Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Turashvili G. Yolk sac tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumoryolksac.html. Accessed August 21st, 2025.
Definition / general
- Primitive germ cell tumor with a variety of morphologic patterns, ranging from endodermal extraembryonic structures (secondary yolk sac, allantois) to, less commonly, endodermal somatic tissues (intestine, liver, mesenchyme)
Essential features
- Most common before the age of 30
- Usually occurs as a pure form or rarely as a component of a mixed germ cell tumor
- Numerous morphologic patterns, with the hallmark Schiller-Duval bodies in some cases and immunohistochemical expression of SALL4, glypican 3 and AFP
- Often associated with elevated serum alpha fetoprotein (AFP)
- Usually favorable clinical outcomes due to chemosensitivity
Terminology
- Primitive endodermal tumor (not recommended)
- Endodermal sinus tumor (not recommended)
ICD coding
- ICD-O: 9071/3 - yolk sac tumor
- ICD-10: C56 - malignant neoplasm of ovary
- ICD-11
- 2C73.5 - endodermal sinus tumor, unspecified site, female
- 2C73.Y & XH09W7 - other specified malignant neoplasms of the ovary & yolk sac tumor
Epidemiology
- ~20% of malignant germ cell tumors of the ovary (Obstet Gynecol 2006;107:1075)
- Second most common malignant ovarian germ cell tumor after dysgerminoma
- Mean age is 19 years; most common in the second and third decades of life (Int J Surg Pathol 2014;22:677)
Sites
- Usually ovary
- Less common in uterus, vagina, vulva and peritoneum (Am J Surg Pathol 2017;41:1)
Pathophysiology
- Chromosome 12 abnormalities, usually isochromosome 12p, in ~75% of patients (Cancer Res 1998;58:3105)
Clinical features
- Abdominal enlargement or pain
- Lower abdominal or pelvic mass (Int J Surg Pathol 2014;22:677)
