Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Fatima S, Ud Din N. Pilomatricoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticpilomatrixoma.html. Accessed October 5th, 2025.
Definition / general
- Pilomatricoma is a benign skin adnexal tumor originating from hair matrix and cortex
Essential features
- Benign skin adnexal tumor originating from hair matrix and cortex
- Most commonly occurs in head and neck, extremities and trunk in children
- Grossly appears as circumscribed hard dermal tumor with cheesy material
- Most cases behave indolently without recurrences
Terminology
- Pilomatrixoma
- Calcifying epithelioma of Malherbe (not recommended)
ICD coding
- ICD-O: 8110/0 - pilomatrixoma, NOS
- ICD-11: 2F22 & XH9E37 - benign neoplasms of epidermal appendages & pilomatricoma, NOS
Epidemiology
- Pilomatricoma, being the most common adnexal neoplasm in children, favors young age (Actas Dermosifiliogr 2010;101:771)
- However, a wide age range has been described from 3 months to 93 years
- Females are affected slightly more than males
- Usually solitary but multiple lesions can occur (Int J Dermatol 2017;56:1032)
Sites
- Head and neck are the most common sites of involvement, followed by upper and lower extremities and then trunk
- Ear (J Pediatr 2011;158:511, Ear Nose Throat J 2013;92:34)
- Eyelid (Int J Trichology 2011;3:31)
- Digits
- Male breast (Breast J 2019;25:1012)
Pathophysiology
