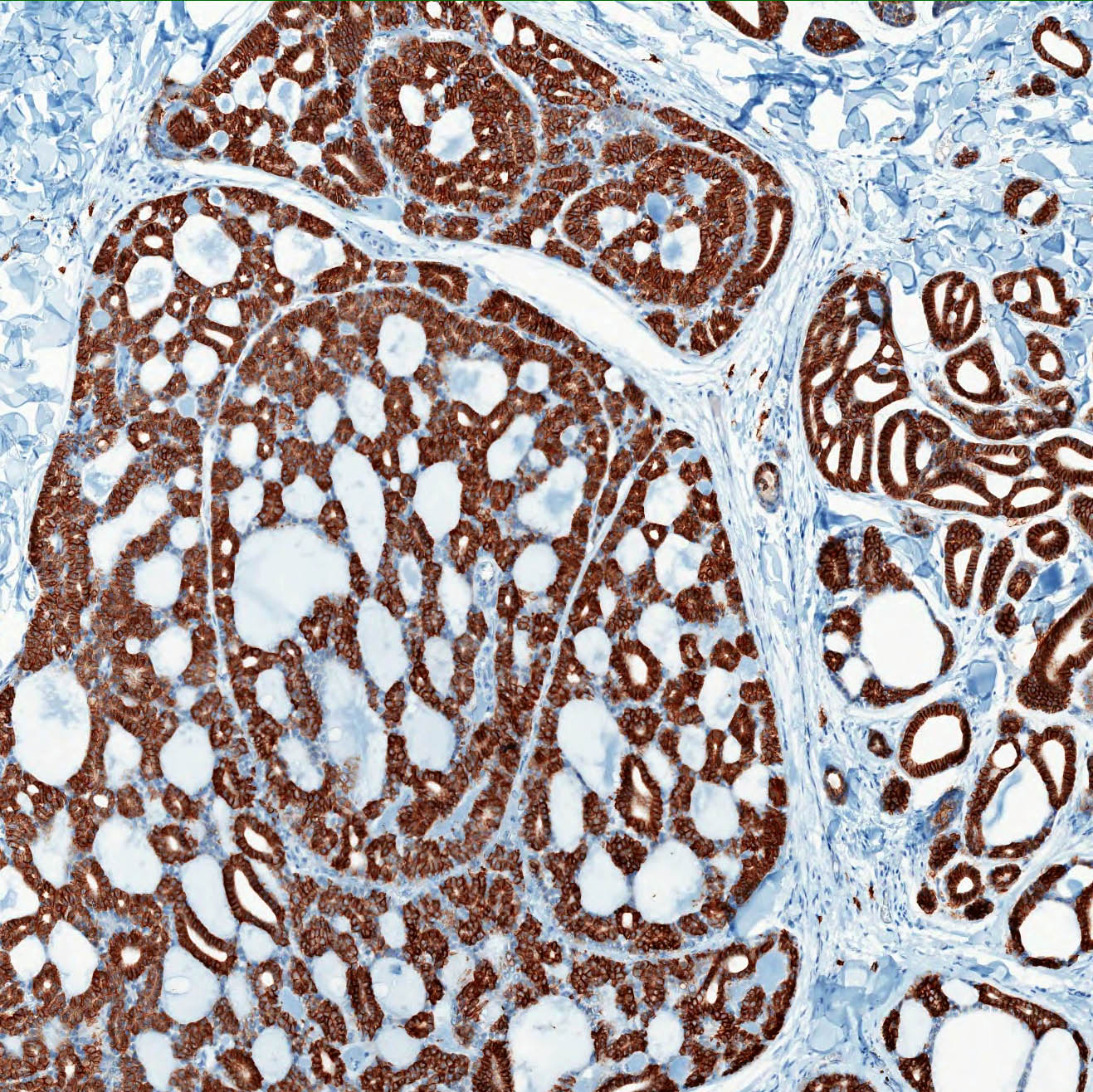
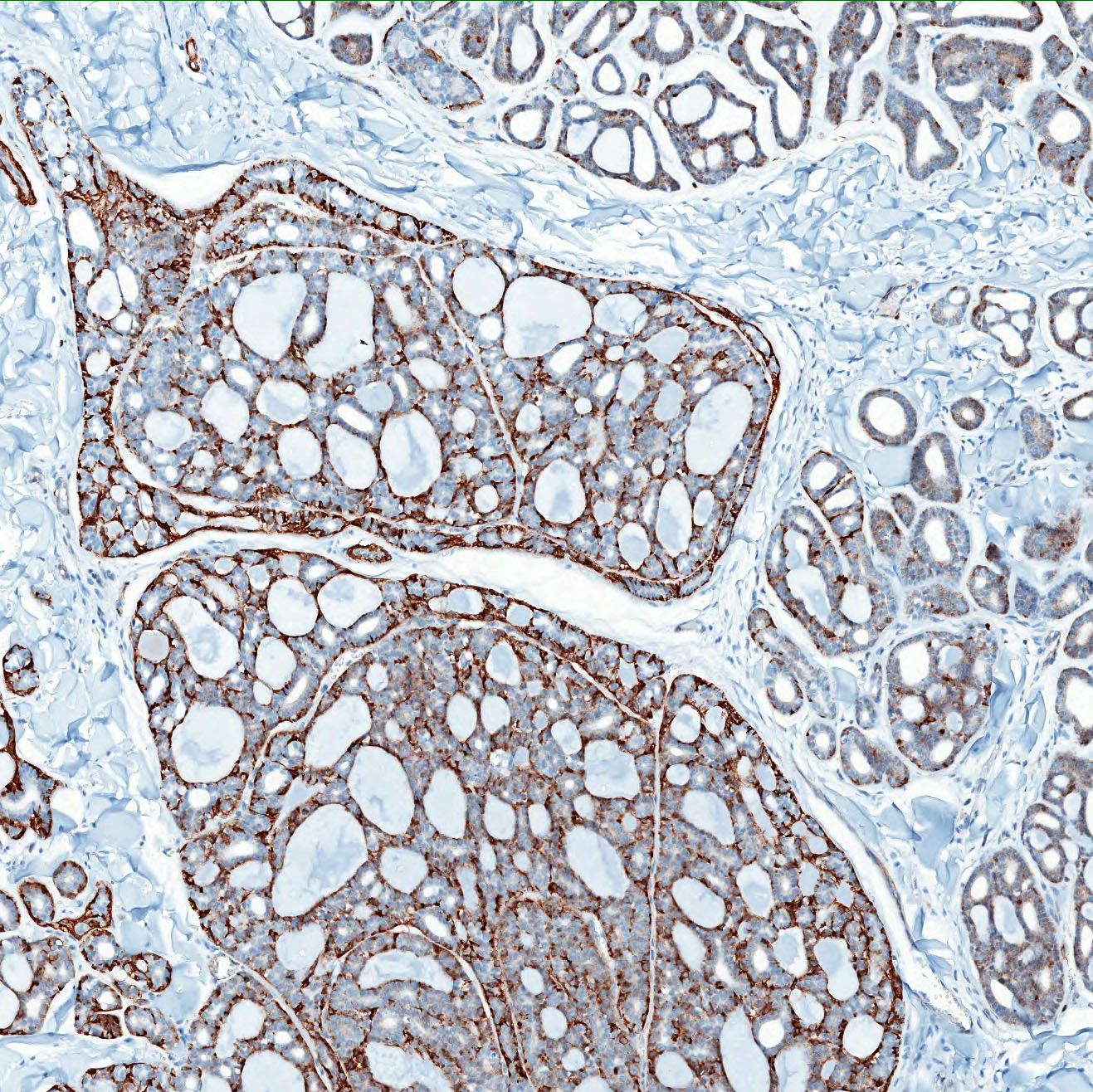
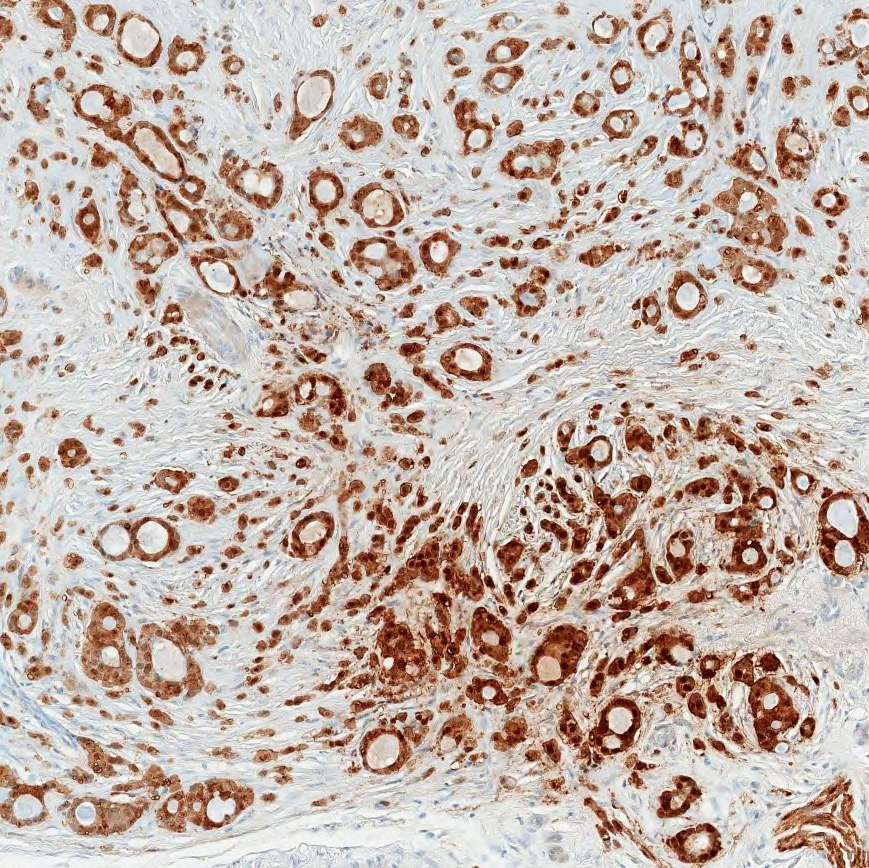
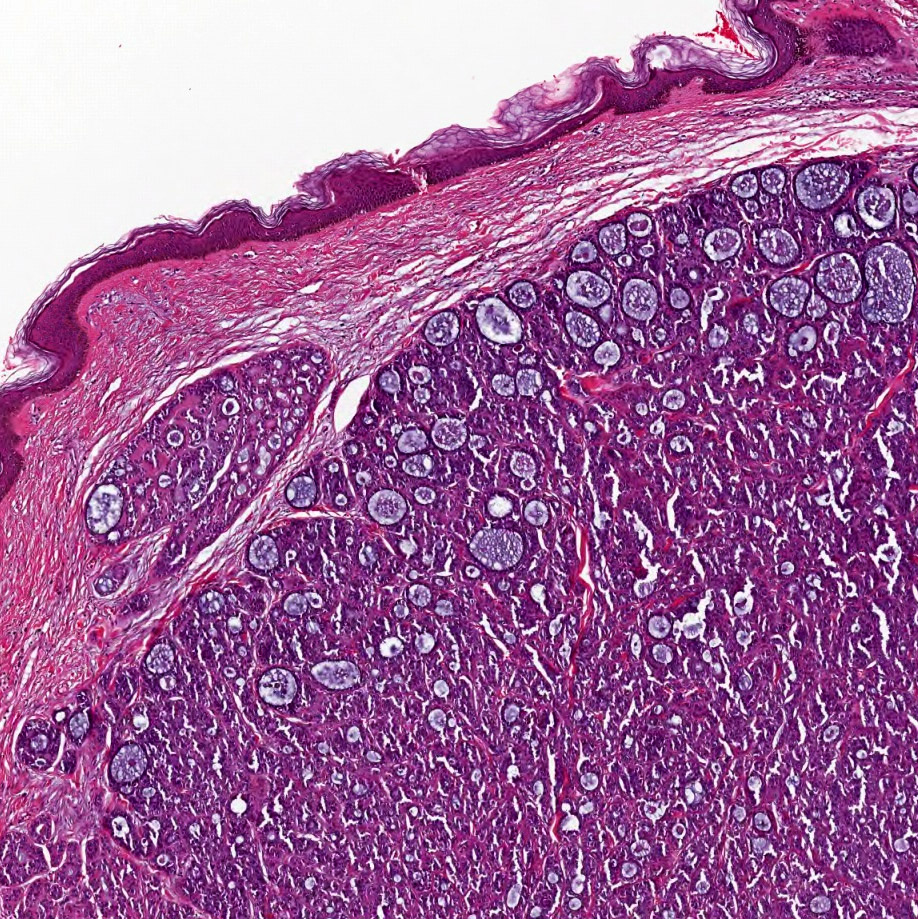
Microscopic (histologic) description
- Poorly circumscribed, dermal based basaloid neoplasm with numerous ductular and cystic spaces
- Often with subcutaneous extension; epidermal involvement unusual but has been reported (Am J Dermatopathol 2019;41:619)
- An essential diagnostic feature is the coexistence of true small bilayered ducts and pseudocysts (Histopathology 2022;80:407)
- Sparse ductal structures composed of inner epithelial cells surrounded by an outer layer of basal / myoepithelial cells; intraluminal secretion may be present