- Rarely hormonal manifestations
Diagnosis
- Microscopic examination
Laboratory
- Elevated serum levels of AFP (may be used diagnostically and in monitoring therapy)
Radiology description
- Ultrasonography:
- Both echogenic and hypoechoic components (AJR Am J Roentgenol 1996;167:791)
- Computed tomography:
- Usually appears as a unilateral large complex mass with solid and cystic components, heterogeneous enhancement and enlarged intratumoral vessels with hemorrhage and capsular tear (Acta Radiol 2016;57:197)
- Helpful features for differentiating yolk sac tumor from other ovarian tumors include a mixed solid / cystic nature, intratumoral hemorrhage, marked enhancement and dilated intratumoral vessels (Sci Rep 2015;5:11000)
- Intratumoral calcification and fatty tissue if associated with teratoma
- Magnetic resonance imaging:
- Prominent signal voids (J Comput Assist Tomogr 2000;24:605)
- Often with areas of hemorrhage
Prognostic factors
- Usually favorable prognosis due to chemosensitivity, with complete cure in > 80% of cases
- Stage dependent, with 5 year survival rates of > 95% for stage I - II, 70% for stage III and 50% for stage IV (Gynecol Oncol 2017;147:296, Int J Gynecol Cancer 2018;28:77)
- Prominent polyvesicular vitelline pattern associated with more indolent behavior (Am J Surg Pathol 2013;37:393)
- Pure hepatoid and glandular intestinal type yolk sac tumors associated with poorer prognosis
Case reports
- 12 year old girl with ovarian yolk sac tumor presenting with acute abdominal pain and elevated serum AFP (Acta Biomed 2019;90:599)
- 17 year old girl with bilateral metachronous ovarian yolk sac tumors (J Pediatr Adolesc Gynecol 2017;30:259)
- 19 year old woman with mixed germ cell tumor (yolk sac tumor and choriocarcinoma) arising in gonadoblastoma (Int J Surg Pathol 2018;26:287)