- Pilomatricoma development is associated with mutations in CTNNB1 gene located in the exon 3 region encoding beta catenin, a 92 kDa molecule involved in cell - cell adhesion
- As an integral component of Wnt signaling pathway, beta catenin monitors cell proliferation, differentiation and survival
- Beta catenin expression in hair matrix during human embryogenesis signifies its importance in hair follicle development and thus pilomatricoma origin
- BCL2 oncoprotein is also implicated in its development (Arch Pathol Lab Med 2014;138:759)
Etiology
- Although pilomatricoma are usually not hereditary, familial cases have been recognized
- Familial forms have been seen in myotonic dystrophy Curschmann-Steinert (an uncommon autosomal dominant disorder characterized by hypotonia, muscle wasting, cataracts, hypogonadism, progressive mental retardation and frontal baldness), familial adenomatous polyposis related syndromes (including Gardner syndrome), Turner syndrome, Rubinstein-Taybi syndrome, trisomy 9, gliomatosis cerebri (Paller: Hurwitz Clinical Pediatric Dermatology - A Textbook of Skin Disorders of Childhood and Adolescence, 5th Edition, 2015, Pediatr Dermatol 2020;37:9, An Bras Dermatol 2020;95:619, Pediatr Dermatol 2009;26:75)
- Rare association with Kabuki syndrome has also been described as characterized by ectodermal abnormalities (Pediatr Dermatol 2013;30:253)
- Multiple giant pilomatricoma were reported with familial Soto syndrome, panhypopituitarism, MYH associated polyposis and DICER1 syndrome (Pediatr Dermatol 2008;25:122)