- Cystic spaces (larger than ducts) contain abundant basophilic mucinous material or hyalinized eosinophilic material
- Deposition of hyaline basement membrane material on the intraluminal aspect of cystic spaces
- Mixture of cribriform, tubular and solid patterns (Am J Surg Pathol 2013;37:1603)
- Cells are typically small and monomorphic appearing with hyperchromatic nuclei and scant cytoplasm
- Mitotic activity is typically low
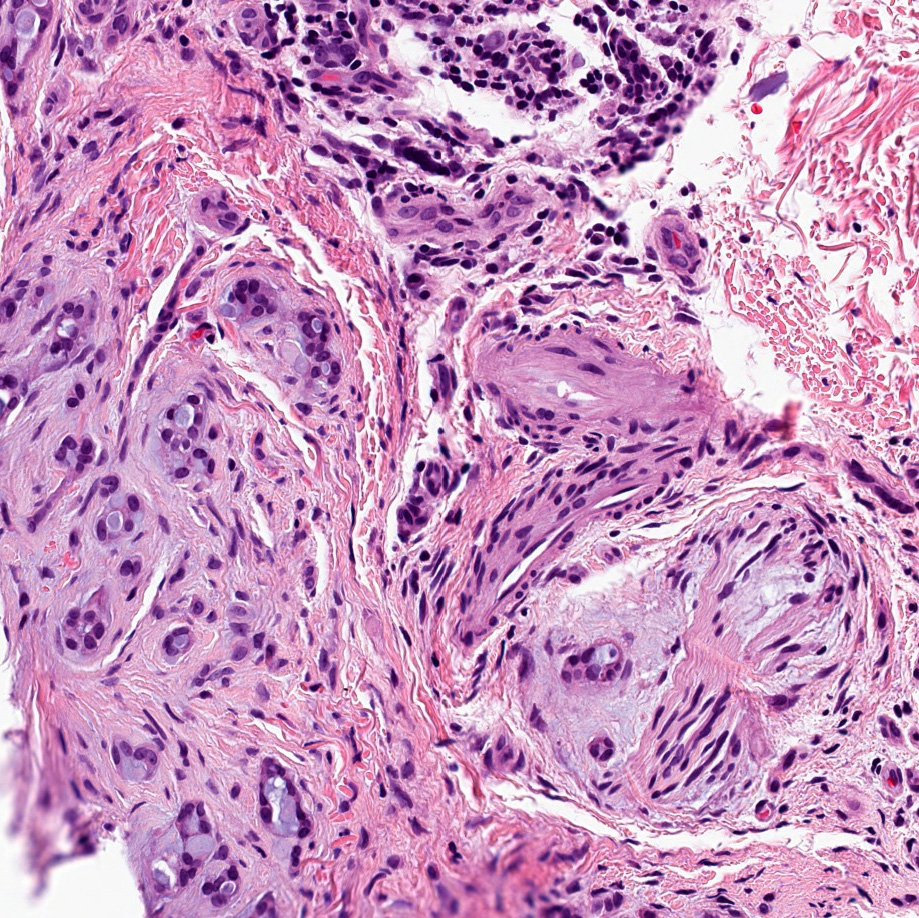
- Perineural invasion is a common finding
Grading criteria (Histopathology 2022;80:407)
| Grade I | Grade II | Grade III | |
| Histologic features |
|
|
|
| Solid area | None | < 30% | > 30% |
