Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Turashvili G. Fibroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorfibroma.html. Accessed April 26th, 2024.
Definition / general
- Benign stromal tumor composed of fibroblastic cells within a variably collagenous stroma
Essential features
- Benign stromal tumor composed of spindled, ovoid to round cells within a variably collagenous stroma
- Variants include fibroma with minor sex cord elements, cellular fibroma and mitotically active cellular fibroma
- Important differential diagnoses for cellular fibroma include diffuse adult type granulosa cell tumor and fibrosarcoma
- Gorlin syndrome should be suspected in young patients with bilateral ovarian fibroma
- Long term follow up is recommended for cellular fibromas associated with rupture and adhesions due to increased risk of recurrence
ICD coding
Epidemiology
- Most common ovarian stromal tumor
- ~4% of all ovarian tumors (Cancer 1981;47:2663)
- Cellular fibromas represent ~10% of all ovarian fibromas
- Mean age 48 years, uncommon before 30
- Occurs in ~25% of patients with nevoid basal cell carcinoma syndrome (Gorlin syndrome) (J Med Genet 1993;30:460)
- Autosomal dominant disease due to mutations of the human homologue of the Drosophila gene PTCH (patched)
Sites
- Ovary
Pathophysiology
- Neoplastic transformation of ovarian stromal cells due to hereditary or sporadic genetic abnormalities (see Molecular / cytogenetics description)
Clinical features
- Most commonly symptoms related to an ovarian mass, such as abdominal pain or distension and increased urinary frequency or may be incidental
- Can be associated with ovarian torsion (BMC Surg 2014;14:38)
- Rarely hormonal manifestations
- Ascites in large (> 10 cm) tumors in 10% of cases (Am J Obstet Gynecol 1970;107:538)
- Syndromic ovarian fibromas:
- Often diagnosed before the age of 30 years, including children
- Usually bilateral (75%), calcified and nodular, often overlapping medially (leading to misdiagnosis as calcified uterine leiomyoma) (Genet Med 2004;6:530)
- May be renin secreting, leading to gestational hypertension (Br J Obstet Gynaecol 1994;101:1015)
- May recur (Hum Reprod 2001;16:1261, Obstet Gynecol 1983;61:95S)
- Meigs syndrome occurs in ~1% of cases (Am J Obstet Gynecol 1937;33:249, Eur J Obstet Gynecol Reprod Biol 2000;92:199)
- Characterized by the triad of benign adnexal mass, ascites and pleural effusion