- Constitutional mismatch repair deficiency (CMMRD) syndrome, biallelic mutations in DNA mismatch repair genes (MLH1, MSH2, MSH6 or PMS2) (Pediatr Dermatol 2020;37:1139)
- Germline mutation in PLCD1 has been identified as the genetic cause of familial multiple pilomatricomas (FMPs); PLCD1 is essential for maintaining skin function (J Invest Dermatol 2021;141:533)
Clinical features
- Pilomatricoma presents as slow growing, dermal based, asymptomatic nodule measuring 0.5 - 3 cm (Arch Argent Pediatr 2019;117:340)
- Flesh colored to white, firm papules / nodules that may have an overlying pink to blue hue (Paller: Hurwitz Clinical Pediatric Dermatology - A Textbook of Skin Disorders of Childhood and Adolescence, 5th Edition, 2015)
- Pain, pruritus or discharge can occur at times (Arch Craniofac Surg 2020;21:288)
- Occasionally, skin ulceration may be seen simulating squamous cell carcinoma (Int J Trichology 2012;4:280)
- Rare appearances may include bullous / anetodermal / lymphagiectatic, giant, perforating, pigmented lesions, keloid-like (J Cutan Pathol 2009;36:67, Indian J Dermatol Venereol Leprol 2020;86:55, Pediatr Dermatol 2013;30:e68, Int J Clin Exp Pathol 2013;6:1890, Case Rep Dermatol 2022;14:230)
- Recently a pseudocystic presentation has been documented (Australas J Dermatol 2021;62:60)
Diagnosis
- Generally very hard, owing to calcification; skin lesions that are calcified tend to display positive teeter totter and tent signs