| Cytologic features | No cellular atypia | Atypia > grade I but < grade III | Significant cellular atypia |
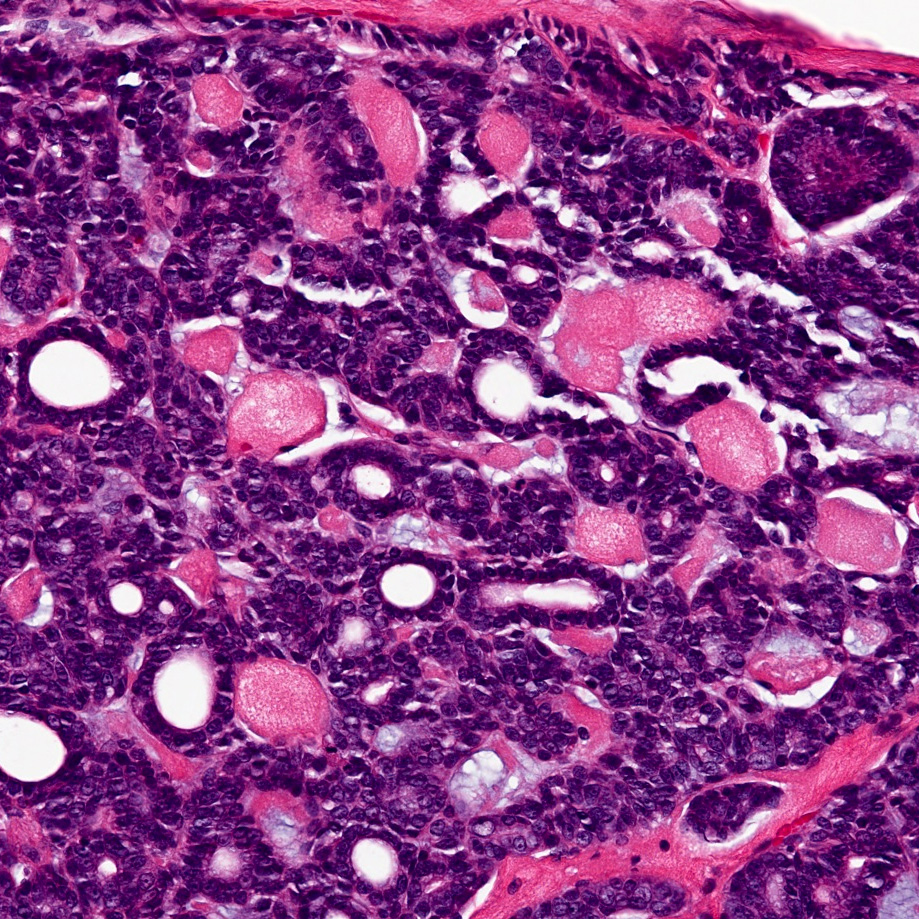
- High grade transformation (HGT), previously known as dedifferentiation
- Distinct population of anaplastic cells with loss of the biphasic ductal - myoepithelial differentiation
- Loss of myoepithelial cell differentiation is more usual; however, 1 PCACC case with HGT showed loss of epithelial cell differentiation and was diagnosed as myoepithelial carcinoma
- Nuclear enlargement, higher mitotic counts and necrosis are commonly seen
- Distinct population of anaplastic cells with loss of the biphasic ductal - myoepithelial differentiation