- Due to seepage of fluid from ovary into peritoneal cavity and then into 1 or both pleural cavities either via lymphatics or through a communication between abdominal and pleural cavity (lumbocostal triangle)
Diagnosis
- Histologic examination for definitive diagnosis
- Tentative diagnosis can be made grossly and at frozen section evaluation (Semin Diagn Pathol 2002;19:237)
Laboratory
- Can lead to nonspecific increase in serum CA125 (Gynecol Oncol 1995;59:405)
Radiology description
- Ultrasonography:
- Usually solid, homogeneous and hypoechoic mass with posterior acoustic shadowing, similar to a pedunculated subserosal uterine leiomyoma (AJR Am J Roentgenol 1985;144:1239)
- Heterogeneous echogenicity in tumors with necrosis, hemorrhage or cystic degeneration
- Computed tomography:
- Slightly hypoattenuating solid mass with poor, very slow contrast enhancement (Radiographics 2002;22:1305)
- Rarely calcifications
- Magnetic resonance imaging (MRI):
- T1: homogeneous low signal intensity
- T2:
- Well circumscribed mass with low signal intensity (J Magn Reson Imaging 1997;7:465)
- Hyperintense areas due to edema or cystic degeneration
- Characteristic feature is a band of T2 hypointensity separating the tumor from the uterus on all imaging planes
- Gadolinium: heterogeneous enhancement
- May mimic malignancy (Radiographics 2002;22:1305)
Radiology images
Prognostic factors
- Excellent in most cases
- Ovarian surface involvement and extraovarian adhesions occur in 6% of cellular fibromas and 10% of mitotically active cellular fibromas (Am J Surg Pathol 2006;30:929)
- Extraovarian spread at surgery in 11% of cellular fibromas and 13% of mitotically active cellular fibromas (Am J Surg Pathol 2006;30:929)
- Cellular fibromas may recur, often after a long interval, warranting long term follow up (Cancer 1981;47:2663)
Case reports
- 15 year old girl with bilateral ovarian fibroma associated with Gorlin syndrome (J Pediatr Adolesc Gynecol 2011;24:e5)
- 19 year old woman with large ovarian fibroma presenting with spontaneous abdominal bleeding (Case Rep Obstet Gynecol 2019;2019:9834915)
- 34 year old woman with mitotically active cellular fibroma that recurred 16 years later (Int J Gynecol Pathol 2020 [Epub ahead of print])
- 40 year old woman with bilateral ovarian fibroma presenting as Meigs syndrome (J Obstet Gynaecol 2013;33:636)