- 20 year old woman with fertility sparing surgery for ovarian yolk sac tumor (J Clin Diagn Res 2017;11:QD12)
- 21 year old woman with ovarian yolk sac tumor associated with granulomatous reaction resembling tuberculosis (Turk Patoloji Derg 2016;32:126)
Treatment
- Unilateral salpingo-oophorectomy (Eur J Surg Oncol 2006;32:1063)
- Adjuvant multiagent combination chemotherapy
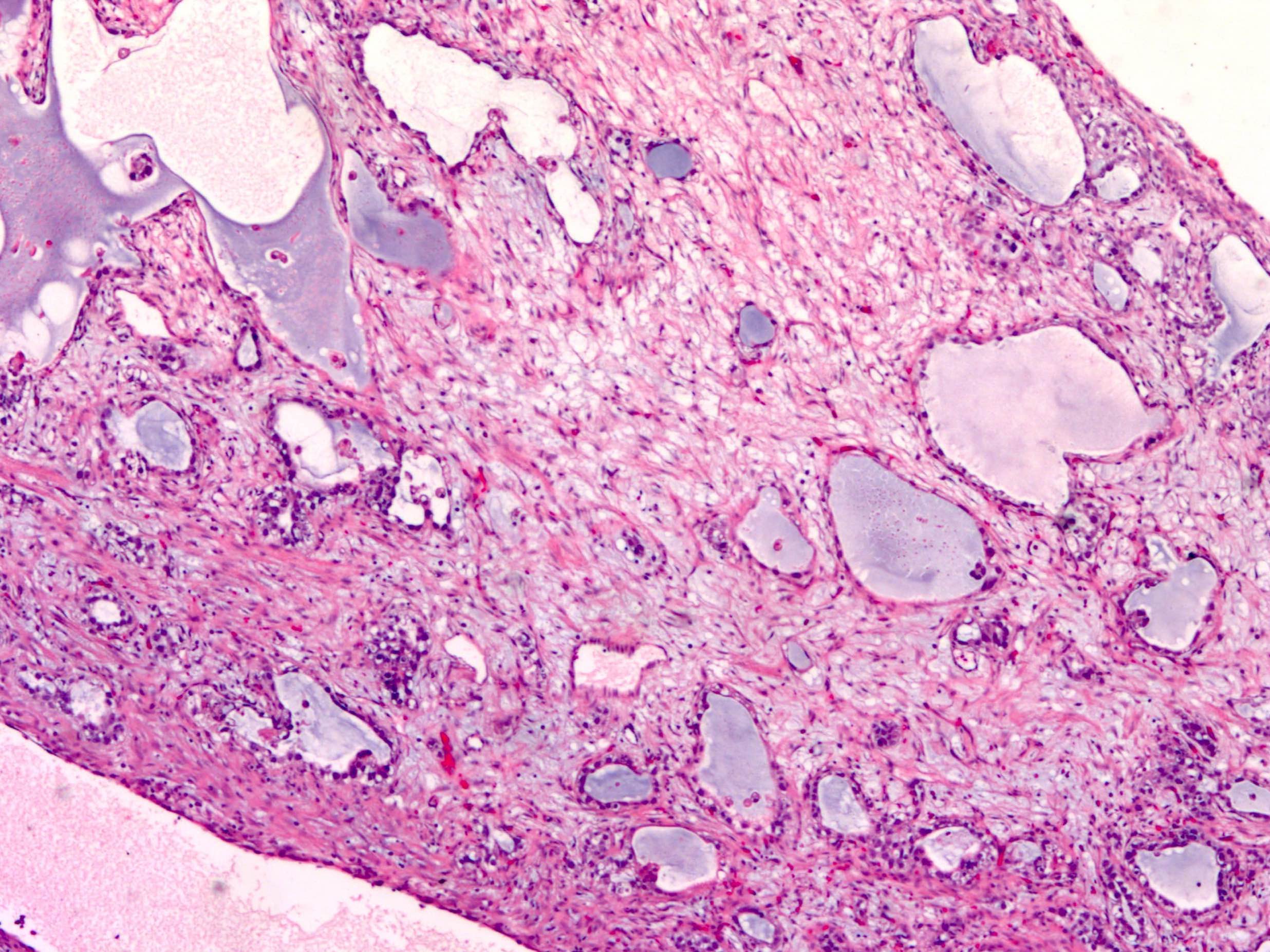
Gross description
- Usually unilateral ovarian mass with predilection for right ovary
- Encapsulated with smooth and glistening surface, round, oval or globular, may be firm or somewhat lobulated
- Rupture in 25% of cases (Int J Surg Pathol 2014;22:677)
- Mean size 15 cm (range 3 - 30)
- Fleshy, gray-yellow to gray-tan, solid and cystic friable cut surface, often with gelatinous changes and areas of hemorrhage and necrosis (Cancer 1976;38:2404)
- May form adhesions to surrounding structures
- When part of a mixed germ cell tumor, other components, such as a mature cystic teratoma or dysgerminoma, may be grossly recognizable
- Honeycomb appearance (multiple small cysts) on cut surface if polyvesicular vitelline component is present (Am J Surg Pathol 2013;37:393)
Gross images
Frozen section description
- Admixure of characteristic growth patterns and tumor cells with clear to eosinophilic cytoplasm, variable cytologic atypia and mitotic activity, with or without Schiller-Duval bodies
Frozen section images
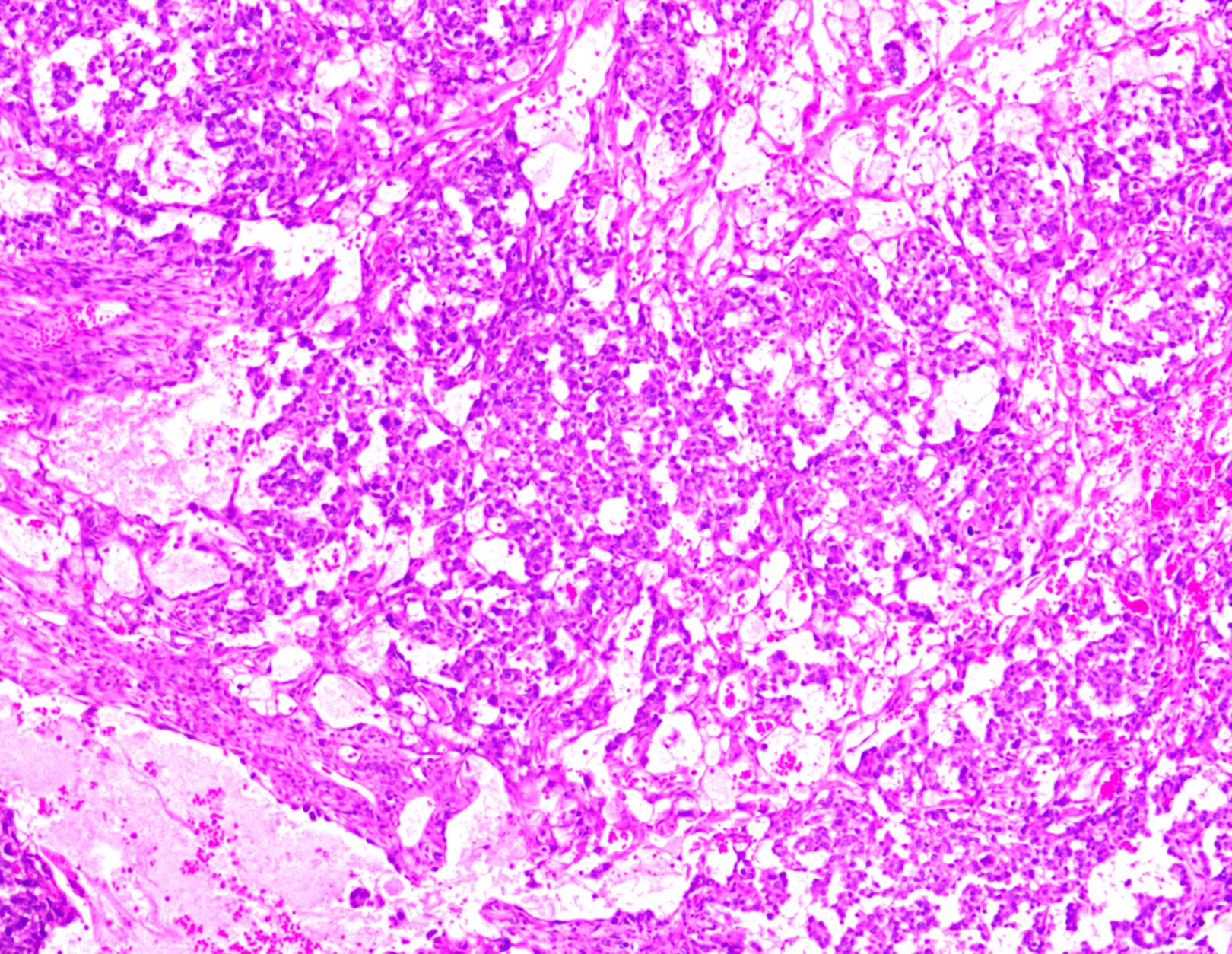
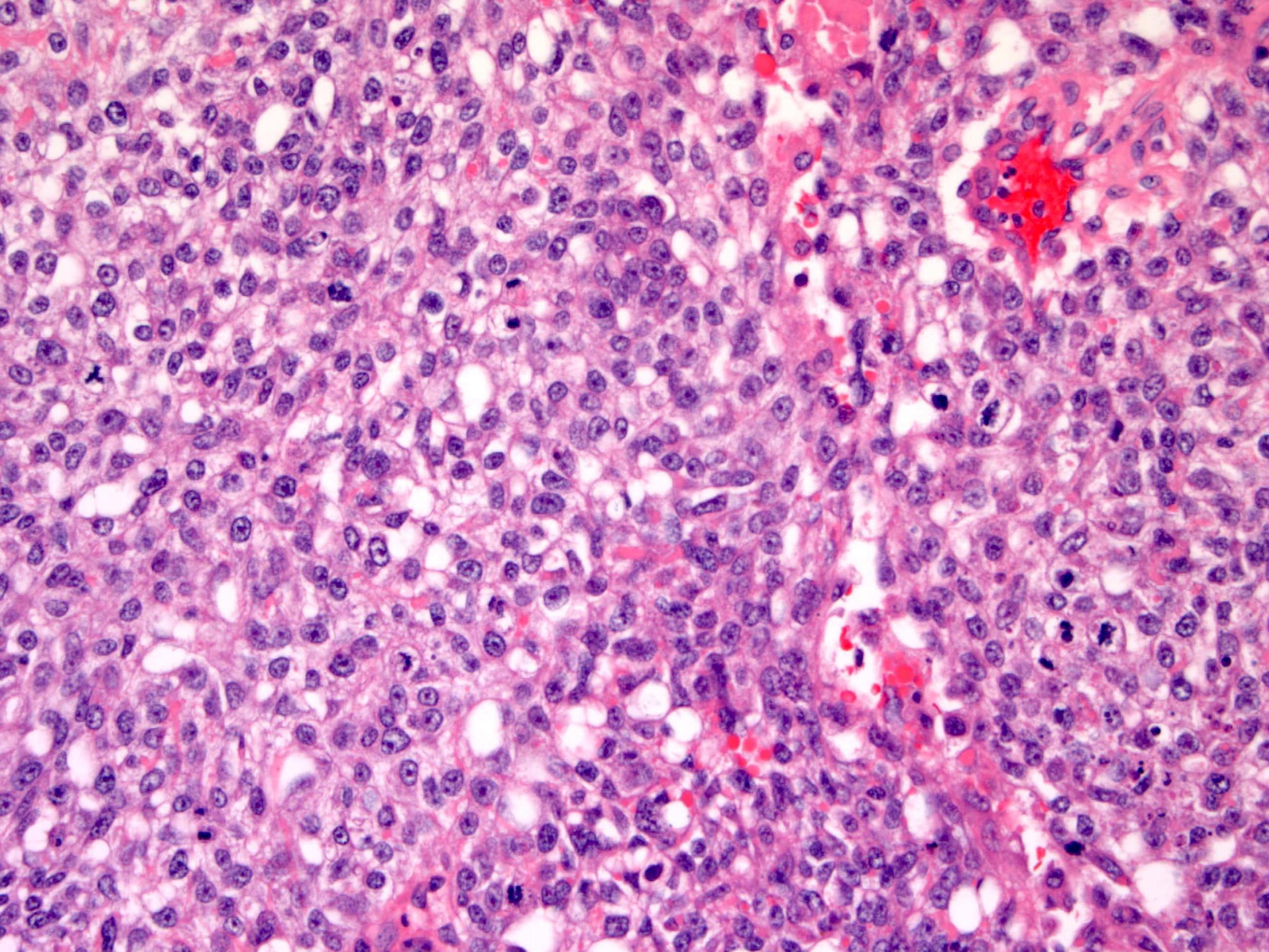
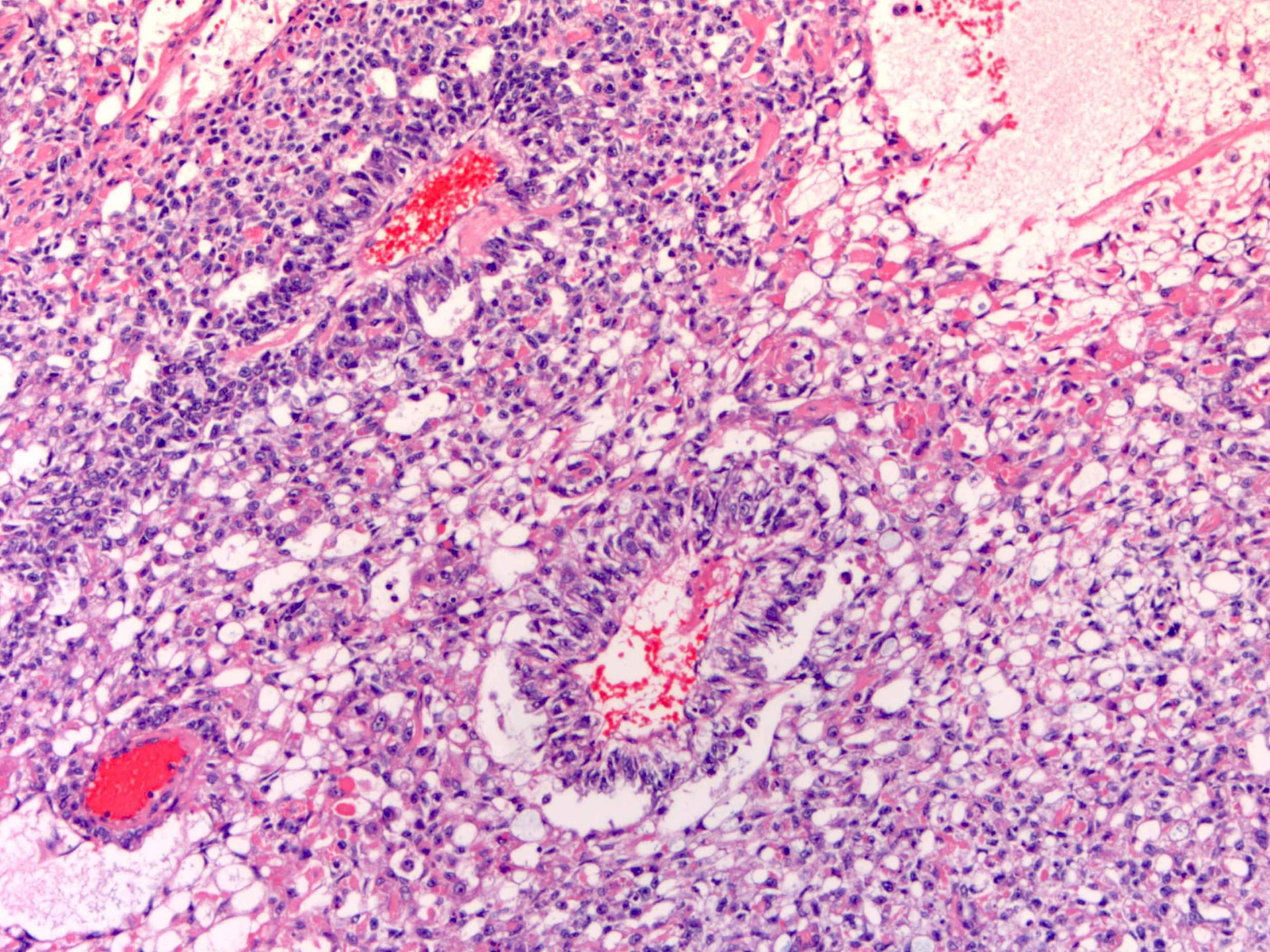
Microscopic (histologic) description
- Multiple histologic patterns with predominance of 1 or 2 patterns
- Reticular / microcystic pattern:
- Most common pattern
- Loose meshwork of anastomosing channels and variably sized cysts (macro or microcysts) lined by primitive tumor cells with varying amounts of clear to eosinophilic cytoplasm (Cancer 1976;38:2404, Histopathology 2012;60:1023, Int J Surg Pathol 2014;22:677)
- Lining cells may be flattened and deceptively bland
- Tumor cells occasionally contain lipid and have a signet ring-like morphology
- Cysts may contain eosinophilic hyaline globules and amorphous, eosinophilic acellular basement membrane-like material
- Loose, hypocellular or myxoid stroma
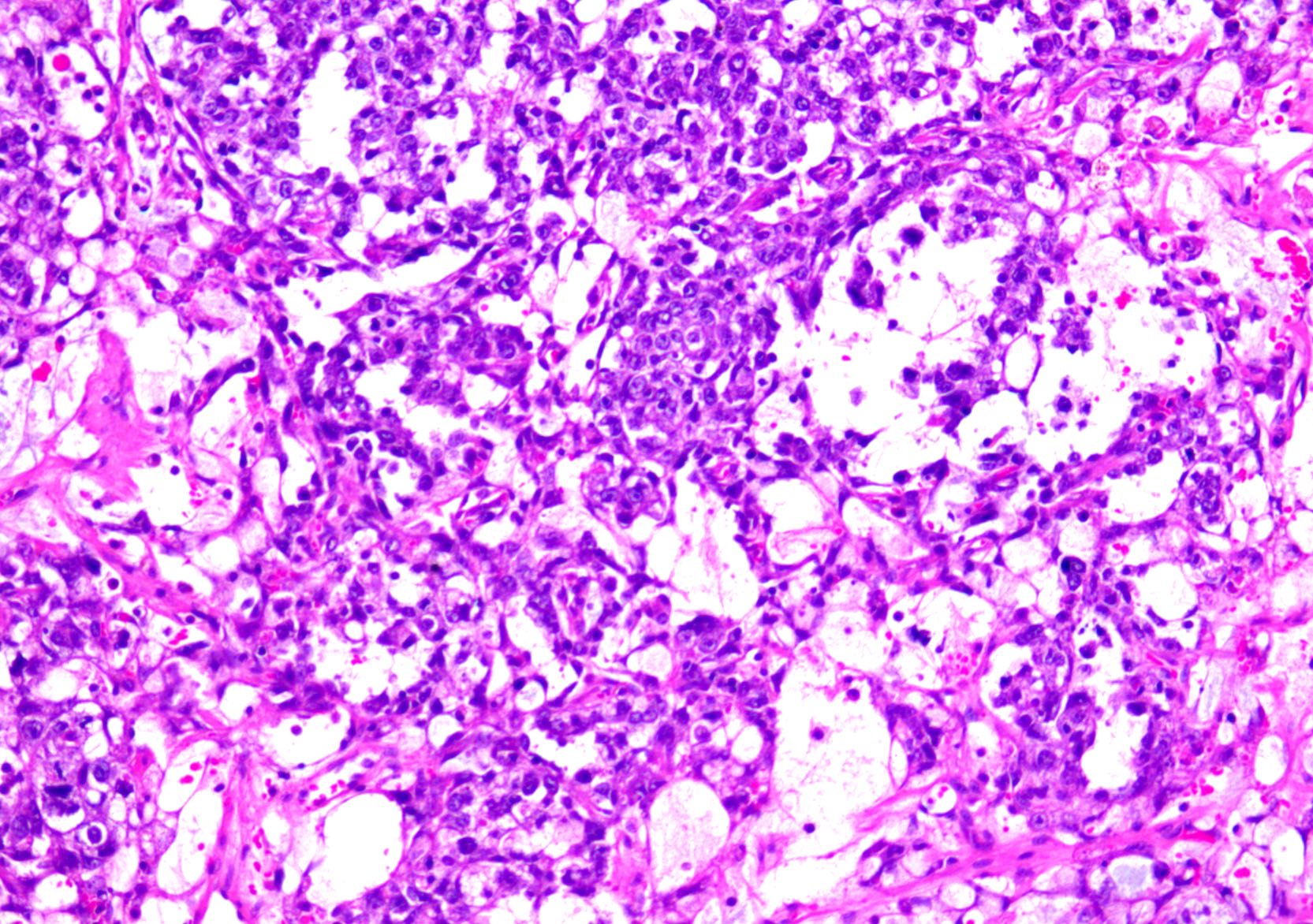
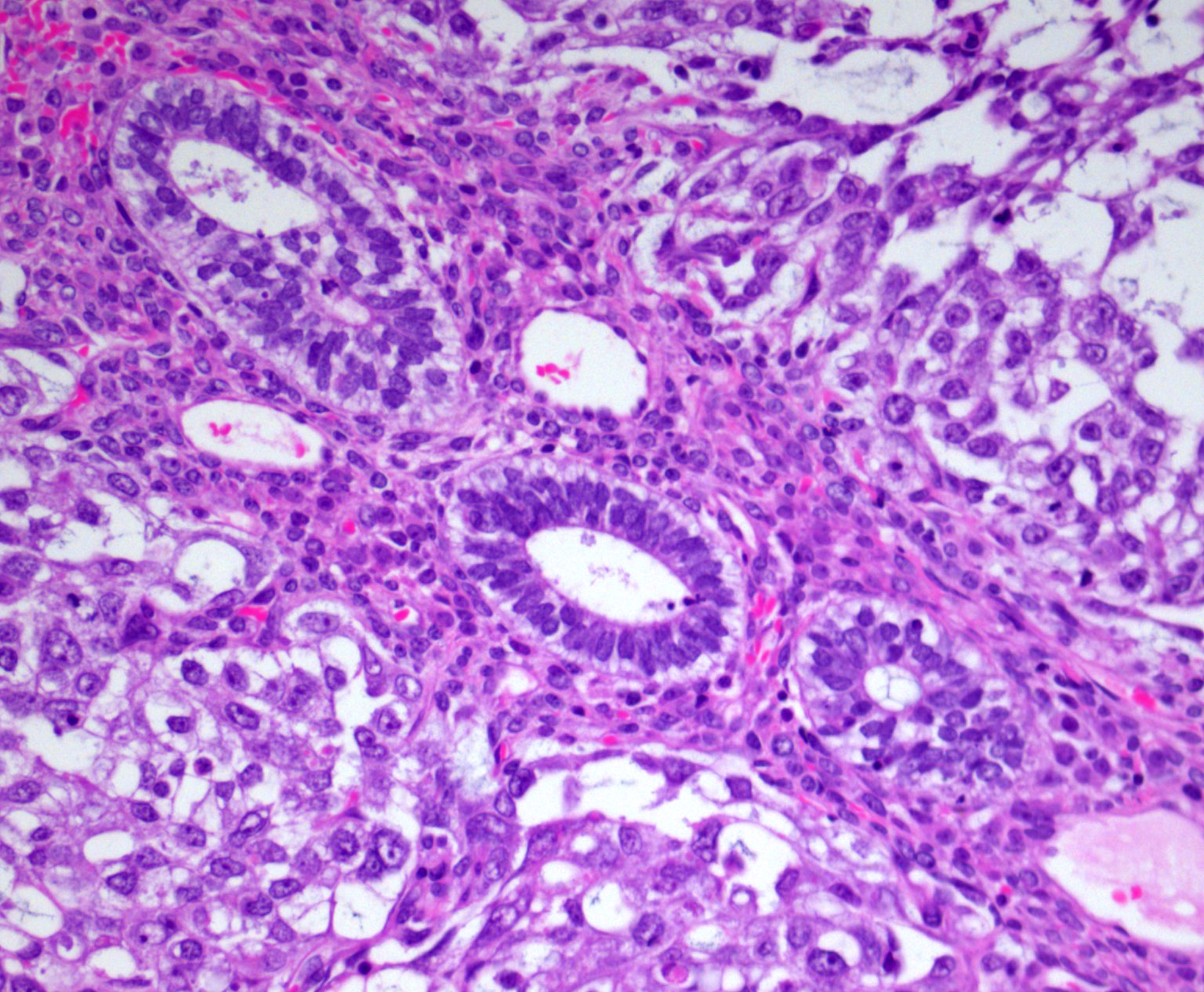
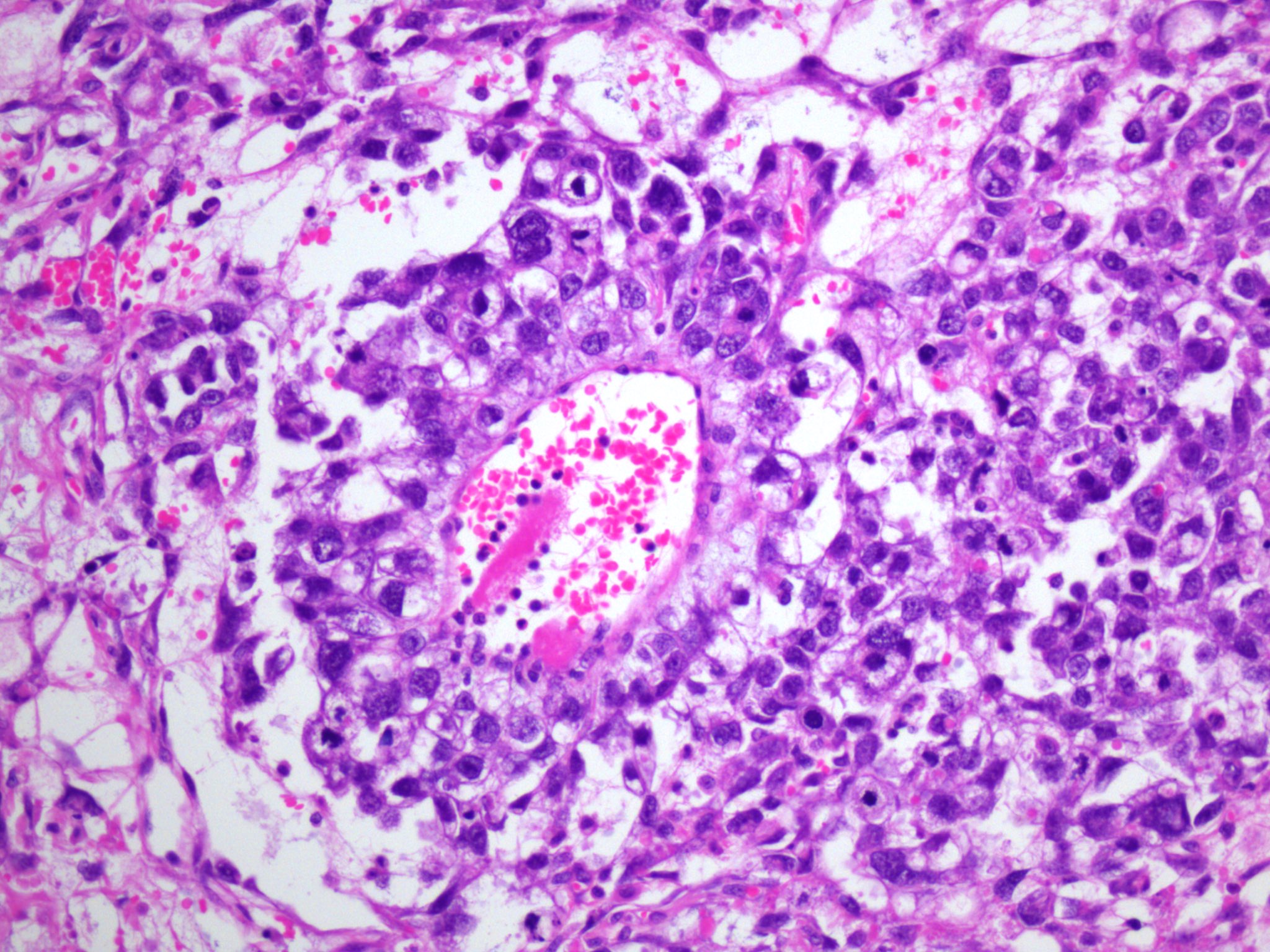
- Endodermal sinus pattern:
- Anastomosing network of labyrinthine-like spaces lined by tumor cells
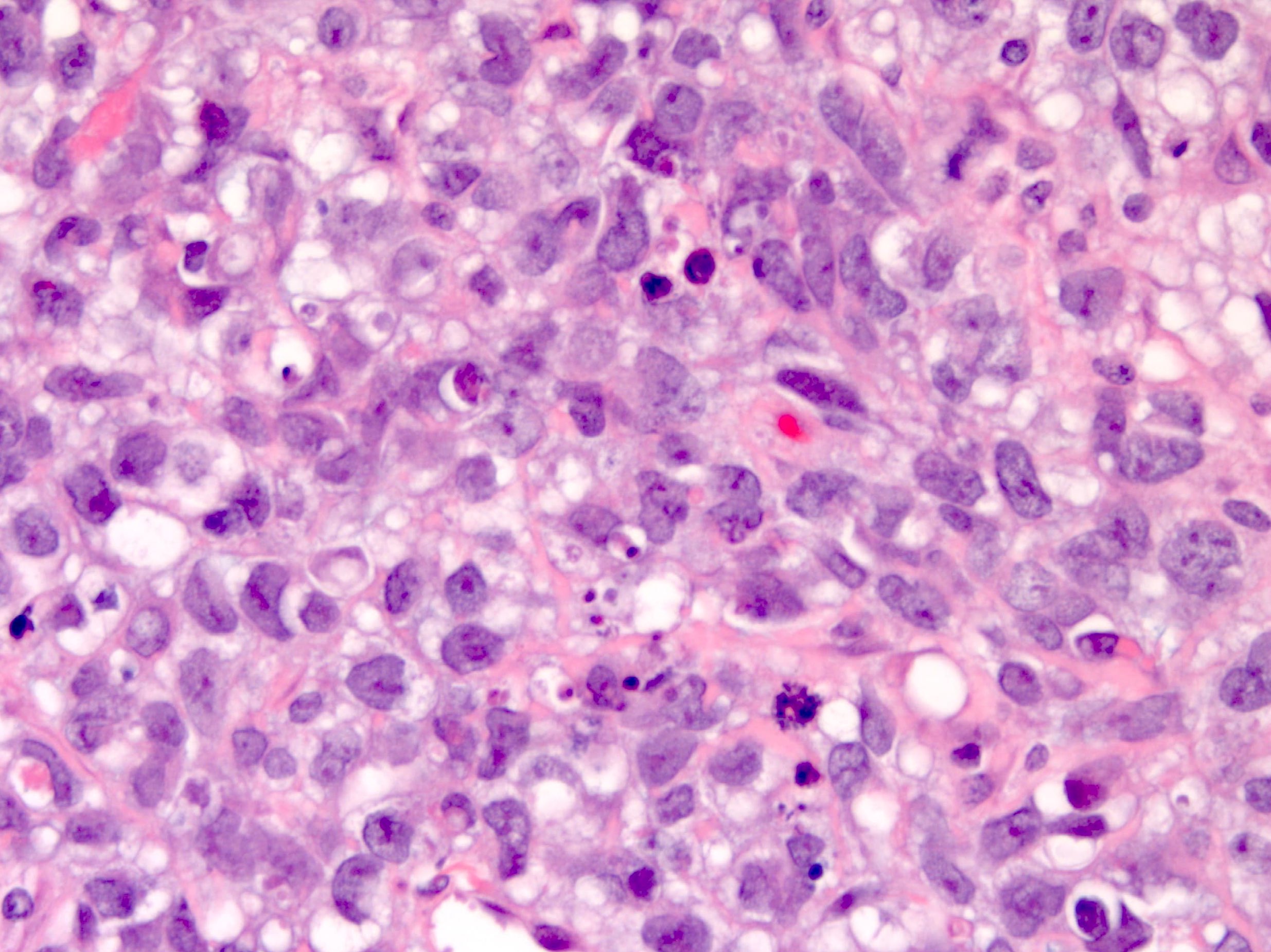
- Formation of vaguely glomeruloid perivascular structures (Schiller-Duval bodies)
- Hallmark of yolk sac tumor but their absence does not rule out the diagnosis
- Variably present, ranging from 20 - 75% of cases (Surg Pathol Clin 2019;12:621)
- Rounded to elongated papillary structures containing a central fibrovascular core with a single central vessel, surrounded by tumor cells projecting into a cystic / sinusoidal space (resembling immature glomeruli) (Histopathology 2012;60:1023)
- Papillary pattern:
- Papillae containing fibrovascular cores lined by pleomorphic tumor cells with brisk mitoses
- Fibrovascular cores may be hyalinized
- May contain tumor giant cells (mono or multinucleated)
- Solid pattern:
- Sheets of polygonal tumor cells with large vesicular or pyknotic nuclei with prominent nucleoli, brisk mitoses, clear to eosinophilic cytoplasm and well defined borders, sometimes with prominent hyaline globules