- HGT should be differentiated from solid type adenoid cystic carcinoma (ACC)
- With HGT, solid transformed areas are
- Separated from the tubular / cribriform component
- Have higher p53 and Ki67 expression
- Solid type ACC
- Solid cell nests are intermixed with cribriform and tubular structures throughout the tumor
- With HGT, solid transformed areas are
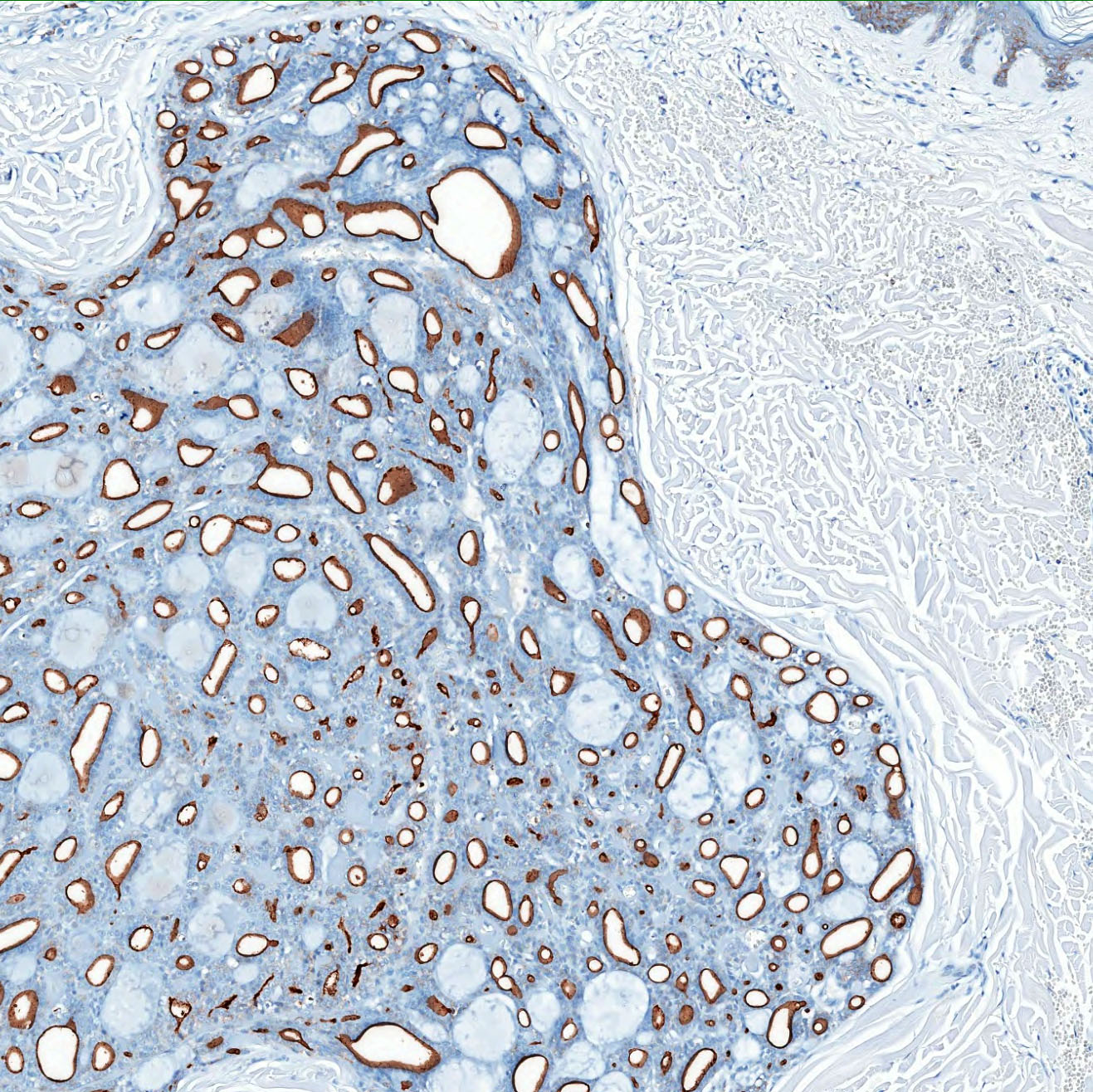
Microscopic (histologic) images
Contributed by Haya Homsi, M.D., M.P.H. and Shira Ronen, M.D.
Positive stains
- EMA, CEA monoclonal (mCEA), CK15 highlight the luminal cells in recognizable ductal structures (Am J Surg Path 2015;39:1347)
- CK7, CD117 (KIT), CD43 and BerEP4 (focally to diffusely positive) (Histopathology 2022;80:407, Case Rep Pathol 2017;2017:7949361, Pathology 2015;47:130)