- 66 year old woman with extraovarian fibroma with minor sex cord elements (Int J Surg Pathol 2017;25:472)
Treatment
- Surgical excision (salpingo-oophorectomy, oophorectomy or ovarian sparing procedure with or without hysterectomy depending on patient’s age)
- Cellular fibromas require long term follow up, particularly in the setting of ovarian surface involvement, intraoperative rupture or extraovarian spread (Cancer 1981;47:2663)
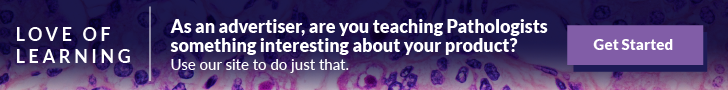
Gross description
- Well circumscribed mass with smooth, lobulated surface
- Firm, chalky, solid, white to yellow-white to tan-yellow cut surface that may be whorled
- Frequent edema resulting in softer consistency
- Mean size 6 cm (range 1 - 21.5)
- Usually unilateral (< 10% bilateral)
- Cystic degeneration in ~25% of cases
- Calcifications in ~10% of cases
- ~20% present as pedunculated or polypoid growths on ovarian surface
- With or without hemorrhage or necrosis
- Cellular fibroma:
- Mean size 8 - 9 cm (range 1 - 19)
- Tan-yellow, soft and fleshy cut surface (Cancer 1981;47:2663)
- With or without surface adhesions
- Fibroma associated with Gorlin syndrome:
- Bilateral, multinodular and calcified (J Pediatr Adolesc Gynecol 2011;24:e5)