- Cells may be smaller and more blastema-like with scant cytoplasm
- May contain tumor giant cells (mono or multinucleated)
- Festoon pattern:
- Complex ribbons and undulating cords
- Occasionally with a drape-like arrangement
- Glandular pattern (forming endodermal somatic derivatives):
- Endometrioid type areas with glandular or villoglandular structures lined by single or multiple layers of tall columnar cells containing subnuclear or supranuclear vacuoles resembling secretory endometrium
- Intestinal type areas with glandular structures lined by mucinous columnar or low columnar glands, ranging from primitive cribriform structures to well differentiated glands with goblet cells and rarely Paneth cells
- Both types may occur in pure form and may contain tumor giant cells (mono or multinucleated)
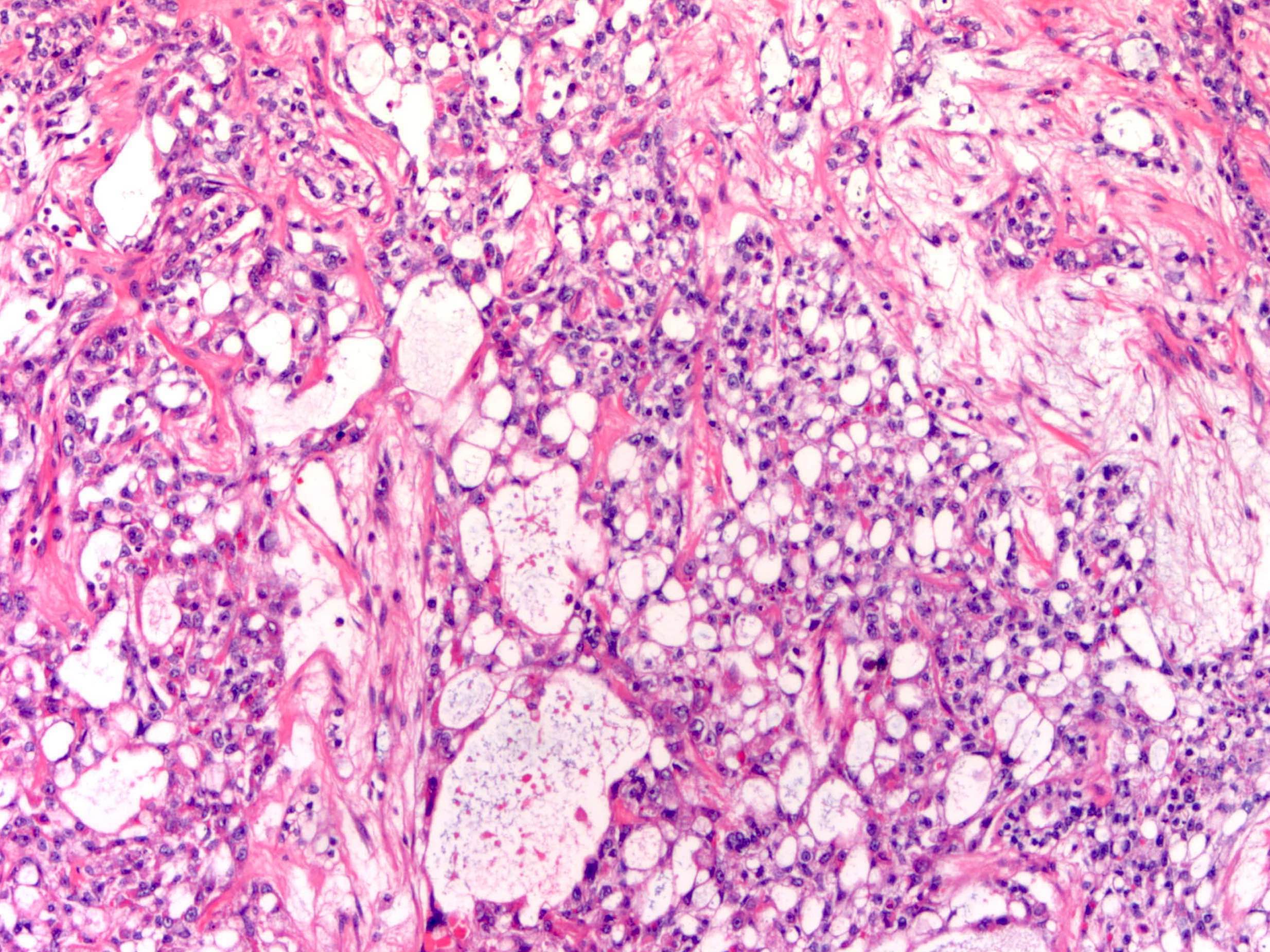
- Polyvesicular vitelline pattern (Am J Surg Pathol 2013;37:393):
- May occur in pure form
- Variably sized cysts or vesicles lined by flat to cuboidal to columnar cells, sometimes with basal or paraluminal vacuolation
- Variably cellular stroma, occasionally with eccentric constriction (resembling subdivision of primary yolk sac vesicle)
- Parietal pattern:
- Tumor cells embedded in extracellular linear bands of PAS positive basement membrane-like material
- Hepatoid pattern:
- Tends to occur in pure form
- Aggregates, clusters or cords of large polygonal cells with abundant uniform or granular eosinophilic cytoplasm, round nuclei and prominent nucleoli, separated by thin fibrous bands (Cancer 1982;50:2355)
- Mesenchyme-like pattern:
- Cords, tubules and gland-like structures of tumor cells scattered in edematous to myxoid stroma
- May be markedly myxoid (magma reticulare)
- General features:
- Variable cytologic atypia and mitotic activity