- Teeter totter sign is observed when applying downward pressure to one end of the lesion causes the other end to spring upwards in the skin
- Tent sign appears when the skin overlying the lesion is stretched, revealing multiple facets and angles, resembling a tent
- Clinical examination alone may not be diagnostic (Am J Dermatopathol 2018;40:631)
- Imaging studies ultrasound, computed tomography and magnetic resonance imaging are helpful; ultrasonography has a high positive predictive value (95.56%) (Arch Craniofac Surg 2020;21:288)
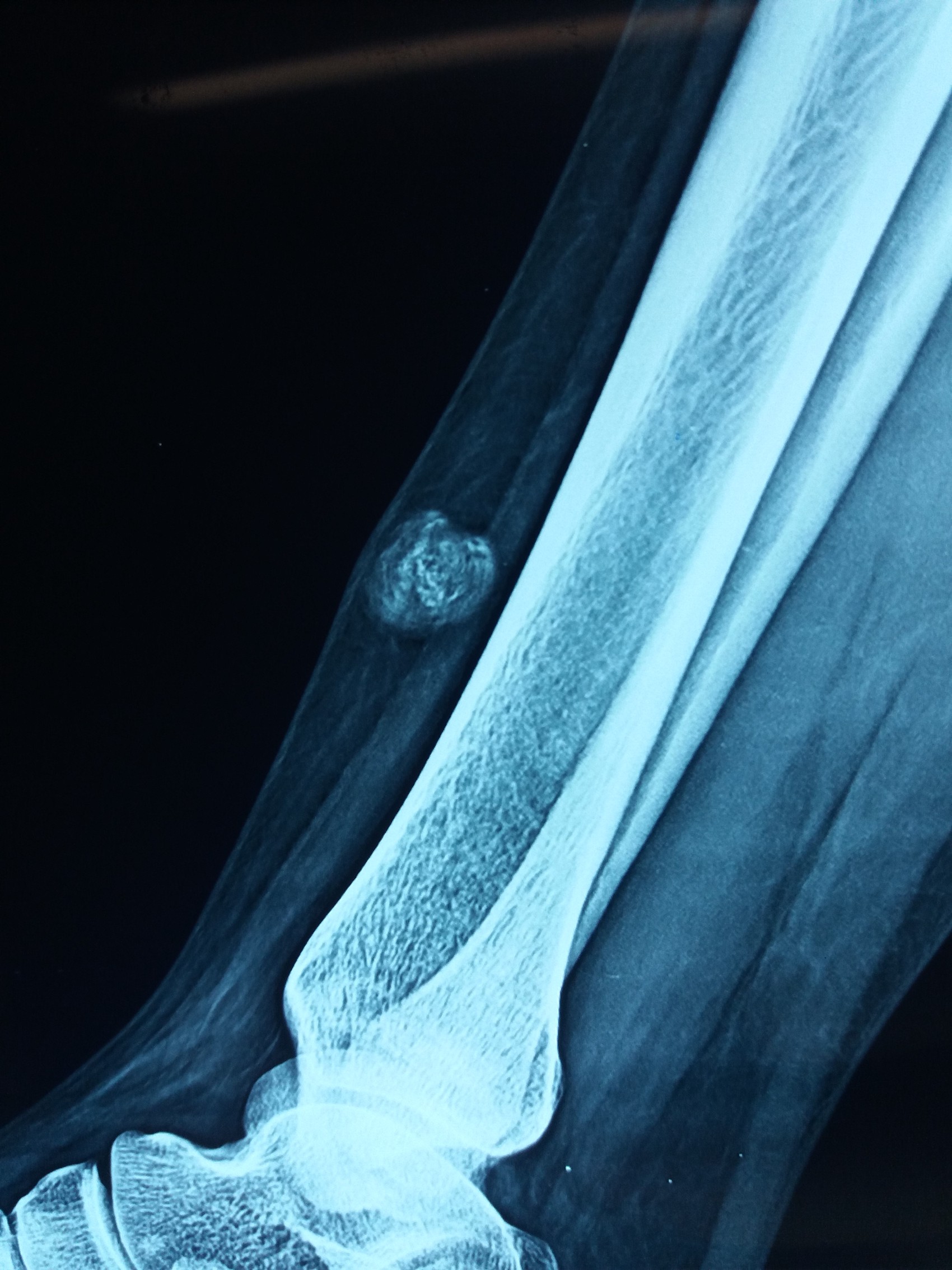
Radiology description
- Ultrasound
- Pilomatricoma present as heterogeneous, well demarcated, hypoechoic mass between the deep dermis and the subcutis on ultra high frequency ultrasonography
- Most common features are internal echogenic foci (calcifying), hypoechoic rim and posterior shadowing (J Ultrasound 2008;11:76, Front Med (Lausanne) 2021;8:673861)
- CT scan
- Appear well demarcated, subcutaneous masses with various levels of calcification
- Inflammatory cell infiltration into fat may result in peritumoral fat stranding on fat suppressed, T2 weighted images (Radiol Med 2019;124:1049)
Radiology images
Prognostic factors
- Rare tumor recurrence of ~1 - 2% is reported with incomplete primary excision (Arch Craniofac Surg 2020;21:288, Am J Dermatopathol 2018;40:631)
- In rare cases, can undergo malignant transformation