Gross images
Frozen section description
- Variably cellular spindle cell neoplasm with fascicular or storiform growth with or without hyaline plaques or calcifications
Frozen section images
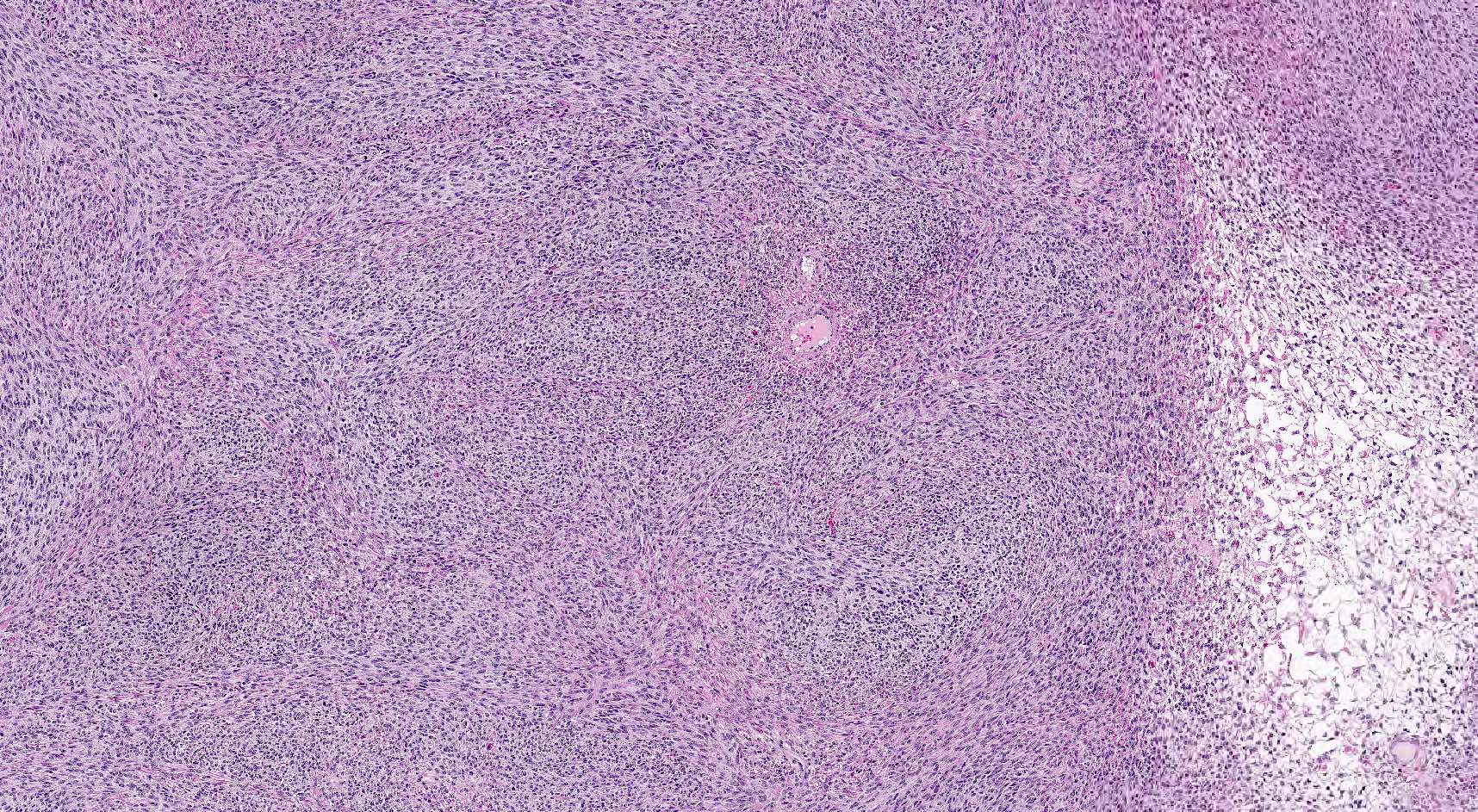
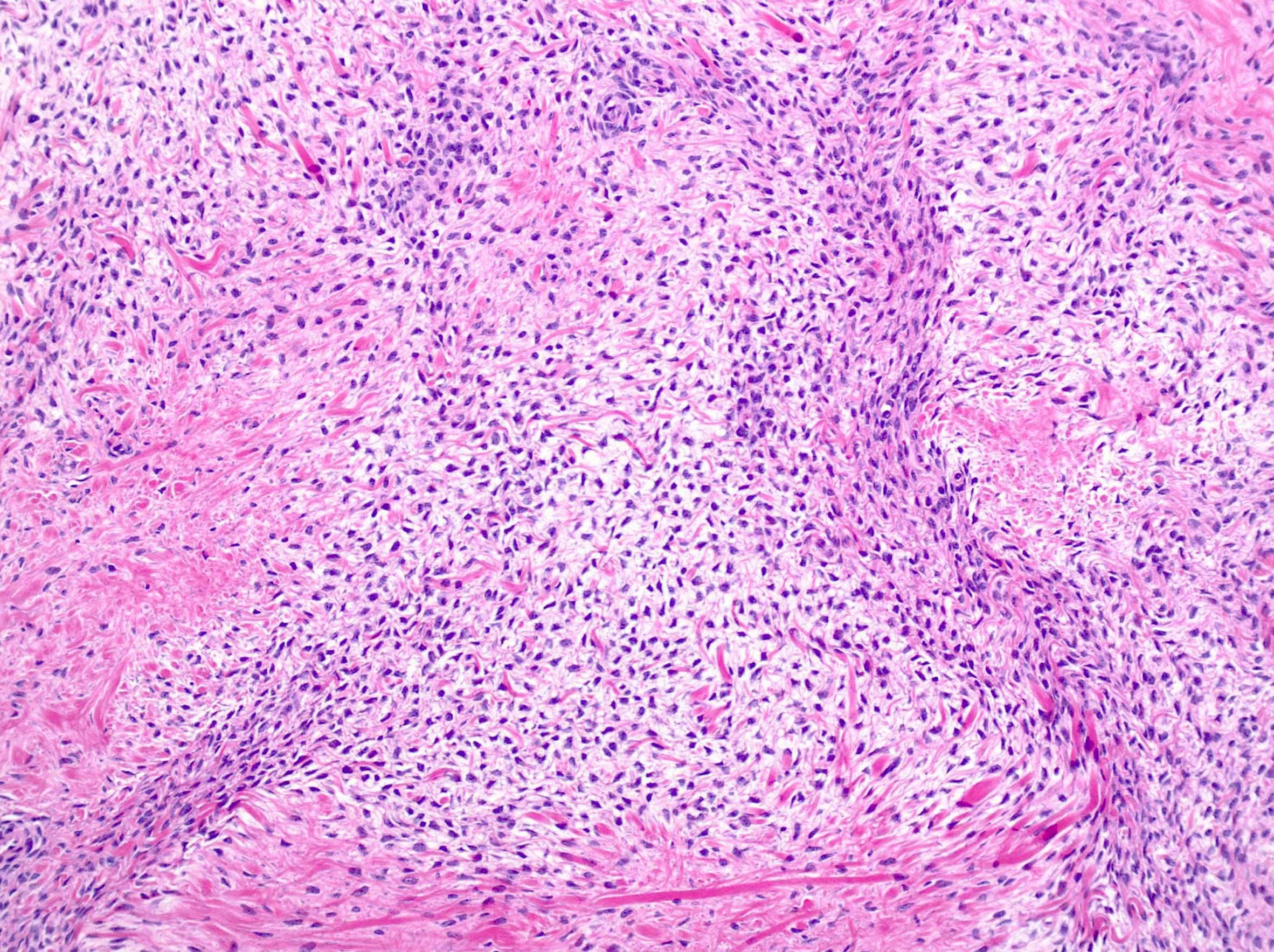
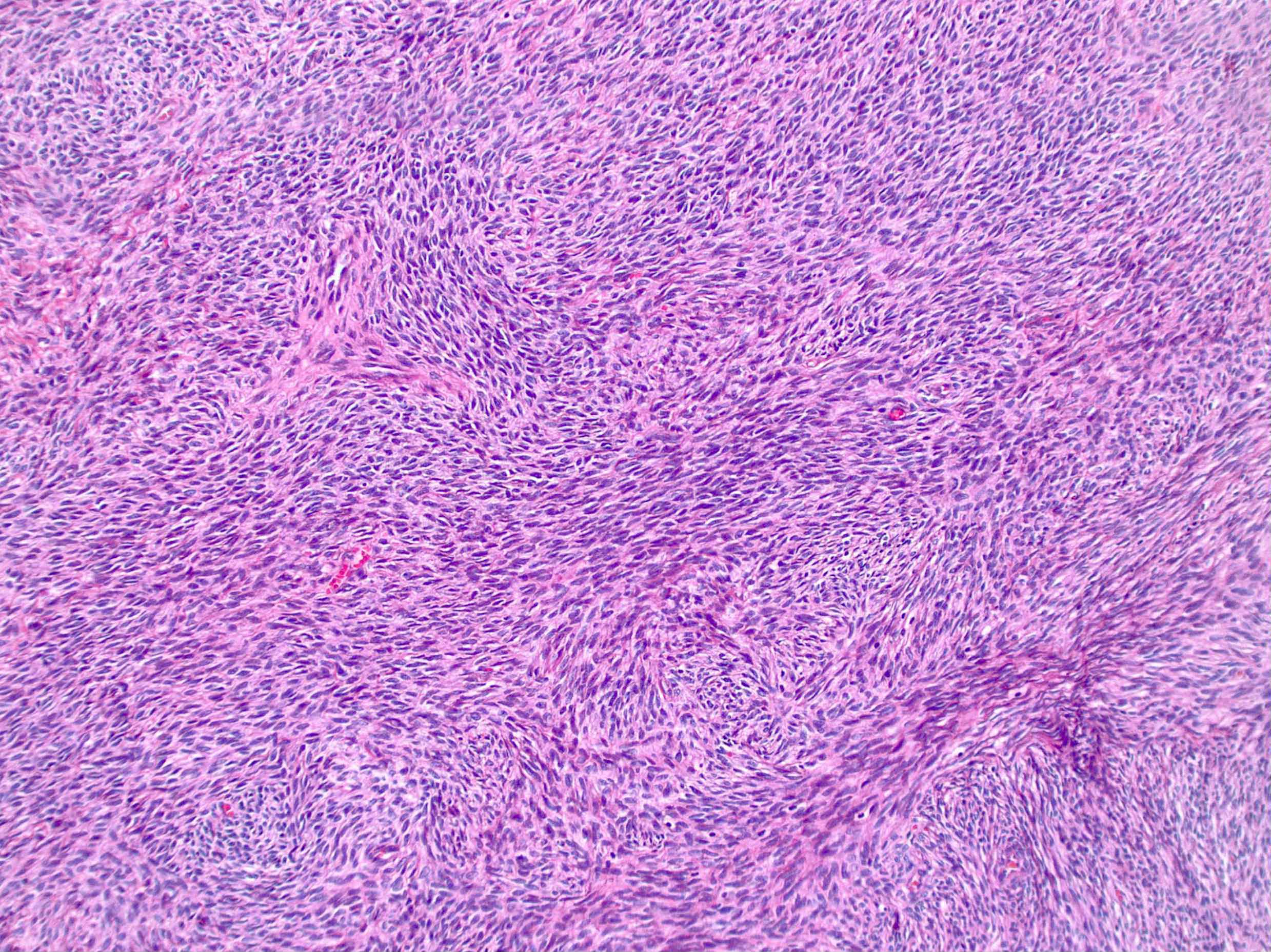
Microscopic (histologic) description
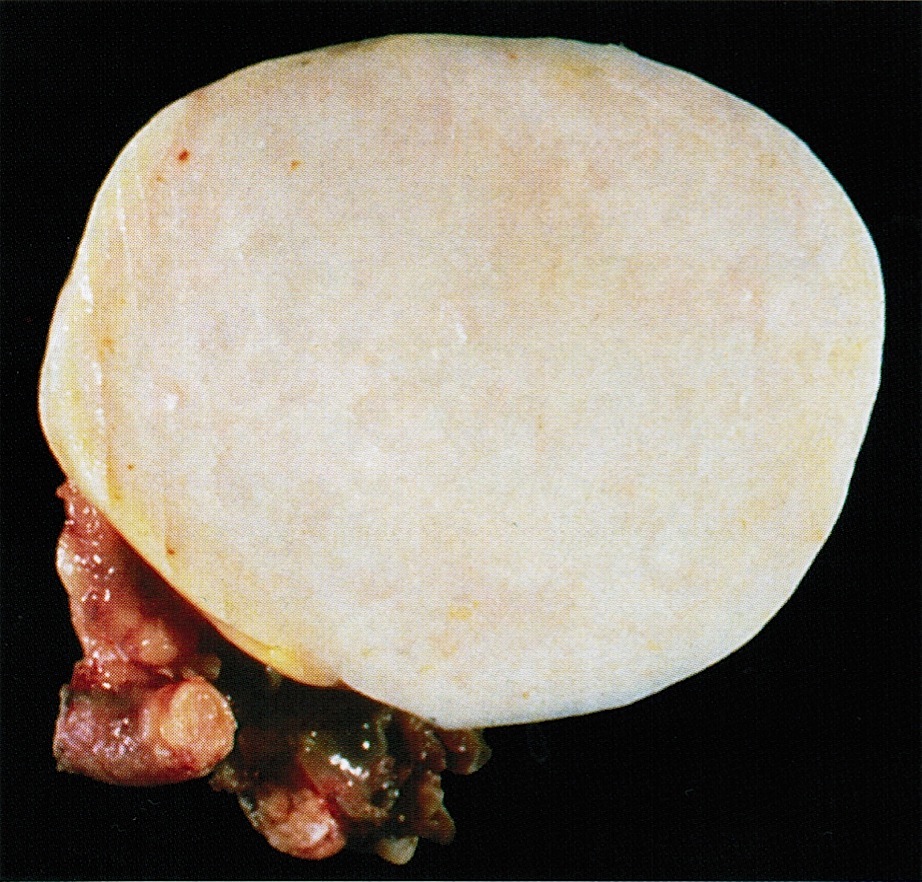
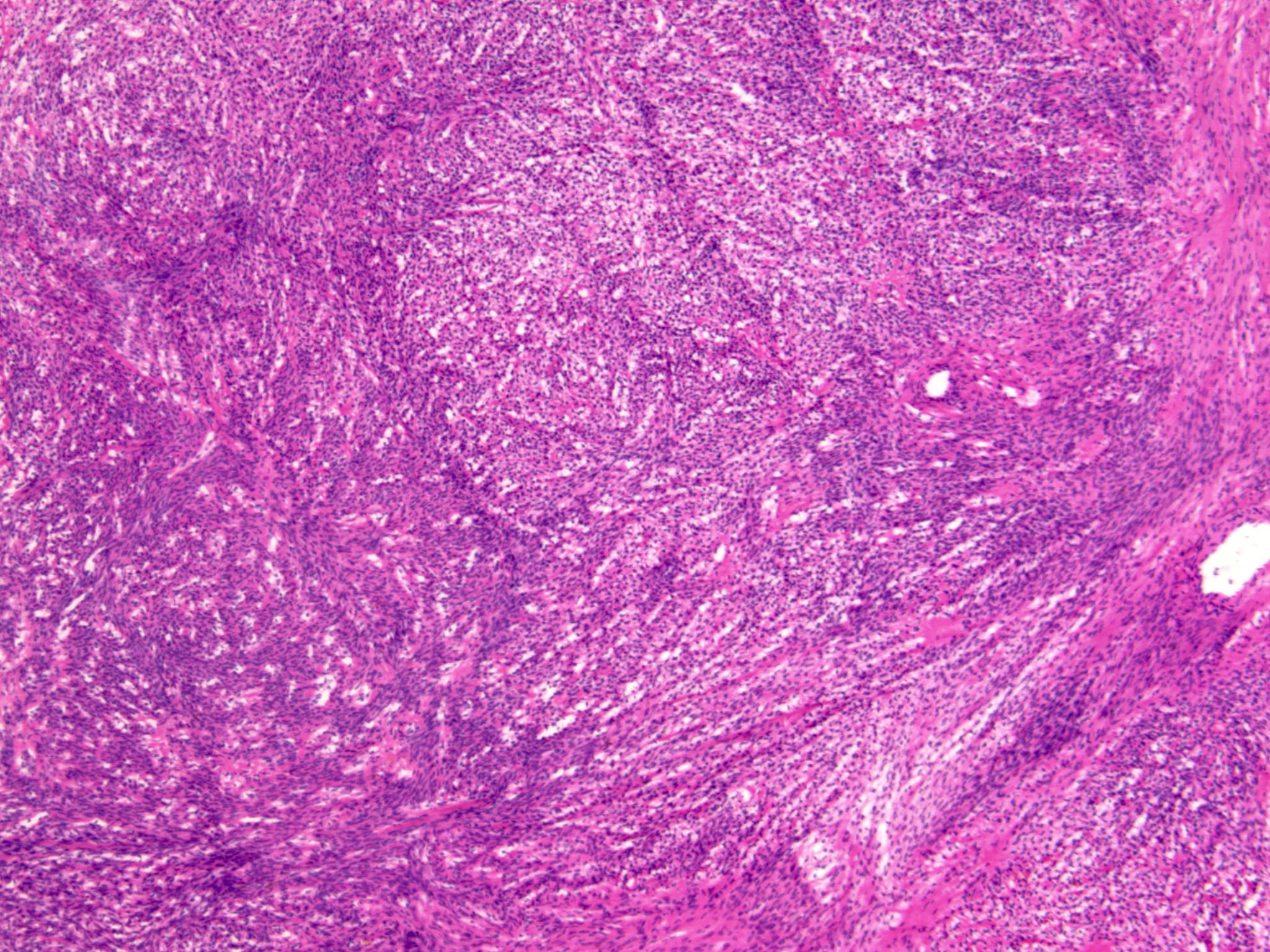
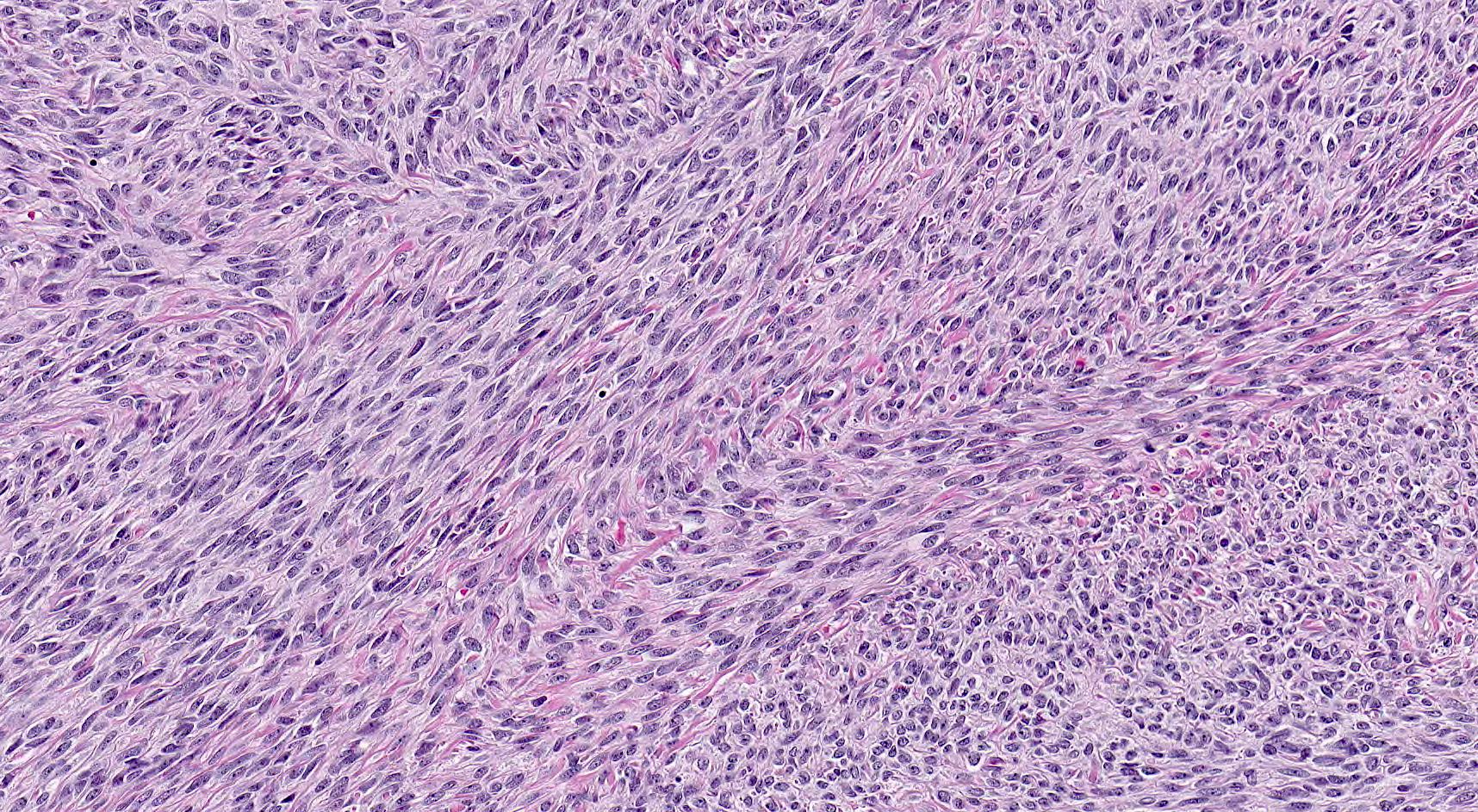
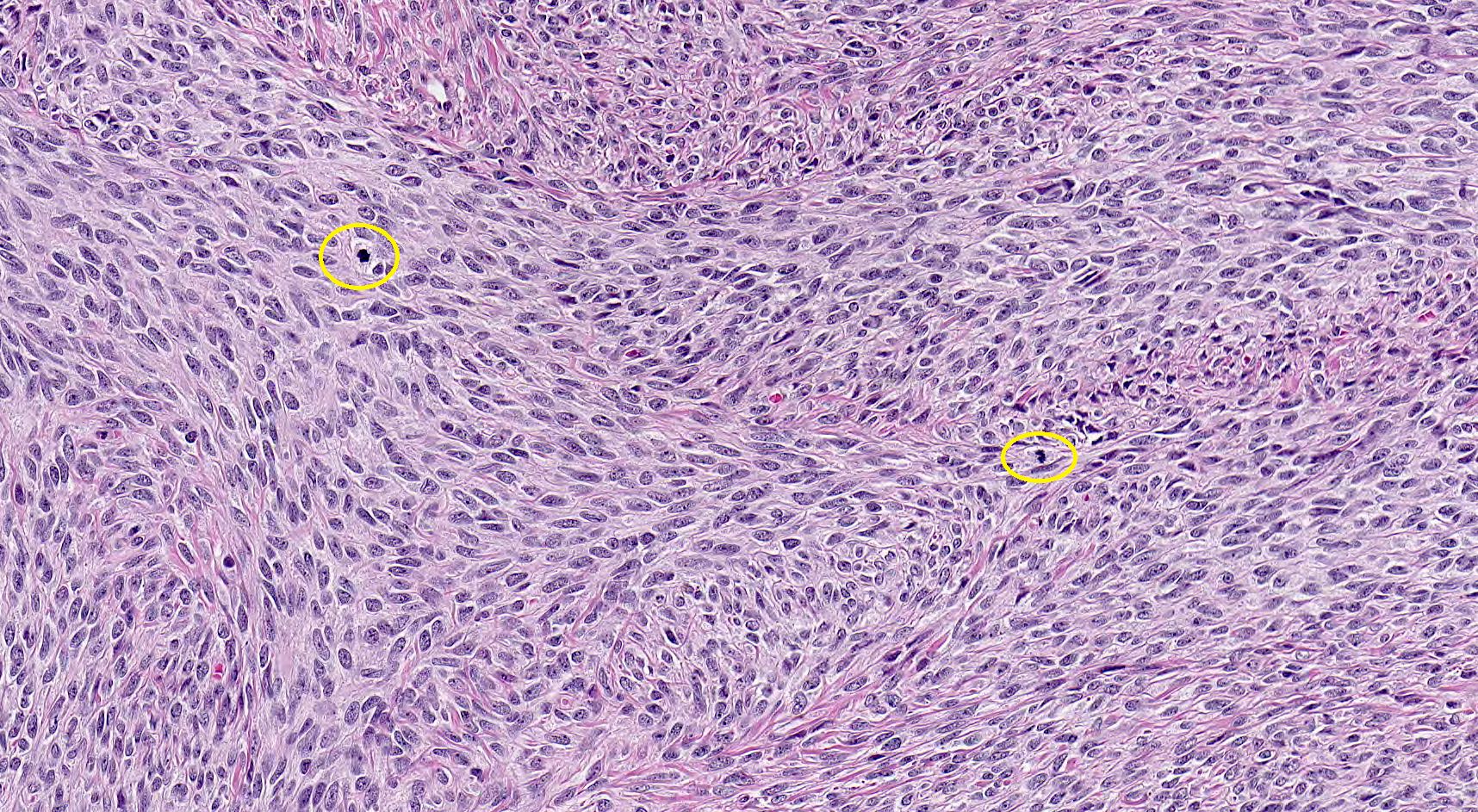
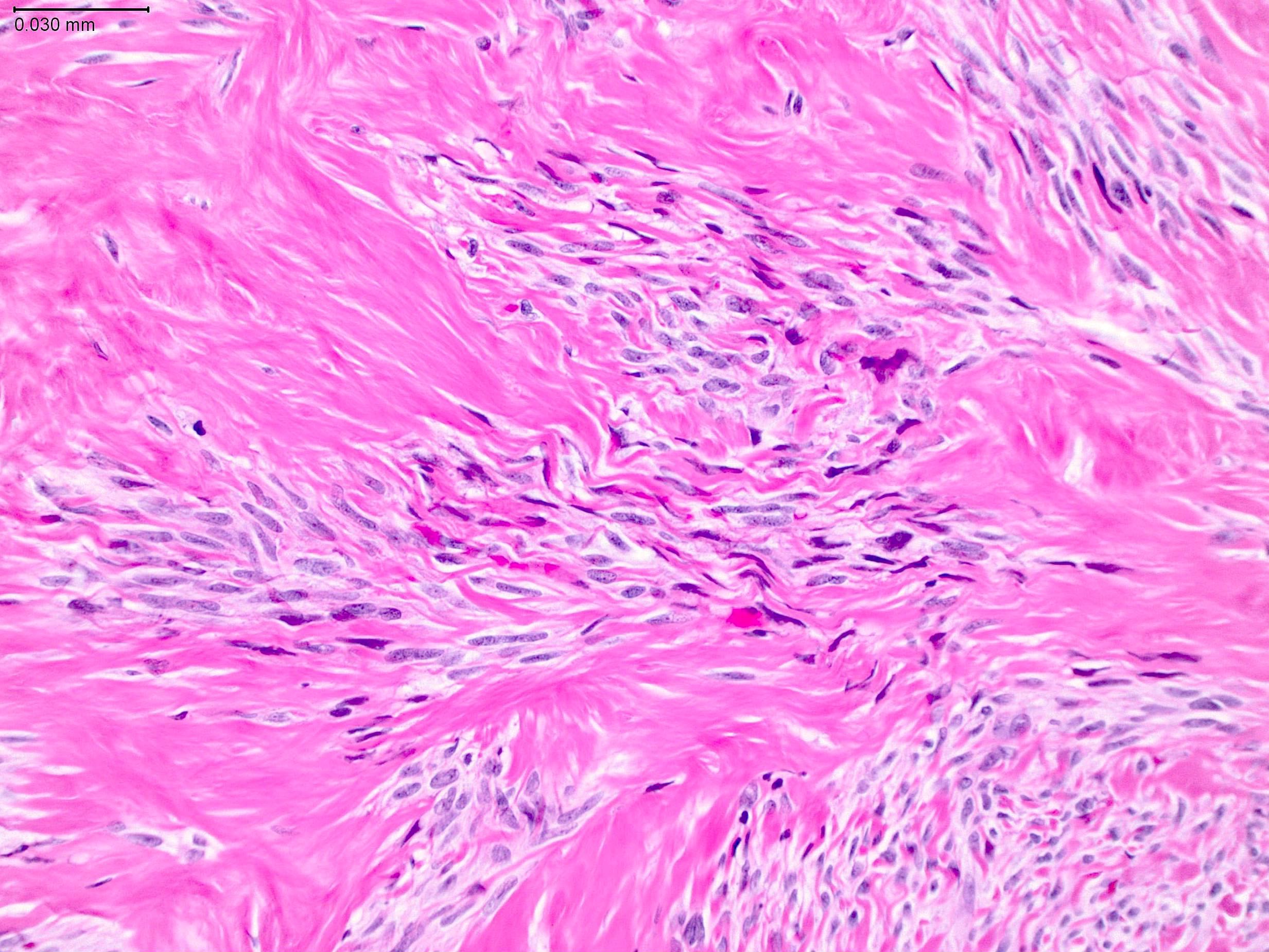
- Conventional fibroma:
- Recapitulates ovarian cortex
- Usually well circumscribed but nonencapsulated
- Variably cellular fascicular or less frequently, storiform growth of tumor cells within a variably collagenous stroma, sometimes with hyaline plaques (Cancer 1981;47:2663)
- Bland spindled to ovoid nuclei with pointy ends and scant eosinophilic cytoplasm blending with surrounding stroma
- Occasional mitoses (usually up to 3 mitoses per 10 high power fields)
- With or without Verocay-like areas (slightly wavy, parallel arrays of spindled nuclei), calcification, edema, hemorrhage, infarct type necrosis, rare groups of luteinized cells