- Pale eosinophilic to clear cytoplasm
- Prominent nucleoli
- Intracellular hyaline globules
- Tumor cells lining cystic structures can be deceptively bland
- Rarely stromal luteinization
- May show areas of extramedullary hematopoiesis
- May be admixed with other malignant germ cell tumor, usually with dysgerminoma or gonadoblastoma in patients with gonadal dysgenesis
- May be associated with synchronous or metachronous ipsilateral or contralateral mature cystic teratoma
Microscopic (histologic) images
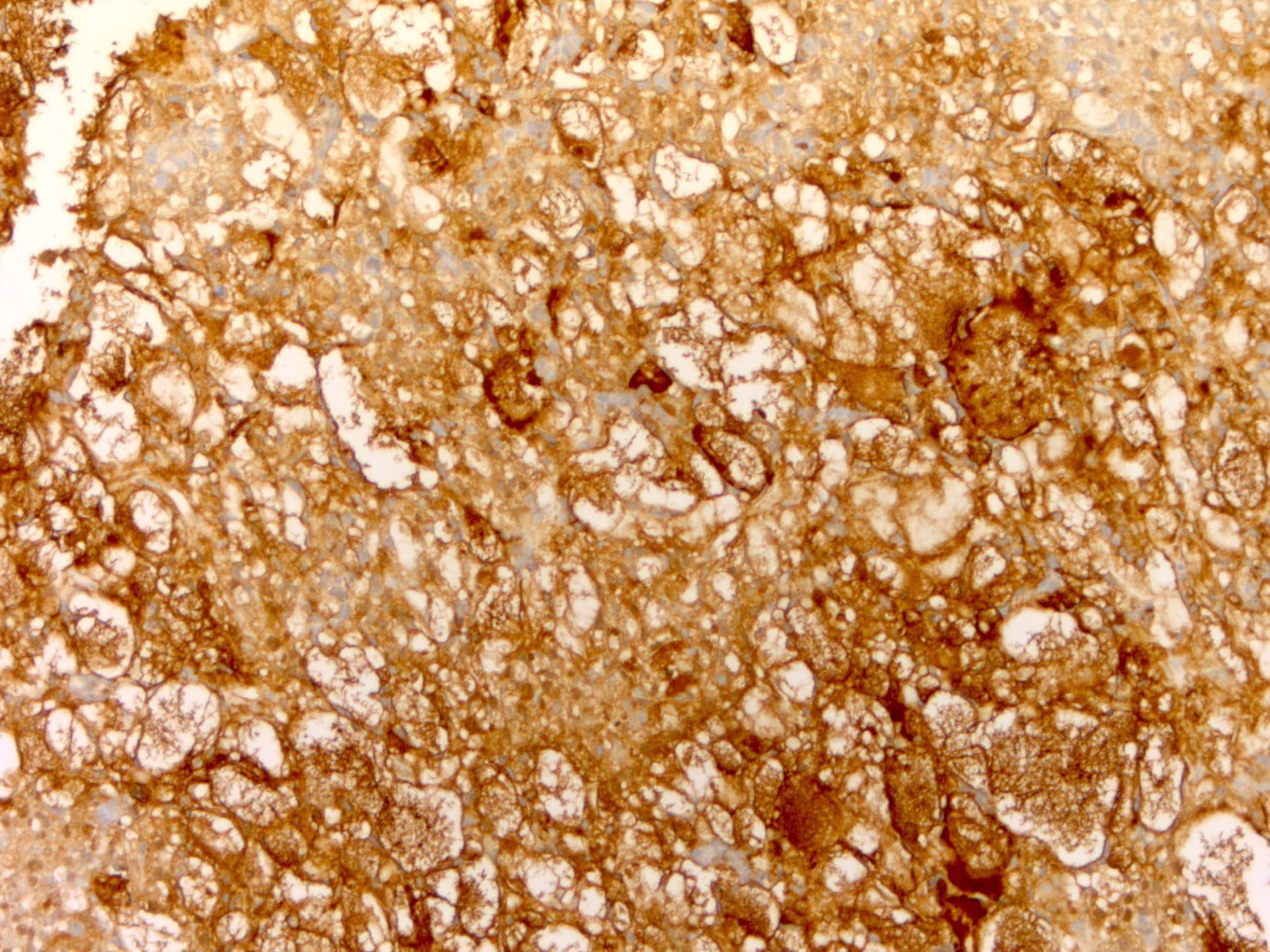
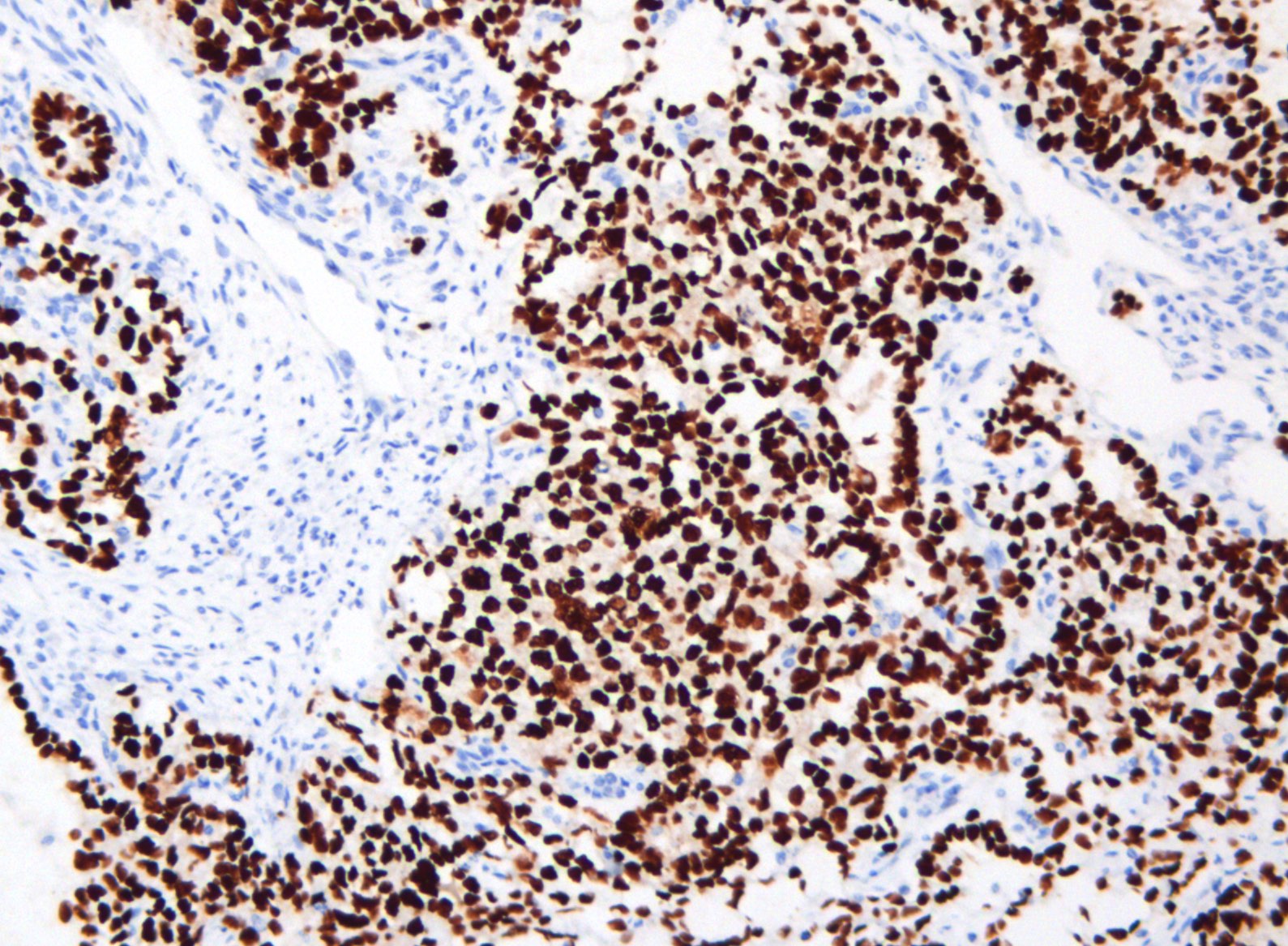
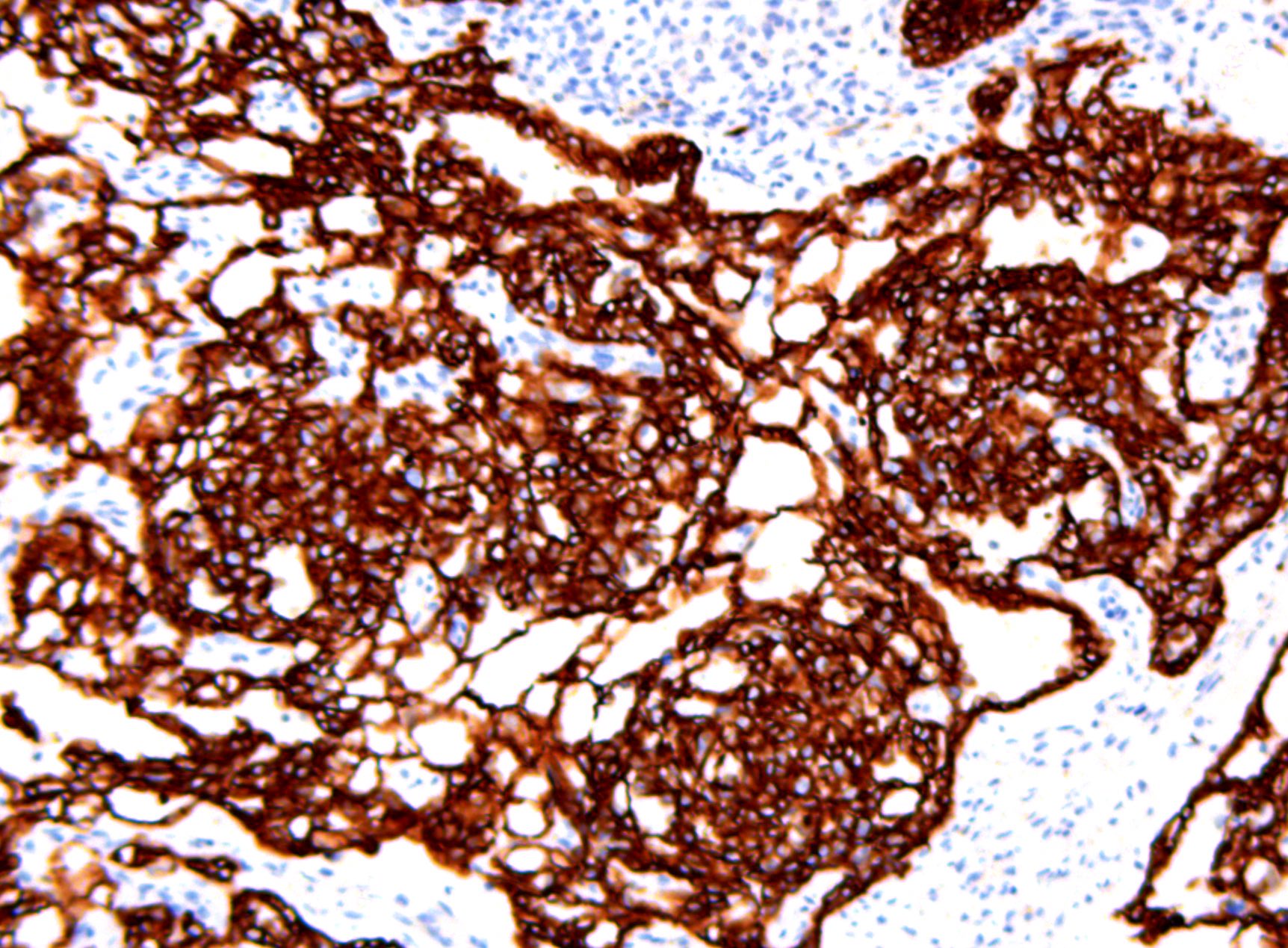
Contributed by Gulisa Turashvili, M.D., Ph.D., Sharon Song, M.D. and AFIP images
Positive stains
- SALL4: marker of primitive germ cell differentiation (Arch Pathol Lab Med 2014;138:351, Am J Surg Pathol 2009;33:894)
- AFP: highly specific but 60% sensitive, often patchy / focal and weak (Histopathology 2013;62:71)
- Glypican 3: less specific but stronger expression (Am J Surg Pathol 2008;32:600)
- PLAP
- HNF1β
- Pancytokeratin
- GATA3: positive in reticular / microcystic, papillary and polyvesicular vitelline patterns but not in the glandular pattern (Histopathology 2016;68:613)
- HepPar1: positive in glandular and hepatoid patterns
- CEA, albumin: positive in hepatoid pattern (Int J Gynecol Pathol 2014;33:365)
- TTF1: positive in foregut / respiratory pattern (Histopathology 2014;65:51)
- CDX2: positive in glandular intestinal type pattern
- Villin: positive in reticular / microcystic and glandular intestinal type patterns
Negative stains
Electron microscopy description
- Glandular intestinal type yolk sac tumor shows large nuclei with prominent nucleolonema, numerous intracytoplasmic ribosomes, rough endoplasmic reticulum, mitochondria and dense amorphous intracellular material (Pathol Res Pract 1987;182:609)