- Most of the reported cases of malignant transformation have occurred in adults, typically in their 40s or 50s
- However, there have been rare cases reported in children as well
- Risk of malignant transformation appears to be higher in large or longstanding pilomatricoma and in those that have been previously treated with radiation therapy (J Dermatol 2010;37:735)
Case reports
- 6 year old girl with a painful swelling over the left buttock (Ann Med Surg (Lond) 2022;84:104847)
- 9 year old girl with keloid-like tumor on posterior part of the auricle (Case Rep Dermatol 2022;14:230)
- 34 year old pregnant woman with rapidly growing giant parotid tumor (Arch Craniofac Surg 2020;21:176)
- 69 and 76 year old men with melanocytic matricoma (JAAD Case Rep 2023;33:51)
- 87 year old woman with a scalp tumor (Cureus 2022;14:e30661)
Treatment
- Surgical excision is curative
Clinical images
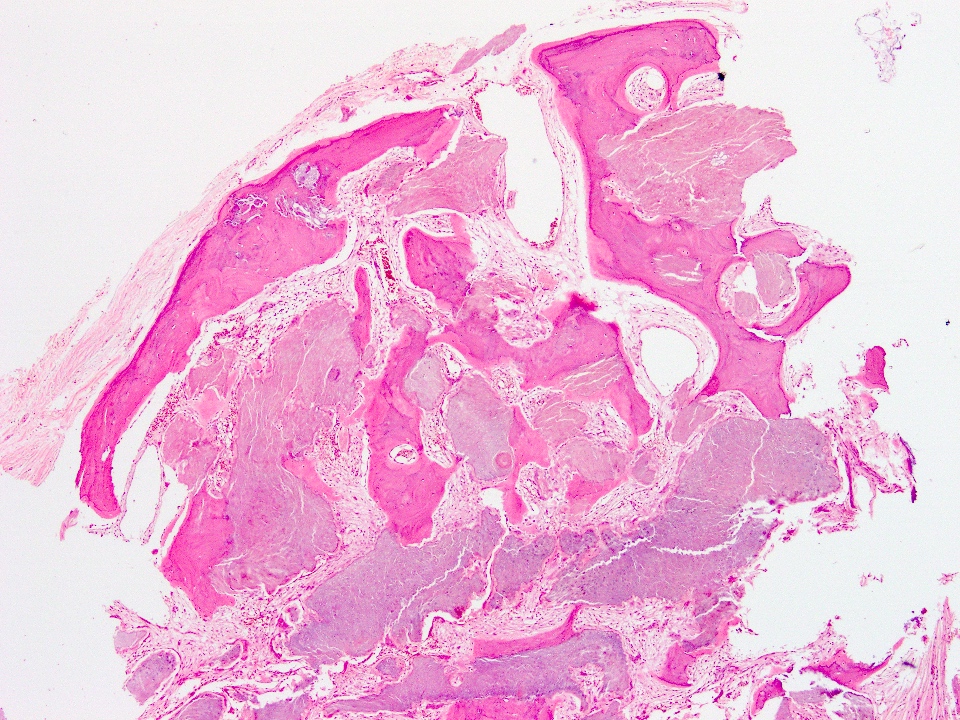
Gross description
- Hard calcified, may be nodulocystic
- Circumscribed edges, lobulated
- Keratinous material appears cheesy while calcified areas are gritty
- Rare ossified area will be difficult to cut
Gross images
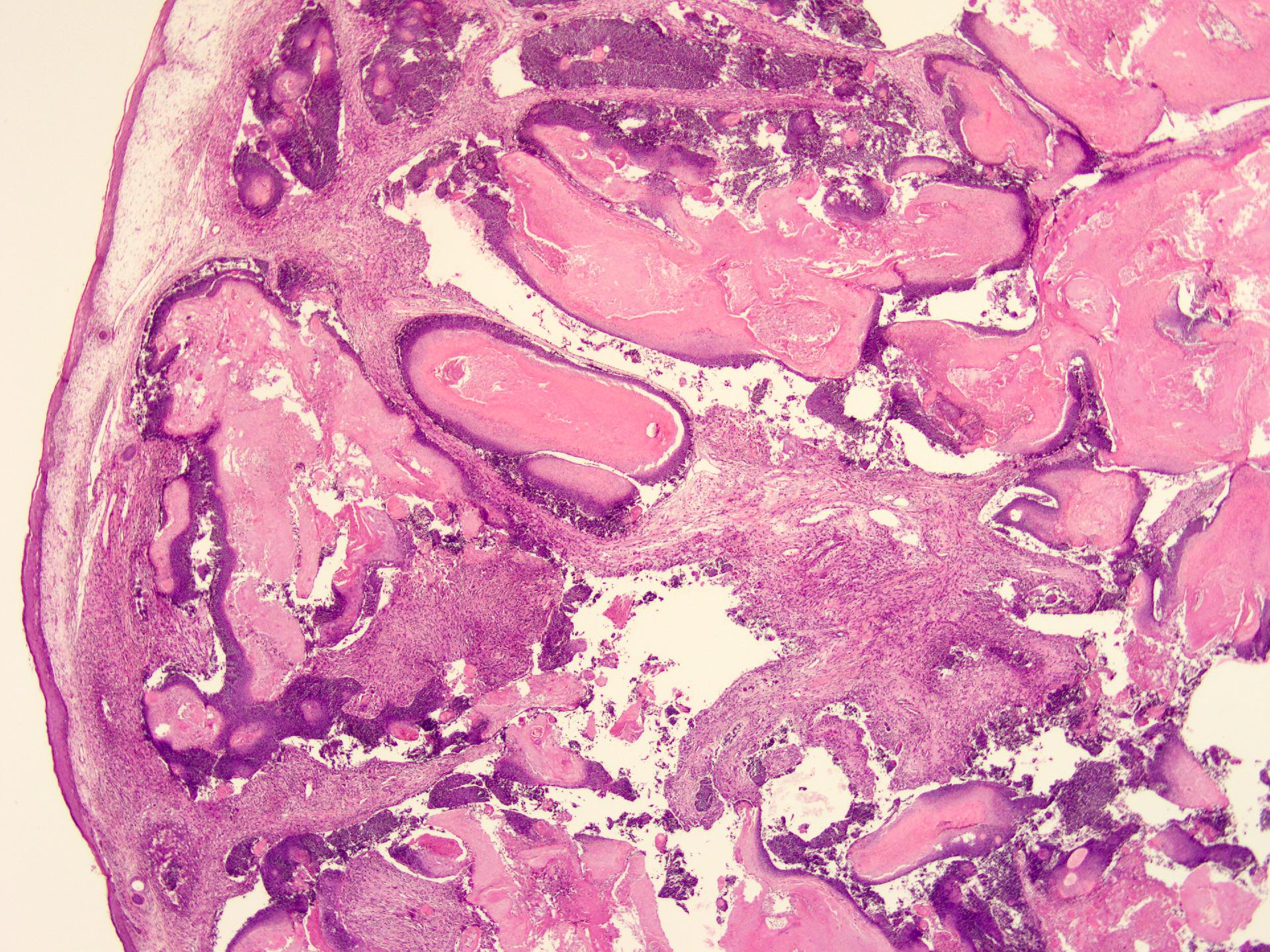
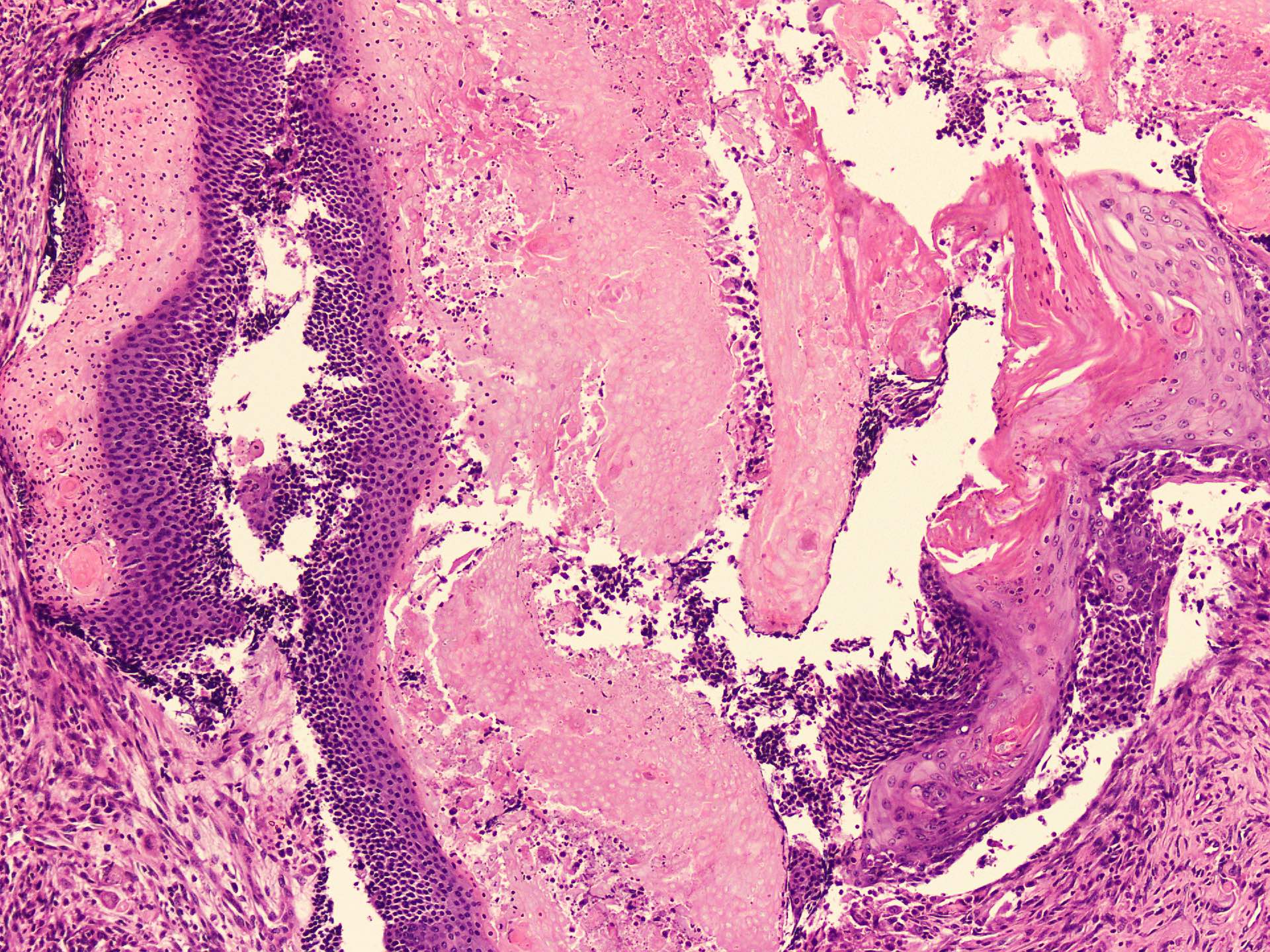
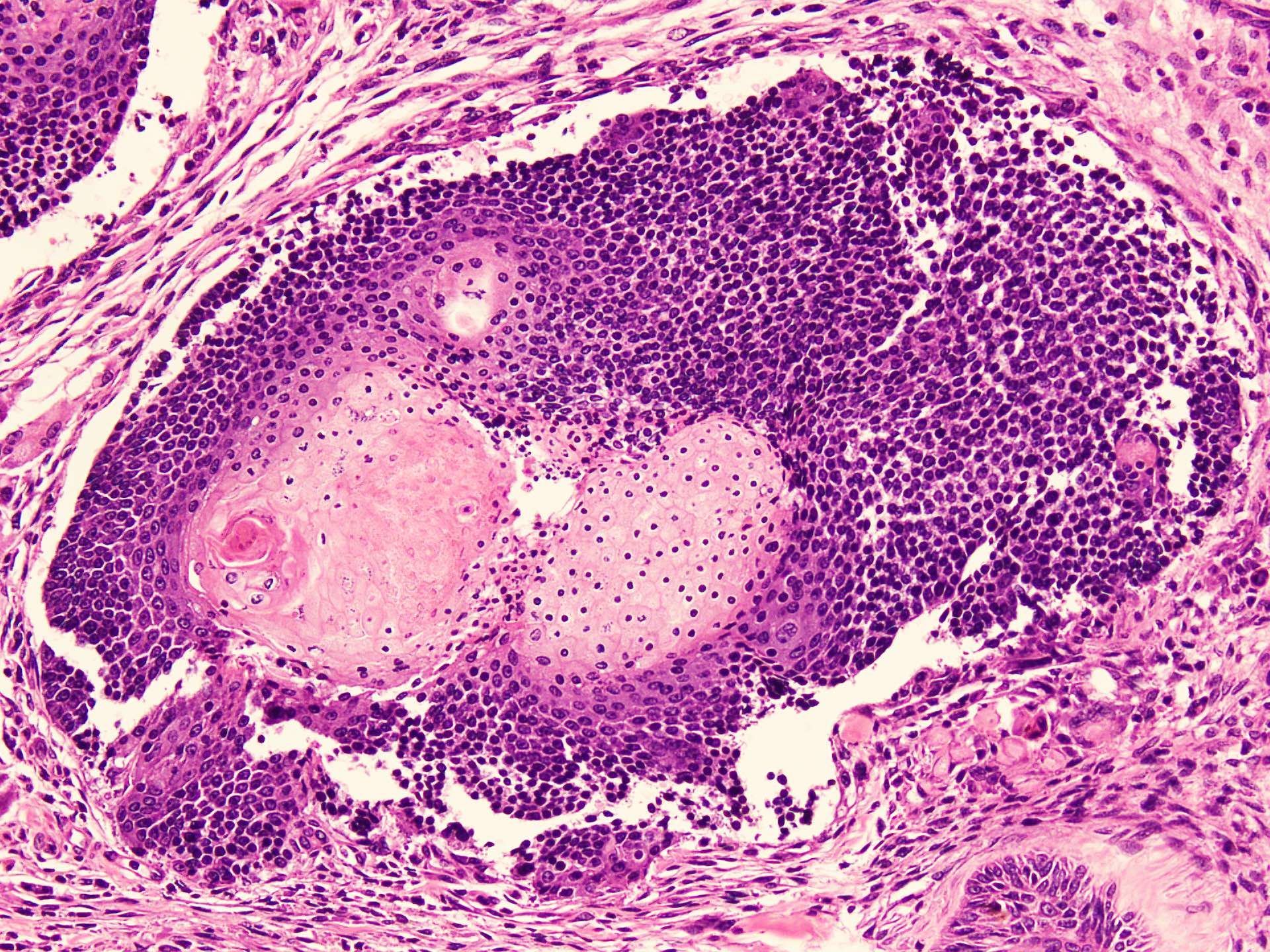
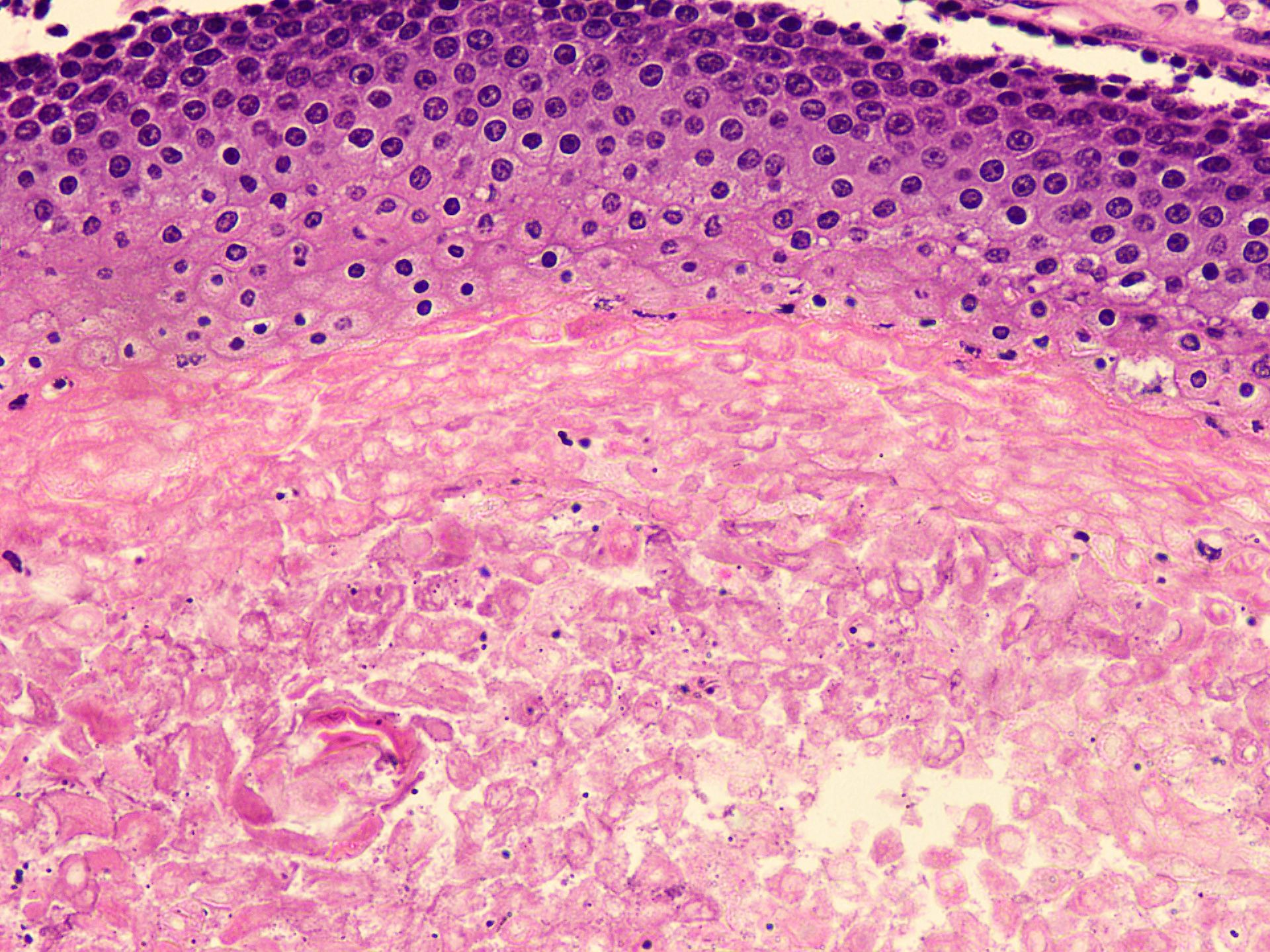
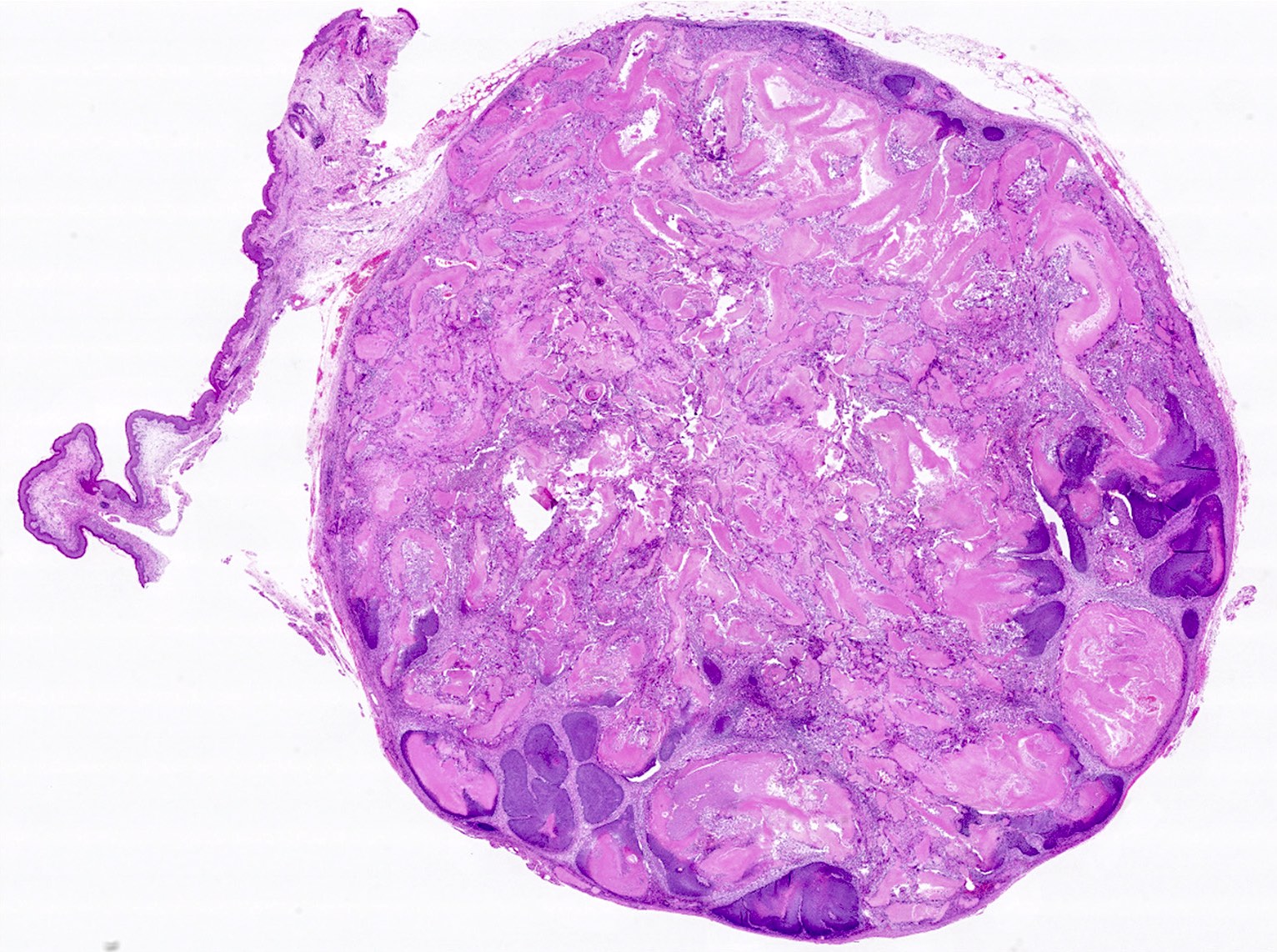
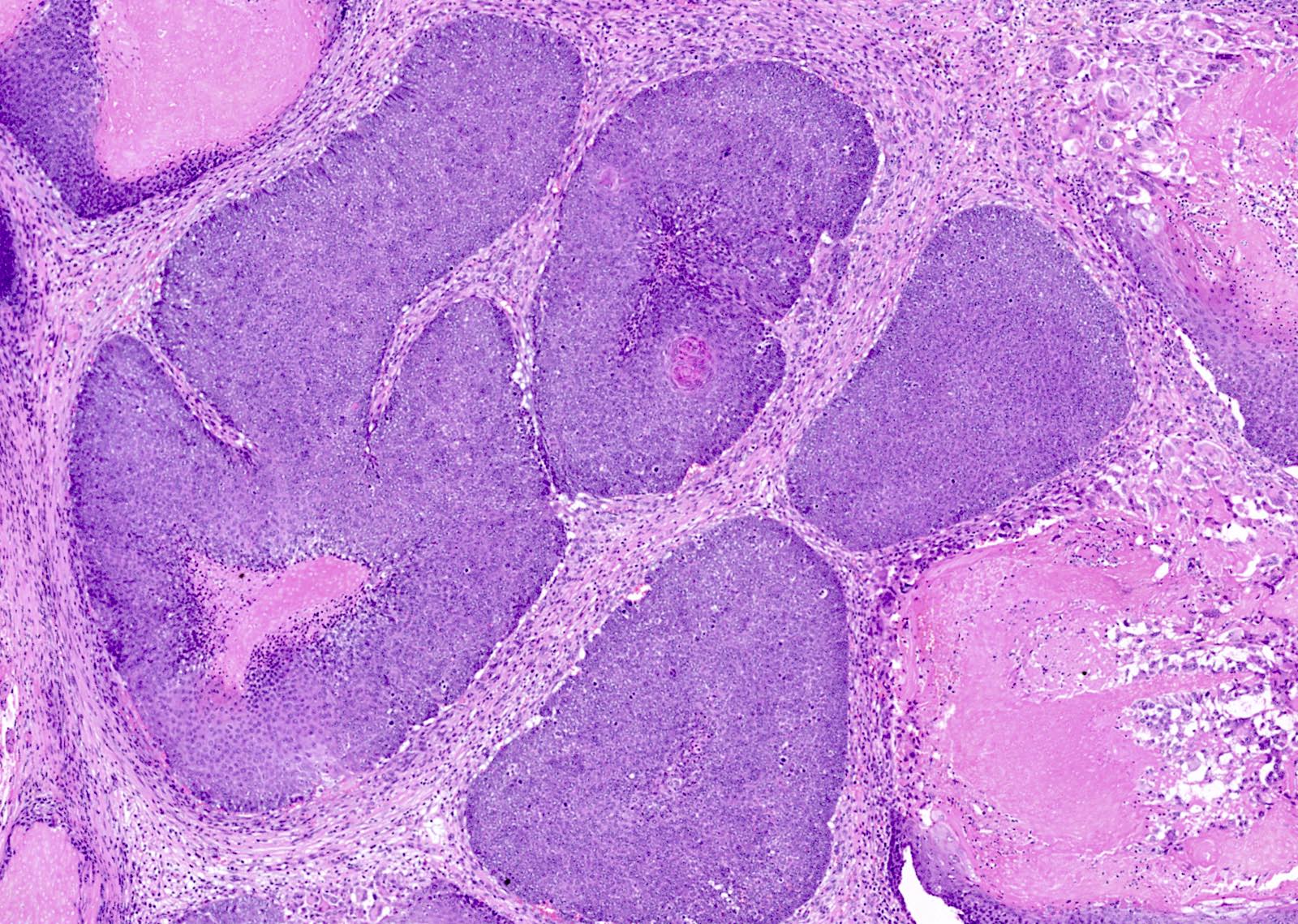
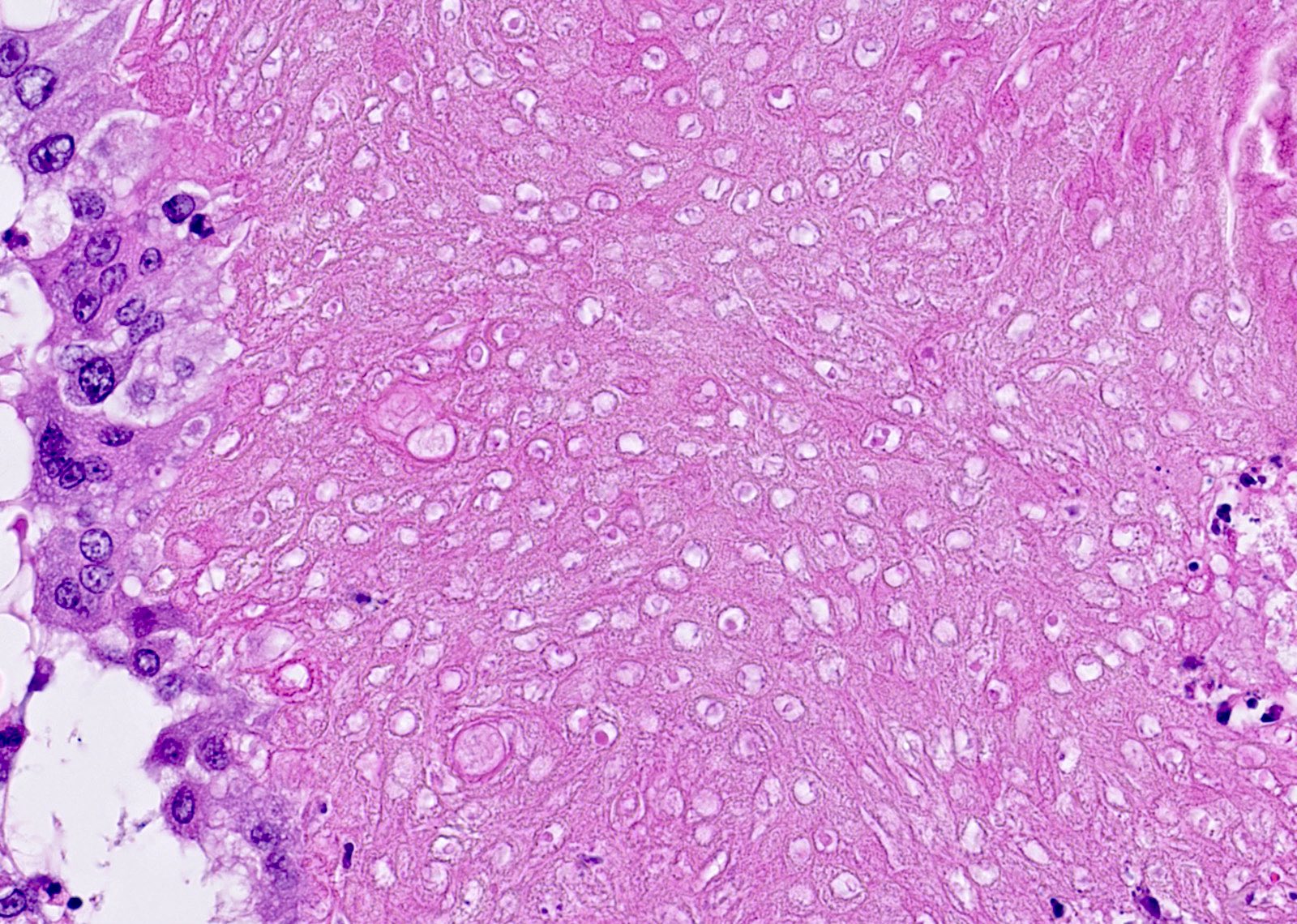
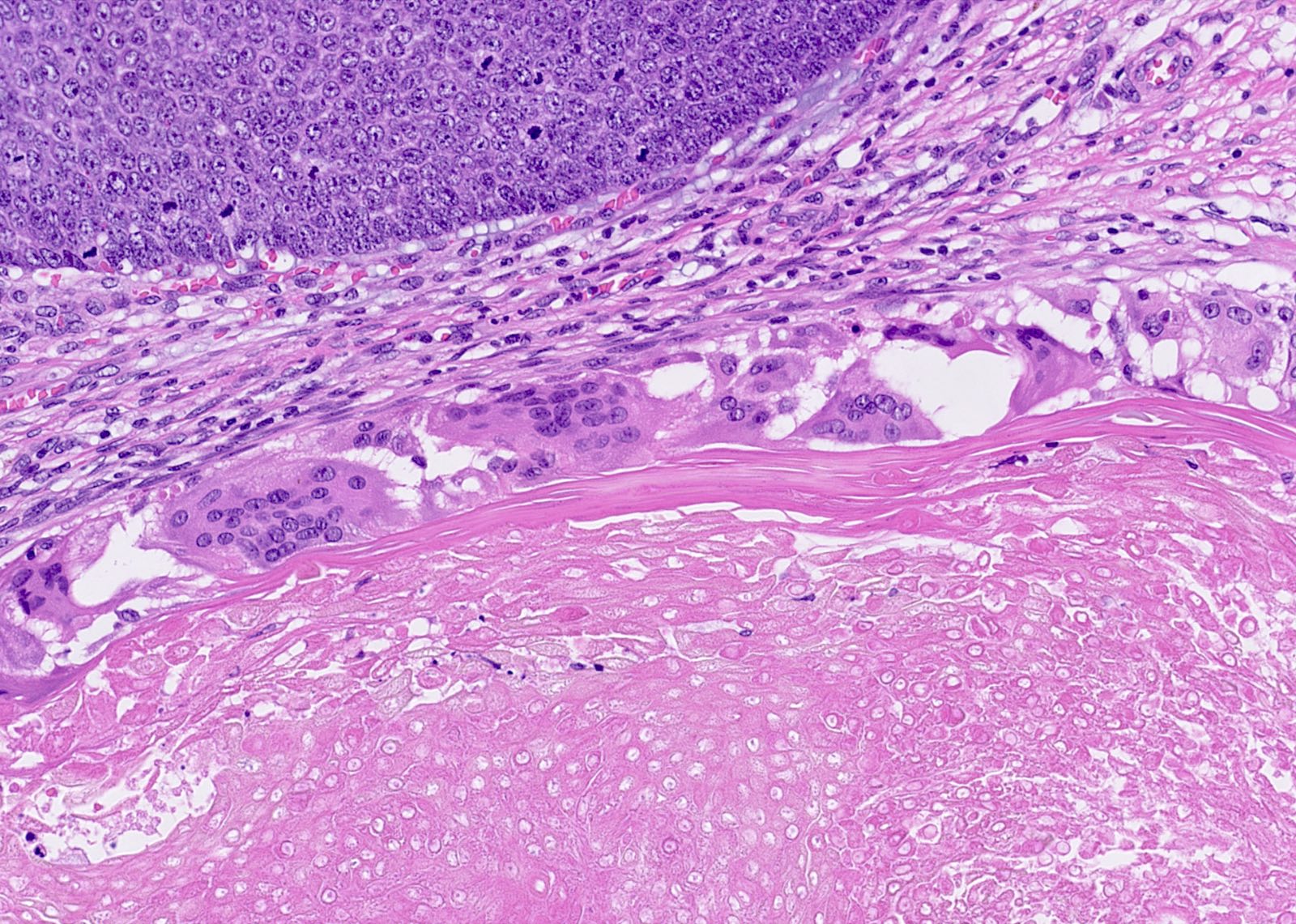