- Rarely intracytoplasmic lipid (may be diagnosed as thecoma), eosinophilic hyaline globules, melanin pigment or bizarre nuclei (Int J Gynecol Pathol 2009;28:356, Int J Gynecol Pathol 2019;38:92, Int J Surg Pathol 2020 [Epub ahead of print])
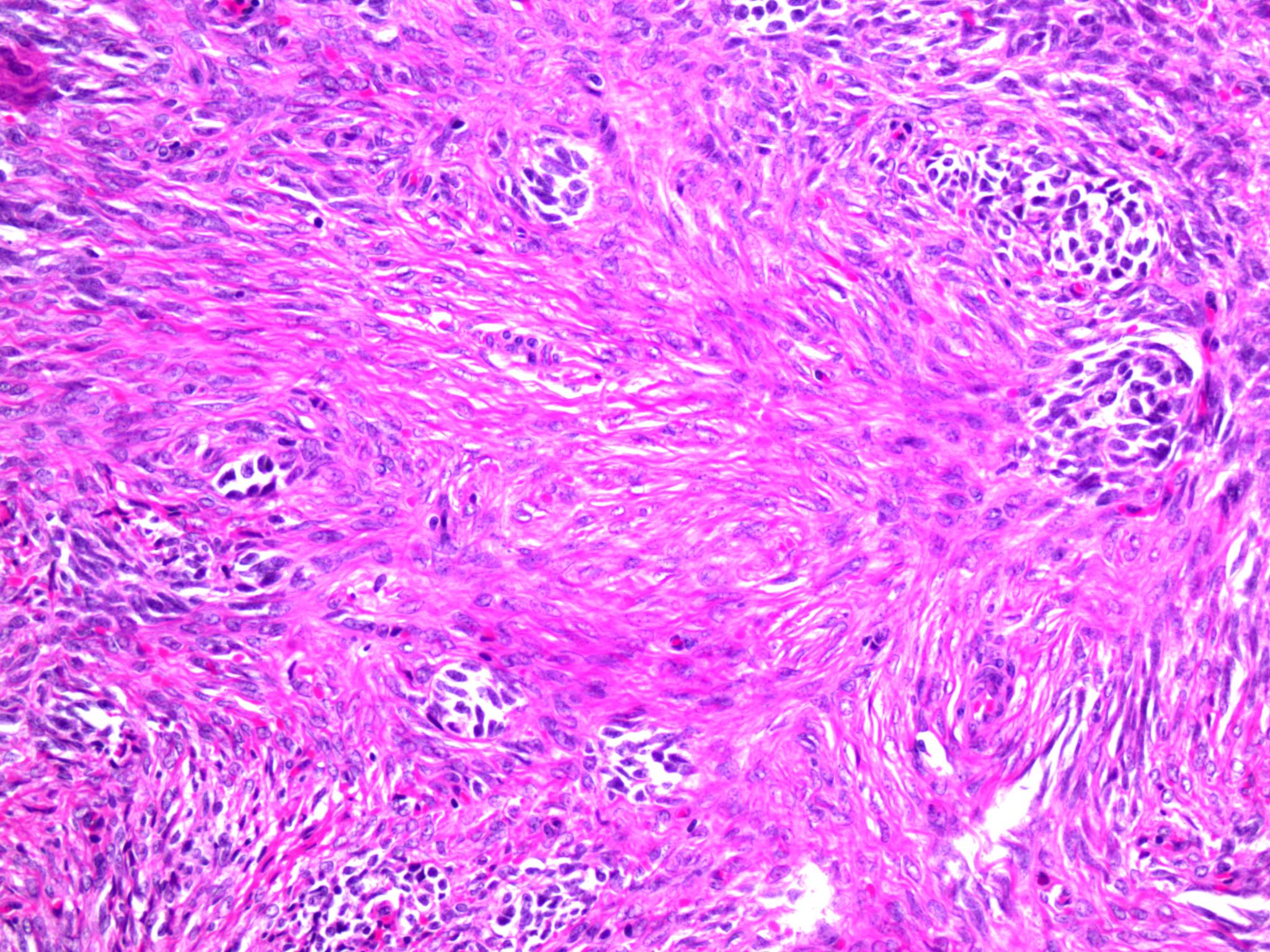
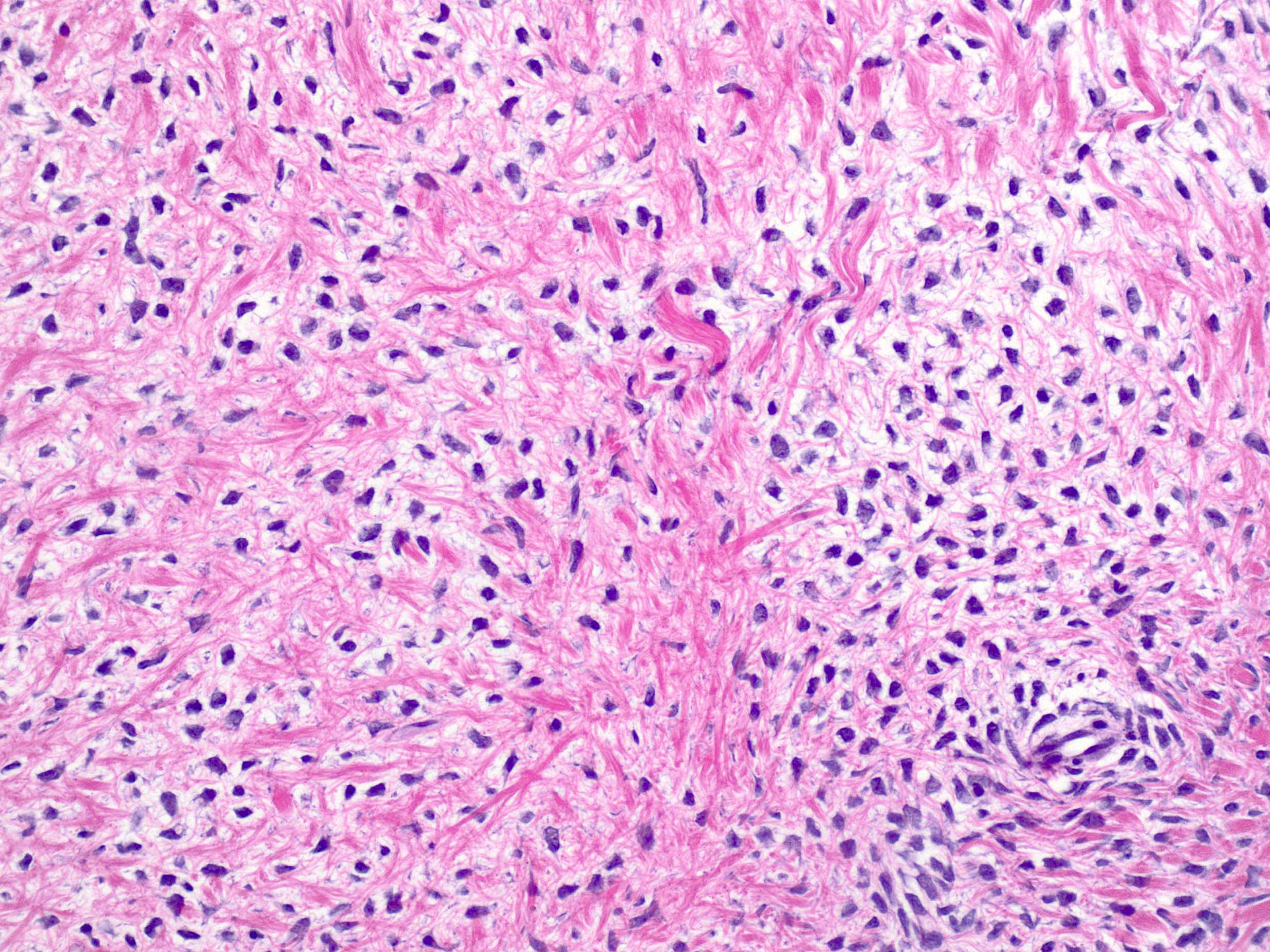
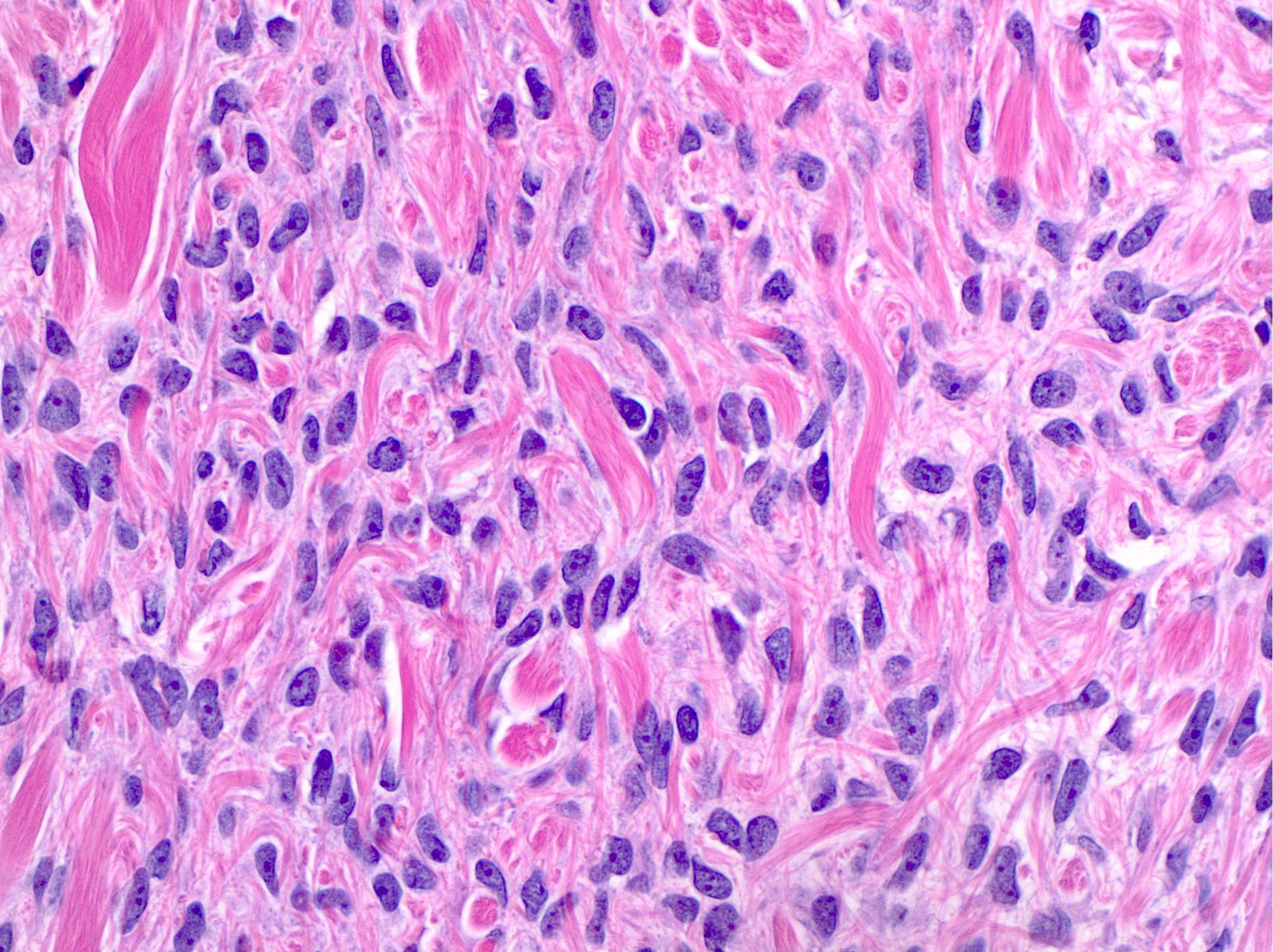
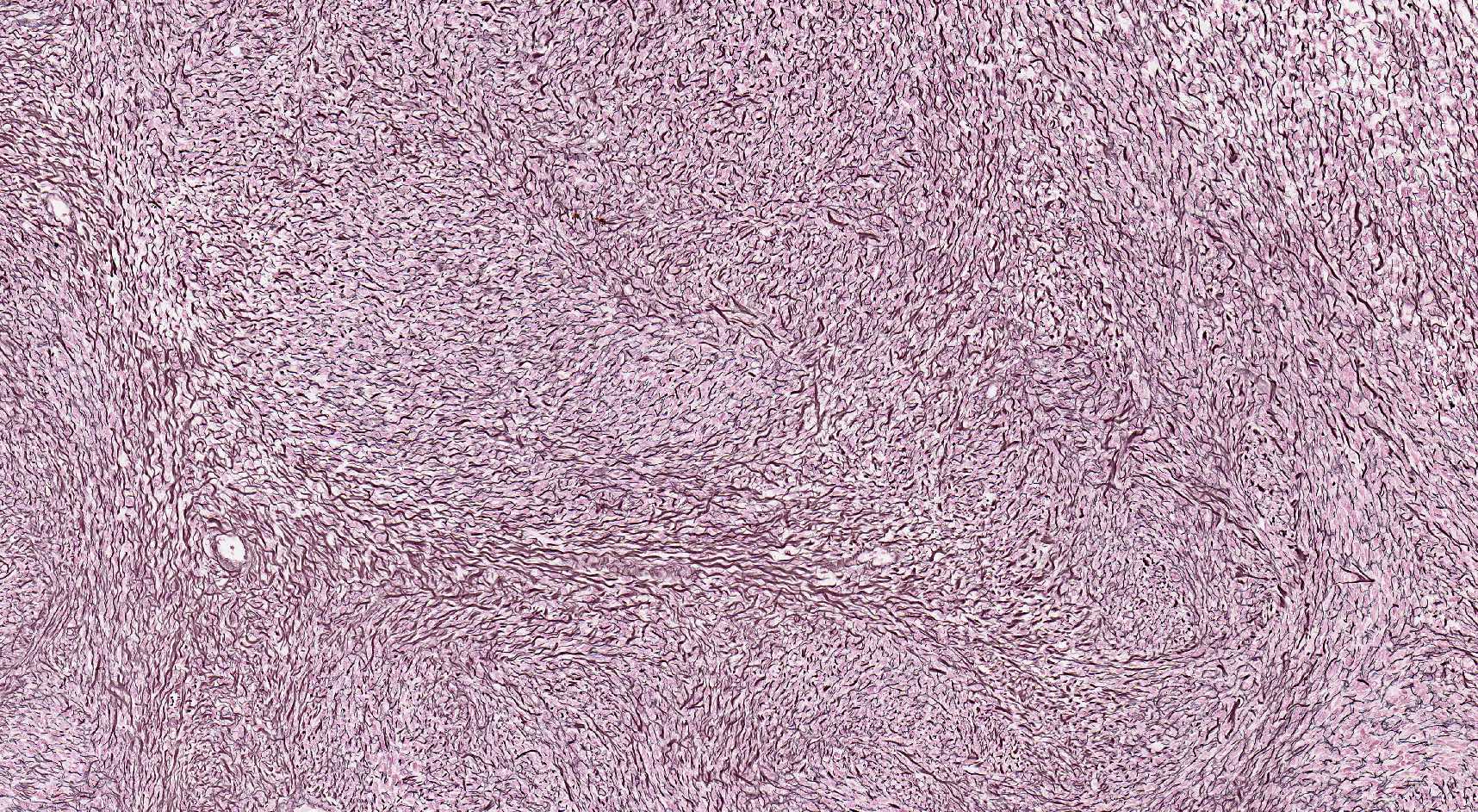
- Cellular fibroma (10% of cases):
- Resembles diffuse type of adult granulosa cell tumor
- Densely cellular with little intercellular collagen
- Bland spindled nuclei with up to 3 mitoses per 10 high power fields (Cancer 1981;47:2663)
- "Mitotically active cellular fibroma" has been proposed for cellular fibromas with ≥ 4 mitoses per 10 high power fields (Am J Surg Pathol 2006;30:929)
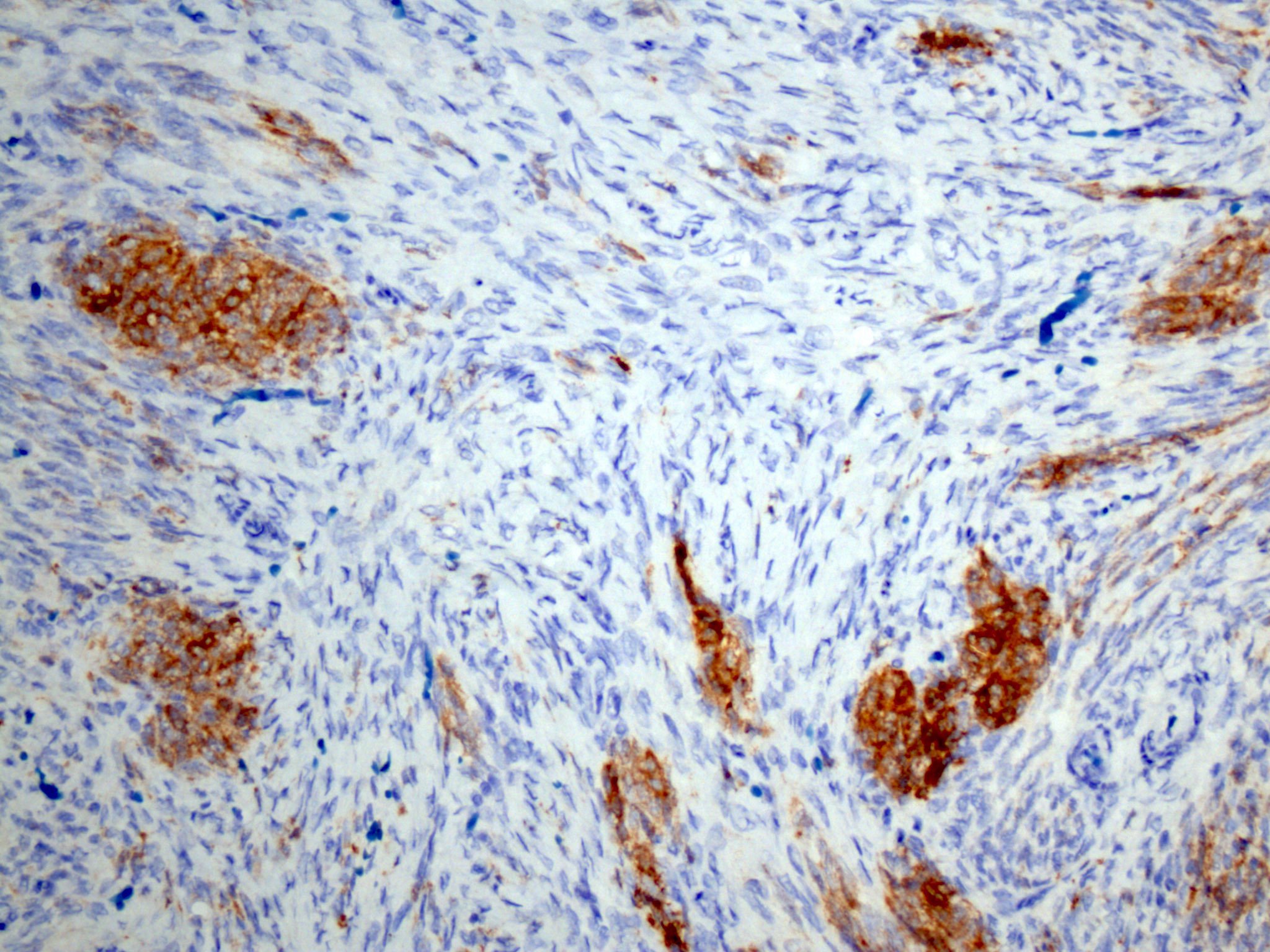
- Fibroma with minor sex cord elements:
- Sex cord component accounting for < 10% of overall tumor volume
- No prognostic significance
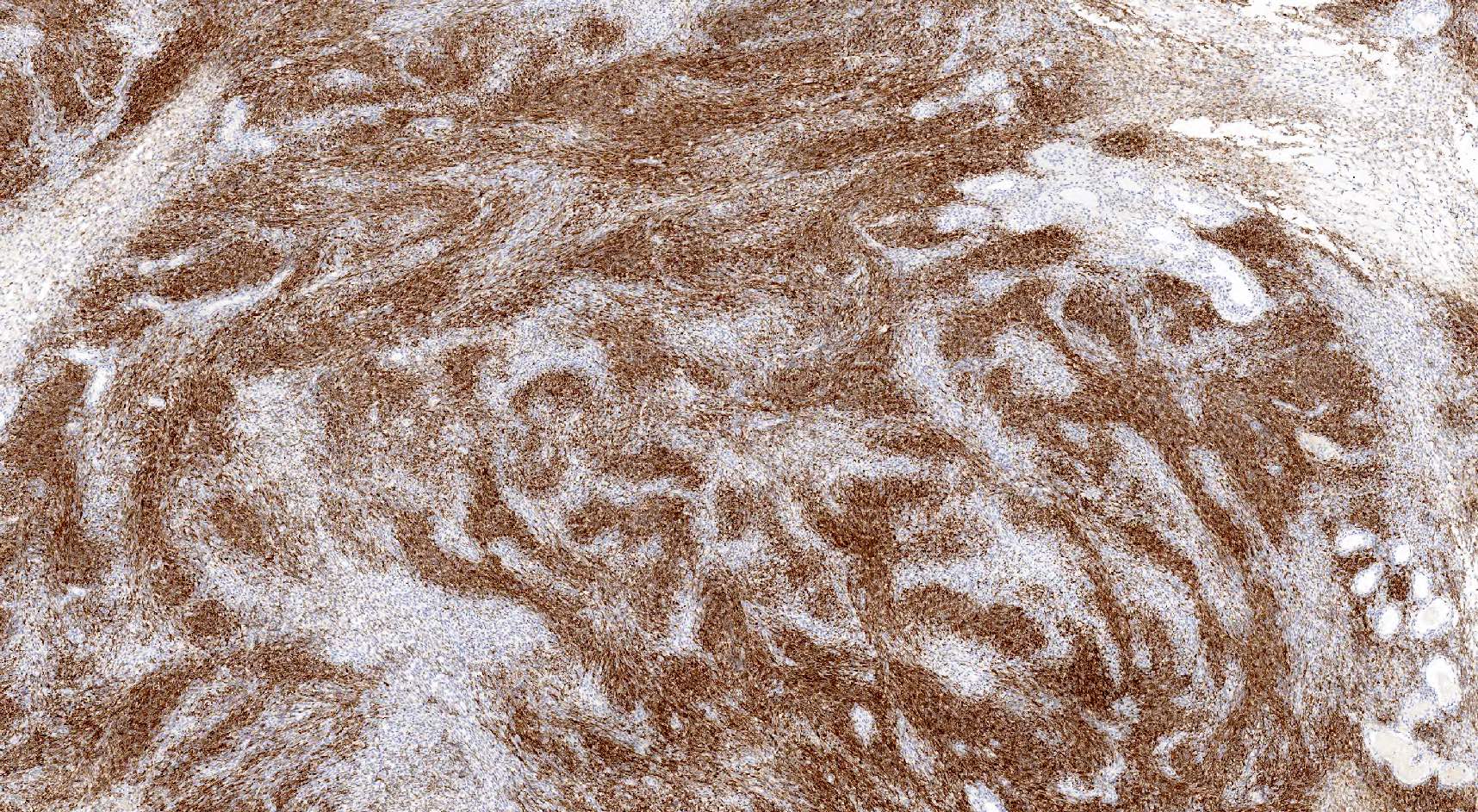
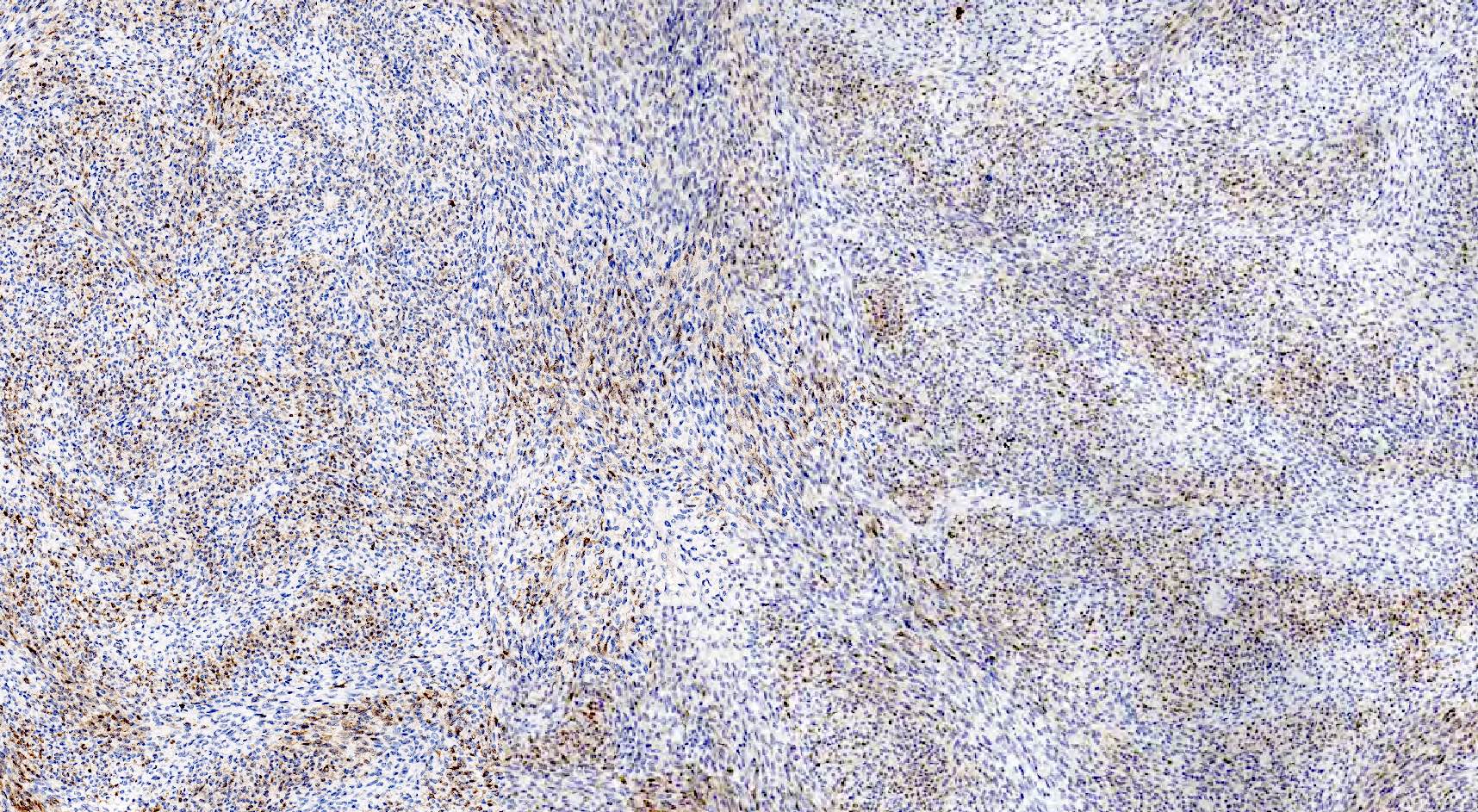
Microscopic (histologic) images
Contributed by Gulisa Turashvili, M.D., Ph.D., Kyle C. Strickland, M.D., Ph.D. and Rex Bentley, M.D.