Molecular / cytogenetics description
- Usually isochromosome 12p (Mod Pathol 2006;19:766)
Sample pathology report
- Right fallopian tube and ovary, salpingo-oophorectomy:
- Ovary: yolk sac tumor (see synoptic report)
- Fallopian tube: benign
Differential diagnosis
- Clear cell carcinoma:
- Typical architectural patterns (tubulocystic, papillary, solid) with or without hobnail cells
- Lack of microcysts and Schiller-Duval bodies
- Discordance between mitotic activity and cytologic atypia
- Stromal hyalinization
- Background adenofibroma or endometriosis
- Positive for napsin A, HNF1β, PAX8, CK7, EMA
- Negative for SALL4 and AFP
- Glypican 3 is not helpful in this differential diagnosis
- Endometrioid carcinoma:
- Usually older patients
- Typical cytology (columnar cells with moderately atypical pseudostratified nuclei)
- Lack of histologic patterns of yolk sac tumor, Schiller-Duval bodies and primitive appearing nuclei (Int J Surg Pathol 2014;22:677)
- Squamous differentiation
- May be associated with endometriosis
- Positive for PAX8, ER, PR, CK7, EMA
- Negative for SALL4 and AFP
- Glypican 3 is not helpful in this differential diagnosis
- Dysgerminoma:
- Monomorphic architecture composed of cells with ample pale cytoplasm and large round nuclei
- Lack of histologic patterns of yolk sac tumor, Schiller-Duval bodies and hyaline bodies
- Associated with lymphocytic and granulomatous reactions
- Positive for OCT 3/4 and D2-40
- Negative for AFP and glypican 3
- Embryonal carcinoma:
- Very rare in pure form in the ovary
- Lack of histologic patterns of yolk sac tumor and Schiller-Duval bodies
- Aggregated of primitive cells with more marked nuclear atypia and more granular cytoplasm