- Myoepithelial cells surrounding ducts and pseudocysts stain positive for S100, p63, SMA, SMMS1, SOX10, MSA, calponin, GFAP, CK5/6 and 34 beta E12 (Am J Surg Pathol 2013;37:1603)
- Basophilic mucinous material within cystic spaces stains with mucicarmine, Alcian blue and colloidal iron (JAAD 1987;17:113)
- Hyalinized eosinophilic material surrounding true lamina gives a positive periodic acid-Schiff (PAS), diastase resistant reaction (J Oncol 2010;2010:469049)
- Basement membrane expresses collagen type IV; laminin is less marked (Am J Surg Pathol 2013;37:1603)
- MYB: it is crucial to highlight that the sole expression of MYB through immunostaining does not suffice for diagnosing PCACC as it is not specific and can be seen in other adnexal tumors, such as cylindromas (Histopathology 2022;80:407, J Cutan Pathol 2017;44:444, Am J Dermatopathol 2017;39:279)
Molecular / cytogenetics description
- ~60% of PCACC cases have been found to harbor MYB gene activations, either through MYB chromosomal abnormalities or MYB::NFIB fusion (J Cutan Pathol 2017;44:201)
- Less commonly, MYBL1 gene alterations have also been reported (Am J Dermatopathol 2018;40:721)
- According to one study, detection of MYB gene alterations does not necessarily correlate with MYB protein expression (i.e., MYB immunohistochemistry staining) (Histopathology 2022;80:407)
Videos
Primary cutaneous adenoid cystic carcinoma
Sample pathology report
- Skin, forehead, excision
- Adenoid cystic carcinoma (see comment)
- Comment: Sections demonstrate an excision specimen containing multiple foci of basaloid nodules with a cribriform architecture and duct formation. Lumen spaces are filled with blue mucin and eosinophilic basement membrane-like material. Cytologically, the tumor cells show scant to moderate pale eosinophilic cytoplasm and oval nuclei with vesicular chromatin. Significant pleomorphism and mitotic activity is not appreciated. Solid growth is not identified. Perineural invasion is present. The margins are negative for tumor.