Microscopic (histologic) description
- Lobulated and circumscribed dermal based neoplasm
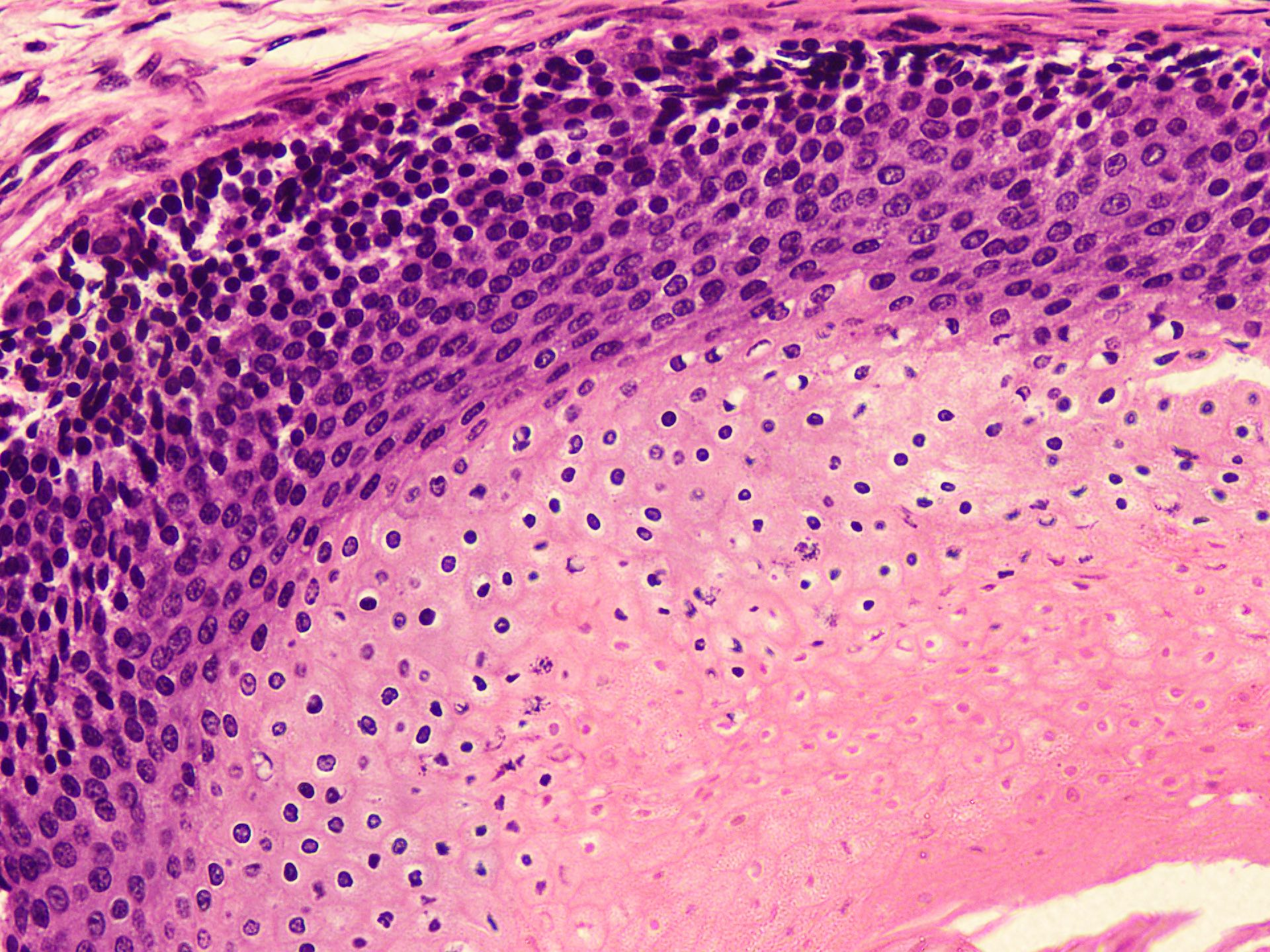
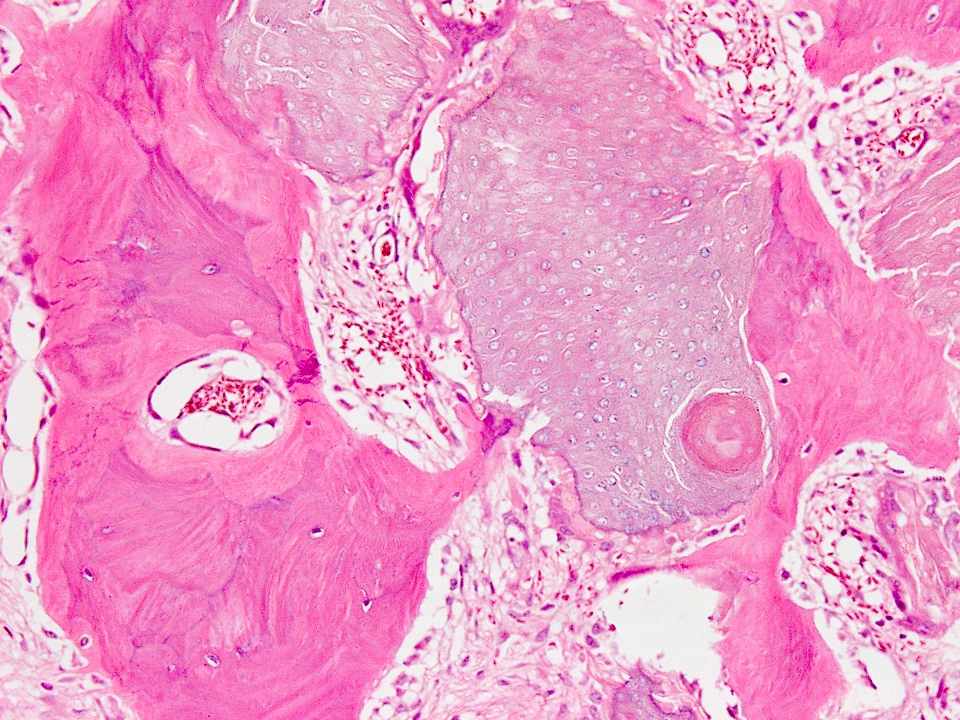
- Islands of basaloid cells exhibiting abrupt keratinization, without intervening granular layer (trichilemmal keratinization)
- Ghost / shadow cells, may predominate
- Basaloid cells show mitotic activity; however, abnormal mitoses are absent
- Intermediary cells progressively more eosinophilic cytoplasm, with pyknotic nucleus
- Tumor keratin may elicit inflammatory response with foreign body giant cells, granuloma, cholesterol clefts and calcification
- Uncommonly metaplastic bone formation is present along with extramedullary hematopoiesis (Cureus 2022;14:e30661)
- Hemosiderin, melanin and amyloid deposition has been reported
- Occasionally tumors exhibit some atypical features that suggest a potential for malignancy but does not fully meet the criteria for pilomatrix carcinoma; these features include a focal infiltrative pattern at the periphery, variable cytological atypia, increased mitotic rate (up to 5/high power field) and irregular foci of central necrosis (Case Rep Dermatol 2021;13:98)
- Histological patterns: pigmented, proliferating, nodulocystic, perforating, bullous, pilomatricoma with osseous metaplasia, melanocytic matricoma (JAAD Case Rep 2023;33:51)
Microscopic (histologic) images
Contributed by Nasir Ud Din, M.B.B.S. and Andrey Bychkov, M.D., Ph.D.