Virtual slides
Positive stains
- WT1 (Am J Surg Pathol 2008;32:884)
- SF1 (Am J Surg Pathol 2009;33:354)
- FOXL2 (Am J Surg Pathol 2011;35:484)
- Inhibin: 50% of cases, often focal or weak (Mod Pathol 1998;11:656, Mod Pathol 2003;16:584)
- Vimentin (J Pathol 1987;152:253)
- CD56 (Am J Surg Pathol 2008;32:884)
- ER beta
- PR
- SMA (Am J Surg Pathol 2008;32:884)
- Reticulin: differentiates fibroma (individual pericellular reticulin staining pattern) from diffuse type of adult granulosa cell tumor (nested reticulin staining pattern)
Negative stains
- CD10 (Int J Gynecol Pathol 2007;26:359)
- Desmin
- Caldesmon
- CD99 (Am J Surg Pathol 2009;33:354)
- Calretinin: positive in 25% of cases, often focal or weak (Am J Surg Pathol 2009;33:354, Am J Surg Pathol 2011;35:484)
- S100 and CD34: occasionally positive (Am J Surg Pathol 2008;32:884)
Electron microscopy description
- Numerous thin, elongated cells with intercommunicating cytoplasmic processes admixed with abundant collagen fibrils (Cancer 1971;27:438)
- Fibrils appear grouped in bundles with a crossbanding pattern composed of a light band bound by two thin dark bands (recurring at intervals of 600 Å)
- Cells have indistinct cell borders and are compressed by collagenous stroma
- Elongated and thin nuclei with marked peripheral heterochromatin condensation
- Scant cytoplasm containing few mitochondria and scant endoplasmic reticulum
Molecular / cytogenetics description
- Trisomy or tetrasomy 12 (Ann Pathol 2001;21:393, Genes Chromosomes Cancer 1990;2:48, Gynecol Oncol 1990;38:28)
- Rarely, IDH1 mutations (Histopathology 2013;62:667)
- Loss of heterozygosity at 9q22.3 (PTCH1) and 19p13.3 (STK11) in cellular fibromas (Hum Pathol 2005;36:792)
- No or rare FOXL2 mutations (Am J Surg Pathol 2013;37:1450, Int J Gynecol Pathol 2018;37:305)
Sample pathology report
- Right ovary and fallopian tube, salpingo-oophorectomy:
- Ovary: fibroma
- Fallopian tube: unremarkable
Differential diagnosis
- Diffuse adult granulosa cell tumor (GCT):
- Typically see the other patterns of granulosa cell tumor
- Diffusely positive for inhibin and calretinin
- Nested reticulin staining pattern (Int J Gynecol Pathol 2018;37:305)
- FOXL2 mutations (Am J Surg Pathol 2011;35:484, N Engl J Med 2009;360:2719)
- Thecoma:
- May present with estrogenic manifestations, including endometrial carcinoma
- Diffuse or rarely, lobulated or nested growth
- Uniform tumor cells with abundant pale gray cytoplasm and indistinct cell membranes imparting a syncytial appearance
- Ovoid to round nuclei, with or without nucleoli or nuclear grooves
- None to minimal mitotic activity
- With or without hyaline plaques, calcifications, adipose metaplasia, small clusters of steroid type cells with eosinophilic to clear cytoplasm (Am J Surg Pathol 2014;38:1023)
- Rarely, scattered pleomorphic bizarre nuclei due to degenerative changes (Int J Gynecol Pathol 1983;1:325, Am J Surg Pathol 2014;38:1023)
- Usually positive for inhibin, calretinin and other sex cord markers
- Sclerosing stromal tumor:
- Often occurs in women in their third to fourth decades
- Alternating cellular and paucicellular areas with prominent staghorn vasculature
- Pseudolobulation and biphasic population of cells (luteinized and spindled)
- Usually positive for inhibin and calretinin
- Leiomyoma:
- Endometrial stromal tumor, low grade:
- Typical features of low grade endometrial stromal neoplasia, including permeative growth and arteriole-like vessels
- Diffusely positive for CD10
- With or without characteristic gene fusions such as JAZF1-SUZ12 (Orphanet J Rare Dis 2016;11:15)
- Metastatic gastrointestinal stromal tumor:
- Ovarian stromal hyperplasia:
- Bilateral
- Diffuse or multinodular proliferation of stromal cells
- Lacking collagenous stroma and hyaline plaques
- Massive edema:
- Unilateral or bilateral
- No well defined mass
- Proliferation of stromal cells with marked intercellular edema
- Entrapment of preexisting ovarian structures (follicles, corpora lutea or albicantia)
- Fibromatosis:
- Unilateral or bilateral
- No well defined mass
- Proliferation of stromal cells with abundant dense collagen
- Entrapment of preexisting ovarian structures
- Fibrosarcoma:
- Exceptionally rare and no longer considered a distinct WHO entity
- Hypercellular, composed of disorderly fascicles of spindle cells with scant cytoplasm and moderate to marked nuclear atypia, elevated mitotic activity including atypical forms (Cancer 1981;47:2663)
- Presence of ≥ 4 mitoses per 10 high power fields is not sufficient to diagnose fibrosarcoma in the absence of significant cytologic atypia (Am J Surg Pathol 2006;30:929)
- With or without necrosis and hemorrhage
- Focally positive for calretinin or inhibin, negative for CD10 (Am J Surg Pathol 2002;26:1477, Int J Gynecol Pathol 2007;26:359)
Additional references
Board review style question #1
Microscopic examination of an 8 cm unilateral ovarian mass demonstrates a densely cellular neoplasm composed of intersecting fascicles of spindle cells with mild cytologic atypia and approximately 9 mitotic figures per 10 high power fields. Reticulin staining shows pericellular staining pattern and molecular testing is negative for FOXL2 mutation.
What is the most likely diagnosis?
- Fibroma
- Fibrosarcoma
- Leiomyoma
- Leiomyosarcoma
- Mitotically active cellular fibroma
Board review style answer #1
Board review style question #2
You receive an intraoperative consultation for bilateral multinodular ovarian masses in a 16 year old patient. Microscopic examination demonstrates bland, monomorphic spindled cells within a collagenous stroma.
Mutation of which of the following genes is most likely associated with this entity?
Mutation of which of the following genes is most likely associated with this entity?
- FOXL2
- HMGA2
- JAZF1
- PTCH
- Vimentin
Board review style answer #2
D. PTCH. Bilateral ovarian fibroma in a young patient is most likely associated with Gorlin syndrome.
Comment Here
Reference: Fibroma
Comment Here
Reference: Fibroma