- Positive for OCT 3/4, CD30 and SOX2
- Negative for AFP and glypican 3
- Sertoli-Leydig cell tumor:
- Androgenic manifestations
- Morphologic patterns of Sertoli cell tumor or Leydig cells
- Positive for inhibin, calretinin, FOXL2 and SF1
- Negative for SALL4, AFP and glypican 3
- Juvenile granulosa cell tumor:
- Solid or follicular growth composed of polygonal cells with eosinophilic to clear cytoplasm and hyperchromatic nuclei without grooves
- Lack of histologic patterns of yolk sac tumor and Schiller-Duval bodies
- Positive for inhibin, calretinin, FOXL2 and SF1
- Negative for SALL4, AFP and glypican 3
- Metastatic hepatocellular carcinoma:
- Immature teratoma:
- Admixture of endodermal, mesodermal and ectodermal elements
- Somatic yolk sac tumor:
- Yolk sac tumor associated with a somatic epithelial neoplasm, usually high grade (Histopathology 2016;69:739)
- Thought to be due to transdifferentiation of high grade carcinoma to yolk sac tumor, rather than a true mixed or collision tumor (i.e. somatic rather than germ cell origin) (Histopathology 2016;69:739, Int J Gynecol Pathol 2011;30:442)
- Typically displays a reticular pattern (Histopathology 2017;71:562)
- Occurs in postmenopausal women and exhibits poor prognosis (Int J Gynecol Pathol 2011;30:442)
Additional references
Practice question #1
Practice answer #1
Practice question #2
Which of the following is true about yolk sac tumors?
- Call-Exner bodies
- Expression of SALL4, AFP and glypican 3 by immunohistochemistry
- Homer Wright rosettes
- Low serum AFP levels
- Most common in postmenopausal women
Practice answer #2
B. Expression of SALL4, AFP and glypican 3 by immunohistochemistry
Comment Here
Reference: Yolk sac tumor
Comment Here
Reference: Yolk sac tumor