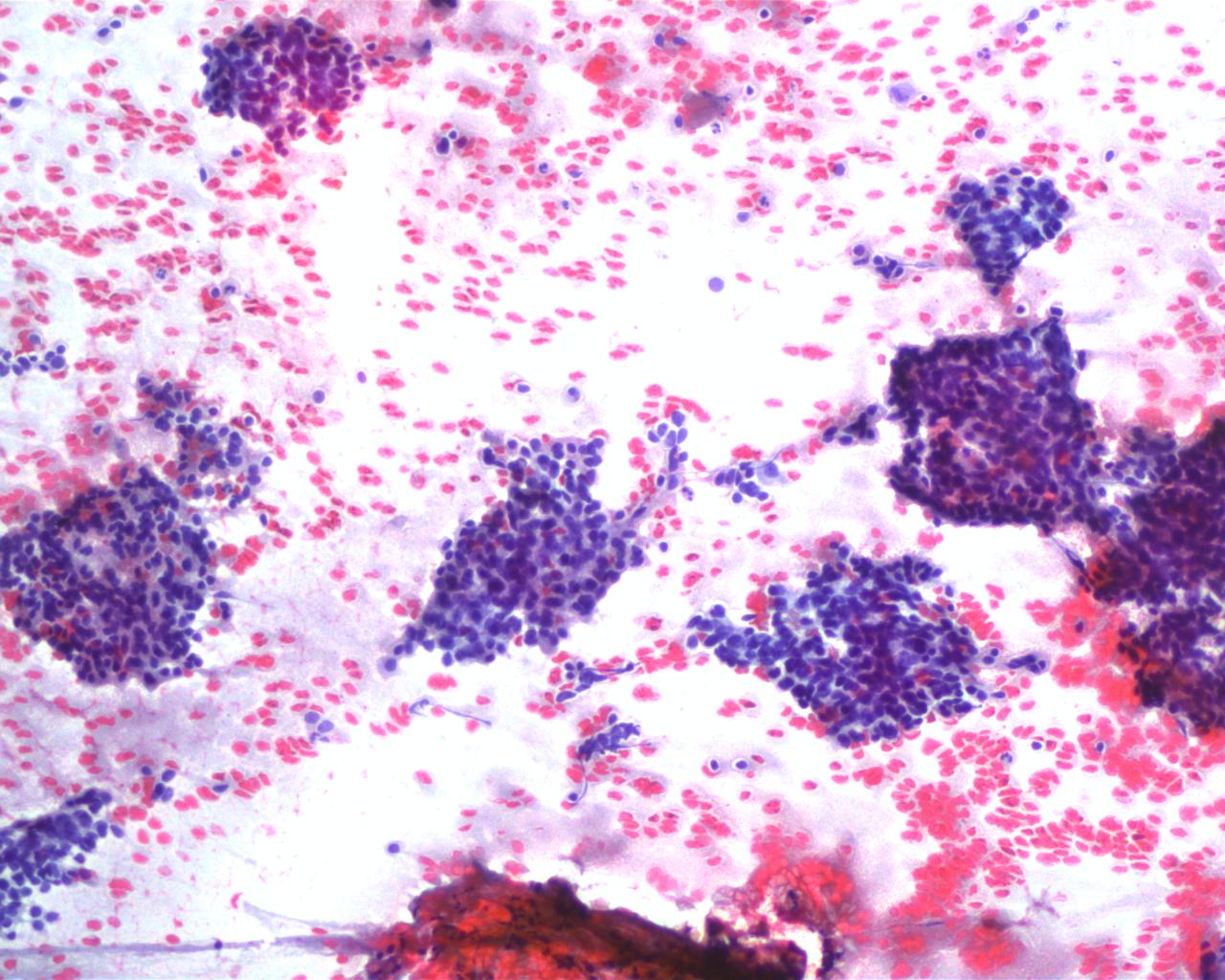
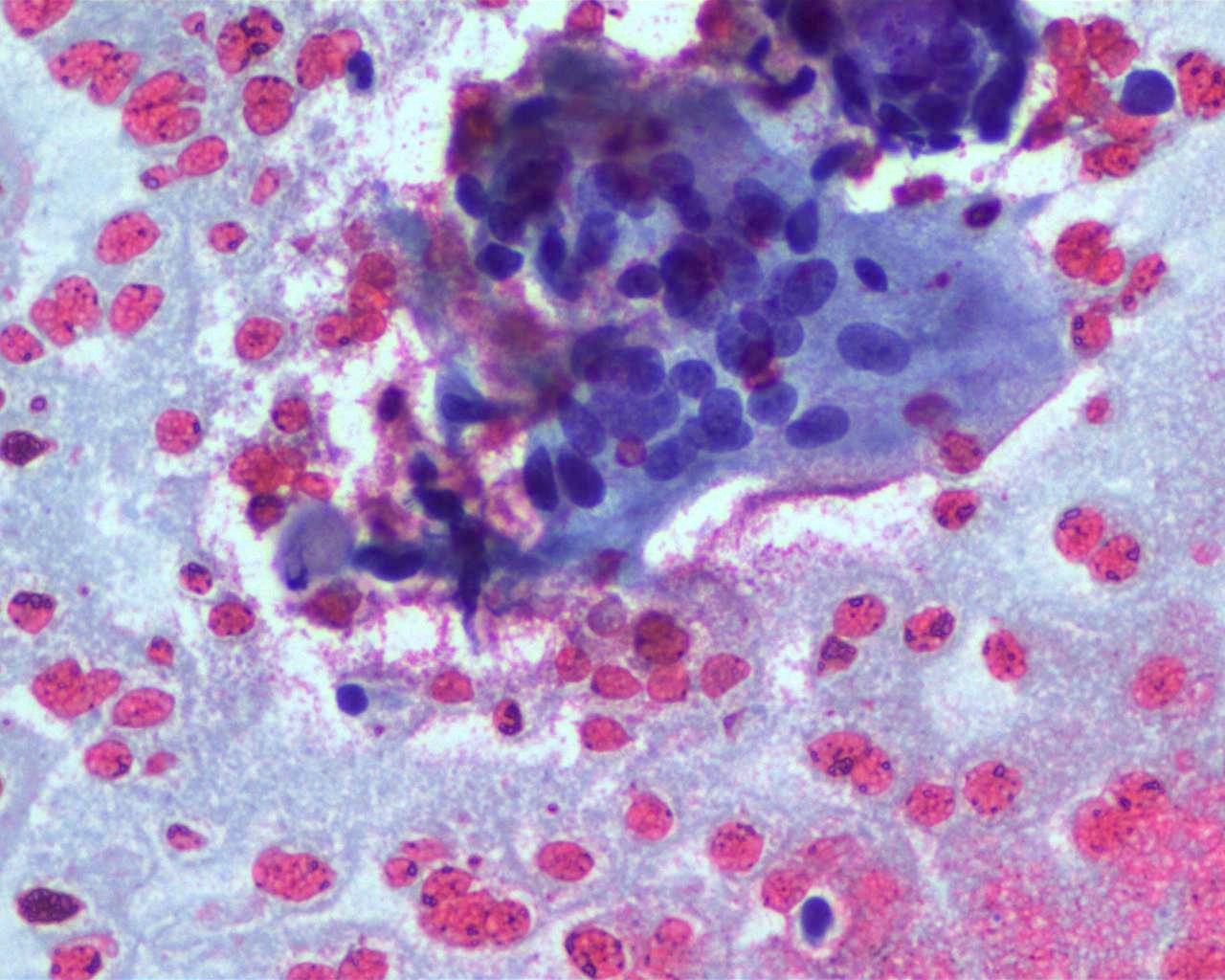
Cytology description
- Clusters of basaloid cells with round to ovoid nuclei, nucleated squamous cells and anucleated squames as well as clusters of shadow cells are consistent with the characteristics typically seen in pilomatricoma (Diagn Pathol 2018;13:65)
- Foreign body giant cells may be present; markedly calcified lesion may yield scanty material (Int J Trichology 2012;4:280)
- Shadow cells are specialized cells, the result of a process called shadow cell degeneration, in which the cells lose their nuclei and undergo a series of structural changes
- Cytoplasm of shadow cells often contains basophilic (blue) granules, which are thought to represent remnants of the cellular organelles
Cytology images
Positive stains
- Pancytokeratin, cytokeratin 5/6
- Hard keratins hHa1, hHa2 and hHa5 are positive in pilomatricoma but not in other tumors of follicular origin
- Beta catenin: nuclear and membrane positivity in basaloid cells, negative in transitional and shadow cells (J Dermatol 2010;37:735)
- BCL2
- CDX2 (Hum Pathol 2022;129:1)
- LEF1 (Childs Nerv Syst 2023;39:821)
- Cyclin D1
- ER, PR
- CD10 and CD138 (Rom J Morphol Embryol 2018;59:917)
- Connexin 43 (Cx43) gap junction protein: Cx43 expression is preserved in benign cutaneous tumors with follicular differentiation (Am J Dermatopathol 2019;41:810)
- PHLDA1 (Am J Dermatopathol 2022;44:129)
Negative stains
- BerEP4
- CK15
- Mart1 and SOX10: negative in basaloid cells (Indian J Dermatol 2021;66:525)
Electron microscopy description
- Cell differentiation and keratinization in shadow cells is similar to the process in the cortex of hair
- Shadow cells are fully keratinized that form a mantle around nuclear remnants
Videos
Diagnostic pearls of pilomatricoma in superficial biopsy
Pilomatricoma: mini tutorial
Sample pathology report
- Left cheek, excision biopsy:
- Pilomatricoma (see comment)
- Comment: There is a well circumscribed, lobulated, dermal based adnexal neoplasm comprising of many islands of basaloid cells with scattered mitoses. These cells exhibit abrupt keratinization transforming to shadow cells. Surrounding stroma has histiocytes, foreign body giant cell reaction and foci of calcification. There is no evidence of atypical mitoses, nuclear anaplasia or destructive infiltration into the surrounding tissue. Immunohistochemical stain beta catenin shows nuclear positivity in basaloid cells. Features are consistent with pilomatricoma, a benign adnexal tumor with hair matrix differentiation. The tumor is completely excised. Local recurrence is uncommon following complete excision.