- To further characterize this case, immunohistochemical stains with SMMS1, CD117 and SOX10 were performed and compared with appropriate controls. The tumor is positive for SOX10, CD117 and SMMS1.
- Molecular studies detected MYB gene rearrangement.
- The histologic and immunohistochemical findings support the diagnosis of adenoid cystic carcinoma. This could be a primary cutaneous lesion but a metastasis from a salivary gland tumor cannot be excluded. An appropriate clinical evaluation to rule out that possibility is recommended.
Differential diagnosis
- Metastatic adenoid cystic carcinoma:
- Can only exclude based on clinical history and imaging studies
- CK15 and vimentin may have some discriminatory value in differentiating between primary cutaneous and salivary gland ACCs; one study found that CK15 and vimentin showed diffuse positivity in 36% and 57% of PCACCs, respectively, whereas all salivary ACCs were negative or only focally positive for either CK15 or vimentin (Am J Surg Path 2015;39:1347)
- Basal cell carcinoma (adenoid type):
- Peripheral palisading
- Retraction artifact
- Mucinous stroma
- Attachment to epidermis often present
- Lack of true ductal structures with myoepithelial cells
- Focal areas of conventional basal cell carcinoma
- Cutaneous secretory carcinoma (Am J Surg Pathol 2017;41:62):
- Back to back tubules and microcysts with intraluminal secretions
- Positive for S100, mammaglobin, STAT5A and NTRK
- Primary cutaneous mucinous carcinoma:
- Primary cutaneous cribriform tumor (J Cutan Pathol 2005;32:577):
- Interconnected cribriform lesion that varies in size and shape
- Focal solid areas
- More eosinophilic cells
- Lacks myoeithelial cells
- Perineural invasion not a common feature
- Cylindroma / spiradenoma:
- Cylindroma: absence of prominent cystic / ductal spaces with mucin
- Spiradenoma: presence of dilated vascular spaces and numerous lymphocytes
- Lack perineural invasion
- Recognition of the typical areas
- Cylindroma: well circumscribed, symmetrical lesion composed of multiple aggregates of basaloid cells surrounded by a prominent basement membrane that appear to fit together in jigsaw puzzle arrangement
- Spiradenoma: regular nodules of small basaloid cells admixed with lymphocytes and basement membrane material
Additional references
Practice question #1
Practice answer #1
C. Perineural invasion is a common finding. Perineural invasion is very common in adenoid cystic carcinoma (ACC). Answer A is incorrect because metastasis from primary cutaneous ACC is rare. Answer B is incorrect because the head and neck, followed by the trunk, are the most common sites. Answer D is incorrect because it appears as a solitary nodule.
Comment Here
Reference: Adenoid cystic carcinoma (primary cutaneous)
Comment Here
Reference: Adenoid cystic carcinoma (primary cutaneous)
Practice question #2
A 70 year old man presented with a scalp nodule. Microscopic examination showed cribriform nests and columns of bland cells arranged concentrically around gland-like spaces filled with homogenous basophilic material. Testing for mutation in which gene should be recommended for this patient?
- CYLD
- BHD
- EGFR
- MYB
Practice answer #2
D. MYB. MYB and MYBL1 gene alterations, including MYB::NFIB or MYBL1::NFIB fusions, are frequently detected in adenoid cystic carcinoma (ACC). Answer A is incorrect because CYLD gene alterations are seen in cylindromas, spiradenomas and trichoepitheliomas. Answer B is incorrect because pathogenic BHD mutations are seen in Birt-Hogg-Dubé syndrome. Answer C is incorrect because EGFR gene alternations are not seen in ACC.
Comment Here
Reference: Adenoid cystic carcinoma (primary cutaneous)
Comment Here
Reference: Adenoid cystic carcinoma (primary cutaneous)