Differential diagnosis
- Basal cell carcinoma:
- Sun exposed areas of skin
- Most often seen in older individuals
- May occur in children in association with basal cell nevus syndrome, xeroderma pigmentosum and organoid nevus
- Nests of basaloid cells palisade at periphery
- Stromal retraction and mucin
- High mitotic activity
- Most show connection to epidermis
- Lacks anucleate shadow cells
- BerEP4 positive
- Basal cell carcinoma with matrical differentiation:
- Typical features of basaloid cells predominate with foci of matrical differentiation
- Pilomatrix carcinoma:
- Older adults; case reports document occurrence in children and young adults, mostly de novo
- Rare cases arise from existing pilomatricoma
- Pleomorphic basaloid cells
- Prominent nucleoli
- High mitotic activity, necrosis, lymphovascular invasion (rare)
- Locally aggressive behavior, infiltrating borders
- Local recurrence common
- Metastases may rarely occur, involving regional lymph nodes and lungs
- Squamous cell carcinoma:
- Intercellular bridges
- Epidermoid keratinization
- Keratin pearl formation
- Lacks shadow cells
- Merkel cell carcinoma:
- Small cells hyper chromatic nuclei; stippled (salt and pepper) nuclear chromatin pattern
- Lacks anucleate shadow cells
- Immunoreactive for neuroendocrine markers, such as chromogranin, synaptophysin, CD56 and CD57
- Dot positivity for CK20
- Epidermal cysts of Gardner syndrome:
- Changes of pilomatricoma can occur
- Other follicular tumors showing matrical differentiation, including
- Trichoblastoma:
- Circumscribed, dermal basaloid tumor without surface connection
- Stromal induction and formation of primitive hair bulbs
- Trichoepithelioma:
- Dermal based, focal epidermal connection, branching nests of basaloid cells
- Aggregations of fibroblasts as abortive attempts to form papillary mesenchyme (papillary mesenchymal bodies)
- Small keratinous cysts
- Panfolliculoma:
- Rare, advanced follicular differentiation
- Overlap features between trichoblastoma and matricoma
- All elements of follicular differentiation
- Trichoblastoma:
- Ghost cells may also be found in noncutaneous tumors, such as calcifying cystic odontogenic tumor (CCOT), dentinogenic ghost cell tumor, odontogenic ghost cell carcinoma and craniopharyngioma; occasionally, these cells are also seen in odontomas, ameloblastoma, adenomatoid odontogenic tumor and ameloblastic fibroma (J Pharm Bioallied Sci 2015;7:S142)
Additional references
Practice question #1
A 5 year old girl presented with a hard nodule on her arm. Fine needle aspiration yielded clusters of epithelial cells with scant cytoplasm, some anucleated and nucleated squamous cells. Focal calcified debris was noticed. Which immunohistochemical stain is helpful in diagnosis?
- Beta catenin
- CK5/6
- Ki67
- p40
- p53
Practice answer #1
A. Beta catenin. Beta catenin is the defining molecular alteration in pilomatricoma and nuclear staining of basaloid cells is diagnostic. Answers B and D are incorrect because CK5/6 and p40 expression is also seen in squamous cell carcinoma and some basal cell carcinoma. Answer E is incorrect because p53 aberrant expression is significant for malignant behavior and does not help in the identification of pilomatixoma. Answer C is incorrect because Ki67 will show increased staining in basaloid cells and other inflammatory cells (if present in the adjacent stroma). Identification of abrupt keratinization and ghost cells is based on H&E section.
Comment Here
Reference: Pilomatrixoma
Comment Here
Reference: Pilomatrixoma
Practice question #2
A 20 year old man had multiple gradually enlarging, itchy scalp tumors for the past 2 years. On examination it was hard nodule and overlying skin was stretched, revealing multiple facets and angles resembling a tent. The excision specimen revealed features as shown in the photomicrograph above. The patient's history is significant for total colectomy a year ago with more than 100 polyps. What is the patient suffering from?
- Gardner syndrome
- Gliomatosis cerebri
- Myotonic dystrophy
- Rubinstein-Taybi syndrome
- Turner syndrome
Practice answer #2
A. Gardner syndrome. The photomicrograph shows a classic picture of basaloid cells and shadow cells, consistent with pilomatricoma. Multiple lesions and past history of total colectomy with more than 100 polyps favors familial adenomatous polyposis related syndrome, specifically Gardener syndrome. Multiple pilomatricoma (6 or more) are significant for association with various syndromes, most involving myotonic dystrophy and familial adenomatous polyposis related syndromes (including Gardner syndrome). Other syndromes include Turner syndrome, Rubinstein-Taybi syndrome, Sotos syndrome (relatively scant) and Kabuki syndrome.
Answer C is incorrect because myotonic dystrophy is part of a group of autosomal dominant disorders with high penetrance that show skeletal and respiratory muscle weakness and myotonia. Other findings may be cardiac muscle abnormalities and conduction defects, cataracts, daytime somnolence and endocrine disorders.
Answer E is incorrect because in Turner syndrome, patients are female and lack part or all of the second sex chromosome. Characteristic features include short stature, premature ovarian failure and high risk for various phenotypic abnormalities (e.g., high palate, nail dysplasia, low posterior hairline, widely spaced nipples, webbed neck and low set or malrotated ears), as well as other medical problems such as cardiovascular defects, skeletal anomalies and autoimmune disorders. It is suggested that growth hormone (or its effector molecule insulin-like growth factor 1) and estrogen may promote hair follicle growth and inhibit apoptosis, as well as produce pilomatricomas.
Answer D is incorrect because Rubinstein-Taybi syndrome is a rare genetic disorder characterized by mental retardation and multiple congenital anomalies. It involves broad thumbs and toes, short stature, distinctive facial features and varying degrees of intellectual disability. Low set ears, cataracts, microcephaly and cryptorchidism may also be seen.
Answer B is incorrect because gliomatosis cerebri is a diffuse growth pattern of glioma that invade multiple lobes of the brain. By definition, more than 2 brain regions have to be affected and symptoms include epilepsy, headaches and behavioral changes.
Comment Here
Reference: Pilomatrixoma
Answer C is incorrect because myotonic dystrophy is part of a group of autosomal dominant disorders with high penetrance that show skeletal and respiratory muscle weakness and myotonia. Other findings may be cardiac muscle abnormalities and conduction defects, cataracts, daytime somnolence and endocrine disorders.
Answer E is incorrect because in Turner syndrome, patients are female and lack part or all of the second sex chromosome. Characteristic features include short stature, premature ovarian failure and high risk for various phenotypic abnormalities (e.g., high palate, nail dysplasia, low posterior hairline, widely spaced nipples, webbed neck and low set or malrotated ears), as well as other medical problems such as cardiovascular defects, skeletal anomalies and autoimmune disorders. It is suggested that growth hormone (or its effector molecule insulin-like growth factor 1) and estrogen may promote hair follicle growth and inhibit apoptosis, as well as produce pilomatricomas.
Answer D is incorrect because Rubinstein-Taybi syndrome is a rare genetic disorder characterized by mental retardation and multiple congenital anomalies. It involves broad thumbs and toes, short stature, distinctive facial features and varying degrees of intellectual disability. Low set ears, cataracts, microcephaly and cryptorchidism may also be seen.
Answer B is incorrect because gliomatosis cerebri is a diffuse growth pattern of glioma that invade multiple lobes of the brain. By definition, more than 2 brain regions have to be affected and symptoms include epilepsy, headaches and behavioral changes.
Comment Here
Reference: Pilomatrixoma